Similar presentations:
Aberration of normal development and involution (andi) of thebreast
1.
Kumar sachinLa1 163(1)
2.
ANDIABERRATION OF NORMAL DEVELOPMENT
AND INVOLUTION (ANDI) OF THEBREAST
3.
Normal three phases of physiology of breast—(1)Lobular development;
(2) Cyclical hormonal modifications;
(3) Involution.
4.
First coined by LE Hughes at Cardiff breast clinic in1987
ANDI includes variety of benign breast disorders
occurring at different periods of reproductive periods
in females—early, matured and involution phase of
reproductive age group.
5.
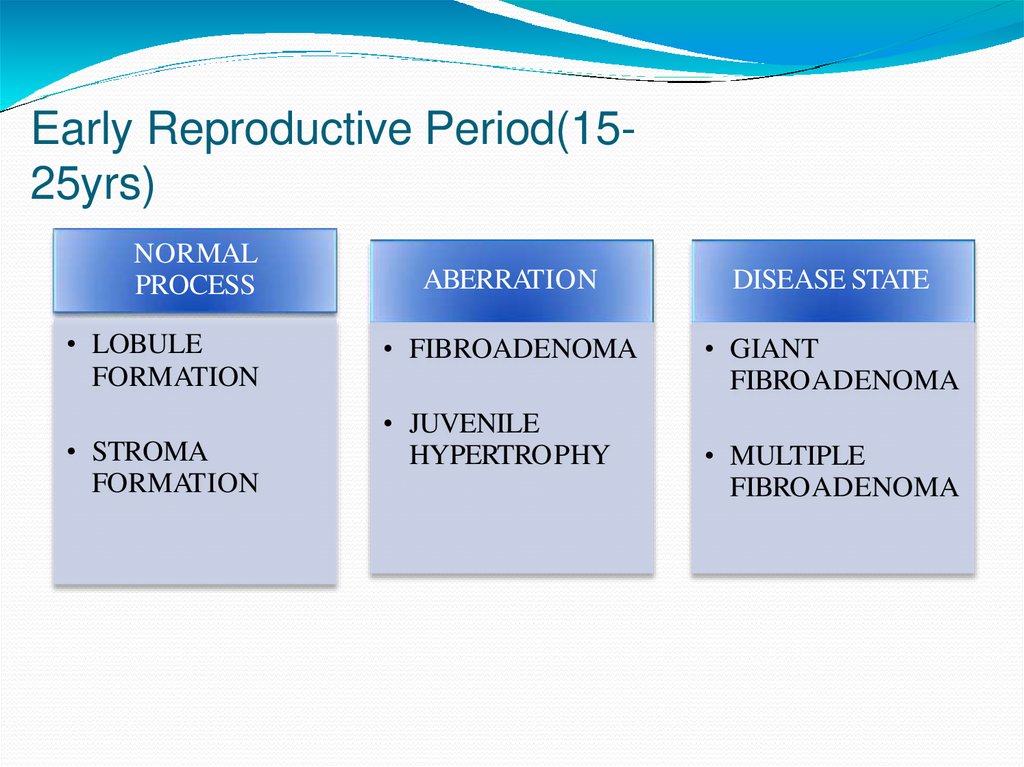
Early reproductive age group (15-25 years)Normal lobule formation may cause aberration as
fibroadenoma.
>5 cm - Giant fibroadenoma as a diseased status. It
is AND of alobule.
Normal stroma may develop juvenile hypertrophy
as aberration and multiple fibroadenoma as
diseased status.
6.
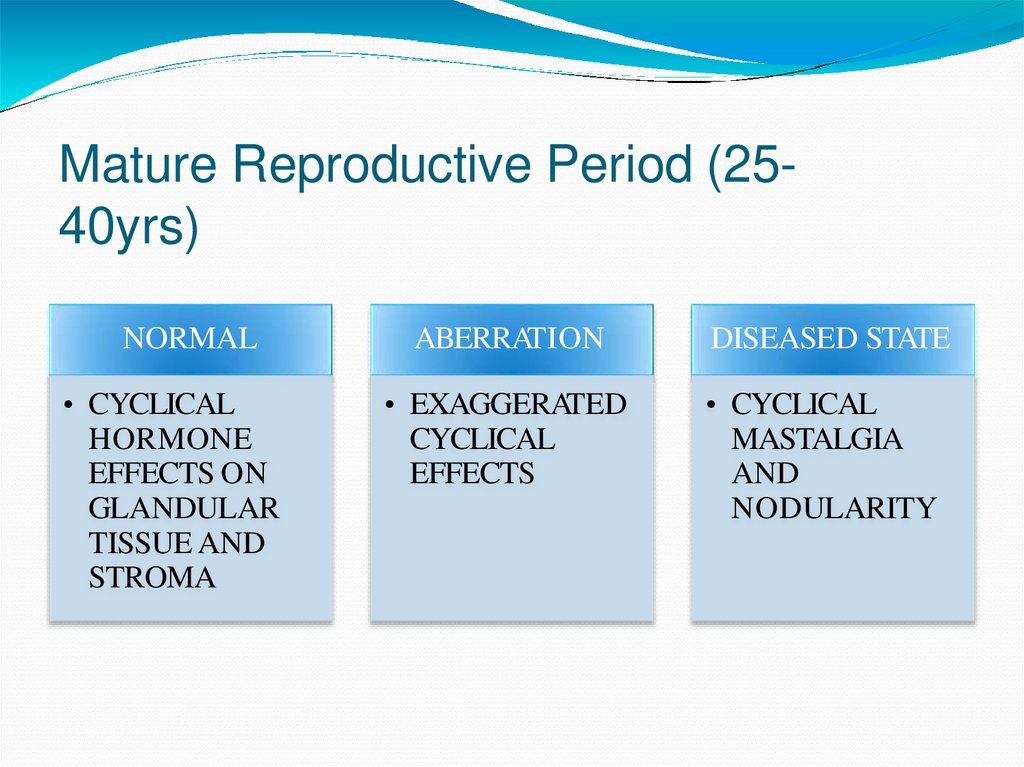
Mature reproductive age group (25-40 years):Normal cyclical hormonal effects on glands and
stroma get exaggerated by aberration causing
generalised enlargement.
Its disease is cyclical mastalgia with nodularity also
called as fibrocystadenosis.
7.
Involution age group (40-55 years):Lobular involution with microcysts, fibrosis, adenosis,
apocrine metaplasia and eventual aberrations as
macrocysts and cystic disease of breast. Macrocyst is
an aberration of normal involution (ANI). Sclerosing
adenosis is also a type of aberration.
8.
Ductal involutionAberration - ductal dilatation and nipple discharge.
Later Disease status develops with
Periductal mastitis,
Nonlactational breast abscess and
Mammary duct fistula.
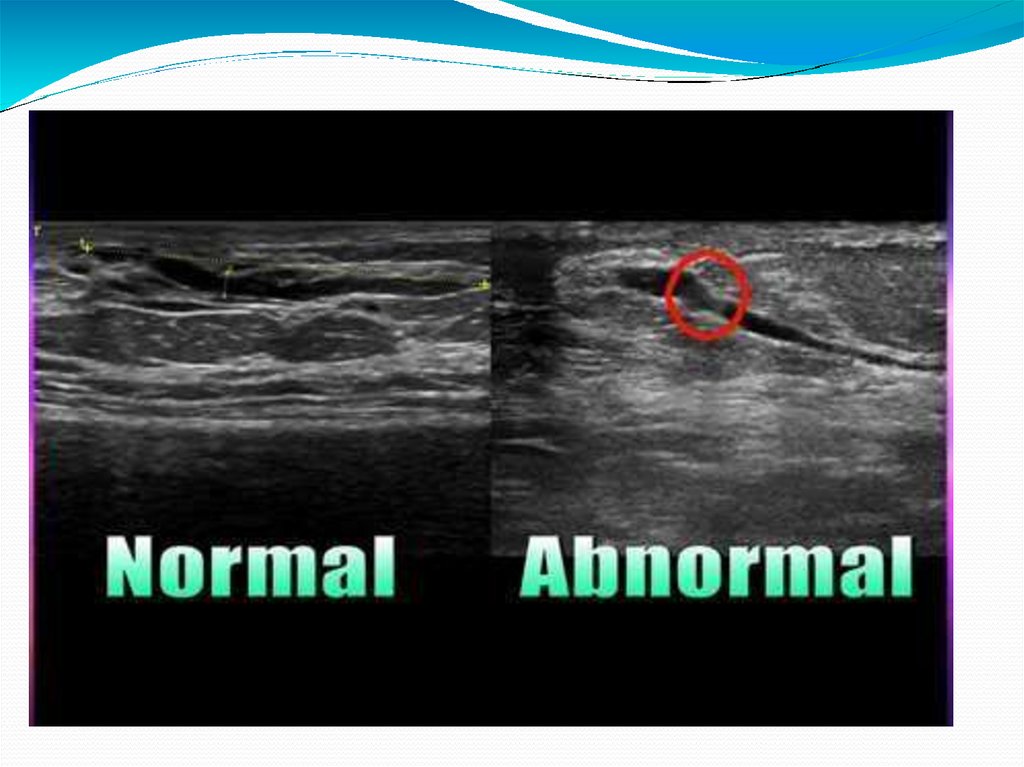
Periductal fibrosis - partial nipple retraction.
Epithelial changes leads into epithelial hyperplasia
and atypia.
9.
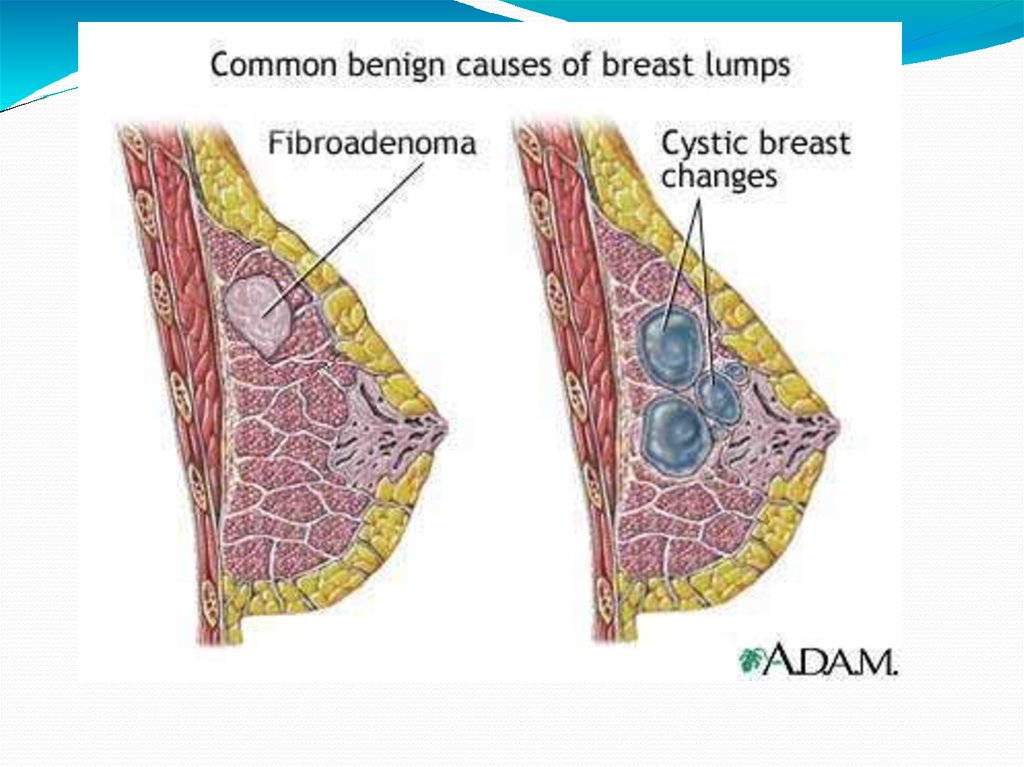
FIBROADENOMAHyperplasia of a single lobule of the breast (AND).
Most common benign tumour of the breast.
Encapsulated tumour common in young females.
Bilateral in 20% of cases. 20% are multiple.
10.
Progression30% of fibroadenomas may disappear or reduce in size
in 2-4 years.
10 -15% will increase in size progressively.
It does not occur after menopause unless women are
on hormones.
11.
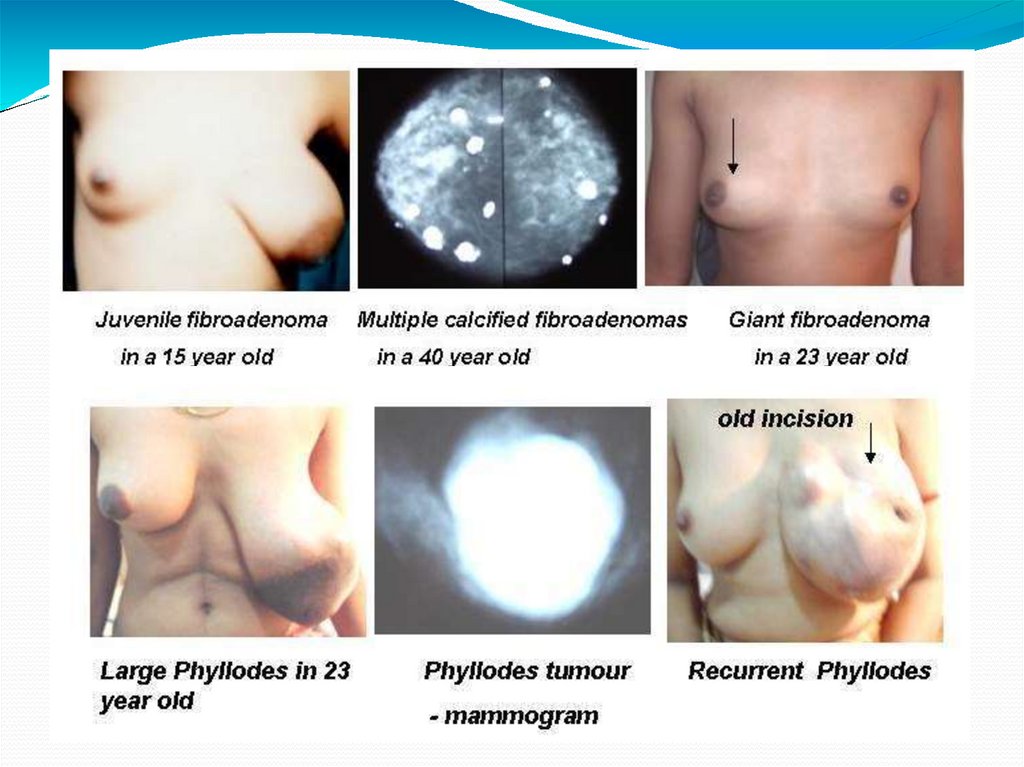
Fibroadenoma Variants1. Juvenile fibroadenoma
Occurs in adolescent girls.
Even though it shows rapid growth with stromal and
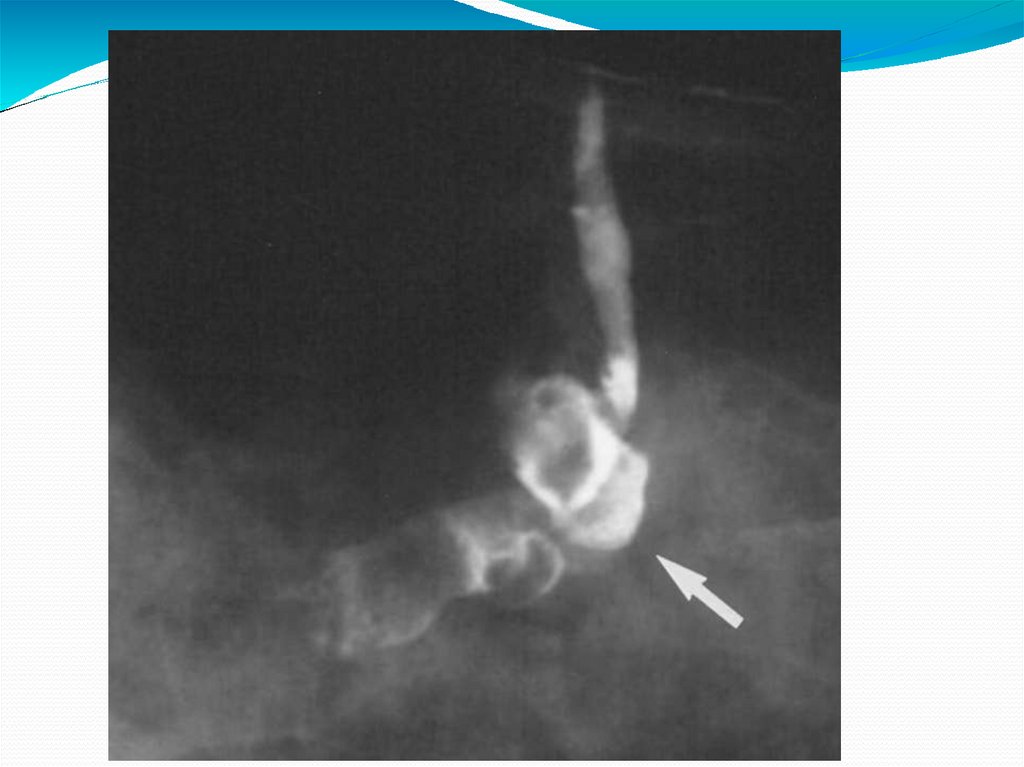
epithelial hyperplasia, it does not show any alteration in
stromal epithelial balance or cellular atypia or periductal
cellular concentration.
Mimic phyllodes tumour.
12.
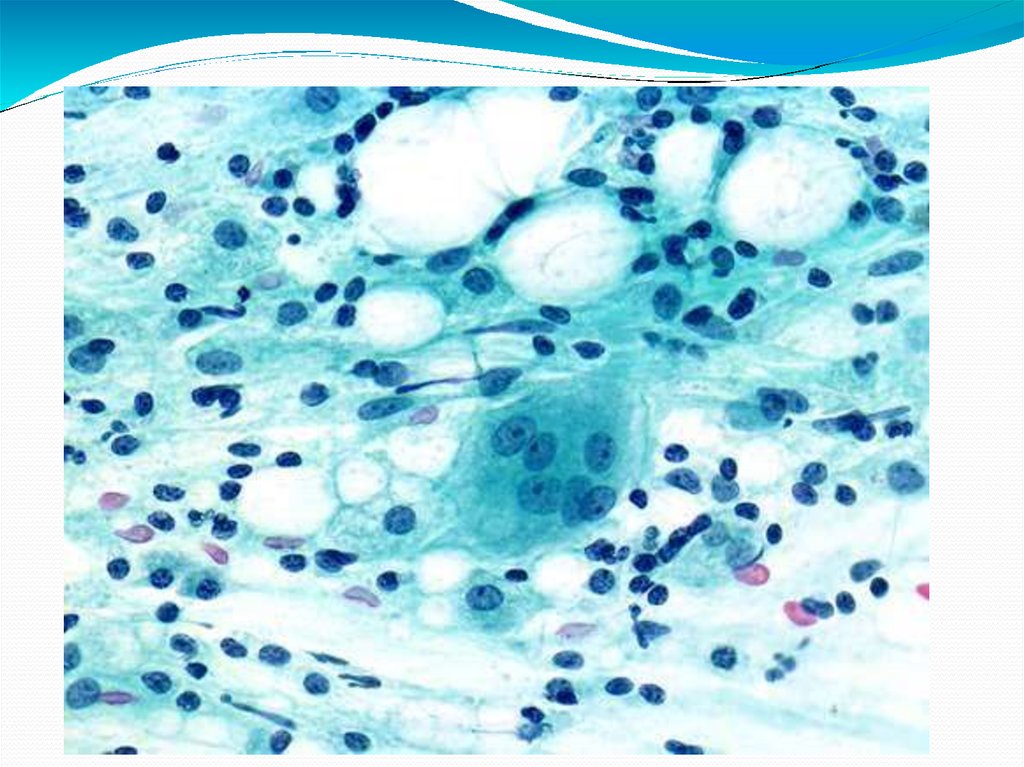
2. Complex fibroadenomaIt occurs in older age group.
Having typical fibroadenoma with fibrocystic changes
like apocrine metaplasia, cyst formation, sclerosing
adenosis.
15% of proven fibroadenomas are complex.
Occasionally it may turn into malignancy unlike usual
fibroadenomas.
13.
Pathological Types1. Intracanalicular: large and soft—mainly cellular.
Stroma with distorted duct.
2. Pericanalicular : small and hard—mainly fibrous.
Stroma with normal duct
14.
Clinical FeaturesPainless swelling
Smooth, firm, nontender, well-localised and
Moves freely within the breast tissue (mouse in the
breast).
15.
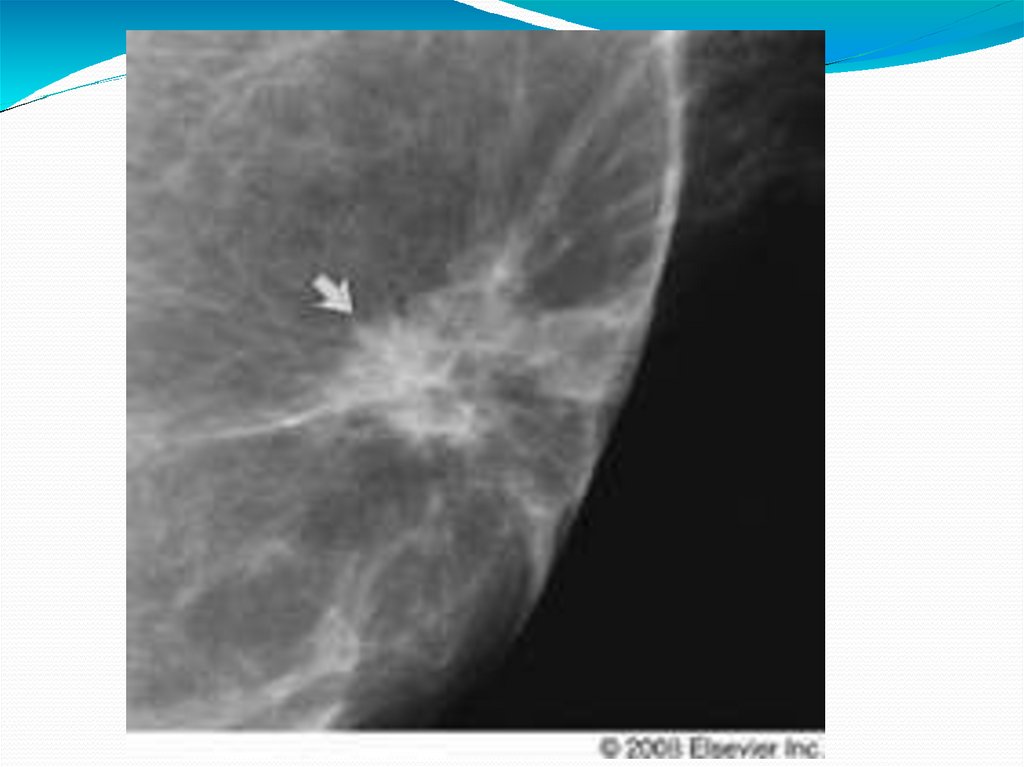
InvestigationsMammography (well-localised smooth regular
shadow).
FNAC.
Ultrasound (to confirm solid nature).
16.
TreatmentFibroadenoma which is small (< 3 cm)/single/age < 30
years can be left alone with regular follow-up with
USG at 6 monthly interval.
Indications for surgery are:
Size > 3 cm.
Multiple.
Giant type.
Recurrence.
Cosmesis.
Complex type.
17.
18.
Early Reproductive Period(1525yrs)NORMAL
PROCESS
• LOBULE
FORMATION
• STROMA
FORMATION
ABERRATION
DISEASE STATE
• FIBROADENOMA
• GIANT
FIBROADENOMA
• JUVENILE
HYPERTROPHY
• MULTIPLE
FIBROADENOMA
19.
20.
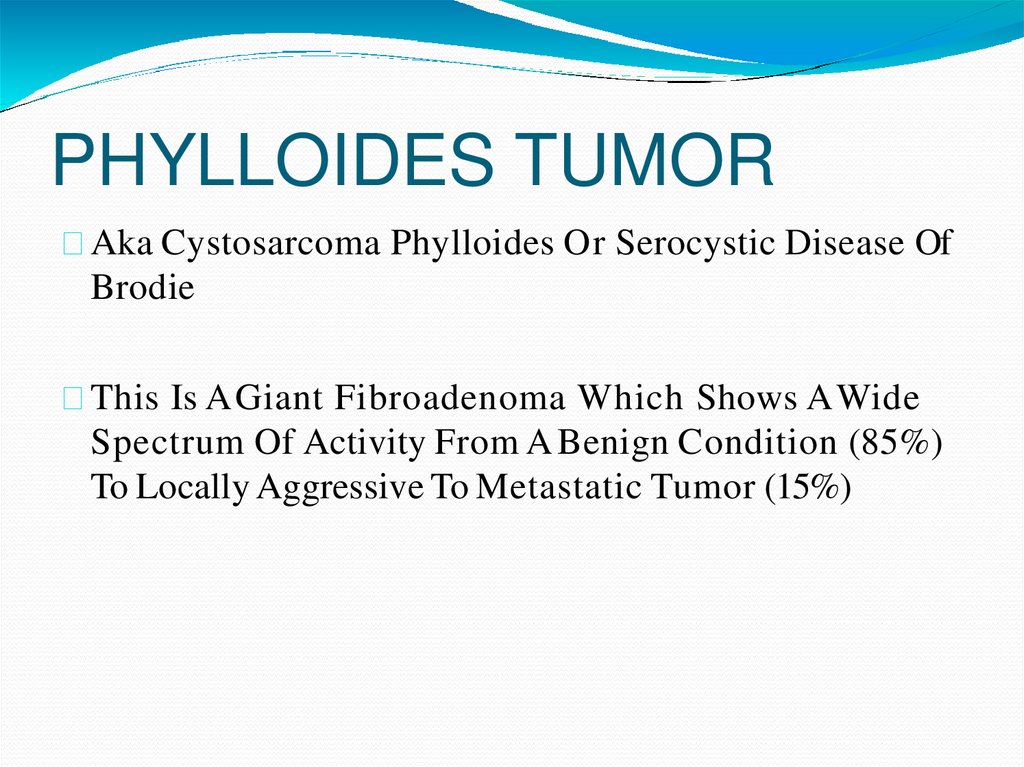
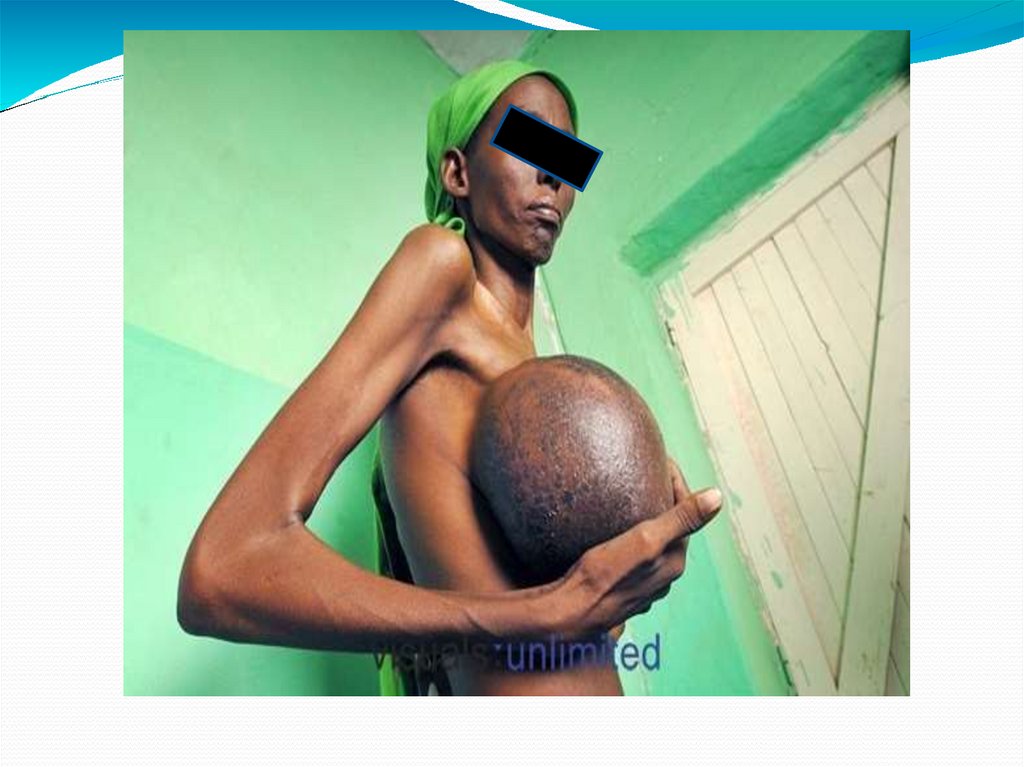
PHYLLOIDES TUMORAka Cystosarcoma Phylloides Or Serocystic Disease Of
Brodie
This Is A Giant Fibroadenoma Which Shows A Wide
Spectrum Of Activity From A Benign Condition (85%)
To Locally Aggressive To Metastatic Tumor (15%)
21.
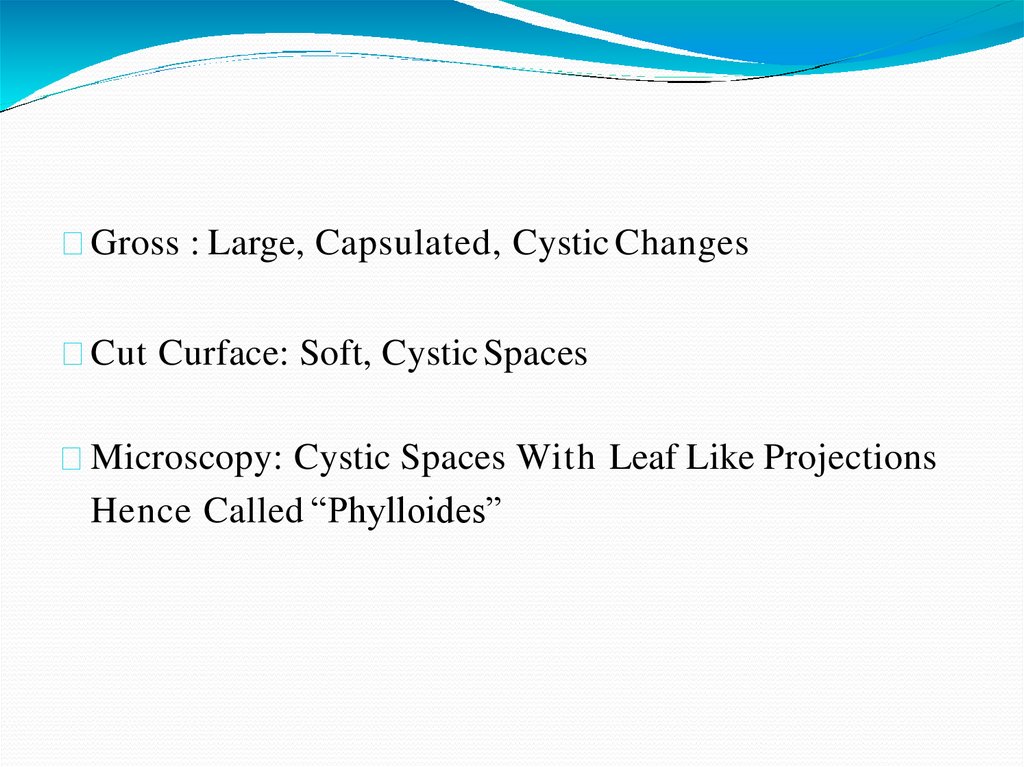
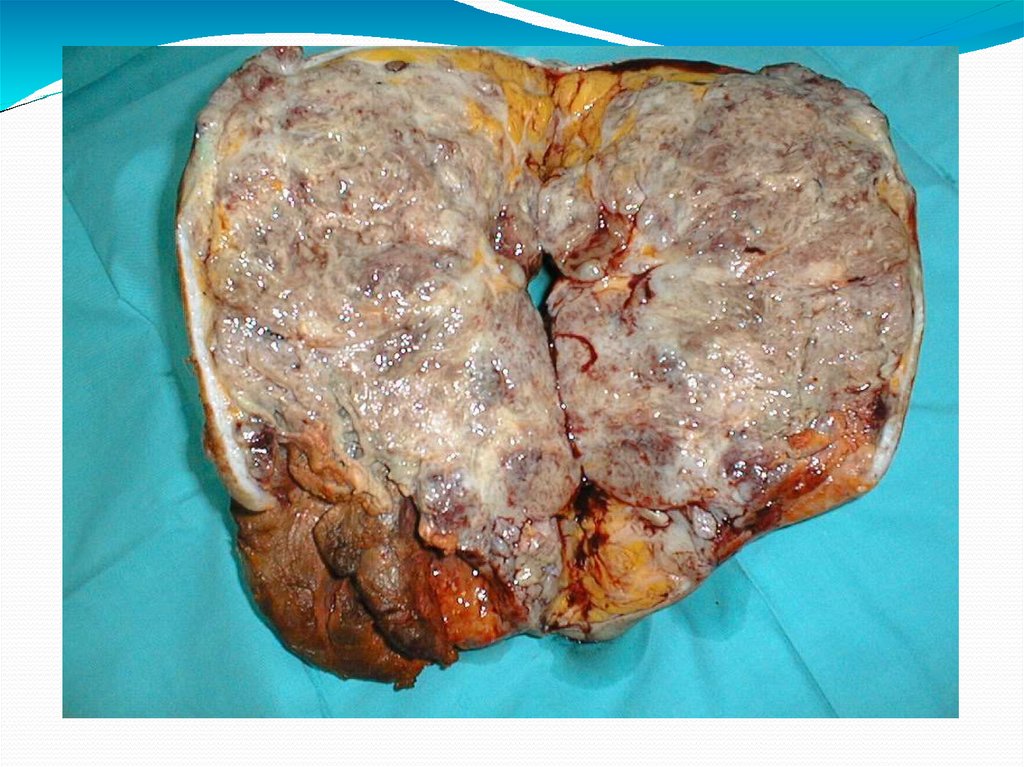
22.
Gross : Large, Capsulated, Cystic ChangesCut Curface: Soft, Cystic Spaces
Microscopy: Cystic Spaces With Leaf Like Projections
Hence Called “Phylloides”
23.
24.
25.
CLINICAL FEATURES30-50yrs
Unilateral
Grows rapidly to attain large size
Bosselated surface with necrosis of skin
Swelling is warm, not fixed to skin or chest wall
26.
27.
INVESTIGATIONSULTRASOUND
FNAC
CHEST XRAY
28.
TREATMEExcision
NT
Total Mastectomy If Malignant
29.
Mature Reproductive Period (2540yrs)NORMAL
• CYCLICAL
HORMONE
EFFECTS ON
GLANDULAR
TISSUE AND
STROMA
ABERRATION
DISEASED STATE
• EXAGGERATED
CYCLICAL
EFFECTS
• CYCLICAL
MASTALGIA
AND
NODULARITY
30.
Cyclical Mastalgia With NodularityAka Fibrocystadenosis / Fibrocystic Disease Of Breast/
Mammary Dysplasia
Estrogen Dependant
31.
32.
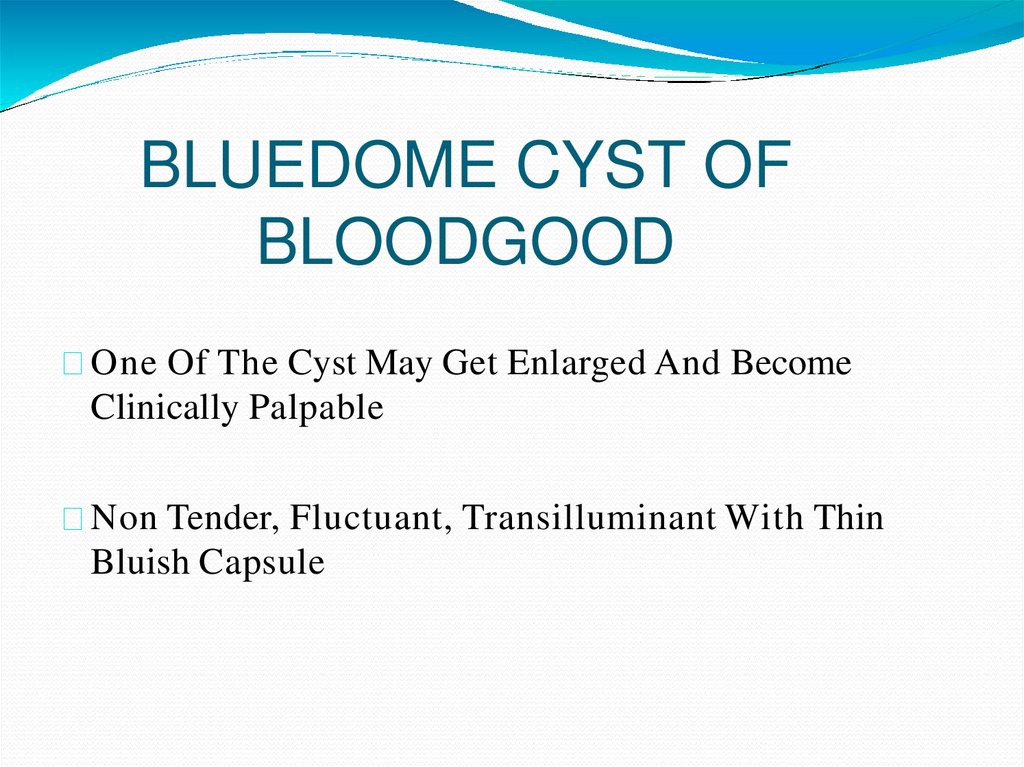
BLUEDOME CYST OFBLOODGOOD
One Of The Cyst May Get Enlarged And Become
Clinically Palpable
Non Tender, Fluctuant, Transilluminant With Thin
Bluish Capsule
33.
Initially AspiratedSurgical Excision Done If Recurs/ Persists/ Blood
Stained/ Residual Lump Remains
Multiple Small Cysts – Schimmelbusch’s Disease
34.
FIBROCYSTADENOSIS35.
CLINICAL FEATURESB/L, Diffuse, Painful, Granular Swelling Better Felt
With Palpating Fingers
Pain And Tenderness More Just Prior To
Menstruatuion
Subsides During Pregnancy/ Lactation/After
Menopause
36.
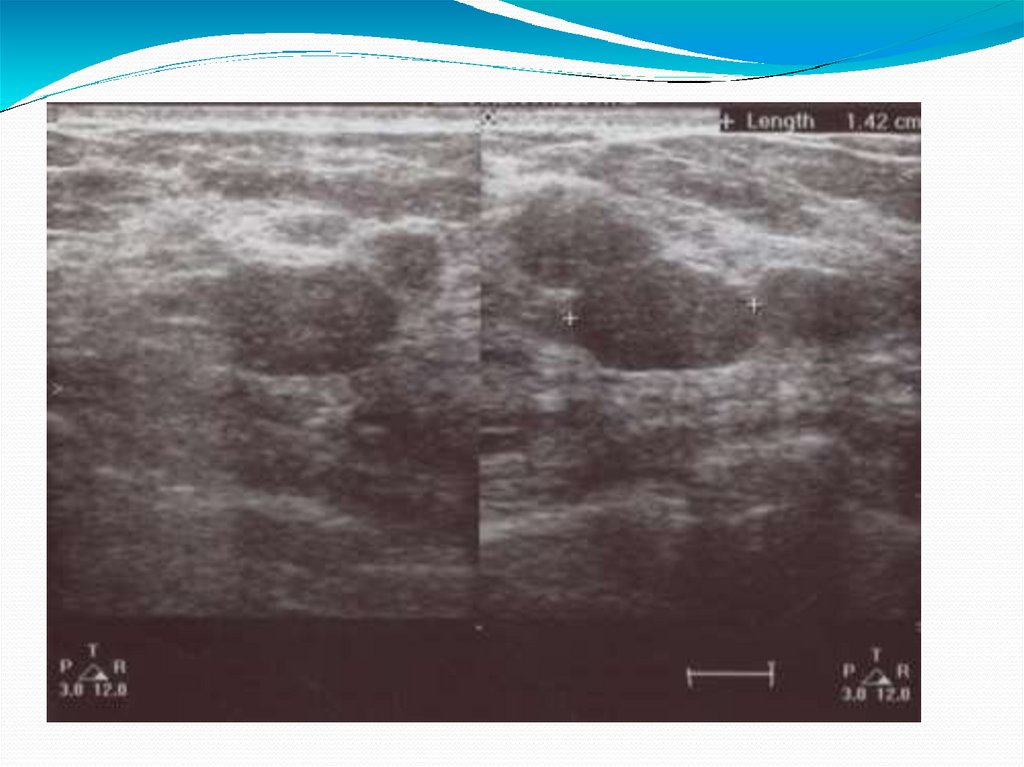
INVESTIGATIONSFNAC- EPITHELIOSIS (PREMALIGNANT)
USG
MAMMOGRAPHY
37.
38.
TREATMENT(A) CONSERVATIVE
Reassurance
Oil Of Evening Primrose: Gamolenic Acid
NSAIDS
Vit E And B6
Bromocriptine- Prolactin Inhibitor
Tamoxifen- Estrogen Antagonist
Danozol- Antigonadotrohin Agent
39.
SURGERYExcision Of Cyst/ Diseased Tissue
D/D: Tietze’s Disease Costochondritis Of Second
Costal Cartilage
40.
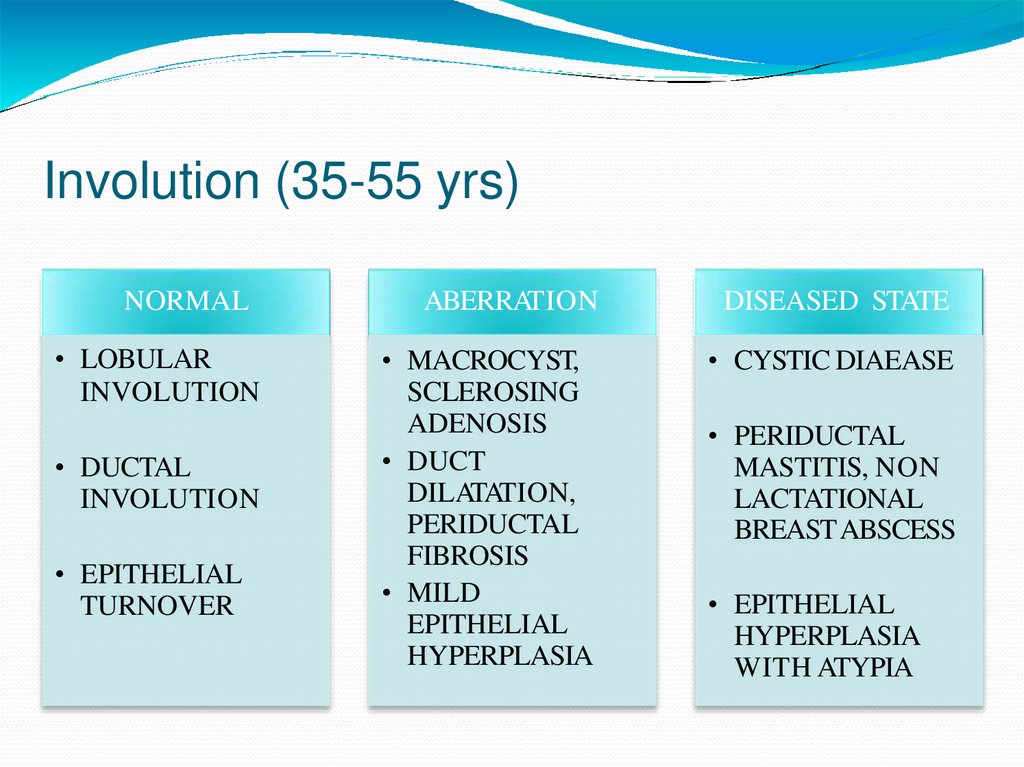
Involution (35-55 yrs)NORMAL
• LOBULAR
INVOLUTION
• DUCTAL
INVOLUTION
• EPITHELIAL
TURNOVER
ABERRATION
DISEASED STATE
• MACROCYST,
SCLEROSING
ADENOSIS
• DUCT
DILATATION,
PERIDUCTAL
FIBROSIS
• MILD
EPITHELIAL
HYPERPLASIA
• CYSTIC DIAEASE
• PERIDUCTAL
MASTITIS, NON
LACTATIONAL
BREASTABSCESS
• EPITHELIAL
HYPERPLASIA
WITH ATYPIA
41.
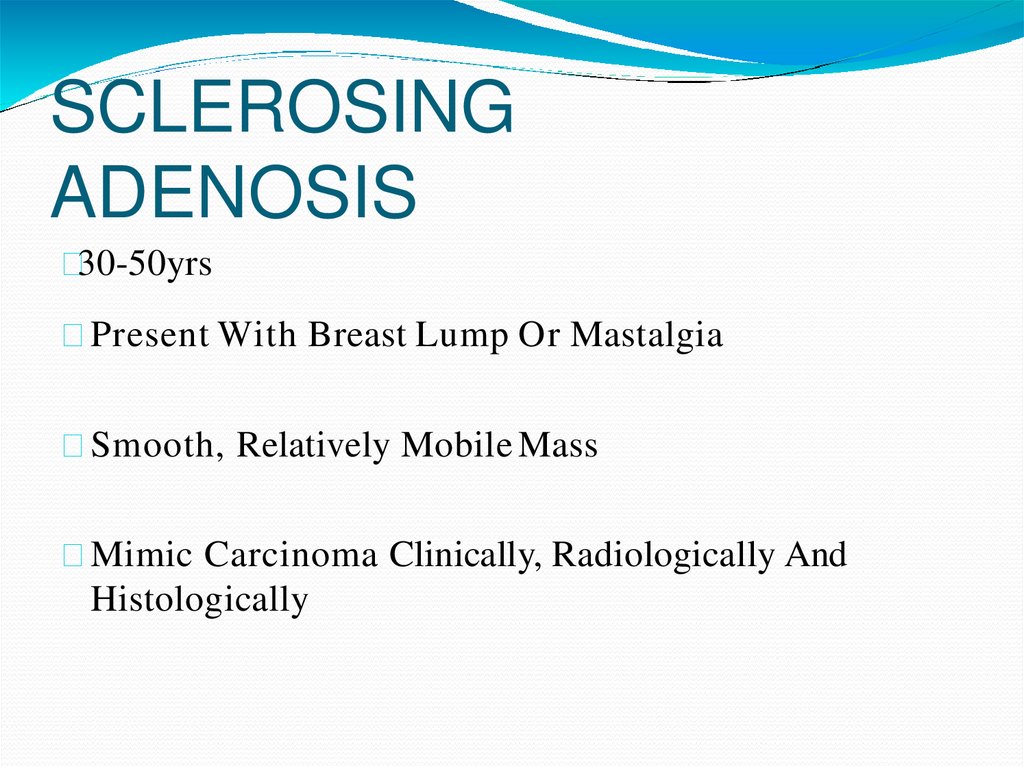
SCLEROSINGADENOSIS
30-50yrs
Present With Breast Lump Or Mastalgia
Smooth, Relatively Mobile Mass
Mimic Carcinoma Clinically, Radiologically And
Histologically
42.
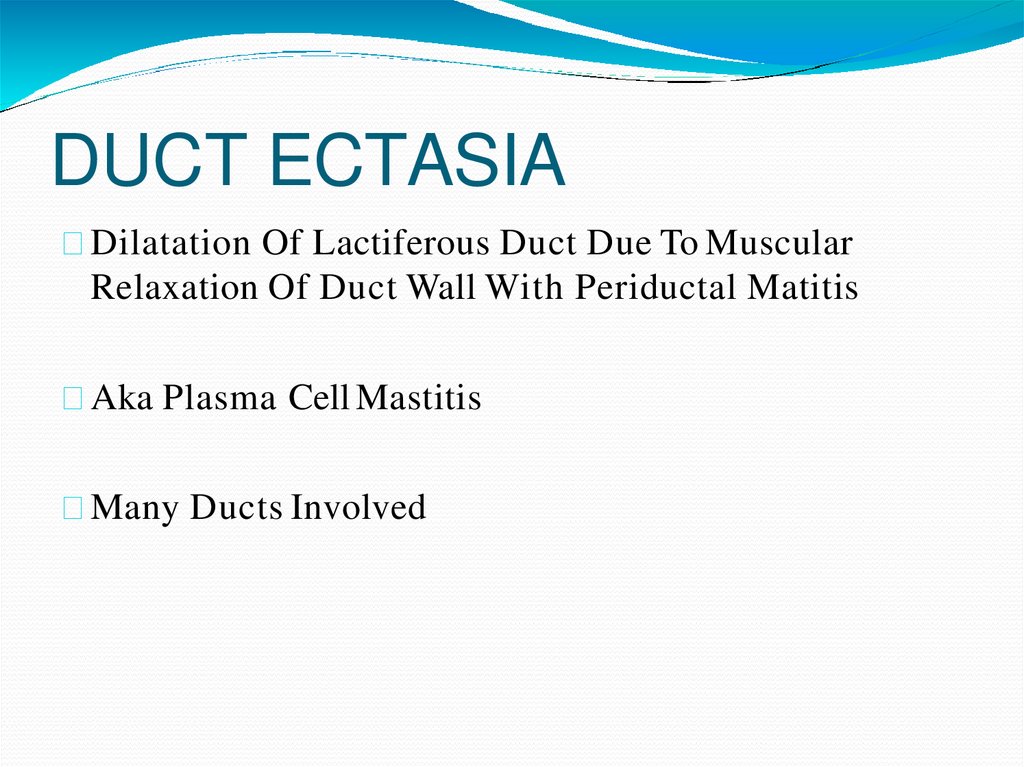
DUCT ECTASIADilatation Of Lactiferous Duct Due To Muscular
Relaxation Of Duct Wall With Periductal Matitis
Aka Plasma Cell Mastitis
Many Ducts Involved
43.
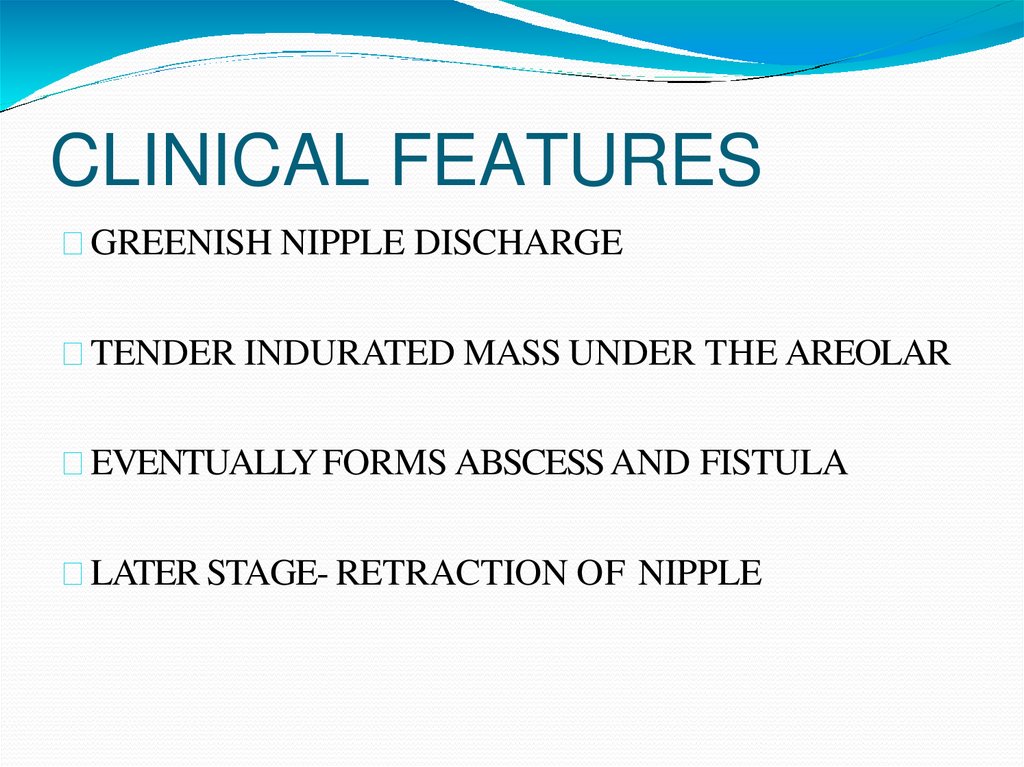
CLINICAL FEATURESGREENISH NIPPLE DISCHARGE
TENDER INDURATED MASS UNDER THE AREOLAR
EVENTUALLY FORMS ABSCESS AND FISTULA
LATER STAGE- RETRACTION OF NIPPLE
44.
COMMON IN SMOKERS- IN RELATION TOARTERIAL PATHOLOGY
B/L AND MULTIFOCAL
D/D –CARCINOMABREAST
45.
46.
47.
TREATMENTSTOP SMOKING
CONE EXCISION OF INVOLVED MAJOR DUCTSHADFIELD OPERATION
ANTIBIOTICS
48.
MASTITISTYPES:
(1)SUBAREOLAR MASTITIS- INFECTED GLAND OF
MONTGOMERY
(2) INTRAMAMMARY MASTITIS
-LACTATING ABSCESS
- NON LACTATINGABSCESS
(3)RETROMAMMARY MASTITIS- TB OF
INTERCOSTAL LYMPH NODES
49.
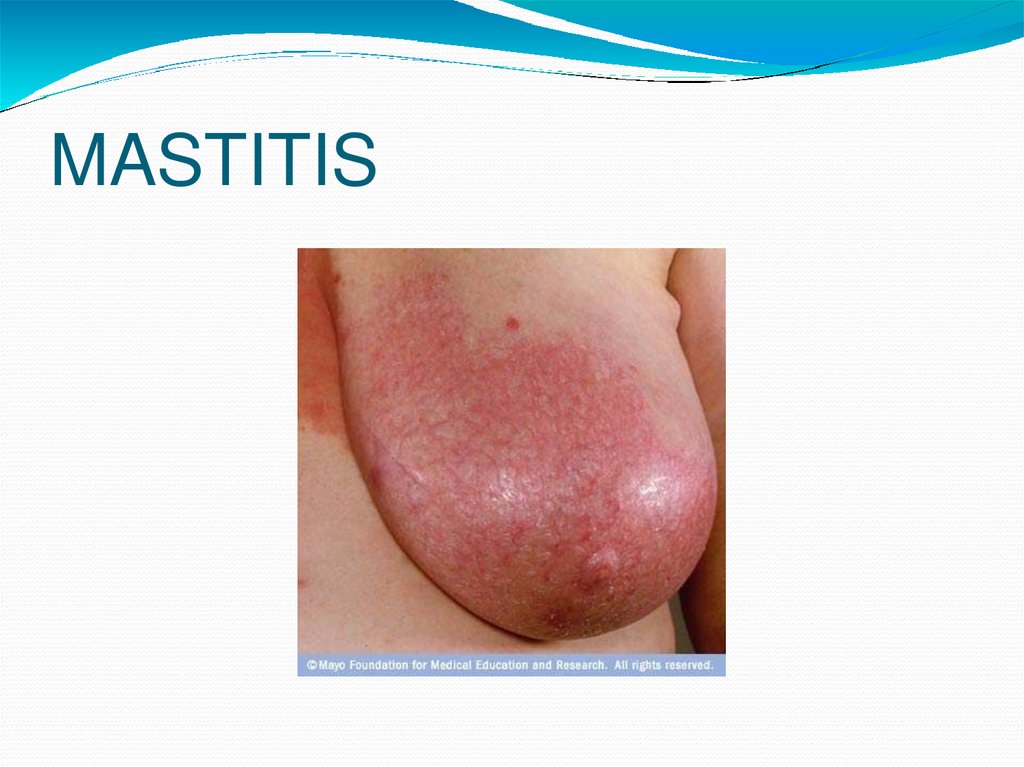
MASTITIS50.
BREAST ABSCESS51.
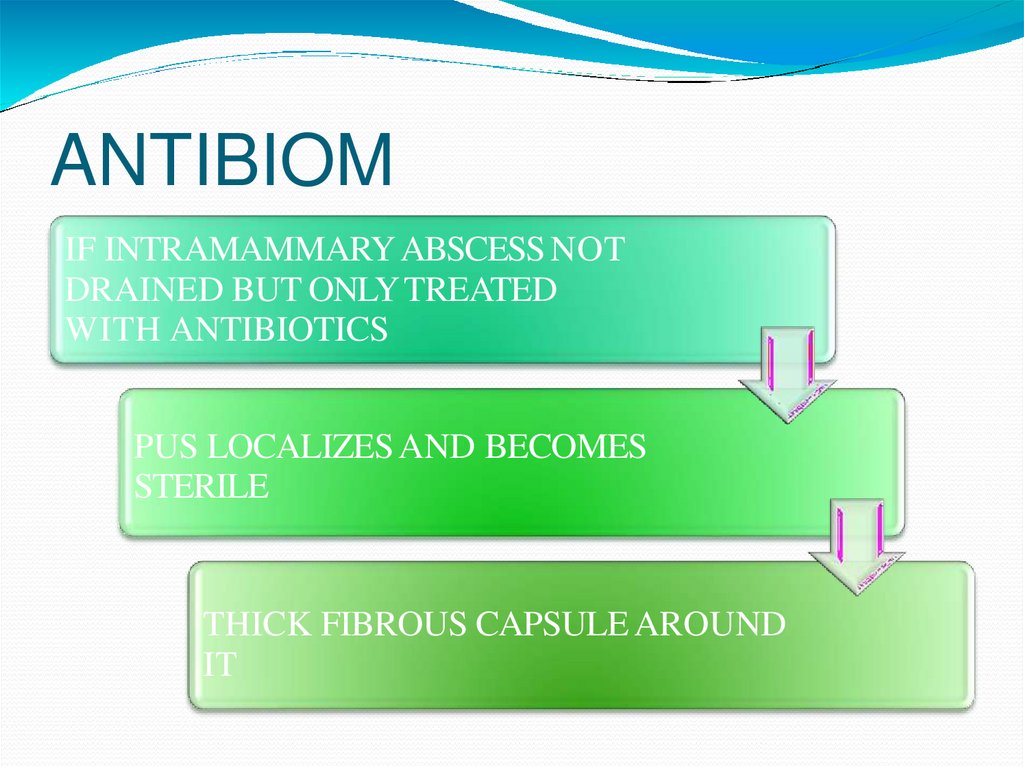
ANTIBIOMINTRAMAMMARY ABSCESS NOT
AIFDRAINED
BUT ONLY TREATED
WITH ANTIBIOTICS
PUS LOCALIZES AND BECOMES
STERILE
THICK FIBROUS CAPSULE AROUND
IT
52.
PREVIOUS HISTORY OF MASTITISD/D- CARCINOMA AS IF HARD AND FIXED TO
BREAST TISSUE
EXCISION
53.
OTHER BENIGN BREASTCONDITIONS
GALACTOCOELE
-SEEN IN LACTATING WOMEN
-RETENSION CYST IN SUBAREOLAR REGION
-BLOCK OF LACTIFEROUS DUCT
-MASSIVE ENLARGEMENT OF LACTIFEROUS
SINUS
54.
PRESENT AS LARGE, SMOOTH, SOFT, FLUCTUANTLUMP
CAN GET INFECTED
EXCISION
55.
56.
TRAUMATIC FATNECROSIS
DIRECT OR INDIRECTTRAUMA
SMOOTH, HARD, NON TENDER, NOTADHERENT
EXCISION
57.
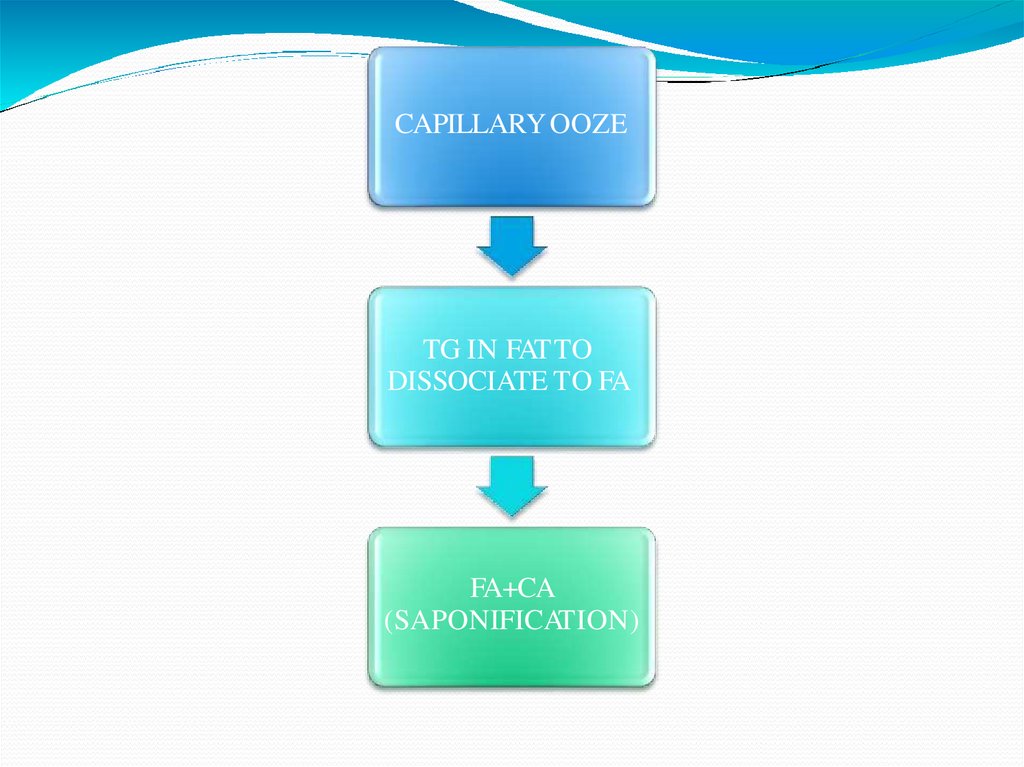
CAPILLARY OOZETG IN FAT TO
DISSOCIATE TO FA
FA+CA
(SAPONIFICATION)
58.
59.
60.
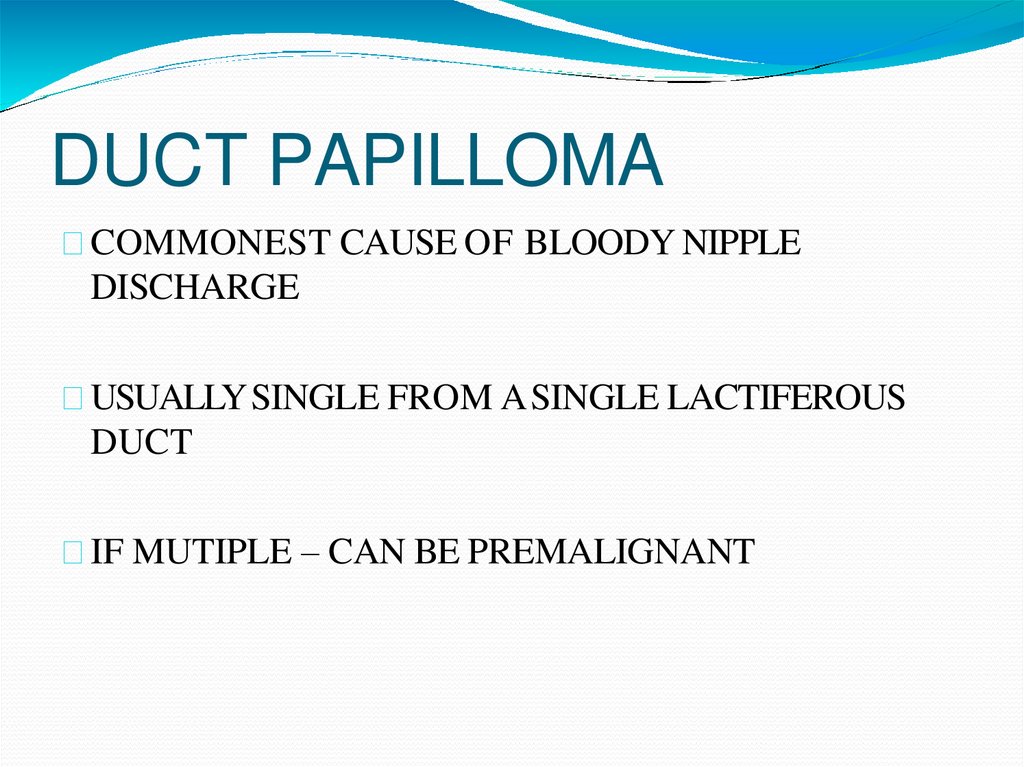
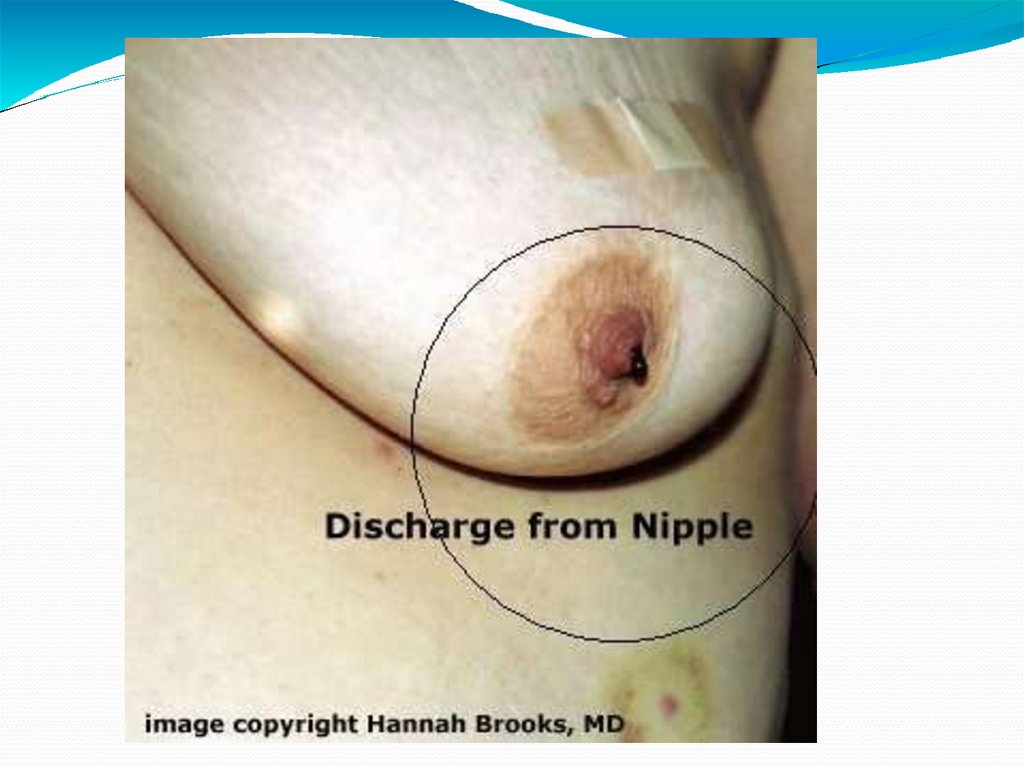
DUCT PAPILLOMACOMMONEST CAUSE OF BLOODY NIPPLE
DISCHARGE
USUALLY SINGLE FROM A SINGLE LACTIFEROUS
DUCT
IF MUTIPLE – CAN BE PREMALIGNANT
61.
62.
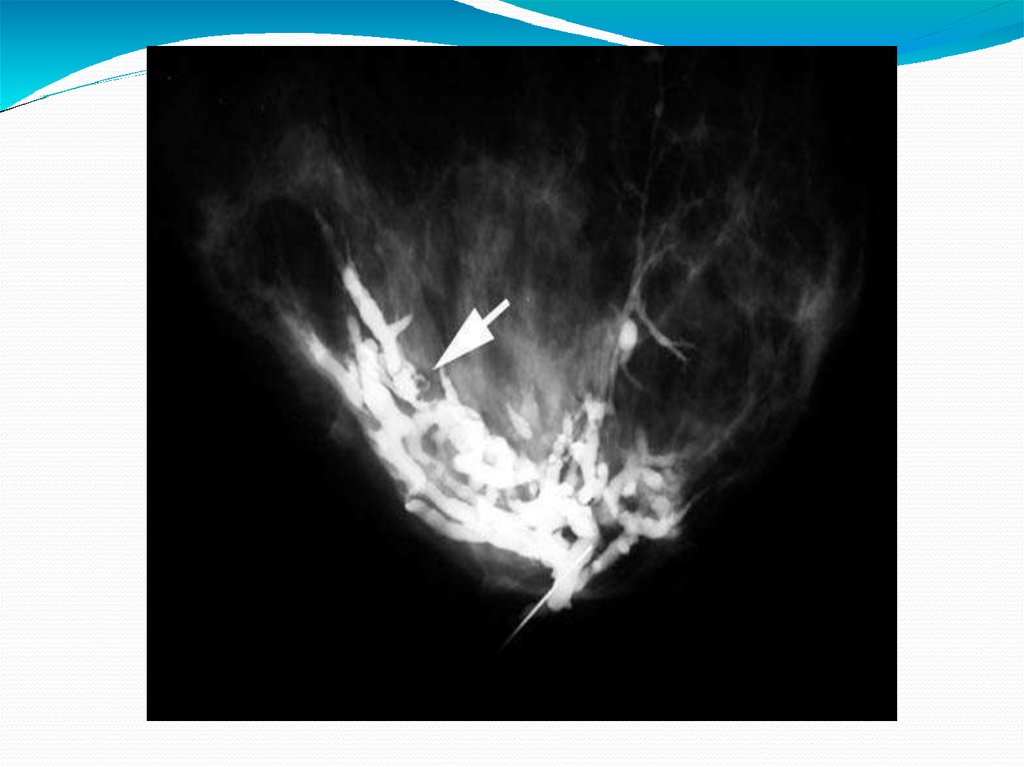
INVESTIGATION- INJECT CONTRAST INTO DUCT(DUCTOGRAM)
MICRODOCHECTOMY: PROBED LACTIFEROUS
DUCT IS OPENED AND THE PAPILLOMAEXCISED
USING TENNIS RAQUET INCISION
63.
64.
THANKYOU









 medicine
medicine