Similar presentations:
Traumatic occlusion and periodontal overload
1.
Traumatic occlusion and periodontaloverload.
A method of selective grinding of teeth
that block the movement of the lower
jaw.
Neuromuscular
and
occlusalarticulation
dysfunctional
TMJ
syndromes
2022 Moscow
2.
Traumatic occlusion is a pathologicalcondition of the closure of the dentition,
in which hyperfunctional tension of
individual teeth or a group of teeth
occurs, leading to changes in
periodontal tissues, muscle
dysfunctions, diseases of the
temporomandibular joints
3.
In turn, long-term traumatic occlusioncauses persistent trophic disorders of
periodontal tissues and accelerates
destruction processes, which leads to a
significant deterioration in the clinical
picture of the disease and the progression
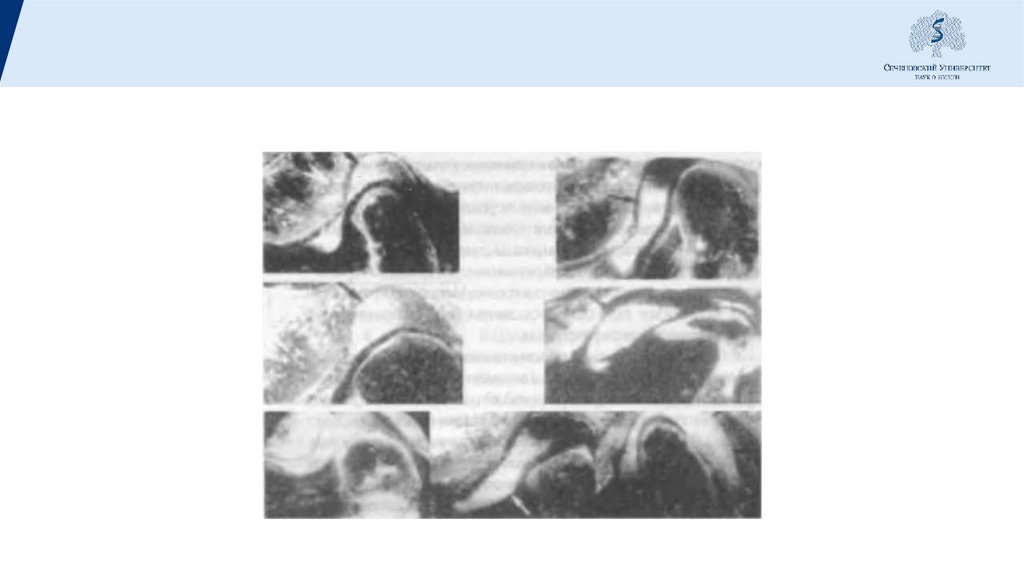
of the pathological process.
4.
Types of traumatic occlusionAccording to the mechanism, they distinguish:
Primary
Secondary
Combined
5.
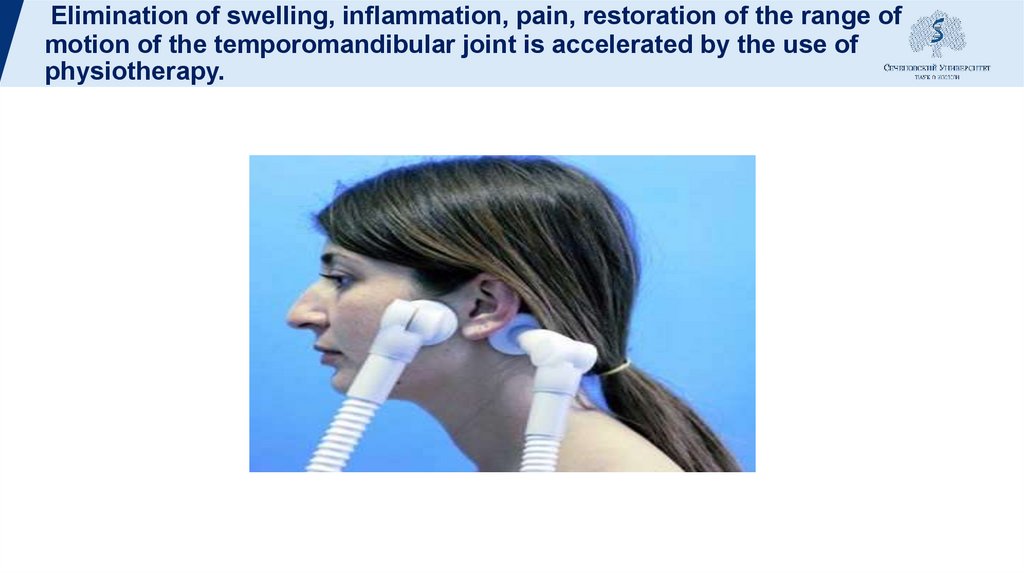
CAUSES OF PRIMARY TRAUMATIC OCCLUSIONAnomalies in the eruption and position of the teeth,
dentition and jaws
Partial loss of teeth
Pathological abrasion of hard dental tissues
Mistakes in dentures and poorly made dentures
Forced orthodontic treatment
Parafunctions of chewing muscles
Bad habits, etc.
6.
CAUSES OF SECONDARY TRAUMATIC OCCLUSIONSecondary traumatic occlusion is caused by both local
(various diseases of the organs and tissues of the
masticatory apparatus) and general (hormonal, etc.)
changes in the human body. Among the local causes
indicate periodontal disease, periodontal disease,
inflammatory, tumor processes, etc.
7.
CAUSES OF COMBINED TRAUMATIC OCCLUSIONThis is the most common form of traumatic
occlusion, which is characterized by
conditions in which an increased load falls
on the affected periodontium.
The occurrence of combined traumatic
occlusion is due to a combination of
etiological factors characteristic of primary
and secondary traumatic occlusion.
8.
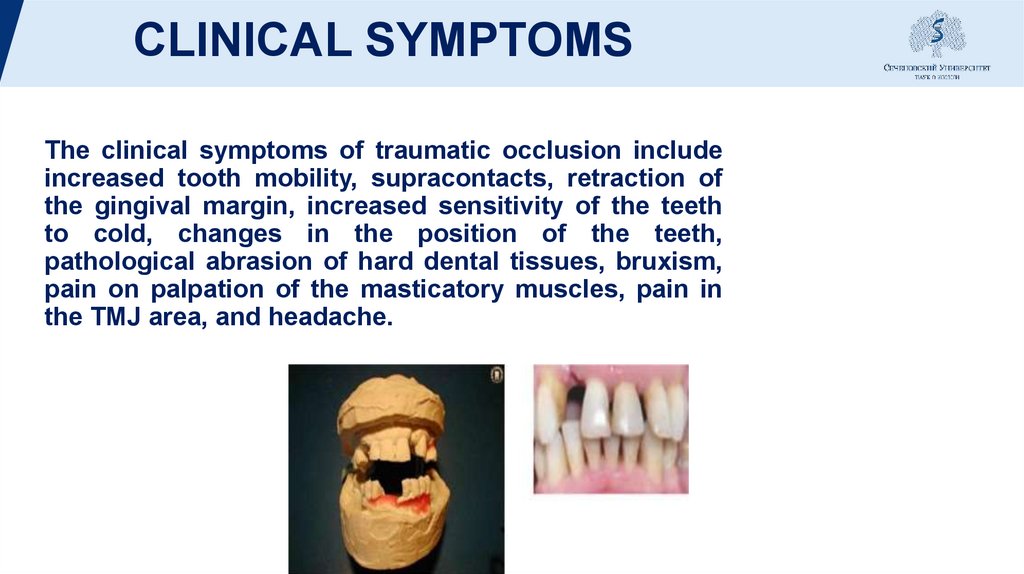
CLINICAL SYMPTOMSThe clinical symptoms of traumatic occlusion include
increased tooth mobility, supracontacts, retraction of
the gingival margin, increased sensitivity of the teeth
to cold, changes in the position of the teeth,
pathological abrasion of hard dental tissues, bruxism,
pain on palpation of the masticatory muscles, pain in
the TMJ area, and headache.
9.
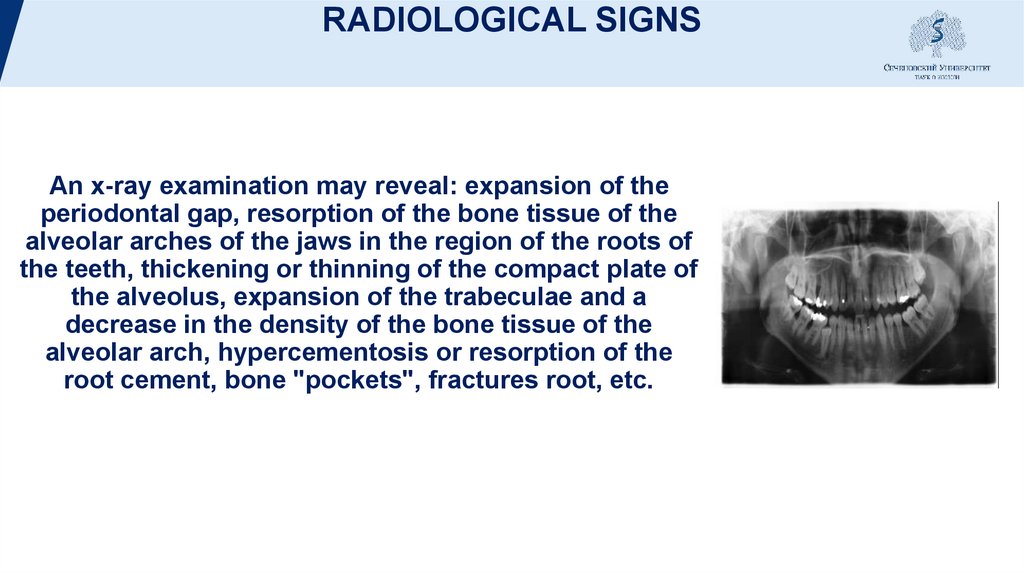
RADIOLOGICAL SIGNSAn x-ray examination may reveal: expansion of the
periodontal gap, resorption of the bone tissue of the
alveolar arches of the jaws in the region of the roots of
the teeth, thickening or thinning of the compact plate of
the alveolus, expansion of the trabeculae and a
decrease in the density of the bone tissue of the
alveolar arch, hypercementosis or resorption of the
root cement, bone "pockets", fractures root, etc.
10.
TREATMENTThe treatment of occlusal trauma is
always complex in nature, using
therapeutic, surgical, orthodontic and
orthopedic methods, which cannot be
considered in isolation from each other.
Treatment is based on the principle of an
individualized approach to each patient,
taking into account the data of the
general and dental status.
11.
In orthopedic treatment of a patient withperiodontal pathology, it is necessary:
correctly distribute the chewing load
among the preserved natural teeth;
remove from some teeth (groups of teeth)
excessive load (traumatic knot) resulting
from the loss of natural teeth or their
extension;
create a lost functional unity for the entire
dentition, connect the disparate links of
the chewing apparatus into a single
system of the dentition;
create conditions of relative rest for the
damaged periodontium and eliminate the
main ailment of the disease - the mobility
12.
SELECTIVE GRINDING OF TEETHConsidering that with the progression of periodontal
diseases, functional and morphological dissociation of
the dentition occurs, which is expressed in a change in
the position of individual teeth, pathological tooth
mobility, a deterioration in the ratio of the extra- and
intra-alveolar parts of the tooth, etc., premature
contacts (supra-contacts) of the teeth and traumatic
occlusion. This requires a mandatory change in the
method of selective grinding of teeth (occlusal
rehabilitation).
13.
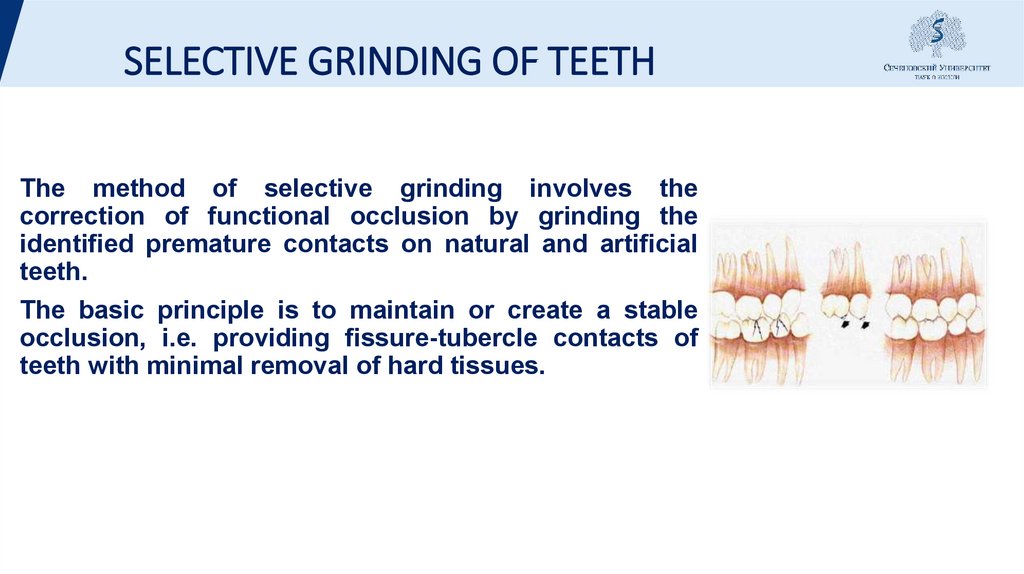
SELECTIVE GRINDING OF TEETHThe method of selective grinding involves the
correction of functional occlusion by grinding the
identified premature contacts on natural and artificial
teeth.
The basic principle is to maintain or create a stable
occlusion, i.e. providing fissure-tubercle contacts of
teeth with minimal removal of hard tissues.
14.
CONTRAINDICATIONSSevere inflammation of the periodontium. In such a situation, before
grinding, it is necessary to carry out preparatory therapeutic
measures: remove dental plaque, conduct a course of antiinflammatory periodontal therapy. However, it should be kept in mind
that supracontacts may support the inflammatory response. In these
cases, both types of treatment should be carried out simultaneously.
Pronounced anomalies and deformities of the dentition, subject to
orthodontic, orthopedic, surgical or combined treatment.
Acute and chronic diseases of the TMJ, accompanied by pain
syndrome of muscular-articular dysfunction. In such patients,
selective grinding is indicated in the remission stage.
15.
Selective teethgrinding method
Method Jankelson V.A.
Jankelson V.A., (1979) proposes to eliminate premature
contacts that appear during central occlusion.
The lateral and anterior articulatory movements of the
lower jaw are not corrected by this technique, since the
position of the lower jaw during anterior and lateral
occlusions appears only with parafunctions of the
masticatory muscles. The Jankelson technique is called
the functional method. In the process of grinding, the
movements of the lower jaw are not manually controlled
or corrected by the doctor. The closure of the dentition is
carried out by the patient himself (without the help of a
doctor) in the most convenient position for him.
16.
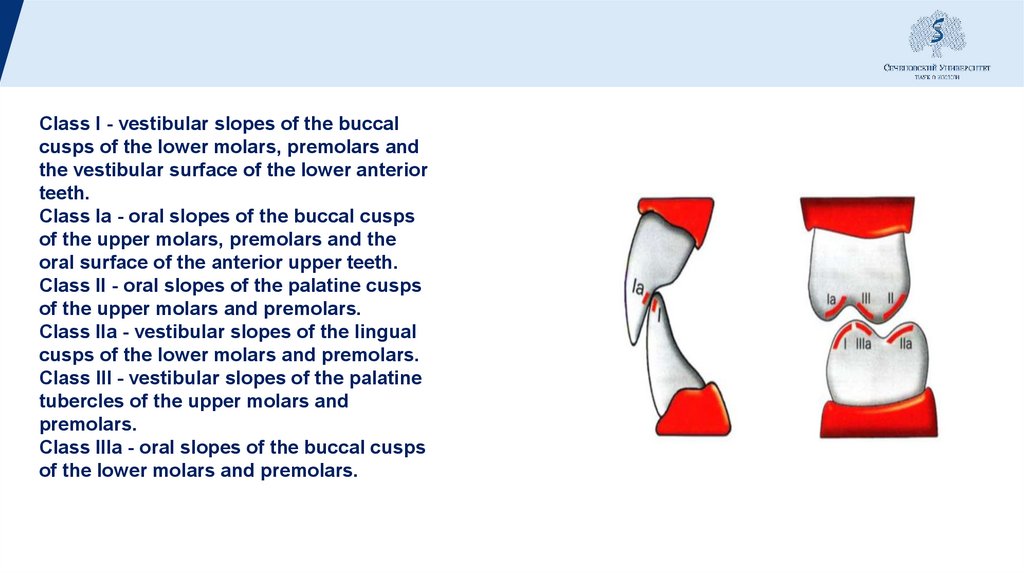
Class I - vestibular slopes of the buccalcusps of the lower molars, premolars and
the vestibular surface of the lower anterior
teeth.
Class Ia - oral slopes of the buccal cusps
of the upper molars, premolars and the
oral surface of the anterior upper teeth.
Class II - oral slopes of the palatine cusps
of the upper molars and premolars.
Class IIa - vestibular slopes of the lingual
cusps of the lower molars and premolars.
Class III - vestibular slopes of the palatine
tubercles of the upper molars and
premolars.
Class IIIa - oral slopes of the buccal cusps
of the lower molars and premolars.
17.
Selective polishing is carried out in 4-5 visits, depending on thesupercontacts (if the contact is 2.5 mm in area, then 5 visits), in order to
facilitate the restoration of the body to a good condition.
18.
1 visitArticulating paper is placed on the upper jaw, while the lower jaw must be
moved back - distal occlusion. Grinding is carried out according to class 3
with a drop-shaped or flame-shaped bur, i.e., sharpen the tubercle, but do
not remove the tubercle itself. After that - remotherapy, fluoride varnish,
protective pastes.
19.
2 visitAfter 3-5 days to a week. Align the supercontacts on
the lower jaw in the central occlusion according to
class 1, do not remove the bumps, but grind to 45
degrees, increase the equator circumference. Then canine and incisors from the vestibular side. Hard
tissues can be removed along the cutting edge, in
height only in one case, if one tooth is clearly lower
than the other teeth. If the tooth is shortened, it will still
go into supercontact.
20.
3 visitAfter 10 days, check the upper teeth in the central occlusion
according to class 2.
21.
4 visitAfter 5-7 days, check the contacts in the central occlusion according to
the 3rd class.
22.
5 visitAfter 10 -14 all three classes are checked. To polish
hard tissues, always remotherapy.
23.
Neuromuscular dysfunctional syndromeEtiology. The cause of neuromuscular dysfunction are
psychogenic factors (stress, hysterical crises, grimaces).
Functional and organic changes in various parts of the
central and peripheral nervous systems, prosthetic errors
(premature contact on individual teeth). The most common
etiological factor is muscle spasm, incoordination of
muscle contractions.
Spasm of the lateral pterygoid muscle can lead to sharp
pain in the TMJ. Spasm of the masticatory muscle and the
temporal muscle lead to facial pain radiating to the joint,
since the nerve endings of the masticatory muscles enter
the joint. Compression of the trigger zone of the
masticatory muscle gives reflected pain in the joint.
24.
ClinicCommon symptoms are:
- muscle pain;
- headache;
- neuralgic pains;
- glossalgia.
25.
Typical symptoms for this pathology are: pain in themasticatory muscles, neuralgic arthrogenic pain that
occurs when there is a violation of the coordination of
muscle contractions, from atypical movements of the lower
jaw. When this happens, compression of individual
sections of the meniscus between the bone elements of the
joint, infringement of the posterior and posterolateral
sections of the articular bag, rich in nerve receptors. Pain
also arises from overstretching of the musculoligamentous apparatus. Pain in the joint can occur with
atypical movements of the heads of the lower jaw from
compression of the branch n. chorda thympani, n.
auriculotemporahs, from spasm of the lateral pterygoid
muscle.
26.
Another symptom is clicking in the joints. Withatypical movements and spasms of the lateral
pterygoid muscle, a strong connection between the
meniscus and the condyle is lost. The meniscus
becomes overly mobile and makes a clicking sound
when it is bent and straightened.
27.
Asynchronous contractions of pairedchewing muscles lead to jerky, zigzag
and circular movements of the lower jaw.
28.
X-ray pictureOn tomograms in the position of central occlusion,
the heads of the lower jaw are in the middle of the
articular fossae. Changes in the bone structure of the
articular surfaces are not observed. With the
maximum open mouth, the heads of the lower jaw are
at the top of the articular tubercles.
29.
30.
Treatment of neuromuscular dysfunctionalTMJ syndrome
is aimed at eliminating the cause that caused the
dysfunctional state, if it continues to act. After that,
treatment should be carried out according to a
certain scheme, which takes into account the nature
of the pathology, includes both general and local
treatment. In case of damage to the central nervous
system, treatment must be carried out in a complex
manner, together with a psychiatrist and a
neuropathologist
31.
Special dental treatment is aimed ateliminating traumatic moments, restoring the
synchronization of contraction of paired
masticatory muscles, strengthening the
musculoskeletal apparatus and reducing the
stretched joint capsule, normalizing the
occlusal-articulatory relationship of the jaws
and dentition. This is achieved through
myogymnastic exercises, selective grinding of
teeth, orthopedic, instrumental treatment,
drug physiotherapy and dental prosthetics.
32.
With sharp unilateral spasms of the lateral pterygoidmuscle, as a rule, the lower jaw is displaced in the
opposite direction
Treatment of patients should begin with
myogymnastic exercises.
33.
Methodology for performing myogymnastic exercises1. With vertical movements, the sick palm of the hand rests on the
chin, tends to move the jaw in the direction opposite to the
displacement.
2. With zigzag movements of the lower jaw, the patient covers it with
the palms of both hands and, holding it in the sagittal plane, makes
vertical movements.
3. With distal shifts of the lower jaw, the patient pushes the lower jaw
forward to the position of orthognathic or direct occlusion and,
holding it in a constructive occlusion, makes vertical movements.
4. With the habitual protrusion of the lower jaw forward at the moment
of opening the mouth, it is fixed by the chin in the distal position
during vertical movements.
Myogymnastics is prescribed 3 times a day until easy fatigue for 1, 2,
3 months.
34.
Patients with jerky and zigzag movements should be treatedwith a non-removable limiting splint Yu.A. Petrosov.
35.
Elimination of swelling, inflammation, pain, restoration of the range ofmotion of the temporomandibular joint is accelerated by the use of
physiotherapy.
36.
Occlusion-articulation syndromeEtiology. Etiological factors are: decreasing occlusion, distal shift of
the lower jaw, loss of chewing teeth, lateral shift of the lower jaw,
bite deformity, prosthetic errors, premature contact on any tubercle,
worn milk fangs, etc.
Point contact, an unusual excursion of the heads of the lower jaw
lead to wear and tear and destructive changes in the meniscus and
cartilaginous surfaces of the head of the lower jaw in the distal or
anterior section, depending on the nature of the pathological
movement.
37.
Costen syndrome (J.V. Costen, b. 1896, Americanotorhinolaryngologist)
- a combination of pathological changes in the
temporomandibular joint (clicking, crunching,
stiffness), hearing loss, feeling of ear
congestion, dull pain in the ear radiating to the
parietal and occipital region, pain and burning in
the tongue, dry mouth, dizziness and neuralgia
trigeminal nerve; observed with a deep bite and
the absence of many teeth, with pathological
abrasion of hard dental tissues, with deforming
arthrosis of the temporomandibular joint.
38.
According to Yu.A. Petrosov (1982), arthrogenic neuralgicpain often occurs as a result of spastic contraction of the
lateral pterygoid muscle, the upper bundles of which are
embedded in the meniscus. With a spasm of the muscle, a
sharp tension of the meniscus and posterior tendons
occurs, which fan-shapedly penetrates into the Glaser gap.
As a result of the tension of the meniscus n. chorda tympani
is infringed between the tendon and the bone edge of the
Glazer's fissure.
39.
Clinic. Patients complain of crunching, clicking, pain, displacement ofthe jaw, asymmetry of the face, partial blockage in the joint. Noise
symptoms are in the form of a scratching sound, the sound of
parchment. Clicking is noted with a slight opening of the mouth,
lateral movements of the lower jaw during the act of chewing, with a
wide opening of the mouth and with the closing of the jaws. The
latter occurs with a decreasing occlusion and a deep traumatic
occlusion.
40.
The symptom of displacement of the lower jaw to the side occurswith uneven increased abrasion of teeth, with errors during
prosthetics. The distal shift of the lower jaw occurs in the
absence of distal support and is accompanied by clicking and
pain in the joint at the time of closing the jaws. When squeezing
the region of the bilaminar zone, rich in blood vessels, there may
be congestion, which leads to an increase in intratympanic
pressure. Similar is observed when squeezing the Eustachian
tube. With atypical movements of the condyle, the meniscus, the
posterior and lateral sections of the articular capsule, rich in
nerve receptors, can be compressed.
41.
There is a close relationship between neuromuscular andocclusal-articulation dysfunctional syndrome. They are
interrelated and mutually condition each other.
42.
X-ray picture. On tomograms, the contours of the articular surfacesare not changed, mostly even, smooth, rounded.
In a number of patients, erasing of individual sections, obliqueness of
the posterior edge of the articular tubercle, with a deep and
decreasing bite, with closed dentition, the posterior and upper joint
spaces are narrowed. The asymmetric position of the condyles is
noted mainly in patients with a lateral shift of the lower jaw. With the
mouth open to the maximum, the heads of the lower jaw reach the
top of the articular tubercles.
43.
Treatment is aimed at eliminating the cause of the disease, levelingthe occlusion. With a decreasing bite, a bite plate is used; with a
distal shift of the lower jaw - myogymnastics, a palatine plate with an
inclined plane in the frontal section, and with periodontitis - a plastic
mouthguard made in a constructive bite. With a combination of
malocclusion and TMJ pathology - treatment of both pathologies.
When combined with neuromuscular syndrome - non-removable
limiting splint. With lateroposition of the lower jaw - myogymnastics
and splints with a lateral inclined plane.
44.
Modified removable dental splint for the lower jaw with aninclined plane.
45.
To relax the chewing muscles, patients are selectivelyprescribed medication. Patients are under constant
outpatient monitoring. To establish the lower jaw in
the mid-sagittal position (with a reverse overlap of the
chewing teeth), a base plate with an oral inclined
plane and with a segmental cut is used.
46.
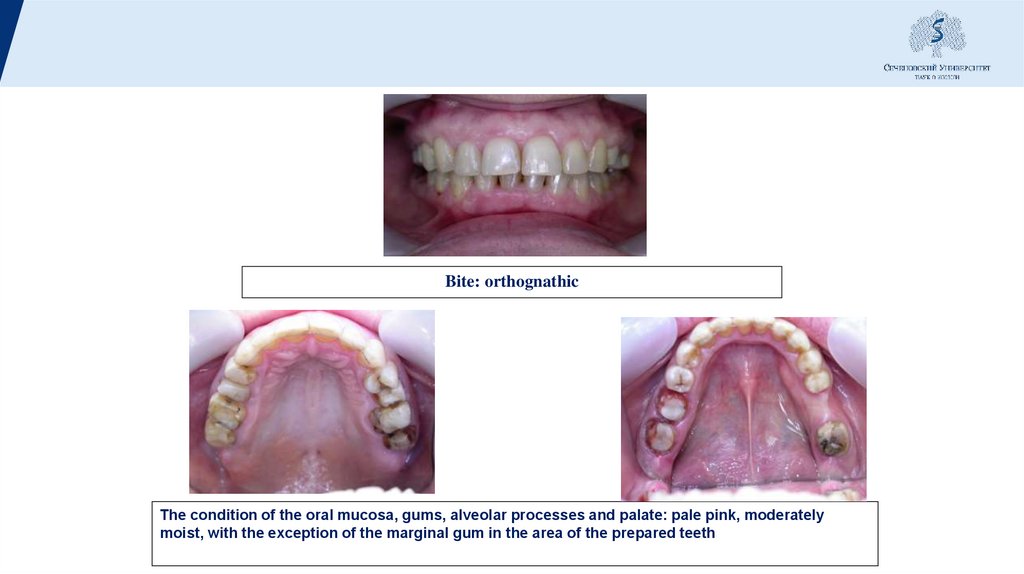
Bite: orthognathicThe condition of the oral mucosa, gums, alveolar processes and palate: pale pink, moderately
moist, with the exception of the marginal gum in the area of the prepared teeth
47.
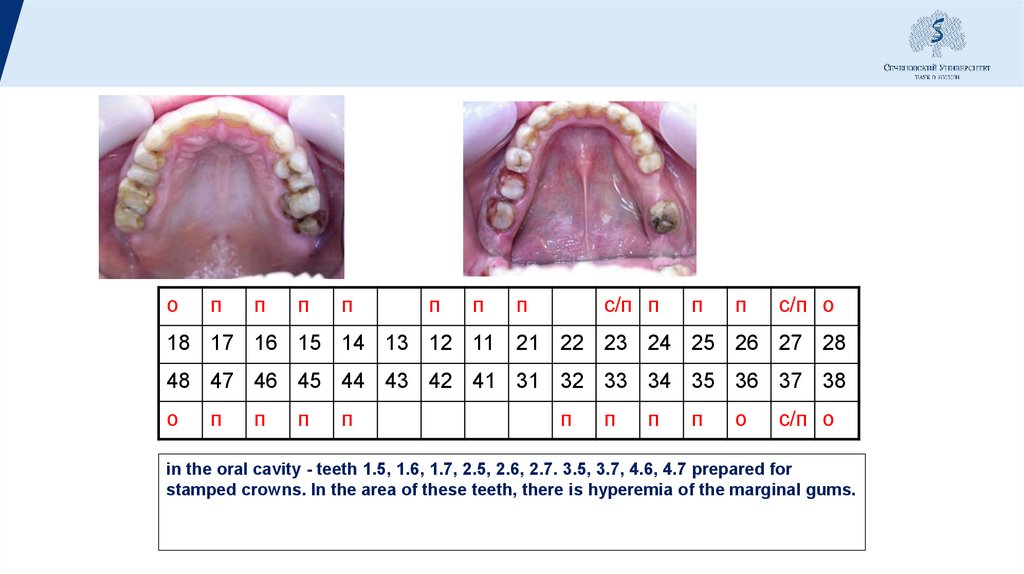
оп
п
п
п
п
п
п
с/п п
п
п
с/п о
18 17 16 15 14 13 12 11 21 22 23 24 25 26 27 28
48 47 46 45 44 43 42 41 31 32 33 34 35 36 37 38
о
п
п
п
п
п
п
п
п
о
с/п о
in the oral cavity - teeth 1.5, 1.6, 1.7, 2.5, 2.6, 2.7. 3.5, 3.7, 4.6, 4.7 prepared for
stamped crowns. In the area of these teeth, there is hyperemia of the marginal gums.
48.
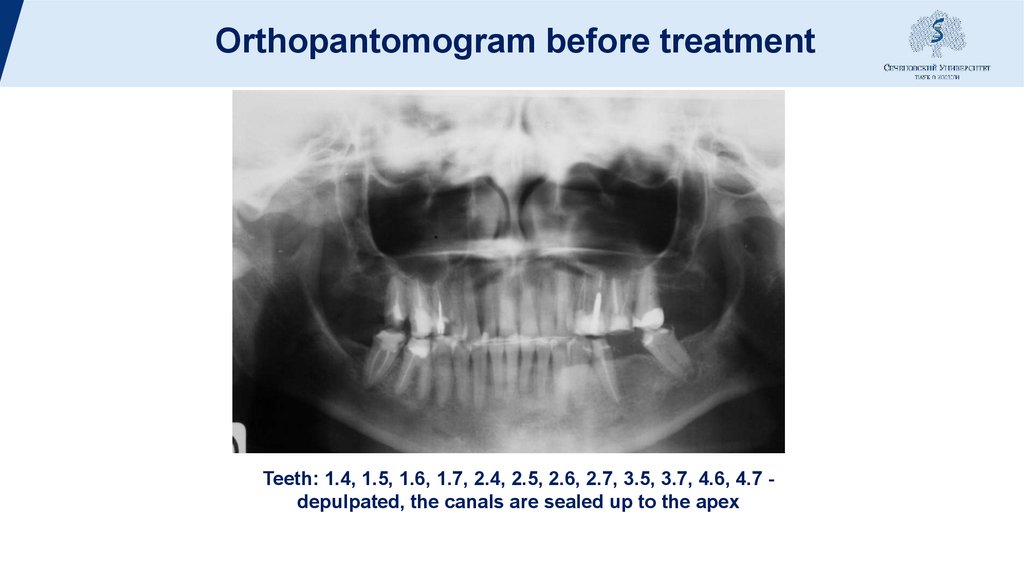
Orthopantomogram before treatmentTeeth: 1.4, 1.5, 1.6, 1.7, 2.4, 2.5, 2.6, 2.7, 3.5, 3.7, 4.6, 4.7 depulpated, the canals are sealed up to the apex
49.
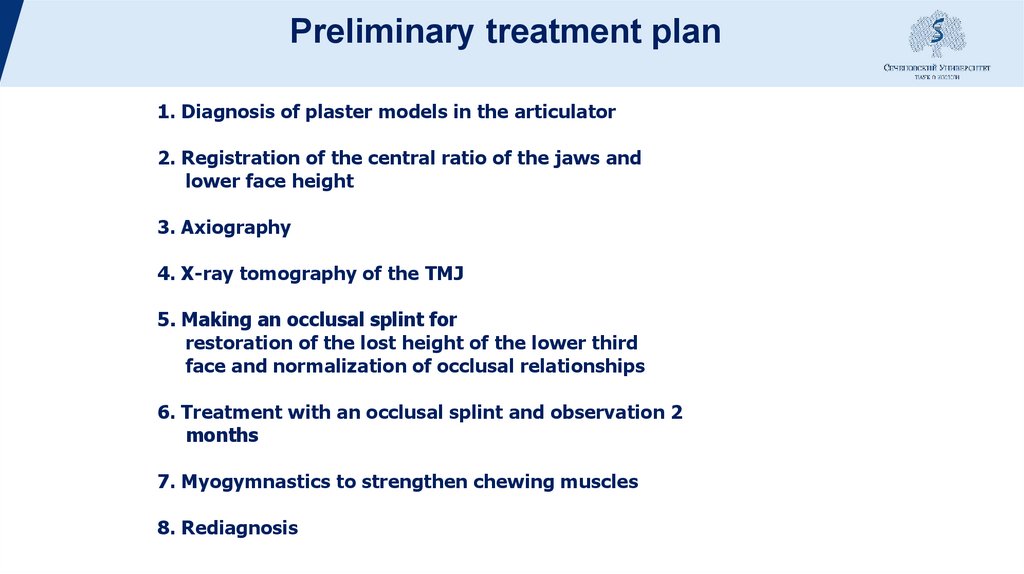
Preliminary treatment plan1. Diagnosis of plaster models in the articulator
2. Registration of the central ratio of the jaws and
lower face height
3. Axiography
4. X-ray tomography of the TMJ
5. Making an occlusal splint for
restoration of the lost height of the lower third
face and normalization of occlusal relationships
6. Treatment with an occlusal splint and observation 2
months
7. Myogymnastics to strengthen chewing muscles
8. Rediagnosis
50.
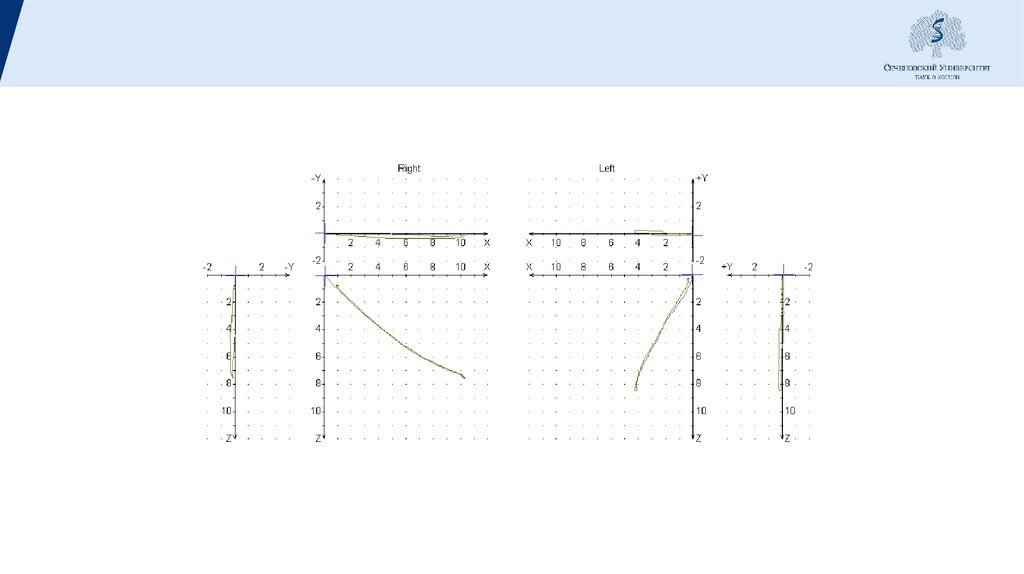
Аксиограмма при открывании рта51.
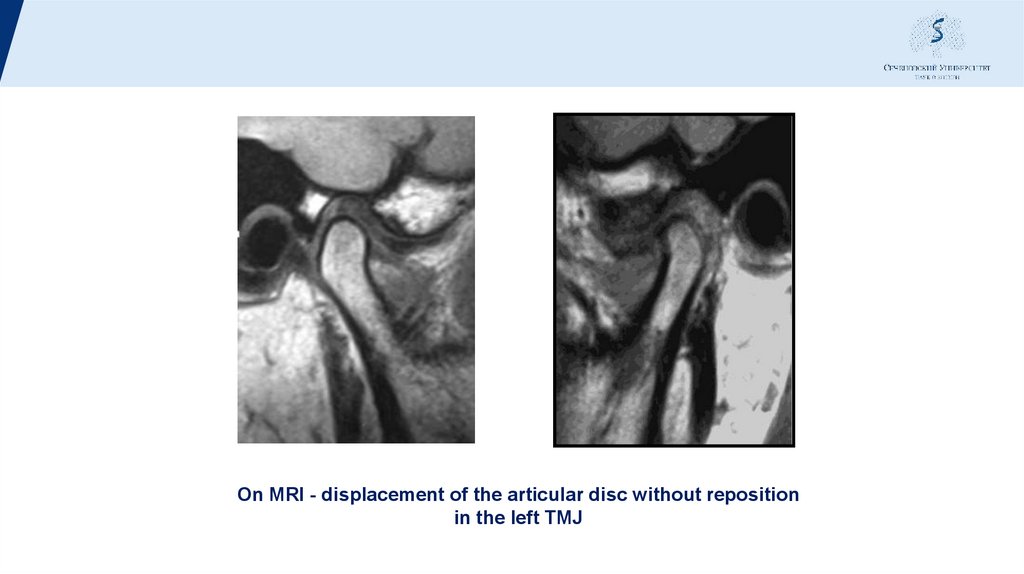
On MRI - displacement of the articular disc without repositionin the left TMJ
52.
DiagnosisPartial secondary adentia on the lower
jaws, class III according to Kennedy
Generalized periodontitis
mild to moderate severity.
Displacement of the articular disc without reposition
in the left TMJ.
Violation of the occlusion of the dentition.
53.
Treatment plan1. Professional oral hygiene and its control
2. Diagnosis of plaster models in the articulator
3. Carrying out wax modeling of the chewing group
teeth in the restored height of the lower third of the face
4. Production of temporary plastic crowns, taking into account
wax modeling
5. Restoration of pulpless teeth with
stump inlays and stumps
6. Production of metal-ceramic crowns and bridges
prosthesis on the chewing group of teeth. wax
modeling of the frontal group of teeth
Restoration of the frontal group of teeth using silicone keys using a composite material
8. Dynamic monitoring of structures and the state of composite restorations
54.
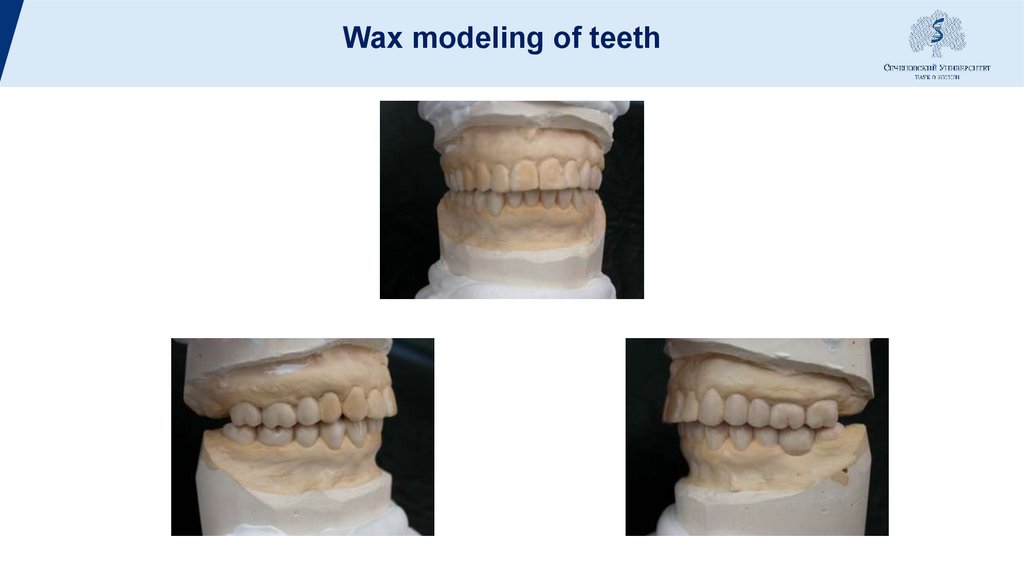
Wax modeling of teeth55.
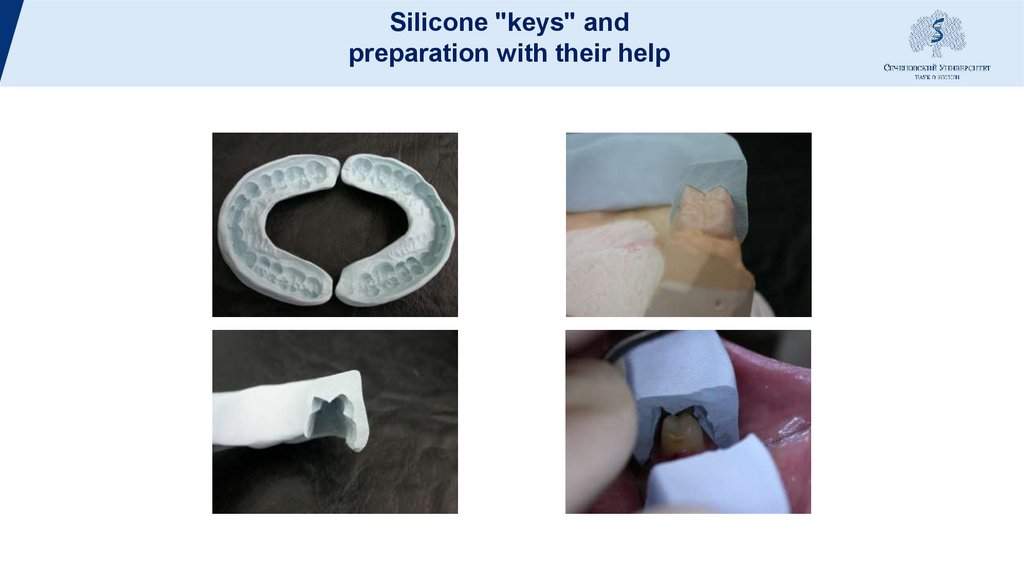
Silicone "keys" andpreparation with their help
56.
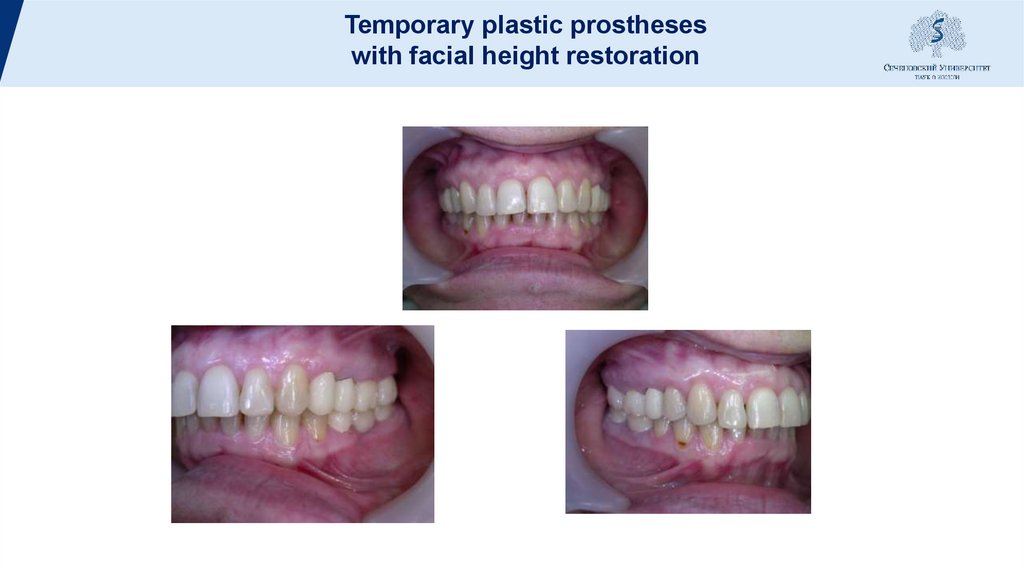
Temporary plastic prostheseswith facial height restoration
57.
Movements n/h with temporary structures58.
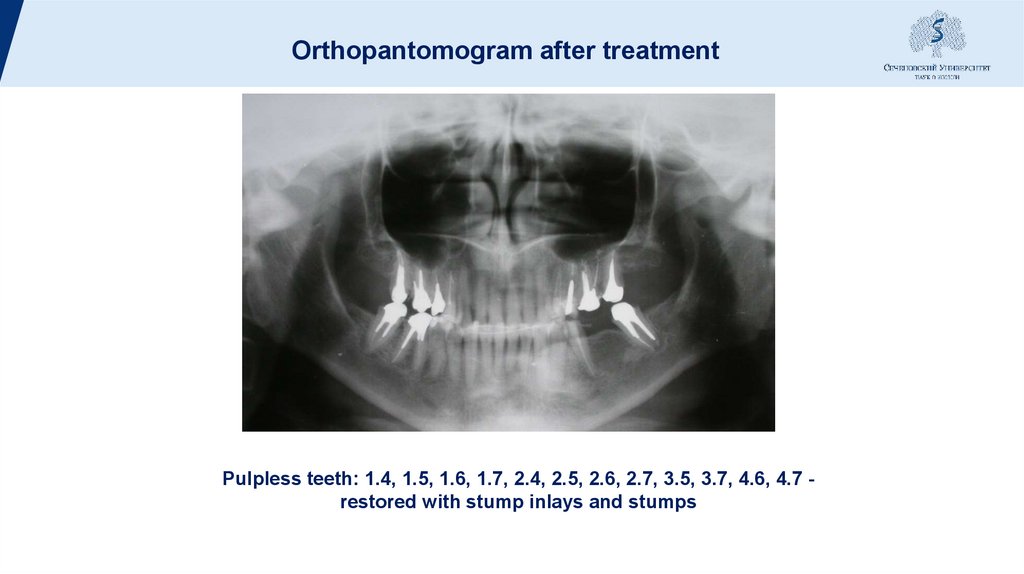
Orthopantomogram after treatmentPulpless teeth: 1.4, 1.5, 1.6, 1.7, 2.4, 2.5, 2.6, 2.7, 3.5, 3.7, 4.6, 4.7 restored with stump inlays and stumps
59.
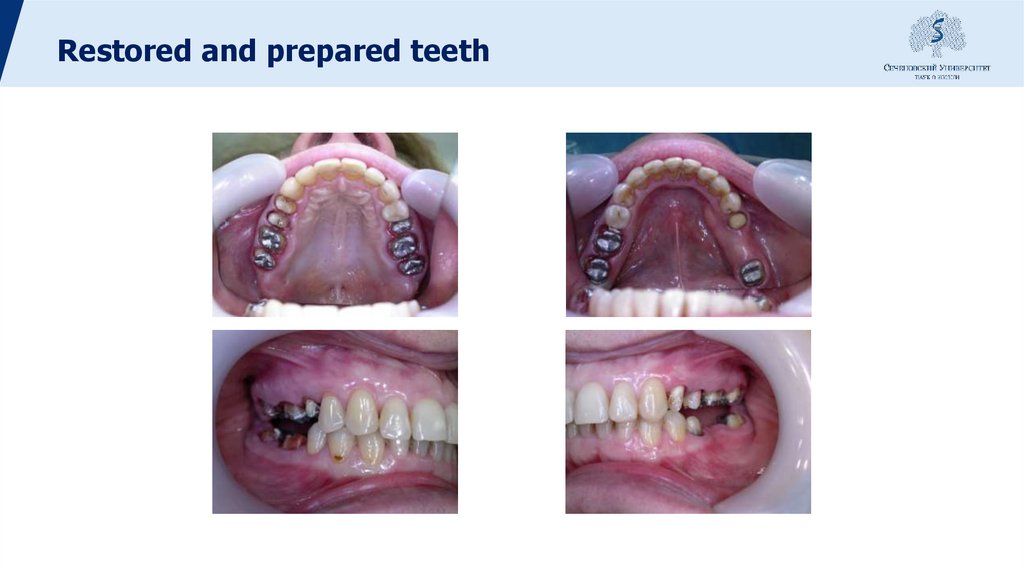
Restored and prepared teeth60.
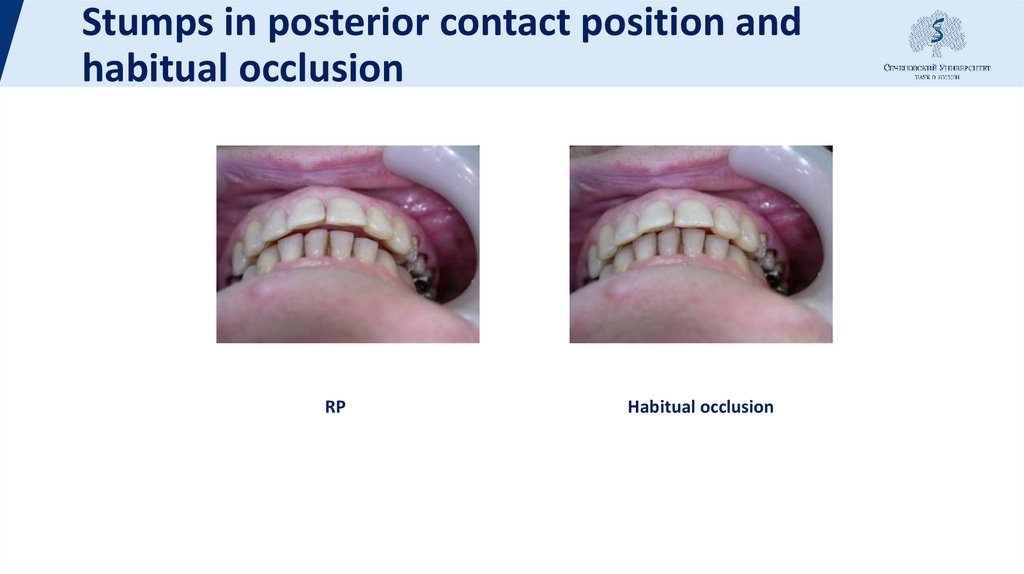
Stumps in posterior contact position andhabitual occlusion
RP
Habitual occlusion
61.
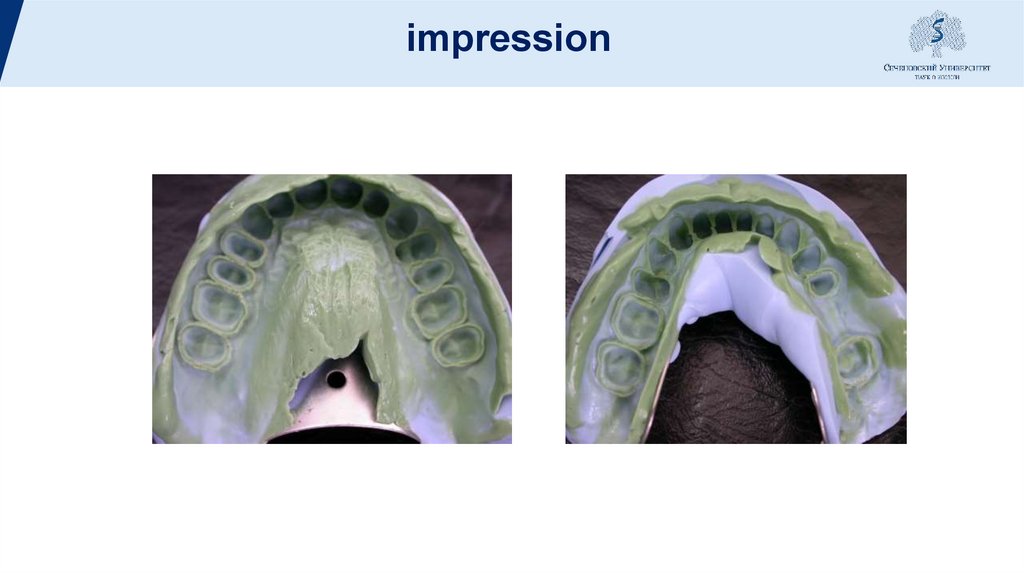
impression62.
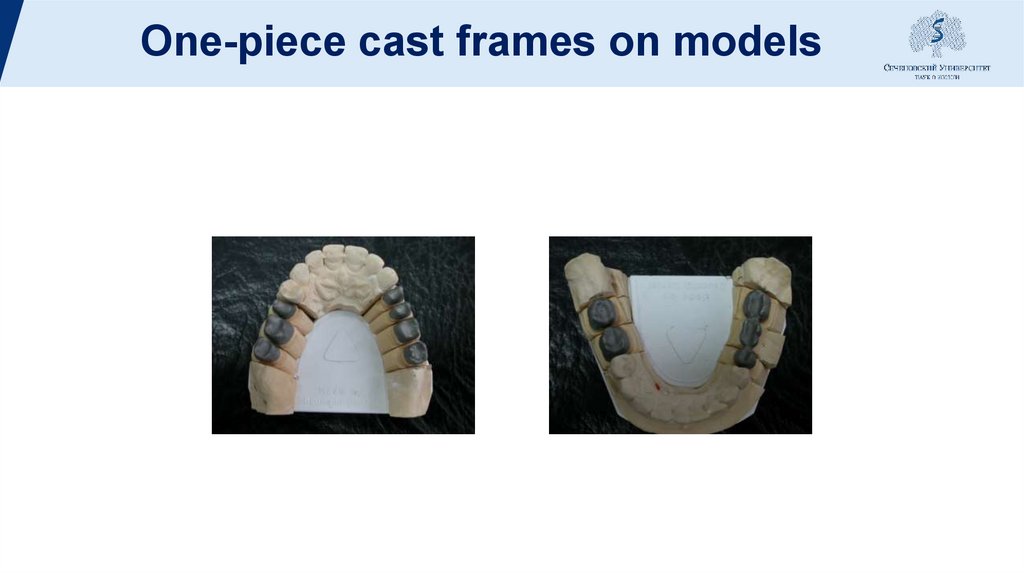
One-piece cast frames on models63.
Registration on wireframes64.
Finished metal-ceramiccrowns and bridges
65.
Silicone keys for restoration66.
Finished metal-ceramiccrowns and bridges
in the oral cavity with restored
anterior teeth
67.
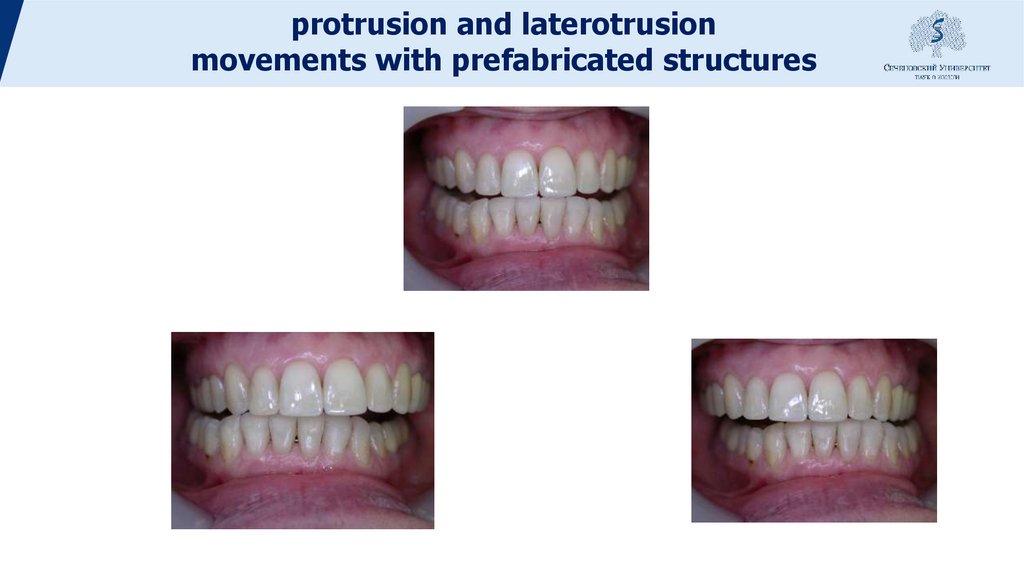
protrusion and laterotrusionmovements with prefabricated structures








 medicine
medicine