Similar presentations:
Breast pathology
1. BREAST PATHOLOGY
2. Pathology of the breast
• normal anatomy• physiologic changes
• developmental abnormalities
• inflammations
• fibrocystic changes
• tumors
• benign
• malignant
• pathology of the male breast
3. Normal anatomy
• before puberty – breasts in bothsexes – ducts
• variable degrees of branching, lack
lobules
• 15 to 25 lactiferous ducts
• start in the nipple – branch
terminal ductal lobular unit
(intralobular duct, multiple lobular
ducts, ductules or acini + intralobular
connective tissue)
• hormonally responsive
4. Physiologic changes
• at birthmale and female breasts
active secretion (transplacental passage of
maternal hormones)
bilateral breast
enlargement
• colostrum-like secretion ("witch's milk")
• recedes several months postpartum
• after menopause – gradual and progressive
involution (lobular atrophy, increased fat,
cystic dilatation of ducts)
5. Physiologic changes
Macromastia• diffuse enlargement of both breasts
• adolescence or pregnancy
• exaggerated response to hormonal stimulation
• Pubertal (Virginal) Macromastia
• 1669 - 23-year-old woman - breasts enlarged
"overnight" to a combined weight of 104 pounds
• Pregnancy
• 1 in 100,000 pregnancies - erythematous, edematous,
painful
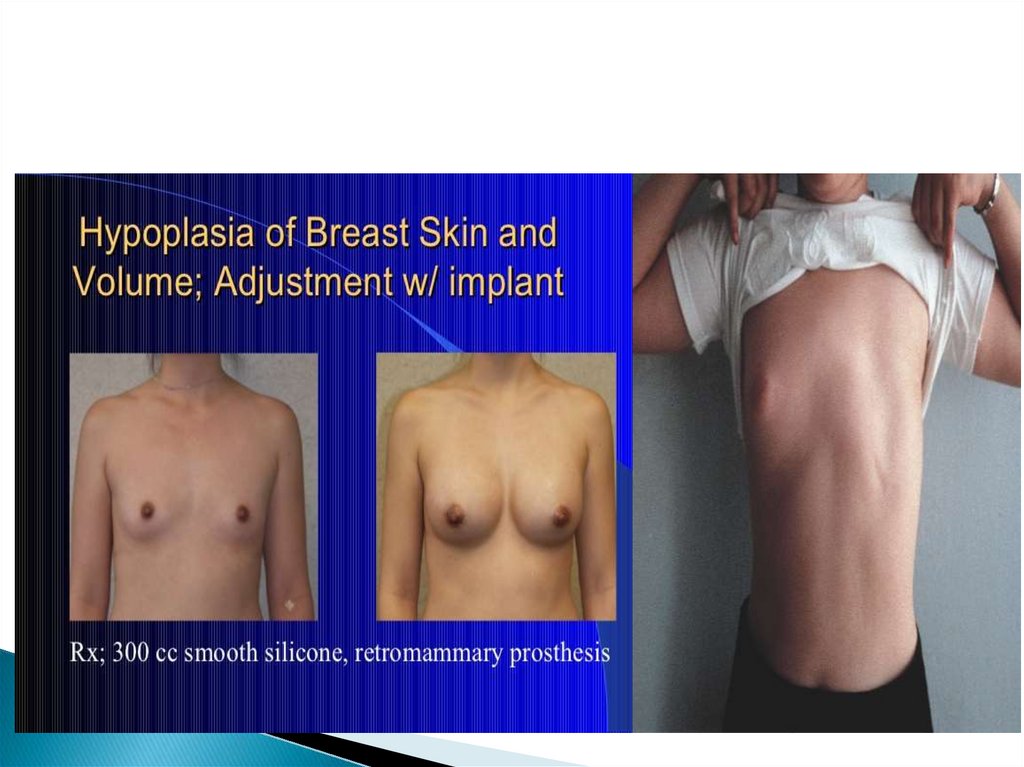
6. Developmental abnormalities
Aplasia and hypoplasia• uncommon – associated with overdevelopment of
the contralateral breast
• acquired (irradiation – chest wall tumors)
• unilateral or bilateral amastia (absence of a nipple,
breast ducts, pectoralis major muscle) – sex-linked
recessive inheritance
7.
8. Developmental abnormalities
Ectopic breast• supernumerary breast (from ectopic breast tissue –
along the milk lines (midaxillae – normal breasts –
medial groin and vulva)
• 1 – 6 % of adult women, much less often in men
• unilateral axillary breast tissue
Polythelia
• areola and underlying mammary ducts
Aberrant Breast
• beyond the usual anatomic extent (no nipple or areola)
9.
10. Inflammatory and reactive conditions
Fat necrosis• can simulate carcinoma clinically and
mammographically
• history of antecedent trauma, prior surgical
intervention)
• histiocytes with foamy cytoplasm
• lipid–filled cysts
• fibrosis, calcifications, egg shell on mammography
11. Inflammatory and reactive conditions
Hemorrhagic necrosis with coagulopathy• Warfarin treatment – shortly after initiation
• edema, hemorrhage, necrosis (thrombi in small blood
vessels )
• protein C deficiency
Breast augmentation
• foreign materials (shellac, glazier's putty, spun glass,
epoxy resin, beeswax, and shredded silk, silicone)
• thin–walled silicone bag – capsule – disfiguration
12.
Puerperal mastitis• early stages (2nd and 3rd W) of lactation – 5%
• stasis of milk in distended ducts + staphylococci
abscess formation (ATB, incision and drainage)
Granulomatous Lobular Mastitis
• etiology unknown, suggests carcinoma
Mammary duct ectasia
• periductal inflammation, duct sclerosis
• intermittent nipple discharge
Tuberculosis
• less developed regions - serious condition
• lactating breast, innoculation via the lactiferous ducts
• slowly growing, solitary, painless mass
13.
14. Benign proliferative lesions
• pathologic spectrum of seemingly related clinicallybenign breast abnormalities
• palpably irregular and painful breasts
• discrete lumps, multiple nodules, cystically dilated
ducts, apocrine metaplasia, interlobular and
intralobular fibrosis
• intraductal epithelial proliferation
fibrocystic disease, fibrocystic
• extremely common (58% F)
changes
15. Benign proliferative lesions
Adenosis• elongation of the terminal ductules
of the lobule
caricature
• sclerosing adenosis
• apocrine adenosis
• tubular adenosis
• nonpalpable lesion, recognized in mammograms
• microcalcifications!
16. Benign tumors
Fibroadenoma• proliferation of epithelial and stromal elements
• most common breast tumor in adolescent and young
adult women (peak age = third decade)
• higher incidence in black patients
• well-circumscribed, freely movable, nonpainful mass
• regress with age if left untreated
• ducts distorted elongated
slit-like structures intracanalicular pattern, ducts not compressed
pericanalicular growth pattern (little practical value)
17.
Tubular adenoma• far less common than fibroadenomas
• young women, discrete, freely movable masses
• uniform sized ducts
Lactating Adenoma
• enlarging masses during lactation or pregnancy
• prominent secretory change
Intraductal papilloma
• in the mammary ducts, subareolar lactiferous ducts
• periductal inflammation, duct sclerosis
• serous or bloody nipple discharge
• fibrosis, infarction, squamous metaplasia
18.
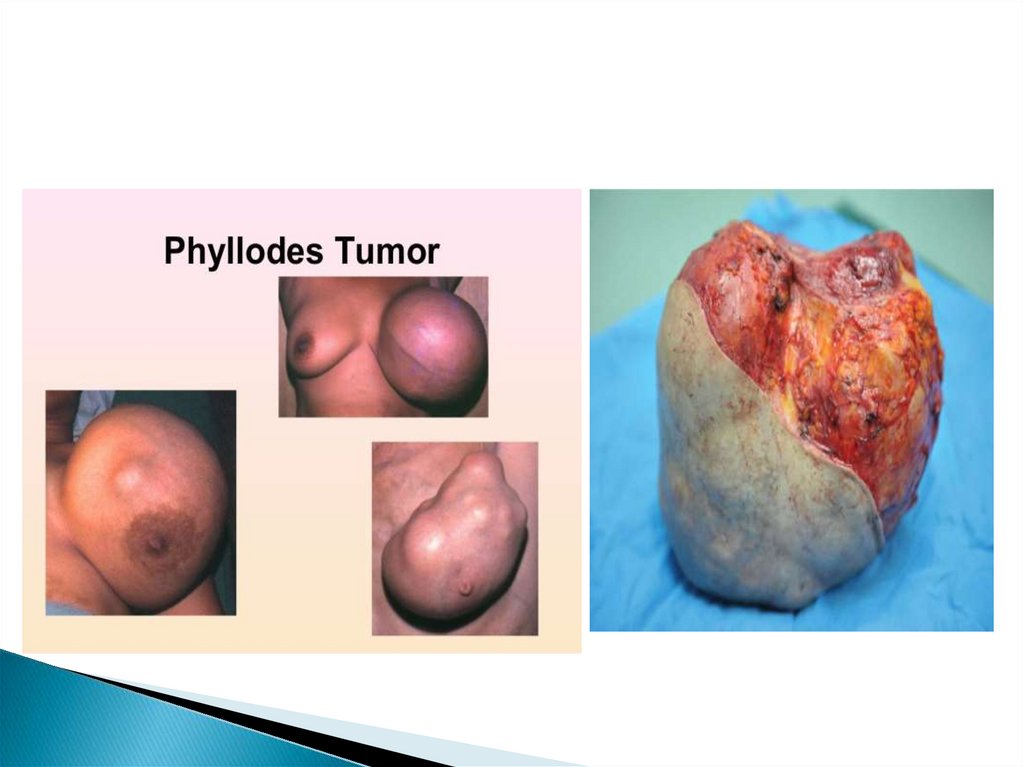
19. Cystosarcoma phyllodes (phyllodes tumor)
• initial description - over 150 years ago - fleshy tumor,leaf-like pattern and cysts on cut surface
• circumscribed, connective tissue and epithelial
elements (× fibroadenomas = greater connective tissue
cellularity), 1-15 cm
• less than 1 % of breast tumors
• benign, malignant
• metastases are hematogenous
low grade
high grade
20.
21.
22. Proliferative changes
• ductal and lobular hyperplasia• atypical ductal and lobular hyperplasia
• higher risk for the cancer than "normal" population
• associated w. microcalcifications (!mammography!)
• incidental histological finding
• atypical hyperplasia = precancerous lesion
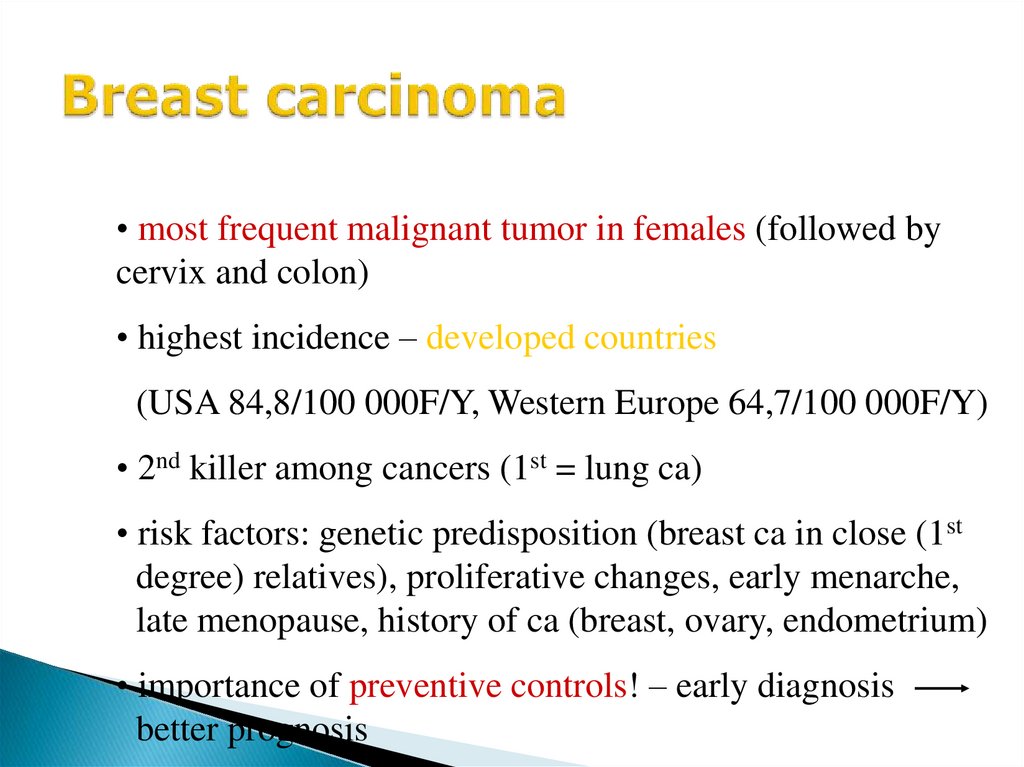
23. Breast carcinoma
• most frequent malignant tumor in females (followed bycervix and colon)
• highest incidence – developed countries
(USA 84,8/100 000F/Y, Western Europe 64,7/100 000F/Y)
• 2nd killer among cancers (1st = lung ca)
• risk factors: genetic predisposition (breast ca in close (1st
degree) relatives), proliferative changes, early menarche,
late menopause, history of ca (breast, ovary, endometrium)
• importance of preventive controls! – early diagnosis
better prognosis
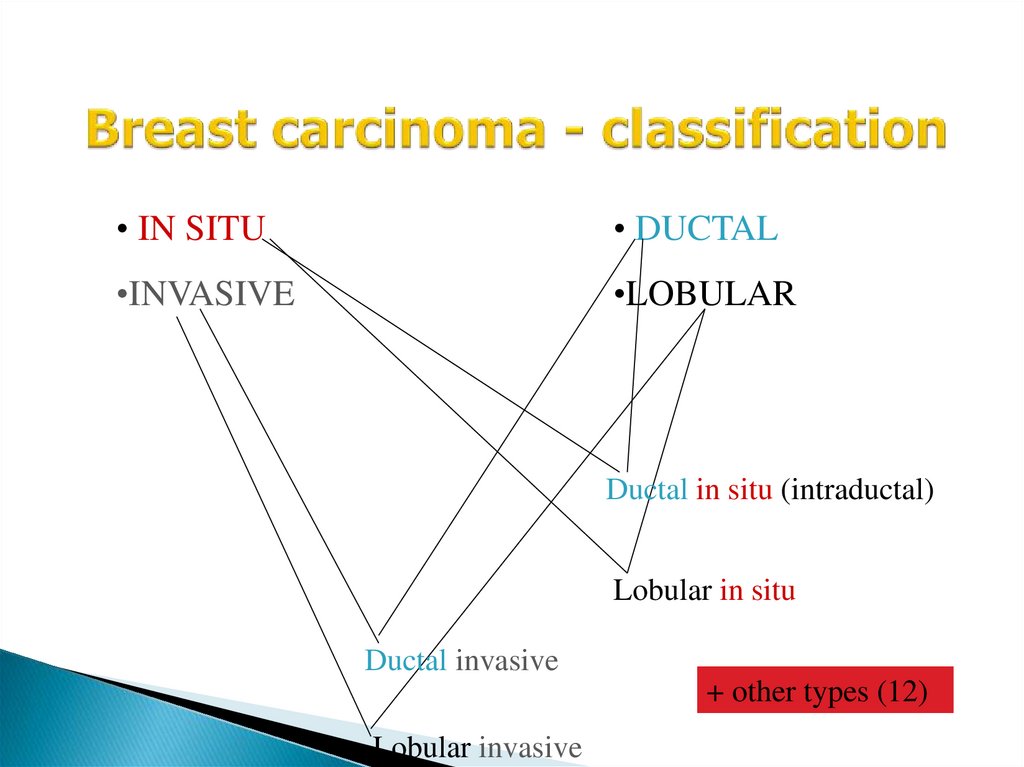
24. Breast carcinoma - classification
• IN SITU• DUCTAL
•INVASIVE
•LOBULAR
Ductal in situ (intraductal)
Lobular in situ
Ductal invasive
+ other types (12)
Lobular invasive
25. Carcinoma in situ
• preinvasive - does not form a palpable tumor• not detected clinically (only X-ray – screening !!!)
• multicentricity and bilaterality (namely LCIS)
• continuum: bland hyperplasia - increasing atypism carcinoma in situ
• no metastatic spread (basement membrane)
• risk of invasion depending on grade
26. Invasive carcinoma
Invasive ductal carcinoma• largest group (65 to 80 % of mammary carcinomas)
• mid to late fifties
• stellate, white, firm (desmoplasia)
• less often circumscribed, soft (medullary ca)
• hormonally dependent (estrogen, progesterone)
Invasive lobular carcinoma
• uniform cells, infiltrative growth (linear arrangement indian file pattern)
27. Invasive carcinoma
• other types: tubular, mucinous, medullary,inflammatory – together about 10 % of breast ca
• metastases: regional lymph nodes (axillary,
parasternal), lungs, liver, bone marrow, brain
• treatment: surgery (radical – mastectomy, breast
conserving surgery – lumpectomy),
radiotherapy
antihormonal therapy (Tamoxifen)
chemotherapy
28. Paget‘s disease of the nipple
• result of intraepithelial spread of intraductalcarcinoma
• large pale-staining cells within the epidermis of the
nipple
• limited to the nipple or extend to the areola
• pain or itching, scaling and redness, mistaken for
eczema
• ulceration, crusting, and serous or bloody discharge
29. Paget’s disease
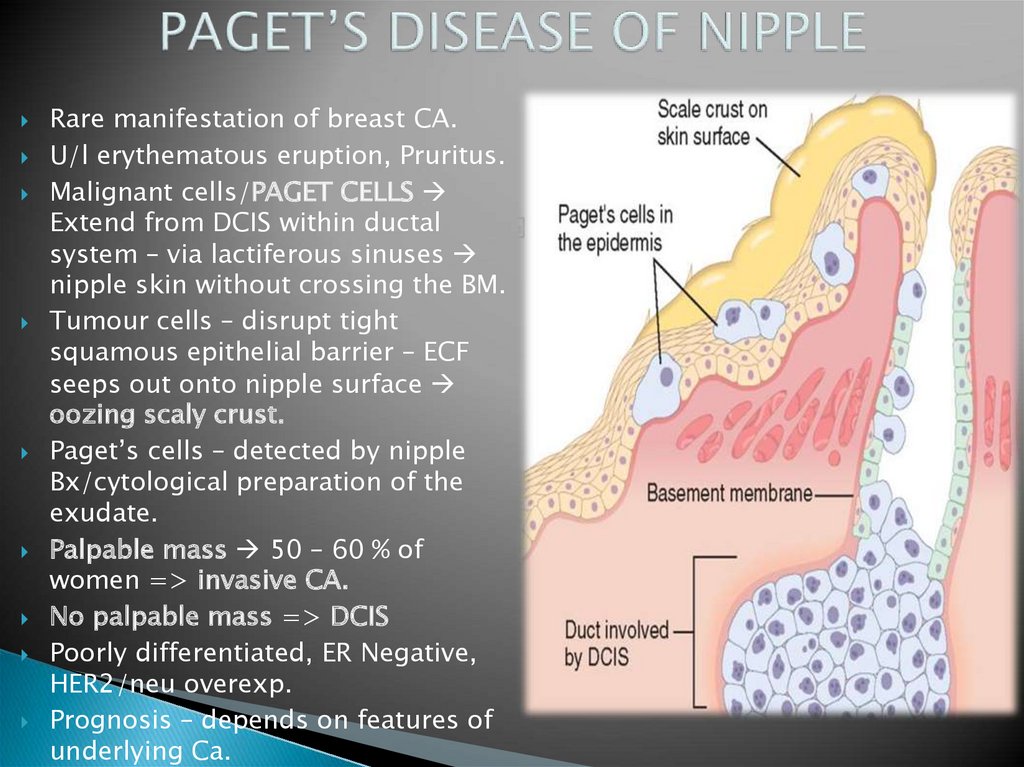
30. PAGET’S DISEASE OF NIPPLE
Rare manifestation of breast CA.U/l erythematous eruption, Pruritus.
Malignant cells/PAGET CELLS
Extend from DCIS within ductal
system – via lactiferous sinuses
nipple skin without crossing the BM.
Tumour cells – disrupt tight
squamous epithelial barrier – ECF
seeps out onto nipple surface
oozing scaly crust.
Paget’s cells – detected by nipple
Bx/cytological preparation of the
exudate.
Palpable mass 50 – 60 % of
women => invasive CA.
No palpable mass => DCIS
Poorly differentiated, ER Negative,
HER2/neu overexp.
Prognosis – depends on features of
underlying Ca.
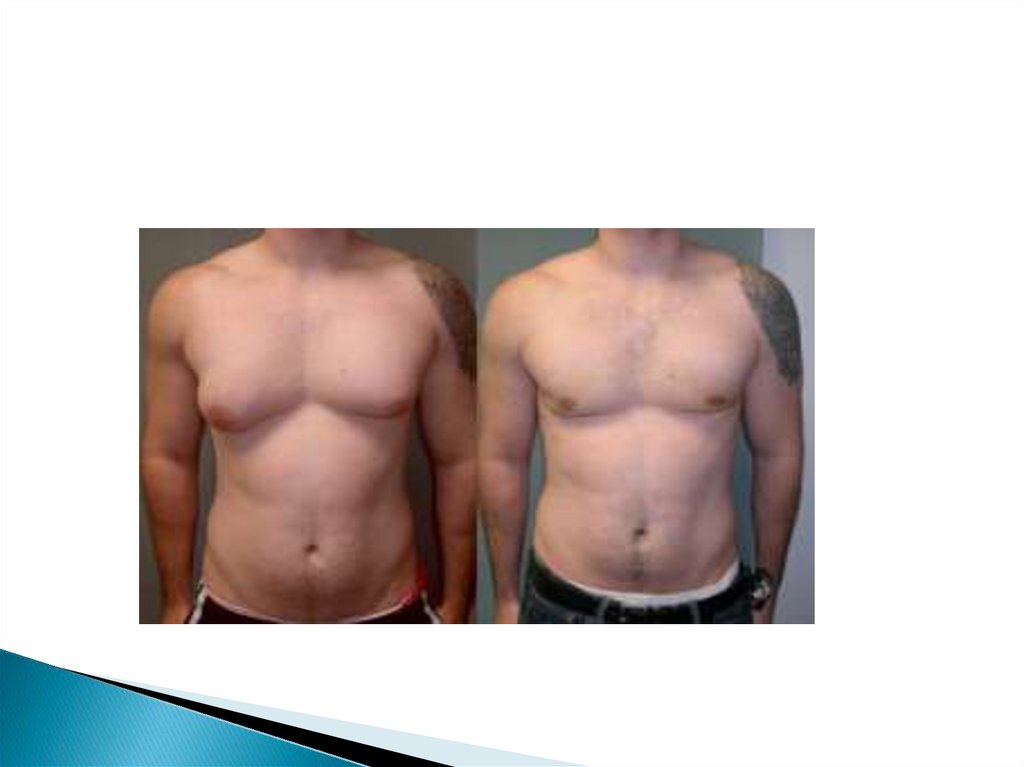
31. Pathology of the male breast
Gynecomastia• most common clinical and pathologic abnormality of the
male breast
• increase in subareolar tissue
• in 30 to 40 percent of adult males, both breasts are
affected in many cases
• associated with hyperthyroidism, cirrhosis of the liver, chronic renal
failure, chronic pulmonary disease, and hypogonadism, use of hormones estrogens, androgens, and other drugs (digitalis, cimetidine, spironolactone,
marihuana, and tricyclic antidepressants)
Carcinoma of the male breast
• uncommon < 1 % of all breast cancers








 medicine
medicine