Similar presentations:
Postpartum Infection
1. Postpartum infection
Teacher: Kamilova Irina KaharovnaStudent: Sulur PerumalSwamy Venkatesh
Prabhu
Group: 163(B)-CO-LA1 Course: 5
Date: 5-10-2020 Year: 2020-2021 Batch
1
2.
Postpartum infection – is aseptic wound infection
distinguished by anatomic
features of female reproductive
organs and their functional status
during pregnancy.
2
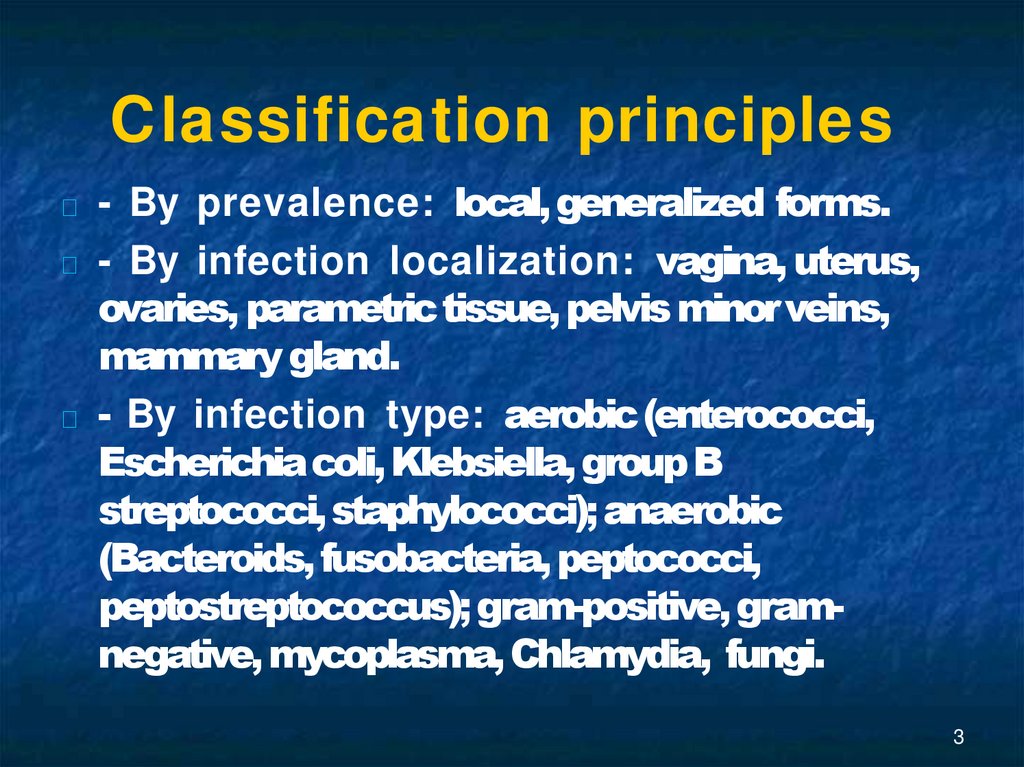
3. Classification principles
- By prevalence: local, generalized forms.- By infection localization: vagina, uterus,
ovaries, parametric tissue, pelvis minor veins,
mammary gland.
- By infection type: aerobic (enterococci,
Escherichia coli, Klebsiella, group B
streptococci, staphylococci); anaerobic
(Bacteroids, fusobacteria, peptococci,
peptostreptococcus); gram-positive, gramnegative, mycoplasma, Chlamydia, fungi.
3
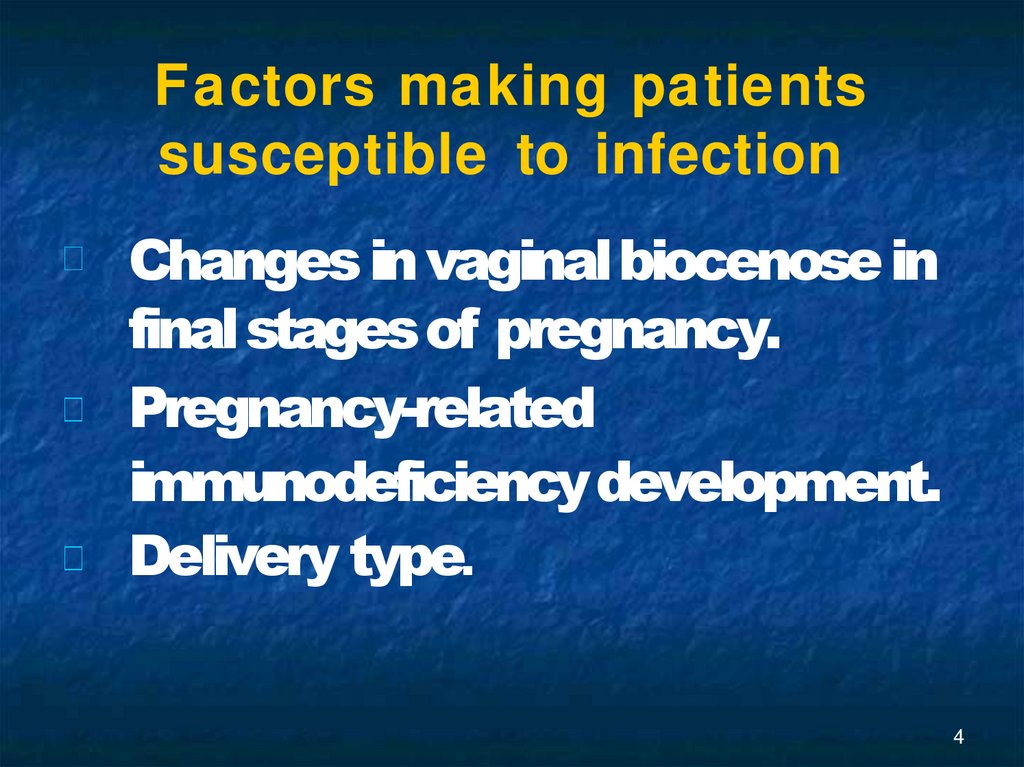
4. Factors making patients susceptible to infection
Changes in vaginal biocenose infinal stages of pregnancy.
Pregnancy-related
immunodeficiency development.
Delivery type.
4
5. Sponsored
Medical Lecture Notes – All SubjectsUSMLE Exam (America) – Practice
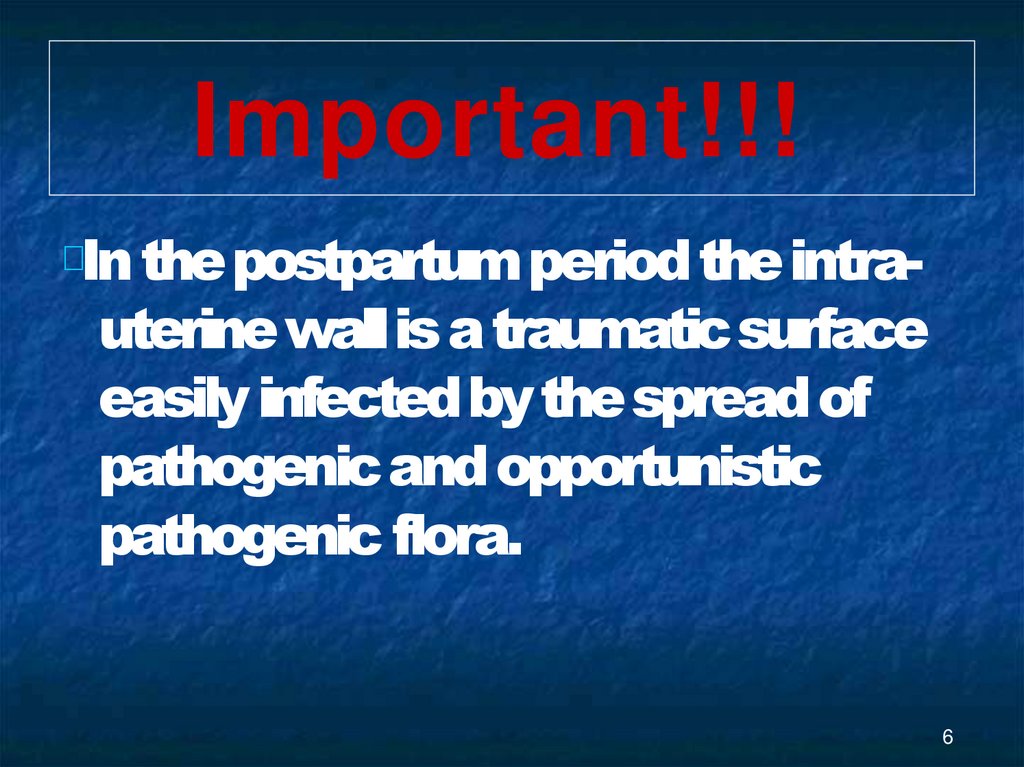
6. Important!!!
In the postpartum period the intrauterine wall is a traumatic surfaceeasily infected by the spread of
pathogenic and opportunistic
pathogenic flora.
6
7. Etiology
Iron-deficiency anemia.Gestosis.
Placental presentation.
Pyelonephritis.
Prolonged labour.
Prolonged anhydrous term.
Serious loss of blood.
Genital tract wounds.
Surgical procedures.
7
8.
Postpartum ulcer – is caused bycontamination of abrasions, fissures,
ruptures of vulval and vaginal mucous
membranes.
The patient’s general condition is
satisfactory.
8
9. Diagnostics
Hyperemia. Edema.
Necrotic or purulent wound
incrustation.
9
10. Treatment
The wounds are cleansed withantisepticslocally (hydrogen peroxide, furacilin,
chlorhexidine, dioxidine, hypertonic solution).
Wound debridement withproteolytic ferments
is performed (tripsin, chemotripsin).
After the wound has been cleansed from pus,
ointment bandages are applied (levomicole,
dioxicole).
10
11.
Postpartumendomyometritis.
The most common
infection in the
postpartum
period!
11
12. CLINICAL SYMPTOMS.
ACUTE FORM.Temperature elevation › 38° on 2-5th day
following delivery.
Chills.
Abdominal pain.
Foul-smelling, pus-containing lochia.
Headache.
Facial hyperemia.
Postpartum psychosis (the degree
depends on the level of intoxication).
12
13. DIAGNOSTICS
Bimanual examination (the uterus is enlarged, painful,softened, contractive movements are restricted).
Clinical blood count.
Ultrasonography.
Thermometry.
Bacterioscopic and bacteriological analysis of vaginal
discharge.
Biochemical blood test (c-reactive protein increase,
hypoproteinemia, hypoalbuminemia).
Coagulogram.
Hysteroscopy.
Clinical urine analysis.
13
14. TREATMENT
Bed rest.Antibiotic therapy (semisynthetic penicillin,
combination of cephalosporin and
metronidazole).
Infusion therapy (combination of colloids and
crystalloids).
10% calcium gluconate, 10 ml i.v.
Vitamin therapy.
Spasmolytics (no-spa, papaverine
hydrochloride).
Immunomodulators.
Intrauterine lavage withantiseptic
14
15. Important!!!
If the examination reveals placental tissues ormembranes in the uterine cavity, it is necessary
to perform curettage or vacuum aspiration of the
uterus.
LOW-GRADE ENDOMYOMETRITIS progresses
without pronounced clinical symptoms. The
onset of the disease is normally on the 7-9th day
following delivery. The most common causes of
the disease are Chlamydia or mycoplasma
infections.
15
16.
Postpartum salpingooophoritis is rarely observed.The ovaries are normally affected
on one side. The clinical history of
the disease is similar to
manifestations of
endomyometritis, which is
followed bysalpingo-oophoritis
16
17.
Postnatal parametritis –the process normally begins
when lacerations or infections
of the cervix are present.
Lateral parts of parametrium
are commonly affected.
17
18. Clinical symptoms
Chills on the 10-12th day followingdelivery.
Temperature elevation to 39 - 40°.
Tensive lowerabdominalpain.
Acruturesis or dyschezia in cases when
the process has spread to front or back
parametrium.
18
19. On bimanual examination a painful infiltrate is found in the fornices, the fornices are shortened.
On bimanual examination apainful infiltrate is found in the
fornices, the fornices are
shortened.
For diagnostics and treatment
see endomyometritis.
19
20.
Postnatal trombophlebitis(affecting pelvis minor veins,
superficial and deep veins of
lower limbs).
Causes
Hypercoagulation.
Vessel wall lesions.
20
21. Clinical symptoms
Temperature elevation.Hyperemia and tenderness along of
varix dilatated shin veins.
Edema (if deep veins of lower limbs
are involved).
21
22. Treatment
Bed rest, lower limb should bemaintained uplifted.
Antibacterial therapy.
Anticoagulants: direct effect (heparin),
indirect effect (kleksan, fraxiparin,
troxevasin, aspirin).
Medicines improving rheological
properties of the blood: rheopolyglukin,
trental, kurantil.
Hirudotherapy.
22
23. Obstetric peritonitis. Causes.
Consequence of endomyometritis.Perforation of inflammatory tubo-ovarian
mass.
Torsion of ovarian tumorpedicle.
Necrosis of the subserous node of
hysteromyoma.
Infected rupture of uterine sutures after
caesarean section.
23
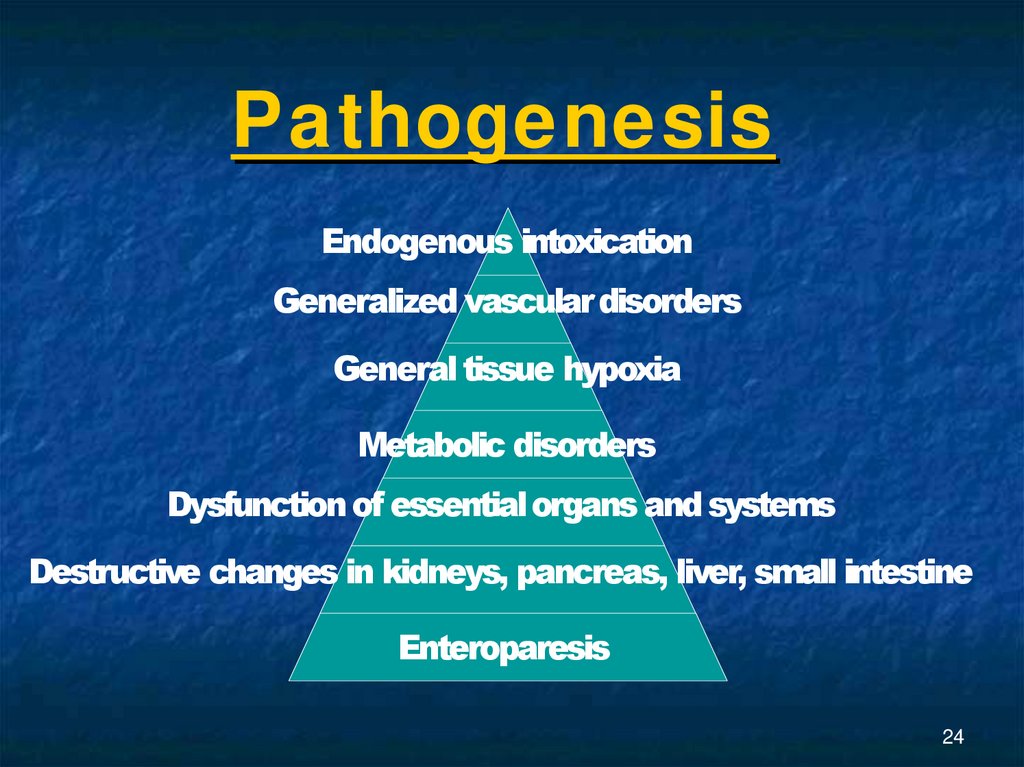
24. Pathogenesis
Endogenous intoxicationGeneralized vascular disorders
General tissue hypoxia
Metabolic disorders
Dysfunction of essential organs and systems
Destructive changes in kidneys, pancreas, liver, small intestine
Enteroparesis
24
25.
Enteroparesis. Motor, secretion, andabsorption functions are affected.
Significant amounts of protein and
electrolyte containing liquid
accumulate in the intestinal lumen.
Overdistension and ischemia of the
intestinal wall cause impairment of
the intestinal barrier function which
leads to increasedintoxication
25
26. Obstetric peritonitis phases
Reactive phase (compensatorymechanisms preserved).
Toxic phase.
Terminal phase.
26
27. Clinical symptoms
psychomotor agitationthirst
dryness of mucous membranes
general weakness
tachycardia (does not correspond to the
body temperature)
fever
pulse rate exceeds 100bpm
shallow breathing
27
28. unsatisfactory sleep absence of appetite
pallor of the skinnausea
eructation
flatulence
vomiting (not always)
the pain syndrome is not evident (due to
overdistension of the front abdominal wall after
delivery).
28
29.
On palpation: the abdomen isdistended, the uterus is enlarged,
softened, the contours are indistinct,
peritoneum irritation symptoms are
not pronounced, sluggish peristalsis,
slow flatusdischarge.
29
30. Treatment.
Preoperative preparation (2 hours): stomachdecompression, infusion therapy intended for
liquidation of hypovolemia and metabolic
acidosis, fluid, protein and electrolytic balance
correction, detoxication of the body,
antibacterial therapy.
Operative treatment: hysterectomy, abdominal
cavity drainage.
30
31. Postoperative period:
- liquidation of hypovolemia andimprovement of rheological properties of
the blood;
- acidosis correction;
-provision for the body’s energy
demands;
-antiferment and anticoagulant therapy
(combination of contrical and heparin);
- maintenance of artificialdieresis;
31
32.
- antibiotictherapy;- cardio-vascular collapse prevention and
treatment;
- vitamintherapy;
- motor and evacuation intestinal function
recovery (proserin, ganglio-blockers);
- ultraviolet irradiation of autoblood,
hyperbaric oxygenation.
32
33.
Postpartum sepsis –severe non-specific infective
process developing and
progressing when normal
reactivity of the organism is
changed.
33
34. Clinical symptoms
Septicemia occurs on the 3-4th dayfollowing delivery, progressesviolently.
Septicopyemia progresses unevenly:
periods of recrudescence caused by
metastatic infection and formation of new
niduses are followed by periods of
amelioration.
34
35. IMPORTANT!!!
The diagnosis is based on thefollowing prerequisites:
- presence of an infection nidus;
- fever and chills;
- etiological factor was detected in
blood.
35
36. Impaired CNS function: euphoria, depression, sleep disturbance. Dyspnea. Cyanosis.
Pale, grey or yellow skin.Tachycardia, pulse lability.
Hypotension.
Enlarged liver and spleen.
36
37. Diagnostics
Clinical blood analysis.Clinical urine analysis.
Coagulogram (platelets).
Blood electrolytes.
Bacteriological analysis.
Lungs radiography.
ECG.
Blood sugar.
Acid-base condition.
Central venous pressure.
Monitoring: arterial pressure, pulse rate, heart
rate, body temperature.
37
38. Treatment
Preoperative preparation during 6-8hours, hypervolemic hemodilution
mode.
Operative treatment – hysterectomy
and salpingectomy, abdominal
cavity drainage.
38
39. Postoperative period:
- liquidation of hypovolemia andimprovement of rheological properties of
the blood;
- acidosis correction;
-provision for the body’s energy
demands;
-antiferment and anticoagulant therapy
(combination of contrical and heparin);
- maintenance of artificialdieresis;
39
40.
- antibiotictherapy;- cardio-vascular collapse prevention and
treatment;
- vitamintherapy;
- motor and evacuation intestinal function
recovery (proserin, ganglio-blockers);
- ultraviolet irradiation of autoblood,
hyperbaric oxygenation, plasmapheresis,
hemosorption, hemodialysis.
40
41. Postpartum lactational mastitis is an inflammation of breast tissue.
Postpartum lactational mastitis is aninflammation of breasttissue.
The most common organism reported in
mastitis is Staphylococcus aureus,
Streptococcus is less common.
The organisms invade the breast tissue
via cracking or fissures in the nipple or
lactiferous ducts. Lactostasis is conducive
to progressing of the inflammatory
process.
41
42. Classification
Serous mastitis.Infiltrative mastitis (diffuse, nodular).
Suppurative mastitis
(intramammary, phlegmonous or
necrotic suppurative,gangrenous).
42
43. Clinical symptoms
Rapid elevation in temperature to 39˚C.Chills.
Painful breast.
Headache.
General malaise, weakness.
Sleep disturbance.
Loss of appetite.
43
44.
Examination shows that the breast isengorged, the skin above the breast is
hyperemic.
With the right treatment the disease is
cured within 1-2 days; if inadequate
therapy is chosen, the disease advances
to the next (infiltrate) stage.
The diagnosis is made on the basis of
clinical symptoms.
44
45. Treatment
Antibacterial therapy.Procedures against lactostasis.
Spasmolytics (no-spa) in combination
withuterotonics(oxytocin).
Parlodel (to decrease milk production).
Vitamin therapy.
Anti-staphylococcus gamma globulin,
hyperimmune anti-staphylococcus
plasma.
45
46. With suppurative mastitis surgical treatment is indicated (incision of the abscess, bathing with antiseptics and drainage of
With suppurative mastitis surgicaltreatment is indicated (incision of
the abscess, bathing with
antiseptics and drainage of the
pus).
IMPORTANT!!! During the course
of treatment for postpartum septic
diseases breastfeeding should be
discontinued as the baby might
receive high doses of medicines
with mother’s milk.
46


 medicine
medicine