Similar presentations:
Pathophysiology of renal failure
1.
Pathophysiology of renalfailure
2.
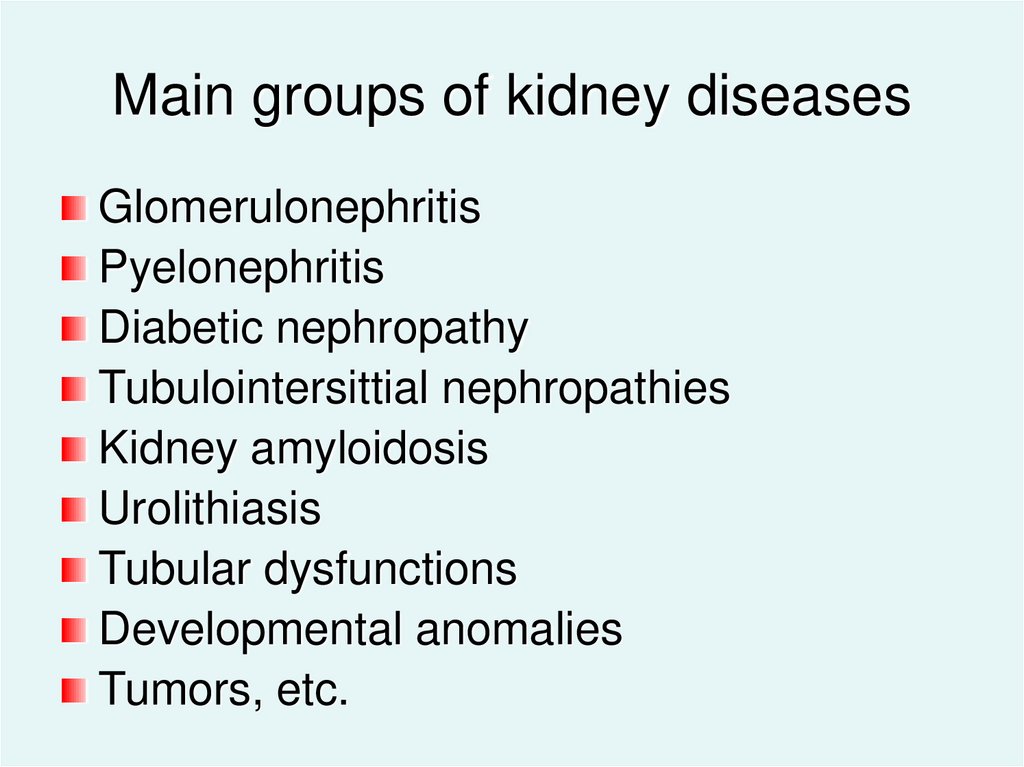
Main groups of kidney diseasesGlomerulonephritis
Pyelonephritis
Diabetic nephropathy
Tubulointersittial nephropathies
Kidney amyloidosis
Urolithiasis
Tubular dysfunctions
Developmental anomalies
Tumors, etc.
3.
Glomerulonephritis4.
GlomerulonephritisA group of diseases characterized by
inflammatory changes, mainly in the
glomeruli of the kidneys, manifested by
changes in urine tests and decreased
renal function
They are divided into primary (idiopathic)
and secondary (for systemic diseases).
5.
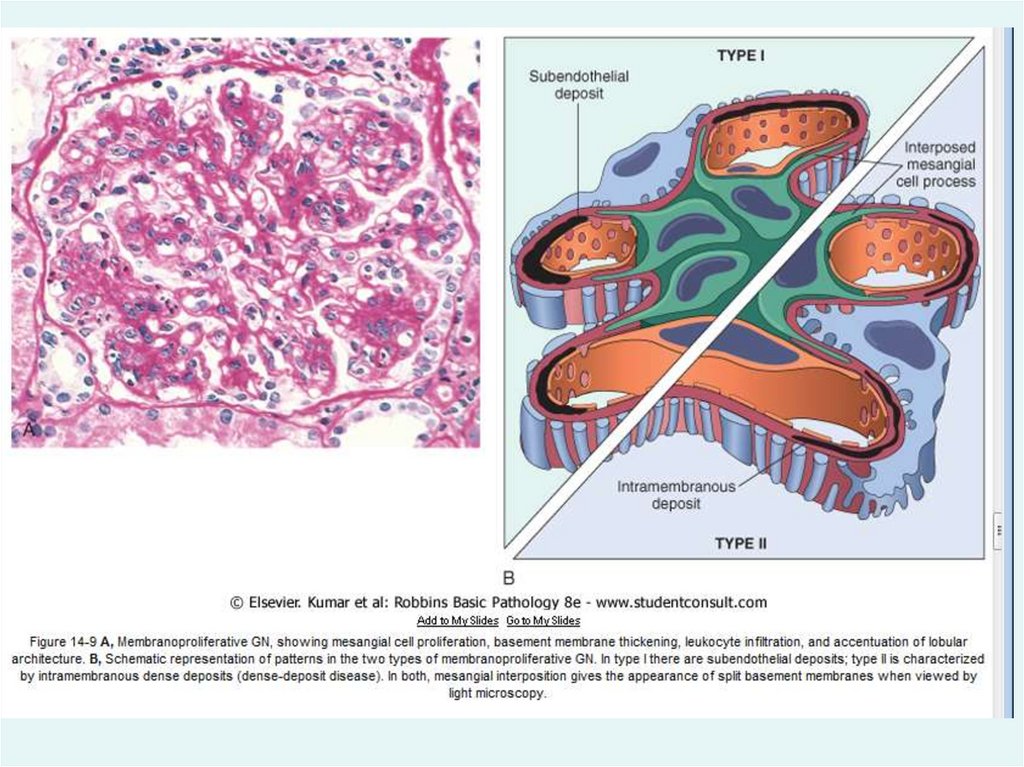
Classification of GNProliferative forms (mesangioproliferative,
diffuse proliferative, extracapillary) – nephritic
syndrome: proteinuria, hematuria, leucocyteuria
Non-proliferative forms – basasl membrane
lesion (membranous nephropathy, minimal
change disease, focal segmental
glomerulosclerosis) – nephrotic syndrome:
massive proteinuria, hypoproteinrmia
Mesangiocapillary (BM proliferation and lesion) a combination of nephritic and nephrotic
syndromes
6.
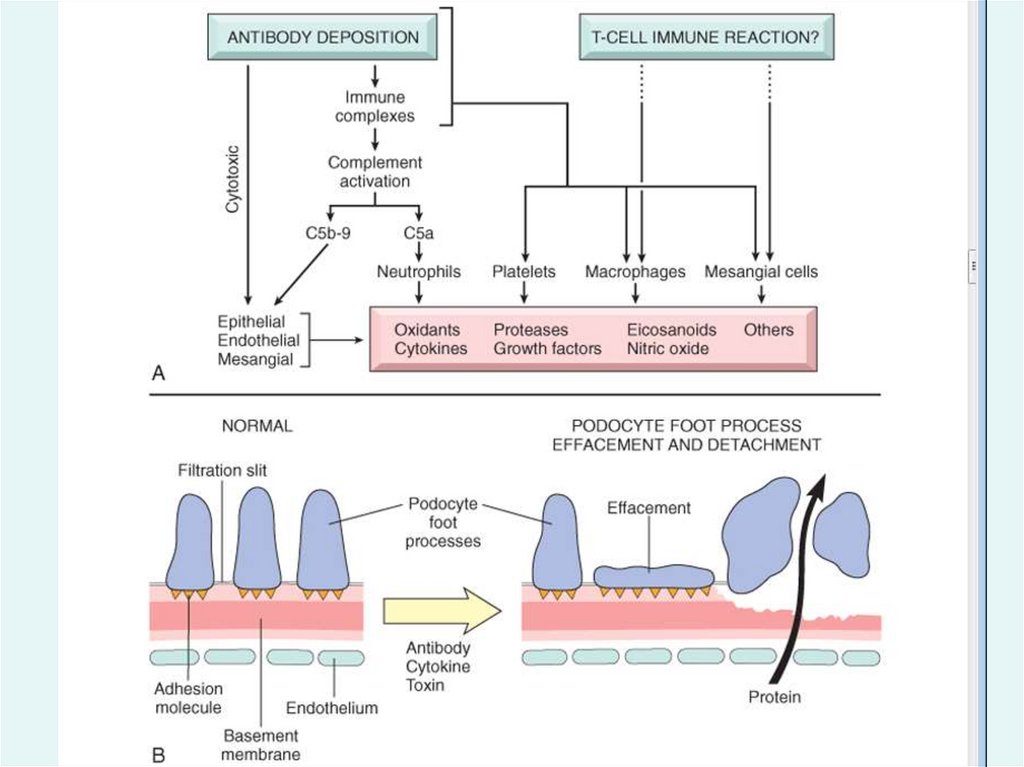
PathogenesisInduction of an altered immune response: infectious
agents, some drugs
Formation and deposition of antibodies and immune
complexes in the glomeruli of the kidneys
Complement activation and attraction of WBC,
synthesis of inflammatory mediators, activation of
hemostasis system
Glomerular and interstitium damage (toxic effect on
tubules of prolonged proteinuria)
Glomerulosclerosis and interstitial fibrosis
Progression of renal failure
7.
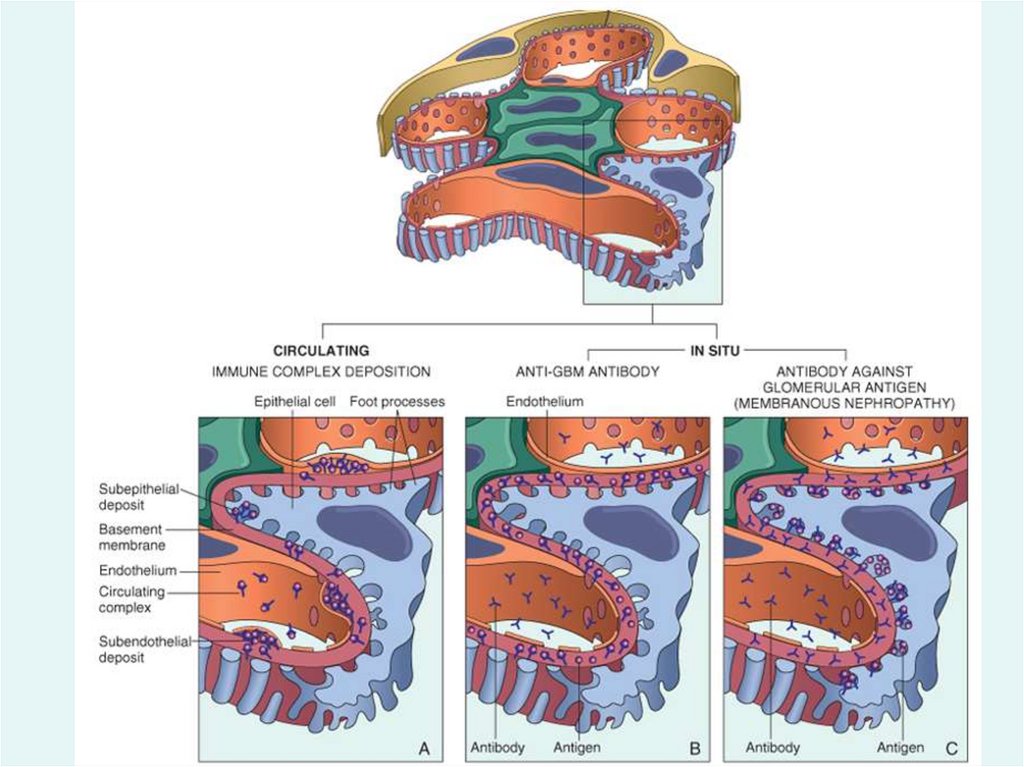
Pathogenetic variants of GNImmunocomplex
* circulating immune complex (CIC) deposition (when the
amount of IC exceeds the cleaning capacity of mesangium
phagocytes; IC are mainly in mesangium)
* IC formation in situ (deposition of antigens first, then
formation of IC in mesangium and subendothelial) The
negative charge of BM promotes the "implantation" of " + "
charged antigenic molecules (bacterial, viral, medicinal,
and tumor AG) into the capillary wall
Antibody (anti-BM of the cells) – AB to the BMC
glycoprotein. Severe structural damage with the
development of half-moons, massive proteinuria, and early
CRF (chronic renal failure)
8.
9.
Damage mediatorsComplement system – local activation on
immune complex (IC) or antibodies (AB) to BM
with the formation of chemotaxis factors and a
membrane-attacking complex
Cytokines and growth factors (platelet-derived
growth factor, transforming factor of growing
(TFG) beta (TNRβ), fibroblast growth factor)
Angiotensin II - induction of growth factors →
cell proliferation and matrix production
10.
Manifestations of an inflammatoryreaction
Proliferation (hypercellularity) due to leukocyte
infiltration and increased proliferation of
mesangial, epithelial and mesangial glomerular
cells
Accumulation of glomerular matrix, often with
glomerular sclerosis and interstitial fibrosis
It is based on a violation of the regulation of
fibrogenesis
11.
12.
13.
Pyelonephritis14.
PyelonephritisInfectious and inflammatory kidney disease
with a predominant lesion of the cup-pelvis
system (CPS), tubulointerstitial tissue and
often with the secondary involvement of the
glomerular apparatus
15.
Classification of pyelonephritisAcute (serous and purulent) and chronic
(causes irreversible changes in the cuppelvis system, sclerosis and wrinkling of the
kidneys)
Obstructive (urolithiasis - stones, organic
narrowing, reflux) and non-obstructive
Special types - pyelonephritis of childhood;
gestational pyelonephritis (in pregnancy)
16.
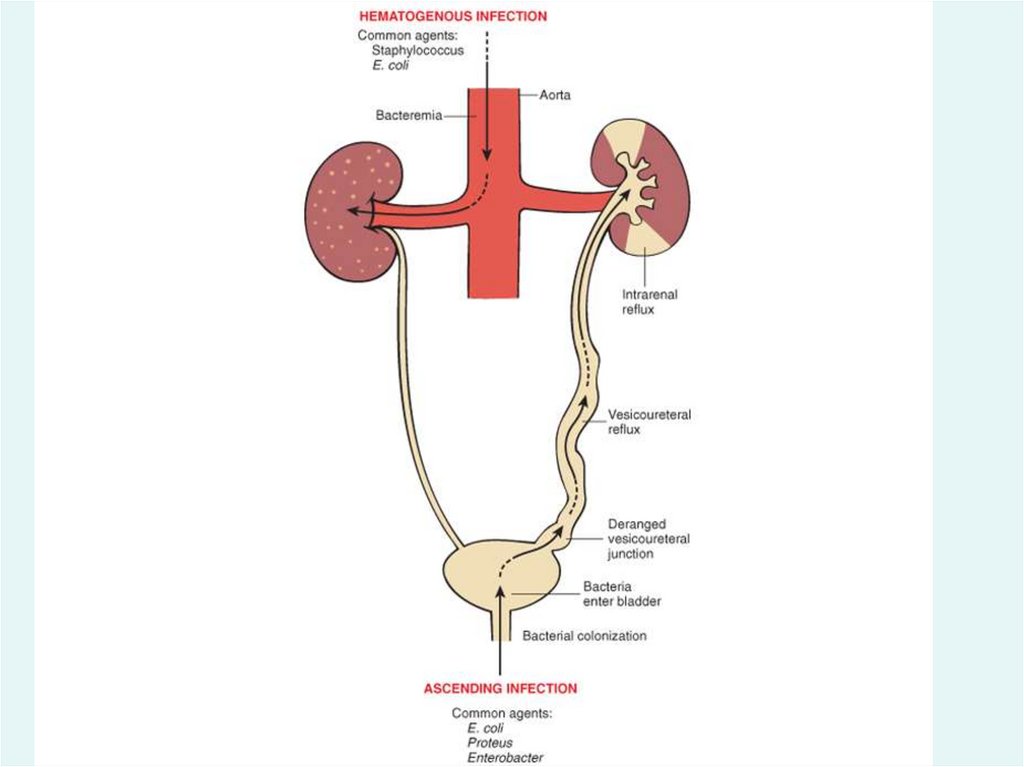
Etiology and pathogenesisPathogens – Enterobacteriaceae:
E. coli –
80%, less often Proteus spp., Klebsiella spp;
sometimes - Gram " + " cocci
Main properties of m/o: the ability of m/o to adhere
and move against the flow of urine; toxins can
cause disturbances in the peristalsis of urinary tract
The main way of infection is ascending
Contribute to urodynamic disorders
Clinic: leukocyturia, bacteriuria, rarely - hematuria;
pain Sd; common symptoms of inflammation
17.
18.
Risk factorsReflux at different levels
Bladder dysfunction
Urolithiasis
Urinary tract tumors
Nephroptosis, kidney dystopia
Malformations of the kidneys and urinary tract
Pregnancy
Diabetes mellitus (DM)
Polycystic kidney disease
Crystalluria
Mechanical injury
Cooling down
Inflammatory diseases of the reproductive system
19.
UrolithiasisA disease characterized by the deposition of
stones in the kidneys and urinary tract
Common kidney disease, incidence 1-2%
It can lead to the development of secondary
pyelonephritis, urinary tract obstruction and the
development of renal failure.
20.
Etiology of urolithiasisExcessive consumption of animal products →
hyperuricemia, ↓Urine pH; hyperoxaluria, hyperCauria
Excessive use NaCl or potassium deficiency →
hypercalciuria, hyperoxaluria
Obesity and hyperuricemia (metabolic Sd)
Alcoholism → induction of hyperuricemia and
hyperthyroidism → Ca-urias
Genetic factors
Medicinal products (Vit C, NSAID)
Oliguria
Urodynamic disorders
Disorders of phosphorus-calcium metabolism, gout
21.
Prevention and treatmentIncreased diuresis to 2.5-3 l / day
Organic production of animal protein and
NaCl, alcohol – in case of lithiase urate
Exclusion of sorrel, spinach, legumes –
with oxalate lithiase
Reducing the acidity of urine
Litholysis with citrate preparations – in case
of urate lithiasis
Shockwave lithotripsy (no more than 25
mm)
Surgical treatment
22.
Ischemic kidney diseaseChronic kidney disease, manifested by signs
of renal hypoperfusion (decreased glomerular
filtration rate (GFR), hypertension) and
increasing nephrosclerosis,
is caused by hemodynamically significant
narrowing of the main renal arteries with
atherosclerotic plaques
23.
EpidemiologyUsually – in patients with advanced
atherosclerosis
Especially often – with type 2 diabetes
melitus (up to 20-25%)
It is often found in patients with treatmentresistant hypertension
It’s often not diagnosed in vivo
24.
Etiology and pathogenesisCauses and mechanisms – that leads to
atherosclerosis development
Possible - genetic predisposition
(endothelial cell defect NO-synthases)
Often – previous hypertension; when
connecting ischemic renal failure (IRF) progression of hypertension
25.
Pathogenesis of ischemickidney disease
Hemodynamically significant renal artery stenosis - more
than 50%
The main link is increasing hypoperfusion of renal tissue
Compensatory reaction: activation of renin and renal
angiotensin II production → maintenance of glomerular
filtration rate (GFR), but increase of systemic hypertension
! Angiotensin converting enzyme inhibitors and angiotensin
receptor blockers lead to increased renal failure
Hypoxia → endothelial dysfunction →
↑ vasoconstrictors + ↓ vasodilators; ↑ growth factors
→ increased fibrogenesis, kidney sclerosis
→ violation of the function
26.
Diabetic nephropathySpecific damage to the renal vessels in DM,
with the formation of diffuse
glomerulosclerosis, leads to the
development of chronic renal failure (CRF)
27.
PathogenesisMetabolic factors
hyperglycemia
* non-enzymatic glycosylation of renal membrane
proteins → impaired structure and function
* direct toxic effect of Glu → activation of protein
kinase C → increased renal vascular permeability
* Activation of SR production → cytotoxic effect
Hyperlipidemia
Modified low-density lipoproteins (LDL) penetrates
through the damaged endothelium, contributes to
the development of sclerotic processes
28.
PathogenesisHemodynamic factor
Systemic hypertension
Intraglomerular hypertension
imbalance between the tone of the bringing
and carrying arterioles:
* vasodilation of the bringer arteriole (action of
hyperglycemia, vasodilating mediators)
* vasoconstriction of the outflow arteriole
(angiotensin II)
29.
Stages of developmentHyperfunction of the kidneys – hyperfiltration,
hyperperfusion, hypertrophy of the kidneys
Initial structural changes – thickening of glomerular
BM, hyperfiltration (more than 2 years)
Incipient nephropathy – microalbuminuria (30-300 mg
/ day), GFR normal or ↑ (more than 5 years)
Severe nephropathy – proteinuria, hypertension, GFR
, sclerosis of 50-75% of glomeruli (more than 10-15
years)
Uremia – GFR less than 10 ml / min, total
glomerulosclerosis (more than 15-20 years)
30.
Diagnostic and treatmentDiagnostics – early detection of
microalbuminuria (MAU)!, later – mild
proteinuria
Prevention and treatment – normalisation
of the glucose level and lipid metabolism;
ACE inhibitors (even in patients with
normal blood pressure); blood pressure
monitoring
31.
Kidneys and pregnancyDuring a normal pregnancy:
placental prostacyclin production and NO
→ systemic vasodilation → increased renal blood
flow and GFR at the same level of reabsorption
↓ blood creatinine; ↑ excretion of glu, uric acid,
amino acids (AA), bicarbonate (alkaline reaction
of urine); physiological proteinuria of pregnant
women (150-300 mg / day).
↓ BP in I trimester, with II trimester – gradual
increase to the initial level
↓BP → RAAS activation → delay of Na and water
→ physiological edema
32.
Nephropathy of pregnantwomen
Complication of the second half of pregnancy,
manifested by hypertension, proteinuria, often in
combination with edema
When progressing, it can cause critical
conditions in the mother and fetus (eclampsia,
HELLP- syndrome, DIC-syndrome, delayed
development and fetal death)
Risk factors: first pregnancy, presence of
somatic pathology, mother's age over 35 and
under 19 years
33.
PathogenesisThe etiology is unclear
Hypothesis – impaired adaptation of the
uterine spiral arteries to developing
pregnancy → circulatory failure
Development of factors causing systemic
endothelial damage by the ischemic placenta
→ generalized endothelial dysfunction,
especially in placental and renal vessels
34.
Consequences of endothelialdysfunction
Decreased synthesis of a/aggregates and vasodilators (NO,
prostacyclin) and increased vasoconstrictor synthesis
(endothelin, TxA2)
→increased tendency to vasospasm → arterial hypertension
→increased vascular permeability →↓blood volume, edema
→activation of the hemostasis system → DIC-syndrome
The result is a violation of tissue perfusion:
- placenta → delayed fetal development, fetal death
- kidney disease → proteinuria, fluid retention, edema
→ preeclampsia, eclampsia (impaired consciousness,
seizures)
liver → may be acute liver failure in case of HELLPsyndrome development (Hemolisis, Elevated Liver enzymes,
Low Platelets)
35.
Chronic renal failure36.
Chronic renal failurea syndrome caused by progressive
sclerosis of the renal parenchyma with the
death of nephrons due to primary or
secondary chronic kidney disease
The incidence of CRF is 100-600 cases
per 1 million adults
37.
Etiology of CRFInflammatory diseases: chronic glomerulonephritis,
chr. pyelonephritis, kidney damage in systemic
connective tissue diseases (SCTD), tuberculosis, HIVnephropathy…
Metabolic and endocrine disorders: Diabetes melitus,
gout, amyloidosis
Vascular diseases: malignant hypertension, ischemic
kidney disease
Hereditary and congenital diseases: polycystic
fibrosis, segmental hypoplasia…
Obstructive nephropathies: urolithiasis, tumors,
hydronephrosis
Toxic and medicinal nephropathies: analgesic,
alcoholic, lead, etc.
38.
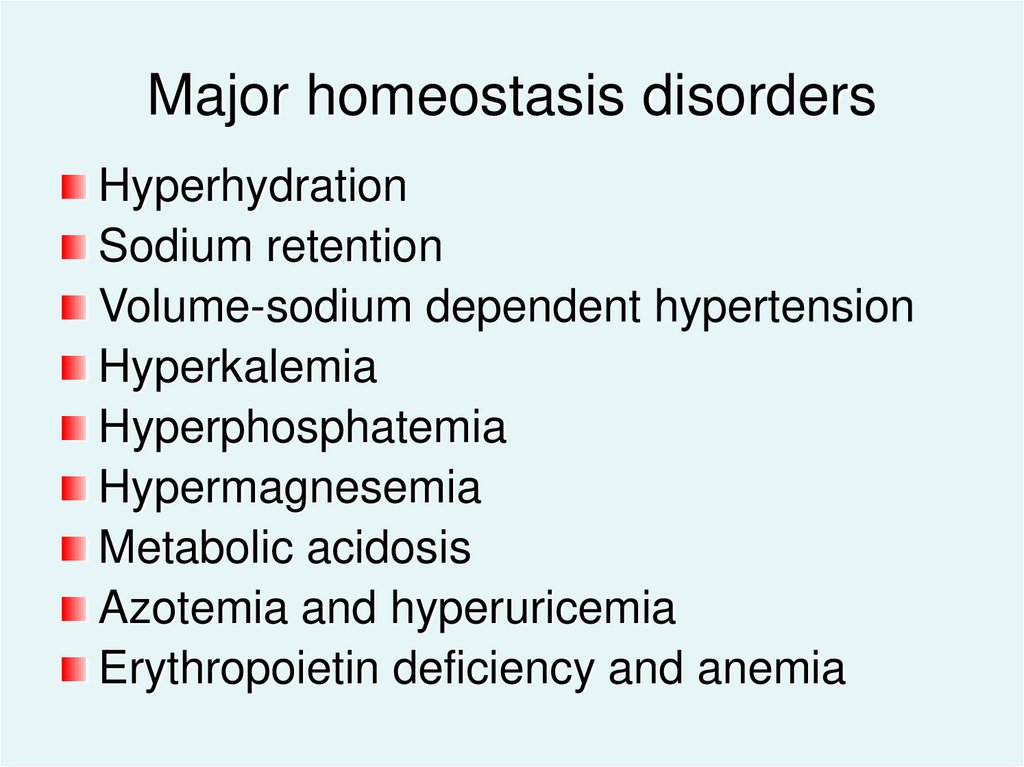
Major homeostasis disordersHyperhydration
Sodium retention
Volume-sodium dependent hypertension
Hyperkalemia
Hyperphosphatemia
Hypermagnesemia
Metabolic acidosis
Azotemia and hyperuricemia
Erythropoietin deficiency and anemia
39.
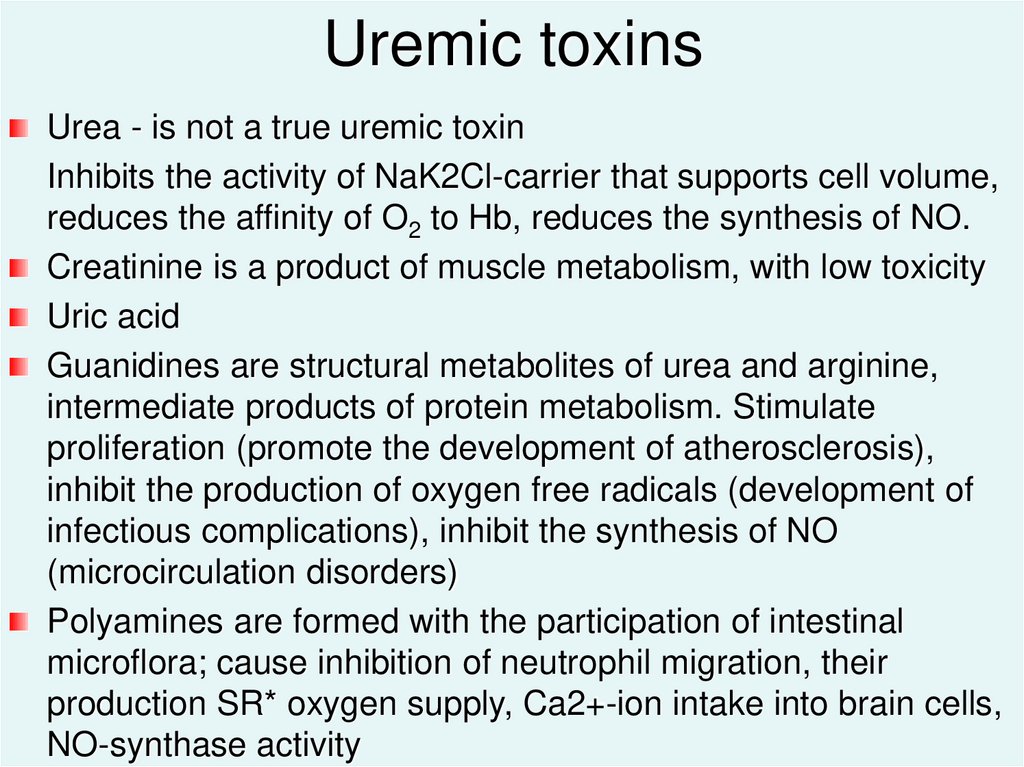
Uremic toxinsUrea - is not a true uremic toxin
Inhibits the activity of NaK2Cl-carrier that supports cell volume,
reduces the affinity of O2 to Hb, reduces the synthesis of NO.
Creatinine is a product of muscle metabolism, with low toxicity
Uric acid
Guanidines are structural metabolites of urea and arginine,
intermediate products of protein metabolism. Stimulate
proliferation (promote the development of atherosclerosis),
inhibit the production of oxygen free radicals (development of
infectious complications), inhibit the synthesis of NO
(microcirculation disorders)
Polyamines are formed with the participation of intestinal
microflora; cause inhibition of neutrophil migration, their
production SR* oxygen supply, Ca2+-ion intake into brain cells,
NO-synthase activity
40.
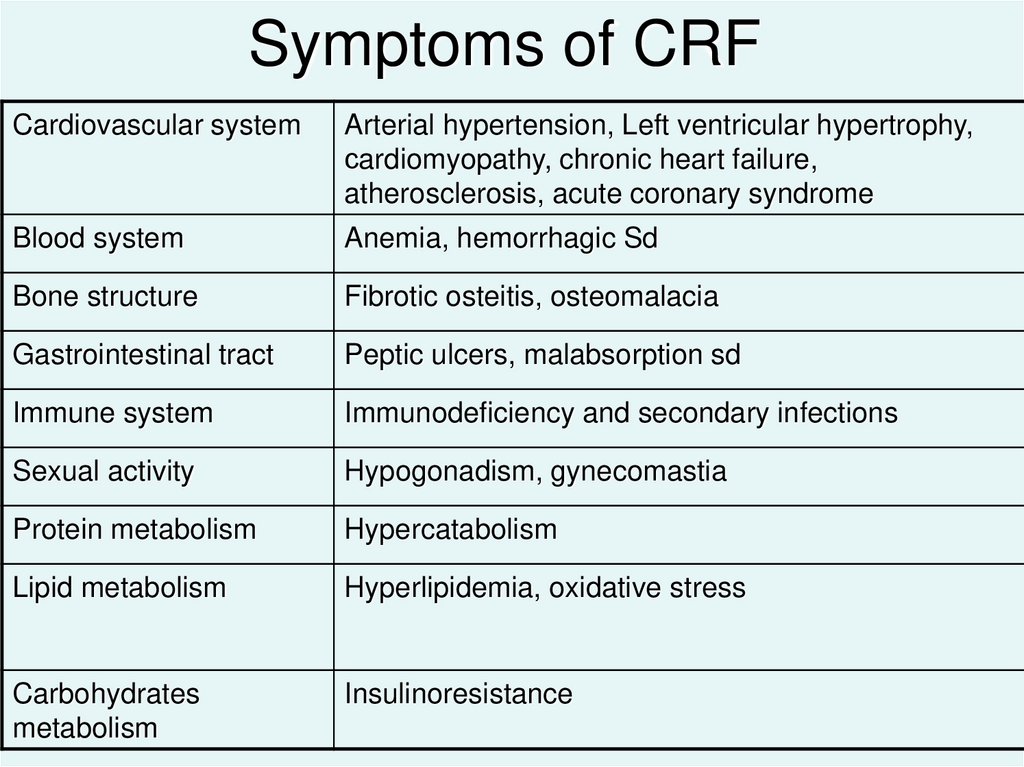
Symptoms of CRFCardiovascular system
Arterial hypertension, Left ventricular hypertrophy,
сardiomyopathy, chronic heart failure,
atherosclerosis, acute coronary syndrome
Blood system
Anemia, hemorrhagic Sd
Bone structure
Fibrotic osteitis, osteomalacia
Gastrointestinal tract
Peptic ulcers, malabsorption sd
Immune system
Immunodeficiency and secondary infections
Sexual activity
Hypogonadism, gynecomastia
Protein metabolism
Hypercatabolism
Lipid metabolism
Hyperlipidemia, oxidative stress
Carbohydrates
metabolism
Insulinoresistance
41.
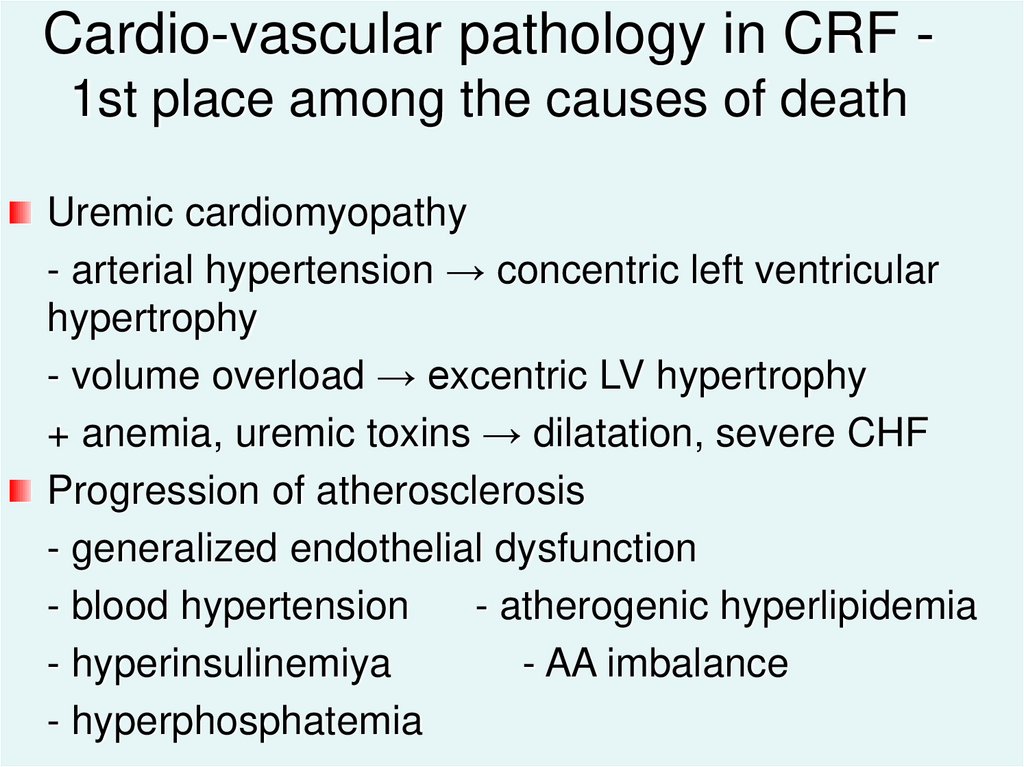
Cardio-vascular pathology in CRF 1st place among the causes of deathUremic cardiomyopathy
- arterial hypertension → concentric left ventricular
hypertrophy
- volume overload → excentric LV hypertrophy
+ anemia, uremic toxins → dilatation, severe CHF
Progression of atherosclerosis
- generalized endothelial dysfunction
- blood hypertension
- atherogenic hyperlipidemia
- hyperinsulinemiya
- AA imbalance
- hyperphosphatemia
42.
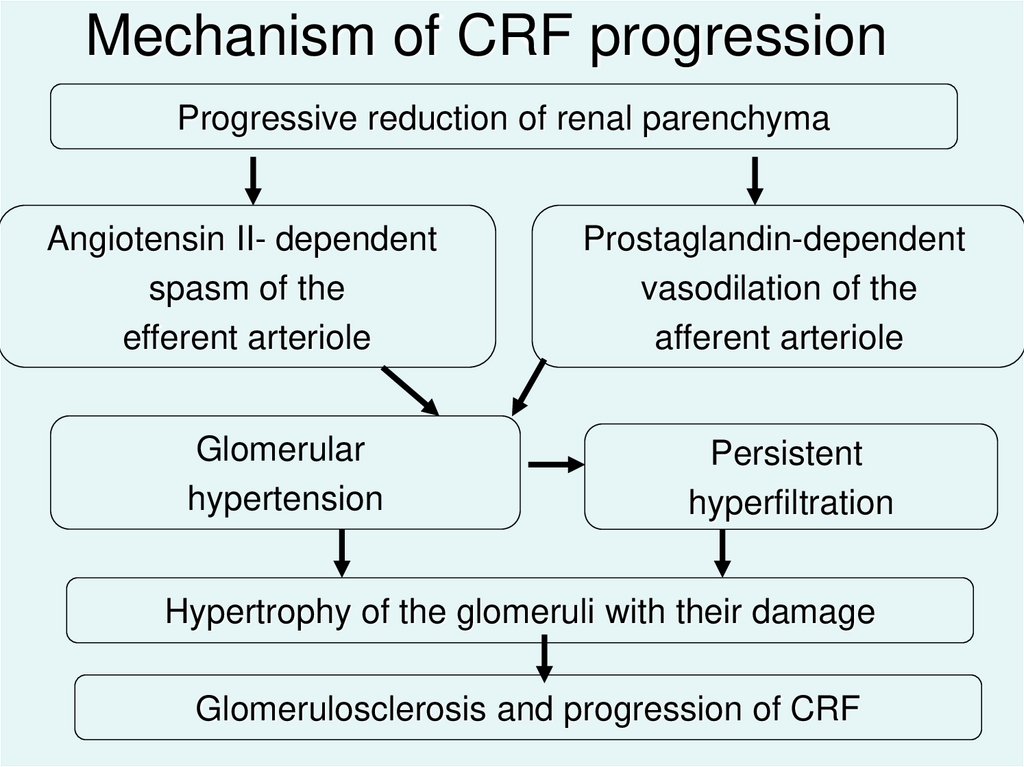
Mechanism of CRF progressionProgressive reduction of renal parenchyma
Angiotensin II- dependent
spasm of the
efferent arteriole
Glomerular
hypertension
Prostaglandin-dependent
vasodilation of the
afferent arteriole
Persistent
hyperfiltration
Hypertrophy of the glomeruli with their damage
Glomerulosclerosis and progression of CRF
43.
Factors that aggravate the courseof CRF
Intercurrent infections, especially of the
urinary tract
Acute ureteral obstruction
Pregnancy
Medications with nephrotoxic effects
44.
Stages of CRF45.
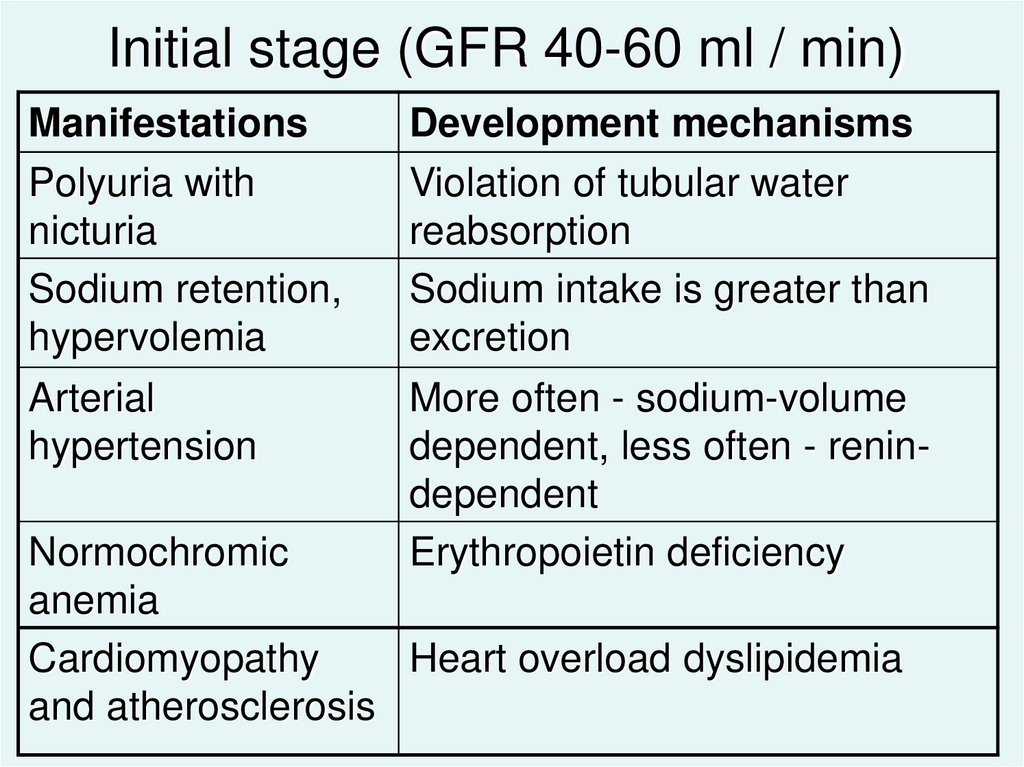
Initial stage (GFR 40-60 ml / min)Manifestations
Development mechanisms
Polyuria with
nicturia
Sodium retention,
hypervolemia
Violation of tubular water
reabsorption
Sodium intake is greater than
excretion
Arterial
hypertension
More often - sodium-volume
dependent, less often - renindependent
Erythropoietin deficiency
Normochromic
anemia
Cardiomyopathy
Heart overload dyslipidemia
and atherosclerosis
46.
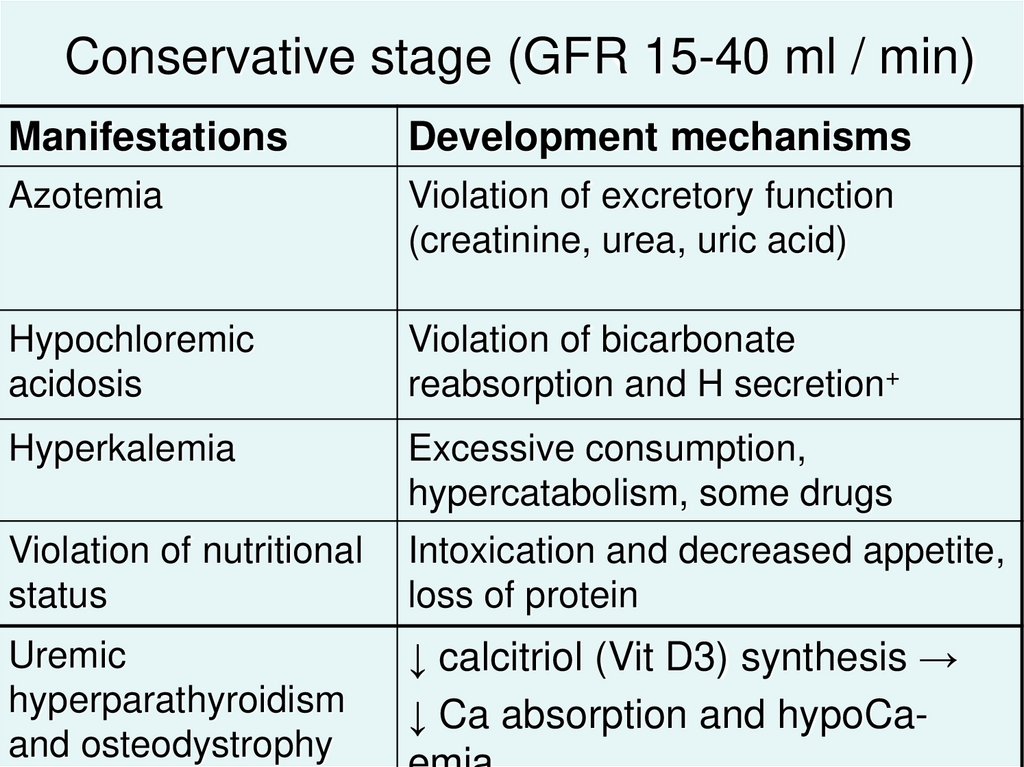
Conservative stage (GFR 15-40 ml / min)Manifestations
Development mechanisms
Azotemia
Violation of excretory function
(creatinine, urea, uric acid)
Hypochloremic
acidosis
Violation of bicarbonate
reabsorption and H secretion+
Hyperkalemia
Excessive consumption,
hypercatabolism, some drugs
Violation of nutritional
status
Intoxication and decreased appetite,
loss of protein
Uremic
hyperparathyroidism
and osteodystrophy
↓ calcitriol (Vit D3) synthesis →
↓ Ca absorption and hypoCa-
47.
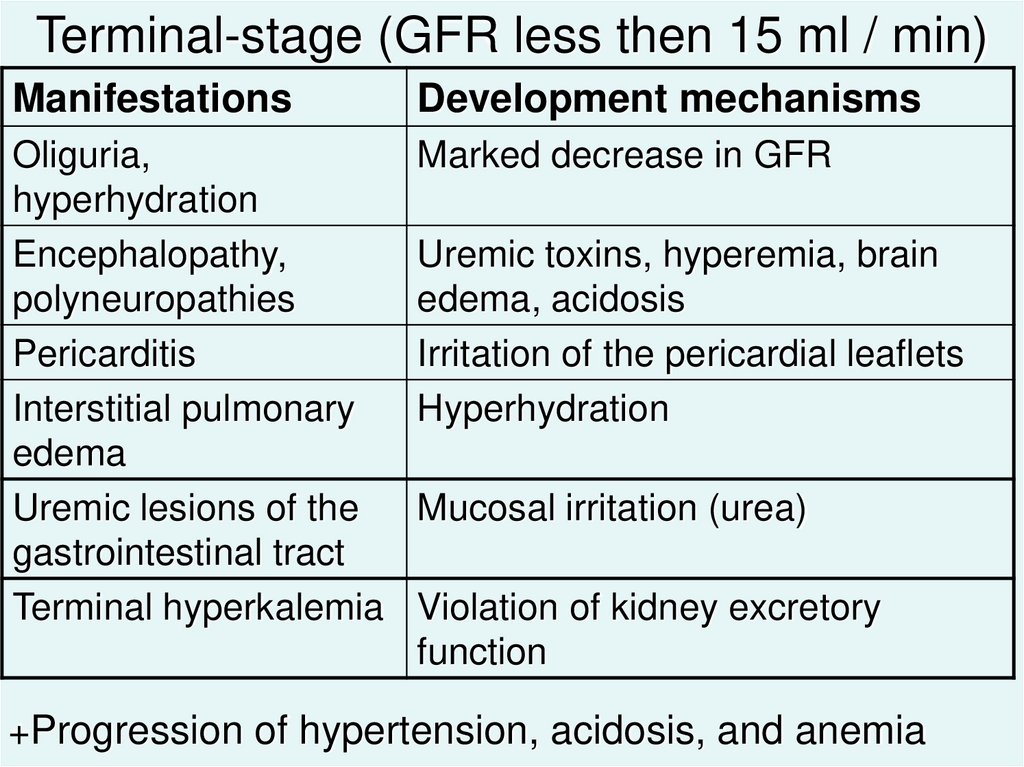
Terminal-stage (GFR less then 15 ml / min)Manifestations
Development mechanisms
Oliguria,
hyperhydration
Encephalopathy,
polyneuropathies
Pericarditis
Interstitial pulmonary
edema
Uremic lesions of the
gastrointestinal tract
Terminal hyperkalemia
Marked decrease in GFR
Uremic toxins, hyperemia, brain
edema, acidosis
Irritation of the pericardial leaflets
Hyperhydration
Mucosal irritation (urea)
Violation of kidney excretory
function
+Progression of hypertension, acidosis, and anemia
48.
Significance of hyperkalemia! Impaired function of excitable tissues due to
hyperpolarization of cell membranes
neuron suppression, paralysis, coma
bradycardia, AV- blockage, cardiac arrest
respiratory disorders
49.
Principles of CRF therapyOn I-II stages:
- treatment of the underlying disease
- Water-electrolyte ballance correction
(diet, diuretics)
- hypotensive therapy
End-stage CRF - hemodialysis or kidney
transplantation









 medicine
medicine