Similar presentations:
Kidneys pathology. (Subject 17)
1.
2. Lecture Plan
3.
The kidneys are essentially regulatory organswhich maintain the volume and composition of
body fluid by filtration of the blood and selective
reabsorption or secretion of filtered solutes.
The kidneys take their blood supply directly from
the aorta via the renal arteries; blood is returned to
the inferior vena cava via the renal veins
The kidneys are critical in regulating the internal
environment of the body.
4.
Homeostasis:Sodium/Volume;
Water/Osmolarity;
Asid/Base;
Electrolytes (K+, Ca++, Mg++, HPO4)
Hemodynamic regulation:
Renin / Angiotensin / Aldosteron;
Sodium balance;
Pressure natriuresis
Endocrine function:
Renin;
Erythropoietin;
1,25 – Vitamin D
Clearance:
Products of metabolism;
Drugs and toxins;
5.
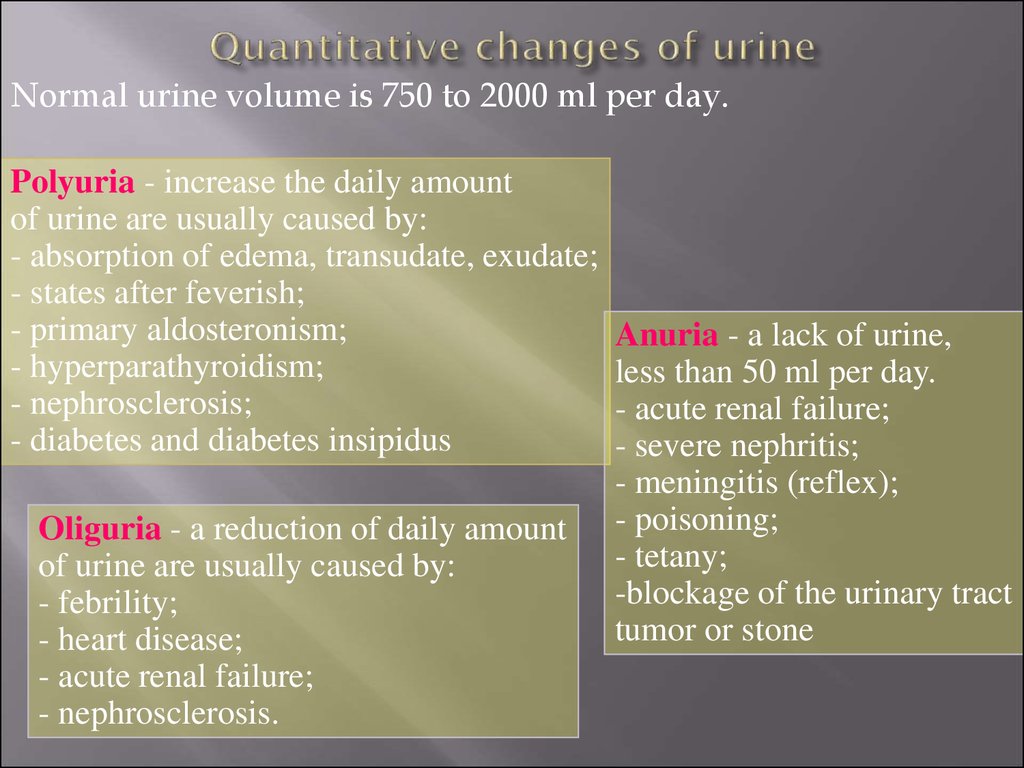
Normal urine volume is 750 to 2000 ml per day.Polyuria - increase the daily amount
of urine are usually caused by:
- absorption of edema, transudate, exudate;
- states after feverish;
- primary aldosteronism;
- hyperparathyroidism;
- nephrosclerosis;
- diabetes and diabetes insipidus
Oliguria - a reduction of daily amount
of urine are usually caused by:
- febrility;
- heart disease;
- acute renal failure;
- nephrosclerosis.
Anuria - a lack of urine,
less than 50 ml per day.
- acute renal failure;
- severe nephritis;
- meningitis (reflex);
- poisoning;
- tetany;
-blockage of the urinary tract
tumor or stone
6.
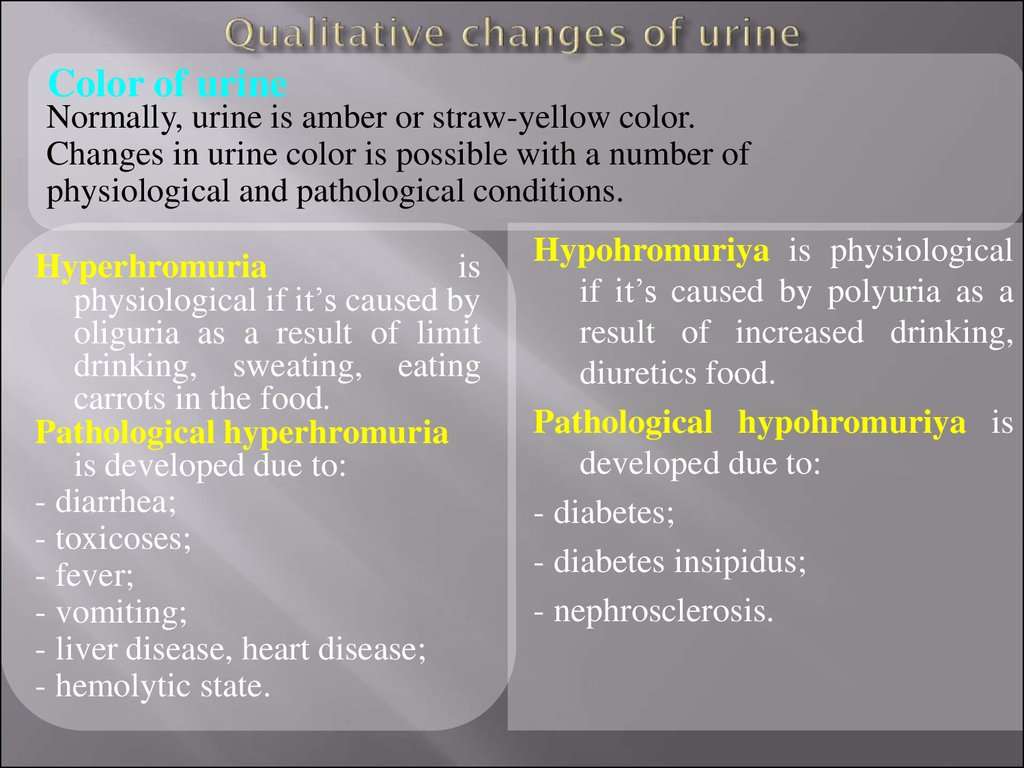
Color of urineNormally, urine is amber or straw-yellow color.
Changes in urine color is possible with a number of
physiological and pathological conditions.
Hyperhromuria
is
physiological if it’s caused by
oliguria as a result of limit
drinking, sweating, eating
carrots in the food.
Pathological hyperhromuria
is developed due to:
- diarrhea;
- toxicoses;
- fever;
- vomiting;
- liver disease, heart disease;
- hemolytic state.
Hypohromuriya is physiological
if it’s caused by polyuria as a
result of increased drinking,
diuretics food.
Pathological hypohromuriya is
developed due to:
- diabetes;
- diabetes insipidus;
- nephrosclerosis.
7.
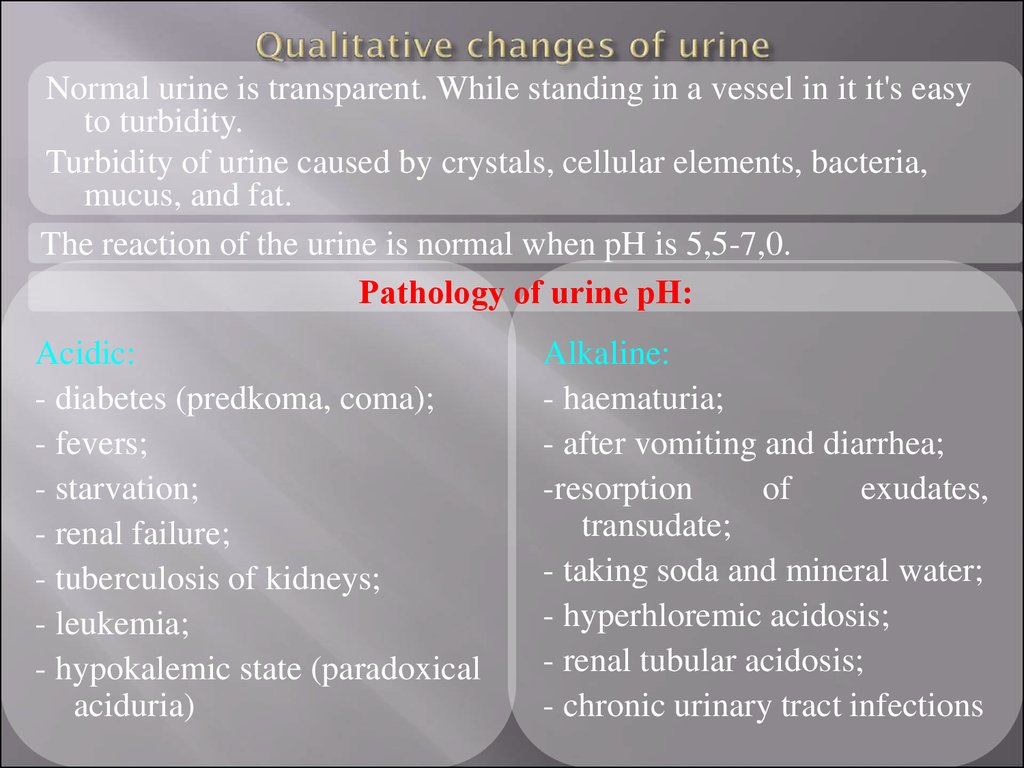
Normal urine is transparent. While standing in a vessel in it it's easyto turbidity.
Turbidity of urine caused by crystals, cellular elements, bacteria,
mucus, and fat.
The reaction of the urine is normal when pH is 5,5-7,0.
Pathology of urine рН:
Acidic:
- diabetes (predkoma, coma);
- fevers;
- starvation;
- renal failure;
- tuberculosis of kidneys;
- leukemia;
- hypokalemic state (paradoxical
aciduria)
Alkaline:
- haematuria;
- after vomiting and diarrhea;
-resorption
of
exudates,
transudate;
- taking soda and mineral water;
- hyperhloremic acidosis;
- renal tubular acidosis;
- chronic urinary tract infections
8.
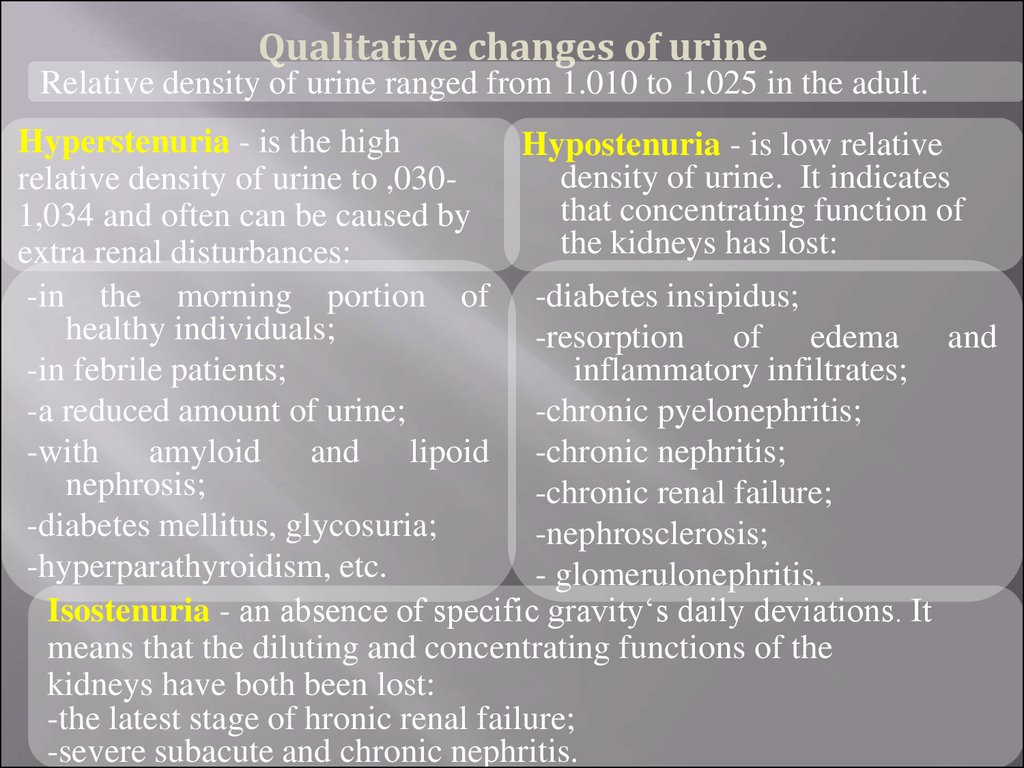
Qualitative changes of urineRelative density of urine ranged from 1.010 to 1.025 in the adult.
Hyperstenuria - is the high
Hypostenuria - is low relative
density of urine. It indicates
relative density of urine to ,030that concentrating function of
1,034 and often can be caused by
the kidneys has lost:
extra renal disturbances:
-in the morning portion of -diabetes insipidus;
healthy individuals;
-resorption of edema and
-in febrile patients;
inflammatory infiltrates;
-a reduced amount of urine;
-chronic pyelonephritis;
-with amyloid and lipoid -chronic nephritis;
nephrosis;
-chronic renal failure;
-diabetes mellitus, glycosuria;
-nephrosclerosis;
-hyperparathyroidism, etc.
- glomerulonephritis.
Isostenuria - an absence of specific gravity‘s daily deviations. It
means that the diluting and concentrating functions of the
kidneys have both been lost:
-the latest stage of hronic renal failure;
-severe subacute and chronic nephritis.
9.
Qualitative changes of urinePathological admixtures in urine
Proteinuria is defined as urinary protein excretion exceeding
150 mg/day.
The mechanism of proteinuria may be related to 2 aspects:
1. Molecular barrier injury: holes on glomerular basement
membrane (GBM) become larger, plasma protein can pass
through the GBM into the urine;
2.
Charge barrier injury: loss of negative charge (glycoprotein)
within GBM, plasma protein (with negative charge) can pass
through the GBM into urine.
10.
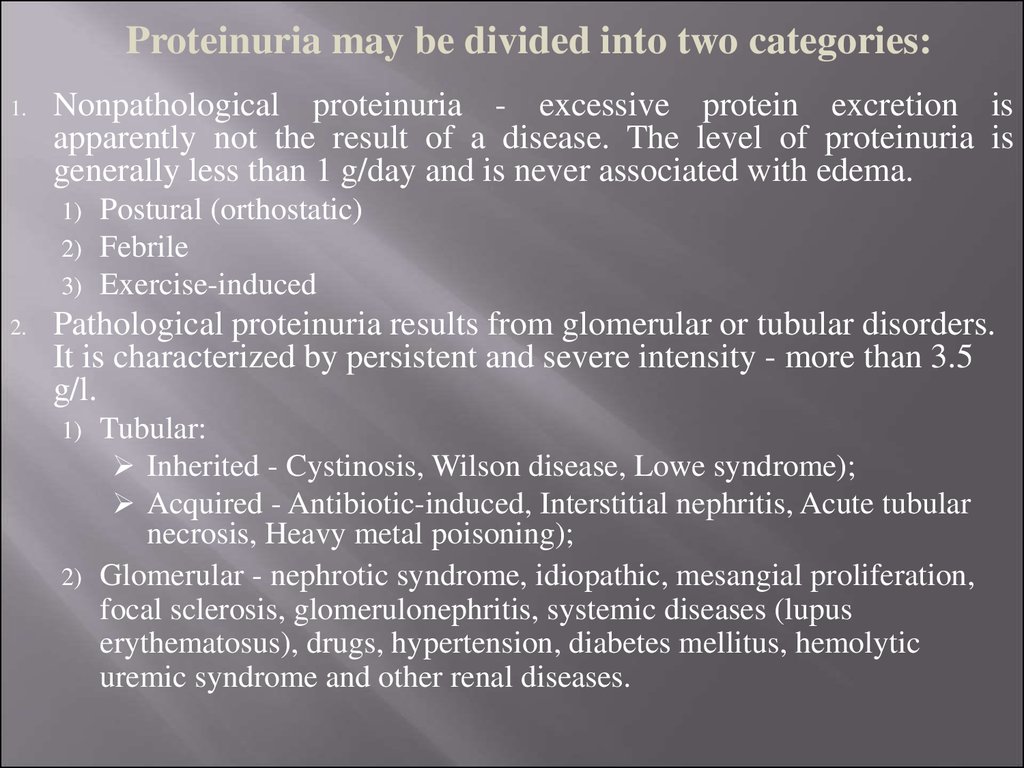
Proteinuria may be divided into two categories:1.
Nonpathological proteinuria - excessive protein excretion is
apparently not the result of a disease. The level of proteinuria is
generally less than 1 g/day and is never associated with edema.
1)
2)
3)
2.
Postural (orthostatic)
Febrile
Exercise-induced
Pathological proteinuria results from glomerular or tubular disorders.
It is characterized by persistent and severe intensity - more than 3.5
g/l.
Tubular:
Inherited - Cystinosis, Wilson disease, Lowe syndrome);
Acquired - Antibiotic-induced, Interstitial nephritis, Acute tubular
necrosis, Heavy metal poisoning);
2) Glomerular - nephrotic syndrome, idiopathic, mesangial proliferation,
focal sclerosis, glomerulonephritis, systemic diseases (lupus
erythematosus), drugs, hypertension, diabetes mellitus, hemolytic
uremic syndrome and other renal diseases.
1)
11.
Qualitative changes of urineHaematuria is defined as appearance of RBC in urine
Common Causes of Glomerular Hematuria:
1. IgA nephropathy (Berger’s disease);
2. Thin glomerular basement membrane disease;
3. Hereditary nephritis (Alport’s syndrome).
Common Causes of Non-Glomerular Hematuria:
Upper Tract:
1. Urolithiasis;
URETERAL
2. Pyelonephritis;
3. Renal cell cancer;
4. Transitional cell carcinoma;
5. Urinary obstruction;
6. Benign hematuria
Lower Tract:
BLADDER
1. Bacterial cystitis;
2. Benign prostatic hyperplasia;
3. Transitional cell carcinoma;
4. Strenuous exercise (“marathon runner’s hematuria”);
5. Spurious hematuria (e.g. menses);
6. Instrumentation;
7. Benign hematuria
RENAL
URETHRAL
12.
Haematuria is most usefully divided into:Visible (macroscopic) haematuria (VH)
Non-visible (microscopic) haematuria (NVH) - is not visible to
the naked eye.
Macroscopic hematuria can be divided into three types:
Initial Hematuria - bleeding that occurs at the start of urination.
This could indicate a problem in the urethra in women or the
prostate (in men).
Total Hematuria - bleeding that occurs while urinating is known as
total hematuria. Men could experience total hematuria because
of an enlarged prostrate. In women, vaginal bleeding during
urination could be an indication of an infection in the bladder,
ureter or kidneys.
Terminal Hematuria - bleeding after urination in men and women.
Blood after urination in women is usually indicative of a
bladder infection. Men can also experience terminal hematuria
because of prostate diseases.
13.
Qualitative changes of urinePathological admixtures in urine
Leukocyturia is the presence of leukocytes in urine
Usually, the WBC's in urine are granulocytes.
The common diseases that may result to the presence of leukocytes in
urine:
1. Urinary tract infection;
2. Cystitis – is the inflammation of the bladder (the infection has
made its way from the urethra to the bladder, spreading the
infection and damaging parts of the kidneys).
3. Pyelonephritis –is case, the infection has affected not only the
urethra and the bladder, but also the kidneys.
14.
Qualitative changes of urinePathological admixtures in urine
Urinary casts are cylindrical aggregations of particulate matter that
form in the distal nephron.
The various types of casts that may be
classified as follows:
I. Acellular casts
Acellular casts II. Cellular casts
1. Hyaline casts - the most common type
of cast, Tamm-Horsfall mucoprotein
secreted from the tubular epithelial cells.
2. Granular casts -result either from the
breakdown of cellular casts, or the
inclusion of aggregates of plasma proteins.
3. Waxy casts - thought to represent the end product of cast
evolution, suggest the very low urine flow associated with severe,
longstanding kidney disease such as renal failure.
4. Fatty casts - formed by the breakdown of lipid rich epithelial cells,
these are hyaline casts with fat globule inclusions.
5. Pigment casts - formed by the adhesion of metabolic breakdown
products or drug pigments.
6. Crystal casts - though crystallized urinary solutes, such as
oxalates, urates, or sulfonamides, may become enmeshed within a
hyaline cast during its formation.
15.
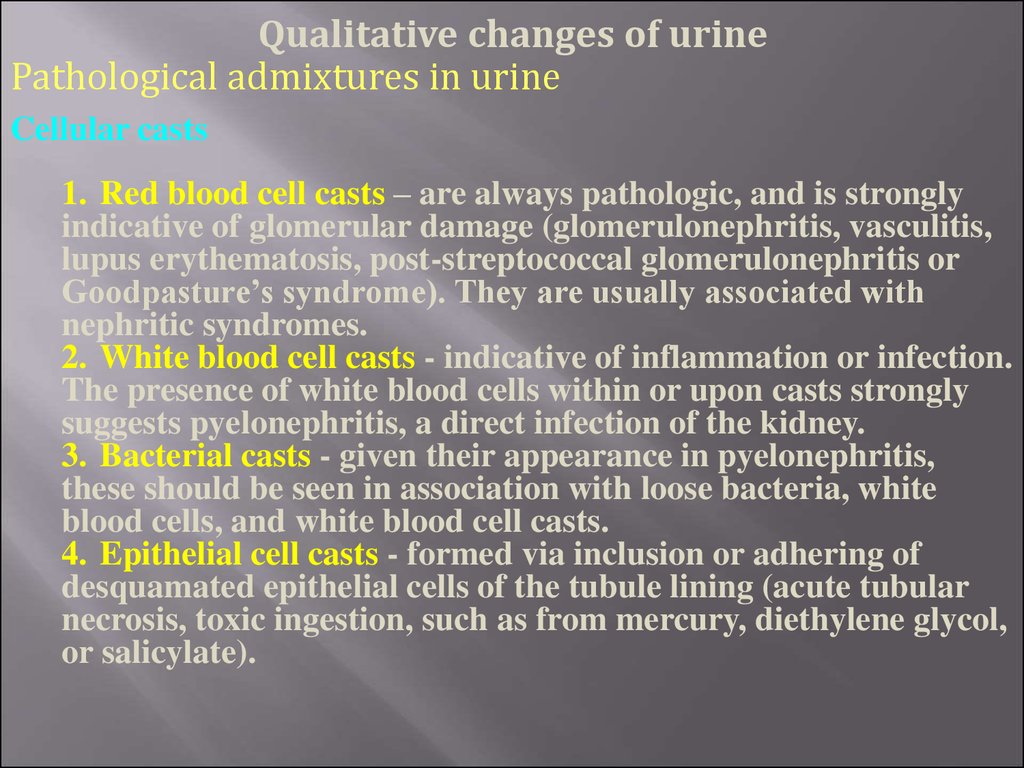
Qualitative changes of urinePathological admixtures in urine
Cellular casts
1. Red blood cell casts – are always pathologic, and is strongly
indicative of glomerular damage (glomerulonephritis, vasculitis,
lupus erythematosis, post-streptococcal glomerulonephritis or
Goodpasture’s syndrome). They are usually associated with
nephritic syndromes.
2. White blood cell casts - indicative of inflammation or infection.
The presence of white blood cells within or upon casts strongly
suggests pyelonephritis, a direct infection of the kidney.
3. Bacterial casts - given their appearance in pyelonephritis,
these should be seen in association with loose bacteria, white
blood cells, and white blood cell casts.
4. Epithelial cell casts - formed via inclusion or adhering of
desquamated epithelial cells of the tubule lining (acute tubular
necrosis, toxic ingestion, such as from mercury, diethylene glycol,
or salicylate).
16.
Qualitative changes of urinePathological admixtures in urine
Glycosuria - is the identification of glucose in urine.
In the urine of healthy human glucose is not detected in the urine
in clinical diagnostic laboratories.
Glucosuria depends on three factors:
1. Blood glucose concentration;
2. Glomerular filtrate kidney in 1 minute;
3. Amount reabsorbed in the tubules of glucose in 1 ml.
Glucosuria appears when blood glucose levels exceed 10 mmol/l –
the “renal threshold” or the glomerular clearance of glucose.
Causes of glycosuria:
1. Insulin deficiency;
2. Decline of renal function and / or liver;
3. Violation of the hormonal regulation of carbohydrate
metabolism;
4. Eating large amounts of carbohydrates
17.
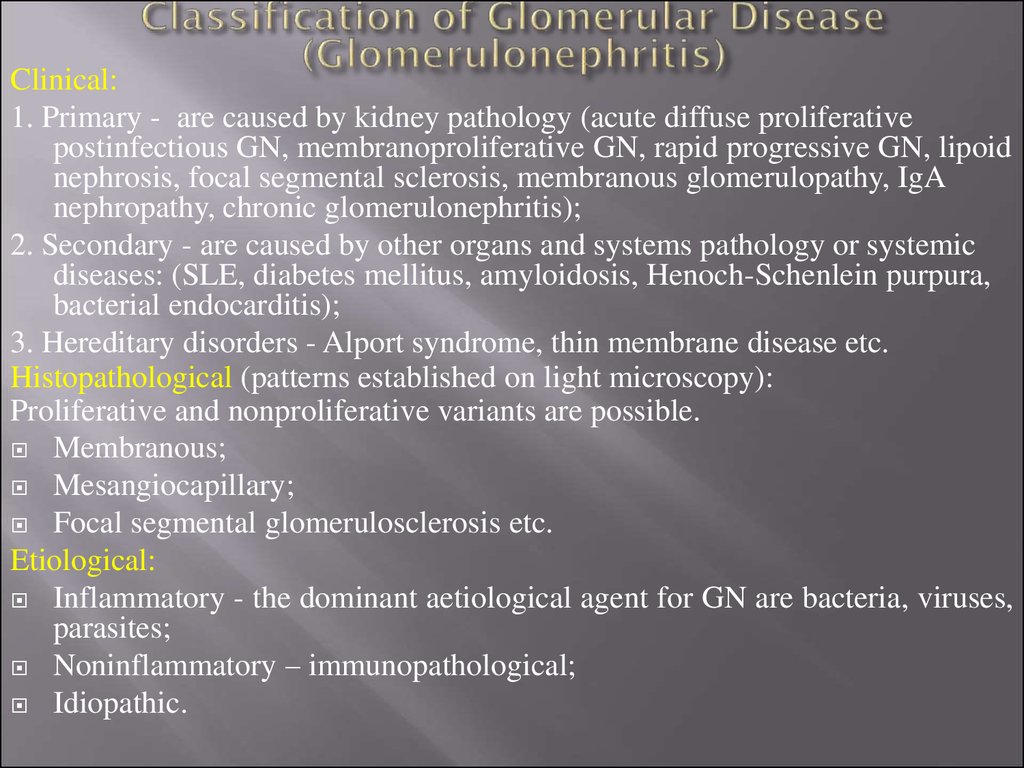
Clinical:1. Primary - are caused by kidney pathology (acute diffuse proliferative
postinfectious GN, membranoproliferative GN, rapid progressive GN, lipoid
nephrosis, focal segmental sclerosis, membranous glomerulopathy, IgA
nephropathy, chronic glomerulonephritis);
2. Secondary - are caused by other organs and systems pathology or systemic
diseases: (SLE, diabetes mellitus, amyloidosis, Henoch-Schenlein purpura,
bacterial endocarditis);
3. Hereditary disorders - Alport syndrome, thin membrane disease etc.
Histopathological (patterns established on light microscopy):
Proliferative and nonproliferative variants are possible.
Membranous;
Mesangiocapillary;
Focal segmental glomerulosclerosis etc.
Etiological:
Inflammatory - the dominant aetiological agent for GN are bacteria, viruses,
parasites;
Noninflammatory – immunopathological;
Idiopathic.
18.
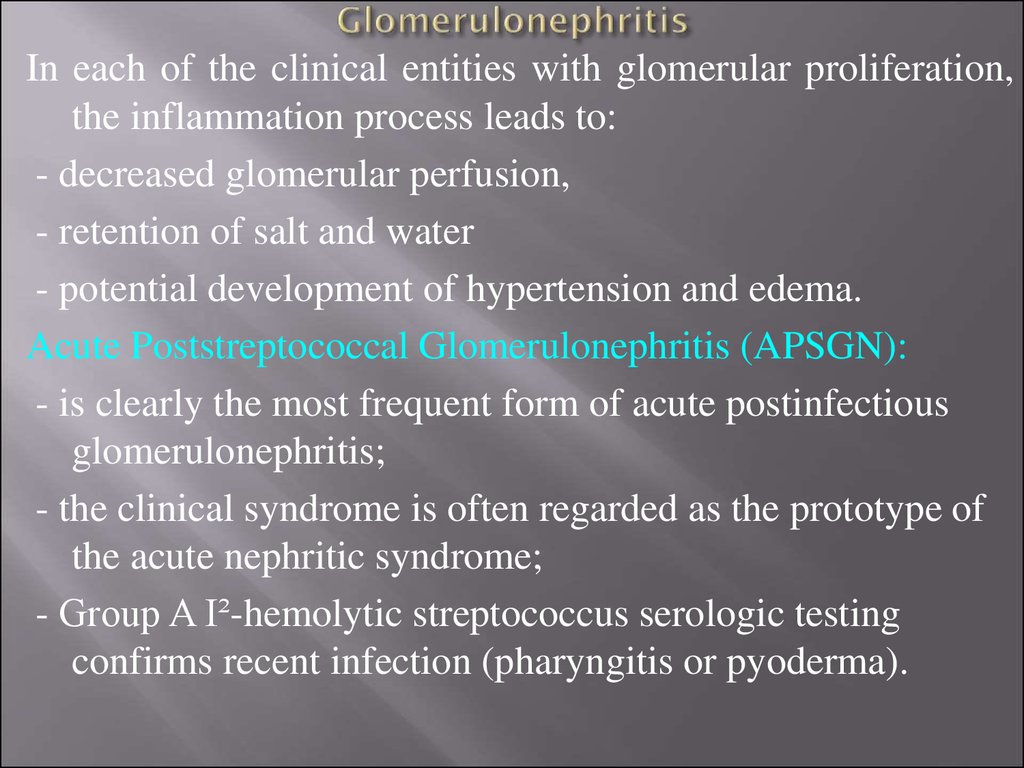
In each of the clinical entities with glomerular proliferation,the inflammation process leads to:
- decreased glomerular perfusion,
- retention of salt and water
- potential development of hypertension and edema.
Acute Poststreptococcal Glomerulonephritis (APSGN):
- is clearly the most frequent form of acute postinfectious
glomerulonephritis;
- the clinical syndrome is often regarded as the prototype of
the acute nephritic syndrome;
- Group A I²-hemolytic streptococcus serologic testing
confirms recent infection (pharyngitis or pyoderma).
19.
APSGN is primarily a disease of school-age children (5 15 years) and is more common in boys.Patients are usually afebrile with a latency period
following pharyngitis of 1 to 2 weeks and 3 to 6 weeks
after a skin infection.
The most common presenting features are edema and
gross hematuria. Essentially all the patients have
microhematuria. The urine often has a color, described as
smoky, cola-colored, or tea-colored.
Hypertension is common but is usually mild to moderate;
rarely, hypertensive encephalopathy has been reported.
Nephritic syndrome is a typical manifestation of APSGN.
Fewer than 5% of patients develop nephrotic syndrome
with significant proteinuria and a slightly depressed
serum albumin level.
20.
PathogenesisStreptococcal Infection
Immune Complexes Formation and
Depositions in Glomerular Basement Membrane (GBM)
Complement System Activated
Low Serum Complement
Immune Injuries
Cellular Proliferation
Capillary Lumen Narrowed
Hematuria
Proteinuria
Glomerular Blood Flow Decreased
Oliguria
Glomerular Filtration Rate
Decreased
Distal Sodium Reabsorption
Retention of Water and Sodium
Blood Volume
GBM Fracture
Odema
Hypertension
21.
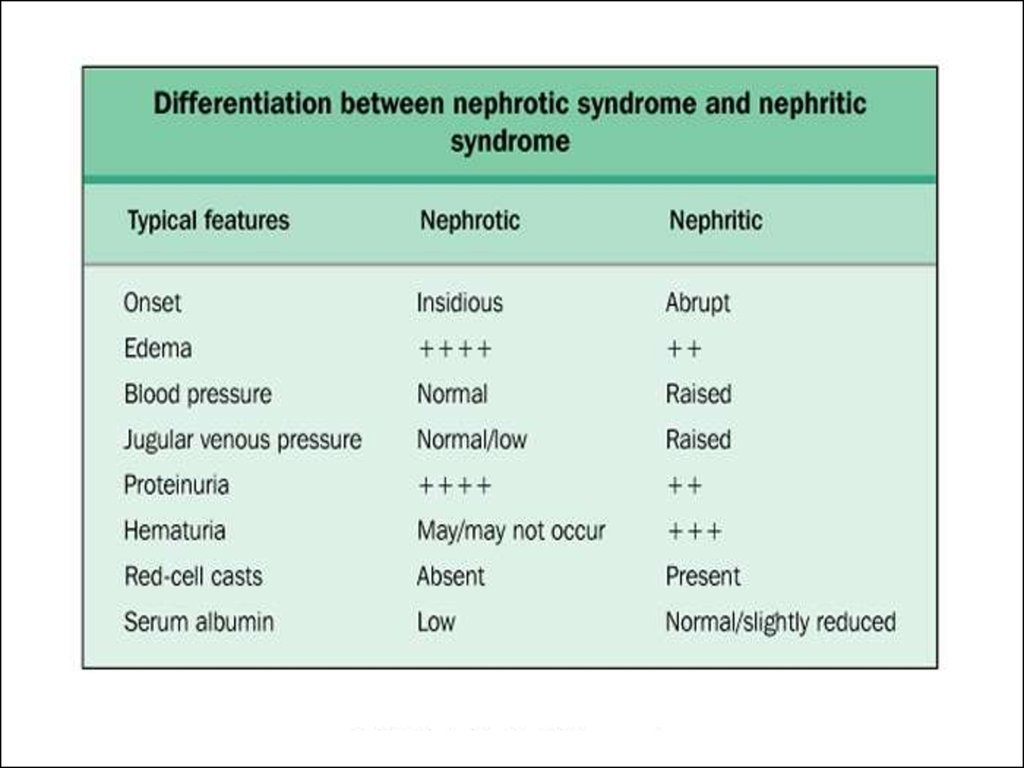
Nephritic Syndrome - is the acute onset of:1.
Hematuria - may be microscopic or macroscopic. Podocytes develop
large pores which allow blood and protein through.
2.
Proteinuria - small amount, < 3.5 g/24 hr).
3.
Hypertension is generally mild.
4.
Oedema is usually mild and results from sodium and water retention.
5.
Oliguria (low urine volume <300ml/day due to renal function been
poor).
6.
Red cell casts
Causes of Acute Nephritis:
I. Primary Glomerulonephritis - acute GN (post-streptococcal, nonstreptococcal, rapidly progressive GN, membrano-proliferative GN,
focal GN, IgA nephropathy).
II. Systemic Disease (SLE, polyarteritis nodosa, Wegener's
granulomatosis, Henoch-Schonlein purpura, cryoglobulinaemia).
22.
Nephrotic syndrome - is a group of diseases having differentpathogenesis and characterized by clinical findings of:
1.
Massive proteinuria (>3.5g in 24hrs, urine looks frothy), mostly
consists of loss of albumin.
2.
Hypoalbuminemia (albumin is lost in the urine due to gaps in
podocytes allowing proteins to escape).
3.
Oedema - is usually peripheral (swelling around ankles & eyes) due
to:
loss of albumin and intravascular oncotic pressure decreasing;
sodium and water retention (secondary hyperaldosteronism, but
osmotic pressure of blood is decreased);
increase of hydrodynamic intravascular pressure and vessels
permobility (fluid moves out of vessels);
4.
Hyperlipidemia/hyperlipiduria is caused by:
1) Hypoproteinemia stimulates protein synthesis in the liver,
resulting in the overproduction of lipoproteins;
2) Lipid catabolism is decreased due to lower levels of lipoprotein
lipase.
Hyperlipiduria is due to hyperlipidemia.
23.
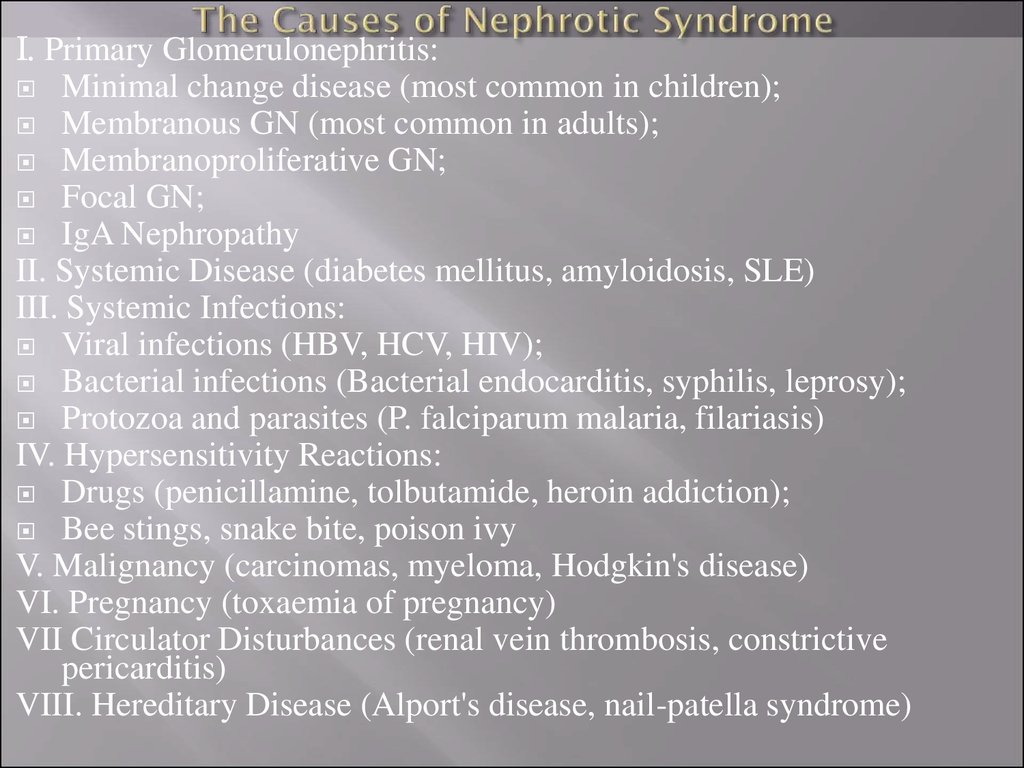
I. Primary Glomerulonephritis:Minimal change disease (most common in children);
Membranous GN (most common in adults);
Membranoproliferative GN;
Focal GN;
IgA Nephropathy
II. Systemic Disease (diabetes mellitus, amyloidosis, SLE)
III. Systemic Infections:
Viral infections (HBV, HCV, HIV);
Bacterial infections (Bacterial endocarditis, syphilis, leprosy);
Protozoa and parasites (P. falciparum malaria, filariasis)
IV. Hypersensitivity Reactions:
Drugs (penicillamine, tolbutamide, heroin addiction);
Bee stings, snake bite, poison ivy
V. Malignancy (carcinomas, myeloma, Hodgkin's disease)
VI. Pregnancy (toxaemia of pregnancy)
VII Circulator Disturbances (renal vein thrombosis, constrictive
pericarditis)
VIII. Hereditary Disease (Alport's disease, nail-patella syndrome)
24.
25.
Renal failure often refers to significant loss of renalfunction.
When less than 10% of renal function remains, this is
termed end-stage renal failure (ESRF).
Renal failure may be:
- acute as usual is reversible process;
- chronic is termed end-stage renal failure (ESRF).
Acute renal failure (ARF) is an abrupt reduction in renal
function with elevation of Blood Urea Nitrogen (BUN)
and plasma creatinine levels, usually associated with
oliguria (urine output of less than 30 ml/hr or less than 400
ml/day), although urine output may be normal or
increased.
26.
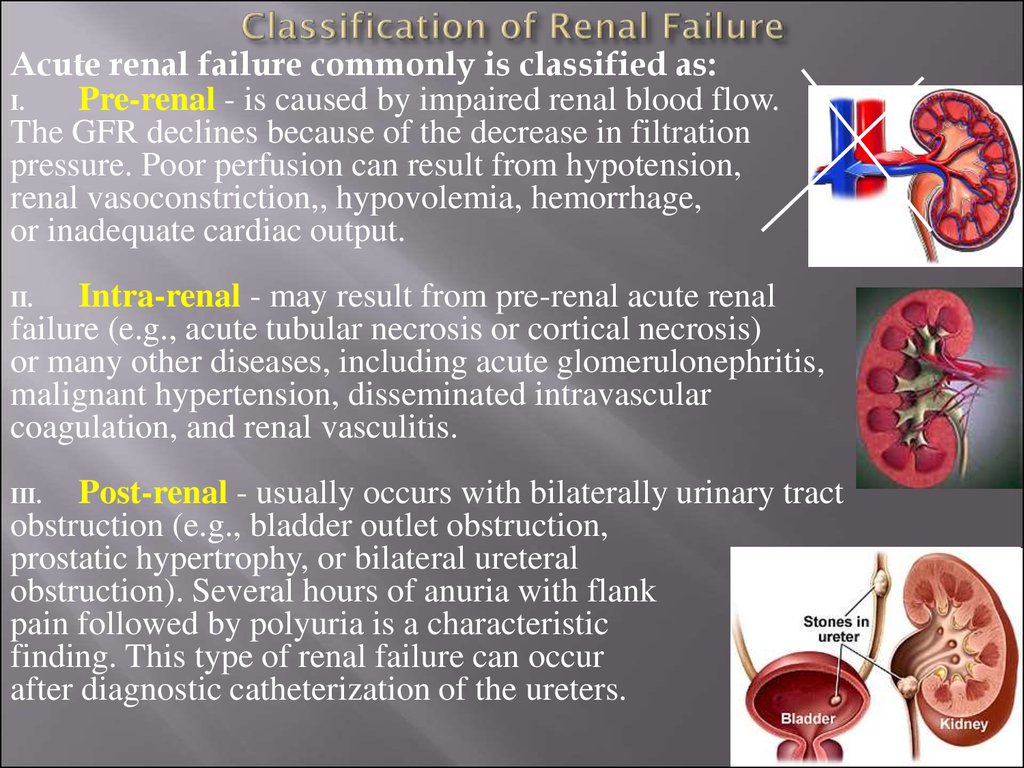
Acute renal failure commonly is classified as:I.
Pre-renal - is caused by impaired renal blood flow.
The GFR declines because of the decrease in filtration
pressure. Poor perfusion can result from hypotension,
renal vasoconstriction,, hypovolemia, hemorrhage,
or inadequate cardiac output.
Intra-renal - may result from pre-renal acute renal
failure (e.g., acute tubular necrosis or cortical necrosis)
or many other diseases, including acute glomerulonephritis,
malignant hypertension, disseminated intravascular
coagulation, and renal vasculitis.
II.
Post-renal - usually occurs with bilaterally urinary tract
obstruction (e.g., bladder outlet obstruction,
prostatic hypertrophy, or bilateral ureteral
obstruction). Several hours of anuria with flank
pain followed by polyuria is a characteristic
finding. This type of renal failure can occur
after diagnostic catheterization of the ureters.
III.
27.
Sudden onset of oliguria (urine volume 20-200 mL/day).Oliguria may not occur).
Proteinuria
Hematuria
Specific gravity of 1.010 -1.016.
Anorexia, nausea and vomiting
Lethargy
Elevation of blood pressure.
Signs of uremia: progressive increase in serum urea nitrogen,
creatinine, potassium, phosphate, sulfate; decrease in sodium,
calcium, bicarbonate.
Spontaneous recovery in a few days to 6 weeks.
28.
Pathophysiology and Clinical manifestations of Uremicsyndrome
Uremia is a syndrome of renal failure and includes
elevated blood urea and creatinine levels accompanied by
fatigue, anorexia, nausea, vomiting, pruritus, and
neurologic changes. Usually develops when the creatinine
clearance falls to less than 10 mL/min.
Azotemia means increased serum urea levels and
frequently increased creatinine levels as well. Renal failure
causes azotemia.
Both azotemia and uremia indicate an accumulation of
nitrogenous waste products in the blood.
29.
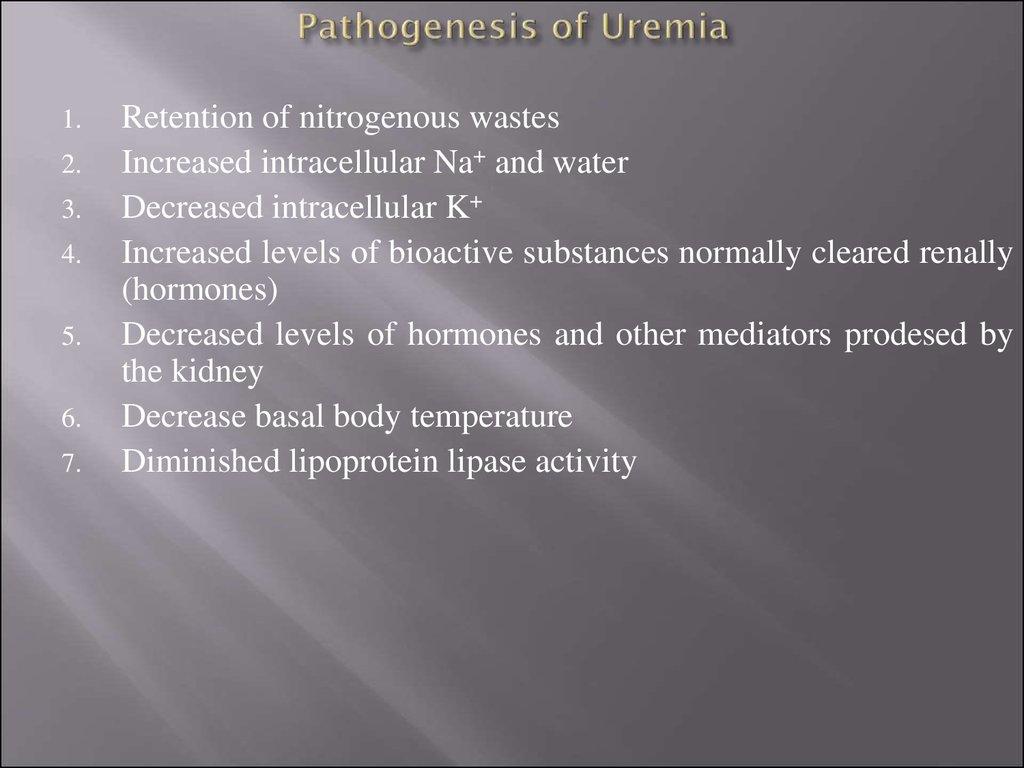
1.2.
3.
4.
5.
6.
7.
Retention of nitrogenous wastes
Increased intracellular Na+ and water
Decreased intracellular K+
Increased levels of bioactive substances normally cleared renally
(hormones)
Decreased levels of hormones and other mediators prodesed by
the kidney
Decrease basal body temperature
Diminished lipoprotein lipase activity
30.
1. Skin manifestations - pruritus, uremic "frost", skin2. Cardiac manifestations - uremic pericarditis
3. Neurological manifestations - peripheral neuropathy
4. Pulmonary complications - pneumonitis and
hemorrhage
5. Hematopoietic manifestations - anemia, bleeding
diathesis
6. Skeletal abnormalities - renal osteodystrophy
(secondary hyperparathyroidism)
7. Other metabolic imbalances
















 medicine
medicine biology
biology