Similar presentations:
Respiratory diseases with bronchial obstruction
1. Respiratory diseases with bronchial obstruction
2. Definition of BO
BO - condition develops due to the presence ofobstacles to the outgoing air flow in the
respiratory tract.
BO syndrome is a complex of symptoms of
obstructive respiratory failure.
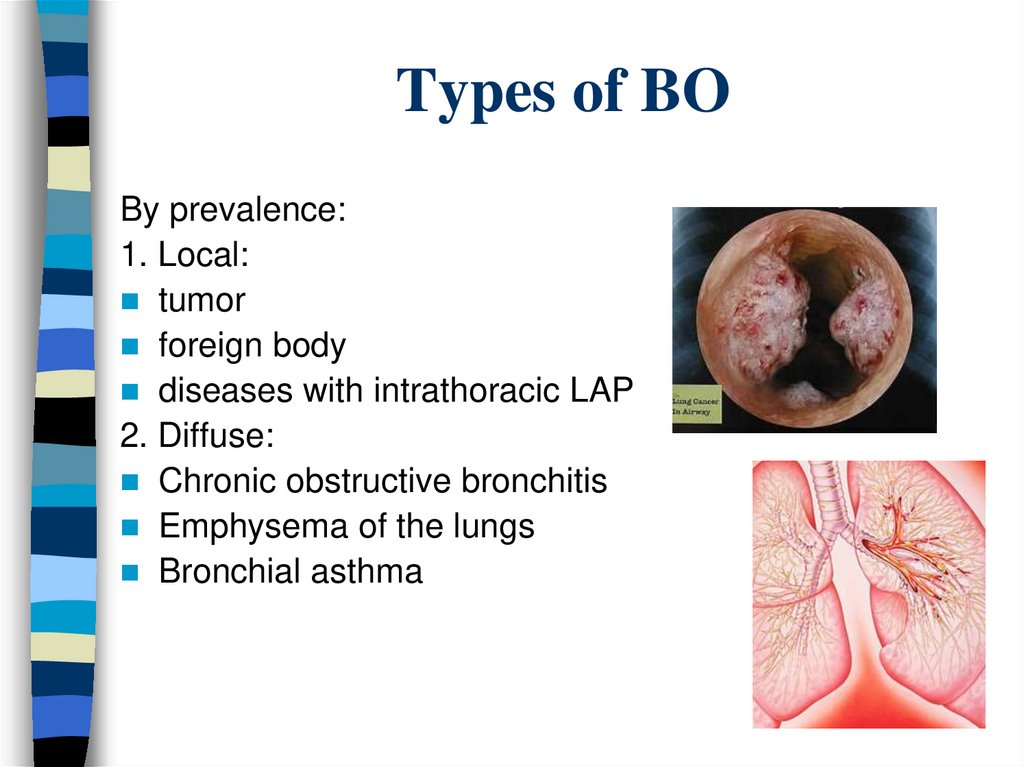
3. Types of BO
By prevalence:1. Local:
tumor
foreign body
diseases with intrathoracic LAP
2. Diffuse:
Chronic obstructive bronchitis
Emphysema of the lungs
Bronchial asthma
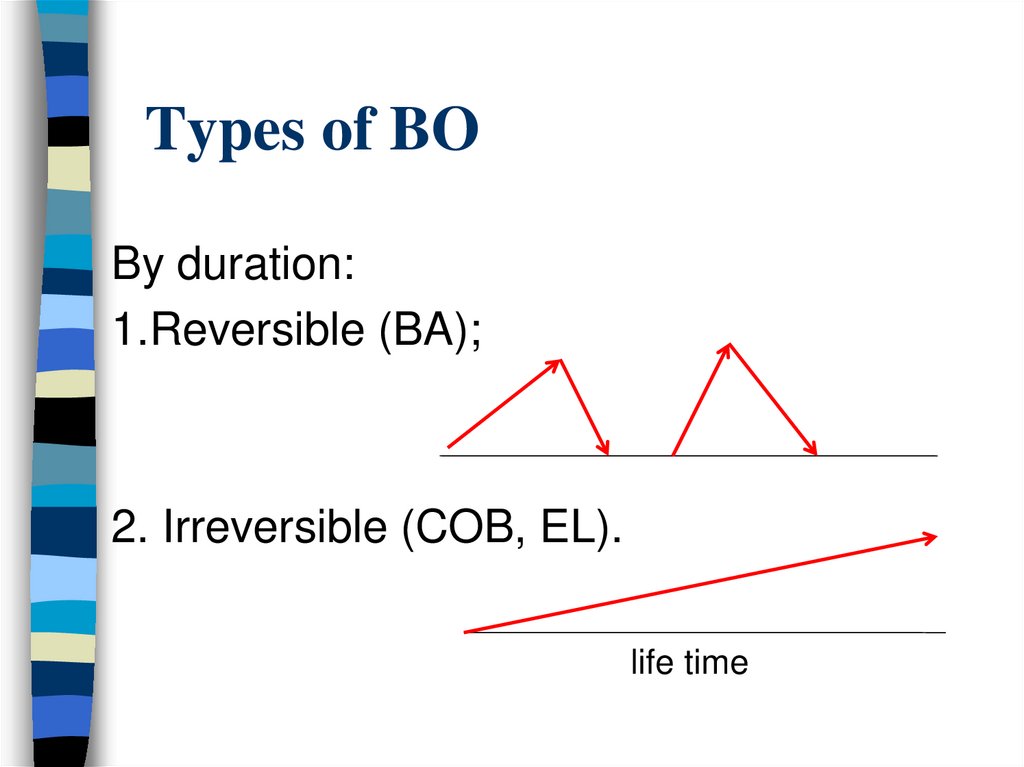
4. Types of BO
By duration:1.Reversible (BA);
2. Irreversible (COB, EL).
life time
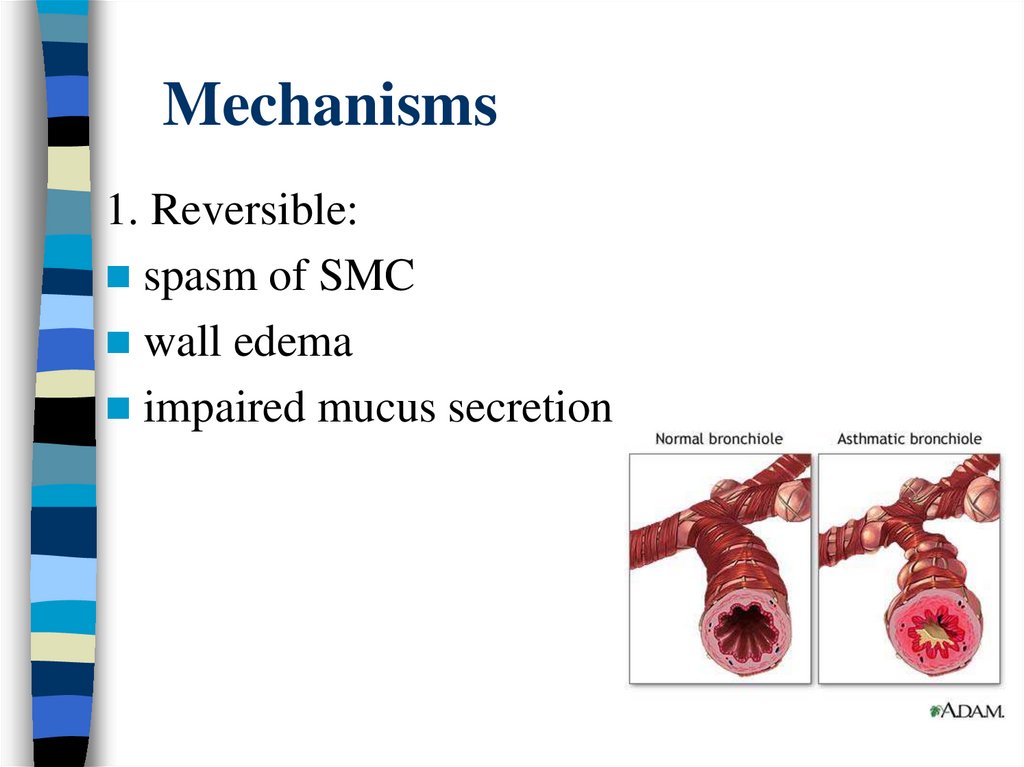
5. Mechanisms
1. Reversible:spasm of SMC
wall edema
impaired mucus secretion
6.
2. Irreversible:fibrosis of the wall
pathological expiratory collapse of bronchioles
(due to the lost of alveolar support and
destruction)
hyperplasia of the epithelium of the bronchial
mucosa
hypertrophy of bronchial submucosal glands
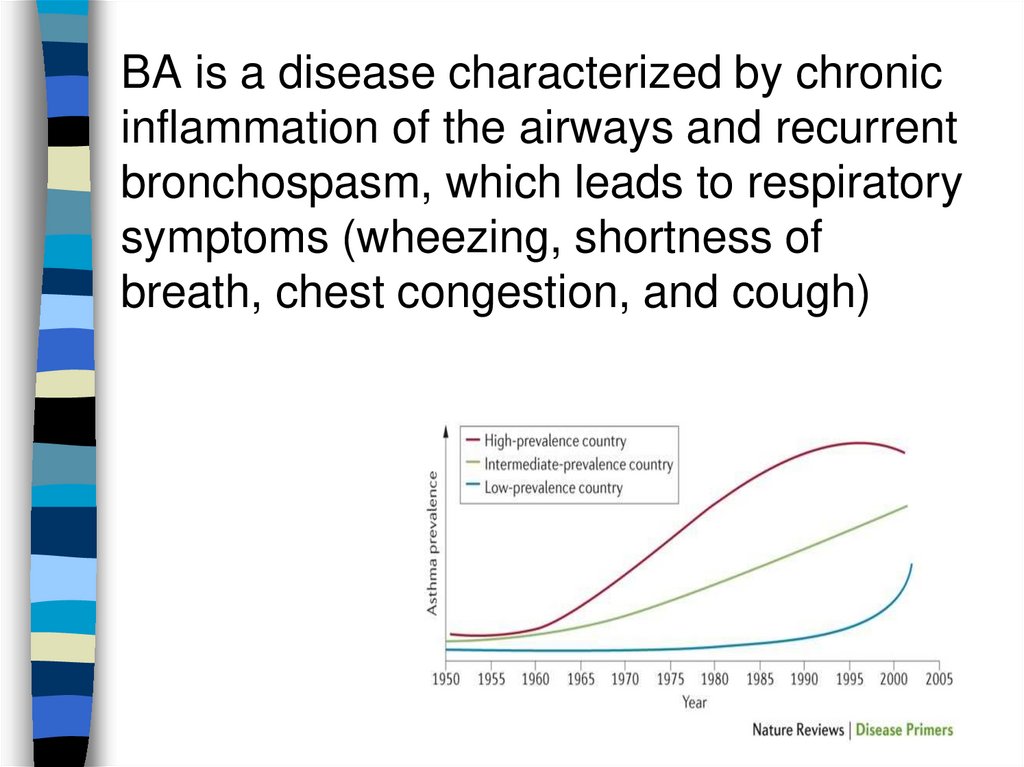
7.
BA is a disease characterized by chronicinflammation of the airways and recurrent
bronchospasm, which leads to respiratory
symptoms (wheezing, shortness of
breath, chest congestion, and cough)
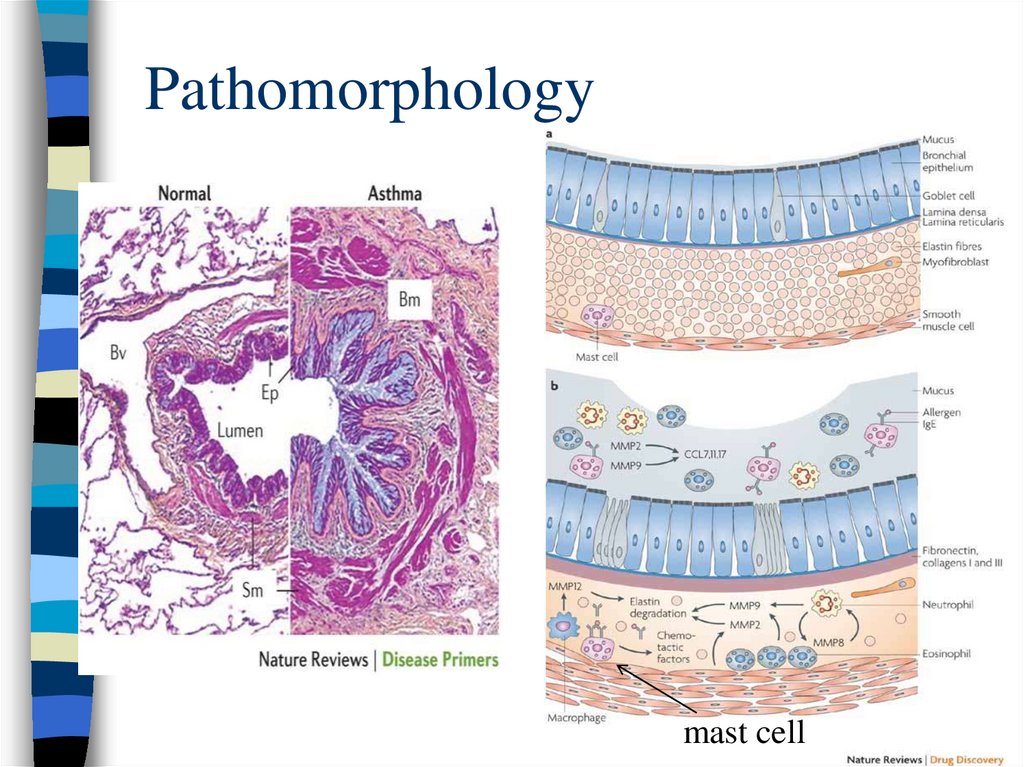
8. Pathomorphology
mast cell9. Inflammation in BA (AD)
The development of AD is based onchronic inflammation in the airways.
Mast cells
Eosinophils
T-lymphocytes
Neutrophils
Macrophages
10. Bronchial hyperreactivity
BHR - the possibility ofdeveloping bronchospasm under
the action of a stimulus that does
not cause bronchospasm in a
healthy person
Inflammation in the airways in
AD leads to BHR
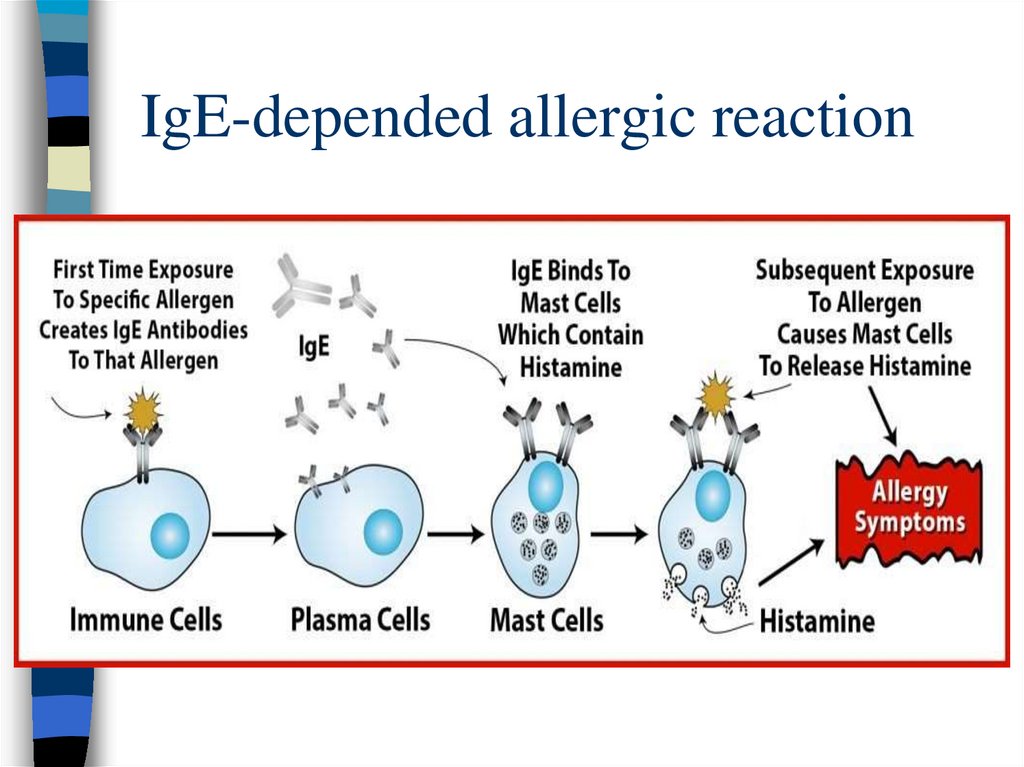
11. Provoking factors of the bronchospasm
Allergen triggers (have a proteinstructure) - cause sensitization
(the appearance of specific IgE)
and provoke bronchospasm
through an IgE-dependent allergic
reaction
Aeroallergens:
household (house dust mite,
cockroaches)
pollen (ragweed ...)
epidermal (animal allergens)
fungal allergens (mold)
12. IgE-depended allergic reaction
13. Provoking factors of the bronchospasm
Nonspecific triggers (non-allergenic) - provokebronchospasm in the presence of bronchial
hyperreactivity
Exercise stress
Cold air
Tobacco smoke
Laughter, emotions
Smells (perfumes, household chemicals,
exhaust gases, gasoline, varnish-and-paint
products ...)
14. Symptoms
Wheezingrales
Feeling of chest congestion
Dyspnea
Unproductive cough (may be the
dominant symptom !)
Choking… is a symptom of severe
asthma exacerbation
15.
Chokingappears with non-stopping
severe attack of asthma,
which is regarded as a
severe exacerbation of
asthma and requires
urgent hospitalization and
emergency care
16. About asthma symptoms (it may help in diagnosis)
Provocation(exercise, exposure to an
allergen, cold air, laughter, irritants)
Paroxysmal
Reversibility (spontaneous or after
inhalation of a bronchodilator)
Variability
Symptoms often worsen at night or early in
the morning
Viral respiratory infections often cause
exacerbations of asthma
17. Patient examination
Important !signs of bronchial obstruction appear only at the time
of an attack of bronchospasm:
- inability to speak in sentences with a severe attack
- orthopnoe, sitting position with an inclination
forward with an emphasis on the hands
- wheezing, breathing with difficulty prolonged
exhalation
- participation in the respiration of additional muscles
with a severe attack - diffuse cyanosis
- achypnoe
- on auscultation - wheezes
18. History of life
Childhood (early beginning)Occupational hazards (risk of occupational
BA)
Living conditions (mold, house dust mites,
pets ...)
Smoking
Heredity (many patients have familial AD
cases, but not all)
Allergic history
Other diseases associated with AD - allergic
rhinitis, atopic dermatitis (not in all patients)
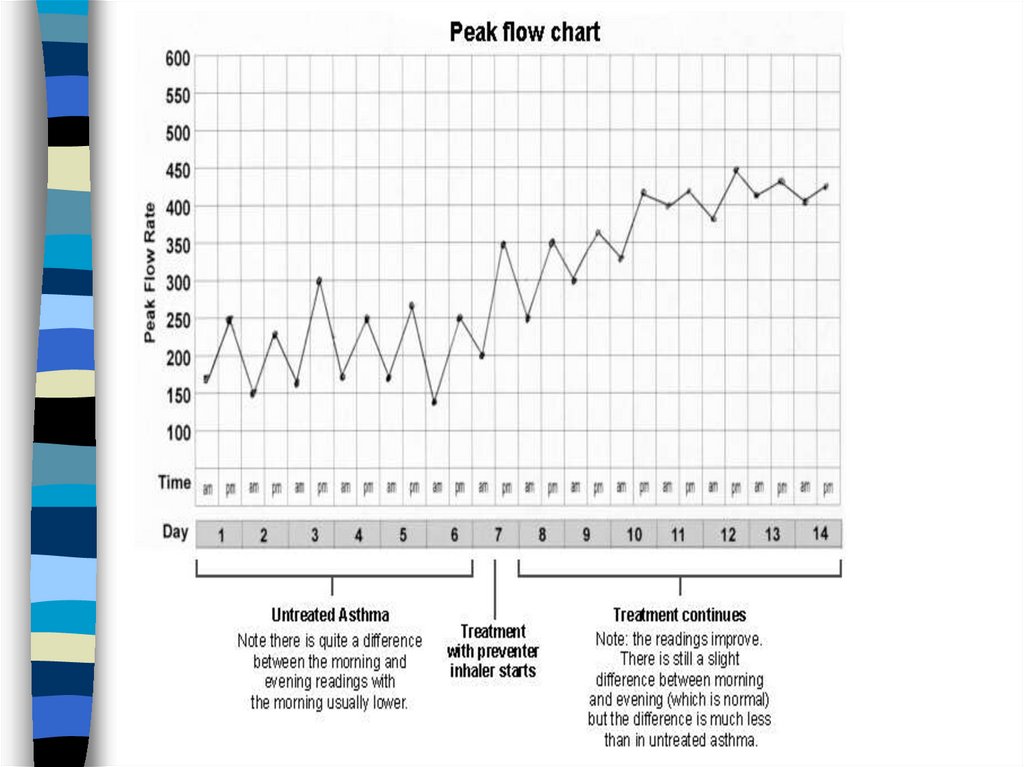
19. Tests
Confirmation of variability ofbronchial obstruction
Peak expiratory flow (PEF)
monitoring - peak flowmetry
Spirometry + test with
bronchodilator
20. Peakflowmeter
21.
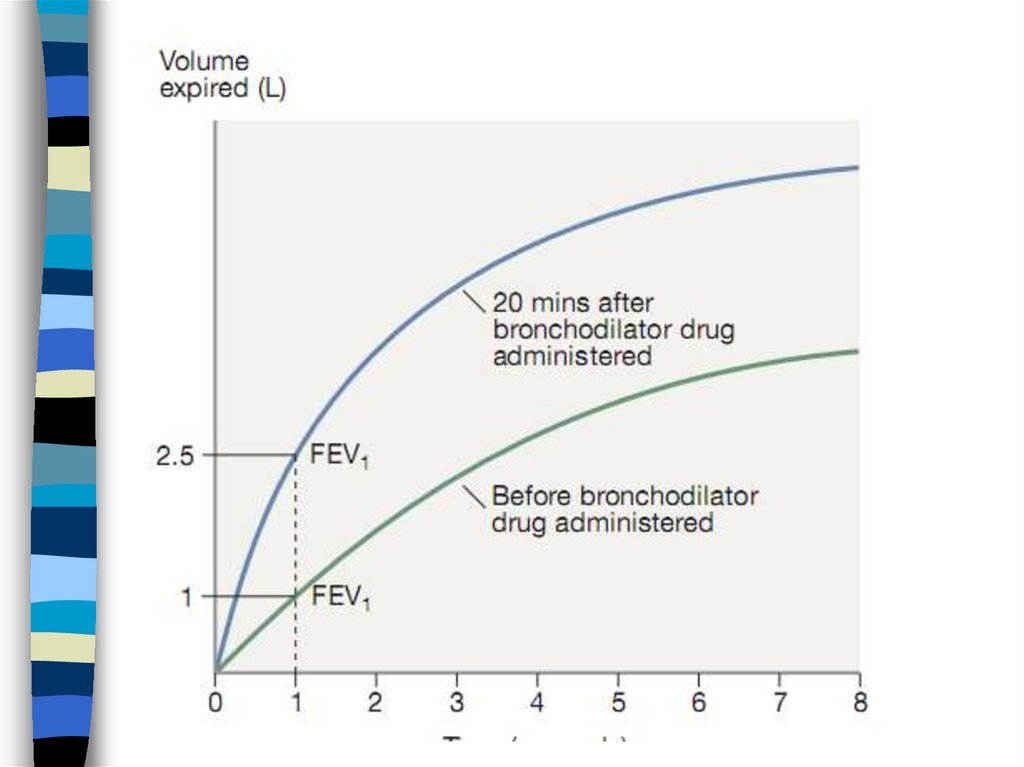
22. Criteria of bronchial obstruction variability
Positive test with bronchodilator (assessed15 min after 400 mcg salbutamol)
FEV1 increase> 12% or 200 ml from the
initial
Increased PEF variability measured twice a
day
mean PEF variability> 10%
23. Положительный тест с бронхолитиком
24.
Can a patient with asthma have normalspirometry and peak flow results?
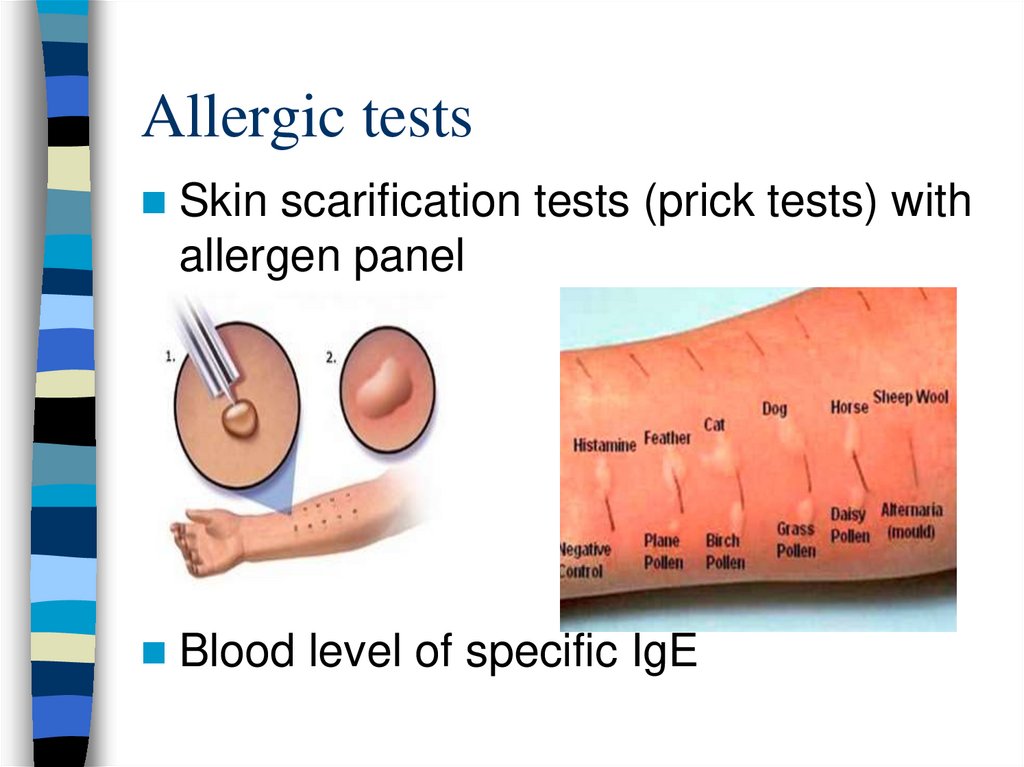
25. Allergic tests
Skin scarification tests (prick tests) withallergen panel
Blood level of specific IgE
26. Others
Eosinophiliais detected in a small
number of patients with AD
In the analysis of sputum,
eosinophils can be detected in
some patients
27. Treatment
1.2.
Long-term (in many patients lifelong) basic
anti-inflammatory therapy with inhaled
glucocorticoids (ICS)
Use of short-acting bronchodilators (SAB)
(salbutamol) as needed
With proper treatment with ICS, asthma symptoms
stop, the need for SAB is minimal, there are no
restrictions on physical activity and there are no
exacerbations of asthma (controlled asthma)
28. Chronic bronchitis
CB - “smoker's cough” when other causes ofcough are excluded (such as asthma,
bronchiectasis, tuberculosis, cancer, pulmonary
fibrosis, sarcoidosis, ACE inhibitors)
The pathological basis of CB is the
hyperproduction of sputum in the bronchi in
response to prolonged irritation by inhaled
particles and gases (more often tobacco smoke)
The only symptom of CB is a chronic cough with
little sputum.
Long-term exposure to tobacco smoking or
occupational exposure to inorganic dust will be
mandatory for the development of CB.
29.
Smokers usually do not seek medicalhelp at the stage of CB, since the cough
in this case is not severe and painful.
Smokers should be actively asked
about coughing
The only treatment is to quit smoking
30. CB =
Chronic productive cough+
Long-term exposure to tobacco smoking
+
Other causes of chronic cough have been
ruled out
31.
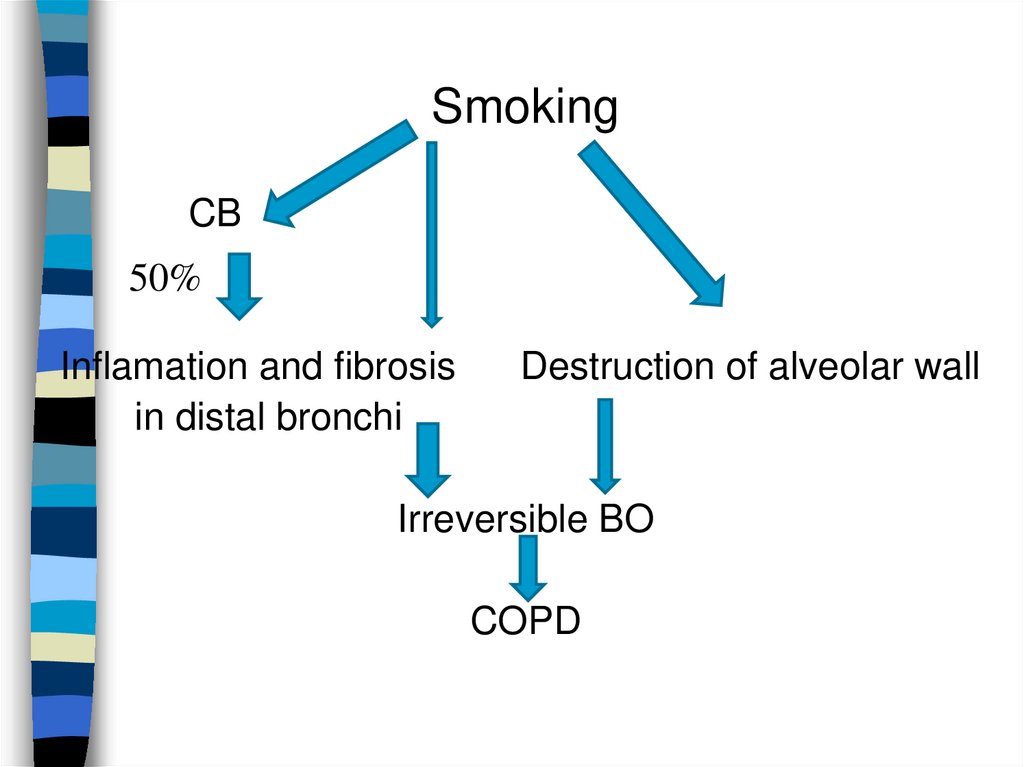
SmokingCB
50%
Inflamation and fibrosis
in distal bronchi
Destruction of alveolar wall
Irreversible BO
COPD
32. Emphysema
Pathomorphological conceptDestruction of the lung parenchyma with
destruction of alveolar septa due to
exposure to tobacco smoke
Now pulmonary emphysema is a
component of the diagnosis of COPD.
33. EL pathogenesis
SmokingActivation of alveolar macrophages
Proteases> Antiproteases (α1-antitrypsin)
Destruction of the alveolar walls
Decreased elastic traction of the lungs
Decreased alveolar support of bronchioles
Early expiratory collapse of bronchioles
(irreversible bronchial obstruction)
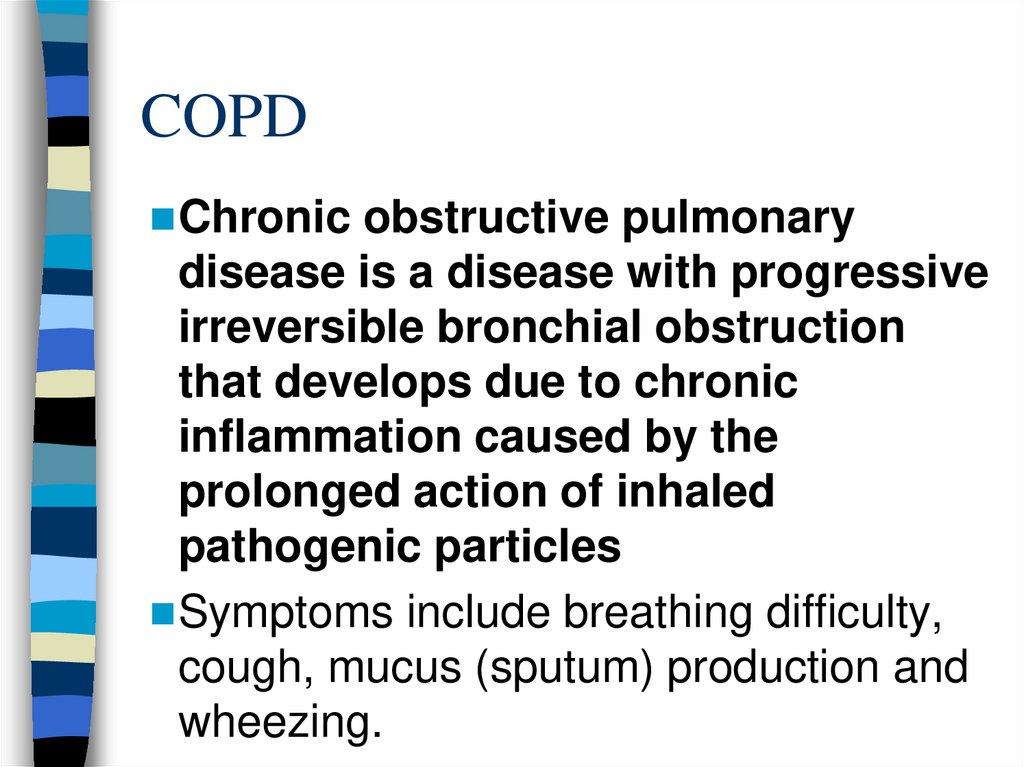
34. COPD
Chronicobstructive pulmonary
disease is a disease with progressive
irreversible bronchial obstruction
that develops due to chronic
inflammation caused by the
prolonged action of inhaled
pathogenic particles
Symptoms include breathing difficulty,
cough, mucus (sputum) production and
wheezing.
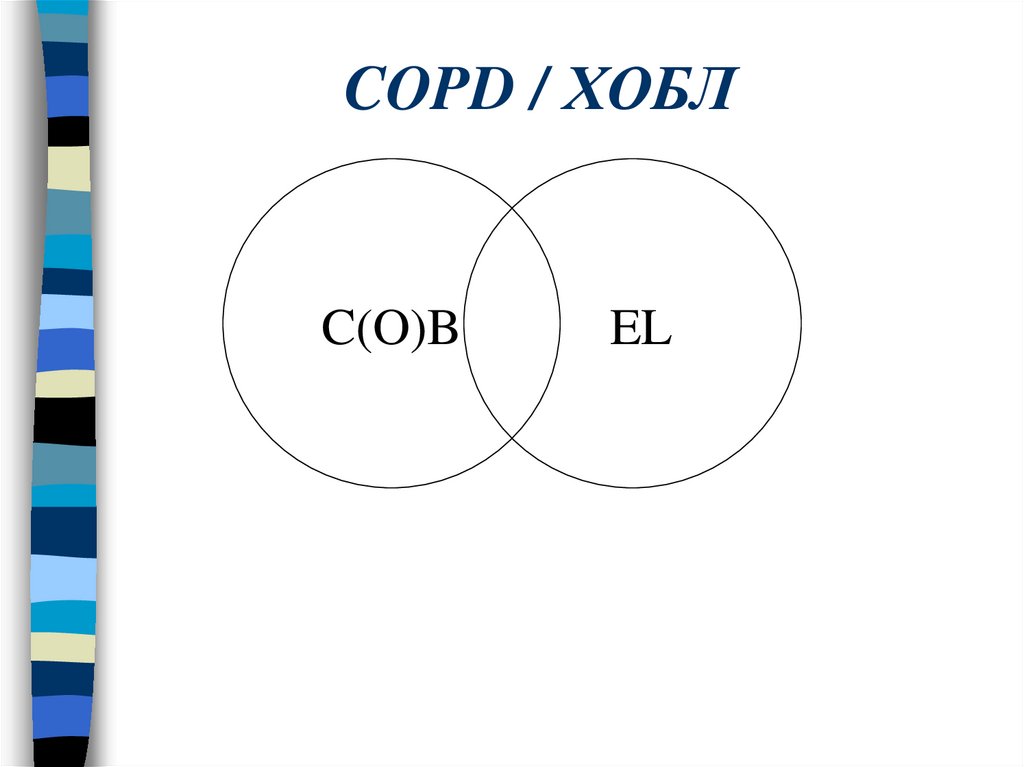
35. COPD / ХОБЛ
C(O)BEL
36. Pathogenesis
- Long-term smoking (smokingexperience 20 packs / years or more,
women may have less smoking
experience)
- Occupational exposure to inorganic dust
(miners)
- Genetic predisposition that determines an
excessive inflammatory response to
inhaled particles
COPD develops in 20-30% of smokers
37.
With the development of bronchialobstruction (narrowing of the distal AW),
the volumetric velocity of the expiratory
air flow is limited, which is the main
feature of COPD.
A patient with COPD cannot quickly
exhale large volumes of air due to an
increase in the resistance of the AW, at
first this feature manifests during
physical activity
38. Air traps (dynamic hyperinflation)
With bronchial obstruction, it is impossible toquickly breathe out a required volume of
air
During physical exertion, with increased
breathing, the expiration time decreases,
which does not allow to fully exhale the
required volume of air (air trap), and the
next inhalation begins after the incomplete
removal of air from the alveoli
39.
Air traps (dynamic hyperinflation)"Air traps" lead to an increase in the residual
volume and a decrease in VC, disrupt the
mechanics of the respiratory muscles
Hyperinflation develops already in the early
stages of the disease and serves as the
main mechanism for the onset of shortness
of breath during exertion in COPD
When the load stops and the respiratory rate
decreases, hyperinflation (air traps) are
resolved
40.
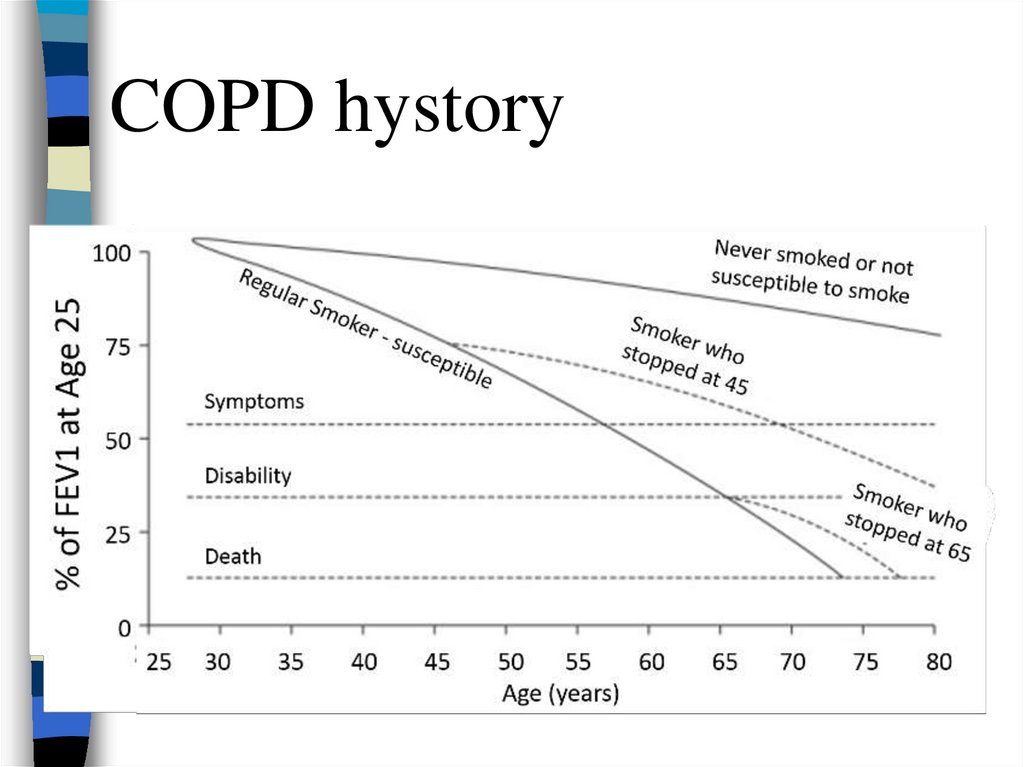
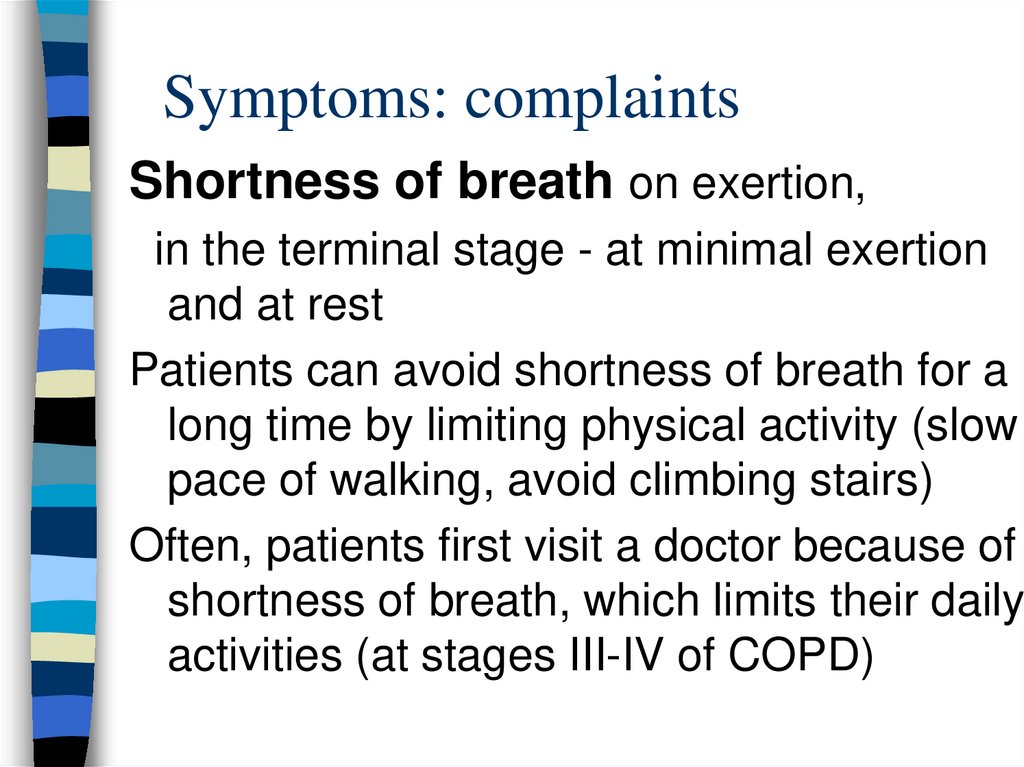
COPD hystory41. Symptoms: complaints
Shortness of breath on exertion,in the terminal stage - at minimal exertion
and at rest
Patients can avoid shortness of breath for a
long time by limiting physical activity (slow
pace of walking, avoid climbing stairs)
Often, patients first visit a doctor because of
shortness of breath, which limits their daily
activities (at stages III-IV of COPD)
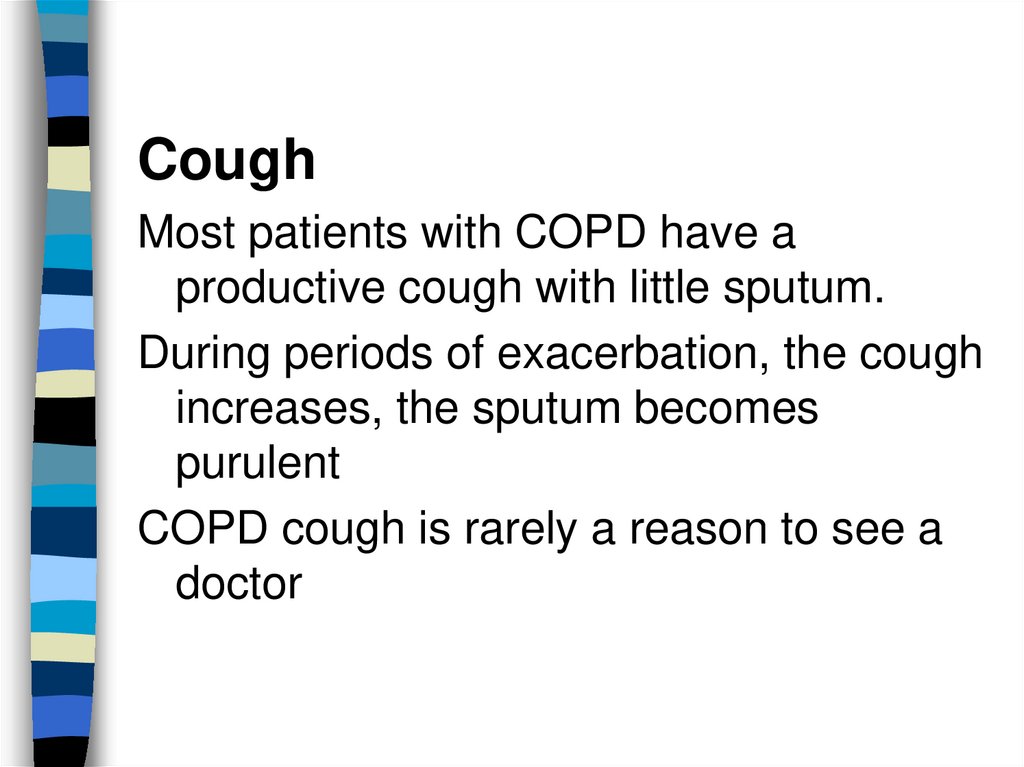
42.
CoughMost patients with COPD have a
productive cough with little sputum.
During periods of exacerbation, the cough
increases, the sputum becomes
purulent
COPD cough is rarely a reason to see a
doctor
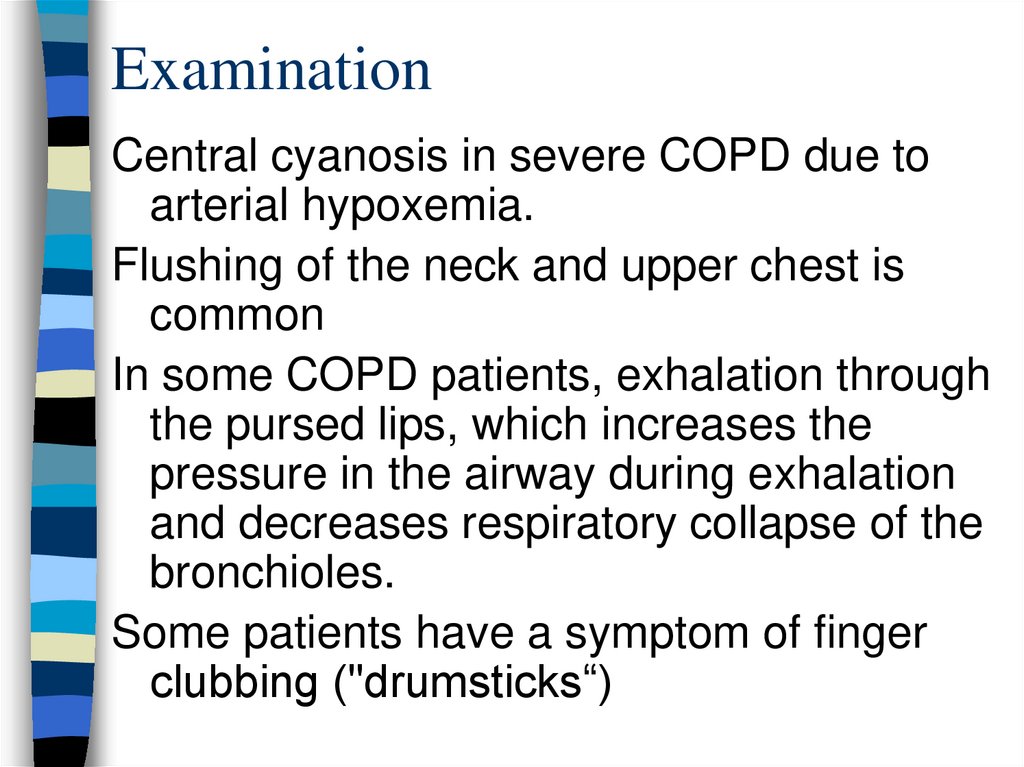
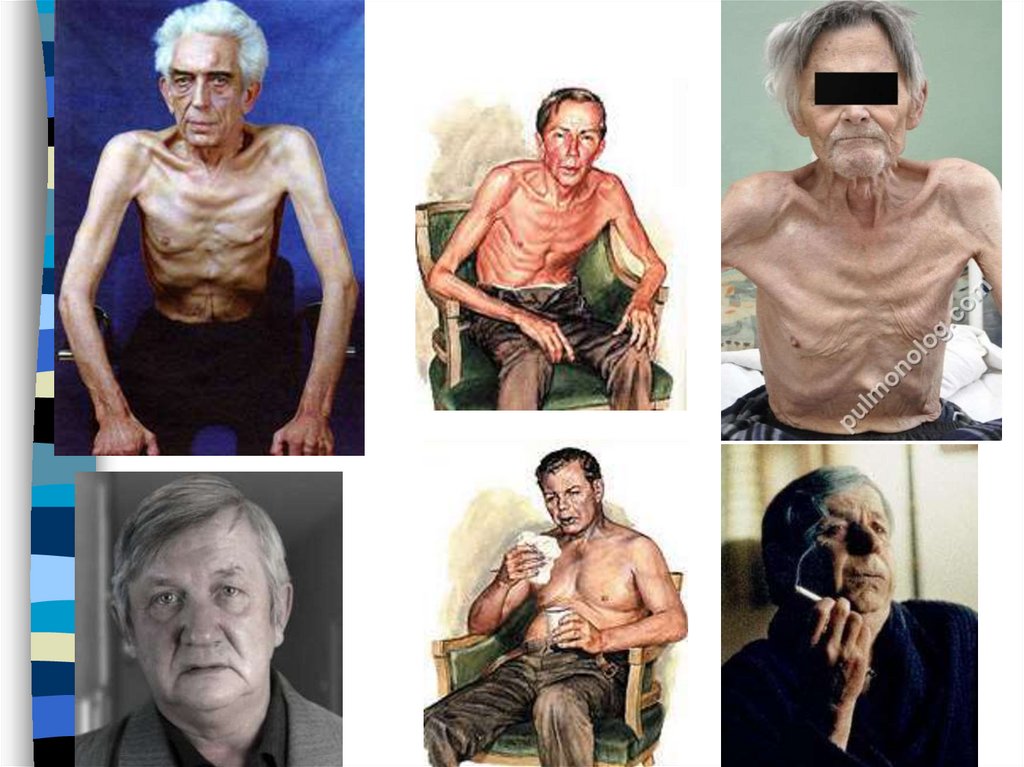
43. Examination
Central cyanosis in severe COPD due toarterial hypoxemia.
Flushing of the neck and upper chest is
common
In some COPD patients, exhalation through
the pursed lips, which increases the
pressure in the airway during exhalation
and decreases respiratory collapse of the
bronchioles.
Some patients have a symptom of finger
clubbing ("drumsticks“)
44.
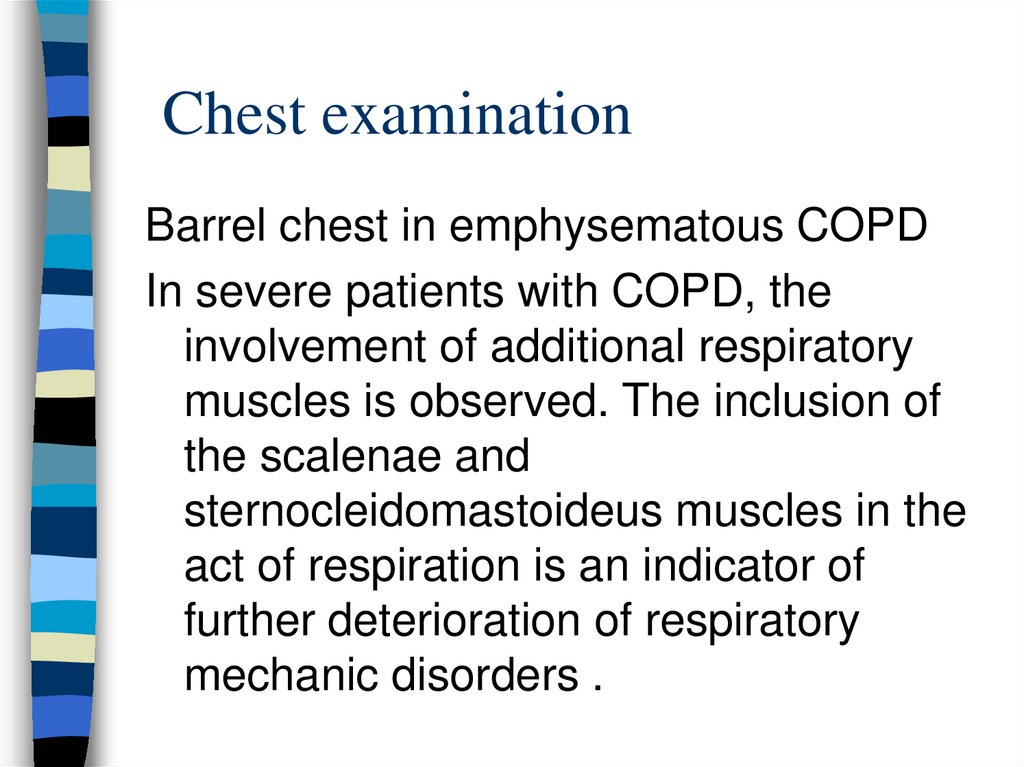
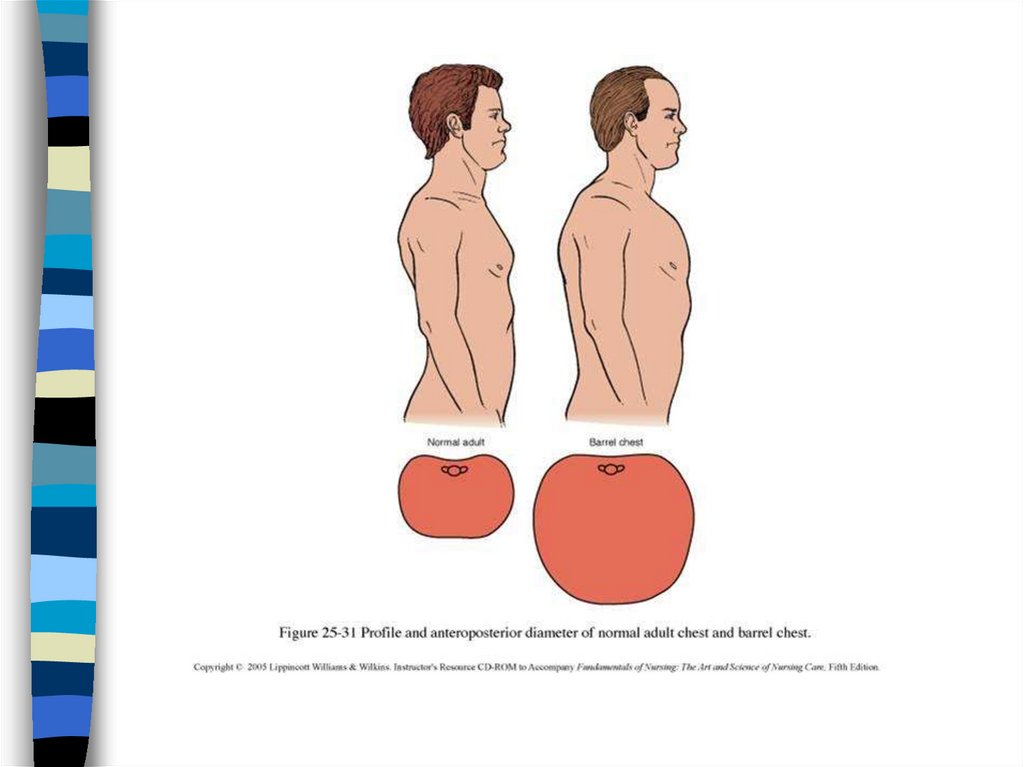
45. Chest examination
Barrel chest in emphysematous COPDIn severe patients with COPD, the
involvement of additional respiratory
muscles is observed. The inclusion of
the scalenae and
sternocleidomastoideus muscles in the
act of respiration is an indicator of
further deterioration of respiratory
mechanic disorders .
46.
47.
48.
Palpation and percussionWith emphysema and pulmonary
hyperinflation, a boxed (hyperresonant)
percussion sound is determined.
Auscultation
Emphysema silence the main breathing
sound and even heart sounds
Adventitious breathing sounds:
Monophonic (rhonchi) and polyphonic high
pitched wheezes may be heard
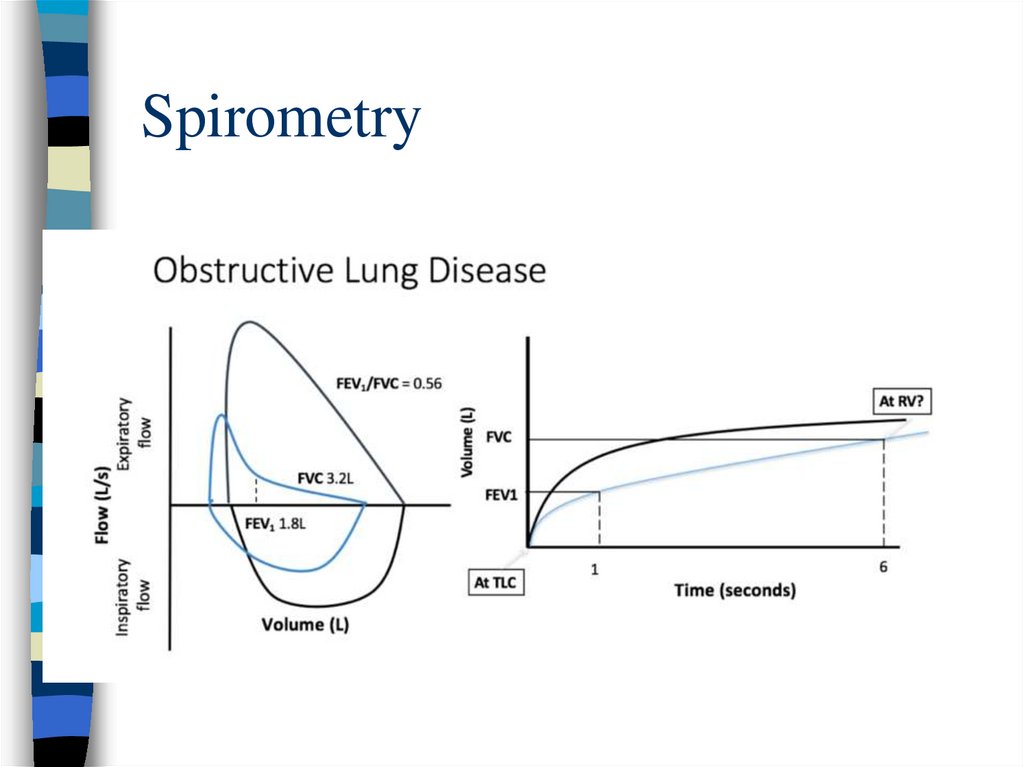
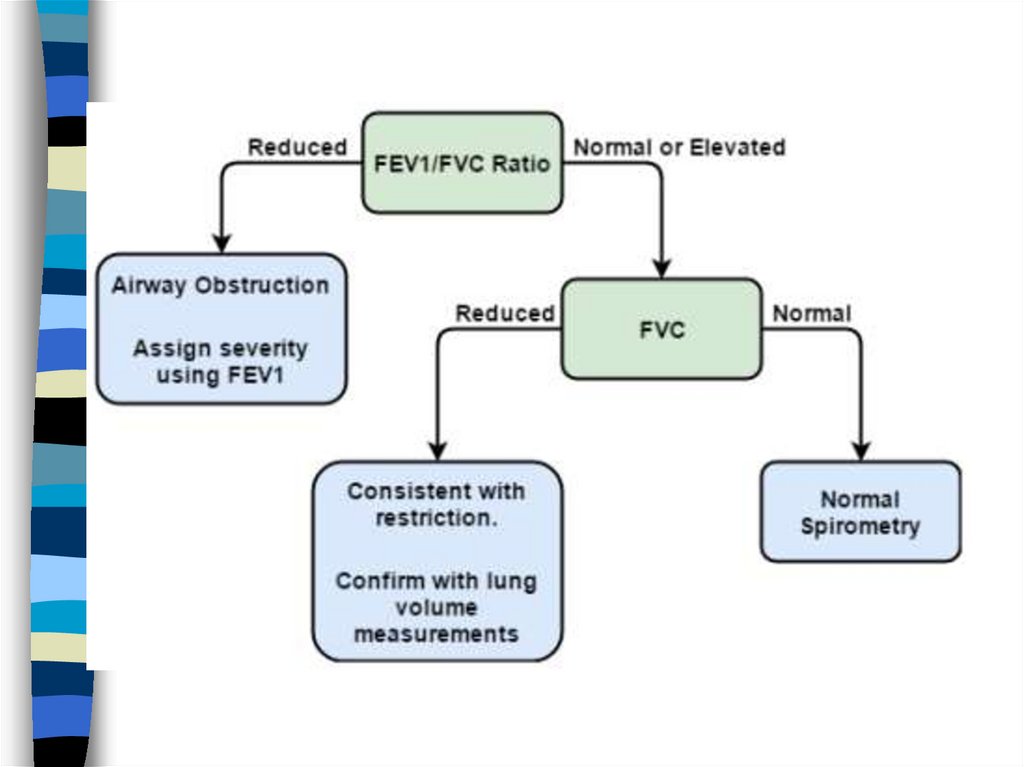
49. Spirometry
50.
51.
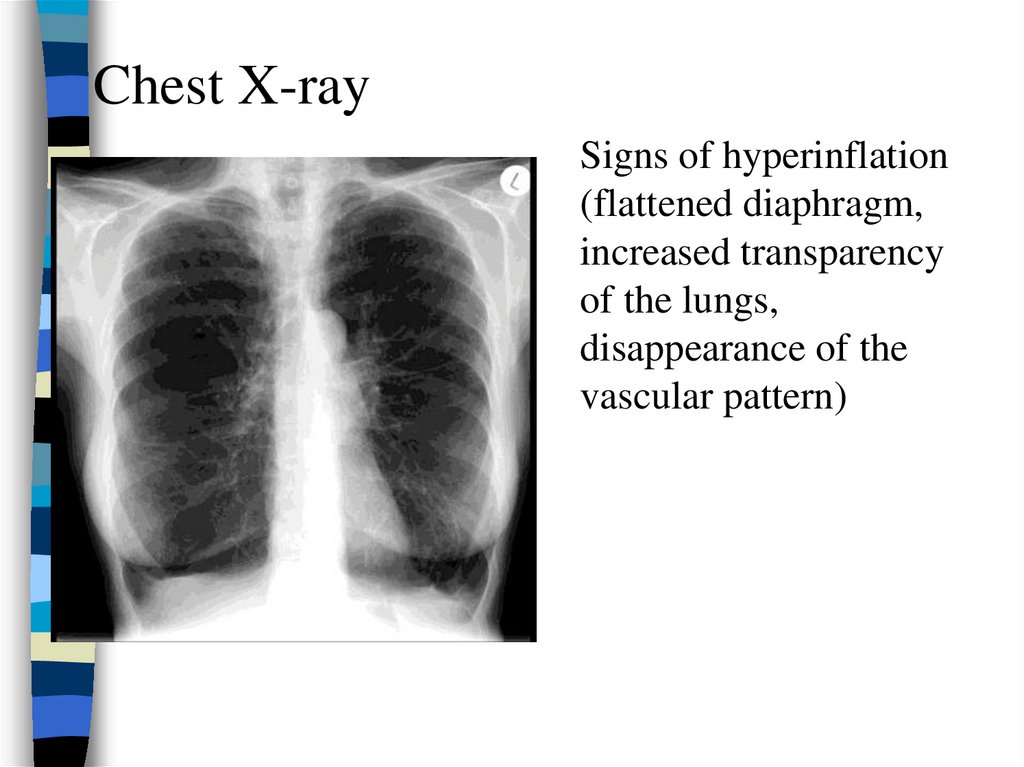
Chest X-raySigns of hyperinflation
(flattened diaphragm,
increased transparency
of the lungs,
disappearance of the
vascular pattern)
52. COPD diagnosis =
Long-term exposure to smoking+
Detection of irreversible BO on spirometry
(Tiffno index <0.7)
+
Other causes of irreversible BO are
excluded
53. Treatment principles
1.2.
3.
QUITING SMOKING is the only
treatment that can slow the
progression of COPD
Bronchodilators on demand (for
shortness of breath, before exercise)
and on an ongoing basis
With the development of severe RF,
long-term home oxygen therapy








 medicine
medicine