Similar presentations:
Disorders of Calcium Metabolism
1. Disorders of Calcium Metabolism
Elena SegalRambam Medical Center
Haifa
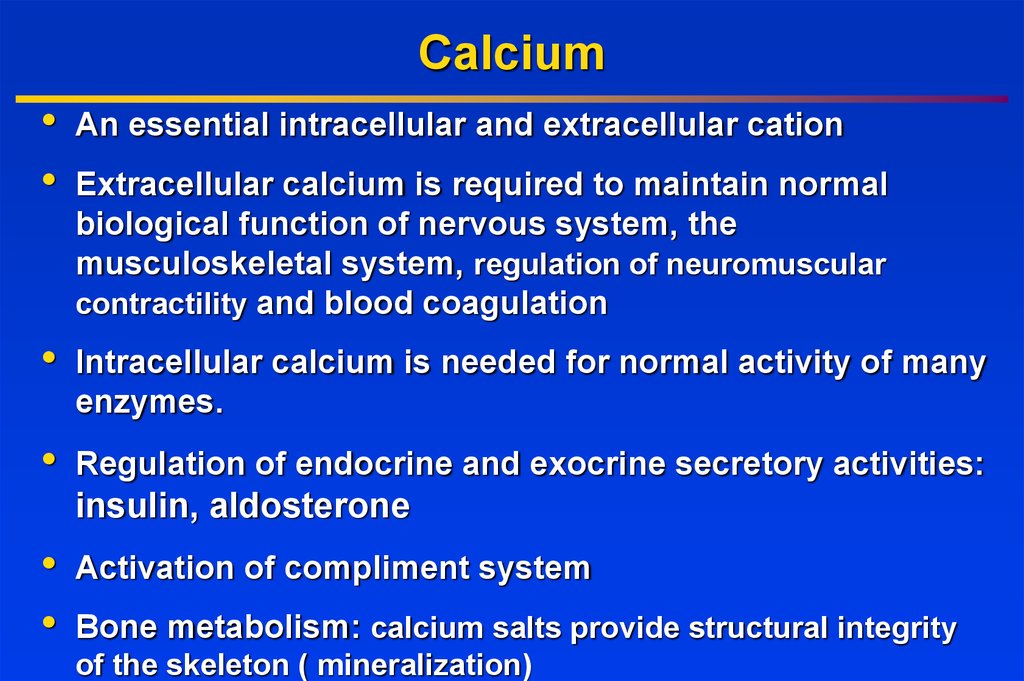
2. Calcium
An essential intracellular and extracellular cation
Extracellular calcium is required to maintain normal
biological function of nervous system, the
musculoskeletal system, regulation of neuromuscular
contractility and blood coagulation
Intracellular calcium is needed for normal activity of many
enzymes.
Regulation of endocrine and exocrine secretory activities:
insulin, aldosterone
Activation of compliment system
Bone metabolism: calcium salts provide structural integrity
of the skeleton ( mineralization)
3.
ECFDiet 0.5-1.5 gr
10%
complexed
citrate, sulphate
Resorption
0.3-0.5 g
Formation
0.3-0.5 g
calcium
8.5–10.5
mg/dl
Bone
1000 g
Filtration
5-7gr
40-45 % Absorption
ionized 0.25-0.5gr
40-45 %
albumin
bound
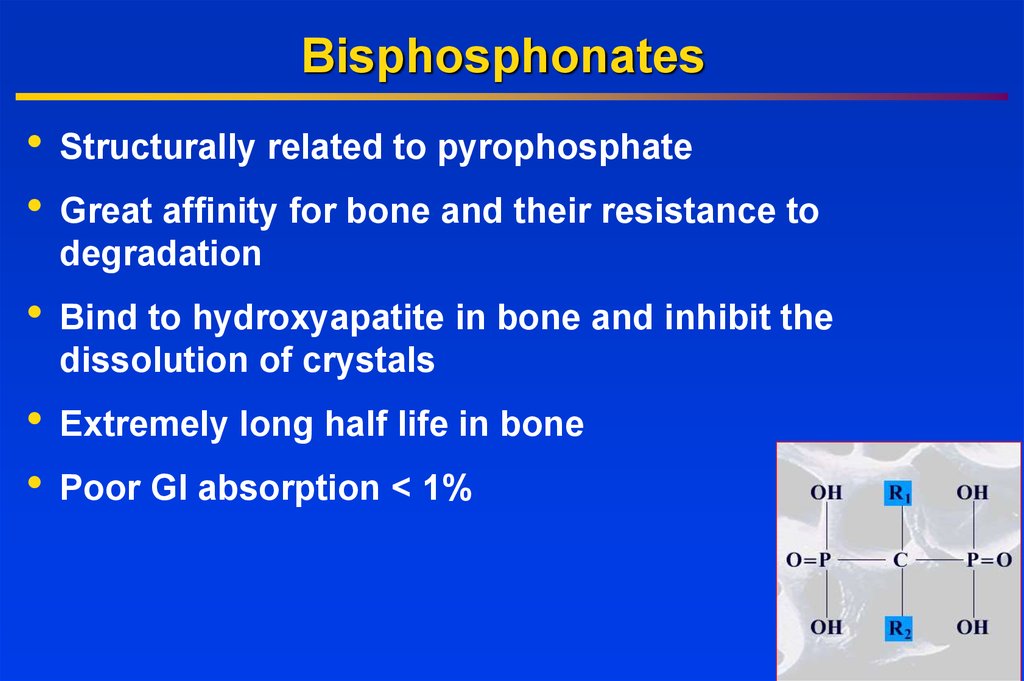
Secretion
0.1-0.2gr
Feces
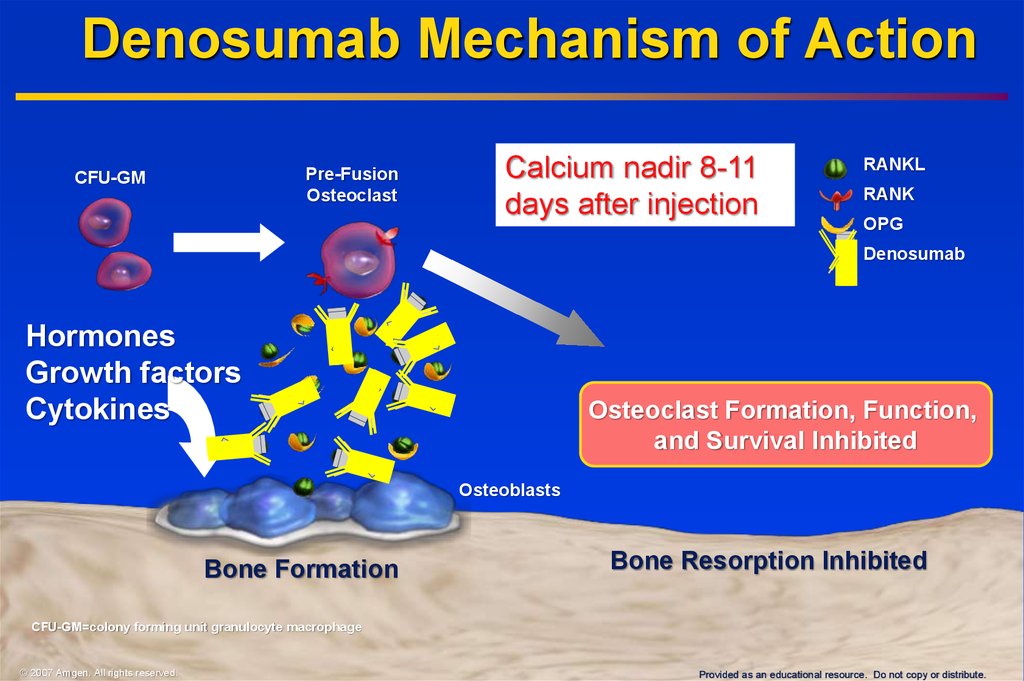
0.35-0.6gr
• Total body Ca
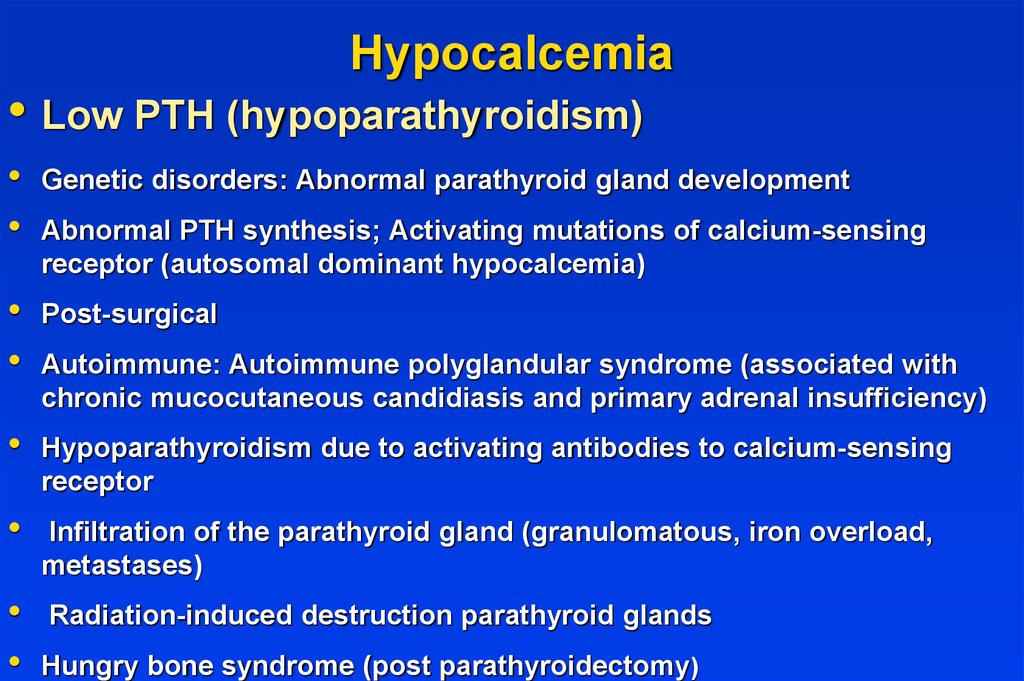
Reabsorption
1 to 1.5 kg
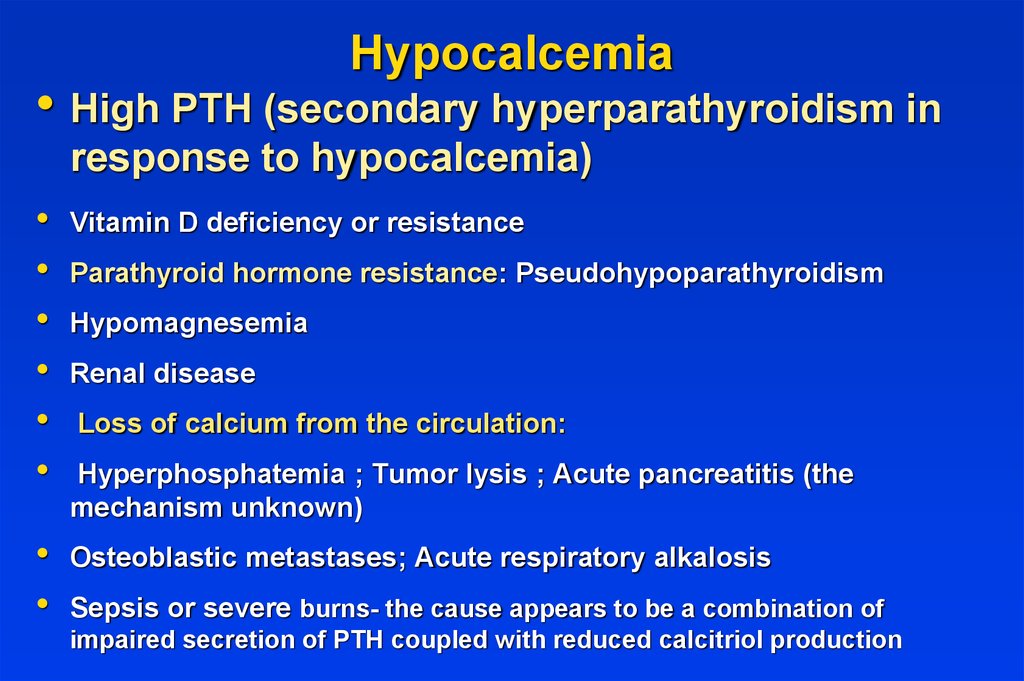
4.9-6.7gr
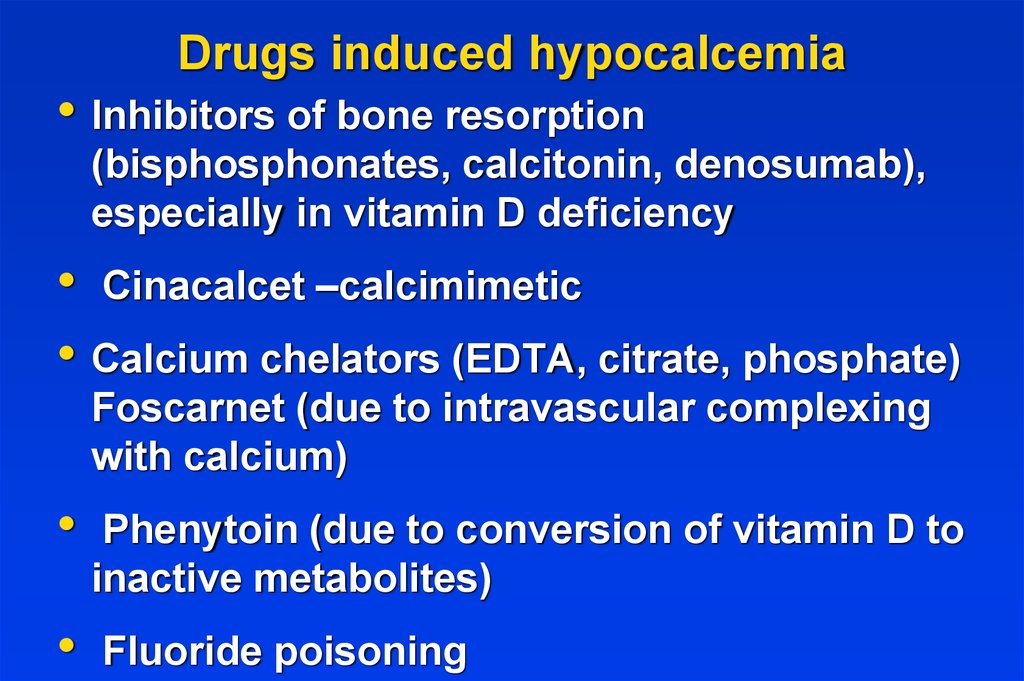
• 99%- skeleton
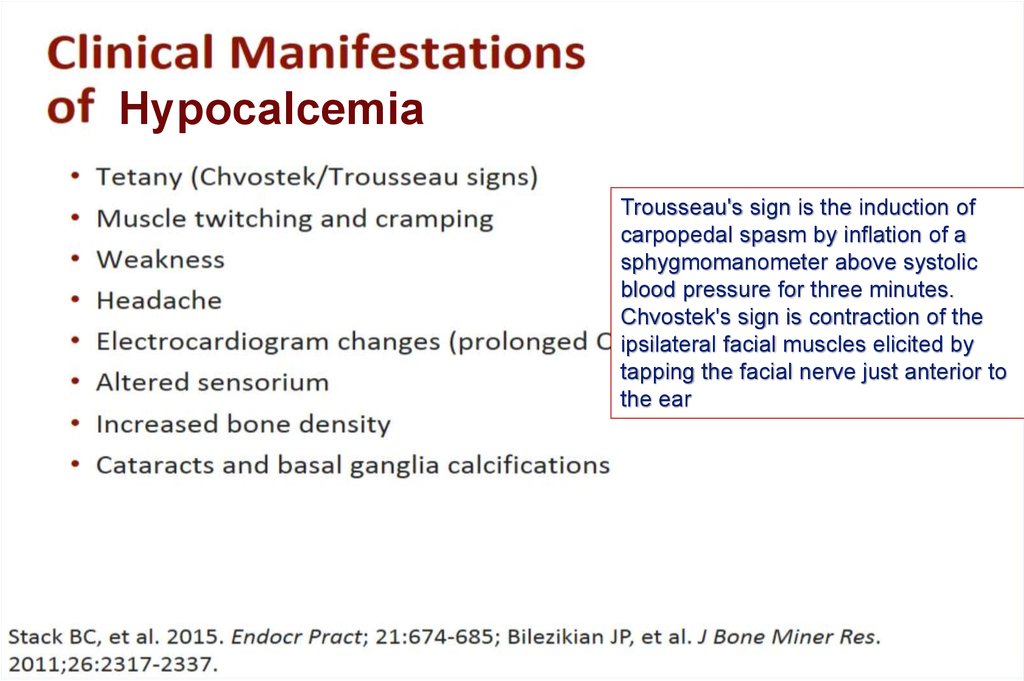
98%
• 0.1% ECF
0.15-0.3 g/24h • rest intracellular
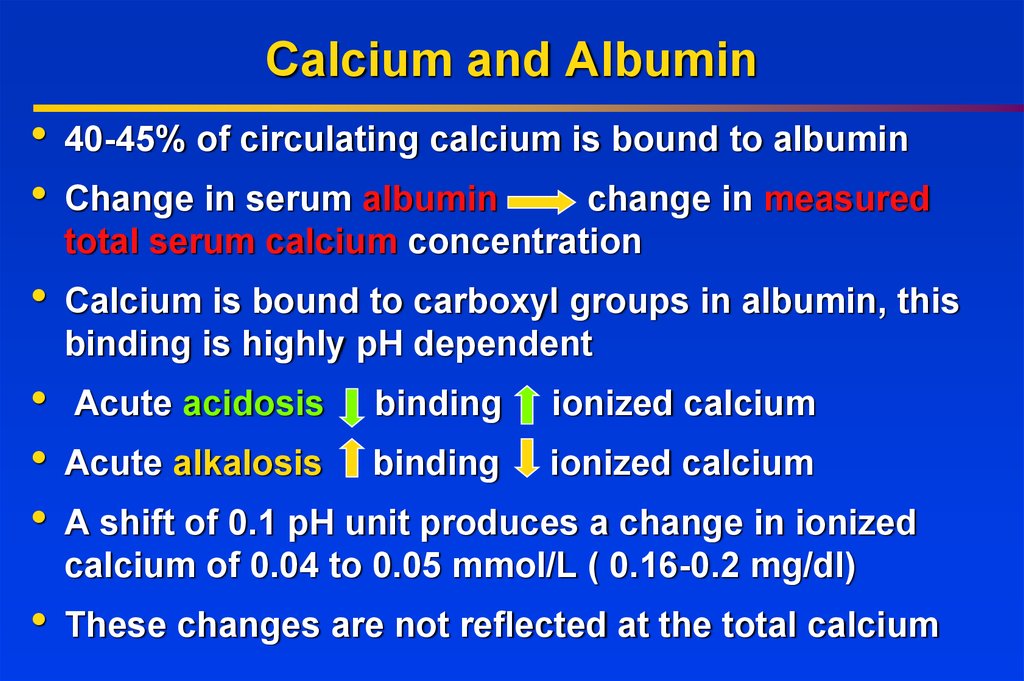
4. Calcium and Albumin
40-45% of circulating calcium is bound to albumin
Change in serum albumin
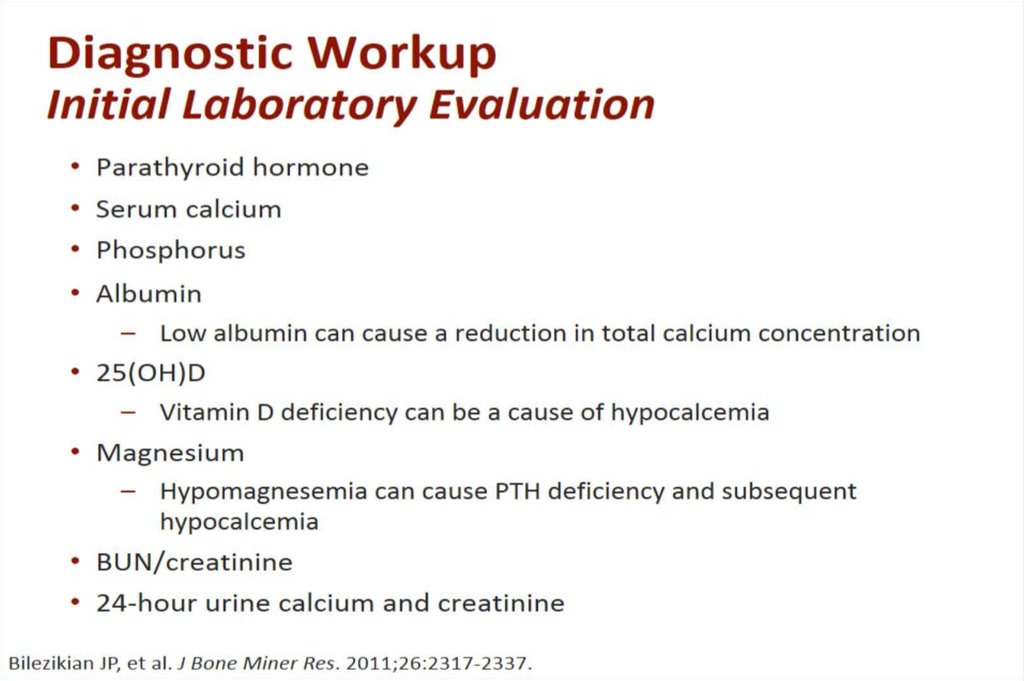
change in measured
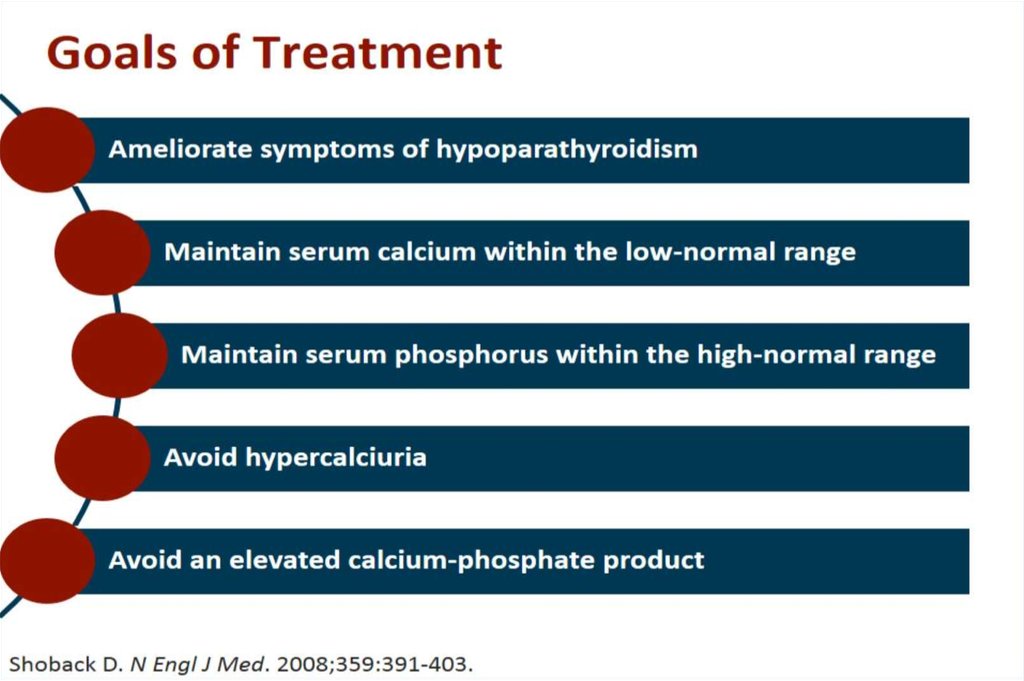
total serum calcium concentration
Calcium is bound to carboxyl groups in albumin, this
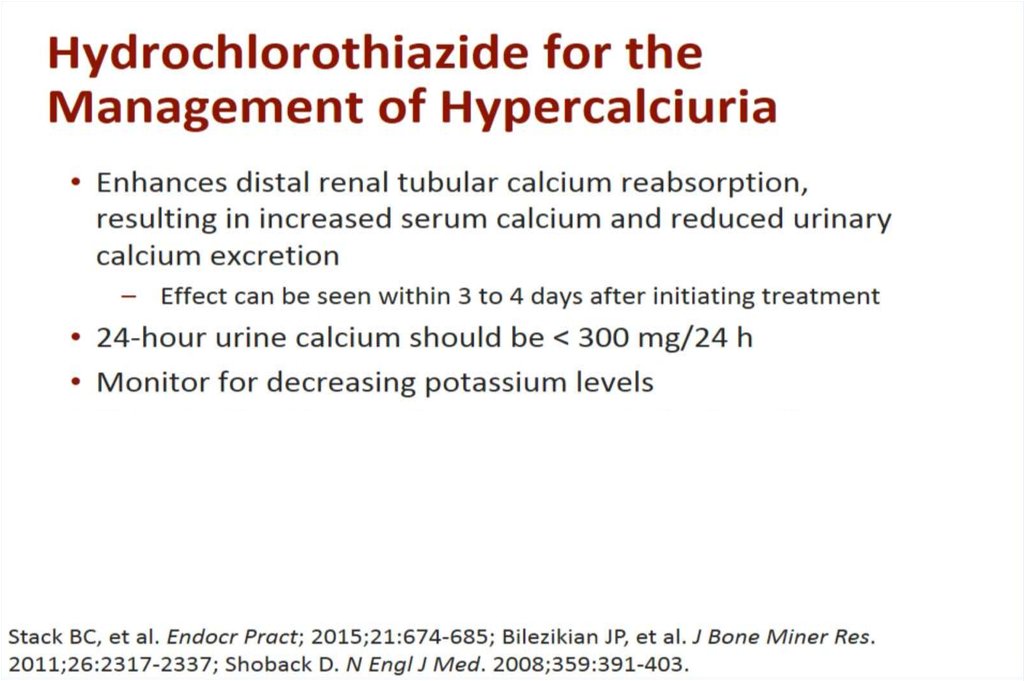
binding is highly pH dependent
Acute acidosis
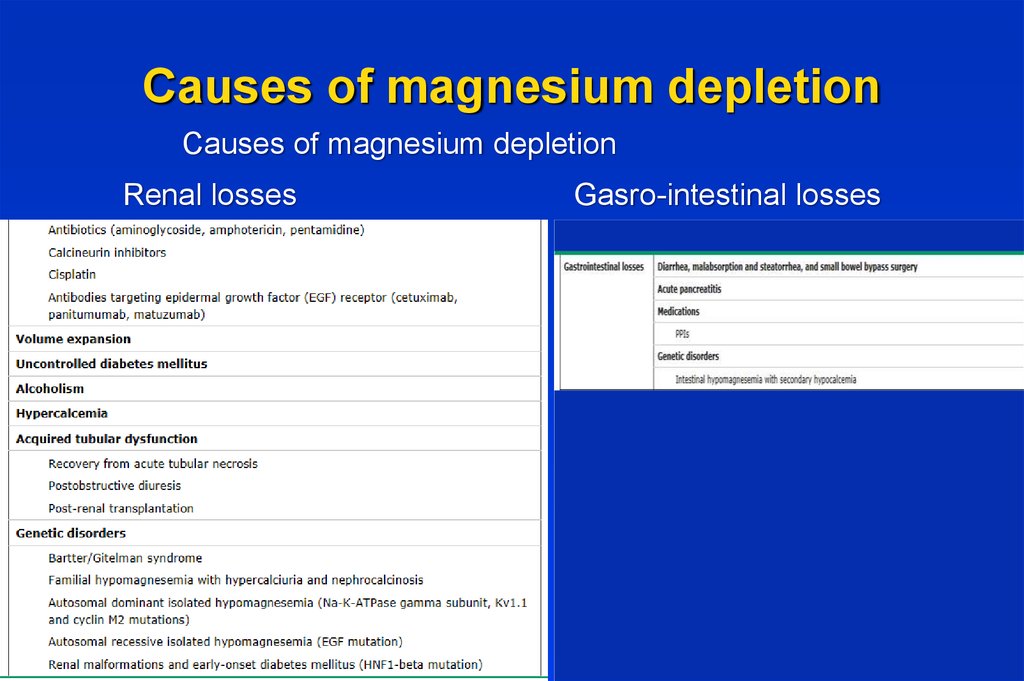
binding
ionized calcium
Acute alkalosis
binding
ionized calcium
These changes are not reflected at the total calcium
A shift of 0.1 pH unit produces a change in ionized
calcium of 0.04 to 0.05 mmol/L ( 0.16-0.2 mg/dl)
5. Calcium and Albumin
At pH 7.4 each g/dl of serum albumin binds 0.8 mg/dl of
calcium
Serum calcium should be “corrected” according to
serum albumin level
Normal level of serum albumin is 4 g/dl
Change of 1 g/dl in serum albumin
serum calcium
0.8 mg/dl in total
Example: A patient with total serum calcium 7.5 mg/dl
albumin 2 g/dl, has corrected serum calcium of 9.1
mg/dl
Ca = SerumCa + 0.8 * (NormalAlbumin - PatientAlbumin)
6. Disorders of Calcium Metabolism
• Hypercalcemia• Hypocalcemia
Serum Calcium >10.4 mg/dl
Serum Calcium < 8.5 mg/dl
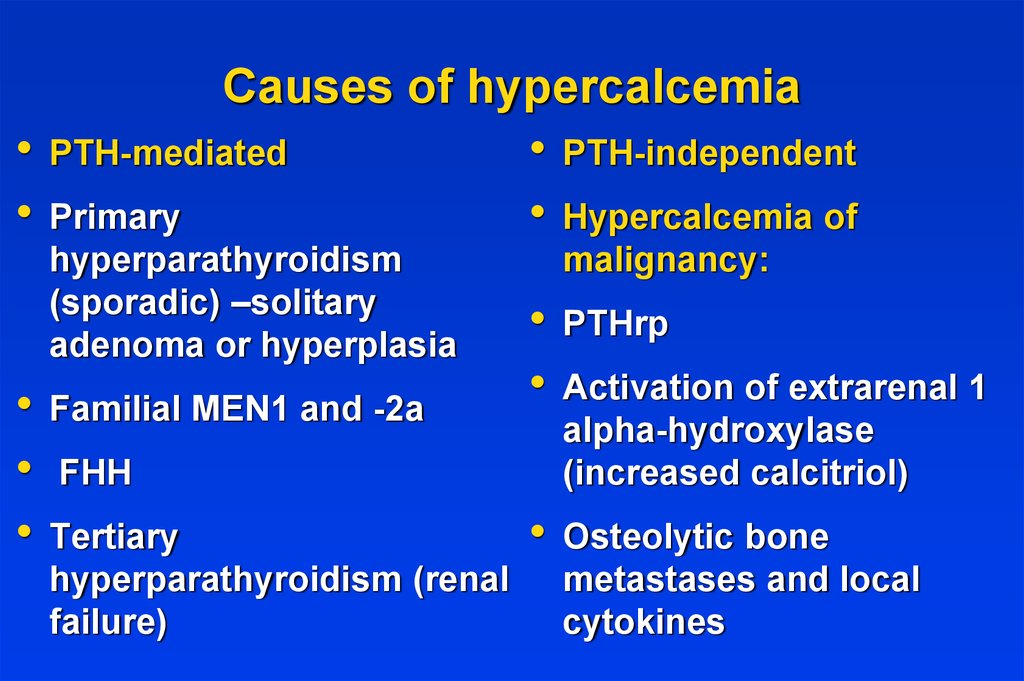
7. Causes of hypercalcemia
• PTH-mediated• PTH-independent
• Primary
• Hypercalcemia of
hyperparathyroidism
(sporadic) –solitary
adenoma or hyperplasia
Familial MEN1 and -2a
malignancy:
FHH
Tertiary
hyperparathyroidism (renal
failure)
PTHrp
Activation of extrarenal 1
alpha-hydroxylase
(increased calcitriol)
Osteolytic bone
metastases and local
cytokines
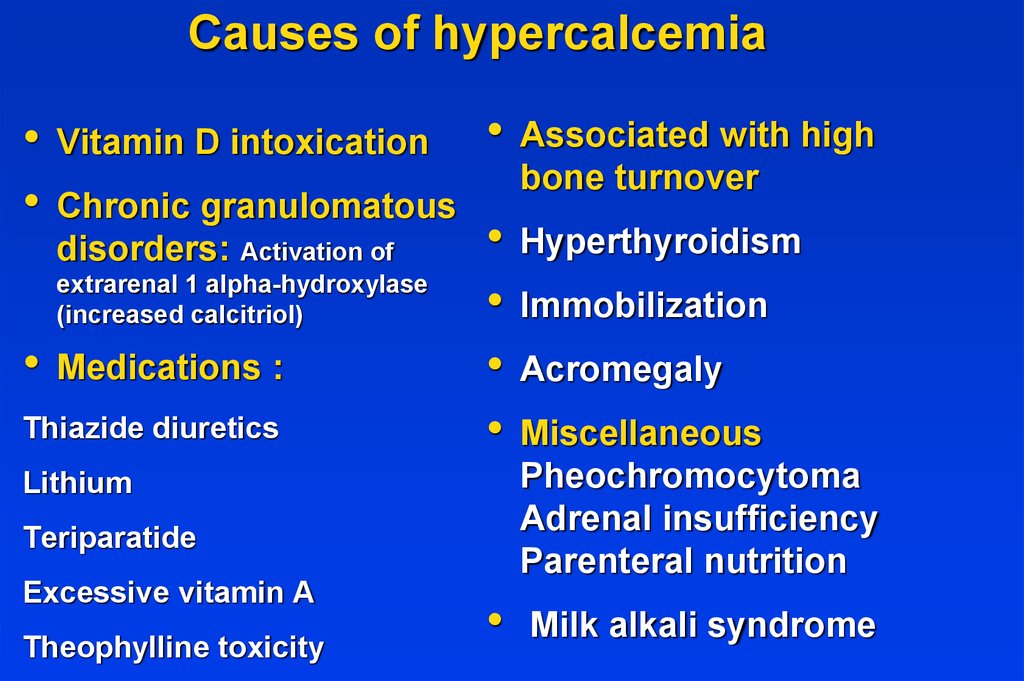
8. Causes of hypercalcemia
Vitamin D intoxication
Chronic granulomatous
disorders: Activation of
extrarenal 1 alpha-hydroxylase
(increased calcitriol)
Medications :
Thiazide diuretics
Lithium
Teriparatide
Excessive vitamin A
Theophylline toxicity
Associated with high
bone turnover
Hyperthyroidism
Immobilization
Acromegaly
Miscellaneous
Pheochromocytoma
Adrenal insufficiency
Parenteral nutrition
Milk alkali syndrome
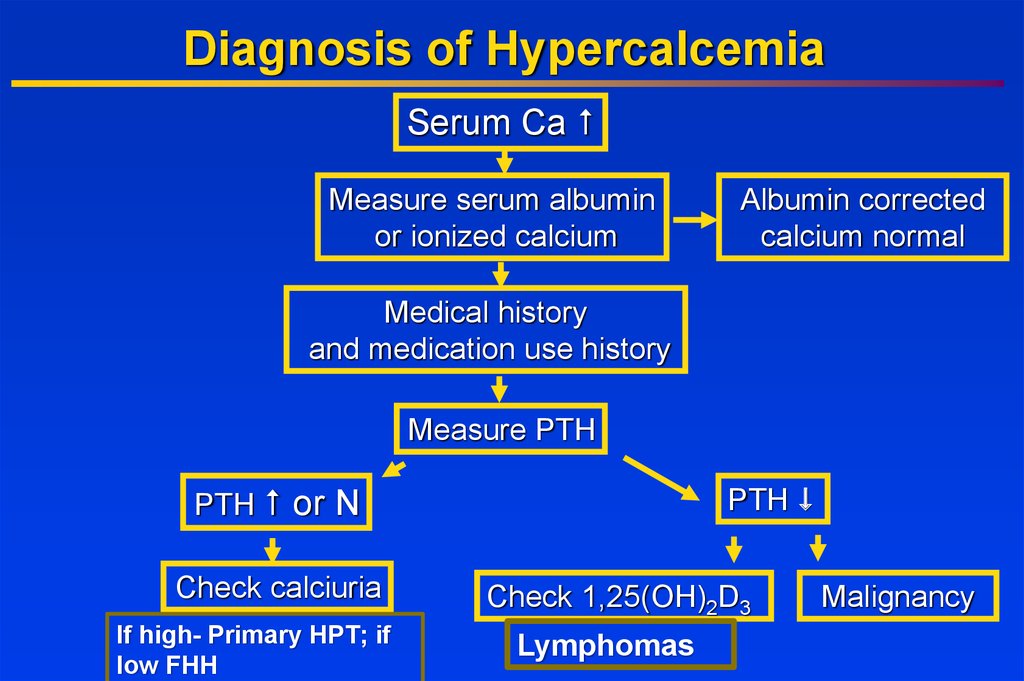
9. Diagnosis of Hypercalcemia
Serum CaMeasure serum albumin
or ionized calcium
Albumin corrected
calcium normal
Medical history
and medication use history
Measure PTH
PTH
PTH or N
Check calciuria
If high- Primary HPT; if
low FHH
Check 1,25(OH)2D3
Lymphomas
Malignancy
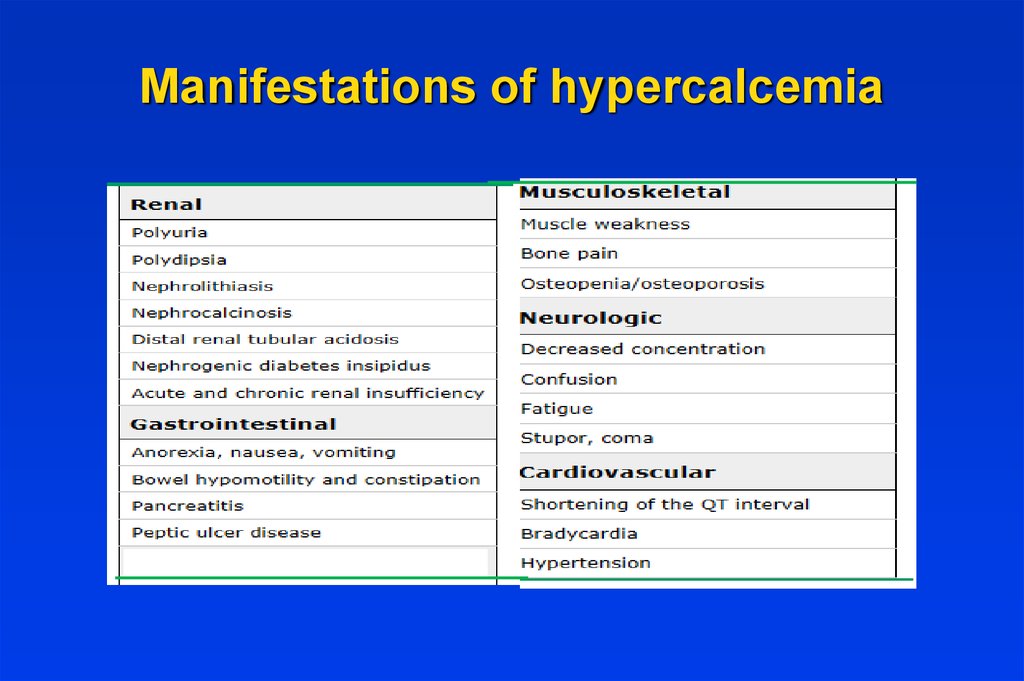
10. Manifestations of hypercalcemia
11. Renal manifestations
The most important renal manifestations are polyuria,
resulting from decreased concentrating ability in the
distal tubule, nephrolithiasis, and acute and chronic
renal insufficiency.
Nephrogenic diabetes insipidus — Chronic
hypercalcemia leads to a defect in concentrating ability
that may induce polyuria and polydipsia in up to 20
percent of patients. The mechanism is incompletely
understood, but the downregulation of aquaporin-2 water
channels receptors, and calcium deposition in the
medulla with secondary tubulointerstitial injury and
impaired generation of the interstitial osmotic gradient
may play important roles.
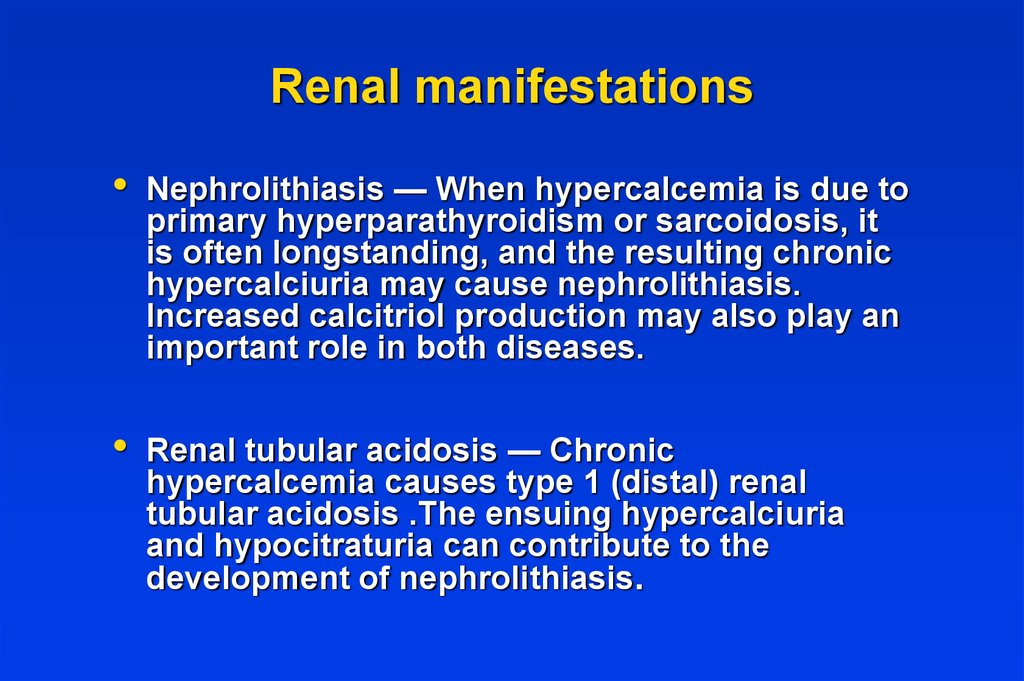
12. Renal manifestations
Nephrolithiasis — When hypercalcemia is due to
primary hyperparathyroidism or sarcoidosis, it
is often longstanding, and the resulting chronic
hypercalciuria may cause nephrolithiasis.
Increased calcitriol production may also play an
important role in both diseases.
Renal tubular acidosis — Chronic
hypercalcemia causes type 1 (distal) renal
tubular acidosis .The ensuing hypercalciuria
and hypocitraturia can contribute to the
development of nephrolithiasis.
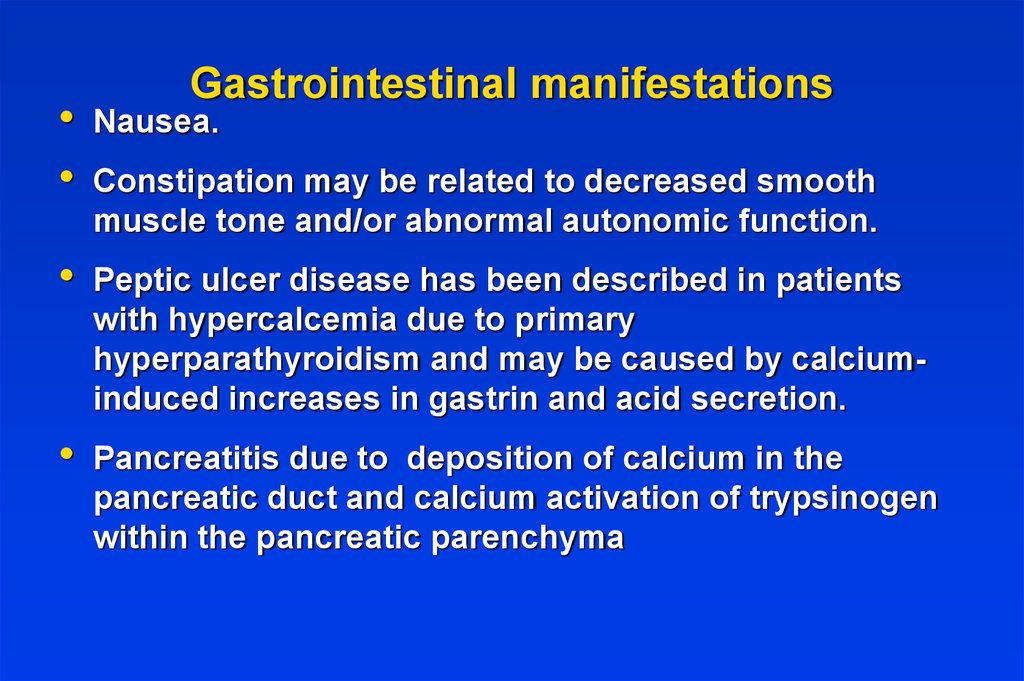
13. Gastrointestinal manifestations
Gastrointestinal manifestations
Nausea.
Constipation may be related to decreased smooth
muscle tone and/or abnormal autonomic function.
Peptic ulcer disease has been described in patients
with hypercalcemia due to primary
hyperparathyroidism and may be caused by calciuminduced increases in gastrin and acid secretion.
Pancreatitis due to deposition of calcium in the
pancreatic duct and calcium activation of trypsinogen
within the pancreatic parenchyma
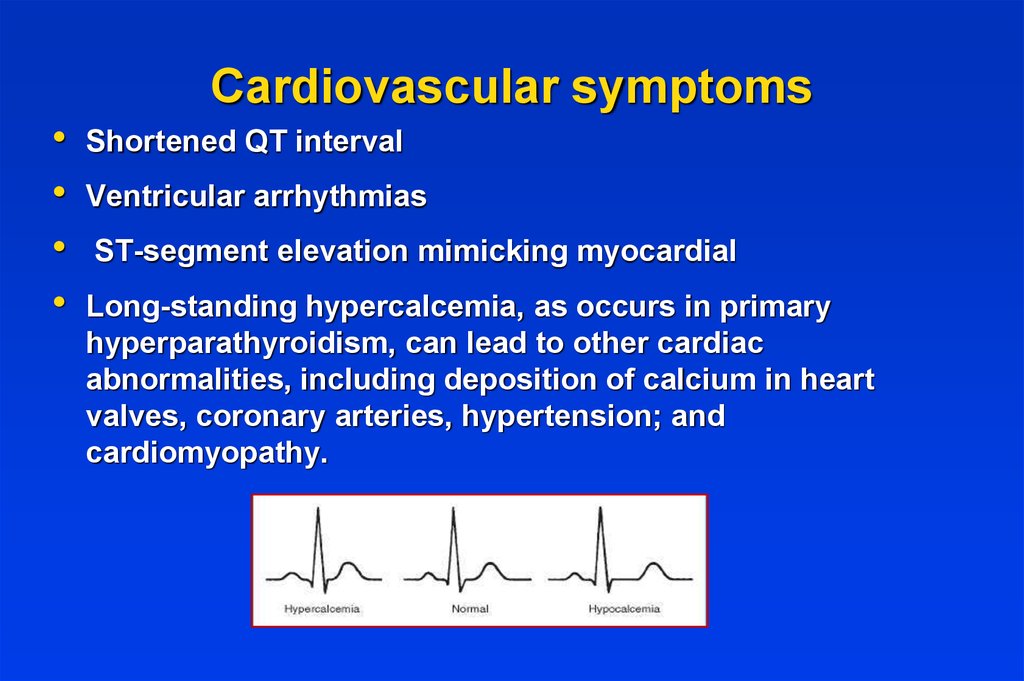
14. Cardiovascular symptoms
Shortened QT interval
Ventricular arrhythmias
ST-segment elevation mimicking myocardial
Long-standing hypercalcemia, as occurs in primary
hyperparathyroidism, can lead to other cardiac
abnormalities, including deposition of calcium in heart
valves, coronary arteries, hypertension; and
cardiomyopathy.
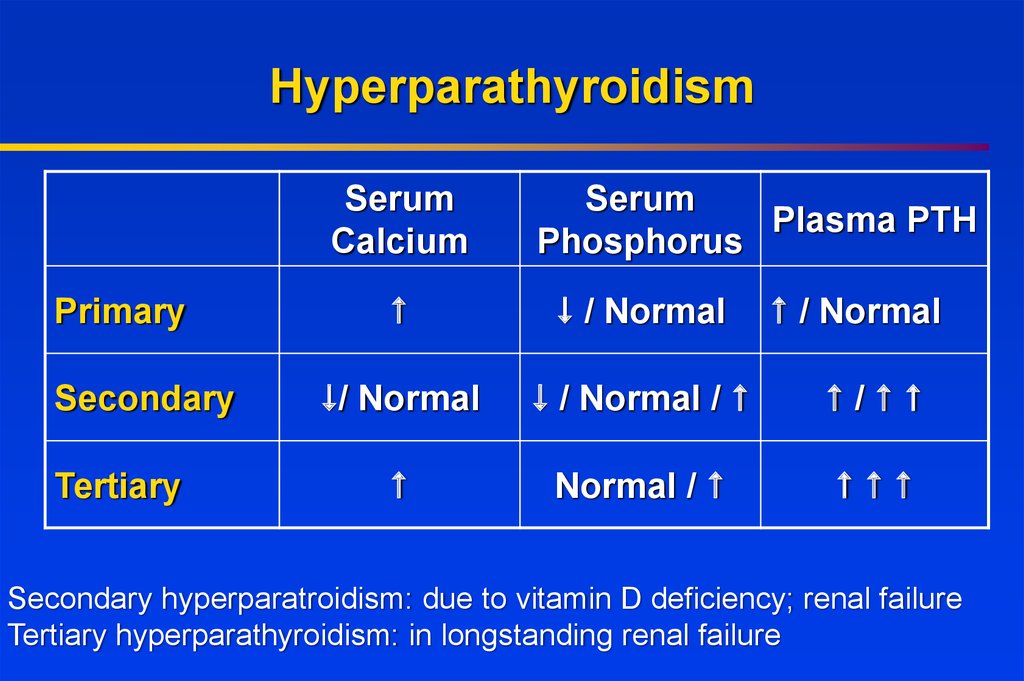
15. Hyperparathyroidism
SerumCalcium
Primary
Secondary
Tertiary
Serum
Plasma PTH
Phosphorus
/ Normal
/ Normal
/ Normal
/ Normal /
/
Normal /
Secondary hyperparatroidism: due to vitamin D deficiency; renal failure
Tertiary hyperparathyroidism: in longstanding renal failure
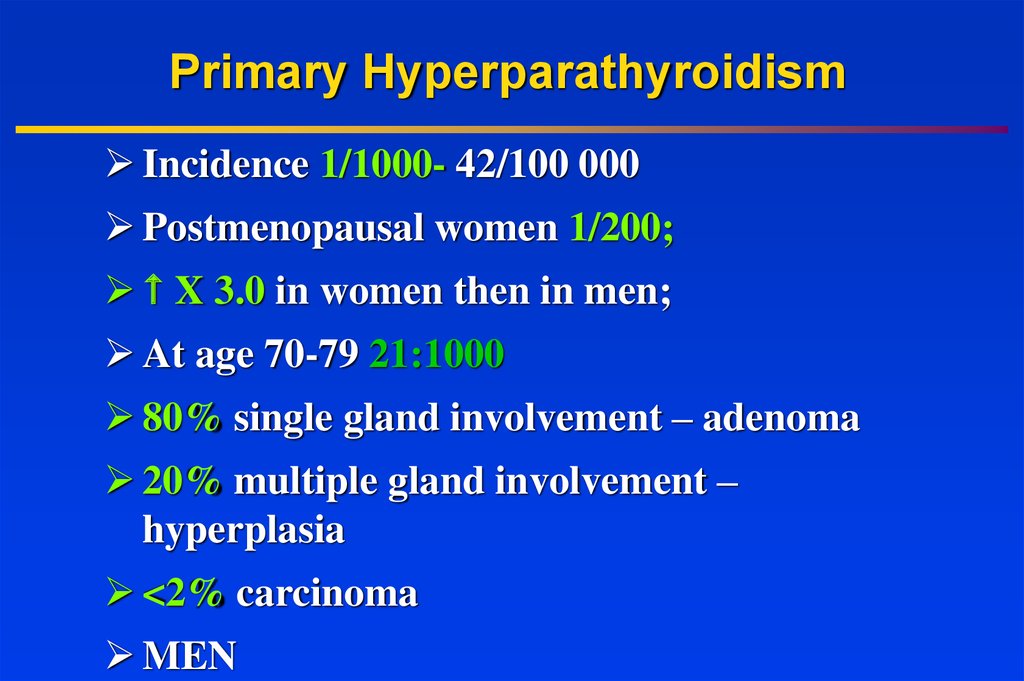
16. Primary Hyperparathyroidism
Incidence 1/1000- 42/100 000Postmenopausal women 1/200;
X 3.0 in women then in men;
At age 70-79 21:1000
80% single gland involvement – adenoma
20% multiple gland involvement –
hyperplasia
<2% carcinoma
MEN
17.
or multiple adenomas,nearly 100%
15-20%
up to 60%
nearly
100%
30-100%
1025%
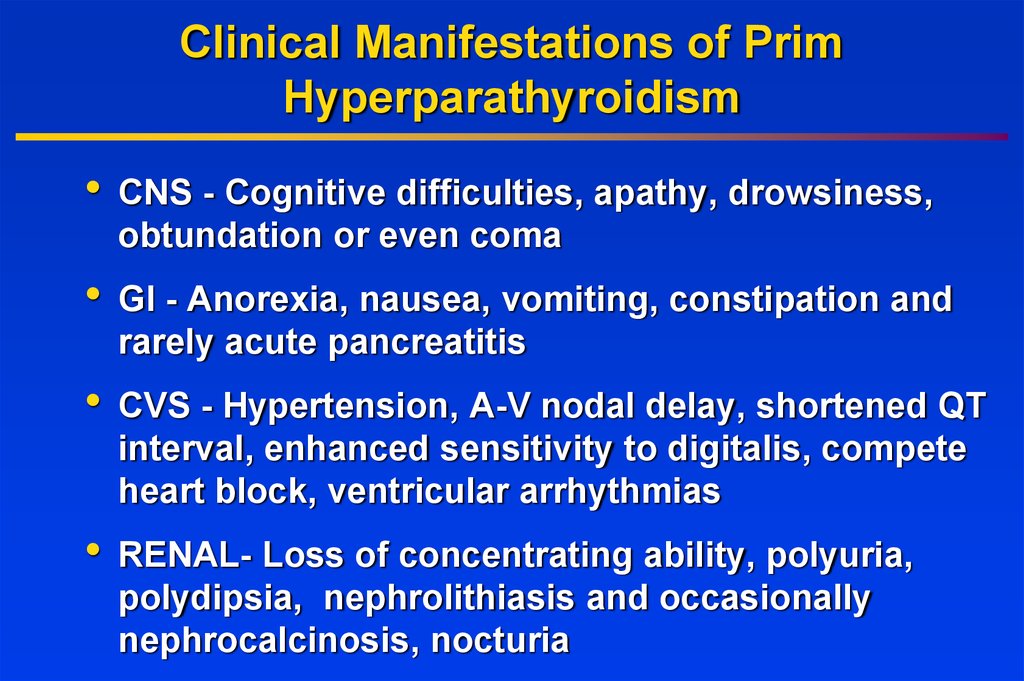
18. Clinical Manifestations of Prim Hyperparathyroidism
CNS - Cognitive difficulties, apathy, drowsiness,
obtundation or even coma
GI - Anorexia, nausea, vomiting, constipation and
rarely acute pancreatitis
CVS - Hypertension, A-V nodal delay, shortened QT
interval, enhanced sensitivity to digitalis, compete
heart block, ventricular arrhythmias
RENAL- Loss of concentrating ability, polyuria,
polydipsia, nephrolithiasis and occasionally
nephrocalcinosis, nocturia
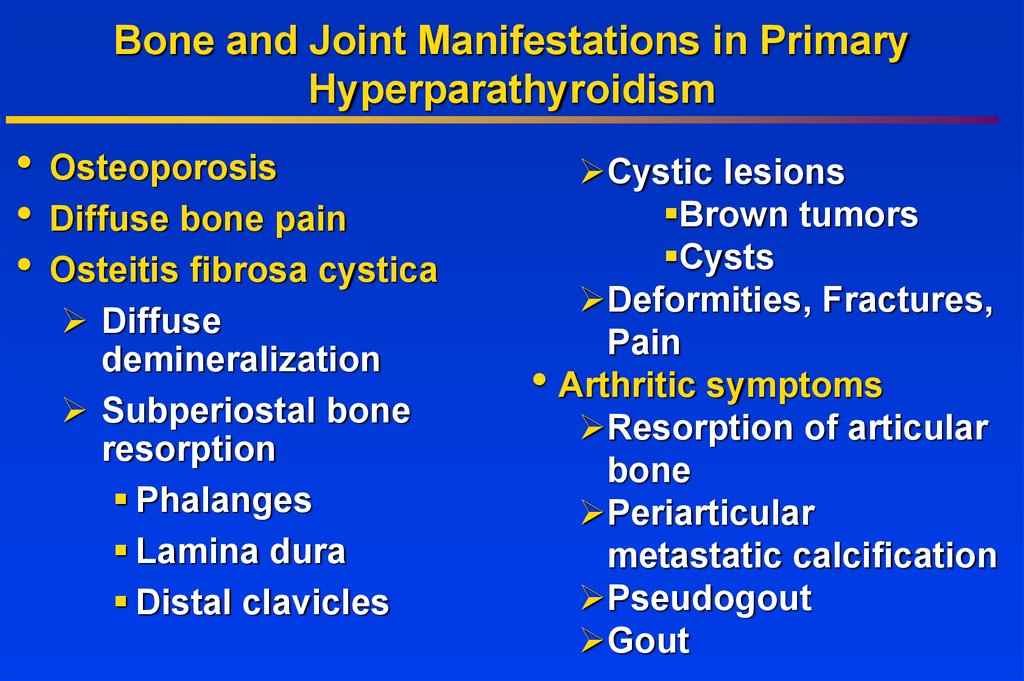
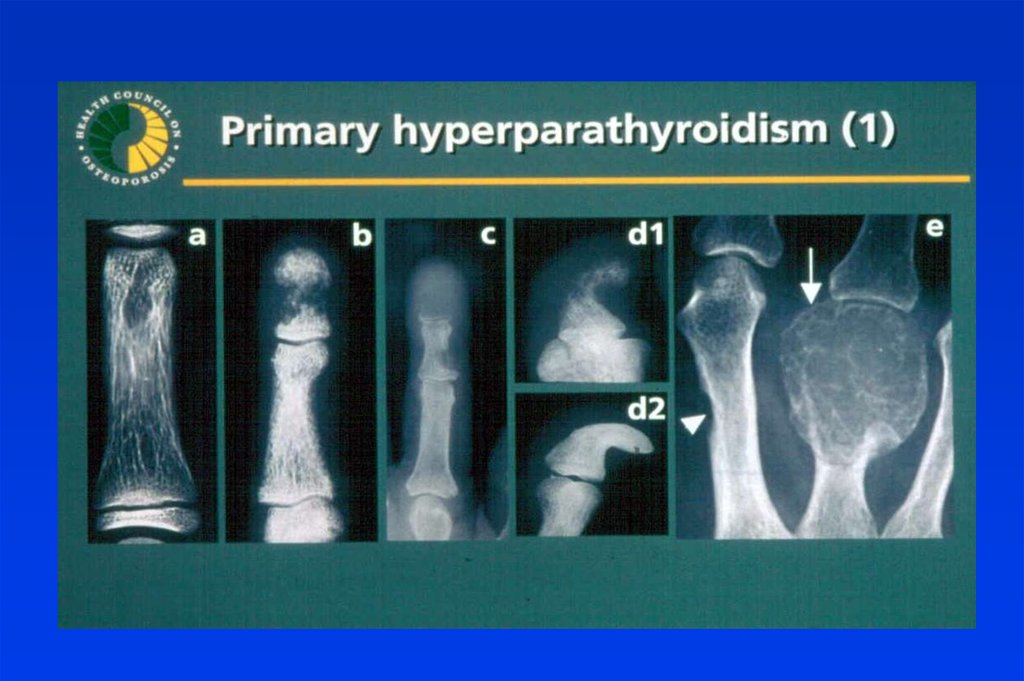
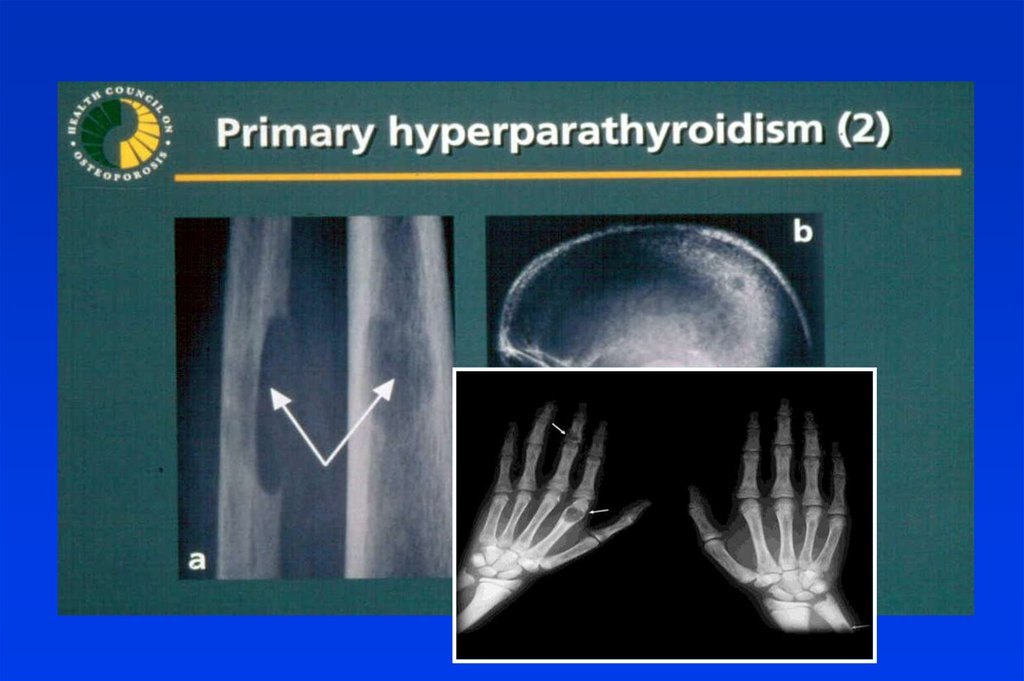
19. Bone and Joint Manifestations in Primary Hyperparathyroidism
Osteoporosis
Diffuse bone pain
Osteitis fibrosa cystica
Diffuse
demineralization
Subperiostal bone
resorption
Phalanges
Lamina dura
Distal clavicles
Cystic lesions
Brown tumors
Cysts
Deformities, Fractures,
Pain
Arthritic symptoms
Resorption of articular
bone
Periarticular
metastatic calcification
Pseudogout
Gout
20.
21.
22. Treatment
When is surgery indicated in PHPT patients?
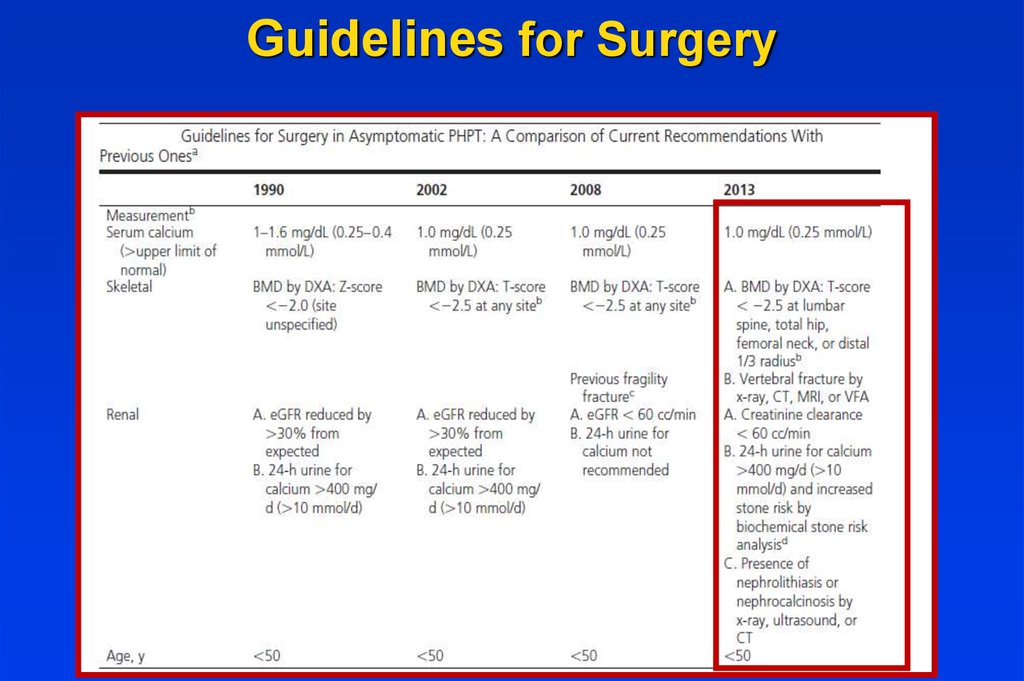
23. Guidelines for Surgery
24. Other Considerations
• Neuropsychological disturbances• Weakness and easy fatigability
• Depression
• Intellectual weariness
• Increased sleep requirements
Improved by surgery
• Onset of Menopause
• Increased bone loss
25. US in the diagnosis of PTA
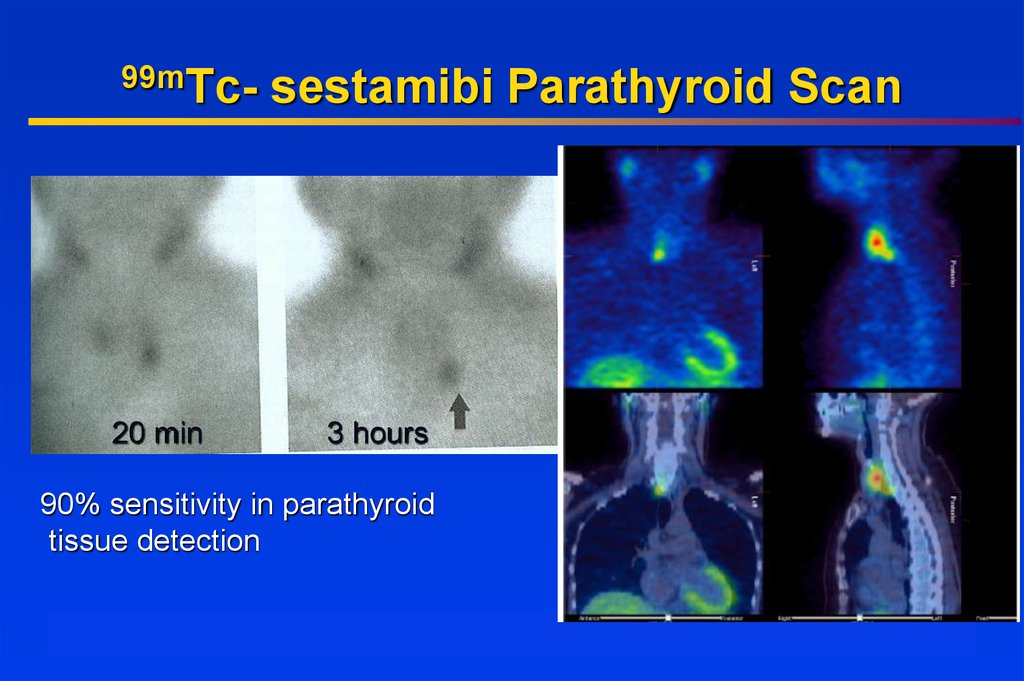
26. 99mTc- sestamibi Parathyroid Scan
99mTc-20 min
sestamibi Parathyroid Scan
3 hours
90% sensitivity in parathyroid
tissue detection
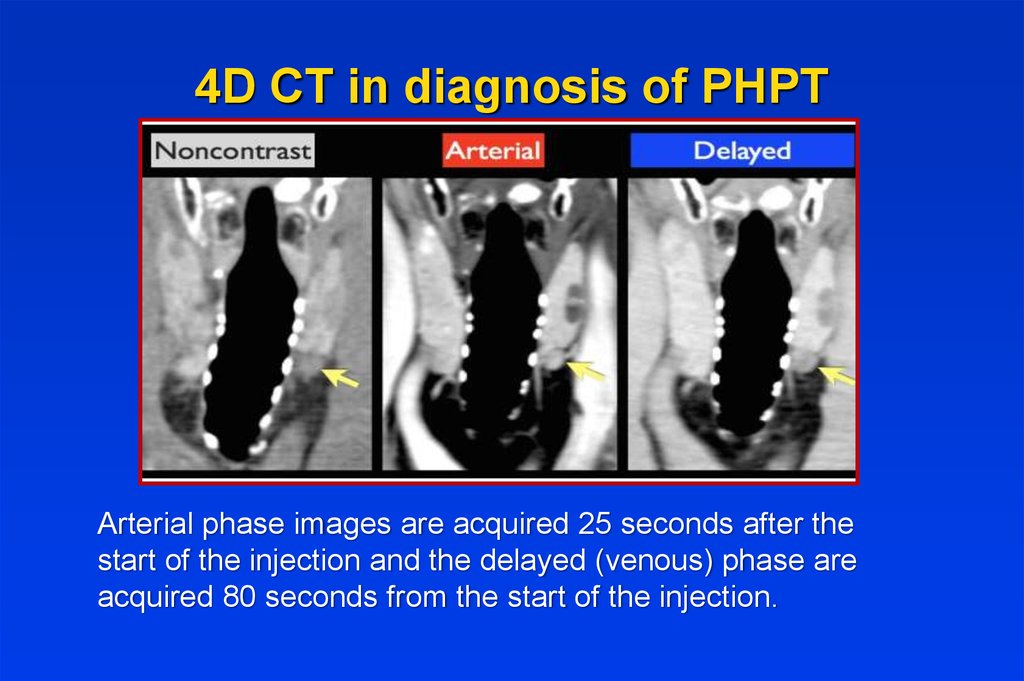
27. What is 4D-CT?
4D CT in diagnosis of PHPTArterial phase images are acquired 25 seconds after the
start of the injection and the delayed (venous) phase are
acquired 80 seconds from the start of the injection.
28. 4D CT in diagnosis of PHPT
Patients who weren‘t operatedMonitoring guidelines29. Patients who weren‘t operated- Monitoring guidelines
General Measures• Hydration
• Adequate Mobility
• Diet neither restrictive nor excessive in
calcium
• Adequate vitamin D status
• Prompt medical attention for the possibility of
worsening of hypercalcemia (intercurrent
illness accompanied by risk of dehydration)
30. General Measures
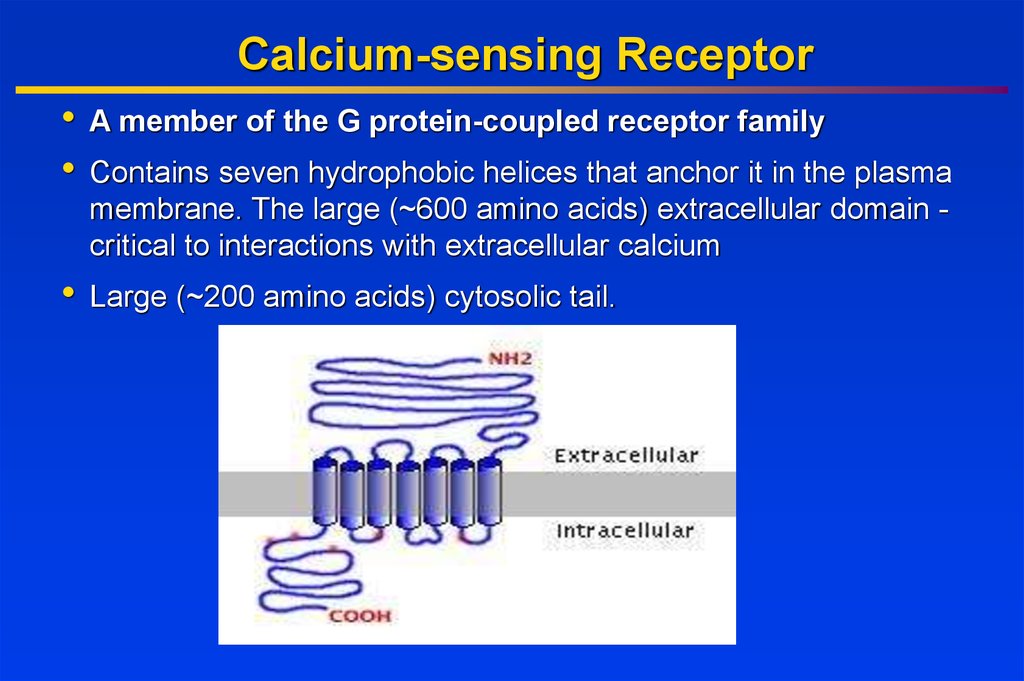
Calcium-sensing ReceptorA member of the G protein-coupled receptor family
Contains seven hydrophobic helices that anchor it in the plasma
membrane. The large (~600 amino acids) extracellular domain critical to interactions with extracellular calcium
Large (~200 amino acids) cytosolic tail.
31. Calcium-sensing Receptor
Inactivating Mutations in CalciumSensing Receptor
Inactivating mutation
– Familial hypocalciuric
hypercalcemia
(FHH)
No need for
parathyroid surgery
in FHH!!
heterozygous
Calcium set point
serum calcium
Urinary calcium reabsorption
urinary
calcium
– Neonatal severe hyperparathyroidism (NSHPT) –
homozygous
homozygous-incompatible
with life if not resect
the parathyroid
parathyroid
32. Inactivating Mutations in Calcium Sensing Receptor
Hypercalcemia of MalignancyLung, breast, and prostate cancer frequently invade
skeleton and destroy bone tissue
Damage to skeleton usually late in course of disease
Bone damage associated with considerable worsening
in patient’s quality of life
Multiple myeloma has skeletal complications in
virtually 100% of cases
Breast and lung cancer also cause hypercalcemia of
malignancy, without invading skeleton
33. Hypercalcemia of Malignancy
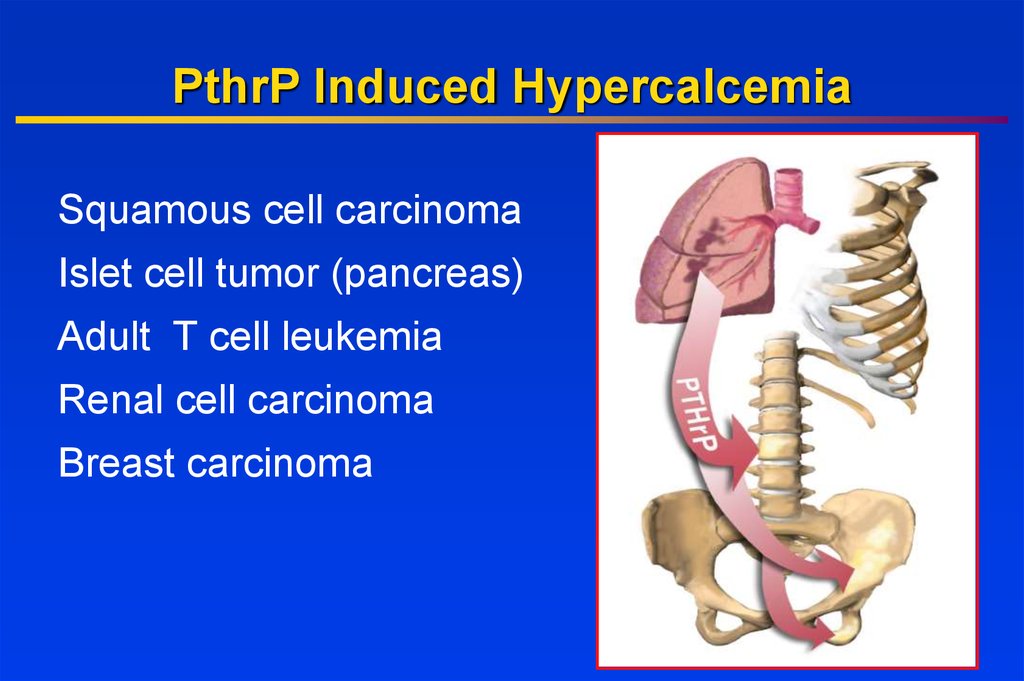
PthrP Induced HypercalcemiaSquamous cell carcinoma
Islet cell tumor (pancreas)
Adult T cell leukemia
Renal cell carcinoma
Breast carcinoma
34. PthrP Induced Hypercalcemia
PTHrP-PTH related peptide• Gen located on the chromosome 12
• Gen is expressed in the embrional tissues: cartilage,
heart, epithelium, hear bulbs
Expression of the PTHrP gen in adult: plays role in
breast development; presents in breast milk in high
concentration
Mutation in embryo:
Heterozygous are normal
Homozygous –lethal mutation with major bone and
cartilage abnormalities
35. PTHrP-PTH related peptide
TreatmentHydration
Bisphosphonates IV,
Denosumab
Calcitonin
Glucocorticoids
Dialysis
36. Treatment
HydrationFirst step in the management of severe
hypercalcemia - Isotonic saline
Usually serum calcium by 1.6-2.4mg/dl
Hydration alone rarely leads to normalization in
severe hypercalcemia
Rate of IV saline based on severity of
hypercalcemia and tolerance of CVS for volume
expansion, if possible achieve urine output of
300 ml/hr, that is then adjusted to maintain the
urine output at 100 to 150 mL/hour.
37. Hydration
Loop DiureticsIn the past intensive administration of
furosemide was used (80 to 100 mg every one to
two hours).
It needs aggressive fluid hydration (10 liters
daily), saline therapy beyond that necessary to
restore euvolemia.
Now use of calcitonin and bisphosphonates is
more effective.
38. Loop Diuretics
Calcitonin• The efficacy of calcitonin (4 IU/kg every
6-12 hours) is limited to the first 48
hours, due to development of
tachyphylaxis, perhaps due to receptor
downregulation .
• Calcitonin and hydration provide a
rapid reduction in serum calcium
concentration, while a bisphosphonate
provides a more sustained effect.
39. Calcitonin
BisphosphonatesStructurally related to pyrophosphate
Great affinity for bone and their resistance to
degradation
Bind to hydroxyapatite in bone and inhibit the
dissolution of crystals
Extremely long half life in bone
Poor GI absorption < 1%
40. Bisphosphonates
Zoledronic Acid (ZOMERA)• Zoledronic acid belongs to a new class of highly
potent bisphosphonates
The calcium levels in 72 hours after
the infusion.
Heterocyclic,
nitrogen-containing bisphosphonate
single dose of ZA 4 mg normalizes
composedAof:
the corrected serum calcium
• A core bisphosphonate
moiety
concentration 88% percent of patients,
• An imidazole-ring side chain containing 2 critically positioned
the median duration of serum calcium
nitrogen atoms
control lasts 32
to 43 days.
OH
O
N
P
N
OH
O
OH
P
HO
OH
41. Zoledronic Acid (ZOMERA)
Denosumab Mechanism of ActionPre-Fusion
Osteoclast
CFU-GM
Calcium nadir 8-11
days after injection
RANKL
RANK
OPG
Denosumab
Hormones
Growth factors
Cytokines
Osteoclast Formation, Function,
and Survival Inhibited
Osteoblasts
Bone Formation
Bone Resorption Inhibited
CFU-GM=colony forming unit granulocyte macrophage
© 2007 Amgen. All rights reserved.
Provided as an educational resource. Do not copy or distribute.
42. Denosumab Mechanism of Action
Glucocorticoids• Inhibit the growth of neoplastic lymphoid
tissue
• Counteract the effects of vitamin D
43. Glucocorticoids
Low PTH Hypocalcemia44.
Hypocalcemia• Low PTH (hypoparathyroidism)
Genetic disorders: Abnormal parathyroid gland development
Abnormal PTH synthesis; Activating mutations of calcium-sensing
receptor (autosomal dominant hypocalcemia)
Post-surgical
Autoimmune: Autoimmune polyglandular syndrome (associated with
chronic mucocutaneous candidiasis and primary adrenal insufficiency)
Hypoparathyroidism due to activating antibodies to calcium-sensing
receptor
Infiltration of the parathyroid gland (granulomatous, iron overload,
metastases)
Radiation-induced destruction parathyroid glands
Hungry bone syndrome (post parathyroidectomy)
45. Hypocalcemia
• High PTH (secondary hyperparathyroidism inresponse to hypocalcemia)
Vitamin D deficiency or resistance
Parathyroid hormone resistance: Pseudohypoparathyroidism
Hypomagnesemia
Renal disease
Loss of calcium from the circulation:
Hyperphosphatemia ; Tumor lysis ; Acute pancreatitis (the
mechanism unknown)
Osteoblastic metastases; Acute respiratory alkalosis
Sepsis or severe burns- the cause appears to be a combination of
impaired secretion of PTH coupled with reduced calcitriol production
46. Hypocalcemia
Drugs induced hypocalcemia• Inhibitors of bone resorption
(bisphosphonates, calcitonin, denosumab),
especially in vitamin D deficiency
• Cinacalcet –calcimimetic
• Calcium chelators (EDTA, citrate, phosphate)
Foscarnet (due to intravascular complexing
with calcium)
Phenytoin (due to conversion of vitamin D to
inactive metabolites)
Fluoride poisoning
47. Drugs induced hypocalcemia
HypocalcemiaTrousseau's sign is the induction of
carpopedal spasm by inflation of a
sphygmomanometer above systolic
blood pressure for three minutes.
Chvostek's sign is contraction of the
ipsilateral facial muscles elicited by
tapping the facial nerve just anterior to
the ear
48. Clinical Manifestations of Hypoparathyroidism
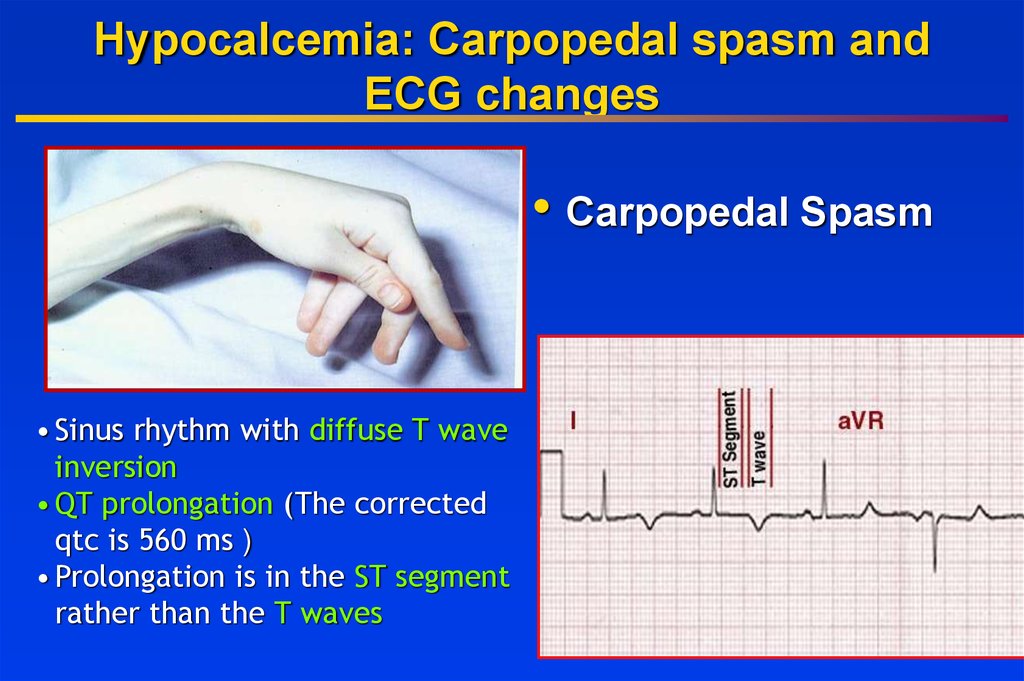
Hypocalcemia: Carpopedal spasm andECG changes
• Carpopedal Spasm
• Sinus rhythm with diffuse T wave
inversion
• QT prolongation (The corrected
qtc is 560 ms )
• Prolongation is in the ST segment
rather than the T waves
49. Hypocalcemia: Carpopedal spasm and ECG changes
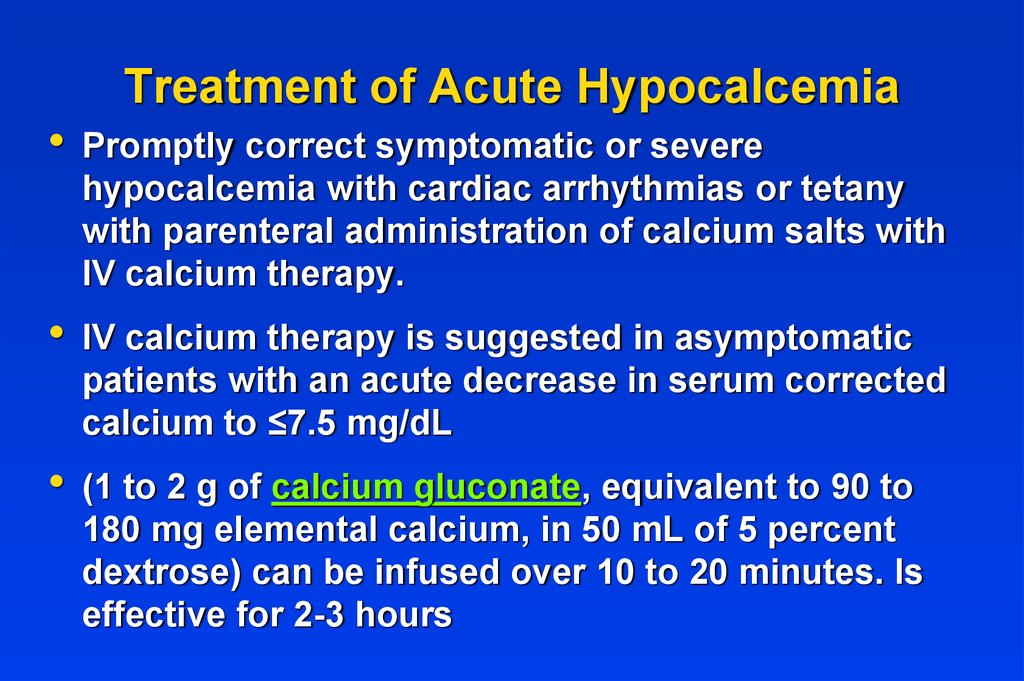
Treatment of Acute Hypocalcemia
Promptly correct symptomatic or severe
hypocalcemia with cardiac arrhythmias or tetany
with parenteral administration of calcium salts with
IV calcium therapy.
IV calcium therapy is suggested in asymptomatic
patients with an acute decrease in serum corrected
calcium to ≤7.5 mg/dL
(1 to 2 g of calcium gluconate, equivalent to 90 to
180 mg elemental calcium, in 50 mL of 5 percent
dextrose) can be infused over 10 to 20 minutes. Is
effective for 2-3 hours
50. Treatment of Acute Hypocalcemia
• Identify and treat the cause of hypocalcemiaand taper the infusion.
• For those with milder symptoms of neuromuscular
irritability (paresthesias) and corrected serum
calcium concentrations greater than 7.5 mg/dL initial
treatment with oral calcium supplementation is
sufficient. If symptoms do not improve with oral
supplementation, intravenous calcium infusion is
required.
To effectively treat hypocalcemia in patients with
concurrent magnesium deficiency,hypomagnesemia
should be corrected first.
51. Treatment of Acute Hypocalcemia
To prevent Hypocalcemia due toHungry bone syndrome
• Start oral calcium and vitamin D
treatment early. Patients with
postparathyroidectomy hungry bone
disease, especially those with osteitis
fibrosa cystica, can present with a
dramatic picture of hypocalcemia.
52. To prevent Hypocalcemia due to Hungry bone syndrome
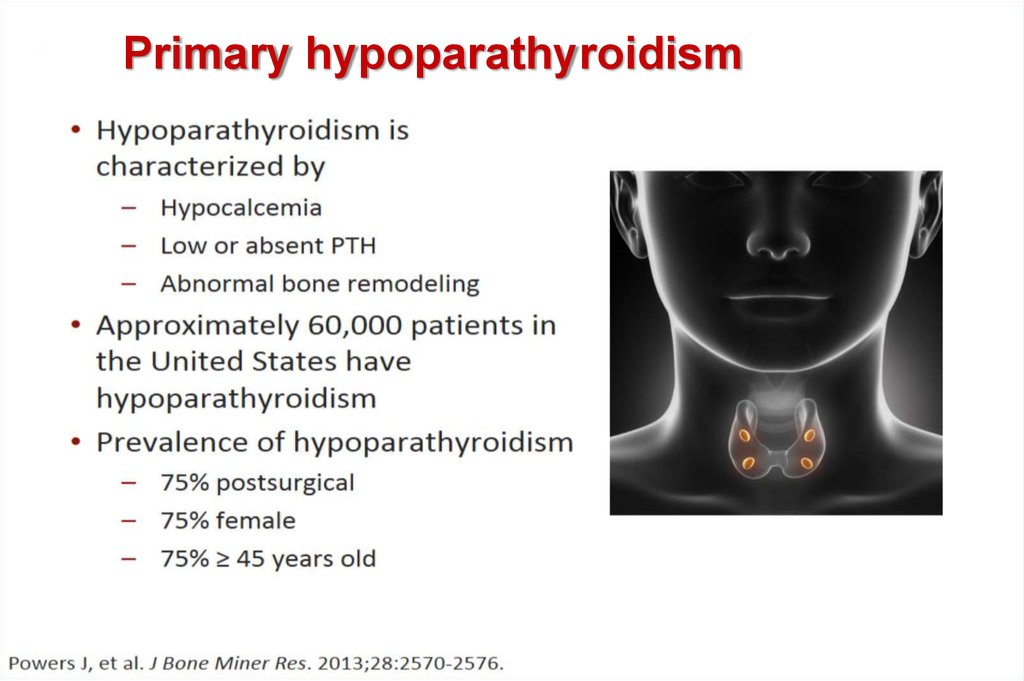
Primary hypoparathyroidism53. Introduction
54. Diagnostic Workup Initial Laboratory Evaluation
55. Goals of Treatment
56. Chronic Treatment With Oral Calcium and Vitamin D Supplementation
57. Hydrochlorothiazide for the Management of Hypercalciuria
NatparaNatpara- for use in patients who
can’t be normalized on regular
oral therapy, or have complication
s due to it (nephrolithiasis, hyper
Calciuria)
58. PTH(1-84) Indication and Safety
Causes of magnesium depletionCauses of magnesium depletion
Renal losses
Gasro-intestinal losses
59. Causes of magnesium depletion
Treatment of HypomagnesemiaOral repletion- if available and tolerable.
A typical daily dose in a patient with normal
renal function is 240 to 1000 mg (20 to 80 meq
[10 to 40 mmol]) of elemental magnesium in
divided doses.
If a sustained-release preparation is not
available, magnesium oxide 800 to 1600 mg
(20 to 40 mmol [40 to 80 meq]) daily in divided
doses may be used for moderate to severe
hypomagnesemia.
Diarrhea frequently occurs with magnesium
oxide therapy.












 medicine
medicine