Similar presentations:
Traumatic rhabdomyolysis
1.
TRAUMATICRHABDOMYOLYSIS
SAVING A LIFE VS. SAVING A LIMB
O.Polivoda , D.Chabanenko, I.Sherbina
Odessa
2022
2.
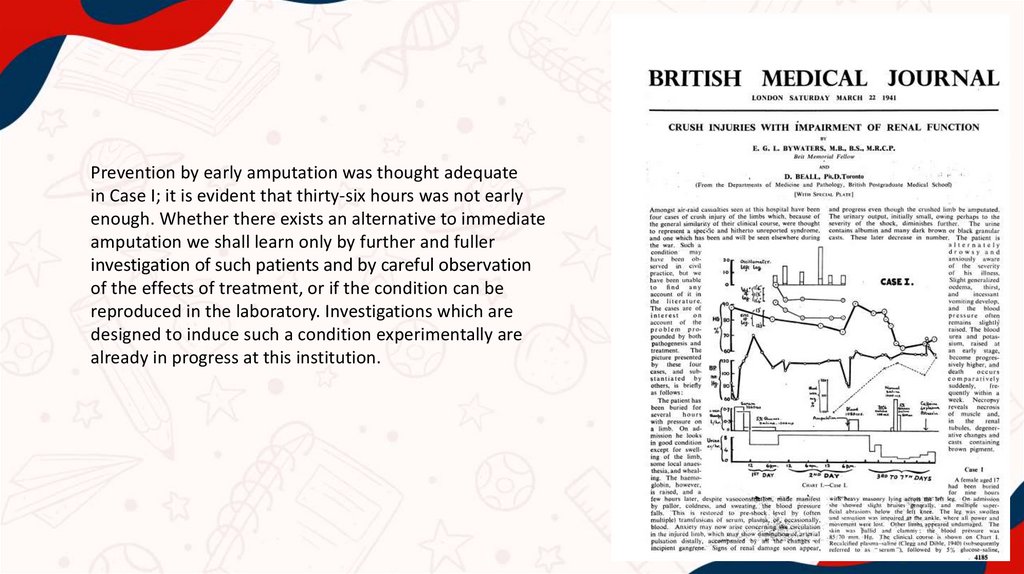
Prevention by early amputation was thought adequatein Case I; it is evident that thirty-six hours was not early
enough. Whether there exists an alternative to immediate
amputation we shall learn only by further and fuller
investigation of such patients and by careful observation
of the effects of treatment, or if the condition can be
reproduced in the laboratory. Investigations which are
designed to induce such a condition experimentally are
already in progress at this institution.
3.
4.
5.
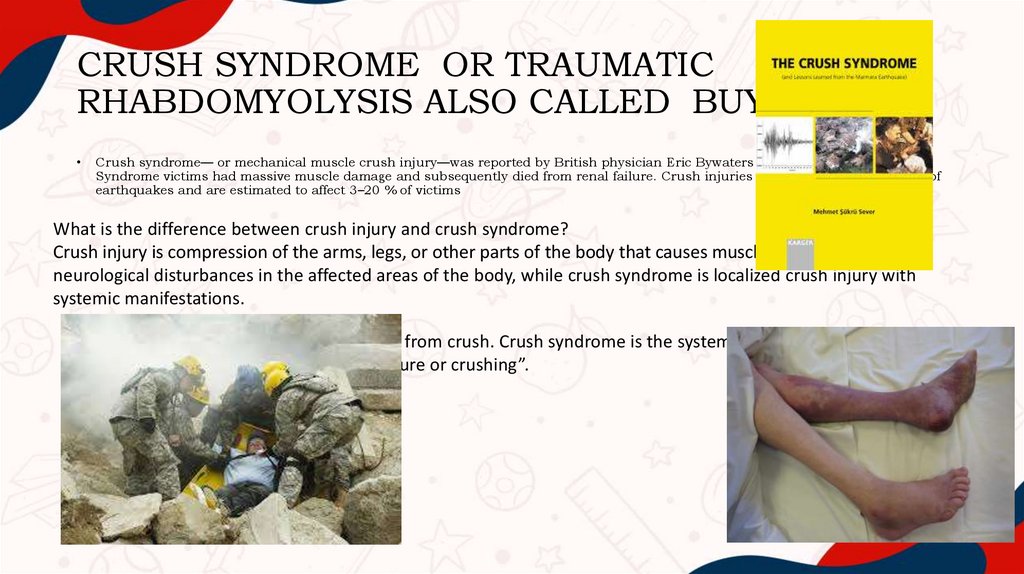
CRUSH SYNDROME OR TRAUMATICRHABDOMYOLYSIS ALSO CALLED BUYWATERS
Сrush syndrome— or mechanical muscle crush injury—was reported by British physician Eric Bywaters during the London Blitz .
Syndrome victims had massive muscle damage and subsequently died from renal failure. Crush injuries are common consequences of
earthquakes and are estimated to affect 3–20 % of victims
What is the difference between crush injury and crush syndrome?
Crush injury is compression of the arms, legs, or other parts of the body that causes muscle swelling and/or
neurological disturbances in the affected areas of the body, while crush syndrome is localized crush injury with
systemic manifestations.
“A crush injury is a direct injury resulting from crush. Crush syndrome is the systemic manifestation of
muscle cell damage resulting from pressure or crushing”.
6.
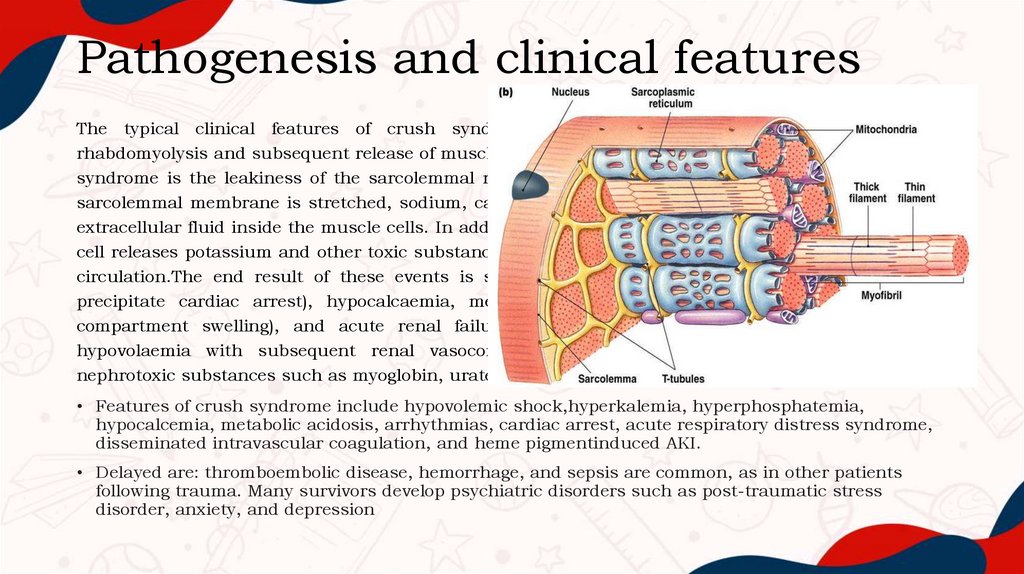
Pathogenesis and clinical featuresThe typical clinical features of crush syndrome are predominantly a result of traumatic
rhabdomyolysis and subsequent release of muscle cell contents. The mechanism behind this in crush
syndrome is the leakiness of the sarcolemmal membrane caused by pressure or stretching. As the
sarcolemmal membrane is stretched, sodium, calcium and water leak into the sarcoplasm, trapping
extracellular fluid inside the muscle cells. In addition to the influx of these elements into the cell, the
cell releases potassium and other toxic substances such as myoglobin, phosphate and urate into the
circulation.The end result of these events is shock (discussed below), hyperkalemia (which may
precipitate cardiac arrest), hypocalcaemia, metabolic acidosis, compartment syndrome (due to
compartment swelling), and acute renal failure (ARF). The ARF is due to a combination of
hypovolaemia with subsequent renal vasoconstriction, metabolic acidosis and the insult of
nephrotoxic substances such as myoglobin, urate and phosphate.
• Features of crush syndrome include hypovolemic shock,hyperkalemia, hyperphosphatemia,
hypocalcemia, metabolic acidosis, arrhythmias, cardiac arrest, acute respiratory distress syndrome,
disseminated intravascular coagulation, and heme pigmentinduced AKI.
• Delayed are: thromboembolic disease, hemorrhage, and sepsis are common, as in other patients
following trauma. Many survivors develop psychiatric disorders such as post-traumatic stress
disorder, anxiety, and depression
7.
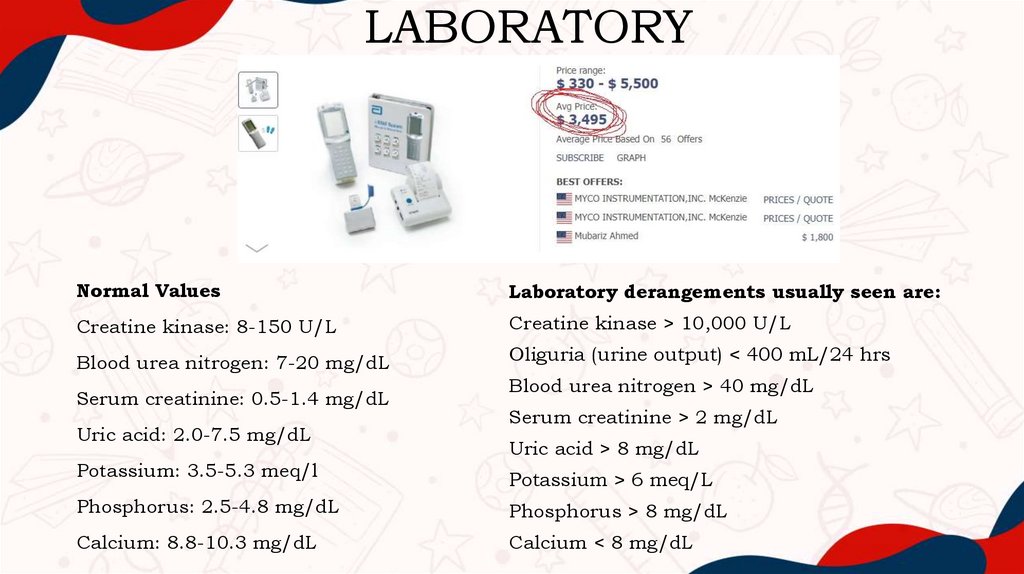
LABORATORYNormal Values
Laboratory derangements usually seen are:
Creatine kinase: 8-150 U/L
Creatine kinase > 10,000 U/L
Blood urea nitrogen: 7-20 mg/dL
Oliguria (urine output) < 400 mL/24 hrs
Serum creatinine: 0.5-1.4 mg/dL
Uric acid: 2.0-7.5 mg/dL
Potassium: 3.5-5.3 meq/l
Blood urea nitrogen > 40 mg/dL
Serum creatinine > 2 mg/dL
Uric acid > 8 mg/dL
Potassium > 6 meq/L
Phosphorus: 2.5-4.8 mg/dL
Phosphorus > 8 mg/dL
Calcium: 8.8-10.3 mg/dL
Calcium < 8 mg/dL
8.
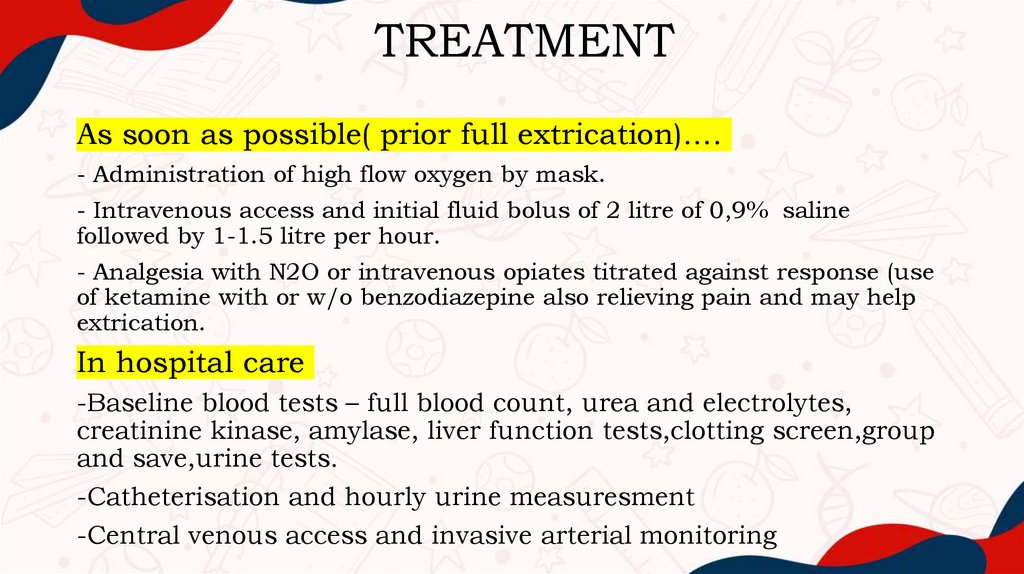
TREATMENTAs soon as possible( prior full extrication)….
- Administration of high flow oxygen by mask.
- Intravenous access and initial fluid bolus of 2 litre of 0,9% saline
followed by 1-1.5 litre per hour.
- Analgesia with N2O or intravenous opiates titrated against response (use
of ketamine with or w/o benzodiazepine also relieving pain and may help
extrication.
In hospital care
-Baseline blood tests – full blood count, urea and electrolytes,
creatinine kinase, amylase, liver function tests,clotting screen,group
and save,urine tests.
-Catheterisation and hourly urine measuresment
-Central venous access and invasive arterial monitoring
9.
DIALYSIS IN CRUSH INJURY• The timing of renal replacement therapy in AKI is controversial.
Compared with AKI by other causes, life-threatening complications
such as acidosis, hyperkalemia,or fluid overload are more frequent in
crush-related AKI, which may necessitate earlier initiation and more
frequent dialysis.
10.
11.
The use of solute-alkaline diuresis• It is recommended that urine pH is measured, and kept above 6.5 by adding 50mmol aliquots
of bicarbonate (50ml 8.4% sodium bicarbonate) to the intravenous fluid regime. Solute diuresis
is affected by administering mannitol at a dose of 1-2g/kg over the first four hours as a 20%
solution, and further mannitol should be given to maintain a urine output of at least 8 litres
per day (300mls per hour). Fluid requirements are high, usually of the order of 12 litres per
day, due to the sequestration of fluid in muscle tissue. Fluid should be given at approximately
500 mls/hour, but regular review of clinical parameters such as central venous pressure and
urine output should dictate exact amounts of fluid given. The maximum daily dose of mannitol
is 200g, and it should not be given to patients who are in established anuria.
• Acetazolamide for preventing metabolic alkalosis
Hyperbaric oxygen therapy is controversial but possible
12.
Arango-Granados MC, Mendoza DFC, Cadavid AES, Mar´ın AFG,Amputation in crush syndrome: A case report, International Journal of Surgery
Case Reports(2020), doi: https://doi.org/10.1016/j.ijscr.2020.05.087
It is known that xanthine dehydrogenase, is proteolytically cleaved to
xanthine oxidase during the ischaemic stage of muscle injury. Odeh’s ‘oxygen
paradox’ theory proposes that reperfusion of ischaemic tissue then provides
oxygen as a substrate for xanthine oxidase and other enzymes to produce
hydroxyl free-radicals (Odeh, 1991a). These reactive oxygen metabolites directly
damage muscle cell membranes by lipid peroxidation (Linas et al., 1990). Freeradicals initiate a chain reaction of further free-radical production explaining the
rapid propagation of myocyte death, and the subsequent damage to other body
organs…
…………29-year-old patient who was trapped for 50 hours under a 40-meter
landslide that fell over his lower body
…….. By that time (24 h after admission), the left lower extremity was distally
cold and cyanotic, so the possibility of disarticulating the affected limb was
discussed. Above-knee amputation was performed.
Two hours after
amputation,vasopressin and norepinephrine were reduced by 50% and 90% of
the maximum dose received, respectively, until the complete withdrawal of
vasopressor support was achieved.
13.
Ning Li, Xinyue Wang, Pengtao Wang, Haojun Fan, Shike Hou & YanhuaGong (2020) Emerging medical therapies in crush syndrome – progress
report from basic sciences and potential future avenues, Renal Failure,
42:1, 656-666, DOI: 10.1080/0886022X.2020.1792928
Most medical therapies highlight the symptoms of circulatory shock,
kidney failure, and arrhythmias in patients and focus on early fluid
resuscitation, forced diuresis and renal replacement therapy (RRT) which
includes dialysis (hemodialysis or peritoneal dialysis), haemofiltration,
haemodiafiltration and kidney transplantation. For renal replacement therapy,
continuous venovenous haemofiltration (CVVHF) is primarily used to remove
myoglobin until the patient’s kidney function returns or hemodialysis can be
initiated.
Studies by Gois et al. showed that allopurinol treatment can reduce
renal dysfunction by reducing oxidative stress (systemic, kidney
and
muscle), inhibiting apoptosis, reducing inflammatory cell infiltration, and
increasing cell proliferation in rhabdomyolysis-related AKI rat model/
14.
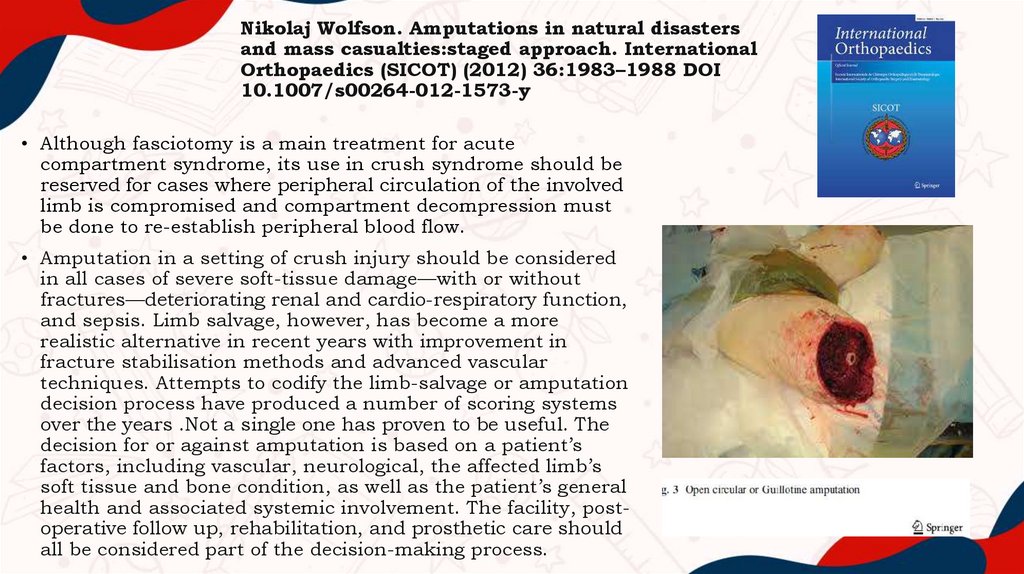
Nikolaj Wolfson. Amputations in natural disastersand mass casualties:staged approach. International
Orthopaedics (SICOT) (2012) 36:1983–1988 DOI
10.1007/s00264-012-1573-y
• Although fasciotomy is a main treatment for acute
compartment syndrome, its use in crush syndrome should be
reserved for cases where peripheral circulation of the involved
limb is compromised and compartment decompression must
be done to re-establish peripheral blood flow.
• Amputation in a setting of crush injury should be considered
in all cases of severe soft-tissue damage—with or without
fractures—deteriorating renal and cardio-respiratory function,
and sepsis. Limb salvage, however, has become a more
realistic alternative in recent years with improvement in
fracture stabilisation methods and advanced vascular
techniques. Attempts to codify the limb-salvage or amputation
decision process have produced a number of scoring systems
over the years .Not a single one has proven to be useful. The
decision for or against amputation is based on a patient’s
factors, including vascular, neurological, the affected limb’s
soft tissue and bone condition, as well as the patient’s general
health and associated systemic involvement. The facility, postoperative follow up, rehabilitation, and prosthetic care should
all be considered part of the decision-making process.
15.
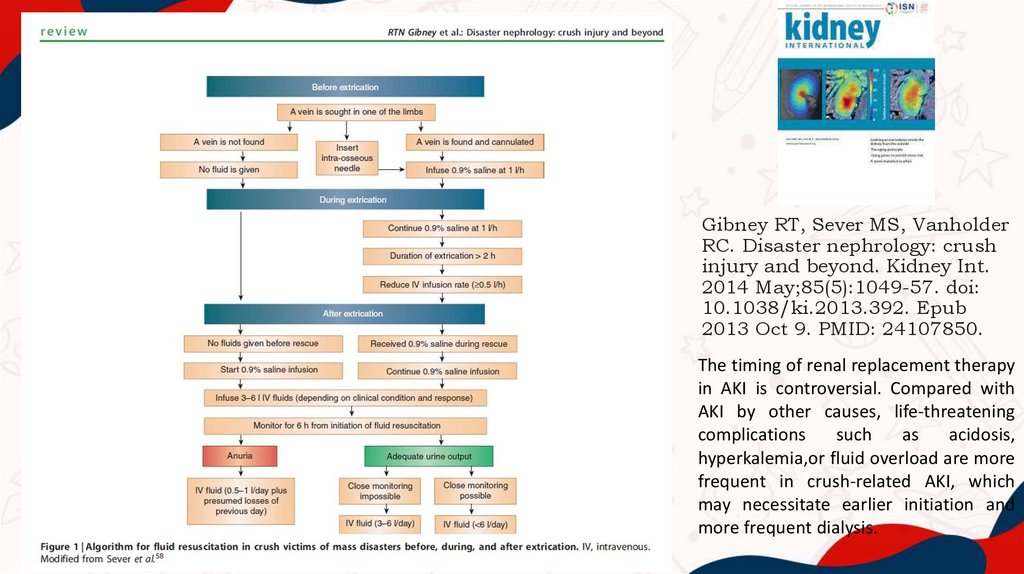
Gibney RT, Sever MS, VanholderRC. Disaster nephrology: crush
injury and beyond. Kidney Int.
2014 May;85(5):1049-57. doi:
10.1038/ki.2013.392. Epub
2013 Oct 9. PMID: 24107850.
The timing of renal replacement therapy
in AKI is controversial. Compared with
AKI by other causes, life-threatening
complications
such
as
acidosis,
hyperkalemia,or fluid overload are more
frequent in crush-related AKI, which
may necessitate earlier initiation and
more frequent dialysis.
16.
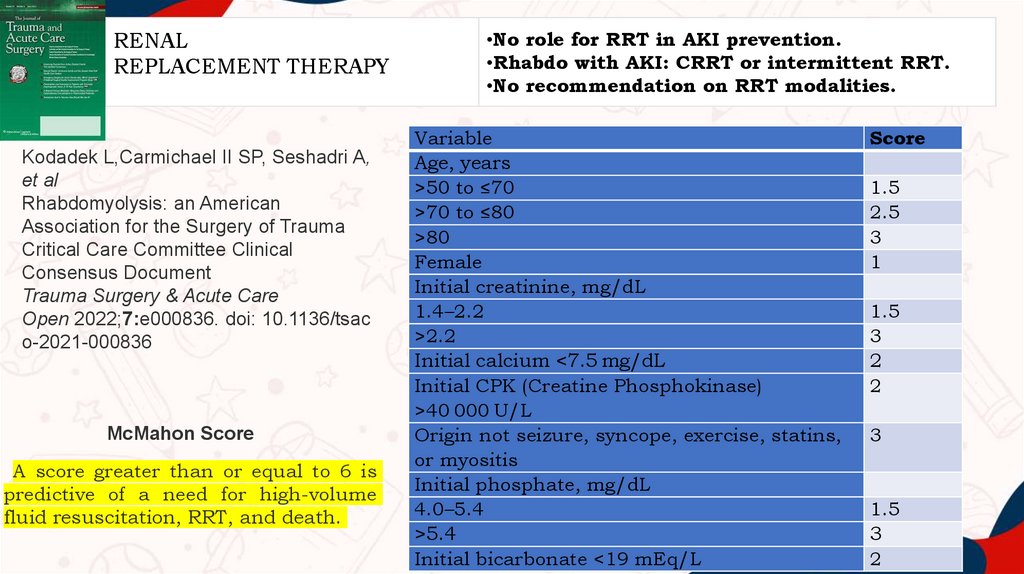
RENALREPLACEMENT THERAPY
Kodadek L,Carmichael II SP, Seshadri A,
et al
Rhabdomyolysis: an American
Association for the Surgery of Trauma
Critical Care Committee Clinical
Consensus Document
Trauma Surgery & Acute Care
Open 2022;7:e000836. doi: 10.1136/tsac
o-2021-000836
McMahon Score
A score greater than or equal to 6 is
predictive of a need for high-volume
fluid resuscitation, RRT, and death.
•No role for RRT in AKI prevention.
•Rhabdo with AKI: CRRT or intermittent RRT.
•No recommendation on RRT modalities.
Variable
Age, years
>50 to ≤70
>70 to ≤80
>80
Female
Initial creatinine, mg/dL
1.4–2.2
>2.2
Initial calcium <7.5 mg/dL
Initial CPK (Creatine Phosphokinase)
>40 000 U/L
Origin not seizure, syncope, exercise, statins,
or myositis
Initial phosphate, mg/dL
4.0–5.4
>5.4
Initial bicarbonate <19 mEq/L
Score
1.5
2.5
3
1
1.5
3
2
2
3
1.5
3
2
17.
Greaves I, Porter KM. Consensus statement on crush injuryand crush syndrome. Accid Emerg Nurs. 2004 Jan;12(1):47-52.
doi: 10.1016/j.aaen.2003.05.001. PMID: 14700572.
Tourniquets.The use of tourniquets has a theoretical role in the management of these patients. If
the release into thecirculation of the contents of crushed muscle cells can be avoided, possibly
with the use of a tourniquet, itmay be of benefit. However, there is currently no available evidence
to support this.
Consensus view. The use of tourniquets should be reserved for otherwise uncontrollable life
threatening haemorrhage. There is no evidence at the moment to support the use of tourniquets
in the prevention of reperfusion injury following extrication, or in the prevention of washing of the
products of rhabdomyolysis into the circulation.
Amputation. Another theoretically advantageous measure is amputation of a crushed limb to
prevent crush syndrome.
Consensus view. There is no evidence to support the use of amputation as a prophylactic
measure to prevent crush syndrome. Reports from the literature suggest that even severely
crushed limbs can recover to full function. If the limb is literally hanging on by a thread, or if the
patient’s survival is in danger due to entrapment by a limb, amputation should be considered
and appropriate expert advice sought.
18.
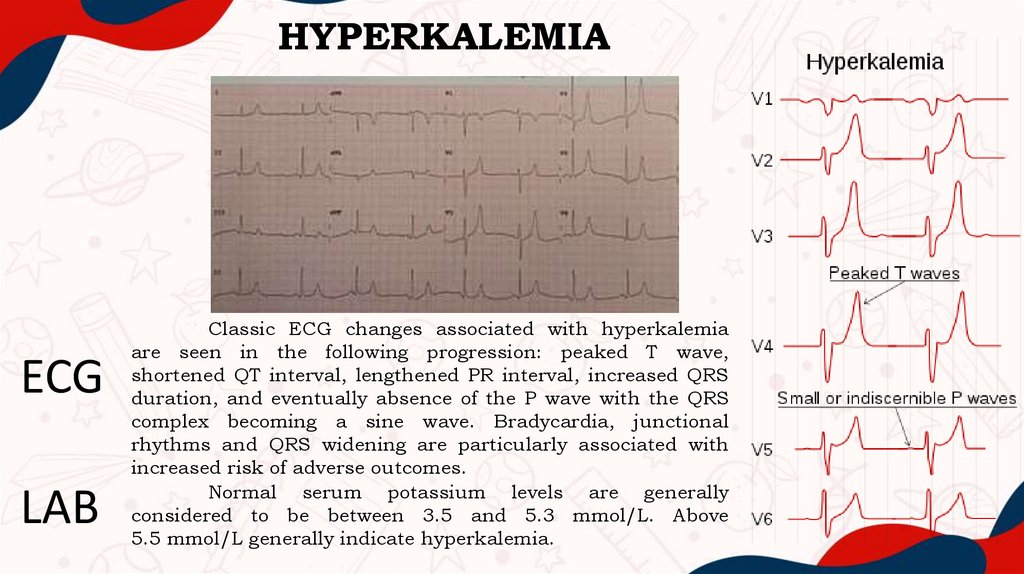
HYPERKALEMIAECG
LAB
Classic ECG changes associated with hyperkalemia
are seen in the following progression: peaked T wave,
shortened QT interval, lengthened PR interval, increased QRS
duration, and eventually absence of the P wave with the QRS
complex becoming a sine wave. Bradycardia, junctional
rhythms and QRS widening are particularly associated with
increased risk of adverse outcomes.
Normal serum potassium levels are generally
considered to be between 3.5 and 5.3 mmol/L. Above
5.5 mmol/L generally indicate hyperkalemia.
19.
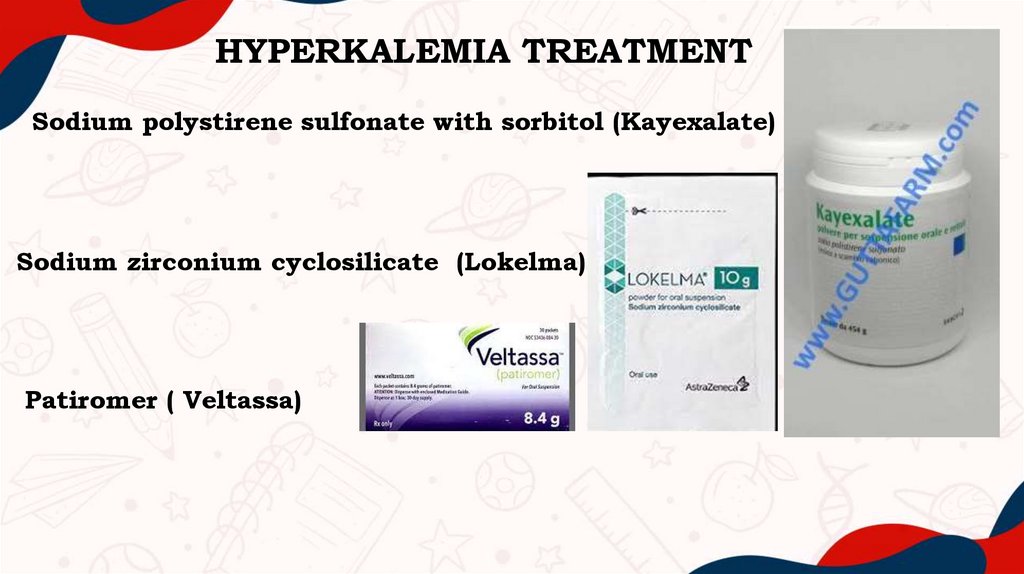
HYPERKALEMIA TREATMENTSodium polystirene sulfonate with sorbitol (Kayexalate)
Sodium zirconium cyclosilicate (Lokelma)
Patiromer ( Veltassa)
20.
10 hours before extrication. No fractures.Traumatic hip dislocation. Death in situ.
21.
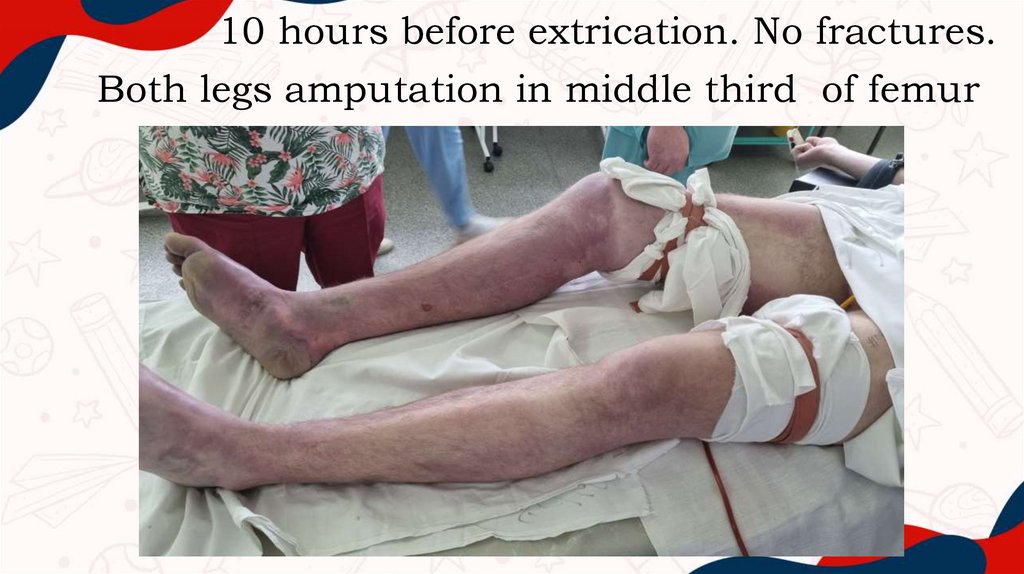
10 hours before extrication. No fractures.Both legs amputation in middle third of femur
22.
23.
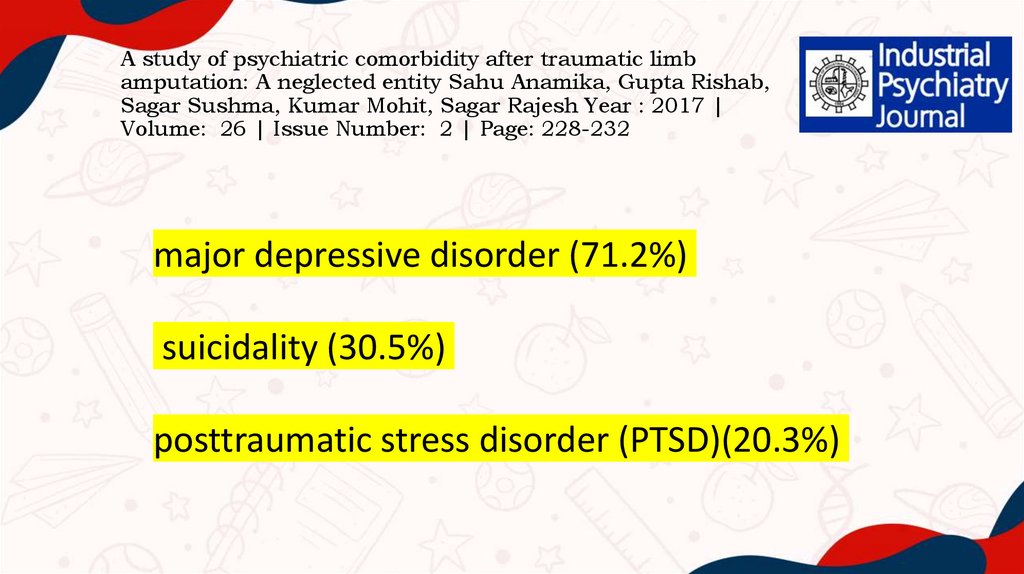
A study of psychiatric comorbidity after traumatic limbamputation: A neglected entity Sahu Anamika, Gupta Rishab,
Sagar Sushma, Kumar Mohit, Sagar Rajesh Year : 2017 |
Volume: 26 | Issue Number: 2 | Page: 228-232
major depressive disorder (71.2%)
suicidality (30.5%)
posttraumatic stress disorder (PTSD)(20.3%)




 medicine
medicine