Similar presentations:
Neuromuscular and occlusive articulatory dysfunctional TMJ syndromes. Arthritis, TMJ arthrosis
1.
Neuromuscular and occlusivearticulatory dysfunctional TMJ
syndromes.
Arthritis, TMJ arthrosis
2.
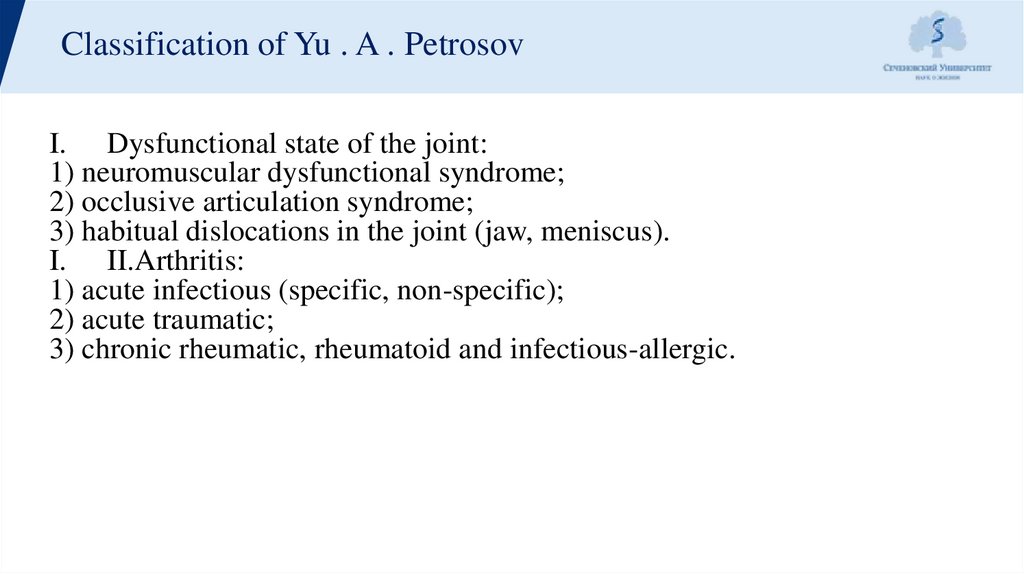
Classification of Yu . A . PetrosovI. Dysfunctional state of the joint:
1) neuromuscular dysfunctional syndrome;
2) occlusive articulation syndrome;
3) habitual dislocations in the joint (jaw, meniscus).
I. II.Arthritis:
1) acute infectious (specific, non-specific);
2) acute traumatic;
3) chronic rheumatic, rheumatoid and infectious-allergic.
3.
Classification of Yu . A . PetrosovIII. Arthrosis:
1) post-infectious (neoarthrosis);
2) post-traumatic (deforming) osteoarthritis;
3) myogenic osteoarthritis;
4) metabolic arthrosis;
5) ankylosis (fibrous and bony).
IV. Combined forms.
V. Neoplasms (benign and malignant) anddysplastic (tumor-like) processes
4.
Neuromuscular dysfunctional syndromeNeuromuscular dysfunctional
syndromeIt is characterized by
severe neuralgic pains of
arthrogenic origin, as well as
muscle pain, clicking in the
joint, displacement (deviation)
of the jaw to the side, jerky,
zigzag movements, headaches,
dizziness, tinnitus, a feeling of
"sand pouring" or a rush of
blood in the ears, bruxism, while
there are no radiological changes
in the joint.
5.
Etiology1. Muscle spasm (premature contacts in the dentition, morphological
changes in muscle fibers, joint elements)
2. Impaired coordination of muscle contractions
3. Overstretching of the musculoskeletal system (excessive opening of the
mouth)
4. Overstrain or atony of muscles (unilateral type of chewing)
5. Injury
6. Hormonal factors
7. Constitutional features of the joint structure
6.
Pathogenesis1. Impaired function of the masticatory muscles
2. Violation of occlusal-articulatory relationships of dentition and
jaws
3. Congenital and acquired abnormalities in the structure of the TMJ
7.
Clinical1. Clicking in the TMJ
2. Pain in the TMJ, in the masticatory muscles, various parts of the
face, neck, head, tongue (spastic contraction of the lateral pterygoid
muscle)
3. Displacement of the jaw to the side
4. Jerky, zigzag movements of the LF
5. Tinnitus, a feeling of sand pouring or a rush of blood in the ears
At the same time, the absence of radiological changes in the joints and
in the occlusal ratios of the dentition and jaws is characteristic.
8.
Diagnostics1. Soreness during palpation
through the external auditory
canal
2. Soreness when pressing on
the chin in the distal direction
3. Soreness during palpation of
the places of attachment of the
masticatory muscles
4. MRI, CT, EMG diagnostics
9.
Tomograms of the rightand left TMJ. Diagnosis:
right-sided
neuromuscular
dysfunctional TMJ
syndrome
10.
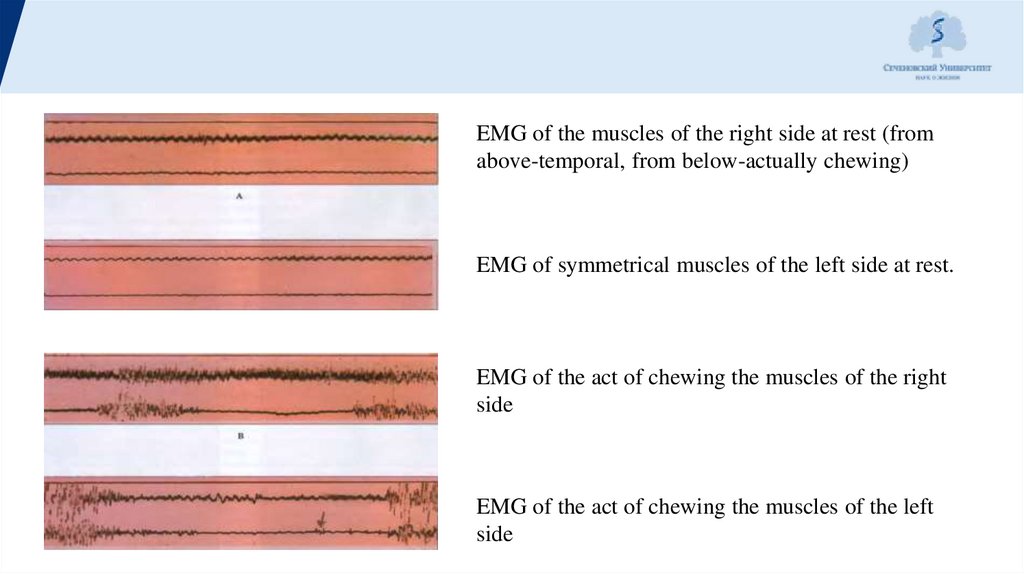
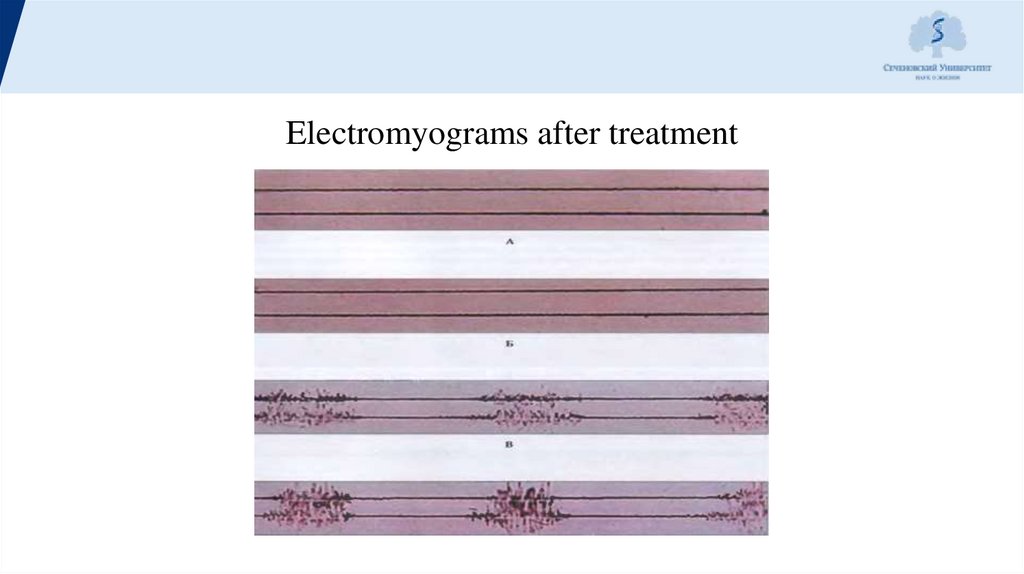
EMG of the muscles of the right side at rest (fromabove-temporal, from below-actually chewing)
EMG of symmetrical muscles of the left side at rest.
EMG of the act of chewing the muscles of the right
side
EMG of the act of chewing the muscles of the left
side
11.
Electromyograms after treatment12.
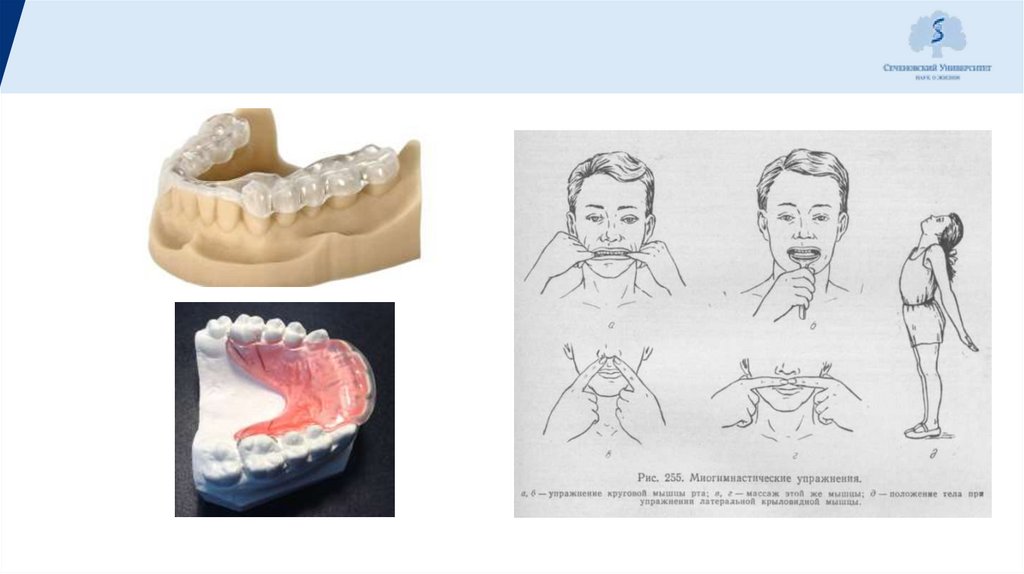
Treatment1. Gymnastic exercises
2. Selective grinding of teeth
3. Orthopedic, hardware (according to indications) method of
treatment:
a. Non-removable limiting splint - with jerky movements of the
woofer
b. Non-removable orthopedic limiting device
IV. Dental prosthetics
V. Drug therapy
13.
Occlusive articulation syndromeOcclusive articulation syndromeThis is a
dysfunctional condition in which the
symptom complex (pain, crunching,
clicking, etc.) is associated with a change
in the occlusal-articulatory relationship of
the dentition and jaws.
14.
Etiology1. Decreasing bite
2. Distal shift of the bass
3. Loss of chewing teeth
4. Lateral shift of the woofer
5. Deep traumatic bite
6. Prosthetics errors
7. Premature contacts (lead to a permanent shift of the LF, and an unusual
excursion of the articular heads leads to dystrophic changes in the intraarticular meniscus, permanent microtrauma of the articular surfaces)
15.
Clinical1. Crunching, clicking in the joint (as a result of the mobility of the meniscus,
its bending and rapid alignment during movement)
2. Pain:
-constant dull aching – with a decreasing bite
-acute short-term - with a sliding bite and prosthetics errors
-acute irradiating – with non-synchronous, atypical movements of the
condyles, sharp lateral and distal shifts of the LF both with a decreasing bite
and with its normal height
3. Low frequency offset, facial asymmetry
4. Stuffiness, tinnitus, dizziness, feeling of high tide when tilting the head
down, feeling of sand pouring over
16.
Treatment1. Only prosthetics or a palatine plate with a bite pad in the frontal
region to restore the height of the bite for 3 months, prosthetics.
2. Myogymnastics, neuromuscular reconstruction with the help of a
bite plate, then complete restoration of the dentition with the fixation
of a non-removable limiting apparatus (a year after the loss of molars,
premolars)
3. With a decreasing bite and distal shift of the LF, myohymnastics for
a month, a palatal plate with an inclined plane in the frontal region for
3-6 months, prosthetics
17.
4. For persons over the age of 25 years: myogymnastics 1-2 months, a fixedtire with an inclined plane on the balancing side and a plastic mouth guard on
the working side 6-8 months. Expanding plastic on the HF with segmental
sawing in the area of the chewing teeth to be moved in the vestibulooral
direction. On the balancing side, the deocclusal gap is filled with an occlusal
pad made of plastic, from which an inclined plane departs downwards.
Prosthetics.
5. With a decreasing bite with the phenomena of bruxism – mouthguards on
the entire dentition of the LF or on the lateral teeth on both sides 3-6 months.
Prosthetics
18.
19.
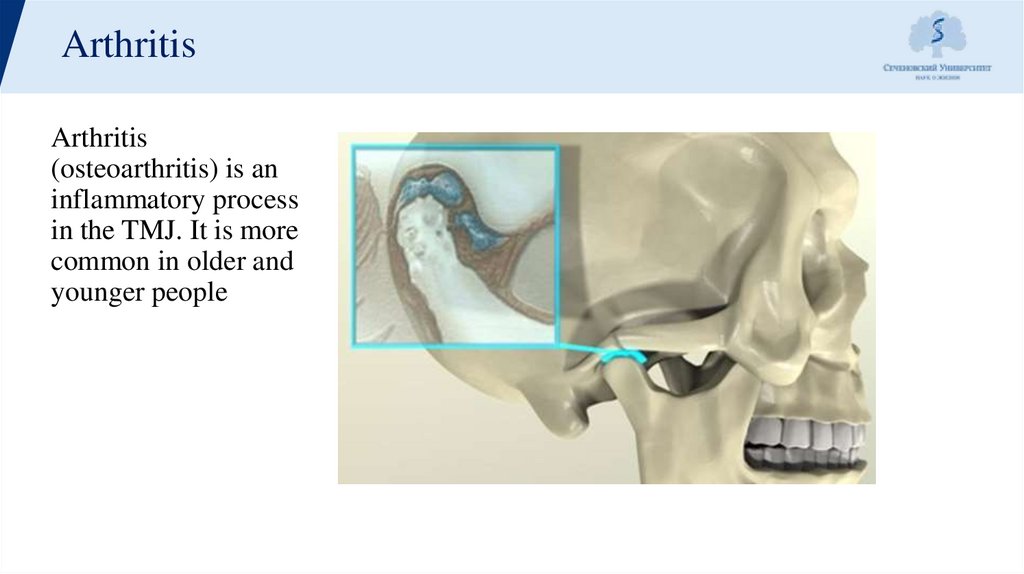
ArthritisArthritis
(osteoarthritis) is an
inflammatory process
in the TMJ. It is more
common in older and
younger people
20.
Etiology1. Local infection - periodontitis, gingivitis, stomatitis, otitis, sore throat,
osteomyelitis
2. Common infectious diseases - SARS, influenza, pneumonia, dysentery,
tuberculosis, syphilis
3. Allergic diseases
4. Traumatic factors
5. Paraallergic factors - hypothermia, increased insolation
6. Changes in the endocrine and nervous system
7. The presence of foci of chronic infection (especially in PR)
21.
Clinical1. Severe joint pain, which increases with the slightest movements of the lower jaw, decreases
only when the lower jaw is at rest
2. Limited opening of the mouth to 10-15 mm (between the central incisors)
3. The lower jaw shifts towards the affected joint (deviation of the lower jaw)
4. A large irradiation zone, possibly in the temporal region of the head, sometimes the neck
5. Has an acute onset
6. There may be swelling, swelling or infiltration of soft tissues in front of the tragus of the
ear
7. Sharp pain during palpation
8. Hyperemia and tension of the skin of the parotid region
22.
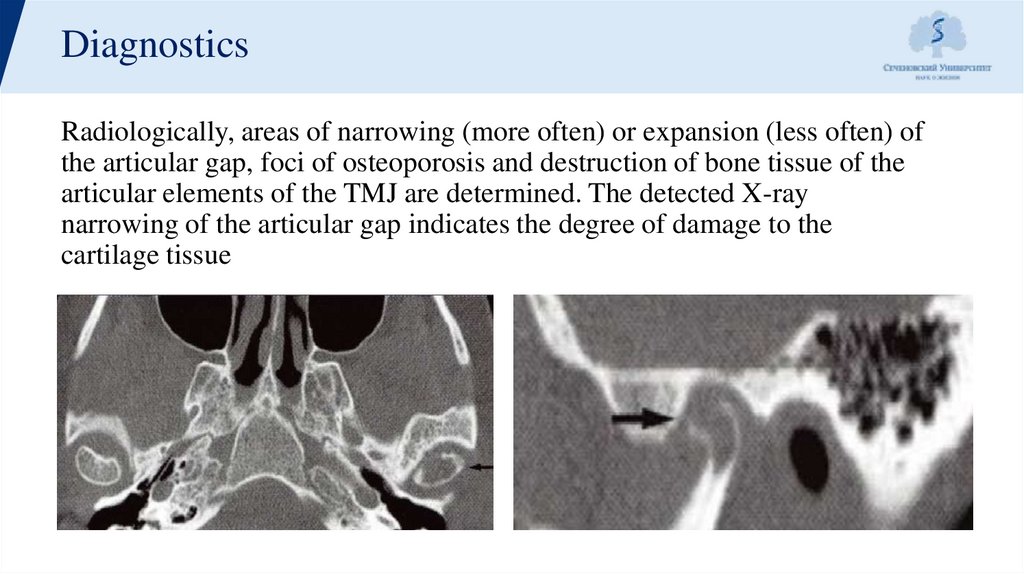
DiagnosticsRadiologically, areas of narrowing (more often) or expansion (less often) of
the articular gap, foci of osteoporosis and destruction of bone tissue of the
articular elements of the TMJ are determined. The detected X-ray
narrowing of the articular gap indicates the degree of damage to the
cartilage tissue
23.
Treatment1. Elimination of the cause
2. Rest in the joint.To separate the articular surfaces, an individually made
splint is used on one of the jaws
3. Blockades of soft tissues by the type of creeping infiltrate into the joint area
with 0.5% trimecaine or lidocaine solution 2 times a week (4-5 times)
4. Medical treatment
5. Physiotherapy treatment: warming compresses, UHF therapy, fluctuation,
electrophoresis with anesthetics
24.
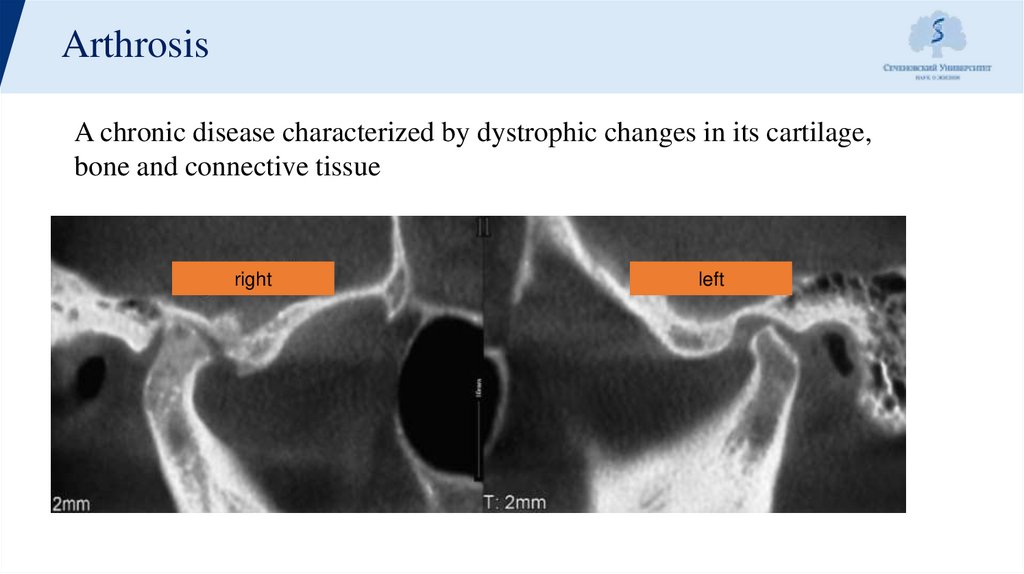
ArthrosisA chronic disease characterized by dystrophic changes in its cartilage,
bone and connective tissue
Хроническое заболевание, характеризующееся
right
дистрофическими
изменениями его хрящевой, left
костной и
соединительной ткани
25.
EtiologyLocal reasons:
1.
2.
3.
4.
5.
Long-term inflammatory process in the joint
2. Excessive load on the articular surface of the head of the lower jaw,
which may be associated with neuromuscular disorder of the
maxillofacial region, for example, with bruxism;
3. Lack of teeth, especially lateral;
4. Deformation of the occlusal surface of the dentition
5. Pathological erasability.
26.
EtiologyGeneral reasons
1.
2.
3.
4.
Exchange violations
Neurodystrophic disorders
Endocrine disorders
Infectious diseases
27.
Clinical1.
Complaints about :
-constant aching, dull pain, which increases with stress on the joint
-the appearance of pathological noises, crunching, crepitation, clicks
-restriction of mouth opening, displacement of the lower jaw to the side
-chewing food only on one side, as chewing on the opposite side causes pain and
inconvenience
2. As a result of the examination of the face, the following can be revealed: a decrease in the
height of its lower part
3. Facial asymmetry due to the displacement of the lower jaw towards the affected joint
4. Palpation and auscultation reveal crunch, crepitation in the joint
28.
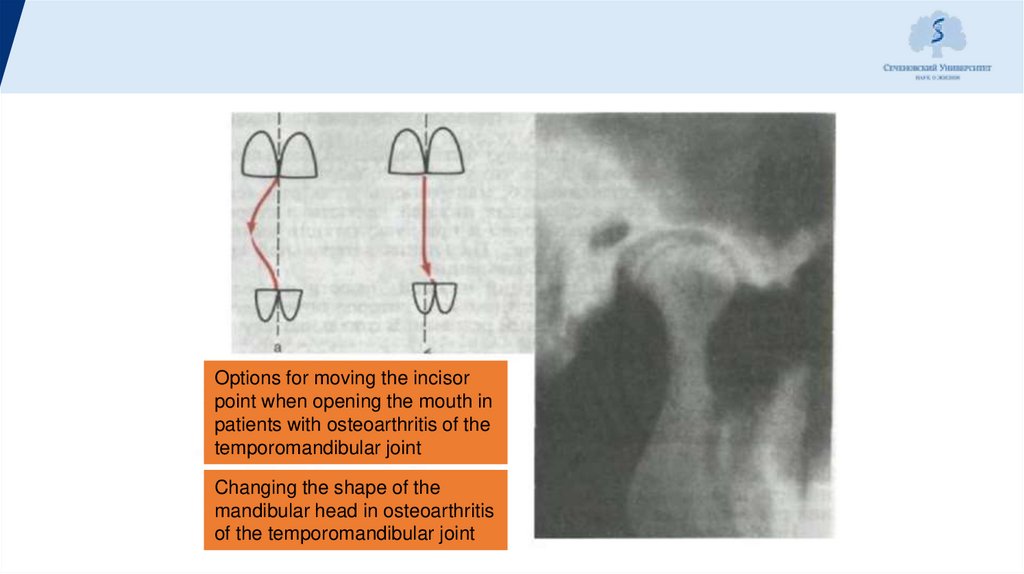
Options for moving the incisorpoint when opening the mouth in
patients with osteoarthritis of the
temporomandibular joint
Changing the shape of the
mandibular head in osteoarthritis
of the temporomandibular joint
29.
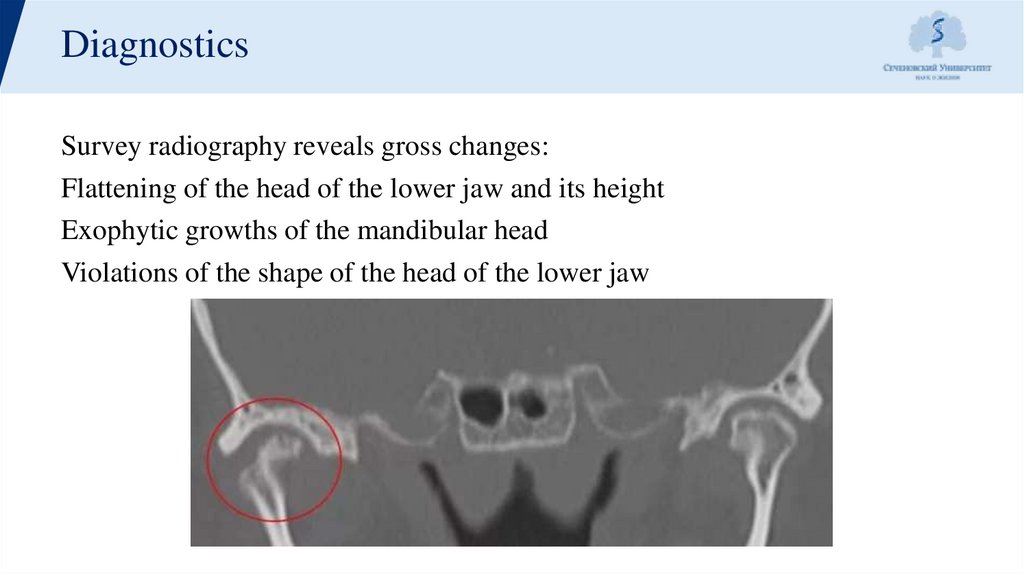
DiagnosticsSurvey radiography reveals gross changes:
Flattening of the head of the lower jaw and its height
Exophytic growths of the mandibular head
Violations of the shape of the head of the lower jaw
30.
Treatment1. Medical treatment
2. Physiotherapy treatment
3. Orthopedic method
4. Surgical method
31.
Medical treatment1. Relief of emotional stress;
2. Spasm relief;
3. Anesthesia, which can be carried out:
-non-narcotic analgesics: acetylsalicylic acid at a dose of 250-500 mg;
metamizole sodium (analgin) at a dose of 500 mg; in-dometacin at a
dose of 25 mg; ibuprofen (brufen) at a dose of 200 mg;
- using blockades with 0.25-0.5% anesthetic solution without
vasoconstrictor, as well as surface anesthesia
32.
Physiotherapy treatment1. Electrophoresis
2. Heat treatment (paraffin, ozokerite)
3. UHF therapy
33.
Orthopedic method1.
2.
3.
4.
Normalization of the ratio of dentition
Normalization of occlusive contacts
Restoration of anatomical integrity of teeth and dentition
Restoration of bite height
34.
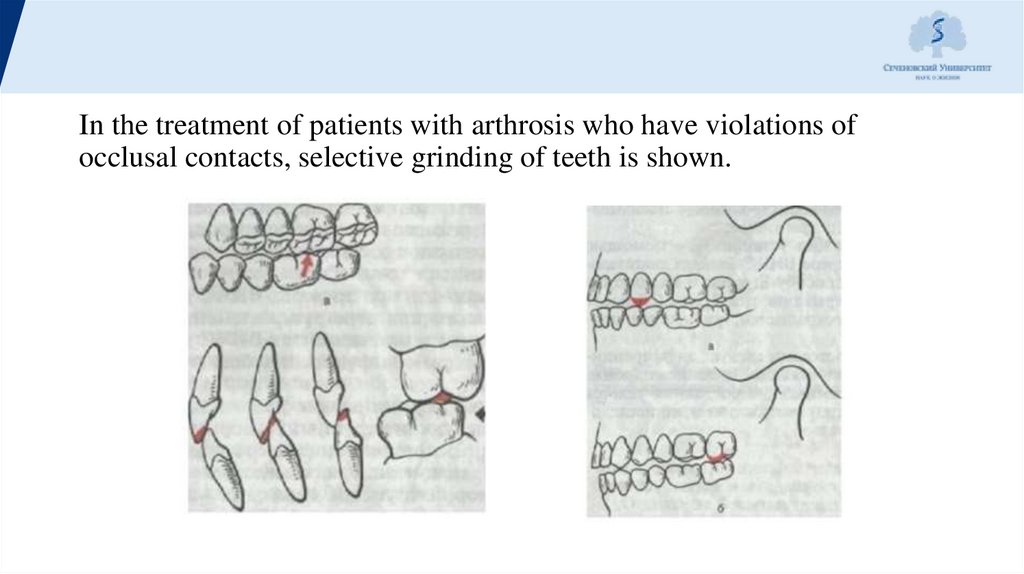
In the treatment of patients with arthrosis who have violations ofocclusal contacts, selective grinding of teeth is shown.
35.
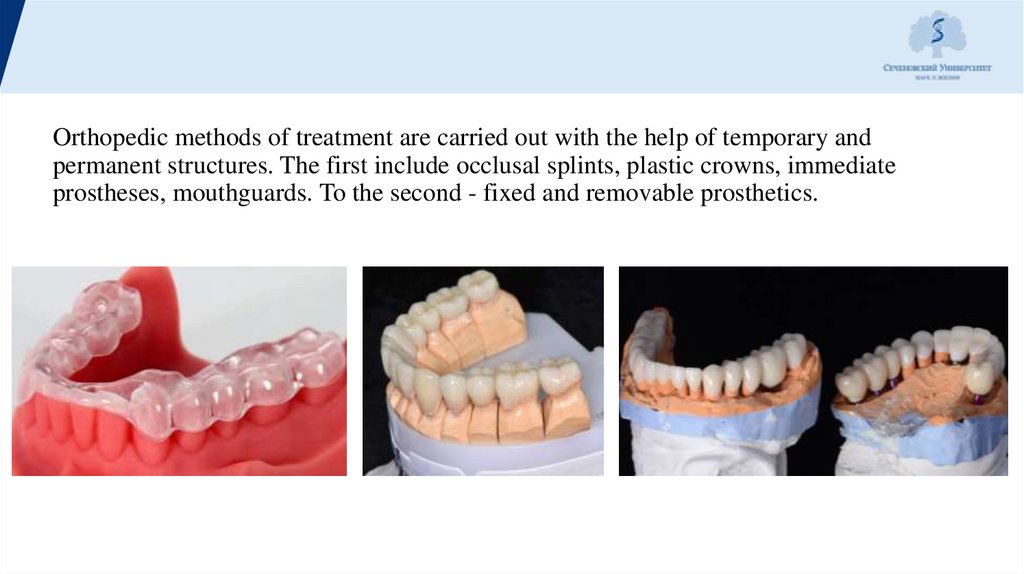
Orthopedic methods of treatment are carried out with the help of temporary andpermanent structures. The first include occlusal splints, plastic crowns, immediate
prostheses, mouthguards. To the second - fixed and removable prosthetics.
36.
Surgical methodIn the treatment of the final stages of osteoarthritis of the jaw joint, 3 main
types of operations are performed:
1.
Removal of the articular head of the lower jaw
2. Removal of the articular disc
3. Removal of the head with its subsequent replacement with a graft.
Arthroplasty is an operation that restores the function of the joint. With
arthroplasty, the articular ends are separated, new articular surfaces are
modeled and pads from the patient's tissues (skin, fascia) are placed between
them
37.
38.
Thanks for yourattention



 medicine
medicine