Similar presentations:
Workshop. Basic manipulation technologies
1.
Workshop.Basic manipulation technologies
Methods of nursing examination: assessment of the general
condition, consciousness, and position of the patient, anthropometry,
thermometry and characterization of human body temperature,
determination of pulse on the radial artery, measurement of blood
pressure by the Korotkov method on the brachial artery, calculation of
the respiratory rate.
Module 1.8
2.
The student must learn:• проводить расспрос пациента, выявлять жалобы;
• собирать анамнез жизни и анамнез заболевания;
• проводить общий осмотр больного;
• оценивать общее состояние больного и сознания;
• оценивать положение пациента;
• проводить антропометрию и взвешивание пациента;
• оценивать состояние кожи и слизистых;
• выявлять скрытые и явные отеки;
• измерять температуру тела;
• определять частоту, глубину, ритм дыхания;
• выявить наличие и вид одышки: экспираторную, инспираторную, смешанного типа;
• проводить пальпацию, перкуссию и аускультацию лёгких;
• прощупать пульс, дать ему оценку;
• измерять АД и оценивать его;
• проводить аускультацию сердца;
• измерять диурез, определять водный баланс.
3.
4.
Introductory testingGive a detailed answer to the question
1. What is the nursing process?
2. What are the stages of the nursing process?
3. What and who can be sources of information at the first stage of a nursing survey?
4. What are the types of problems based on the nature of the patient's response to the disease and
condition?
5. What goals and types of nursing interventions do you know?
6. What is necessary to implement the nursing intervention plan?
7. What are the main criteria for evaluating the effectiveness of nursing care?
8. What types of nursing examinations do you know?
9. What is a subjective nursing examination?
10. Name the methods and basic principles for obtaining complete information from the patient.
11. What information does the medical history consist of?
12. In what order is information collected about the patient's life?
13. What information can be obtained from an additional inquiry about the state of the patient's body
functions?
5.
Nursing survey planNursing process – this is a science-based nursing technology. The nursing process brings a new understanding of
the role of nurses in practical healthcare, requiring them not only to have a good technical background, but also to be
able to be creative in caring for patients. Nursing care is based on the patient as a person who requires
comprehensive care. One of the prerequisites for this process is the participation of the patient (family members) in
making decisions about the goals of care, the plan of nursing interventions and their methods of implementation.
Nursing process – this is the technology that nurses use to provide care and assistance to patients, this is the action
plan that the nurse follows.
This plan consists of five stages.
1. Nursing examination - assessment of the patient's condition.
2. Nursing diagnostics - interpretation of the data obtained during the examination, identification of the patient's
health problems.
3. Goal setting and planning upcoming maintenance work.
4. Implementation of the prepared plan - performing nursing interventions.
5. Evaluation of results, efficiency of nursing care.
6.
The first stage is a nursing examinationStage goal - collecting information about the patient's health status to identify his or her
disturbed needs, existing and potential problems, in order to ensure the patient's quality
of life.
Information sources may include:
* the patient is the best source of information;
* family members, accompanying persons, neighbors in the ward;
* doctors, nurses, ambulance crew members, paramedics;
* medical documentation (survey data, extracts from inpatient or outpatient records);
* special medical literature (reference books on nursing, standards of nursing
manipulation, professional journals).
Distinguish between subjective and objective nursing examination.
Subjective survey – information obtained from the words of a patient or other person.
Subjective information - the patient's perceptions of their health. The usefulness of
information depends on the ability of the sister to arrange the interlocutor to
communicate.
Objective examination - direct examination and additional methods – data from
laboratory and instrumental studies (for example, blood and urine tests, X-ray
examinations) and special ones.
7.
Second stage - nursing diagnostics.Here, the nurse analyzes all the information she has collected and draws conclusions.
Types of problems based on the nature of the patient's reaction to the disease
and their condition:
Physiological factors - reactions to the disease caused by changes in the functions of
organs and systems (the body reacts to inflammatory changes in the lungs with a
violation of the functions of the respiratory system: shortness of breath, cough...).
Psychological issues - reactions that appeared in response to painful changes in the
internal organs (fear, tearfulness, emotional vulnerability).
Social networks - they are associated with a violation of the satisfaction of social needs
due to illness (incomplete family, financial insolvency, disability).
Spiritual ones - reactions of the body that affect the spiritual sphere (loss of the
meaning of life, unwillingness to take care of yourself, withdrawal to religion, loneliness).
The nurse identifies various problems and makes a list of diagnoses. Such a nursing
diagnosis is slightly different from what doctors do.
8.
Third stage – planning of nursing care.Here, the nurse sets goals for herself and plans how she can help the patient. She
develops a plan of action and thinks about how to make the patient feel better. Types of
goals:
Short-term loans – must be completed immediately or within one week (maximum of
two). They are usually detected in the acute phase of the disease in a hospital (for
example: reduction of pain in the postoperative wound area). Long-term - achieved
over a longer period of time, over many weeks. They are usually aimed at prevention of
complications, rehabilitation and social adaptation.
Nursing interventions can be classified into three types::
1. Dependents: they are performed according to the doctor's instructions recorded in
the patient's medical records (injections, distribution of medicines, etc.).
2. Independent: performed by a nurse independently within the scope of their
competence without direct instructions from the doctor, in accordance with standards
and instructions (measuring blood pressure and body temperature, monitoring the
patient during treatment, training skills, etc.).
3. Interdependent: performed by the nurse together with other health care workers,
such as doctors, other nurses,
(for example: preparing for research, assisting with surgery, etc.).
9.
Fourth stage – implementation of the nursing interventionplan.
The nurse begins to carry out her plan. She takes care of the patient, helps him,
monitors his condition and does everything possible to make the patient feel
comfortable and easier.
In the fourth stage of the nursing process, the nurse directly takes care of the patient in
accordance with the prescribed plan.
Implementation of the plan includes the following requirements::
1. Follow the plan systematically.
2. Coordination of actions in accordance with the planned and actual condition of the
patient.
3. Involve the patient and their loved ones in the care process.
4. Performing nursing manipulations according to established algorithms.
5. Providing pre-medical care in accordance with the standards of nursing practice and
taking into account the individual characteristics of the patient.
6. Registration of completed actions in the nursing medical history.
10.
Fifth stage - evaluation of results (efficiency)Key aspects of evaluating results:
* determination of the patient's current condition;
• have your goals been achieved;
* identify aspects that affect the achievement of goals;
• evaluation of the effectiveness of planned nursing interventions;
* comparison of planned and achieved results;
* modification of the nursing diagnosis, goal, and / or care plan, if necessary;
• review activities at all stages and adjust or develop a new plan.
Evaluation of results - this is a report written by the nurse on the patient's response to
nursing care (objective assessment) and the patient's opinion on achieving the goal
(subjective assessment). These estimates may not match, then preference should be
given to the patient's own assessment. Evaluation of the results allows you to determine
the quality of nursing care, the patient's response to interventions, and identify new
patient problems. If something goes wrong, she can change her plan and try other ways
to help the patient. If the goal is achieved (objective and subjective assessments
coincide), a clear entry is made in the care plan: "Goal achieved".
11.
PATIENT EXAMINATION PLANToday we will look at the first stage of the nursing process – nursing examination.
Types of nursing examinations:
Subjective survey – inquiry
* Finding out about complaints.
• Medical history (Anamnesis morbi – recollection of the disease) study of the history of
the origin and development of the present disease.
• Anamnesis of life (Anamnesis vitae-recollection of life). Study of the patient's life
history.
• Additional inquiry on the state of the patient's body functions (Status functionalis).
Objective of the subjective survey - collect, justify and link the received information
about the patient in order to create an information database about him, about his
condition at the time of seeking help.
Objective examination
Physical research methods:
• Inspection (Inspectio);
• Groping - palpation (Palpatio);
• Tapping - Percussion (Regcessio);
• Listening - Auscultation (Auscultatio).
12.
Subjective survey – inquiry (collecting information)Nursing examination it is independent and cannot substitute for or substitute for
medical treatment. The task of a medical examination is to prescribe treatment, and a
nursing examination is to provide motivated, individualized care. The presentation of
information received from the patient is usually preceded by certain introductory
information.
Personal data This information (age, gender, place of residence, occupation) will allow
you not only to determine who the patient is, but also to get a rough idea of what kind of
person they are and what health problems they may have.
Questioning method
it can match one of the following parameters:
two options:
1). Give an opportunity to the patient
speak out in free style on
different stages of collecting complaints and
anamnesis, specifying only individual cases
the details.
2). Ask the patient to respond
short and accurate answers to your questions
questions. At the same time, the following parameters are set:
the patient should have the following questions:
be clear, clear, and understandable.
13.
The second method is preferable, since you are not overloaded with information that does notcarry information about the disease itself, but rather receive concentrated data about the
development of the disease.
To get complete information when communicating with the patient, you must adhere to the
following principles:: 1) questions should be prepared in advance, which facilitates
communication between the nurse and the patient, allows you not to miss important details;
2) use the most reliable source of information - if not the patient himself, then his next of kin; 3)
use the information obtained earlier
information about the patient's diagnoses
(from
medical records, from members
medical team) to
plan in advance on which day
focus information
attention;
4) call the patient by their first name and
please indicate your patronymic and show
friendliness,
participation and care;
5) speak clearly, slowly and clearly.
clearly;
6) during the conversation, it is recommended
to
keep short records to
don't forget important information.
14.
Subjective survey• Finding out about complaints
Main complaints. It is better to write down the words of the patient himself: "My stomach
hurts, I feel very bad." Sometimes patients do not make explicit complaints, but state the
purpose of hospitalization: "I was admitted just for examination."
If the disease is accompanied by pain, we find out the following details::
- location of localization;
- radiation (where does it go?);
- character (what does it resemble?);
- intensity (how strong is it?);
- time of occurrence (when does it start, how long does it last, and how often does it
appear?);
- the circumstances under which it occurs (environmental factors, emotional reactions,
or other circumstances);
- factors that aggravate or relieve pain (physical or emotional stress, hypothermia,
taking medications (what exactly, in what quantities), etc.);
- concomitant manifestations (shortness of breath, arterial hypertension, ischuria,
dizziness, tachycardia, dilated pupils, forced posture, facial expressions, etc.). Need to
find out: what the patient himself thinks about his illness, what made him go to the
doctor, how the disease affected his life and activity.
15.
History of the present diseaseHistory of the present disease –Anamnesis of the disease (Anamnesis morbi)
Here you should clearly indicate in chronological order the health problems that caused
the patient to seek medical help. The information may come from the patient or his
environment. Nursing staff should organize the information.
Immediate reasons for the current hospitalization or current treatment:
- deterioration of the condition;
- ineffectiveness of previous planned treatment;
- emergency admission;
- the appearance of complications that require diagnostic clarification and medical
correction.
Questioning the patient about the development of the disease is carried out
according to a certain scheme:
- The beginning of the disease – (when and how it started, acute or gradual); What were
its first manifestations?
- Further course of the disease – the main stages of its development;
- Previous treatment – what measures and remedies were prescribed?
How were they applied? What are the results of treatment?
16.
History of the present diseaseMedical history (Anamnesis morbi)
The history of the development of chronic diseases must include::
- year of onset of the disease (or how many years the patient considers himself sick);
- the first symptoms of the disease;
- dynamics of the disease in chronological order from diagnosis to the present time;
- periods of exacerbation and remission;
- ongoing medical and preventive measures.
Here you need to detail everything:
- what treatment the patient received (including before hospitalization);
- effectiveness of therapeutic and preventive measures;
- daily dose of the received drugs;
- what symptoms of the disease disappeared, what appeared as a result of taking
medications;
- duration of taking certain medications (days, weeks, years)..
After a detailed inquiry about the present disease, we proceed to inquire about the
entire life of the patient that preceded it, paying special attention to those facts that
could directly affect the development of the disease.
17.
Anamnesis of life (Anamnesis vitae-the memory of life)Anamnesis of life: The patient's condition at the time of examination, living conditions,
habits, and attitude to health allow us to identify the strengths and weaknesses that
need to be taken into account when planning nursing care. Questions about the
patient's life are also conducted in a certain sequence:
- Biographical information. Finding out the place of birth and time of residence in a
certain territory. How it grew and developed in childhood and adolescence. Patient's
education, beginning and nature of work.
- Occupational hazards: stress, hypothermia, radiation energy, vibration, alkalis, acids,
metals, etc., which can lead to the development of diseases.
- Previous illnesses in the past, the presence of chronic diseases, as well as injuries
and operations are subject to detailed clarification, since many diseases leave behind
heart damage, and knowledge of anamnestic data simplifies and accelerates the correct
diagnosis.
- Heredity It plays an important role in the development of many diseases (for example:
polycystic kidney disease, hypertension, diabetes mellitus, etc.), so it is important to find
out the presence of diseases in the patient's parents, brothers, sisters, as well as in his
children. If a family pathology is detected, relatives may be involved in the examination
and treatment.
18.
Life history (Anamnesis vitae)- Bad habits (habitual intoxications) They can be both causes of the disease and
factors that provoke an exacerbation of existing chronic diseases (peptic ulcer of the
stomach and duodenum, chronic bronchitis, chronic hepatitis, etc.). Therefore, it is
important to find out whether the patient is abusing alcohol or not. In what quantity and
how often (daily, periodically, occasionally) the patient consumes alcohol. With regard to
smoking, you should find out at what age the patient smokes? The number of cigarettes
smoked per day? Does he use narcotic drugs and what drugs? When did I first start
using them? What is the daily dose and method of administration? - Allergic history. It
is important to find out whether the patient suffers from allergies in one form or another:
skin rashes, bronchial asthma, urticaria, swelling of the face or larynx, anaphylactic
shock. Did the patient have any allergic reactions to certain foods, odors, medications,
and among them, especially to antibiotics? Data on allergic complications must be noted
on the title page of the medical history.
- Epidemiological history. It provides for the clarification of contacts with infectious
patients, the patient's stay in epidemiologically dangerous regions. Whether there were
blood transfusions. Have you ever had tuberculosis, hepatitis, or sexually transmitted
diseases in the past? If the patient's relatives or neighbors are ill with tuberculosis, then
the group of their dispensary registration should be noted.
19.
Life history (Anamnesis vitae)- Family life and gynecological history (for women). Time of starting a family,
children's health, family relationships. The onset of menstruation, its regularity and
duration, soreness, and the amount of blood loss. Contraceptive use, number of
pregnancies, births, and abortions. In the presence of menopause – the time of its
appearance, features of the course.
- Psychological history it helps you get to know the patient as a person, assess his
likely reactions to the disease, his mechanisms of adaptation to the situation, the
patient's strength, and his anxiety.
- Insurance history. For acute diseases-from what date is the temporary disability
sheet; for chronic diseases-from what date is the last temporary disability sheet? How
many days of disability were there during the year for this disease? If there is a disability
group, what is it and from what time? For what medical condition? As well as the terms
of the last re-examination.
After collecting the patient's complaints and anamnesis, before proceeding to an
objective examination, a cursory, systematic survey of the patient regarding the state of
the most important body functions should be conducted again. Such a survey will allow
you to assess the overall state of the body and exclude possible omissions.
20.
Additional inquiry about the state of the patient's body functions(Status functionalis).
It is called a study of the functional state of the patient:
- general manifestations of the disease: weakness, emaciation, fever;
- central nervous system: headache, fainting spells, convulsions, sleep disorders;
- musculoskeletal system: pain in bones, joints, and muscles;
- respiratory system: chest pain when breathing and coughing, cough dry or with
phlegm, shortness of breath;
- cardiovascular system: pain in the heart, rhythm disturbances( interruptions),
shortness of breath, swelling of the lower extremities, increased blood pressure;
- the digestive system: loss of appetite, nausea, belching, vomiting, bloating,
constipation, diarrhea, taste distortion, and difficulty swallowing;
- urinary system: swelling, pain in the lumbar region, painful urination, discoloration of
urine;
- hematopoietic system: increased bleeding and hemorrhage on the skin and mucous
membranes;
- nervous system: paresthesia, numbness and sensory disturbances in the extremities;
- endocrine system: thirst, dry mouth, changes in body weight, convulsions, increased
excitability, severe weakness, headache.
After the interview, the nurse organizes and records the data obtained, noting the points
that are not fully clarified, if any.
21.
Objective examination22.
Introductory testingGive a detailed answer to the question
1. What sections does the objective survey include?
2. What sections does the general inspection consist of?
3. How is the patient's general condition assessed?
4. What are the types of consciousness?
5. What scale is most often used to assess the degree of impaired consciousness?
6. What are the main positions of the patient?
7. Types of functional positions of the patient in bed?
8. List the main methods of anthropometry.
9. The main body types of a person?
10. What stages does the algorithm for determining the patient's body weight consist of?
11. How is the patient's height measured?
12. What are the changes in the color of the skin and mucous membranes?
13. What should I pay attention to when assessing the state of the senses?
14. What is included in the assessment of the upper body?
15. What is the patient's facial expression?
16. Why do I need to assess the condition of the mammary glands?
17. What is necessary to determine the state of the musculoskeletal system?
23.
Objective examinationNursing process –a mandatory component of nursing activities, so the patient's
examination is recommended to be carried out according to a certain plan in compliance
with the necessary rules. Assessment of the patient's condition begins with a general
examination, then proceeds to palpation( palpation), percussion (tapping), auscultation
(listening).
Perfect command of percussion, palpation and auscultation is a professional task
of a doctor and a nurse with a higher education.
Objective examination the patient begins with a general examination. For a nurse, the
objective research method is essential, as it provides the most complete objective
information about the patient, so the nurse should be well versed in this research
method.
Observation should be carried out in diffused daylight or bright artificial light, and the
light source should be located on the side, so the contours of various parts of the body
stand out more clearly.
24.
Assessment of the patient's general conditionGeneral examination of the patient — this is the first, initial stage of objective
research, and it is also one of the methods of physical examination. It is performed after
collecting complaints and anamnesis, and is performed through visual examination.
General examination of the patient includes assessment of the general condition of the
patient, assessment of his consciousness, determination of the patient's position in bed,
assessment of the condition of the skin and visible mucous membranes, skin and its
appendages, subcutaneous fat, peripheral lymph nodes, and musculoskeletal system.
25.
General condition of the patientThere are the following gradations of the general condition::
Satisfactory condition it is determined when the functions of vital systems are
compensated, subjective and objective manifestations of the disease are not
pronounced sharply, consciousness is clear, the position is active, nutrition is not
disturbed, the temperature is normal or subfebrile.
Moderate condition It is determined when the functions of vital systems are in the
stage of subcompensation (partial disorder, when the clinical symptoms gradually
increase and the state of health worsens), but do not pose an immediate threat to the
patient's life. Subjective and objective manifestations of the disease are expressed,
consciousness is preserved or its confusion is noted. The patient's motor activity is
limited, the position in bed is usually forced, but the patient can usually serve himself.
Chills, high fever, weight loss and swelling are possible.
Serious condition it usually develops as a result of decompensation of vital body
systems and can pose a threat to the patient's life. Consciousness is depressed (stupor
or sopor), delirium is possible. The patient's position is passive or forced, and the patient
cannot serve himself. The symptoms of the disease are pronounced, signs of
complications of the underlying disease are revealed, sometimes rapidly progressing,
which often obscures the clinic of the underlying pathology (for example, the clinic of
cerebral circulation disorders in a patient with hypertension).
26.
General condition of the patientExtremely severe (pre-diagonal) condition it is observed with a sharp violation of the
function of vital systems of the body, and so pronounced that without urgent medical
measures, the patient may die in the near future. Consciousness is usually disturbed
(from stunning to coma), although in some cases it remains clear. The position is most
often passive or forced, possibly motor arousal, convulsions.
Terminal (agonal) state — these are conditions that borderline between life and death,
a critical level of vital activity disorder with a catastrophic drop in blood pressure, a deep
violation of gas exchange and metabolism. It is characterized by fading of
consciousness, relaxation of muscles; the cornea becomes cloudy, breathing becomes
periodic (like Kussmaul, Cheyne-Stokes, or Biot); the functions of the nervous system
fade. The duration of the terminal (agonal) state can vary from a few minutes to
several hours.
Clinical death status — this is a terminal state of the body, in which there is no
respiration and heartbeat, the pulse is not felt even on the carotid arteries, lack of
reflexes; dilated pupils, lack of reaction to light; The state of clinical death usually lasts
from 3 to 6 minutes. With a longer absence of heartbeat and breathing, a person dies.
The main difference between clinical and biological death is reversibility, the ability to
bring a person back to life if resuscitation measures are carried out in time.
27.
Patient's state of consciousnessWhen evaluating them, you need to find out how well they perceive the environment,
how they react to the medical staff, whether they understand the questions they are
asked, how quickly they respond, and whether they tend to lose the thread of
conversation, fall silent, or fall asleep.
If the patient does not answer the questions, you can use the following
techniques::
speak loudly to him;
shake it slightly, as you do when you wake up a sleeping person. If the patient is still
unresponsive, it should be determined whether he is in a state of stupor or coma.
The loss of consciousness can be short-term or long-term.
Assessment of the state of consciousness:
1. Clear consciousness - the patient is oriented in space and time, is able to
adequately perceive and comprehend the surrounding reality. Answers your questions
appropriately, quickly, and concretely.
2. Confusion - the patient is sluggish, answers questions correctly, but slowly, with
difficulty.
3. Stupor state (stupor) - a state of deafness, numbness, the patient is poorly oriented
in the environment, the patient answers questions late and does not make sense.
28.
Assessment of the state of consciousness:4. Soporotic state (sopor) - pathological deep sleep, the patient is unconscious,
reflexes are not preserved, a loud voice can bring him out of this state, but he soon falls
back into sleep.
5. Comatose state (coma) - complete suppression of the functions of the central
nervous system: consciousness is absent, muscles are relaxed, lack of sensory and
motor reflexes. It occurs with acute cerebrovascular accident – brain hemorrhages,
diabetes mellitus, kidney and liver failure.
In some diseases, there are disorders of consciousness which are based on the
excitation of the central nervous system. These include delusions, hallucinations
(auditory and visual).
To assess the degree of impaired consciousness and comas of children over 4
years of age and adults are widely used the Glasgow Coma Scale. It consists of three
tests to evaluate: eye-opening responses (E), speech responses (V), and motor
responses (M). After each test, a certain number of points are awarded, and then the
total amount is calculated. Interpretation of the results obtained:
15 points - clear mind;
13-14 points - stunning;
9-12 points - sopor;
6-8 points - moderate coma;
4-5 points - terminal coma;
3 points - death of the bark.
29.
Coma scale Glasgow – The Glasgow Coma Scale (GCS)30.
Patient's position.It depends on the general condition. There are three types of patient position: active,
passive, and forced.
Active – the patient can change his position independently, move easily, take any
position, sit down, get up, move around, serve himself. This situation is typical for
patients with a mild course of the disease. Passive – the patient cannot perform active
movements, is sedentary, cannot turn independently, raise his head, arm, or change
body position. Causes: depression of consciousness, extreme weakness, intoxication,
damage to the nervous and muscular systems.
Forced position the patient takes medication to relieve their condition (reduce
shortness of breath, cough, pain):
- for abdominal pain associated with inflammation of the peritoneum, the patient lies
with his legs bent, avoiding any contact with the abdomen;
- in pleurisy, the patient lies on the affected side to reduce pain and ease the excursion
of a healthy lung;
- with shortness of breath, he sits with his legs down, holding hands on a chair, couch,
bed. Pain is indicated by suffering on the face, increased sweating. When placing the
patient, it is necessary to attach functional provisions they promote the
physiological location of body parts and reduce the risk of developing potential
complications due to immobility.
31.
Types of functional positions of the patient in bedLying on your back. Lying on your stomach. Lying on your side. Sitting.
Trendelenburg's position - lying horizontally on your back, without a pillow, with your
legs raised. Promotes blood flow through the veins of the lower extremities and blood
flow to the head. It is recommended for the prevention of thromboembolism, acute
vascular insufficiency (syncope, collapse, shock), signs of bleeding from the
gastrointestinal tract.
Fowler (reclining/half-sitting) - lying on your back with the headboard raised at an
angle of 45-60%. Bedsore prevention, breathing relief, communication and patient care
are provided.
Sims ' position – an intermediate position between lying on the stomach and on the
side - to facilitate breathing in patients with neurological diseases, including stroke.
Orthopnea position - sitting, with the torso tilted forward, resting your hands on the bed
to facilitate breathing, the pose allows the lungs to expand freely and makes breathing
easier.
When placing the patient in the desired position, it is necessary to use additional pillows
and rollers, a stop for the feet and other devices.
To create a comfortable patient content, a functional bed is used, equipped with three
movable sections, side handrails. The bed has a built-in bedside table, nests for a
vessel and a urinal, and other additional devices that facilitate the patient's condition
and care.
32.
AnthropometryAnthropometry - methods for determining the features of a person's physique and
physical development. We find out from the patient what his usual body weight is,
whether it has changed recently.
In patients with impaired nutritional needs and excretion of waste products from the
body, body weight and height data are used as the main indicators for treatment. A
person's body weight depends to a large extent on their diet, heredity, previous illnesses,
and socio-economic status.
It is not uncommon for nursing staff to determine patients ' height and body weight,
especially during routine checkups. The scale-growth meter device produced by the
medical industry allows you to make these measurements with great time savings.
With the simplest method of calculation, the normal body weight of a person should be
equal to his height in centimeters minus 100. So, when a person is 170 cm tall, the
normal body weight is 70 kg.
Body Mass Index (BMI or body mass index BMI) – this is the ratio of weight to height
squared:
20-25 is the ideal weight, and the health risks are minimal.
25-30 – the presence of excess weight.
30-35 – the first stage of obesity, a significant increase in health risks. 35 or more –
obesity, weight correction is necessary.
33.
human body typesThere are three main types of human physique::
1. Mesomorphic (normosthenics). This type includes people whose anatomical
features are close to the average parameters of the norm (taking into account age,
gender, etc.).
2. Brachymorphic (hypersthenics). People of this type are mostly transverse in size,
well-muscled, and not very tall.
3. Dolichomorphic (asthenics). People of this type are characterized by a
predominance of longitudinal dimensions, have relatively longer limbs, poorly developed
muscles and a thin layer of subcutaneous fat, narrow bones.
34.
Algorithm for determining the patient's body weightGoal: assessment of physical development or the effectiveness of treatment and
nursing.
Indications: routine checkup, diseases of the cardiovascular, respiratory, digestive,
urinary, or endocrine systems. Prepare the patient:
a) warn about manipulation, in the morning on an empty stomach before eating;
b) offer to empty your bladder and bowel;
c) ask the patient to strip down to their underwear and be sure to take off their shoes.
Sequence of actions:
1. Check the health and accuracy of the medical scale.
2. Place a disposable napkin or plain sheet of paper on the scale pad.
3. Invite the patient to stand in the middle of the scale platform, with the shutter lowered.
4. Lift the scale's lock, adjust the balance using the weights located on the upper and
lower bars of the scale - as a result, you will get the patient's body weight. Help the
patient off the weighing platform.
5. Enter the received data in the appropriate column in the patient's condition monitoring
sheet. Share the data with the patient.
6. Remove the napkin from the pad and throw it in the trash can. Wash your hands.
35.
Algorithm for measuring patient heightGoal: assessment of physical development.
Indications: check-up at admission to the hospital or a routine check-up. Sequence of
actions:
1. Check that the height meter is working properly.
2. Place a napkin on the height meter pad.
3. Lift the height meter bar up and ask the patient to stand on the height meter platform
with his back to the scale so that the back of his head, shoulder blades, buttocks and
heels fit snugly against it.
4. The head should be in such a position that the upper edge of the external ear canal
and the corners of the eyes are on the same horizontal line.
5. Lower the bar to the patient's crown and mark the length of his body along the lower
edge of the bar. Help the patient get off the height meter.
6. Write down the received data in the observation list. Report the received data to the
patient.
7. Remove the foot cloth from the height meter pad and throw it in the trash can.
Note. If the patient is unable to stand, the measurement is performed while the patient is
in a sitting position. The patient should be offered a chair. The points of fixation will be
the sacrum and the interscapular space. Measure your height in a sitting position.
Record the results.
36.
Measurement algorithm chest circumferenceSequence of actions:
1. Check the integrity of the centimeter tape and the clarity of the numbers applied.
2. Wash and dry your hands and put on gloves.
3. Ask the patient to release the chest from the clothes and move the arms slightly to the
sides.
4. Apply a centimeter tape from the back - at the lower corners of the shoulder blades, in
front - in mizhchins at the level just below the nipples, in women-on 4 ribs, above the
base of the breast or under the mammary glands. The tape is applied tightly, but without
tension.
When measuring, the patient's hands are lowered, and breathing is free.
To determine the respiratory excursion of the chest is performed
measuring chest circumference three times:
a) at rest;
b) at maximum inspiration;
c) at maximum exhalation;
the difference between these measurements is equal to the chest breathing excursion;
5. At the end of the procedure, inform the patient of the measurement result, place a
centimeter tape in a container with a disinfectant solution, treat your hands in a hygienic
way, dry them and record the results in the appropriate medical documentation.
37.
Measurement of abdominal circumference:Goal:
a) detection of fluid accumulation in the abdominal cavity (ascites);
b) measurement of the abdominal circumference of a pregnant woman;
c) specifying the volume of the abdomen for selecting the size of underwear.
Sequence of actions:
1. Warn the patient the day before that a measurement will be performed on an empty
stomach in the morning.
2. Place a centimeter tape at the back-at the level of the third lumbar vertebra, in front-at
the level of the navel.
3. Inform the patient of the measurement result. Enter the received data in the
observation list.
Algorithm dimensions circles heads.
Preparing for the procedure:
1. Prepare the necessary equipment.
2. Introduce yourself to the patient and explain the course of the upcoming
procedure.
3. Treat your hands in a hygienic way, dry them.
4. Ask the patient to sit down.
Performing the procedure:
5. Apply a centimeter tape to the head patient's reference points: occipital
protuberance at the back, brow ridges at the front.
6. Determine the measurement result. Inform the patient of the measurement result.
Enter the received data in the observation list.
38.
Assessment of skin and visible mucous membranesThere are several characteristic changes in the color of the skin and mucous
membranes:
1. Hyperemia (redness). It can be temporary, due to taking a hot bath, alcohol, fever,
strong excitement, and permanent, associated with arterial hypertension, working in the
wind or in a hot room.
2. Pallor. Pallor of a temporary nature can be caused by excitement or hypothermia.
Pronounced pallor of the skin is characteristic of blood loss, fainting, collapse.
Hyperemia and pallor are most noticeable on the nail plates, lips and mucous
membranes, especially on the oral mucosa and conjunctiva.
3. Cyanosis (cyanosis). It can be general or local, central or peripheral. Common is
characteristic of cardiovascular insufficiency. Local, for example, for thrombophlebitis.
Central cyanosis is more pronounced on the lips and the mucous membrane of the
mouth and tongue.
4. Icteric (jaundice) sclera indicates a possible liver pathology or increased hemolysis.
Jaundice of the palms, face and soles may be due to the high carotene content in the
patient's food.
Subcutaneous fat. Degree of development (excessive, moderate, weak, insufficient,
etc.). Distribution (uniform, if uneven, indicate the places of predominant fat deposition).
Edema: localization, density, and pasty content.
39.
Assessment of skin and visible mucous membranesElasticity and turgor (elasticity). It is necessary to determine whether the skin easily
gathers into a fold (elasticity) and whether it quickly straightens after that (turgor).
Palpation is a commonly used method for assessing skin elasticity.
A decrease in the elasticity and firmness of the skin, its tightness is observed with
edema, scleroderma. Dry and inelastic skin can indicate tumor processes and
dehydration of the body.
Pathological elements of the skin. When detecting pathological elements, it is
necessary to indicate their features, localization and distribution on the body, the nature
of their location, the specific type and time of their occurrence (for example, in a rash).
During the examination, it is necessary to pay special attention to them, since the cause
of their occurrence can be not only dry skin, allergic reactions, diabetes mellitus or other
pathology, but also a scabies mite.
Hairline. During the examination, it is necessary to pay attention to the nature of hair
growth, the amount of hair of the patient. People often worry about hair loss or
excessive hair loss. A thorough examination allows you to identify people with
pediculosis (lice). Nails. It is necessary to examine and feel the nails on the hands and
feet. Thickening and discoloration of the nail plates, their fragility can be caused by
fungal damage.
40.
Assessment of the state of the sensesOrgans of vision. Assessment of the patient's visual organs can begin with the
questions: "How are your vision problems?", " Are your eyes bothered?". If the patient
notices a deterioration in vision, it is necessary to find out whether this has happened
gradually or suddenly, whether he wears glasses, where and how he keeps them.
Organs of hearing. Before proceeding with their examination, you should ask the
patient if he hears well. If a person complains of hearing loss, it is necessary to find out
whether it affects both ears or one, whether it occurred suddenly or gradually, whether it
was accompanied by discharge or pain. You need to find out if the patient is wearing a
hearing aid, and if so, the type of hearing aid.
Using the information obtained about hearing loss and visual acuity, the nurse will be
able to communicate effectively with the patient.
Organs of smell. First, you need to find out how much the patient is susceptible to
colds, whether he often notes nasal congestion, discharge, itching, whether he suffers
from nosebleeds. If the patient has allergic rhinitis, you should specify the nature of the
allergen and the previously used methods of treating this disease. It is necessary to
identify pollinosis, pathology of the paranasal sinuses.
Oral cavity and pharynx. When examining the oral cavity, you need to pay attention to
the condition of the patient's teeth and gums, ulceration on the tongue, dry mouth, if
there are dentures, check their fit. Plaque on the tongue – can be the cause of bad smell
and reduced taste sensations, and sore throat-the cause of sore throat or ARVI.
All this should be taken into account when planning nursing care.
41.
Upper body assessmentHead. First of all, you need to find out if the patient has any complaints of headache,
dizziness, or injuries. Headache is very common in patients of all ages. It is necessary
to find out its nature (it is constant or throbbing, acute or dull), localization, whether it
first appeared or is characterized by a chronic course. When migraines are often
observed not only headache, but also its accompanying symptoms (nausea and
vomiting).
Hair: type of hair loss (male, female), severity and localization of baldness, gray hair.
Nails: shape (normal, flat, spoon-shaped, in the form of watch glasses), the presence of
trophic disorders (dull .brittle, crumbling).
Neck. When examining the neck, various swellings, swollen glands, goiter, and pain are
detected. Thyroid gland. Degree of development, size, location of lobes, density,
uniformity of compaction, presence of nodes, isthmuses, mobility.
Lymph nodes. Localization: occipital, parotid, submandibular, cervical, supraclavicular,
subclavian, axillary, ulnar, inguinal, popliteal (palpable, not palpable). Size in
centimeters, consistency, soreness, mobility.
When assessing the condition of the upper body, pay attention to the proportionality of
the structure of individual parts of the body: evaluate the symmetry of both halves of the
trunk, the shape and size of the head, the length of the neck and limbs, the ratio of the
size of the thoracic and abdominal parts.
42.
Upper body assessmentPay attention to the patient's face and eyes. Facial expression allows you to judge the
internal state of the patient. It can express anxiety, longing, or fear.
The face of a feverish patient - against the background of a pale face, bright eyes and
flushed cheeks.
The face of "nephritik"- puffiness, pallor of the face, swollen eyelids, especially in the
morning.
Myxedema patient's face (lack of thyroid hormones) - pale, without facial expressions,
masked, puffy face.
Face of a patient suffering from mitral heart disease - a cyanotic blush in the shape
of a butterfly against a pale face.
"The Face of Corvisar" - edematous yellowish-pale, cyanotic, eyes dull, mouth slightly
open-characteristic of heart failure.
"The face of bazedovik", suffering from thyrotoxicosis - a frightened look, wide-open
eye slits and bulging of the eyeballs (exophthalmos-popeye).
«The face of Hippocrates"- his eyes were sunken, his nose pointed, and his skin was
pale and bluish, covered with sweat.
Constriction of the pupils - it is observed with alcohol, drug poisoning, as well as with
uremia. Dilated pupils - for atropine poisoning. A fixed gaze directed at one point is
found in meningitis.
43.
Breast health assessmentOn inspection they find out whether a woman makes an independent examination of
the mammary glands, whether there is discomfort in the mammary gland, whether a
woman is seen by an oncologist, whether there are menstrual disorders, whether there
is an engorgement and soreness of the glands in the premenstrual period. It is
necessary to regularly conduct a self-examination of the mammary glands, usually
every month. It is better to examine the breast for 5-7 days after the end of
menstruation.
With discharge from the nipple specify when they appeared, their color, consistency,
and amount; they are released from one or both glands. During the survey breast
asymmetry, engorgement, compaction, or the absence of one or both mammary glands
may be detected. The risk of developing breast cancer increases in the presence of a
number of factors: older age, obesity, alcohol consumption, family history of breast
cancer, history of radiation exposure, reproductive history (for example, age of
menstruation and age of first pregnancy), tobacco use and hormone therapy during
postmenopause. Pathology of the mammary glands is quite common in women,
including young ones. It must be remembered that the loss of a breast can be a great
psychological trauma for a woman and affect the satisfaction of her needs for sex. If the
patient does not know how to perform a breast exam on her own, you can include
training in these techniques in the nursing plan.
44.
Assessment of the musculoskeletal systemTo determine the state of this system, you first need to find out if the patient is
concerned about pain in the joints, bones and muscles. When complaining of pain, you
should find out their exact localization, area of distribution, symmetry, radiation, nature
and intensity. It is important to determine what contributes to the increase or decrease in
pain, how physical activity affects it, and whether it is accompanied by any other
symptoms.
Examination reveals deformities (curvatures, thickenings), their localization, limited
mobility of the skeleton, joints. Soreness: conditions of occurrence (when beating, when
feeling).
Joint examination. When joint mobility is restricted, it is necessary to find out what
movements and to what extent are disrupted: whether the patient can freely walk, stand,
sit, bend over, get up, comb his hair, brush his teeth, eat, dress, wash. Changes in the
shape (swelling, deformity). Changes in the skin over the joints. Skin temperature.
Soreness during palpation and movement. Volume of active and passive movements.
Limited mobility leads to limited self-service. Such patients are at risk of developing
pressure sores and infection, and therefore require increased attention from nursing
staff.
Assessment of muscle condition. The nurse examines the muscles for their volume,
tone (muscle relaxation when at rest), strength, and soreness. Also, the muscles are
checked for twitches and involuntary movements.
45.
Introductory testingGive a detailed answer to the question
1. How is the skin temperature measured in humans?
2. What are the main types of thermometers for measuring body temperature?
3. Methods and locations for measuring human body temperature?
4. What is the human body temperature?
5. What can be the types of fevers by the nature of temperature fluctuations?
6. Fever periods and nursing interventions, depending on the period?
7. What are the stages and types of breathing?
8. What are the rhythms of respiratory movements and types of shortness of breath?
9. What are the variants of abnormal breathing?
10. What stages does chest palpation involve?
11. What is chest percussion?
12. What is auscultation?
13. Tasks and rules of lung auscultation?
14. What side respiratory noises are detected during auscultation of the lungs?
46.
Thermometry and characterization of human body temperatureSkin temperature. By touching the patient's skin with the back of your fingers, you can
judge its temperature. In addition to evaluating the overall temperature, it is necessary
to check the temperature on any reddened area of the skin. With the inflammatory
process, a local increase in temperature is noted. Body temperature is usually
measured with a maximum medical thermometer. Medical mercury (maximum)
thermometer is called because it shows the maximum height of the mercury column
rise. It can measure temperatures from 34 to 42 degrees Celsius.
47.
Types of thermometers for measuring body temperature• Mercury (maximum) thermometer. It is considered one of the most accurate types
and at the same time affordable. In addition, it is used in hospitals and clinics, as it is
easily disinfected and can be used for a large number of people. Disadvantages include
slow temperature measurement and brittleness. And a broken thermometer is
dangerous with toxic mercury vapors. Therefore, for children today it is used quite
rarely, it is not used for oral measurement.
48.
Types of thermometers for measuring body temperature• Electronic (digital) thermometer. The most popular type for home use. It quickly
measures the temperature (from 30 seconds to 1.5 minutes), notifies you of heating with
an audible signal, after which the thermometer must be held for at least 1 more minute,
otherwise the indicators will be incorrect! Electronic thermometers can be equipped with
soft tips (for rectal temperature measurement in a child) and hard ones (universal
devices). If the thermometer is used rectally or orally, it must be individual – only for one
person, and after each use it must be disinfected to prevent the growth of bacteria.
49.
Types of thermometers for measuring body temperature• Infrared thermometer. It is used to measure temperature in a non-contact way, for
example, in the ear, on the forehead or temple. The speed of getting the result is 2-5
seconds. A slight error of 0.2-0.5°C is allowed. A significant disadvantage of the
thermometer is its limited use – it is not used for measurements by the usual methods
(axillary, rectal, oral). In addition, each model is designed for its own method (forehead,
temple, ear) and cannot be used in other areas.
50.
Methods and locations for measuring body temperatureMethods for measuring body temperature:
Usually, body temperature is measured 2 times a day (at 7-9 in the morning and at 1719 in the evening). As a rule, systematic measurement of body temperature 2 times a
day makes it possible to get an idea of its daily fluctuations, so measure the temperature
at shorter intervals (6-4-2 hours). no need.
Main body temperature measurement area - armpit area; the skin should be
dry, as if perspiration is present, the thermometer may indicate a temperature 0.5°C
lower than the real one. The duration of measuring body temperature with a mercury
thermometer is at least 10 minutes. After measuring, the thermometer is shaken and
lowered into a container with a disinfectant solution.
Places where body temperature is measured:
• armpits - 10 minutes;
• oral cavity (the thermometer is placed under the tongue) - 1 minute;
• inguinal folds (for children) - 5 minutes;
• rectum - 5 minutes
(the temperature in the rectum is 0.5-1°C higher than in the armpit).
51.
Characteristics of human body temperature1) hypothermic - below 35 ° C;
2) normal – 36.2-36.9 ° C;
3) subfebrile – 37-38 ° C;
4) febrile – 38.1 -39.0 ° C;
5) pyretic – 39.1-41.0 ° C;
6) hyperpyretic more than 41 ° C.
Maximum (lethal) the body temperature is 43 °C, with irreversible changes at the
cellular level, metabolism is disrupted and death occurs.
Minimum body temperature, at which irreversible processes are also observed, — 2315 °C.
Classification of fevers:
By duration:
fleeting – up to 2 hours;
acute – from several hours to 15 days;
acute, ephemeral – from a few hours to 2 days;
subacute – from 10 days to 45 days;
/ chronic – more than 45 days.
52.
Types of fevers by the nature of temperature fluctuations:1. Permanent – daily fluctuations within a degree (typical for croup pneumonia, typhus).
2. Relaxing (remitting) – fluctuations with a temperature difference of more than 1 ° C
in the morning and evening (typical for purulent diseases).
3. Debilitating (hectic) – fluctuations with a temperature difference during the day from
2 to 4 ° C (typical for tuberculosis, sepsis, lymphogranulomatosis).
4. Perverted –it is characterized by a rise in the morning temperature to a greater
extent than in the evening (typical for tuberculosis, sepsis).
5. Atypical – irregular, of various sizes and duration (typical for influenza, rheumatism,
dysentery).
6. Intermittent – or intermittent, characterized by a sharp rise to 39-40 ° C and above,
lasts for several days, and then its cycle repeats (typical for malaria).
7. Undulating – it is characterized by alternating periods of growth with periods of
falling to normal (typical for lymphogranulomatosis, brucellosis).
53.
Fever periods and nursing interventions1 period – body temperature rise. Heat production prevails over heat transfer. The
patient has chills, general malaise, weakness, and body aches. Shivering on
examination, skin pale and cold to the touch.
Purpose of nursing care: ease the patient's condition.
Nursing interventions: 1. Create peace (bed rest, silence, dimmed lights) - reducing
the load on vital organs.
2. Cover up, apply hot water bottles to your feet, provide plenty of warm drinks (reducing
chills, reducing heat transfer).
3. Monitor the general condition, TSC, blood pressure, pulse, and BPD (early detection
of complications).
54.
Fever periods and nursing interventions2 period – relative constancy of temperature. Heat production is balanced with
increasing heat transfer.
The patient has fever, decreased appetite, dry mouth. On examination, hyperemia of the
face, the skin is hot. At high T, delusions and hallucinations are possible.
Purpose of nursing care: help reduce T, prevent complications.
Nursing interventions:
1. Cover the patient with a light sheet, blow his body with a fan, wipe the skin with
slightly evaporating liquids, apply an ice pack or cold compress to the head (increased
heat transfer).
2. Provide with a drink-not less than 1.5-2 liters, feed with liquid, semi-liquid easily
digestible food 5-6 times a day (reducing intoxication). 3. Irrigate the oral mucosa and
lips with water, lubricate the lips with glycerin, treat cracks on the lips with antiseptic
solutions (elimination of dryness of the oral mucosa and lips, treatment of cracks on the
lips).
4. Conduct dynamic monitoring of the general condition, T, blood pressure, pulse, BPD,
monitor behavioral reactions and especially diuresis- (early detection of complications).
5. When T is higher than 39 ° C, enter antipyretics (treatment of hyperthermia) as
prescribed by a doctor.
55.
Fever periods and nursing interventions3 period - decrease in body temperature. Heat output is reduced compared to heat
transfer.
Body temperature may decrease gradually (leasing services) for several days-optimal
for the patient.
Another option is to reduce the T sharply, within a few hours (crisis)- may be
complicated by a decrease in vascular tone, a sharp drop in blood pressure, up to
collapse.
Collapse - manifestation of acute vascular insufficiency with a sharp decrease in blood
pressure and a disorder of peripheral blood circulation. Symptoms of collapse:
weakness, dizziness, tinnitus, decreased visual acuity. The patient's skin is pale, sticky
sweat, pulse is rapid, threadlike, blood pressure is sharply reduced (systolic up to 80
mmHg).
Nursing interventions for lysis:
Purpose of nursing care: creating a comfortable environment, avoiding complications
1. Provide a change of underwear and bed linen if necessary, eliminate drafts
(prevention of complications, ensuring comfort).
2. Ensure adequate drinking and nutrition (reduce intoxication).
3. Monitor the general condition, T, blood pressure, pulse, BPD (early detection of
complications).
56.
Fever periods and nursing interventionsCrisis nursing interventions:
Purpose of nursing care: prevent acute vascular insufficiency
1. Call a doctor through an intermediary (ensuring continuity). 2. Lay the patient
horizontally, without a pillow (improving blood flow to the head).
3. Cover up, attach a hot water bottle to the feet, drink hot coffee, strong tea (prevention
of acute vascular insufficiency).
4. Prepare and administer medications that increase blood pressure (treatment of acute
vascular insufficiency) as prescribed by a doctor. The patient is given a horizontal
position and covered with hot water bottles. Subcutaneously, it is recommended to
introduce tonics-cordiamine, sulfocamphocaine or mezaton. If the use of these drugs
does not give a positive result, intravenous drip administration of 1-2 ml of 0.2%
norepinephrine solution in 150-200 ml of glucose solution or isotonic sodium chloride
solution is indicated.
By monitoring the patient's temperature, the nurse assesses the severity of the
condition, plans care activities that can alleviate the patient's condition, prevent
complications, and promote recovery.
57.
Assessment of the state of the respiratory system58.
Assessment of the state of the respiratory systemBreathing (inhalation or ventilation) — this is a rhythmic process of air movement in
(inhalation) and out (exhalation) of the lungs to facilitate gas exchange with the internal
environment, mainly for oxygen intake and carbon dioxide removal.
59.
Assessment of the state of the respiratory systemThe respiratory cycle consists of two phases:
• inhale (inspiration);
• exhale (expiration).
STAGES OF BREATHING: 1. Ventilation of the lungs - the entry of air into the airways and the exchange
of gases between the alveoli and the environment;
2. Gas exchange in the lungs - gas exchange between alveolar air and blood;
3. Transport of gases by blood – O2 from lungs to tissues and CO2 from body tissues to lungs;
4. Gas exchange in tissues – gas exchange between blood and body tissues;
5. Tissue respiration - consumption of O2 by tissues and release of CO2.
There are three types of breathing:
1. Thoracic type - breathing movements are carried out mainly due to the contraction of intercostal
muscles. At the same time, the chest expands and rises slightly during inhalation, and narrows and
slightly descends during exhalation. This type of breathing is typical for women.
2. Abdominal type - breathing movements are carried out mainly by contracting the muscles of the
diaphragm and abdominal wall. The movement of the diaphragm muscles increases intra-abdominal
pressure and when inhaled, the abdominal wall moves forward. When you exhale, the diaphragm relaxes
and rises, which shifts the abdominal wall back. This type of breathing is also called diaphragmatic. It
occurs mainly in men.
3. Mixed type - breathing movements are performed simultaneously by contracting the intercostal
muscles and the diaphragm.
First of all, it is necessary to pay attention to the change in the patient's voice; frequency, depth, rhythm
and type of breathing; chest excursion, assess the nature of shortness of breath, if any, the patient's
ability to transfer physical activity, find out the date of the last X-ray examination.
60.
Assessment of the state of the respiratory systemBreathing consists of the phases of inhalation and exhalation, which are carried
out in a certain constant rhythm-16-20 per minute in adults and 40-45 per minute in
newborns. The rhythm of breathing movements is breathing movements at certain
intervals. If these intervals are the same – breathing is rhythmic, if not - arrhythmic. In a
number of diseases, breathing can be shallow or very deep.
Tachypnea - frequent shallow breathing. Occurs when the level of carbon dioxide
concentration in the blood increases. It is observed with fever, pneumonia, congestion in
the lungs, atelectasis.
Bradypnea - rare breathing that occurs when the respiratory center is affected and
depressed against the background of hypoxia, edema, ischemia, or exposure to narcotic
substances.
Sleep Apnea - absence or stopping of respiratory movements. A pathological process
associated with a pathology of the respiratory muscles, for example, poisoning with
poison, or paralysis of the respiratory center, for example, as a result of brain edema or
traumatic brain injury. Shortness of breath or dyspnoea - violation of the frequency
and depth of breathing, accompanied by a feeling of lack of air. Inspiratory dyspnea
(difficult to inhale) - appears when the passage of air through the upper respiratory
tract is disrupted during inhalation. Expiratory dyspnea (difficult to exhale) occurs
when the lumen of small bronchi and bronchioles is narrowed (for example, in bronchial
asthma) or when the elasticity of the lung tissue is lost (for example, in emphysema).
61.
Abnormal types of breathingChain–Stokes Breathing it is characterized by alternating groups of respiratory
movements with increasing amplitude and periods of apnea (respiratory arrest). It
should be noted that Cheyne-Stokes respiration can occur not only in pathological
conditions, but also in normal conditions: in healthy people during sleep, in premature
babies with an immature respiratory regulation system, in old age (when there is an
increase in the threshold of excitability of the respiratory center).
Biot Respiration – this is an alternation of uniform breathing movements and long
pauses. There is no strict pattern of the number of breaths and the duration of pauses.
Causes: diseases of the nervous system (meningitis, meningoencephalitis, heat stroke,
severe poisoning).
Grokk's Breath – undulating breathing, which alternates between periods of shallow
and deep breathing. It occurs in the initial stages of coma development, when the
respiratory center loses its ability to coordinate its actions with other parts of the nervous
system. As a result, the respiratory muscles cannot contract in concert and provide
normal breathing phases.
Kussmaul's Breath - large, noisy, deep breathing (”the breath of a hunted beast") is
characterized by separate convulsive contractions of the main and auxiliary respiratory
muscles. This type of breathing indicates deep hypoxia of the brain. It is characteristic of
uremic and diabetic coma and other terminal conditions.
62.
Chest palpationChest palpation includes the following steps::
Detection of soreness. Palpation of the anterior surface of the chest is performed from
top to bottom with light pressure of the fingers, without missing the ribs, intercostal
spaces, and sternum. Then feel the axillary zones, starting from the armpits, and the
posterior surface of the chest in the following order: supracapular, interscapular and
subscapular areas. Pay attention to the presence of soreness, seals, protrusions and
depressions of the chest areas, crepitating crunch in case of rib fracture and
subcutaneous emphysema.. Normally, the chest is painless.
Determination of compliance (resistance) chest area. Hands are placed with the
palm surface on the chest and squeezed, first in the anterior-posterior direction, and
then in the lateral parts. Determine the degree of compliance of the chest (elasticity or
rigidity). Normally, the chest is pliable, elastic, in pathology-not elastic, not pliable. Voice
shake detection. Hands are placed with the palm surface on symmetrical areas of the
chest in the subclavian zones. Offer the patient to say in a low chest voice words
containing the letter " r " ("three hundred and thirty-three"). Determine the degree of
severity of trembling and carrying out the voice on the surface of the chest.
Examine the patient in the "sitting" or "standing" position.
63.
Chest percussionChest percussion – this is the application of percussion blows to the chest, which
cause the underlying organs to vibrate.
General rules of percussion:
• Percussion is performed on the naked body.
* The patient's position should be comfortable, the muscles relaxed, breathing calm and
even.
* The plessimeter finger fits snugly on the body, but without deep immersion.
* Strike the plessimeter finger in a strictly perpendicular direction.
* The percussion blow should be light, short, jerky, and always of equal force.
There is a distinction between comparative and topographical percussion:
Comparative percussion evaluates the nature of percussion sound over anatomically
equally located areas of the right and left lungs: in front-above and below the clavicles,
from the sides - along the axillary lines, from the back-along the paravertebral and
scapular lines. Sound-clear pulmonary, blunted, blunt, boxy, tympanic – specify
localization.
Topographic percussion it is used to determine the boundaries of the lungs. The
plessimeter finger is located parallel to the desired border and moves from a clear
pulmonary sound to a blunt one. The border is marked on the side of the plessimeter
that faces the clear sound. Chest percussion is performed in an upright position of the
patient-standing or sitting.
64.
Auscultation of the lungsAuscultation of the lungs – physical method of medical diagnosis, which consists in
listening to sounds generated during the functioning of the lungs.
Auscultation tasks:
* determination of the nature of breathing – the main respiratory noises;
* determination of side respiratory noises – wheezing, crepitation, pleural friction noise.
Rules for auscultation of the lungs:
Carry out in a vertical, horizontal or sitting position of the patient. Start listening from the
tops, assessing the nature of breathing (vesicular, bronchial, amphoric, the presence of
side respiratory noises) on the right and left sides comparatively. The patient is asked to
breathe deeply through the nose to assess the duration of the inhalation and exhalation
phase. Continue listening on symmetrical areas of the front surface of the chest, moving
the phonendoscope from top to bottom, bypassing the heart area.
I'm fine during auscultation, vesicular and laryngotracheal respiration can be heard.
Vesicular respiration (alveolar) - this is a soft blowing noise, similar to the "F" sound,
produced at the moment of inspiration and associated with vibrations of the walls of the
alveoli. Laryngotracheal (bronchial) respiration – this is a loud, high-frequency and
rough noise that occurs when air passes through the glottis. Adverse respiratory
noises - wheezing, crepitation and pleural friction noise are detected only in pathology.
65.
Lung auscultation pointsDuring auscultation from behind, the patient leans forward slightly, crossing his arms over his
chest. Auscultation from behind is performed in the position to the left of the patient. During
auscultation of the lungs, the main respiratory noises are determined first – vesicular (alveolar)
breathing and bronchial (laryngotracheal)condition breathing, and then – side respiratory
noises.
66.
Adverse respiratory sounds during auscultation of the lungsAdverse respiratory noises: wheezing, crepitation, pleural friction noise. There are
dry and wet wheezes. They are formed when air passes through the bronchial tree and
are heard both during the inhalation and exhalation phases. Also select wired wheezes,
the source of which is a lesion of the upper respiratory tract.
Dry wheezing they appear in the presence of a thick and viscous secretion in the
bronchi. By nature, dry wheezes can be high and low, or whistling and humming, or
treble and bass. Wheezing sounds are characteristic of bronchial asthma. For acute
bronchitis, pneumonia and other diseases associated with the accumulation of sputum
in the respiratory tract, the appearance of wet wheezing is characteristic.
Wet wheezes according to the caliber, they can be small-bubble, medium-bubble, and
large-bubble. It depends on the caliber of the bronchi that the exudate fills. Wheezing
occurs when the bronchi are filled with liquid secretions. Wet wheezing is formed in the
bronchi surrounded by airless, compacted lung tissue, for example, in croup pneumonia,
or in large smooth-walled cavities of the lungs surrounded by a dense inflammatory
roller. Most often, wet wheezing is observed in chronic bronchitis, as well as in the stage
of resolution of an attack of bronchial asthma.
67.
Adverse respiratory sounds during auscultation of the lungsCrepitus it is formed when the collapsed alveoli containing a small amount of fluid are
straightened. The walls of the alveoli stick together due to their impregnation with
exudate, transudate or blood. Crepitation is heard in croup pneumonia (the walls of the
alveoli are saturated with exudate), in lung infarction (the walls of the alveoli are
saturated with blood), in congestion in the lungs (the alveoli are saturated with
transudate). By ear, the sound of crepitation resembles the crunch of snow or the sound
produced by rubbing a tuft of hair over the ear. It is similar to small bubbly wet wheezes.
However, crepitation is heard only at the height of inspiration and does not change when
coughing.
Pleural friction noise it appears in patients with dry pleurisy. It differs from other side
respiratory noises in that it increases when the phonendoscope is pressed, is heard in
both phases of breathing, and does not change after coughing.
Other reasons the appearance of wheezing includes diseases of the cardiovascular
system systems associated with a violation of the contractility of the myocardium and
leading to stagnation of blood in the vessels of the lungs. This causes an increase in
pressure in the vessels, and the liquid part of the blood (plasma) sweats into the lumen
of the respiratory tract and alveoli. Then crepitation and dry, soon turning into wet
wheezing appear, the severity of which is determined by the degree of heart failure.
68.
Introductory testingGive a detailed answer to the question
1. How does the assessment of the state of the cardiovascular system begin?
2. What are the main complaints of patients with diseases of the cardiovascular system?
3. What are the main indicators of the state of the cardiovascular system?
4. What do tachy-and bradycardia mean?
5. What is blood pressure and its measurement algorithm?
6. What is blood pressure?
7. What is heard during auscultation of the heart?
8. What points of heart auscultation do you know?
9. What do we hear at the heart auscultation points?
10. How do heart tones differ from heart murmurs?
11. What are heart murmurs?
12. How is the state of the gastrointestinal tract assessed?
13. Nursing examination and assessment of the urinary system?
14. How is the endocrine system assessed during a nursing examination?
15. How is the assessment of the nervous system performed by a nurse?
16. Nursing survey and examination to assess the state of the reproductive system.
69.
Assessment of the state of the cardiovascular system70.
Assessment of the state of the cardiovascular systemAssessment of the state of the CVS it begins with an examination of the skin, most
often cyanosis, pallor or hyperemia are determined. Cyanosis of the lips, nose tip, ears,
hands and feet is called acrocyanosis which is often found in heart failure and mitral
defects. Facies mitralis - a sign of mitral stenosis (cyanotic blush of the cheeks and
cyanosis of the lips, nose tip and earlobes). Hyperemia of the face it occurs with arterial
hypertension, pallor of the skin - with aortic malformations and significant age-related
atherosclerosis. Corvisar's face characteristic of chronic heart failure: flabby features,
drowsy, dull expression, yellowish-pale complexion with acrocyanosis, constantly watery
eyes and half-open mouth. Pulsation of the neck vessels evaluate in the vertical and
horizontal position of the patient. Carotid artery pulsation - an important symptom of
aortic insufficiency. Pulsation of the cervical veins - tricuspid valve insufficiency.
When examining the heart area you can detect a local protrusion of the chest – heart
hump which is formed in congenital heart defects (CHD). Pay attention also to the nature
of the apical push, which can significantly bulge during systole due to increased pulsation
(with left ventricular hypertrophy) or retract during systole (negative apical push) in
patients with pericarditis.
71.
Assessment of the state of the cardiovascular systemMain complaints which are presented by patients with diseases of the cardiovascular
system, are: shortness of breath, pain in the heart and, especially, behind the sternum,
palpitations and interruptions in the heart, cough, swelling, headache, dizziness, general
weakness.
For complaints the patient's response to pain in the heart area should clarify its nature,
localization, radiation, and duration. In the case of a long-term or recurrent illness, you
need to find out what medications the patient usually relieves pain. Characteristic
feature cardiovascular pathology – edema. They occur due to the accumulation of fluid
in the tissues and cavities of the body. If, when pressing on the skin and subcutaneous
fat with your finger, where they are closest to the bone (for example, the middle third of
the anterior surface of the lower leg), a long-lasting fossa forms in this place, then there
is edema. Assessment of the state of the patient's cardiovascular and respiratory
systems allows us to judge the degree of satisfaction of the need for oxygen, which
occupies a leading place in the vital activity of the body. Key indicators The conditions
of the cardiovascular system are: heart rate and blood pressure. Determining the state
of your heart rate – pulse) is basic and easily recorded information.
72.
Assessment of the state of the cardiovascular systemPulse rate - these are fluctuations in the arterial wall that occur under the influence of a
blood pressure wave with each heart contraction. Pulse assessment is usually
performed on the radial arteries, but other arteries – temporal, carotid, brachial, femoral,
popliteal, posterior tibial and rear foot arteries-also need to be palpated to detect
weakened pulsation. The rhythmic pulse rate is determined by counting pulse waves for
10, 15 or 20 seconds and multiplying the resulting amount by 6, 4 or 3 (respectively). If
the pulse rate is less than 60 per minute, then it is called rare (bradycardia), and more
than 80 – frequent (tachycardiaNonrhythmic rapid pulse is called tachyarrhythmia,
nonrhythmic rare-bradyarrhythmia. Rapid, rapid and high pulse rate is characteristic of
aortic insufficiency,
and slow, rare and small – for oral stenosis
aortic stenosis. If on palpation
the loss of individual pulse signals is determined
waves, this is typical for extrasystoles.
In case of irregularity, lack of rhythm,
the appearance of pulse waves should be assumed
whether the patient has atrial fibrillation or
atrioventricular block.
73.
Blood pressure measurementBlood pressure (BP) – this is the pressure of blood on the walls of blood vessels, in
other words, the excess of fluid pressure in the circulatory system over atmospheric.
Blood pressure is one of the most important parameters that characterize the
functioning of the circulatory system. Blood pressure is determined by the volume of
blood, the elasticity of the vascular wall, the total size of the vascular lumen and the
resistance of the vascular bed. Upper (systolic) - this is the level of pressure in the
arteries at the time of maximum contraction of the heart muscle-systole. On average,
this parameter is 100-120 mm Hg.. Lower (diastolic) - the level of pressure during the
period of relaxation of the heart-diastole. This indicator reflects the tension of the arterial
wall, in other words, their elasticity. It is 60-80 mm Hg.. Difference between upper and
lower pressure it's called pulse pressure. It shows how much systolic pressure exceeds
diastolic. Normally, the value is 35-40 mm Hg..
The generally accepted norm is considered to be indicators of 120/80, but small
deviations in one direction or another with normal health are quite acceptable.
Persistent increase in blood pressure above 140/90 mm Hg. (arterial hypertension) or
persistent lowering of blood pressure below 90/60 (arterial hypotension) they can be
symptoms of various diseases.
74.
Types of blood pressure monitors for measuring blood pressureMechanical devices. The device consists of a pressure gauge with a digital scale, a
cuff and a bulb for pumping air. The mechanical tonometer itself does not determine the
level of blood pressure, it only shows the level of air pressure in the cuff. Blood pressure
is determined by a person using a stethoscope, which can be built into the cuff.
Electronic devices. Automatic and semi-automatic electronic tonometers determine
blood pressure without human hearing, due to automatic detection of short-term
pressure surges that occur at the time of pulsation of the artery in the cuff.
75.
Algorithm for measuring blood pressure1. Sit or lay the patient down, depending on the patient's condition.
2. Expose the patient's hand, placing it palm up, at the level of the heart.
3. Place a roller or fist under the patient's elbow.
4. Place the tonometer cuff on the patient's shoulder 2-3 cm above the elbow bend (a
finger should pass freely between the cuff and the patient's hand).
5. Find palpation on the brachial artery pulsation, apply a phonendoscope.
6. Connect the cuff to the blood pressure monitor.
7. Gradually pump the air with the cylinder until the pulsation disappears +20-30 mm Hg
in addition.
8. Using the cylinder valve, gradually reduce the movement in the cuff by opening the
valve slightly with the thumb and index finger of the right hand counterclockwise.
9. Remember on the scale on the tonometer the appearance of the first tone - this is
systolic pressure.
10. Mark on the scale on the tonometer the end of the last loud tone, with a gradual
decrease in pressure - this is diastolic pressure.
11. For accurate results, measure the pressure 3 times on different hands.
12. Take the minimum blood pressure value and write the data to the dynamic
observation sheet.
76.
Classification of blood pressure (BP)levelsCategory
Systolic blood
Diastolic blood
pressure
pressure
Optimal
<120
<80
Normal
<130
<85
Increased value
130-139
85-89
Arterial
hypertension
1 degree
2 degrees
3 degrees
140-159
160-179
>180
90-99
100-109
>110
77.
HEART AUSCULTATION ALGORITHMAuscultation tasks include the assessment of normal heart tones, extratones, and noise
detection. To listen to the heart, you must use both tips of the stethophonendoscope: "bell"
(a stethoscope) and a rigid membrane attachment (phonendoscopeHigh-frequency
sounds – heart tones I and II, systolic clicking, regurgitation noise-are best evaluated using
a phonendoscope. To detect sounds that have a low frequency, use a stethoscope ("bell"),
and it should be applied to the chest without pressure.
Standard heart auscultation points:
1st point - the apex of the heart or the area of the apical push (the point of listening to the
mitral valve). 2nd point – the second intercostal space directly at the right edge of the
sternum (aortic valve auscultation point). 3rd point — the second intercostal space directly
at the left edge of the sternum (auscultation point of the pulmonary artery valve). 4th point the lower third of the sternum at the base of the xiphoid process (the tricuspid valve is
listened to).
5th point (or Botkin's point) — at the site of attachment of the fourth rib to the left edge of
the sternum (the point of anatomical projection of the mitral valve).
6th point (or Botkin-Erb point) — in the third intercostal space to the left of the sternum
and corresponds to the anatomical projection of the aortic valve.
78.
Standard heart auscultation points79.
Heart tonesHeart tones – these are sound waves that occur as a result of the work of the heart
muscle and heart valves. Tones are formed due to fluctuations in the structures of the
heart, the initial segments of the aorta and the pulmonary trunk. They can be heard by
applying a phonendoscope or ear to the front chest wall.
There are four different tones:
First tone it appears during contraction of the heart muscle. It is quite low, long,
sonorous and starts after a relatively long pause. According to the acoustic properties of
tones: in a healthy person, the I tone is longer and lower in key than the II tone.
Second tone higher, louder, shorter, and occurs after a short period of silence. The
duration of diastole is approximately twice as long as systole, and therefore it is easy to
distinguish the I tone from the II.
Third and fourth tones they are heard after the second one-in the diastolic phase of
the cardiac cycle. First tone called with a systolic tone, because it is heard at the
beginning of the systole, and second tone — diastolic (heard at the beginning of
diastole). Third and fourth — diastolic.
The first and second tones are always there. Third it can be heard in healthy people
and in various pathological conditions.
Audible fourth tone always pathological.
80.
Heart tonesThere are two main groups of reasons why heart tones sound different from normal::
Physiological factors – they are related to the characteristics of the person under
study and their functional state. For example, on the front wall of the chest in obese
people, sound conduction worsens, so heart tones become muffled. Pathological
conditions - they occur when the structures of the heart and the vessels extending from
it are damaged. So, narrowing of the atrioventricular opening and compaction of its
valves leads to the appearance of a clicking first tone. Muted heart tones they are
called when they lose their clarity and become poorly distinguishable in: diffuse
myocardial damage with a decrease in its ability to contract-extensive myocardial
infarction, myocarditis, atherosclerotic cardiosclerosis; effusion pericarditis;
emphysema of the lungs, pneumothorax.
Muting the first tone at the top of the heart indicates myocarditis, sclerosis of the
heart muscle, partial destruction or insufficiency of atrioventricular valves.
Muting the second tone in 2nd intercostal space on the right it occurs when the
aortic valve is insufficient or its mouth is narrowed (stenosis).
Muting of the second tone in the 2nd intercostal space on the left indicates
insufficiency of the pulmonary trunk valve or stenosis of its mouth.
81.
Heart murmursHeart murmurs – this is an acoustic phenomenon that reflects, first of all, the operation
of valves, as well as hemodynamic disorders (blood movement) of various etiologies.
Heart murmurs during auscultation are divided into organic and functional.
Organic noises they occur with various structural changes of the heart, for example,
with malformations (congenital or acquired). They may indicate a lesion of the heart
valves (stenosis, valvular insufficiency, or their simultaneous combination). Also, organic
noise appears in cardiomyopathy (expansion of the heart chamber cavity or hypertrophy
(thickening) of the myocardium), endocarditis (inflammation of the inner lining of the
heart) and acute pericarditis (inflammation of the pericardial sheets lining the heart from
the outside). Functional noises they are not related to the heart or are based on
abnormalities that do not affect its work. They can occur due to vegetative-vascular
dystonia, as well as during the period of rapid growth in children and adolescents. Also,
sometimes they indicate some features of the structure of the human heart that have
arisen during intrauterine development. For physiological causes of noise it will have
a soft, not very sonorous character, and with organic damage to the valves, a rough or
blowing systolic or diastolic noise is heard.
82.
Heart murmursCongenital causes of heart murmurs include holes in the heart. A hole can form
before birth in the wall between the upper or lower chambers of the heart. For example,
an atrial septal defect and an interventricular septal defect. Ventricular septal defect
(IVD) – one of the most common congenital heart defects. With it, in the intrauterine
period, the formation of the septum between the right and left ventricles is disrupted,
which leads to their communication. In the future, this can cause the development of
heart failure. Atrial Septal Defect (ATRI) – this is a congenital heart defect, in which a
hole is formed in the septum. Through it, blood flows from the left atrium to the right, as a
result of which the pulmonary vessels receive an excess volume of blood, which
increases the pressure in the pulmonary artery and is manifested by cyanosis of the skin.
Over time, defects can lead to the formation of a heart shunt.
Adults usually have heart murmurs related to heart valve problems. These include:
Calcium deposits – can cause the heart valve, mitral or aortic, to become rigid and
narrow. Endocarditis - bacteria enter the heart through the blood, and if the infection is
not treated, it affects the heart valves and makes noise. Rheumocarditis – this serious
complication of pharyngitis can occur in those who do not receive or complete treatment.
83.
84.
Assessment of the state of the gastrointestinal tract (GIT)Patients with diseases of the digestive system make complaints, which are conditionally
divided into non-specific and specific. Non-specific ones: weakness, malaise, weakness,
poor sleep, irritability, decreased performance, etc. Specific features: abdominal pain, loss
of appetite; belching, heartburn, nausea, vomiting (gastric dyspepsia syndrome); bloating –
flatulence, diarrhea, constipation, rumbling (intestinal dyspepsia syndrome) and
manifestations of gastrointestinal bleeding. Inspection it is advisable to start with the
tongue-the mirror of the stomach. You should pay attention to plaque and bad breath,
assess the patient's appetite, find out his food preferences, and nutrition model. It is
necessary to note the shape and size of the abdomen, its symmetry. Abdominal
examination allows you to identify a network of anastomoses on the anterior abdominal
wall between the portal and vena cava systems. Dilated, swollen and convoluted veins,
which are located around the navel, radiating from it, and form the so-called “medusa's
head”, are characteristic of portal hypertension syndrome, which is observed in cirrhosis of
the liver. An increase in the abdomen can be observed with obesity, the accumulation of a
large amount of gases in the intestines, the presence of fluid in the abdominal cavity
(ascites). Bulging of some part of the abdomen occurs with an increase in the liver (mainly
in the right hypochondrium), spleen (in the left hypochondrium), the presence of a tumor,
hernial protrusions.
85.
Assessment of the state of the gastrointestinal tract (GIT)If necessary, the nursing staff performs a palpation of the abdomen. Palpation of the
abdomen allows you to get information about the location of abdominal organs, their
shape, size, consistency, and soreness. In case of acute pain of unclear origin, it is
necessary to urgently invite a doctor.
86.
Assessment of the state of the gastrointestinal tract (GIT)With abdominal auscultation in a healthy person, periodic intestinal motility is heard,
which can increase after eating food rich in plant fiber, with inflammation of the small
intestine (enteritis). Aboutweakening of intestinal motility is heard in patients with
intestinal atony (for example, in the elderly with atonic constipation), and a sharp
weakening or even absence of intestinal motility (“grave silence”) – in patients with
peritonitis. Significant indicators that characterize the state of the gastrointestinal tract
are the frequency of stool, its color, and the amount of feces. Normally, a person's stool
is released daily at the same time. You can talk about its delay if it is absent for 48
hours. Fecal incontinence is often associated with diseases of the central nervous
system. Defecation disorders can be caused not only by organic pathology, but also by
the psychological state of the patient.
After a nursing survey and examination the nurse records it in the nurse's medical
history or observation sheet. Received information about rectal bleeding or tarry stools,
hemorrhoids, constipation, diarrhea, abdominal pain, intolerance to certain foods,
flatulence, jaundice associated with liver and gallbladder pathology, etc. Information
about a colostomy or ileostomy will help you create an individual plan for nursing care,
training relatives in proper patient care.
87.
Assessment of the state of the urinary systemDuring a nursing survey and examination it is necessary to assess the nature and
frequency of urination in the patient, the color of urine, its transparency, and identify
disorders of the urinary system (qualitative and quantitative). Puffiness of the eyelids
and hands, if it is combined with swelling of other parts of the body, is observed in
kidney diseases. Urinary incontinence is not only a risk factor for developing bedsores in
a patient, but also a major psychological and social problem. If the patient is wearing a
permanent catheter or has had a cystostomy, the nursing staff should plan measures to
adapt the patient to the environment, as well as to prevent infection of the urinary
system.
Determining the water balance it consists in calculating the ratio between the amount
of fluid entering the body and the amount of fluid removed from it over a certain period.
Calculation formula: the amount of urine released is divided by the amount of liquid
consumed/administered and multiplied by 100. If the amount of urine released is more
than 80%, the water balance is considered positive, if less than 80% - negative.
Daily diuresis rate in an adult, it is approximately 1-2 liters. However, this indicator may
vary depending on age, gender, physical activity, and fluid intake.
88.
Endocrine system assessmentEndocrine system it regulates the activity of internal organs, as well as coordinates the
normal growth and development of the body through hormones. Endocrine gland
dysfunction is the cause of common diseases – obesity, diabetes mellitus, osteoporosis,
etc. The dominant value in the pathology of the endocrine glands is the data of
anamnesis and examination. It is necessary to clarify the patient's hereditary
predisposition to diseases of the endocrine system (diabetes mellitus and diabetes
insipidus, thyroid diseases, obesity, adrenal gland pathology). When evaluating the
endocrine system the nurse should pay attention to the nature of the patient's hair, the
distribution of subcutaneous fat, and the visible enlargement of the thyroid gland. Many
autoimmune diseases (rheumatoid arthritis, vitiligo, etc.) are accompanied by the
appearance of pathology of the internal secretion organs with the development of
diabetes mellitus, adrenal insufficiency, hypothyroidism, thyrotoxicosis. Previous
infections: sore throat, pneumonia, ARVI can lead to the development of inflammation of
the thyroid gland (thyroiditis). Excessive body and limb hairiness (hypertrichosis) in
women, especially in combination with the growth of a mustache and beard (hirsutism),
it is observed in Itsenko-Cushing's disease and syndrome, acromegaly, ovarian tumors.
89.
Endocrine system assessmentIncreased thirst occurs in diabetes insipidus and diabetes mellitus. Headaches occur
due to increased blood pressure or when the pituitary gland and dura mater are
compressed by a growing tumor. In patients with thyrotoxicosis, the skin is constantly
moist, warm, thin, velvety to the touch, and in hypothyroidism, on the contrary, it is dry,
cold, rough, thick, dense and rough. Small-scale flaking of the skin is characteristic of
hypothyroidism. Multiple combs may indicate persistent itching of the skin in diabetes
mellitus. A sign of thyrotoxicosis is popeye (exophthalmus). Difficulty swallowing and
breathing is characteristic of diffuse goiter.
From the endocrine glands, palpation is available only to the thyroid gland, which gives
an idea of its size, the nature of the surface, density, the presence of nodes, soreness.
Reproductive disorders in endocrine pathology are manifested by decreased libido
(sexual desire), erectile dysfunction (impotence), amenorrhea (lack of menstruation),
metrorrhagia (uterine bleeding), gynecomastia (breast enlargement in men),
gigantomastia (large breast size in women), lactorrhea (milk release from the mammary
glands outside of lactation).
Often, disorders of the endocrine system associated with changes in appearance cause
psychological discomfort of the patient.
90.
Assessment of the state of the nervous systemWe start by collecting an anamnesis. We find out if the patient has had episodes of loss
of consciousness, convulsions, and whether he sleeps well. It is necessary to ask the
patient about his dreams, the duration and nature of sleep (deep, calm or shallow,
restless). It is important to find out if the patient uses sleeping pills, if so, which ones,
and how long ago they started using them. The beginning of the first symptoms – when
the complaints first appeared (age or year of onset of
headache/pain/weakness/numbness, etc.). If the patient has tremor of the limbs, gait
disorders, you should find out if he has had any head or spine injuries in the past.
Symptoms of neurological disorders in the patient may include headache, loss and
changes in sensitivity. Sensation of numbness: in the case of hemihypesthesia - in the
arm and leg on one side; in the case of spinal damage-below the level of the lesion (on
the abdomen and leg/legs, on the chest, abdomen and leg/legs, etc.; in the case of
polyneuritic syndrome-complaints of impaired sensitivity in the hands and/or feet). Does
not feel when he touches objects, does not feel the floor, "walks like cotton wool". Does
not distinguish between cold and hot touch(burns with hot water). Feeling of stiffness in
the limbs, stiffness, difficulty bending or unbending the arm / leg (with increased tone).
The limb has lost weight (in the presence of hypotrophy/atrophy). We evaluate tendon
reflexes (normally they should be called symmetrically from 2 sides).
91.
Assessment of the state of the nervous systemNeurological examination – this is a primary step in the diagnosis of many
neurological diseases. Neurological examination can reveal signs of pathologies such
as migraines, Parkinson's disease, epilepsy and other diseases of the nervous system.
We ask the patient to walk with his eyes open and observe his gait for
unsteadiness/ataxia when walking. We ask you to walk with your eyes closed (insuring
the patient from falling, we walk side by side) and observe how the degree of ataxia of
walking changes outside of visual control. We ask the patient to walk along one
imaginary line, placing their feet "heel of one foot to the toe of the other" with their eyes
open, controlling walking with their eyes and evaluating the stagger when walking, the
ability to walk along one line, and falling.
Finger-nose test: we ask the patient to spread his hands apart, close his eyes and touch
the tip of his own nose with the tip of his index finger, and assess the presence of tremor
(increased tremor when approaching the tip of the nose).
Actions of nursing staff They should be aimed at ensuring the safety of such a patient
during his stay in the hospital.
If the patient's physical activity is restricted due to weakness, paresis or paralysis,
special measures for the prevention of pressure sores should be included in the nursing
plan.
92.
Assessment of the state of the reproductive systemWhen talking to patients about this topic nursing staff should use therapeutic
communication techniques and the greatest sense of tact. In women, they find out the
time of onset of the first menstruation; regularity, frequency, duration, number of
secretions; date of the last menstruation. It is necessary to find out if the patient has
bleeding in the intermenstrual period. Many girls are concerned about the irregularity or
delay of menstruation. By asking questions, the nurse can understand the patient's
awareness of the female sexual sphere.
In a middle-aged woman, you should find out if she stopped menstruating and when,
and whether her cessation was accompanied by any symptoms. You can also ask how
she felt about this event, whether menopause affected her life in any way. In the nursing
history of the disease, past venereal diseases are noted, methods of their treatment; the
number of pregnancies, childbirth, abortions; ways to prevent pregnancy; sexual
preferences of the patient. During a nursing survey and examination, discharge, itching,
ulceration, and swelling of the genitals are detected. In men, the state of the
reproductive system is determined after checking the state of the urinary tract. The
questions asked are aimed at identifying local symptoms that indicate violations of
sexual function.
93.
End of the surveyAt the end of the survey nursing staff draws conclusions about the violation of the patient's needs,
records them in the nursing medical history.
After completing the survey and examination, you should transfer the initiative to the patient by asking him
a leading question: "What have we not talked about yet?" or by asking: "Do you have any questions for
me?". It is necessary to explain to the patient what awaits him next, introduce him to the daily routine,
employees, premises, neighbors in the ward, and hand over a memo about his rights and obligations. In
the future, the dynamics of the patient's condition should be displayed daily in the observation diary (SIB)
throughout the entire hospital stay. The first steps at the beginning of practical work of nursing staff can be
cautious and uncertain. When examining patients, students sometimes worry more than the patient
himself. Often there is a feeling of awkwardness and uncertainty. The interview turns into an interrogation,
and the examination is delayed. Touching the intimate parts of the patient's body causes a sense of
shame. In these cases, you should try to master yourself, keep calm, collected, and as confident as
possible. The skills of maintaining an educational medical history help to conduct a nursing survey
competently and fully in the future. If the conversation with the patient is already over, and you realize that
you missed something important, you can go back and politely say that you need to clarify something.
You can not betray your irritation, anxiety, disgust. A medical worker has no right to negative emotions at
the patient's bedside.
Self-confidence comes with time. With the acquisition of practical skills, the process of nursing
examination becomes a familiar procedure, carried out without causing any particular inconvenience to
the patient. Experienced nursing staff pay attention to the patient's reactions, not to their own
experiences. Improving professionalism for a true doctor becomes the work of his whole life.
94.
conclusions95.
conclusions1. Collecting patient information at the first stage of the nursing process has a huge
impact on the quality of subsequent nursing care. The main sources of information about
the patient are themselves, their relatives and acquaintances, medical personnel,
medical documentation, and specialized medical literature.
2. There are two types of patient information: subjective and objective. Subjective
information is collected through a survey. First, personal data is recorded indicating the
source of information received.
3. Subjective examination includes the collection of basic complaints, medical history, life
history, self-assessment of the patient's condition at the time of examination, family and
psychological history.
4. During an objective examination, the nursing staff determines the general condition of
the patient, measures his height, body weight, temperature; assesses the state of vision,
hearing, skin and visible mucous membranes, musculoskeletal, respiratory,
cardiovascular systems, gastrointestinal tract, urinary, endocrine, nervous and
reproductive systems.
5. Distinguish between clear and confused (inhibited, deafened, sopor) states of
consciousness.
6. Objective examination reveals the patient's position: active, passive and forced.
96.
conclusions. To assess whether a patient's body weight of a certain height and age corresponds to
the ideal body weight, special tables should be used.
8. When examining the skin and visible mucous membranes, its color, moisture and fat
content, temperature, elasticity and turgor are evaluated, and pathological elements on
the skin are identified.
9. When examining the musculoskeletal system, first of all, they find out whether the
patient has pain in the joints and muscles, if so, their nature, bone deformities, limited
mobility.
10. When examining the respiratory system, find out the characteristics of breathing; 11.
When examining the cardiovascular system, pulse, blood pressure, pain in the heart,
edema are recorded.
12.During the examination of the gastrointestinal tract, there are violations of appetite,
heartburn, nausea, vomiting, belching, flatulence, constipation or diarrhea.
13. When examining the urinary system, the nature and frequency of urination, the color
of urine, its transparency are determined, and the fact of urinary incontinence is
recorded.
14. When examining the endocrine system, they find out the nature of hair growth, the
distribution of body fat, and an increase in the thyroid gland.
97.
conclusions15. During the examination of the nervous system, attention is paid to the nature of
sleep, tremors, gait disorders, episodes of loss of consciousness, convulsions, and
sensitivity disorders.
16. When examining the reproductive system, a gynecological history is collected in
women; in men, after clarifying the state of the urinary tract, pathologies of the
reproductive system are detected.
And, of course, do not forget about the documentation. The nurse records all her actions
and results. After all, it is important to have good records so that you always know what
has been done and what still needs to be done.
So, the nursing process is such a smart system that helps nurses do their job
even better. They research, think, plan, and care for patients. They are real heroes
in white coats!
98.
Final testing Theoretical part1. Subjective method of nursing examination:
a) examination of the patient;
b) definition of edema;
c) questioning the patient;
d) blood pressure measurement.
2. The second stage of the nursing process includes:
a) planning the scope of nursing interventions;
b) identifying the patient's problems;
c) collecting patient information;
d) defining the goals of nursing care.
3. The main sign of the first period of fever:
a) chills;
b) thirst;
c) feeling hot;
d) vomiting.
4. Hyperpyretic fever is the body temperature (in ° C):
a) 37-38;
b) 39-41;
c) 38-39;
d) above 41.
99.
Final testing Theoretical part5. Increasing blood pressure is:
a) hypotension;
b) tachycardia;
c) hypertension;
d) bradycardia.
6. The number of breaths per minute in an adult is normal:
a) 30-36;
b) 16-20;
c) 22-28;
d) 10-12.
7. The most interrelated properties of the pulse:
a) tension and filling;
b) tension and rhythm;
c) frequency and rhythm;
d) speed and frequency.
8. What are the names of biologically active substances secreted by the endocrine glands?: a)
enzymes;
b) hormones;
c) vitamins;
d) cytokines.
100.
Final testing Theoretical part9. Pulse deficit occurs when:
a) tachycardia;
b) lowering blood pressure;
c) atrial fibrillation;
d) bradycardia.
10. Diffuse thyroid enlargement syndrome is characterized by the following::
a) occurs when there is an excess of iodine in water and food;
b) always accompanied by thyrotoxicosis;
c) complaints of the patient about pressure in the neck area in the side position;
d) difficulty swallowing, difficulty breathing.
11. What is the name of a complete loss of any kind of sensitivity:
a) hypesthesia;
b) anesthesia;
c) hyperesthesia;
d) polyesthesia.
12. Tachypnea is:
a) heart rate reduction;
b) decreased breathing;
c) increased heart rate;
d) increased breathing.
13. What is the name of an isolated violation of some types of sensitivity while maintaining others:
a) polyesthesia;
b) hypesthesia;
c) dissociation;
d) dysesthesia.
101.
Final testing Theoretical part14. The most interrelated properties of the pulse:
a) tension and filling;
b) tension and rhythm;
c) frequency and rhythm; d) speed and frequency.
15. The ratio of the amount of liquid consumed and excreted is called:
a) daily diuresis;
b) water balance;
c) anurez;
d) daily diuresis.
16. Fowler's position:
a) on the back;
b) on the side;
c) on the stomach;
d) half-lying, half-sitting.
17. Priority physiological problem of the patient:
a) weakness;
b) worry;
c) pain;
d) lack of appetite.
18. Documentation of the stages of the nursing process is carried out by::
a) in the patient's medical record of observation;
b) in the outpatient card;
c) in the appointment list;
d) in the nurse's medical history.
102.
Final testing Theoretical part19. In the first period of fever, it is possible to use:
a) wet wrap;
b) hot water bottles;
c) cold compress;
d) an ice bubble.
20. Measurement of height and body weight-a survey method:
a) subjective;
b) additional;
c) objective;
d) clinical.
21. Subfebrile body temperature is:
a) 39-39. 5°C;
b) 38-38. 5°C;
c) 38.1-38.2°C;
d) 37.1-38°C.
22. Pulse rate in an adult is normal (beats per minute):
a) 100-120;
b) 90-100;
c) 60-80;
d) 40-60.
23. Which of the symptoms is manifested in fever of the second period:
a) weakness;
b) feeling hot;
c) profuse sweating;
d) drowsiness.
103.
Final testing Theoretical part24. What indicator of blood pressure can we judge when the disappearance of Korotkov tones
over the brachial artery
a) pulse pressure;
b) diastolic pressure;
c) systolic pressure;
d) blood pressure.
25. Choose which of the listed treatments you can use during the second period of fever
a) hot compress;
b) warming compress;
c) hot water bottle;
d) an ice bubble.
26. Where is an adult thermometer most often placed?:
a) into the rectum;
b) in the groin area;
c) in the armpit;
d) into the oral cavity.
27. When measuring blood pressure, the nurse heard the appearance of Korotkov tones (systolic
pressure), but could not determine the diastolic. What is the reason?
a) too little air in the cuff;
b) the phonendoscope head is too tightly pressed against the brachial artery;
c) too much air in the cuff;
d) air is released from the cuff too quickly.
104.
Final testing Theoretical part28. Pathological breathing loss is:
a) bradypnea;
b) apnea;
c) tachypnea;
d) dyspnoea.
29. Normal diastolic blood pressure values (mmHg):
a) 120-130;
b) 80-84;
c) 100-110;
d) 110-120.
30. Shortness of breath when breathing is difficult is called shortness of breath.:
a) expiratory;
b) pathological;
c) mixed;
d) inspiratory.
31. The body mass index is calculated by the formula:
a) body weight in kg divided by height in cm;
b) height in cm minus 100;
c) body weight in kg divided by height, expressed in meters, squared;
d) height in m minus 100.
32. The most important task of the nursing process:
a) establish a diagnosis of the disease;
b) determine the forecast;
c) specify the causes of the disease;
d) professional care.
105.
Final testing Theoretical part1. What is a subjective nursing examination?
2. How is the human body mass index calculated?
3. How does wheezing differ from other side respiratory noises?
4. How is the patient's general condition assessed?
5. Fever periods and nursing interventions, depending on the period?
6. What is heard during auscultation of the heart?
7. What types of functional positions do you know about the patient in bed?
8. How do heart tones differ from heart murmurs?
9. What does life history and medical history mean?
10. What is characteristic of the third stage of fever?
11. What is normal breathing during auscultation?
12. What are the stages of the nursing process?
13. What is the Glasgow Coma Scale used for?
14. What is the heart rate indicator?
15. What are the variants of abnormal breathing?
16. What do we hear when performing auscultation for pneumothorax?
17. What are the types of consciousness?
18. Heart auscultation points and their localization?
106.
Final testing Practical partThe student must be able to:
* conduct patient interviews, identify complaints;
* collect life and medical history;
* conduct a general examination of the patient;
* assess the patient's general condition and consciousness;
* assess the patient's position;
* perform anthropometry and weighing of the patient;
* assess the condition of the skin and mucous membranes;
* detect hidden and obvious edema;
* measure body temperature;
* determine the frequency, depth, and rhythm of breathing;
* detect the presence and type of shortness of breath;
* perform palpation, percussion and auscultation of the lungs;
• take your pulse and evaluate it;
* measure blood pressure and evaluate it;
* perform auscultation of the heart;
* determine the water balance.
107.
Methods of nursing examination and basicmanipulation technologies

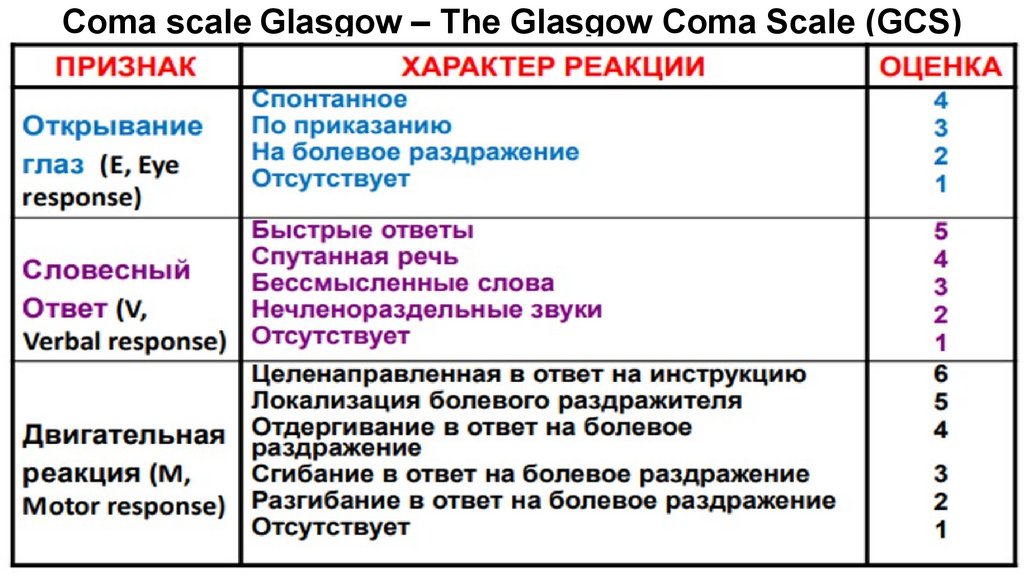
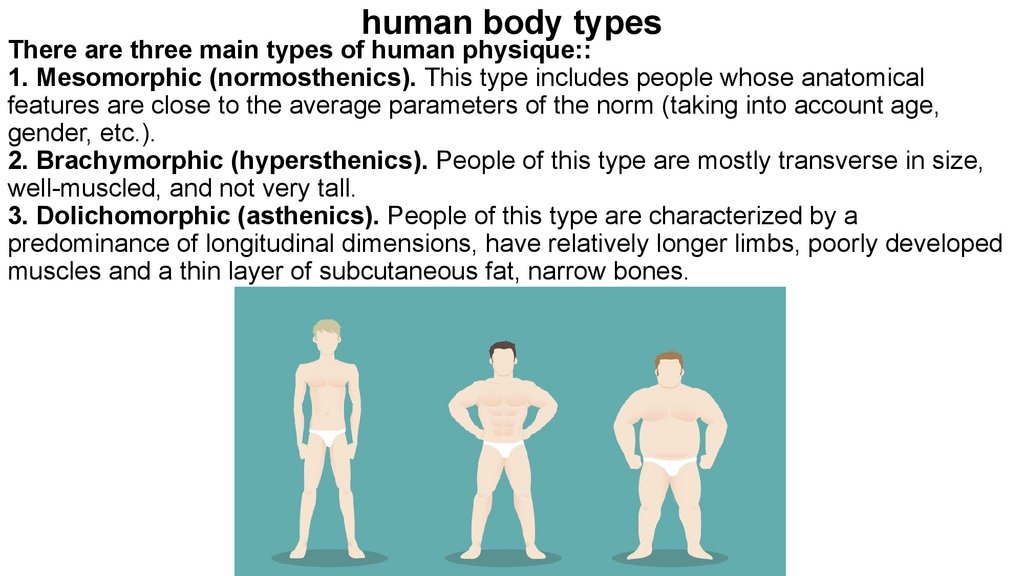
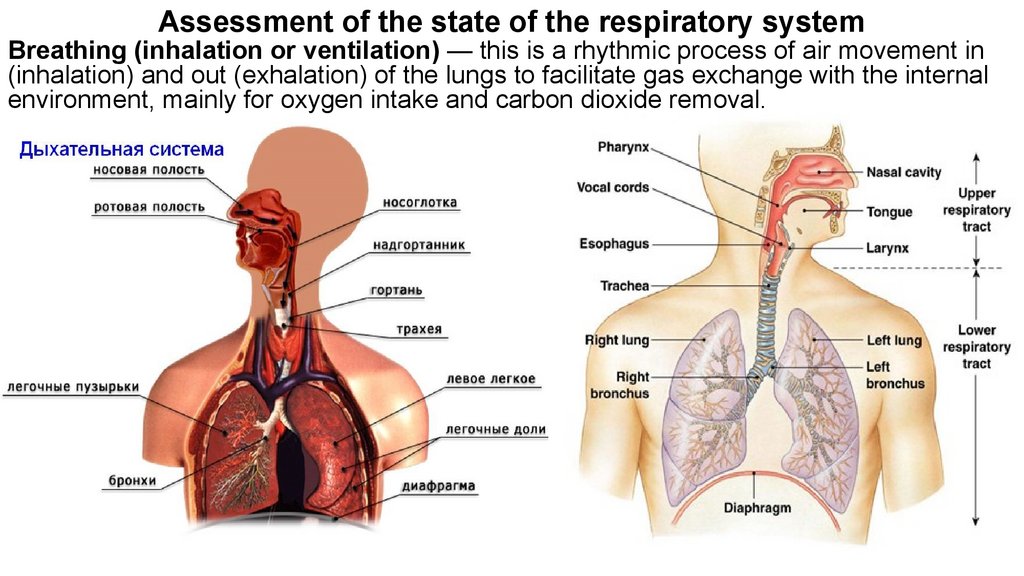
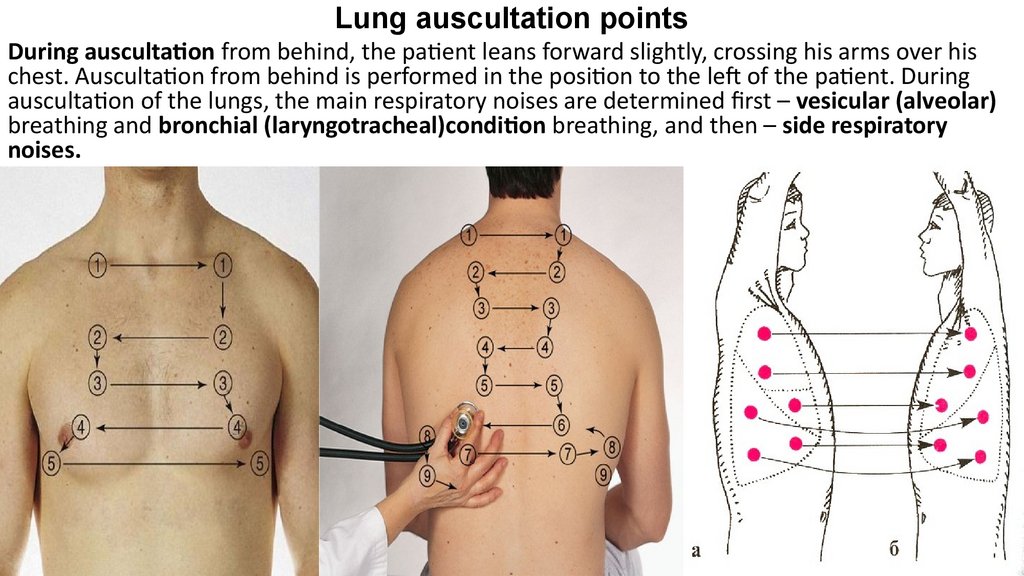
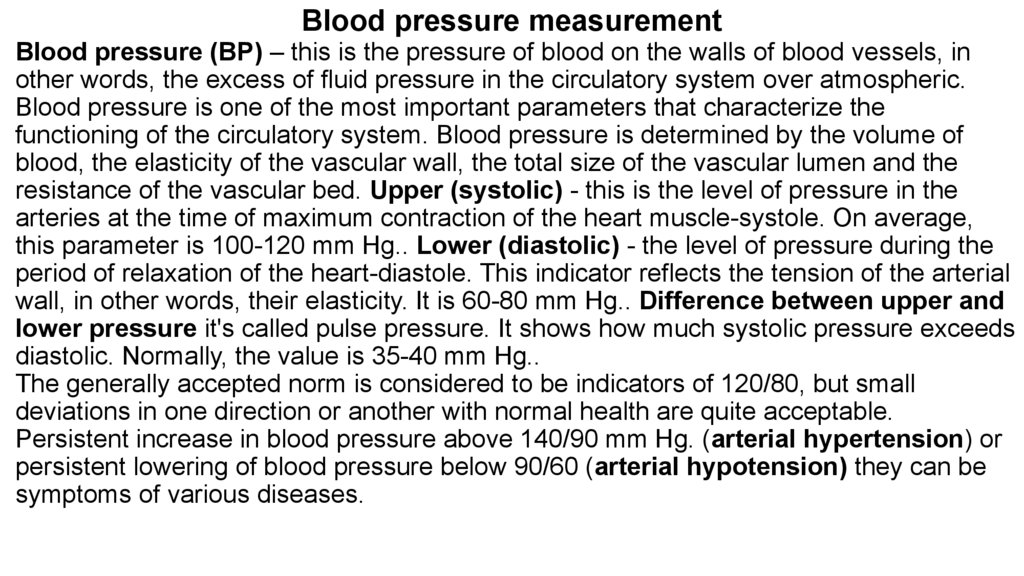
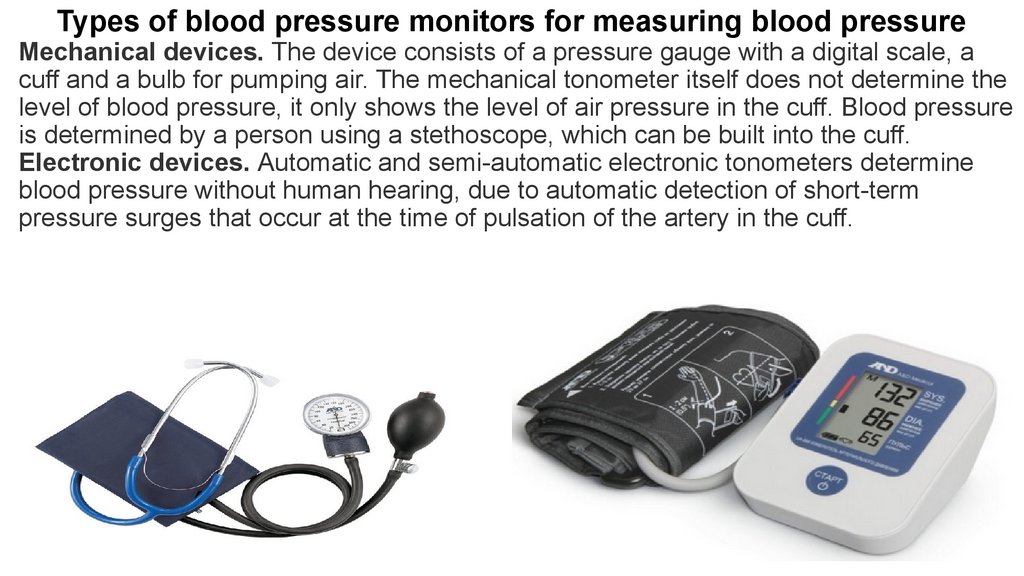
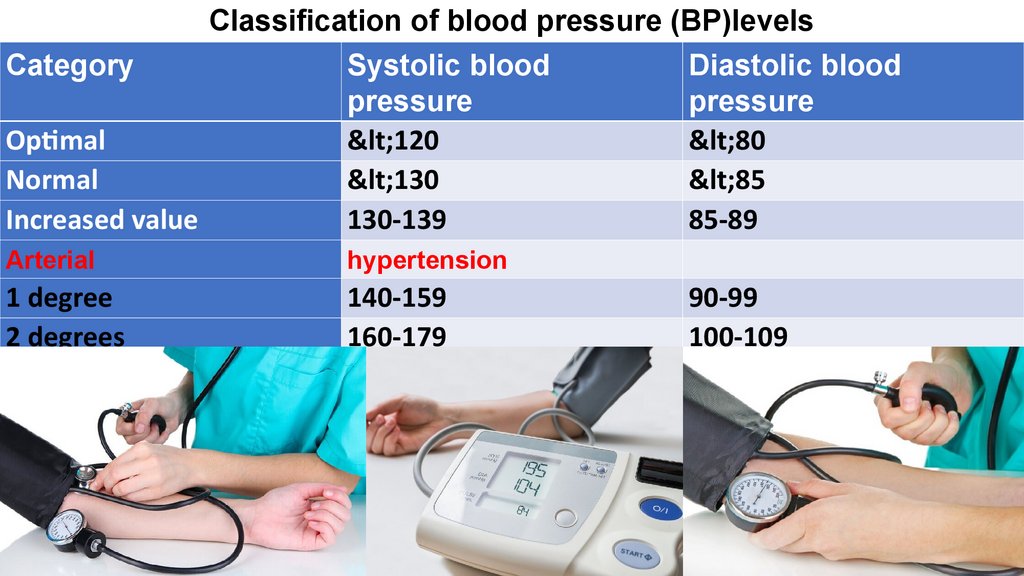
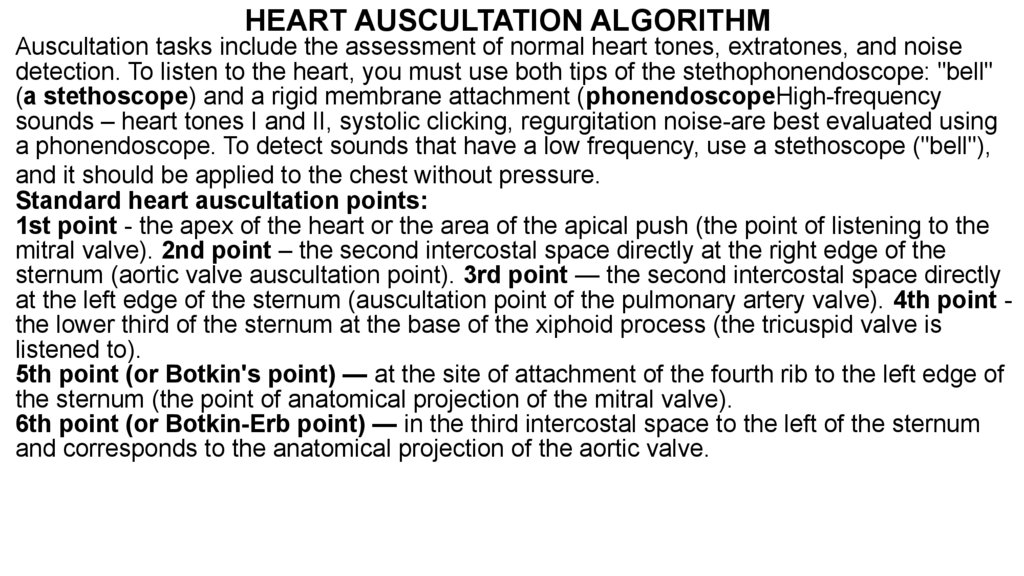
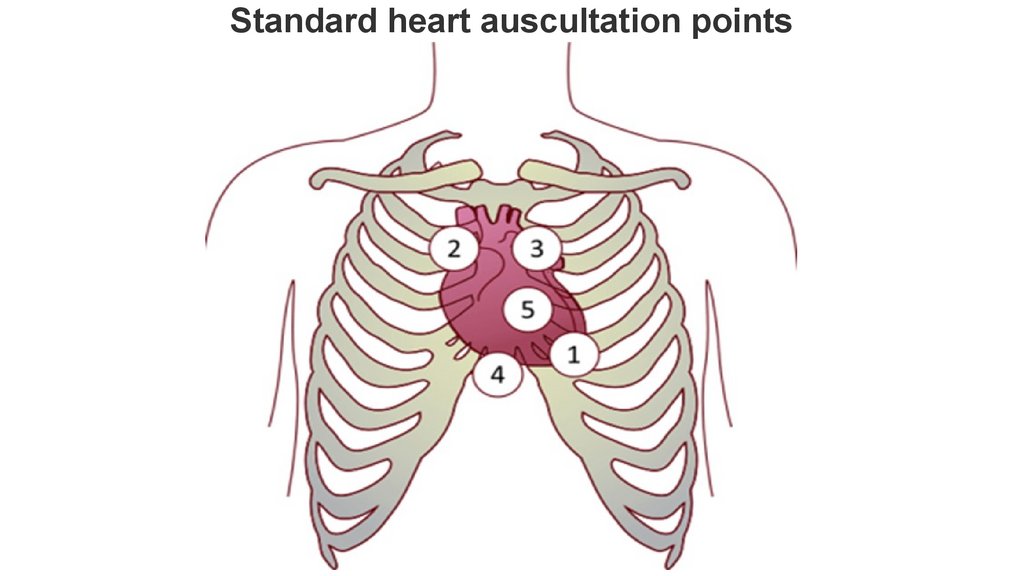
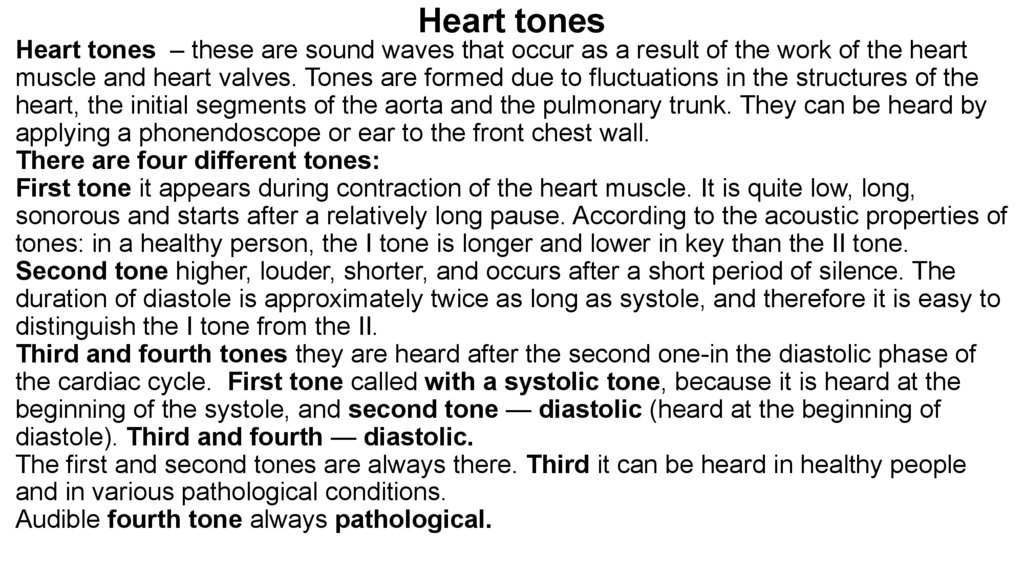
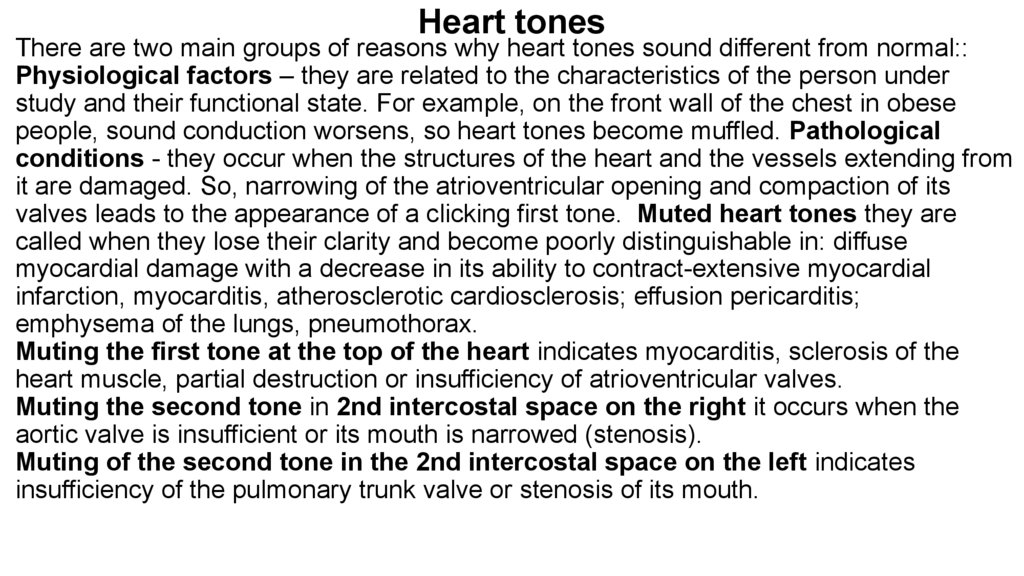


 medicine
medicine