Similar presentations:
Bronchial asthma
1. Bronchial asthma
Kazakh National Medical University named after Asfendiyarov S.D.Bronchial asthma
Faculty: GM
Group: 57-2
Student: Yessetova Gulnur
Almaty-2015
2. Definition
Bronchial asthma is a chronic, inflammatorydisease of the respiratory tract, which is
characterized by bronchial hyperreactivity and
respiratory obstruction.
3. Etiology
1.2.
3.
4.
5.
The development of bronchial asthma
is a multicausal process, which is
caused
by
exogenic
factors
(environmental factors), and also by
genetic dispositions. In addition, the
course of the disease can be
influenced by climatic changes and
mental factors. Important exogenic
activators are:
Allergens: environmental allergens
(house dust mites, pollen),allergenic
work substances (flour), food
allergens
Toxins or chemical irritants
Respiratory diseases
Pseudoallergic reactions (PAR) to
analgesics (analgesic-induced asthma)
Physical exertion (mainly in children)
4. Epidemiology
As a rule, bronchial asthma already occurs ininfancy and is the most common chronic disease of
this stage of life.
5. Classification
According to etiologyAllergic or extrinsic asthma
Non-allergic or intrinsic asthma
Mixed forms
According to degree of severity
Grade 1: Intermittent
Grade 2: Persistent, mild (symptoms more than twice a
week, but no more than once in a single day )
Grade 3: Persistent, moderate (symptoms once a day and
more than one night a week )
Grade 4: Persistent, severe (symptoms throughout the day
on most days and frequently at night )
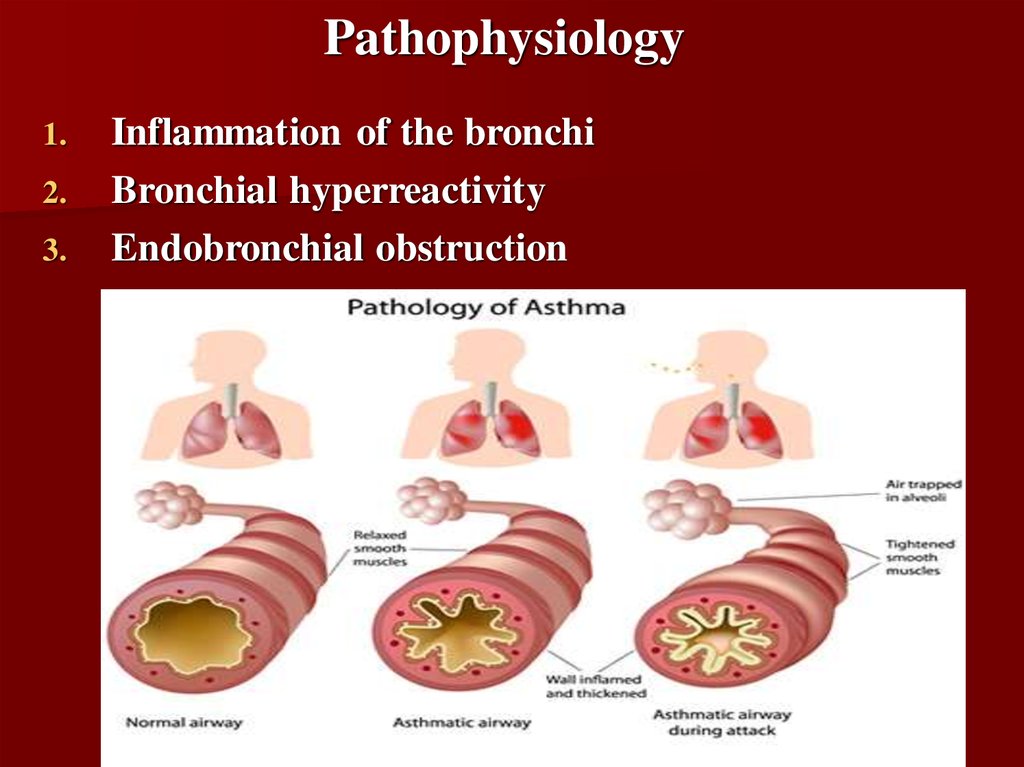
6. Pathophysiology
1.2.
3.
Inflammation of the bronchi
Bronchial hyperreactivity
Endobronchial obstruction
7. Inflammation of the bronchi
Allergens or infections elicit an infectious reaction of the bronchialmucous membrane. In allergic asthma, an IgE-induced reaction of
the immediate type (Type 1 reaction) occurs immediately after
inhalation of the allergen. The mast cells in the mucous membrane
degranulate and thereby release inflammation mediators like
histamine, ECF-A, bradykinin and leukotrienes ("immediate
reaction"). Apart from this immediate reaction, there also exists an
IgG-induced late reaction after 6-12 hours or a combination of both
reaction types ("dual reaction"). As a rule, the triggering allergen can
only be identified at the early stage of the disease. In the course of
years, the range of allergens often becomes wider, thereby making it
more difficult or even impossible for the patient to avoid allergens.
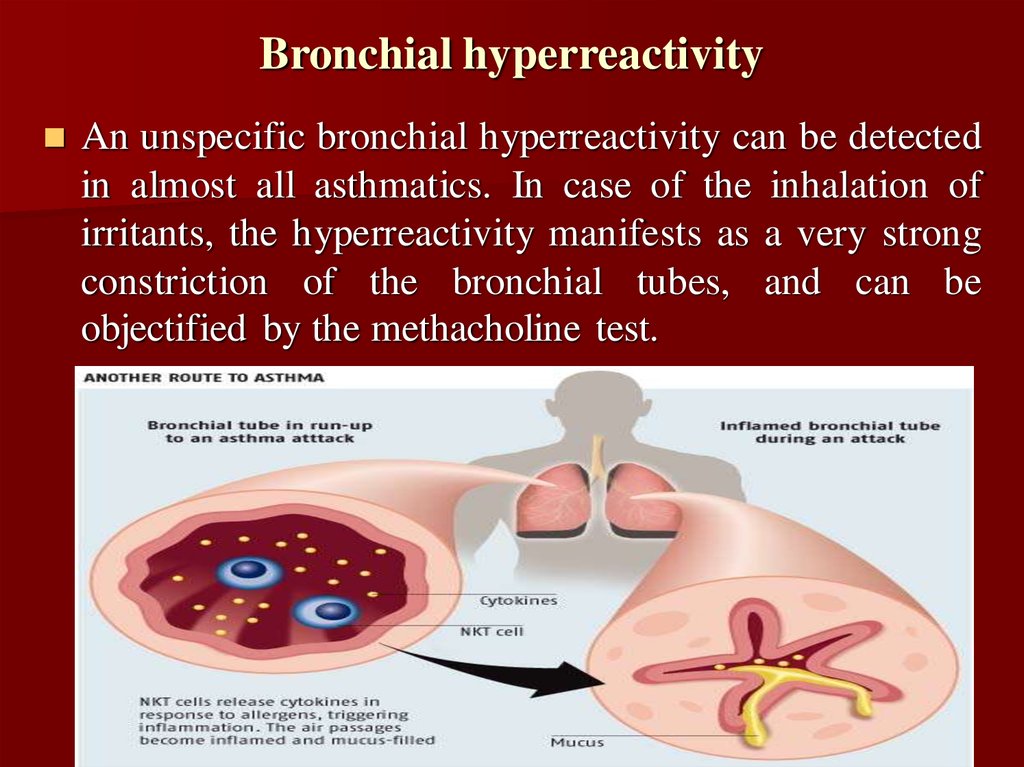
8. Bronchial hyperreactivity
An unspecific bronchial hyperreactivity can be detectedin almost all asthmatics. In case of the inhalation of
irritants, the hyperreactivity manifests as a very strong
constriction of the bronchial tubes, and can be
objectified by the methacholine test.
9. Endobronchial obstruction
The endobronchial obstruction is quasi the first clinicallydiscernible "end product" of the pathophysiological
processes of bronchial asthma. It develops through the shift
of the bronchial lumen as a consequence of mucosal
edema, increased mucus secretion (dyscrinism) and
bronchospasms.
10. Symptoms
Cough with or without sputum (phlegm) productionPulling in of the skin between the ribs when breathing (intercostal retractions)
Shortness of breath that gets worse with exercise or activity
Wheezing
Emergency symptoms that need prompt medical help:
Bluish color to the lips and face
Decreased level of alertness, such as severe drowsiness or confusion, during an
asthma attack
Extreme difficulty breathing
Rapid pulse
Severe anxiety due to shortness of breath
Sweating
Other symptoms that may occur:
Abnormal breathing pattern --breathing out takes more than twice as long as
breathing in
Breathing temporarily stops
Chest pain
Tightness in the chest
11.
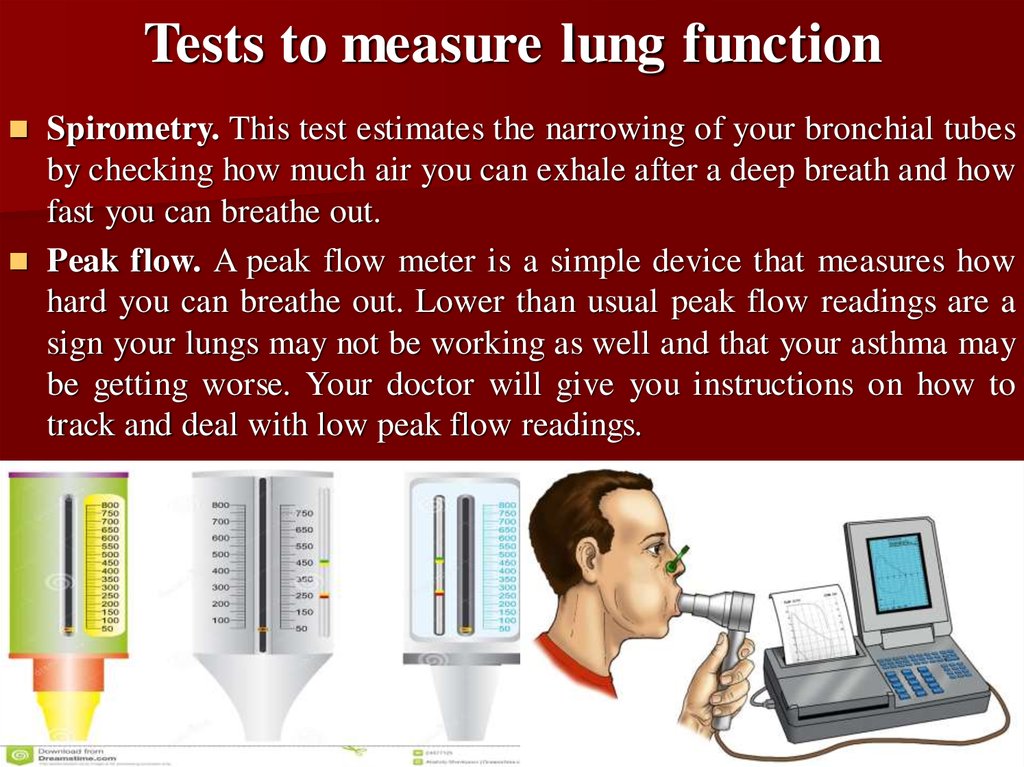
12. Tests to measure lung function
Spirometry. This test estimates the narrowing of your bronchial tubesby checking how much air you can exhale after a deep breath and how
fast you can breathe out.
Peak flow. A peak flow meter is a simple device that measures how
hard you can breathe out. Lower than usual peak flow readings are a
sign your lungs may not be working as well and that your asthma may
be getting worse. Your doctor will give you instructions on how to
track and deal with low peak flow readings.
13. Additional tests
Methacholine challenge. Methacholine is a known asthmatrigger that, when inhaled, will cause mild constriction of your
airways. If you react to the methacholine, you likely have
asthma. This test may be used even if your initial lung function
test is normal.
Imaging tests. A chest X-ray and high-resolution computerized
tomography (CT) scan of your lungs and nose cavities (sinuses)
can identify any structural abnormalities or diseases (such as
infection) that can cause or aggravate breathing problems.
14. Additional tests
Allergy testing. This can be performed by a skin test or blood test.Allergy tests can identify allergy to pets, dust, mold and pollen. If
important allergy triggers are identified, this can lead to a
recommendation for allergen immunotherapy.
Provocative testing for exercise and cold-induced asthma.In
these tests, your doctor measures your airway obstruction before
and after you perform vigorous physical activity or take several
breaths of cold air.
15. Treatment
Non-pharmacological treamentRemoval of allergens (especially pets with feathers or fur) (evidence level A)
Structured patient education: improved self-management leading to better
symptomatic control, reduction of the number of asthma attacks and
emergency situations, improved quality of life, and improvement in various
other parameters of disease course including days taken off from school or
work and days spent in hospital (evidence level A)
Physical training (reduction of asthma symptoms, improved exercise
tolerance, improved quality of life, reduced morbidity) (evidence level C)
Respiratory therapy and physiotherapy (e.g., breathing techniques, pursedlip breathing) (evidence level C)
Smoking cessation (with medical and non-medical aids, if necessary)
(evidence level B)
Psychosocial treatment approaches (family therapy) (evidence level C)
For obese patients, weight loss (evidence level B)
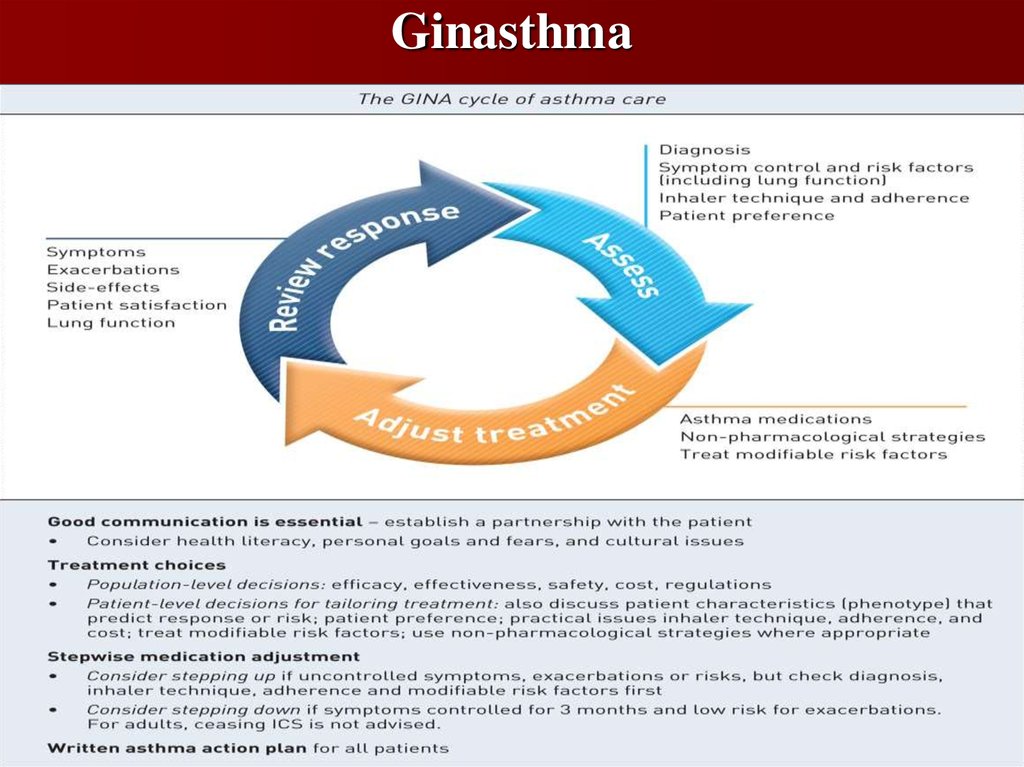
16. Ginasthma
17. GINA
The Global Initiative for Asthma (GINA) was establishedin 1993 by the World Health Organization and National
Heart Lung and Blood Institute to develop a global
strategy for managing and preventing asthma. GINA
reports, now funded independently through the sale of
GINA products, have provided the foundation for many
national guidelines. They are prepared by international
experts from primary, secondary and tertiary care, and are
annually updated following a review of evidence.
18. Литература
1.Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al.
Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy
Clin Immunol . 2010;126:466-76. Greaves M: Childhood leukaemia. BMJ 2002, 324:
283 [PMID: 11823363]
2. Lugogo N, Que LG, Fertel D, Kraft M. Asthma. In: Mason RJ, Broaddus VC, Martin
TR, et al., eds. Murray & Nadel's Textbook of Respiratory Medicine . 5th ed.
Philadelphia, Pa.: Elsevier Saunders; 2010:chap 38.
3. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm.




 medicine
medicine








