Similar presentations:
Managemeht of patients with joint syndrome. Osteoarthritis .gout
1.
MANAGEMEHT OF PATIENTS WITHJOINT SYNDROME.
OSTEOARTHRITIS .GOUT.
Department Internal Disease №2
Docent Аnna Zayayeva
2. Definition
Gout is a heterogeneous disorder that resultsin the deposition of uric acid salts and crystals
in and around joints and soft tissues or
crystallization of uric acid in the urinary tract.
Gout is a disorder that manifests as a
spectrum of clinical and pathologic features
built on a foundation of an excess body
burden of uric acid, manifested in part by
hyperuricemia, which is variably defined as a
serum urate level greater than either 6.8 or
7.0 mg/dl (ACR, 2012) or 0,42 mmol/l (Russia)
3. Heterogeneous group of diseases involving :
An elevated serum urate concentration(hyperuricemia)
Recurrent attacks of acute arthritis in which
monosodium urate monohydrate crystals are
demonstrable in synovial fluid leukocytes
Aggregates of sodium urate monohydrate crystals
(tophi) deposited chiefly in and around joints,
which sometimes lead to deformity and crippling
Renal disease involving glomerular, tubular, and
interstitial tissues and blood vessels
Uric acid nephrolithiasis
4. Epidemiology
Most common of microcrystalline arthropathy.Affects about 2.1million worldwide
Peak incidence occurs in the fifth decade, but
can occur at any age
Gout is more common in males than premenopausal females; incidence in women
increases after menopause. After age 60, the
incidence in women approaches the rate in men.
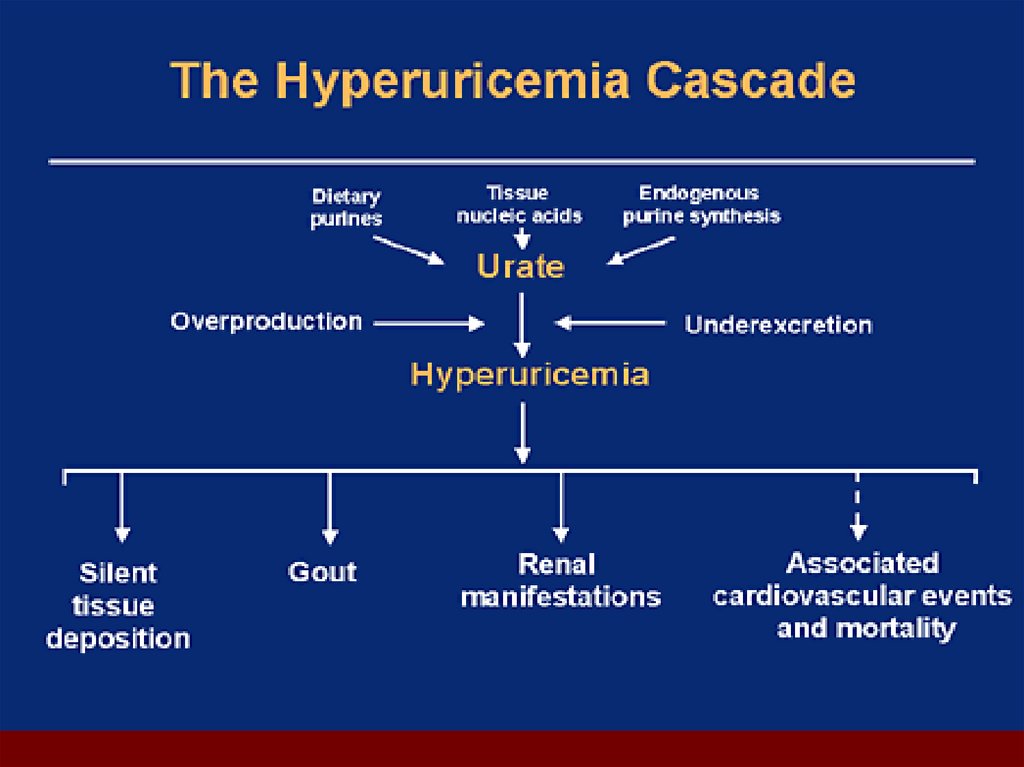
5. Classification of Hyperuricemia
Uric acid overproduction– Accounts for 10% of hyperuricemia
– Defined as 800mg of uric acid excreted
– Acquired disorders
Excessive cell turnover rates such as myleoproliferative
disorders, Paget’s disease, hemolytic anemias
– Genetic disorders: derangements in mechanisms that regulate
purine neucleotide synthesis.
Uric acid underexcretion
– Accounts for >90% of hyperuricemia
– Diminished tubular secretory rate, increased tubular
reabsorption, diminished uric acid filtration
Drugs, other systemic disease that predispose people to
renal insufficiency
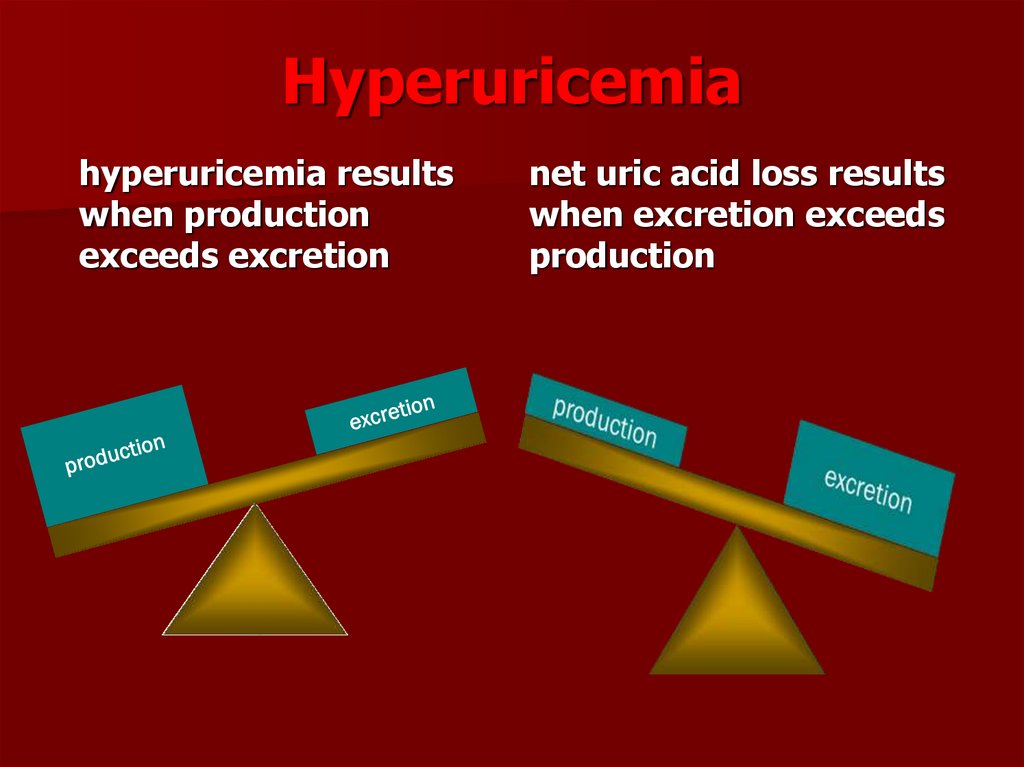
6. Hyperuricemia
hyperuricemia resultswhen production
exceeds excretion
net uric acid loss results
when excretion exceeds
production
7. Predisposing Factors
HeredityDrug usage
Renal failure
Hematologic Disease
Trauma
Alcohol use
Psoriasis
Poisoning
Obesity
Hypertension
Organ transplantation
Surgery
8.
9.
10.
11. Classification of Gout
Primary gout is caused by inborn defects inpurine metabolism or inherited defects of the
renal tubular secretion of urate.
Secondary gout is caused by acquired
disorders that result in increased turnover of
nucleic acids, by defects in renal excretion of
uric acid salts, and by the effects of certain
drugs
12. Classification of Hyperuricemia and Gout
Primary Hyperuricemia and Goutwith No Associated Condition
Uric acid undersecretion
(80%–90%)
Idiopathic
Urate overproduction
(10%–20%)
Idiopathic
HGPRT (hypoxanthine-guanine
phosphoribosyl transferase)
deficiency
PRPP synthetase (phosphoribosyl
pyrophosphate) overactivity
Secondary Hyperuricemia and
Gout with Identifiable
Associated Condition
Uric acid undersecretion
Renal insufficiency
Polycystic kidney disease
Lead nephropathy
Drugs (Diuretics, Salicylates (low
dose), Pyrazinamide, Ethambutol,
Cyclosporine)
Urate overproduction
Myeloproliferative/ Lymphoproliferati
ve diseases / Hemolytic
anemias/ Polycythemia /Other
malignancies
Psoriasis/Glycogen storage disease
Dual mechanism
Obesity, Hypoxemia and
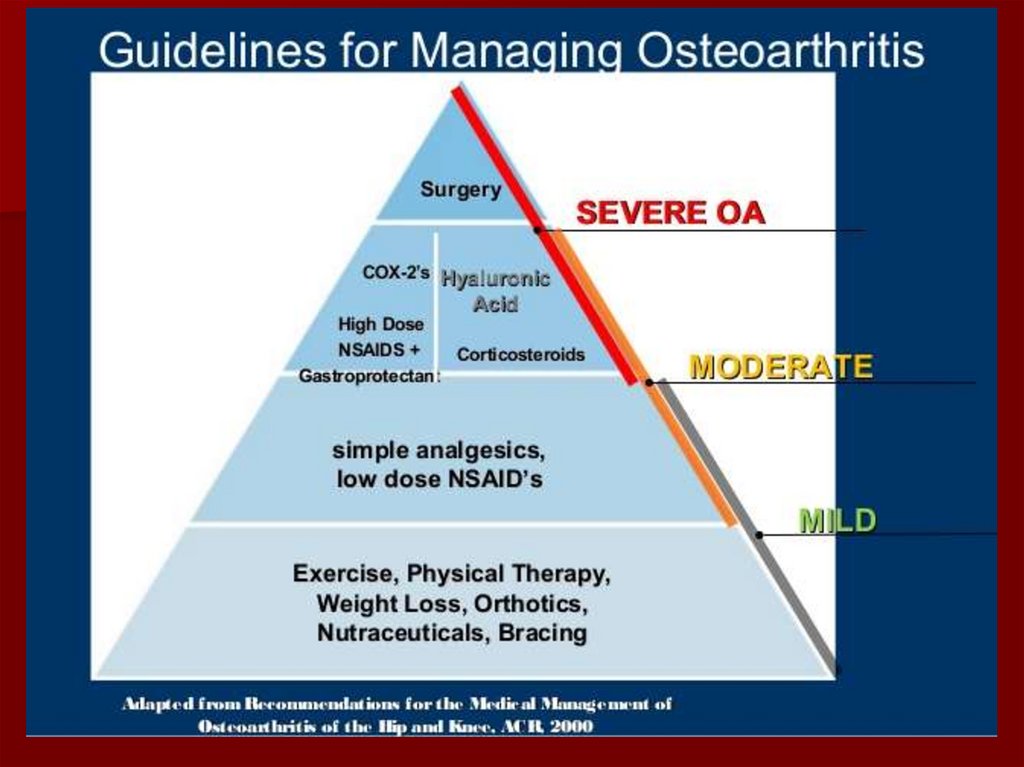
hypoperfusion
13. Pathogenesis of Gouty Inflammation
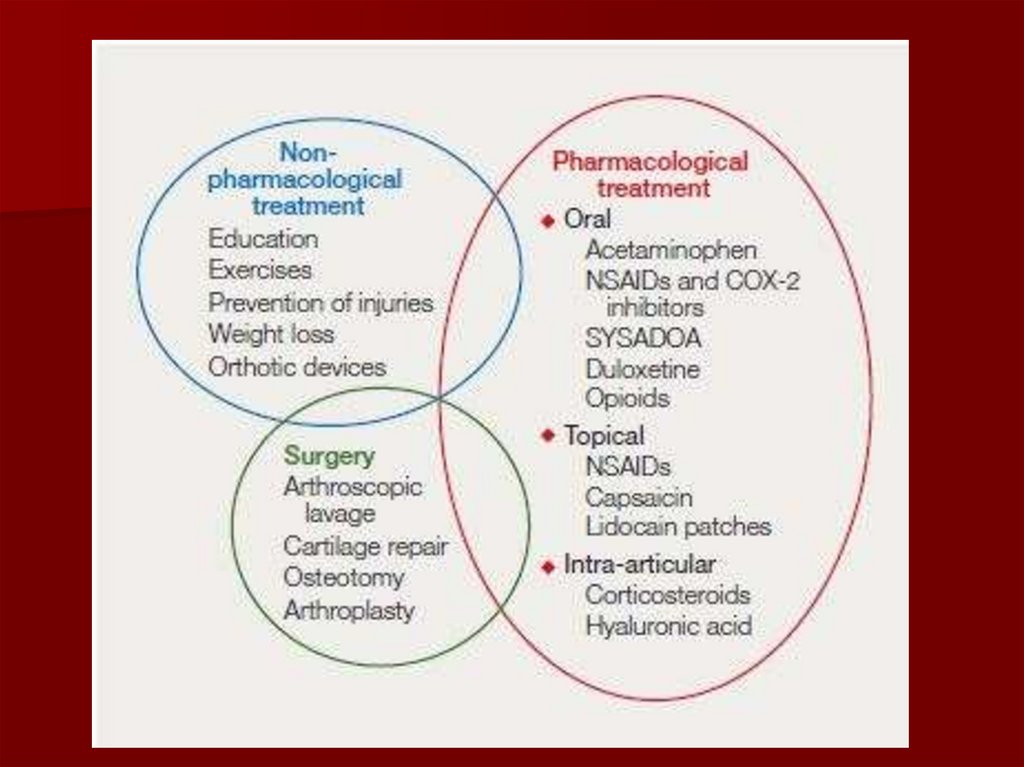
Urate crystals stimulate the release of numerousinflammatory mediators (IL-1β) in synovial cells
and phagocytes
The influx of neutrophils is an important event
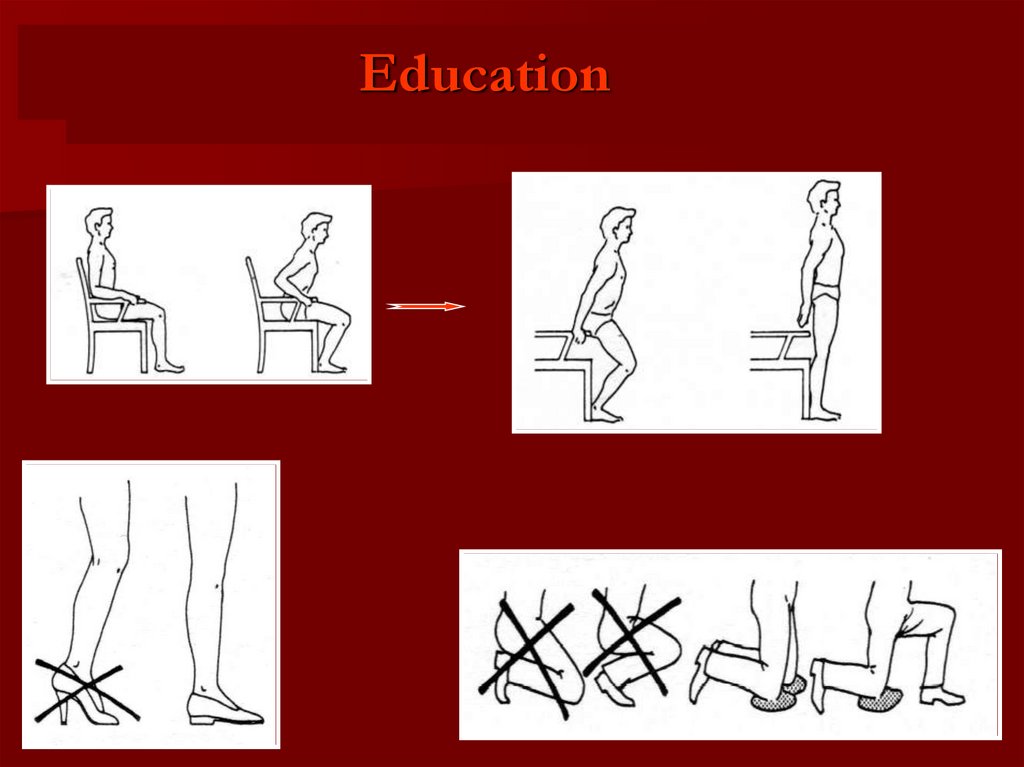
for developing acute crystal induced synovitis
Chronic gouty inflammation associated with
cytokine driven synovial proliferation, cartilage
loss and bone erosion
14. Presenting Symptoms
Systemic: fever rare but patients may havefever, chills and malaise
Musculoskeletal: Acute onset of
monoarticular joint pain. First MTP most
common. Usually affected in 90% of patients
with gout. Other joints knees, foot and
ankles. Less common in upper extremities
Skin: warmth, erythema and tenseness of
skin overlying joint. May have itching and
desquamation
Urogenital system: Renal colic with renal
stones formation in patients with
hyperuricemia
15. Gout - cardinal manifestations
tophiarthritis
acute &
chronic
HYPERURICEMIA
nephrolithiasis
nephropathy
16.
17. Acute gout attack
The most common signsof gout attack are:
A nighttime attack
Erythema overlying affected joint
Can’t bear touch or pressure to
affected joint
Great difficulty with walking or
inability to use joint
Swelling, tenderness, redness
Sharp pain in a big toe
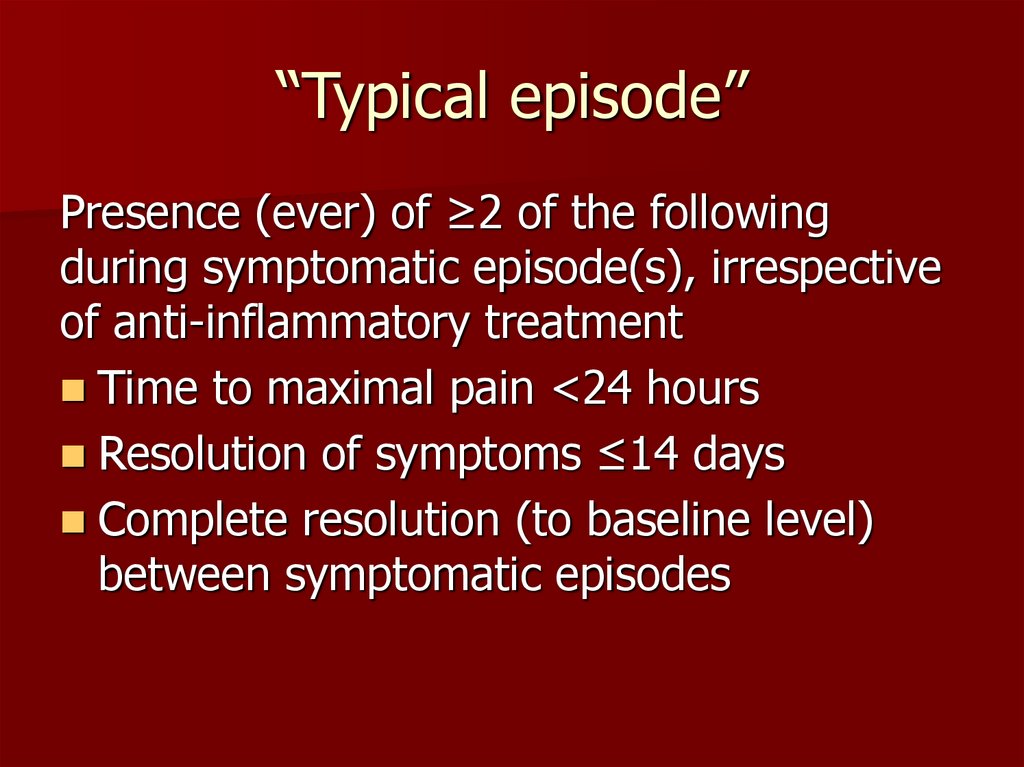
18. “Typical episode”
Presence (ever) of ≥2 of the followingduring symptomatic episode(s), irrespective
of anti-inflammatory treatment
Time to maximal pain <24 hours
Resolution of symptoms ≤14 days
Complete resolution (to baseline level)
between symptomatic episodes
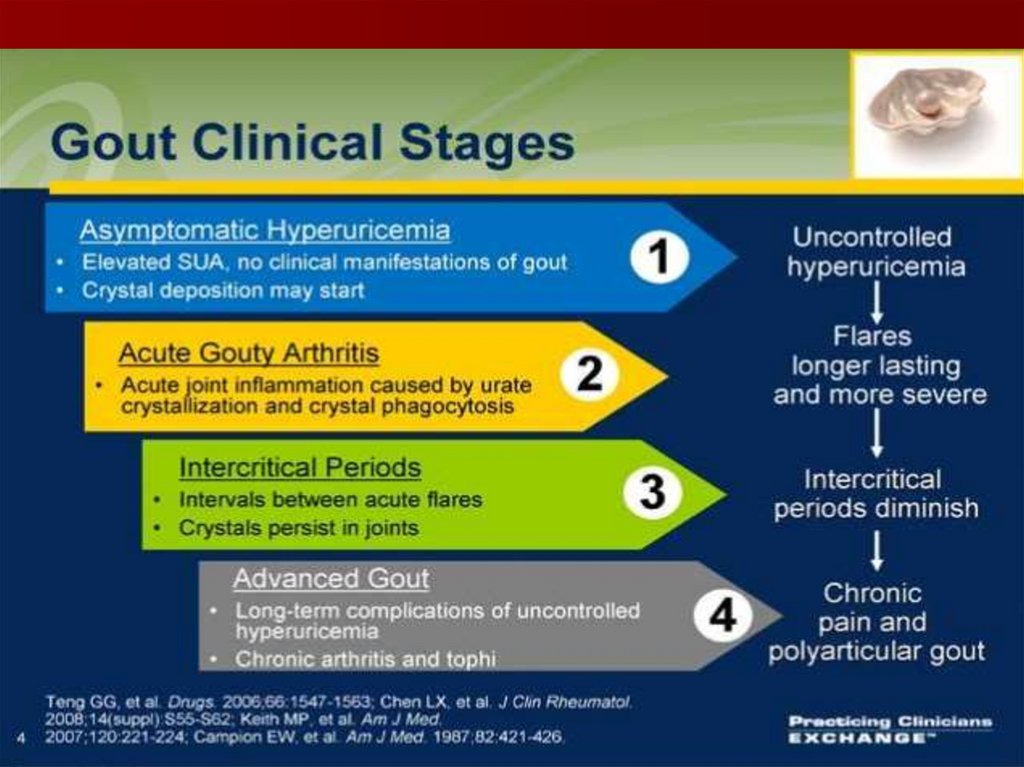
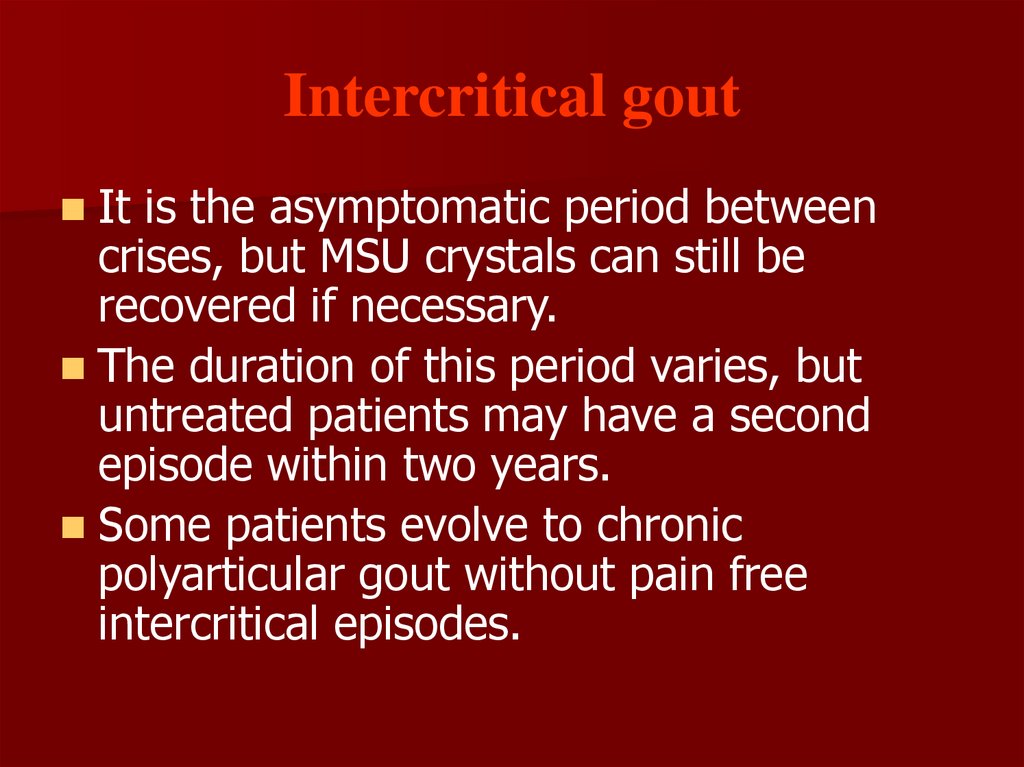
19. Intercritical gout
It is the asymptomatic period betweencrises, but MSU crystals can still be
recovered if necessary.
The duration of this period varies, but
untreated patients may have a second
episode within two years.
Some patients evolve to chronic
polyarticular gout without pain free
intercritical episodes.
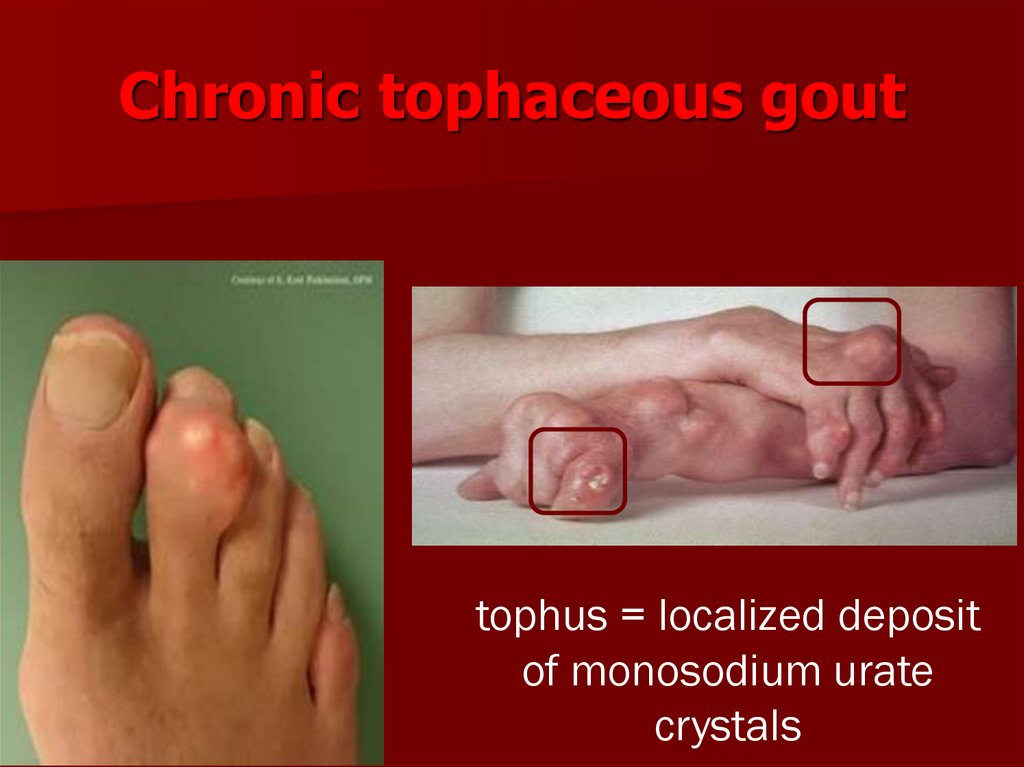
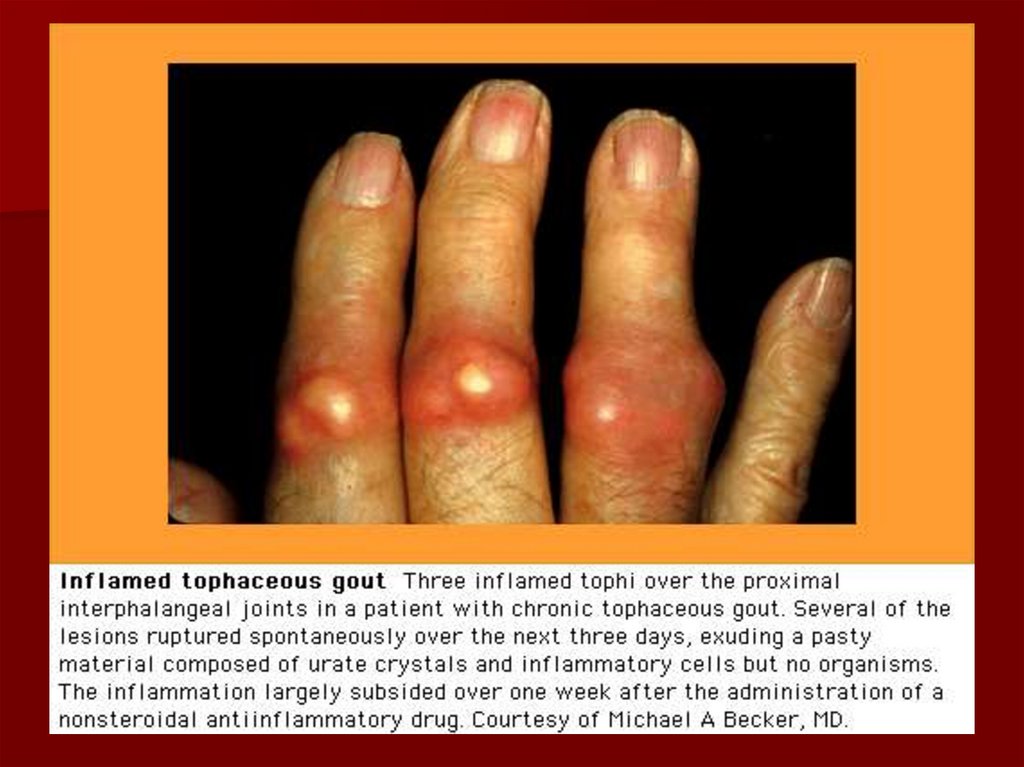
20. Chronic tophaceus Gout
The clinical characteristic is the deposition ofsolid urate in the connective tissue.
It is associated with early age of onset, long
duration of untreated disease, frequent attacks,
upper extremity involvement, polyarticular
disease and elevated serum uric acid.
Transplant patients treated with cyclosporine
and/or diuretics have an increased risk for
tophaceus gout.
The most common sites for tophi are: the
olecranon, prepatellar bursa, ulnar surface and
Achilles tendon.
21. Gout - tophus
Draining or chalk-likesubcutaneous nodule
under transparent skin
with overlying vascularity
Typical locations:
Ears, olecranon bursa,
finger pads, tendon (e.g.,
Achilles)
classic location of
tophi on helix of ear
22. Chronic tophaceous gout
tophus = localized depositof monosodium urate
crystals
23.
24.
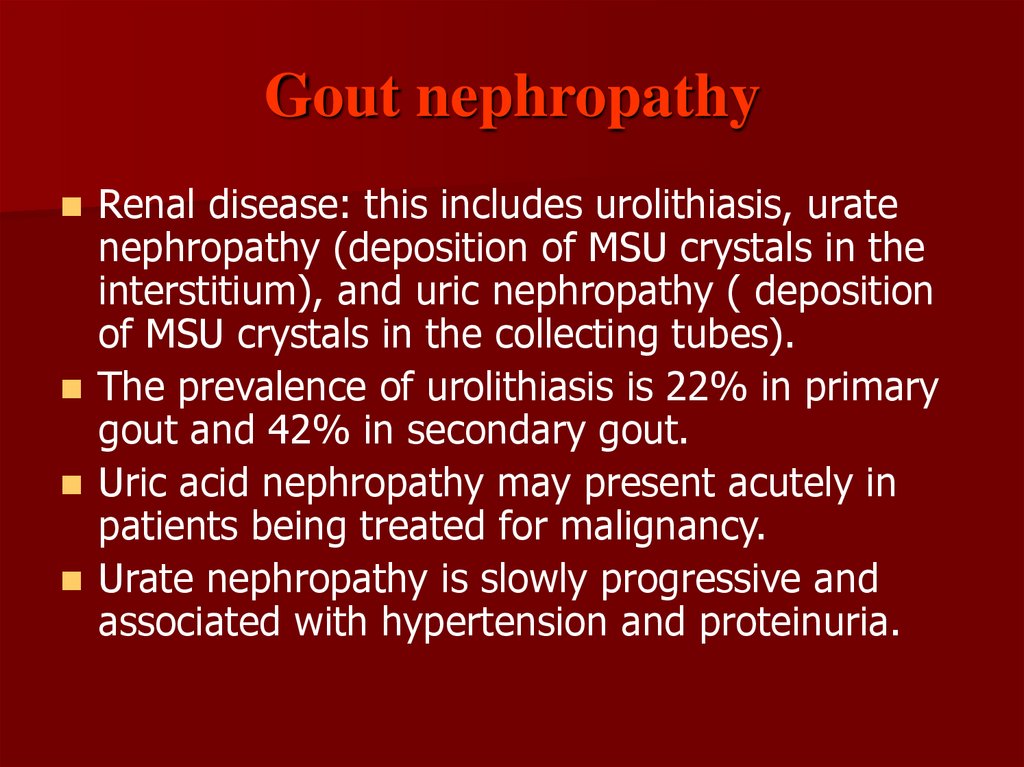
25. Gout nephropathy
Renal disease: this includes urolithiasis, uratenephropathy (deposition of MSU crystals in the
interstitium), and uric nephropathy ( deposition
of MSU crystals in the collecting tubes).
The prevalence of urolithiasis is 22% in primary
gout and 42% in secondary gout.
Uric acid nephropathy may present acutely in
patients being treated for malignancy.
Urate nephropathy is slowly progressive and
associated with hypertension and proteinuria.
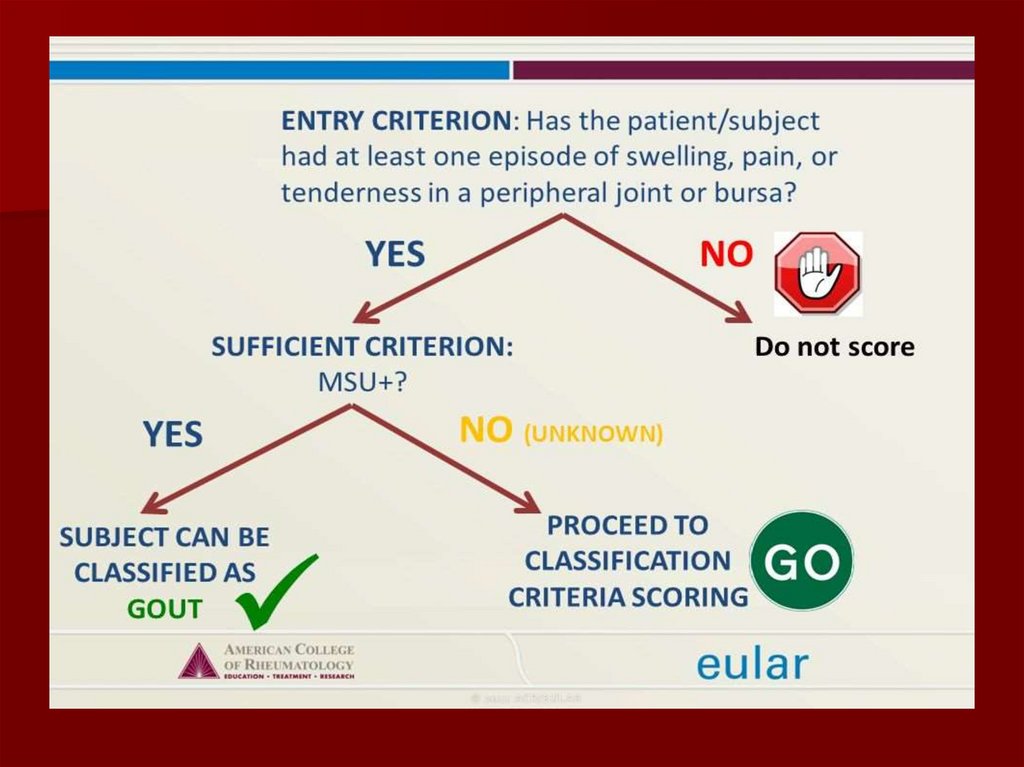
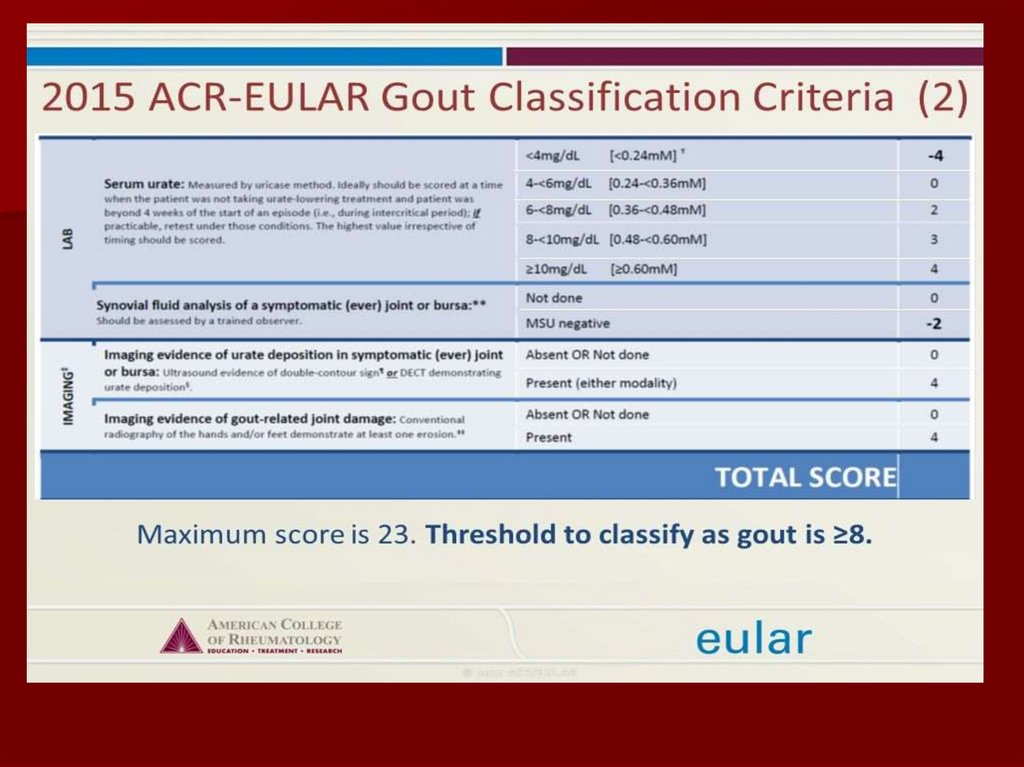
26.
ACR preliminary criteria for the clinical diagnosisof gout
6 or more of these criteria are needed to make a
diagnosis:
-More than one attack of acute arthritis
-Maximum inflammation developed within one day
-Attack of monoarthritis
-Redness over joints
-Painful or swollen first metatarsophalangeal joint
-Unilateral attack on first metatarsophalangeal joint
-Unilateral attack on tarsal joint
-Tophus (proved or suspected)
-Hyperuricaemia
-Asymmetric swelling within a joint on radiograph
-Subcortical cysts without erosions on radiograph
-Joint fluid culture negative for organisms during attack
27.
28.
29.
30.
31. Diagnosis
Definitive diagnosis onlypossible by aspirating
and inspecting
synovial fluid or
tophaceous material
and demonstrating MSU
crystals
Polarized microscopy, the
crystals appear as bright
birefringent crystals that
are yellow (negatively
birefringent)
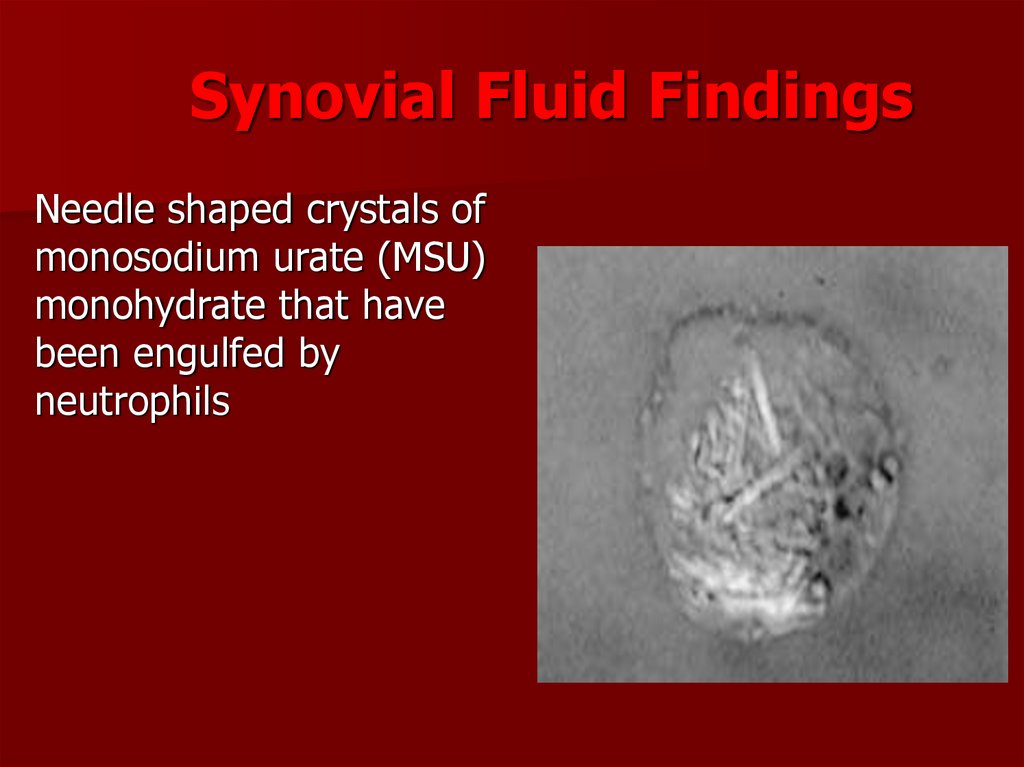
32. Synovial Fluid Findings
Needle shaped crystals ofmonosodium urate (MSU)
monohydrate that have
been engulfed by
neutrophils
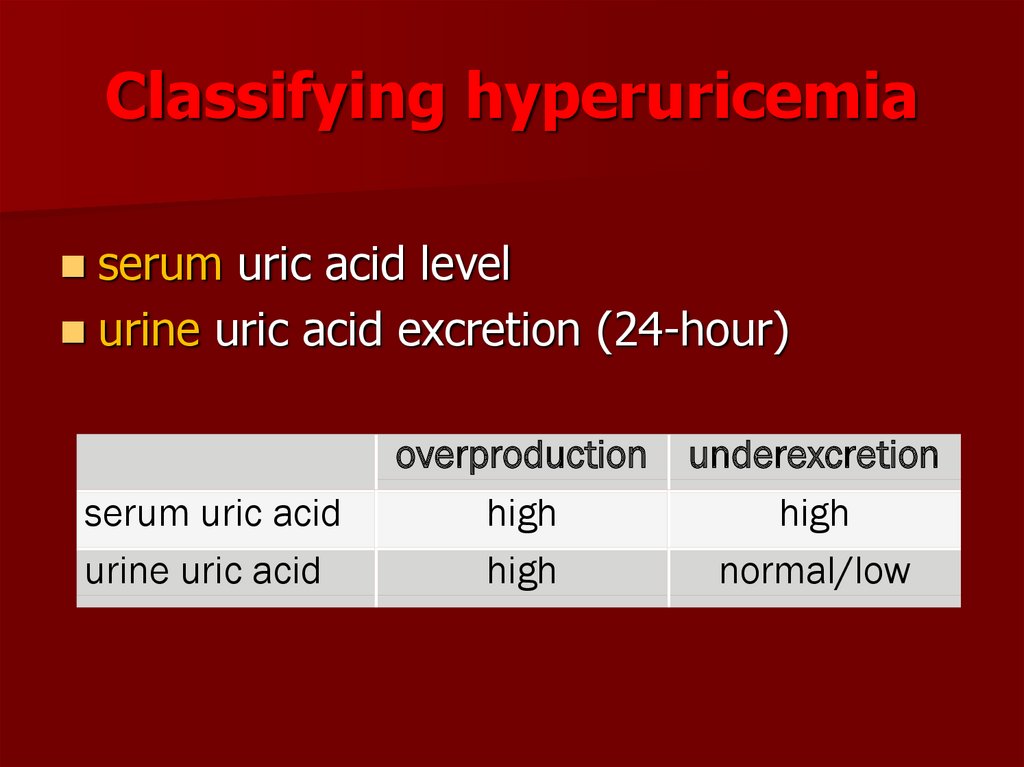
33. Classifying hyperuricemia
serum uric acid levelurine uric acid excretion (24-hour)
serum uric acid
urine uric acid
overproduction
high
high
underexcretion
high
normal/low
34. Diagnostic Tests
Uric Acid: normal values range from 4.0to 8.6 mg/dl (0,21-0,42 mmol/l) in men to
3.0 to 5.9 mg/dl (0,15-0,35 mmol/l) in
women. Urinary levels are normal less
750 mg/ 24h.
Urinary levels above 750 mg/dl in 24h in
gout or > 1100 mg/dl in asymptomatic
hyperuricemia indicates urate
overproduction.
35. Diagnostic Tests
24 urinecollection for
uric acid
determination is
useful in
assessing the
risk of renal
stones and
planning for
therapy.
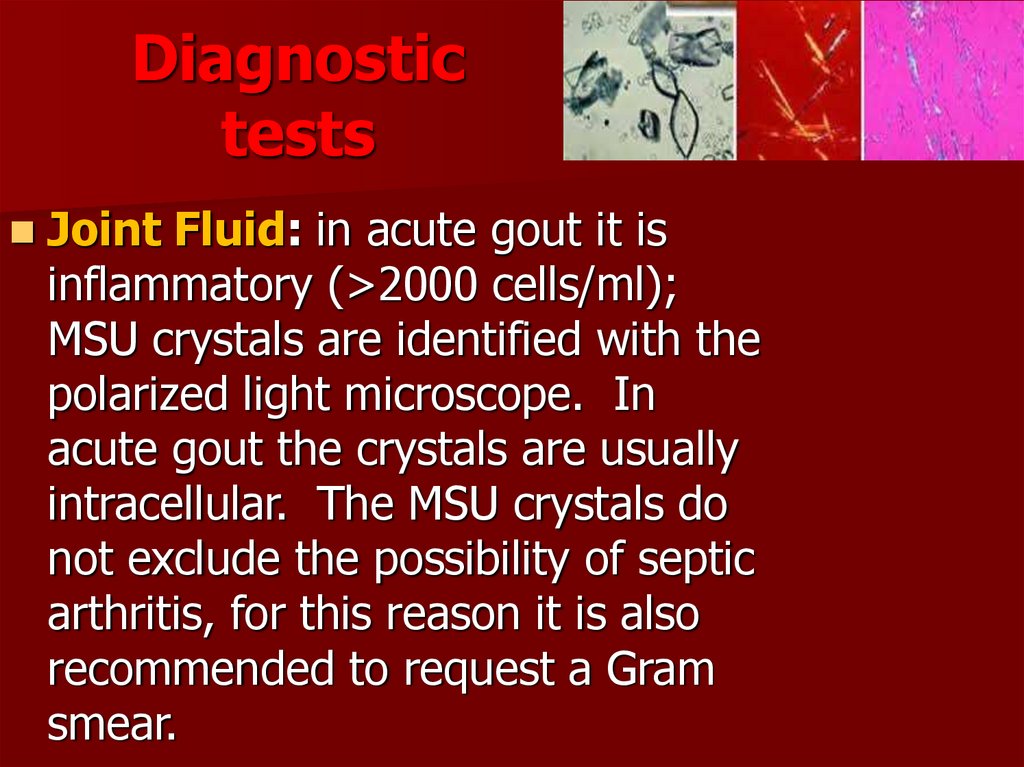
36. Diagnostic tests
Joint Fluid: in acute gout it isinflammatory (>2000 cells/ml);
MSU crystals are identified with the
polarized light microscope. In
acute gout the crystals are usually
intracellular. The MSU crystals do
not exclude the possibility of septic
arthritis, for this reason it is also
recommended to request a Gram
smear.
37. Diagnostic Tests
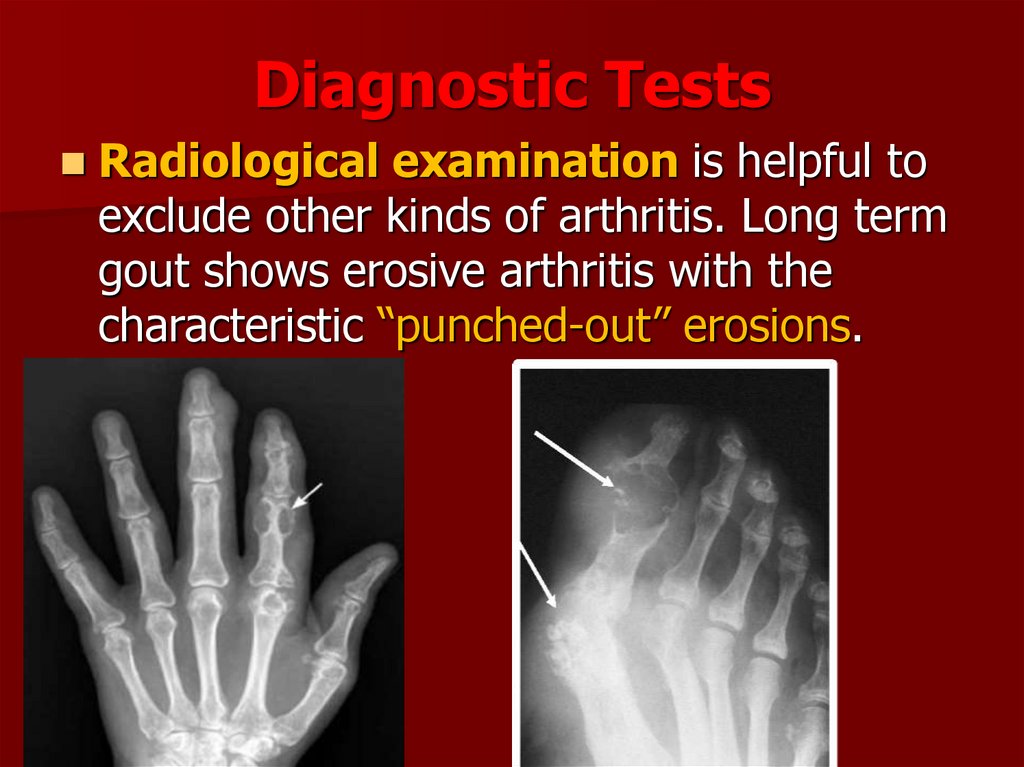
Radiological examination is helpful toexclude other kinds of arthritis. Long term
gout shows erosive arthritis with the
characteristic “punched-out” erosions.
38. Gout - X-ray changes
bony “punched-out”erosions
39. Gout - X-ray changes
DIP jointdestruction
phalangeal bone
cysts
40.
41.
42.
43.
44. Differential Diagnosis
TraumaInfections
– septic arthritis, gonococcal arthritis
Inflammatory
– Rheumatic arthritis, Reiter’s syndrome,
Psoriatic arthritis
Metabolic
– pseudogout
Different
– Osteoarthrtis
45. Diagnostic Studies
Uric Acid– Limited value as majority of hyperuricemic patients will never develop
gout
– Levels may be normal during acute attack
CBC
– Mild leukocytosis in acute attacks, but may be higher than 25,000
ESR
– mild elevation or may be 2-3x normal
24hr urine uric acid
– Only useful in patients being considered for uricosuric therapy or if
cause of marked hyperuricemia needs investigation
Trial of colchicine
– Positive response may occur in other types of arthritis to include
pseudogout.
46. Complications
Renal Failure– ARF can be caused by hyperuricemia,
chronic urate nephropathy
Nephrolithiasis
Joint deformity
Recurrent Gout
Often accompanies heart problems,
including high blood pressure, coronary
artery disease, and congestive heart failure.
Hyperuricemia, in fact, has been associated
with a higher risk of death from these
conditions.
47. Treatment Goals
Gout can be treated without complications.Therapeutic goals include :
– terminating attacks
– providing control of pain and inflammation
– preventing future attacks
– preventing complications such as renal
stones, tophi, and destructive arthropathy
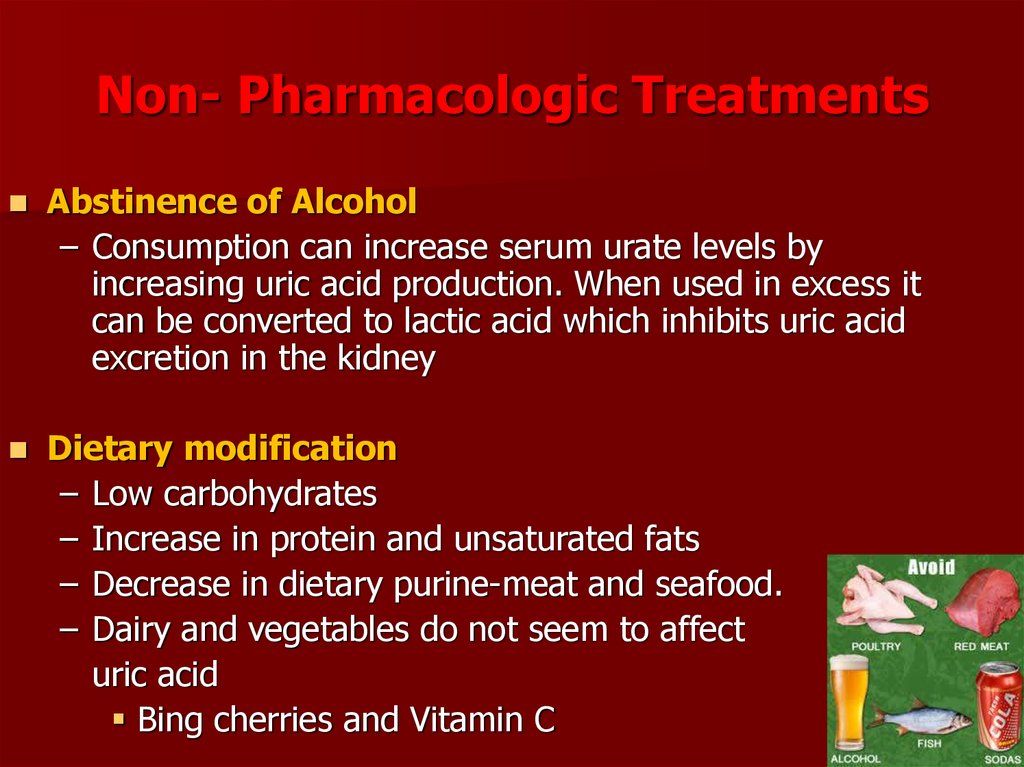
48. Non- Pharmacologic Treatments
Abstinence of Alcohol– Consumption can increase serum urate levels by
increasing uric acid production. When used in excess it
can be converted to lactic acid which inhibits uric acid
excretion in the kidney
Dietary modification
– Low carbohydrates
– Increase in protein and unsaturated fats
– Decrease in dietary purine-meat and seafood.
– Dairy and vegetables do not seem to affect
uric acid
Bing cherries and Vitamin C
49.
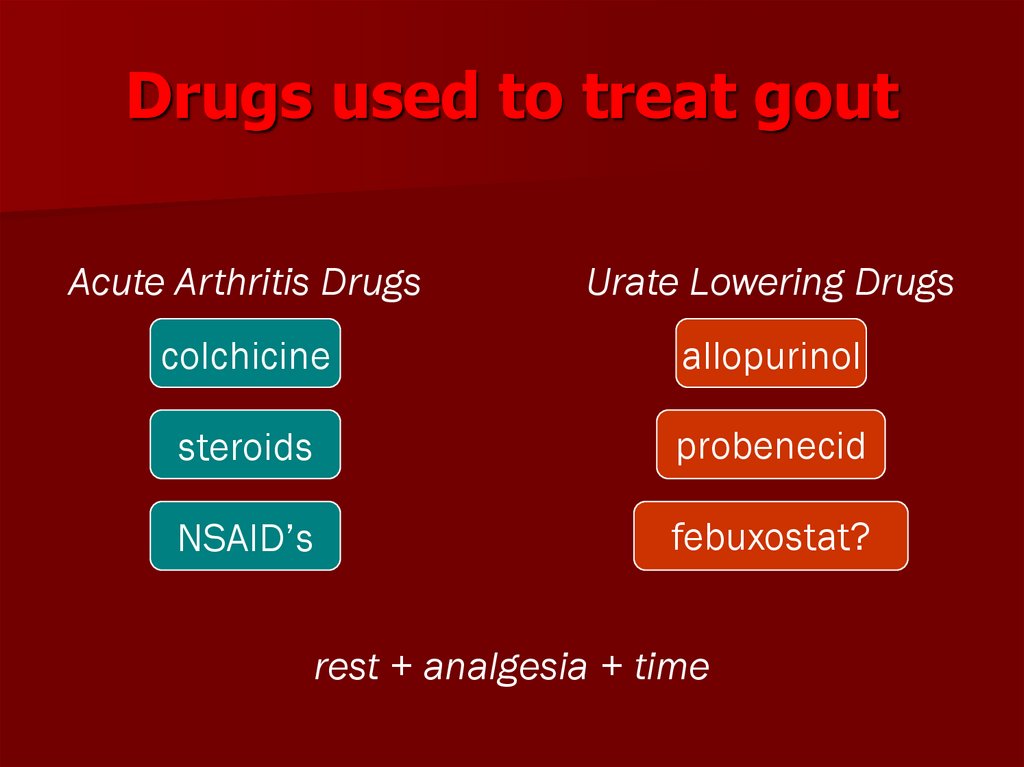
50. Drugs used to treat gout
Acute Arthritis DrugsUrate Lowering Drugs
colchicine
allopurinol
steroids
probenecid
NSAID’s
febuxostat?
rest + analgesia + time
51. Acute gout attacks
Educate patients to treat gout attacks as soon as they occur andthroughout the attack.
Advise patients that joints affected by gout should be rested, elevated,
and cooled. Bed-cages and ice packs may be useful.
Use a maximally dosed NSAID with colchicine dosed at 500 μg 2 to 4
times a day, the drugs of choice, in the absence of contraindications.
Drug choice depends on patient preference, kidney function, and
comorbidities. Prescribe gastroprotective agents for patients receiving
NSAIDs.
Aspirate and inject a joint with corticosteroids for acute single-joint gout.
This may be the best treatment in patients with acute attacks and
comorbidities. A possible alternative: a short course of oral corticosteroid
or a single injection of an intramuscular steroid. Systemic steroid therapy
is also appropriate for single or multiple joint attacks.
Combine treatments for patients with acute gout where monotherapy
has failed.
Consider interleukin-1 inhibitors for patients who don’t respond to
standard treatment.
52.
53. Acute Gout Treatment
NSAIDs– Most commonly used.
– No NSAID found to work better than others
– Regimens:
Nimesulide 100 mg 2 time / day
Indometacin 50mg po bid-tid for 2-3 days and then
taper
Ibuprofen 400mg po q4-6 hr max 3.2g/day
Ketorolac 60mg IM or 30mg IV X1 dose in patients<65
– 30mg IM or 15mg IV in single dose in patients >65
yo, or with patients who are renally impaired
Continue meds until pain and inflammation have
resolved for 48hr
54.
55. Colchicine - plant alkaloid
“only effective in gouty arthritis”not an analgesic
does not affect renal excretion of uric acid
does not alter plasma solubility of uric acid
neither raises nor lowers serum uric acid
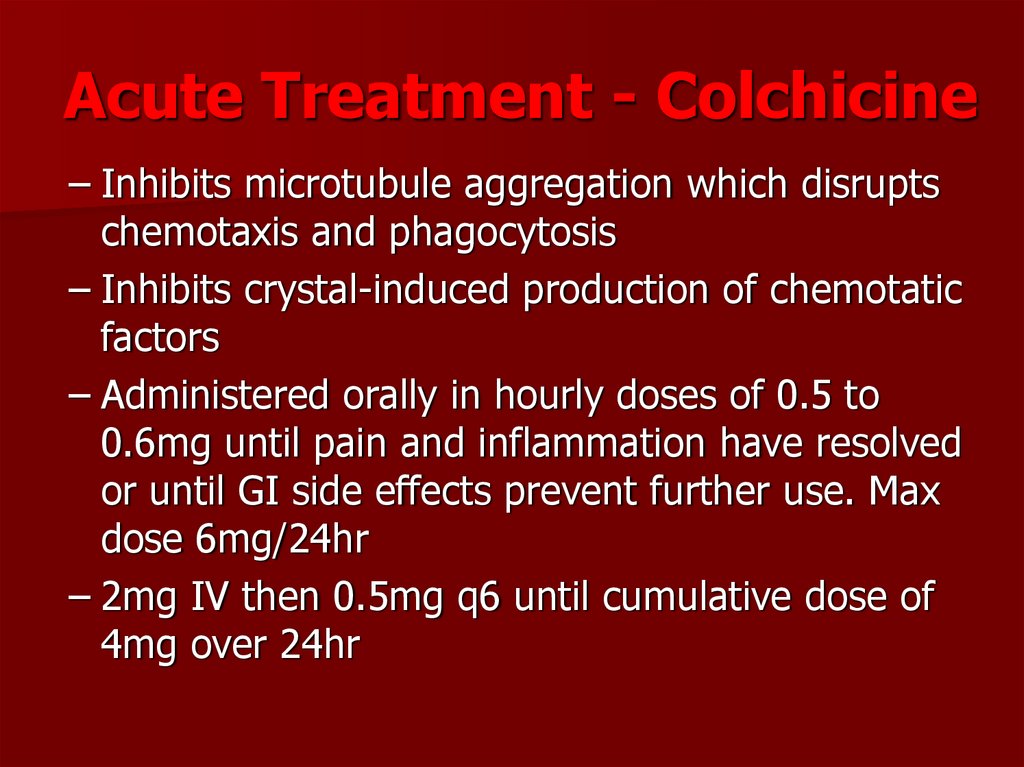
56. Acute Treatment - Colchicine
– Inhibits microtubule aggregation which disruptschemotaxis and phagocytosis
– Inhibits crystal-induced production of chemotatic
factors
– Administered orally in hourly doses of 0.5 to
0.6mg until pain and inflammation have resolved
or until GI side effects prevent further use. Max
dose 6mg/24hr
– 2mg IV then 0.5mg q6 until cumulative dose of
4mg over 24hr
57. Colchicine - toxicity
gastrointestinal (nausea, vomiting,cramping, diarrhea, abdominal pain)
hematologic (agranulocytosis, aplastic
anemia, thrombocytopenia)
muscular weakness
adverse effects dose-related & more common when
patient has renal or hepatic disease
58.
59.
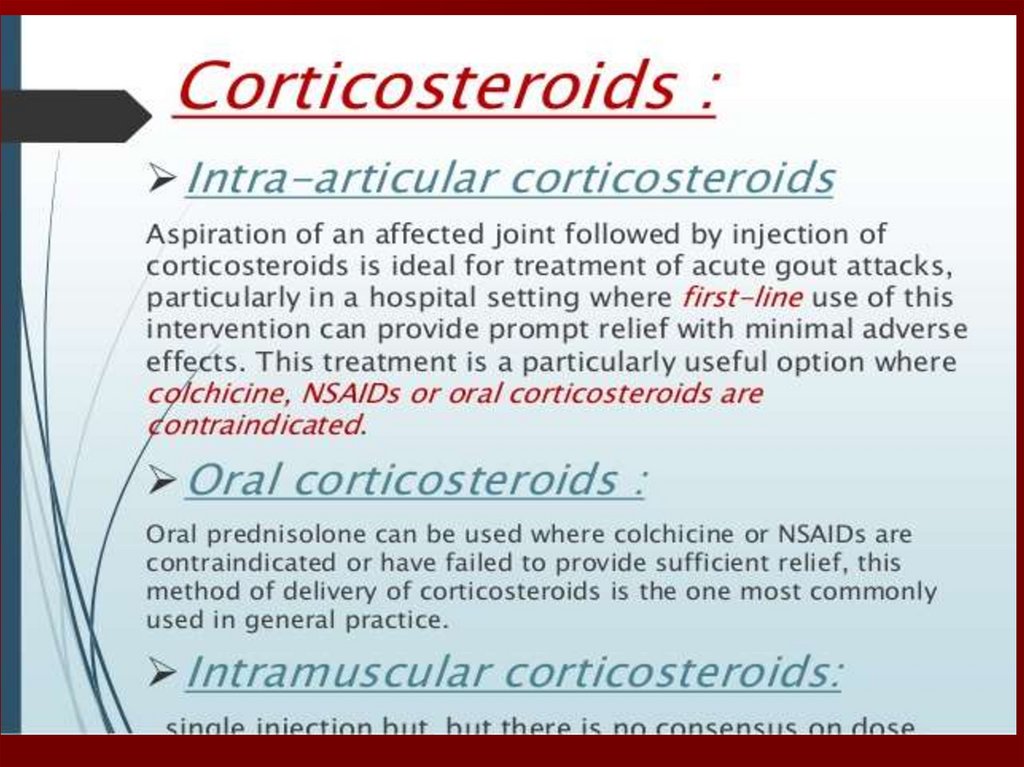
60. Acute treatment
Glucocorticoids– Patients who cannot tolerate NSAIDs, or failed
NSAID/colchicine therapy
– Daily doses of prednisone 40-60mg a day for 3-5 days
then taper 1-2 weeks
– Improvement seen in 12-24hr
Intra-articular injection with glucocorticoids
Beneficial in patient with one or two large joints affected
– Good option for elderly patient with renal or PUD or
other illness
– Triamcinolone 10-40mg or Dexamethasone 2-10mg
alone or in combination with Lidocaine
61.
62.
63. Allopurinol
inhibitor of xanthine oxidaseeffectively blocks formation of uric acid
how supplied - 100 mg & 300 mg tablets
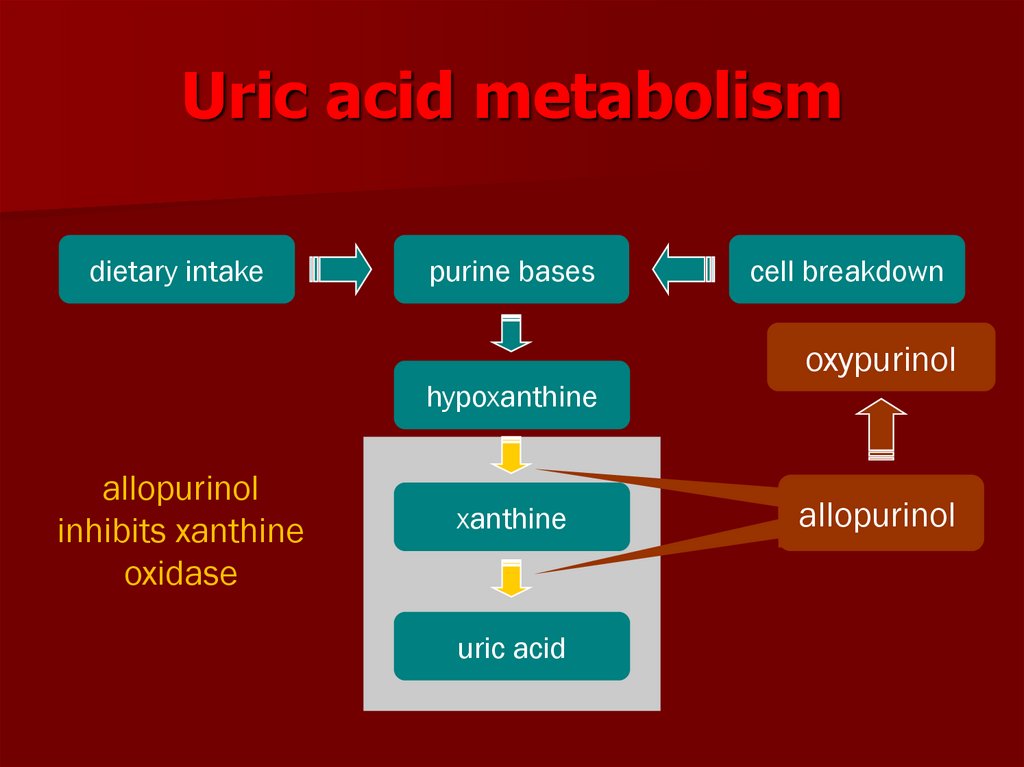
64. Uric acid metabolism
dietary intakepurine bases
cell breakdown
oxypurinol
hypoxanthine
allopurinol
inhibits xanthine
oxidase
xanthine
uric acid
allopurinol
allopurinol
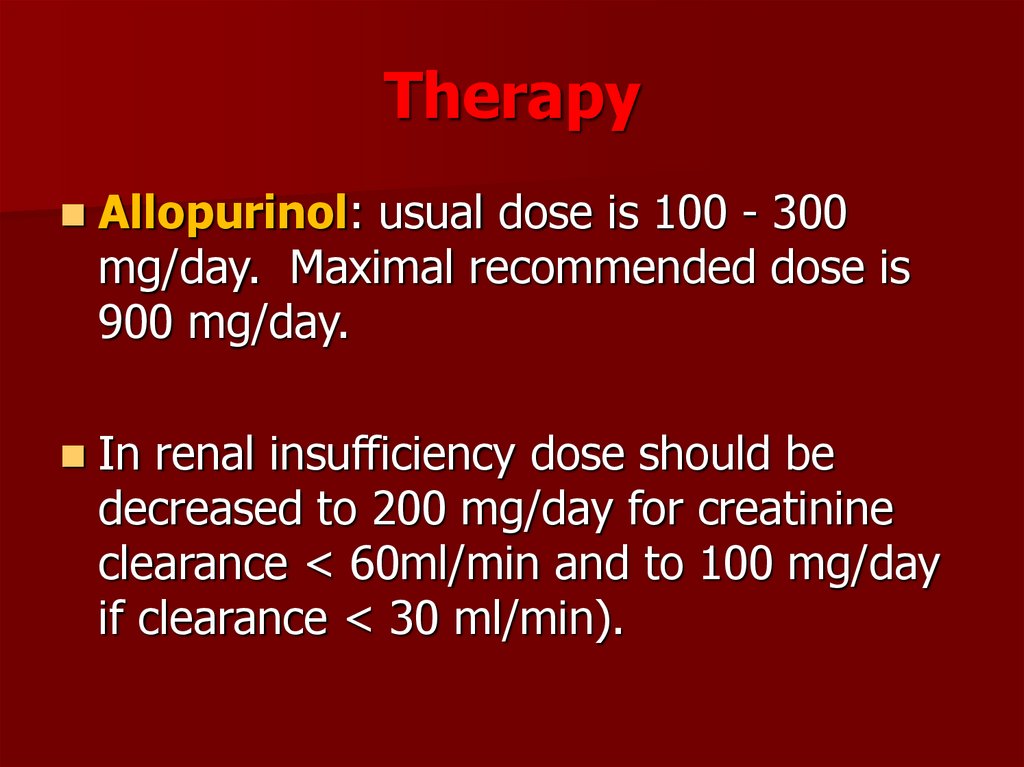
65. Therapy
Allopurinol: usual dose is 100 - 300mg/day. Maximal recommended dose is
900 mg/day.
In renal insufficiency dose should be
decreased to 200 mg/day for creatinine
clearance < 60ml/min and to 100 mg/day
if clearance < 30 ml/min).
66. Allopurinol
Start with small doses of allopurinol to reducethe risk of precipitating an acute gout attack.
Most common side effects are rash (2% of
patients) but rarely patients can develop
exfoliative dermatitis that can be lethal.
Side effect: diarrhea, nausea, abnormal liver
tests, acute attacks of gout, rash
67. Allopurinol - serious reactions
fever, rash, toxic epidermal necrolysishepatotoxicity, marrow suppression
vasculitis
drug interactions (ampicillin, thiazides,
mercaptopurine, azathioprine)
death
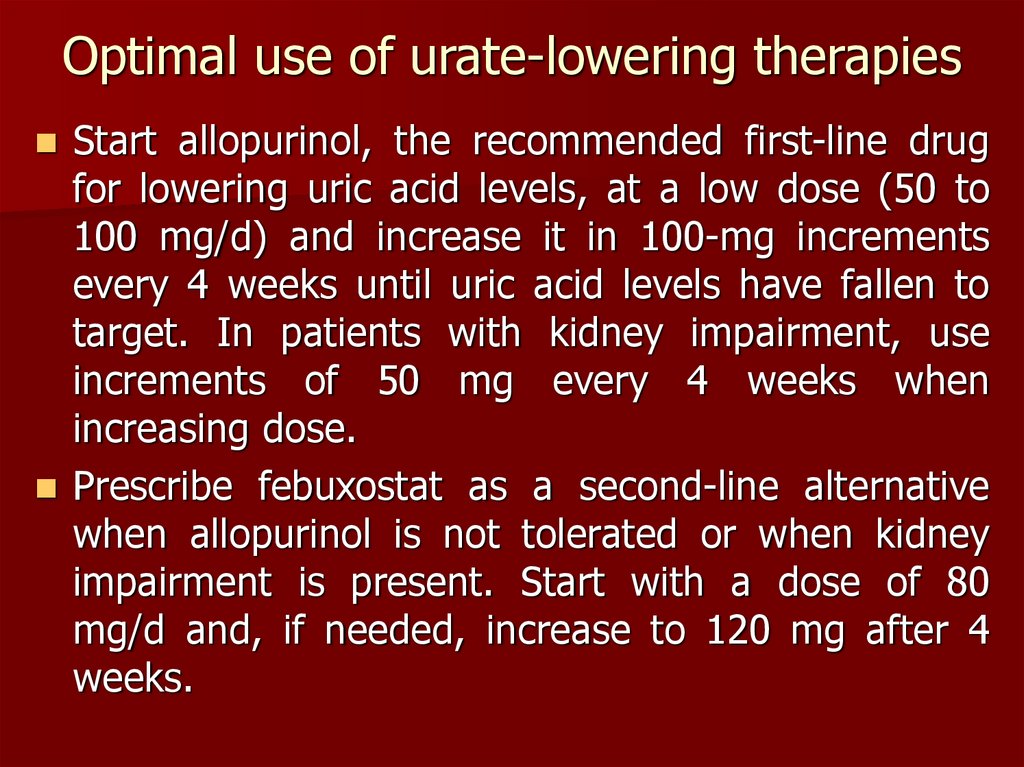
68. Optimal use of urate-lowering therapies
Start allopurinol, the recommended first-line drugfor lowering uric acid levels, at a low dose (50 to
100 mg/d) and increase it in 100-mg increments
every 4 weeks until uric acid levels have fallen to
target. In patients with kidney impairment, use
increments of 50 mg every 4 weeks when
increasing dose.
Prescribe febuxostat as a second-line alternative
when allopurinol is not tolerated or when kidney
impairment is present. Start with a dose of 80
mg/d and, if needed, increase to 120 mg after 4
weeks.
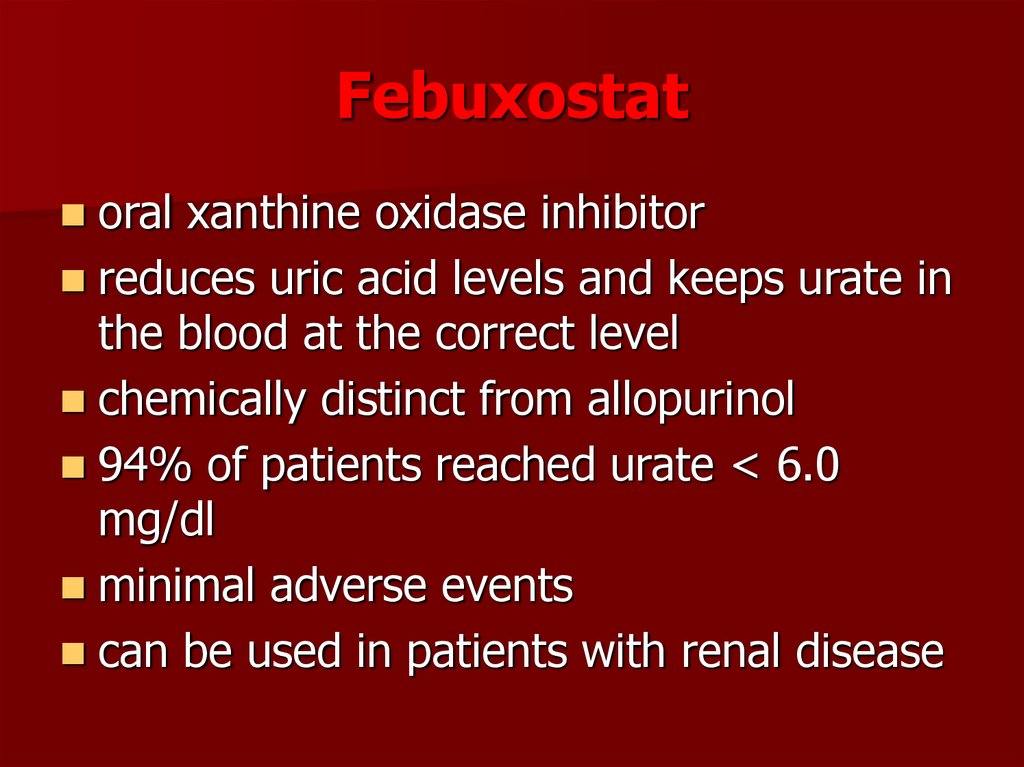
69. Febuxostat
oral xanthine oxidase inhibitorreduces uric acid levels and keeps urate in
the blood at the correct level
chemically distinct from allopurinol
94% of patients reached urate < 6.0
mg/dl
minimal adverse events
can be used in patients with renal disease
70. Febuxostat- most common side-effects
diarrheaheadaches
rashes
nausea (feeling sick)
abnormal liver test results
an increase in gout symptoms
71.
72. Uricosuric therapy probenecid, sulfinpyrasone
blocks tubular reabsorption of uric acidenhances urine uric acid excretion
increases urine uric acid level
decreases serum uric acid level
73. Uricosuric therapy
contra-indications– history of nephrolithiasis
– elevated urine uric acid level
– existing renal disease
less effective in elderly patients
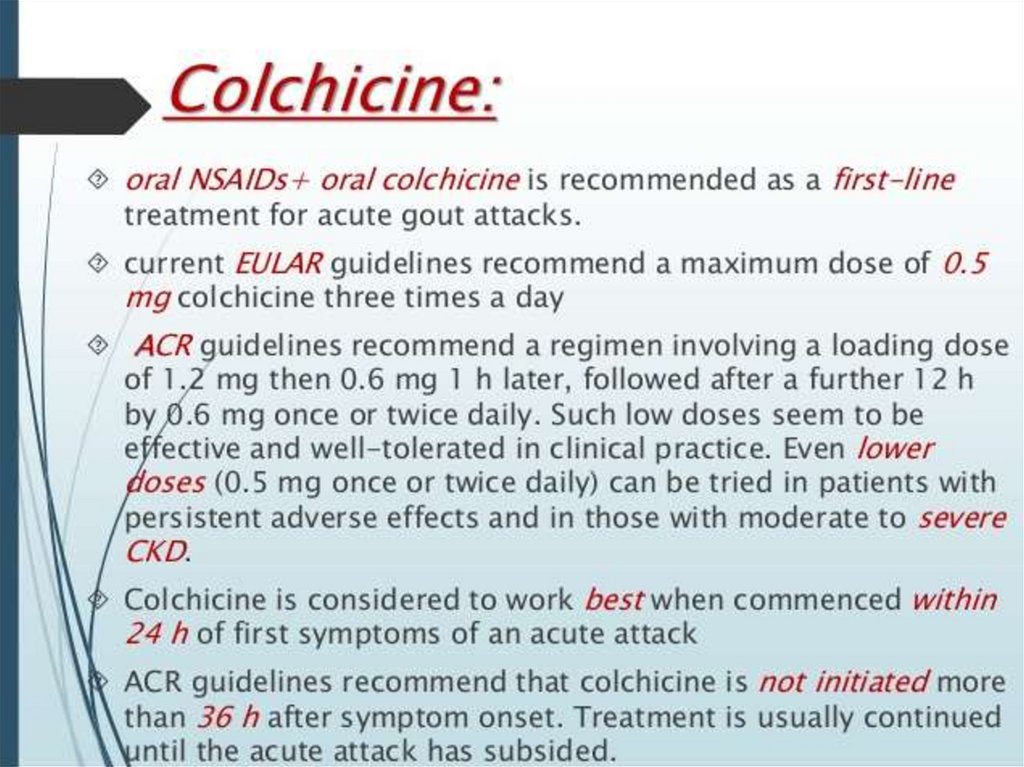
74. Final EULAR 2016 Gout Management Recommendations
Final EULAR 2016 GoutManagement Recommendations
Acute gout flares should be treated as soon as diagnosed.
First line options identified for acute flare
include: colchicine, loading dose of 1 mg, 0.5 mg on day 1,
or a nonsteroidal antiinflammatory drug (NSAID), oral
corticosteroids (equivalent prednisolone dose of 30–35
mg/day for 3–5 days), or joint aspiration with intraarticular
injection of corticosteroids. Avoid colchicine and NSAID
administration in patients with renal impairment.
Interleukin(IL)-1 blockers should be considered in patients
with both frequent disease flares and contraindications to
receiving colchicine, NSAIDs, or corticosteroids.
75.
Urate-lowering therapy (ULT) should be accompanied byprophylaxis in the first 6 months of treatment. This panel
recommends colchicine, at a dose of 0.5–1 mg/day, with
adjustments for renal impairment. When colchicine is not
tolerated well or is contraindicated, prophylaxis with NSAIDs
at a low dosage can be considered.
Patients with definitive gout diagnosis and ≥2 gout
flares/year, tophi, urate arthropathy, or recurrent kidney
stones should be considered for ULT. Patients who are <40
years old or have SUA levels >8 mg/dL (480 µmol/L), or
other comorbidities should receive early ULT.
SUA targets of <6 mg/dL (360 µmol/L) should be targeted
with ULT therapy, SUA targets of <5 mg/dL (300 µmol/L)
may be appropriate in patients with severe gout. Long-term
SUA levels of <3 mg/dL are generally not recommended.
Initiation of low-dose ULTs are recommended, with upward
titration until SUA goal is attained.
76.
Allopurinol is recommended by the task force as first-line ULT,beginning with 100 mg/day and increasing by 100 mg
increments every 2–4 weeks if needed to attain SUA goal.
Febuxostat or a uricosuric should be started if allopurinol alone
cannot be used to attain target SUA, or if it is not well tolerated.
Creatinine clearance should be used to adjust allopurinol
maximum daily doses for patients with renal impairment.
When target SUA levels cannot be attained in patients with
debilitating chronic tophaceous gout and crystal-proven disease,
pegloticase is indicated.
If a patient presents with gout and is on loop or thiazide
diuretics, it is recommended that the diuretic be switched.
Losartan or calcium channel blockers should be considered to
replace diuretic indicated for hypertension and a statin should be
considered for hyperlipidemia.
77. Duration of therapy
NSAIDsLocal
steroids
NSAIDs
colchicine (low-dose)
allopurinol
days 1-10
days 11-365
days 365+
78.
OSTEOARTHRITIS(Osteoarthrosis)
79. Definition
Osteoarthritis is a type of arthritis withaltered hyaline cartilage of one or more
joints and characterized by loss of
articular cartilage and hypertrophy of
bone, producing osteophytes.
Degenerative joint disease or
Osteoarthrosis or Hypertrophyc
Osteoartritis
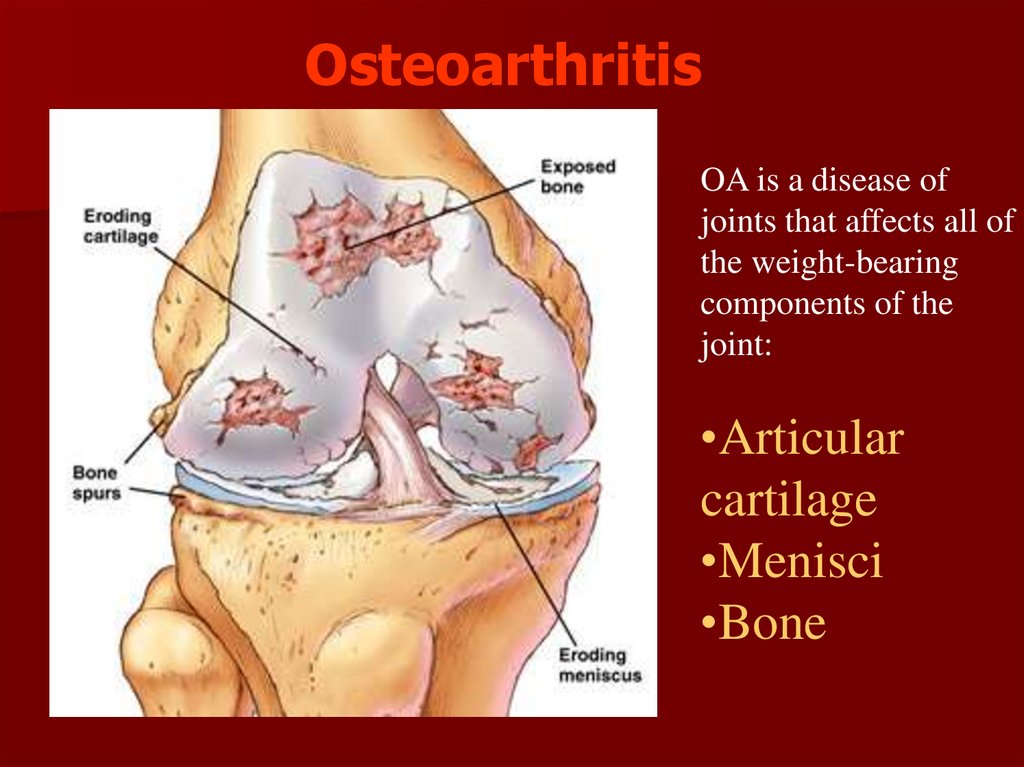
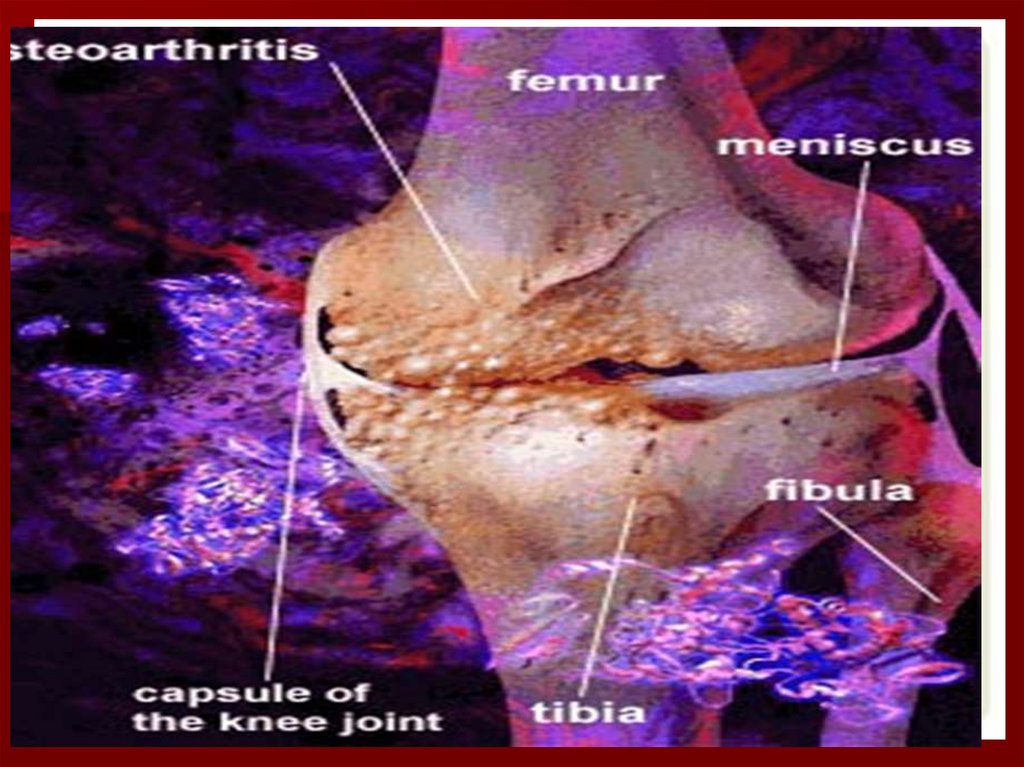
80. Osteoarthritis
OA is a disease ofjoints that affects all of
the weight-bearing
components of the
joint:
•Articular
cartilage
•Menisci
•Bone
81. Epidemiology
Most prevalent rheumatic diseaseEnormous disability and loss of productivity
Prevalence and severity increases with age
Degree of OA almost universal > 75 years
True incidence unknown
Women more often affected especially nodal
OA
82. Pathophysiology
Biomechanical and biochemical forces are involved incartilage destruction, which is at the core of osteoarthritis.
Cytokines and growth factors are thought to play a role
in the pathophysiology of the disorder.
IL-1 and TNF-β may function to activate enzymes
involved in proteolytic digestion of cartilage.
Growth factors such as tissue growth factor-β and insulin
growth factor-1 may play a role in the body's attempts to
repair cartilage through cartilage synthesis.
When catabolism exceeds cartilage synthesis, osteoarthritis
develops.
Collagenolytic enzymes are thought to contribute to the
breakdown of cartilage.
Collagenase 1 (matrix metalloproteinase-1 [MMP-1]) is a
fibroblast collagenase, and collagenase 2 (MMP-8) is a
neutrophil collagenase. Collagenase 3 (MMP-13) may be
particularly important because of its highly potent
collagenolytic activity.
83. Pathology of Osteoarthritis Biochemical Abnormalities
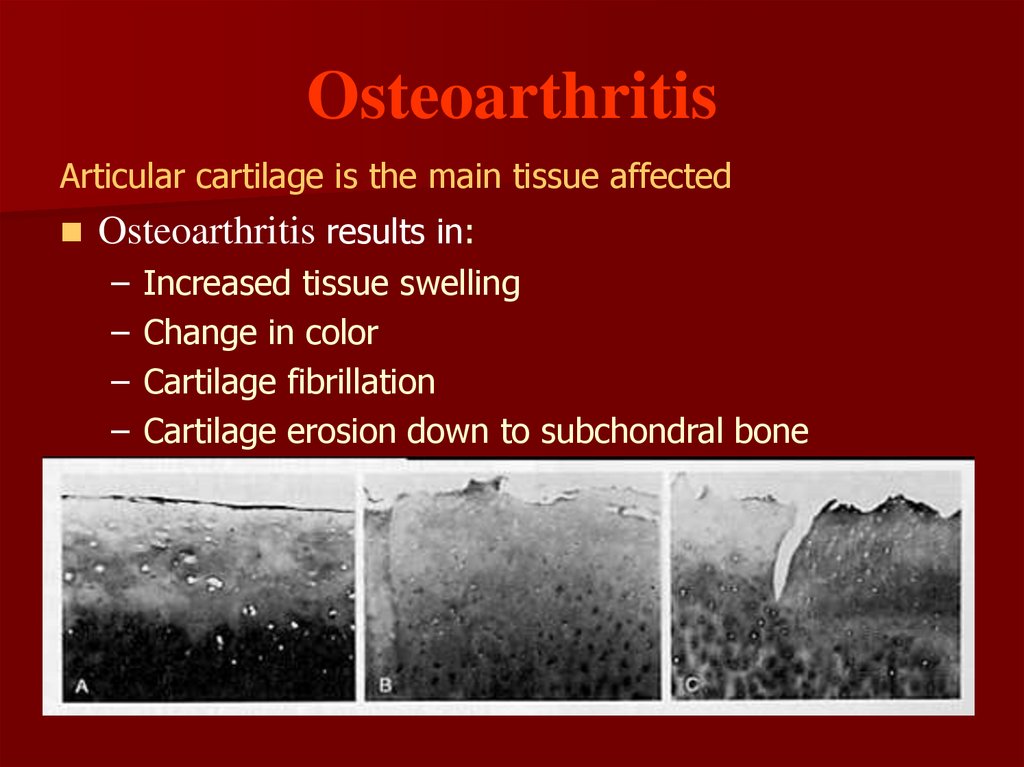
84. Osteoarthritis
Articular cartilage is the main tissue affectedOsteoarthritis results in:
–
–
–
–
Increased tissue swelling
Change in color
Cartilage fibrillation
Cartilage erosion down to subchondral bone
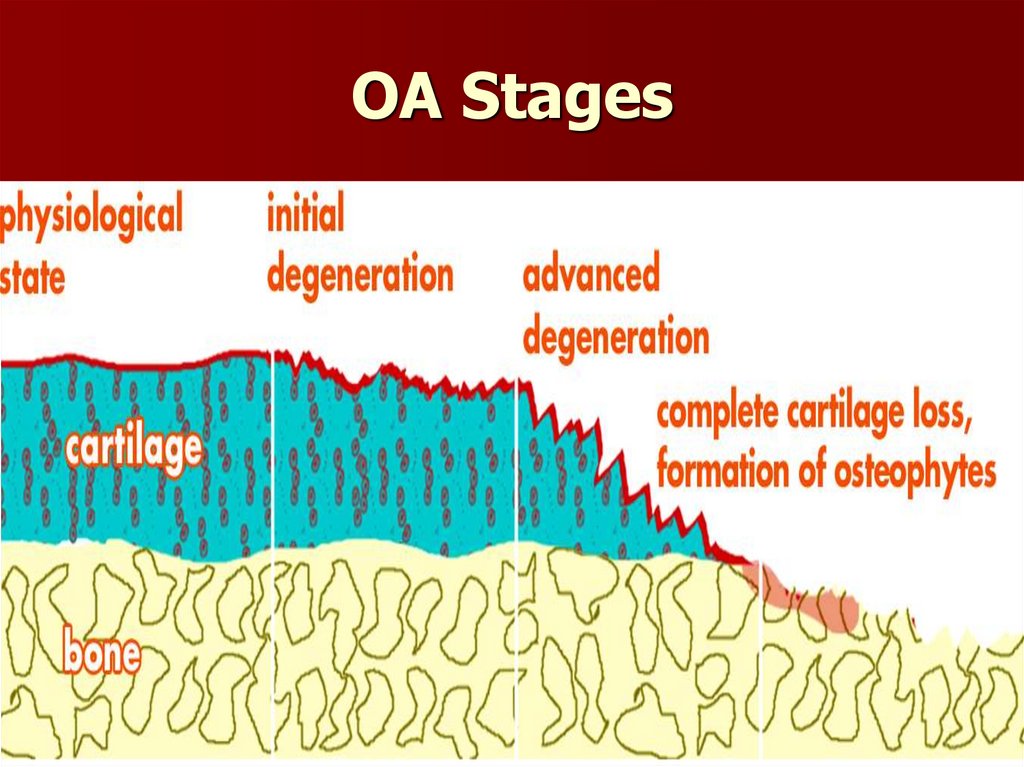
85. OA Stages
86. Osteoarthritis – Articular Cartilage
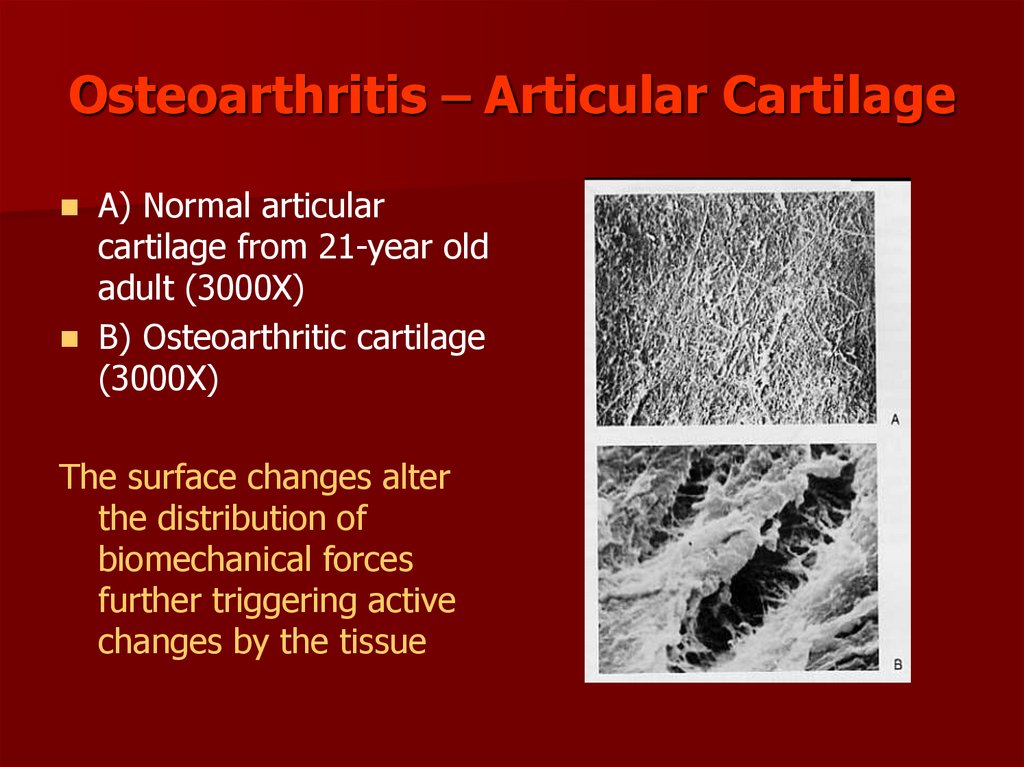
A) Normal articularcartilage from 21-year old
adult (3000X)
B) Osteoarthritic cartilage
(3000X)
The surface changes alter
the distribution of
biomechanical forces
further triggering active
changes by the tissue
87. Primary Risk Factors
AgeGender
Race
Occupation (related to chronic overuse)
Obesity
History of joint trauma
Bone or joint disorders
Genetic mutations of collagen
History of inflammatory arthritis
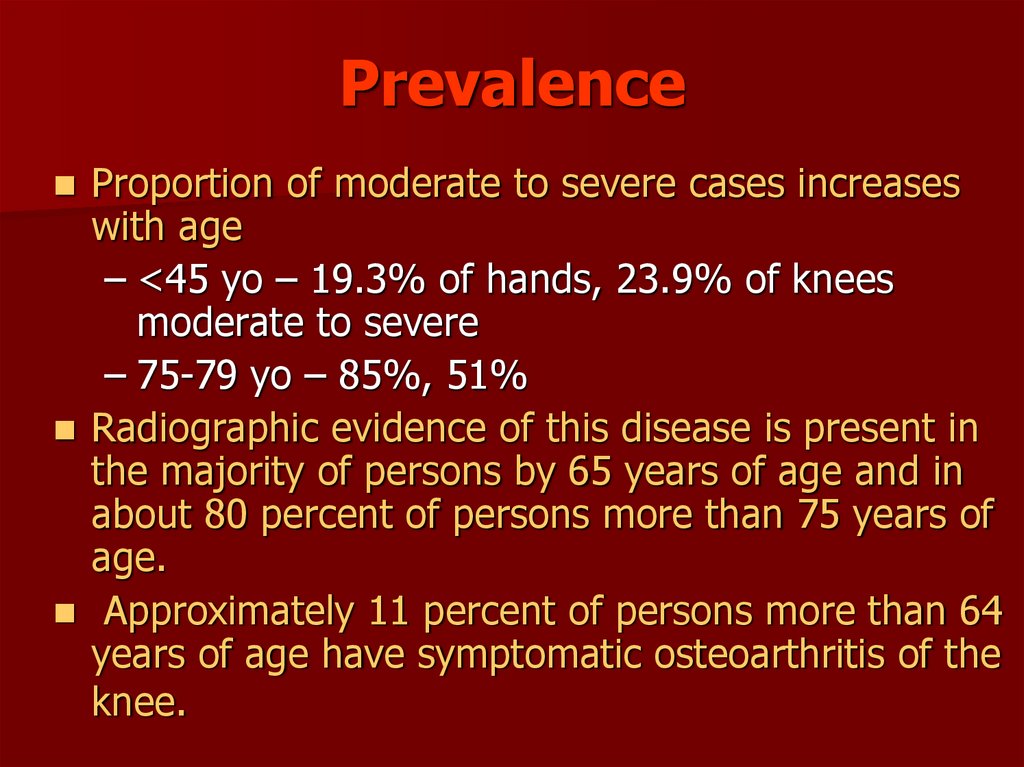
88. Prevalence
Proportion of moderate to severe cases increaseswith age
– <45 yo – 19.3% of hands, 23.9% of knees
moderate to severe
– 75-79 yo – 85%, 51%
Radiographic evidence of this disease is present in
the majority of persons by 65 years of age and in
about 80 percent of persons more than 75 years of
age.
Approximately 11 percent of persons more than 64
years of age have symptomatic osteoarthritis of the
knee.
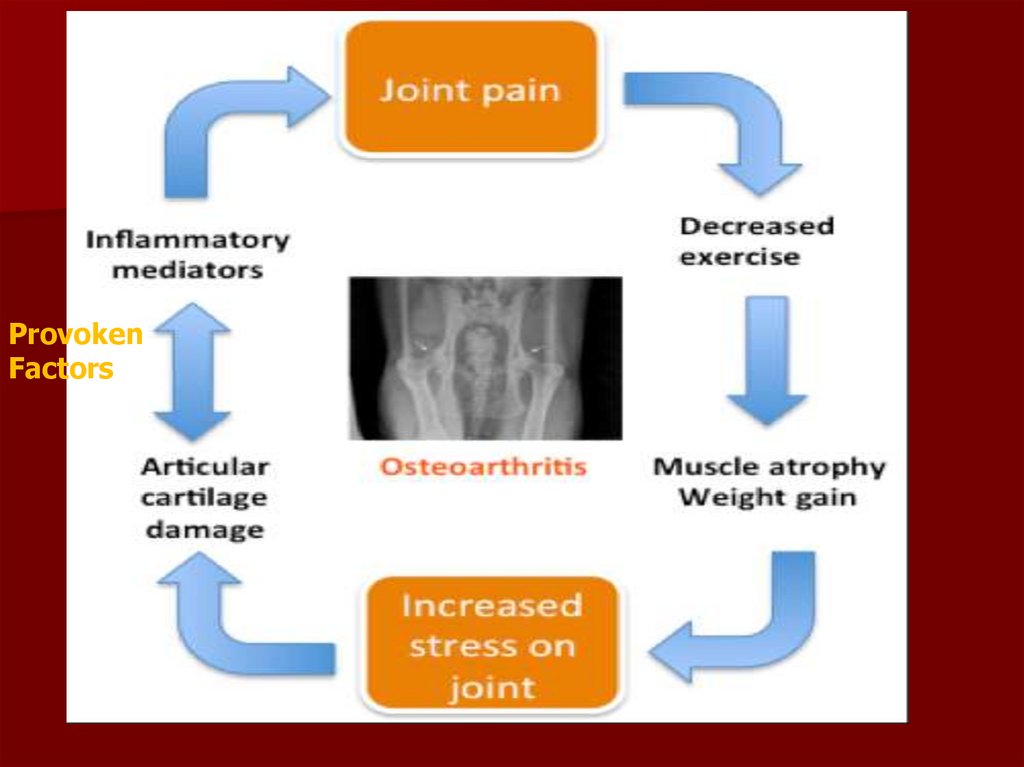
89.
ProvokenFactors
90. Two Major Types of Osteoarthritis
Primary or Idiopathic– Most common type
– Diagnosed when there is no known cause
for the symptoms
Secondary
– Diagnosed when there is an identifiable
cause
– Trauma or Underlying joint disorder
Each of these major types has subtypes
91. Clinical Features of Osteoarthritis
SymptomsJoint pain
Morning stiffness lasting less than 30 minutes
Joint instability or buckling
Loss of function
Signs
Bony enlargement at affected joints
Limitation of range of motion
Crepitus on motion
Pain with motion
Malalignment and/or joint deformity
Pattern of joint involvement
Axial: cervical and lumbar spine
Peripheral: distal interphalangeal joint, proximal
interphalangeal joint, first carpometacarpal joints, knees,
hips
92. PAIN
No nerve supply to the articular cartilagePain may be associated with the following:
Inflammation of the synovium
Medullary hypertension
Microfractures in the subchondral bone
Stretching of periostal nerve endings by
osteophytes (spurs)
Stretching of ligaments
Spasming of muscles around the inflamed joint
capsule
93. Classification Criteria for Osteoarthritis of the Hip
Hip pain plus at least two of the following:-ESR of less than 20 mm per hour
-Femoral or acetabular osteophytes on radiographs
-Joint space narrowing on radiographs
Hip pain plus femoral or acetabular
osteophytes on radiographs
or
Hip pain plus joint space narrowing on
radiographs and an ESR of less than 20
mm per hour.
94. Classification Criteria for Idiopathic Osteoarthritis of the Knee
Knee pain plus osteophytes on radiographs and atleast one of the following:
-Patient age older than 50 years
-Morning stiffness lasting 30 minutes or less
-Crepitus on motion
Knee pain and osteophytes on radiographs
or
Knee pain plus patient age of 40 years or older,
morning stiffness lasting 30 minutes or less and
crepitus on motion
95. Knee Osteoarthritis
may involve medial or lateral femoratibialcompartment and or patellafemoral
compartment
varus (bow-leg) deformity (medial
compartment)
valgus (knock-knee) deformity (lateral
compartment)
“shug sign”- patellofemoral OA
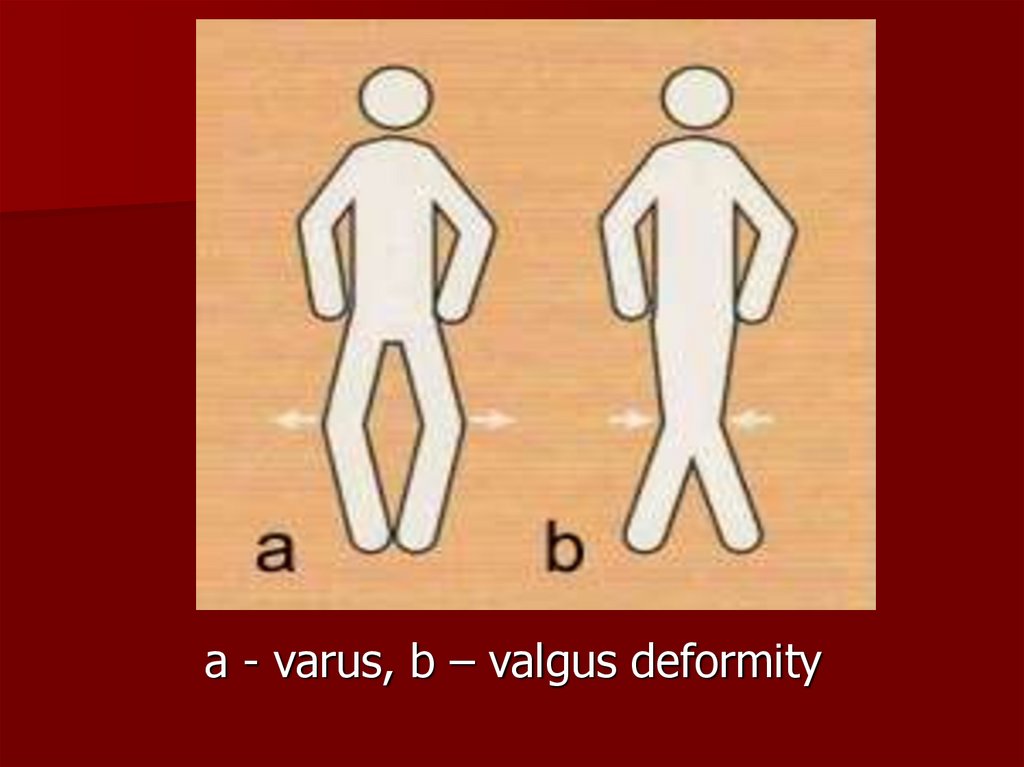
96.
a - varus, b – valgus deformity97.
98. Classification Criteria for Osteoarthritis of the Hand
Hand pain or stiffnessplus
Hard tissue enlargement of two or more of 10
selected joints
plus
Fewer than three swollen metacarpophalangeal
joints
plus
Hard tissue enlargement of two or more distal
interphalangeal joints
or
Deformity of two or more of 10 selected joints
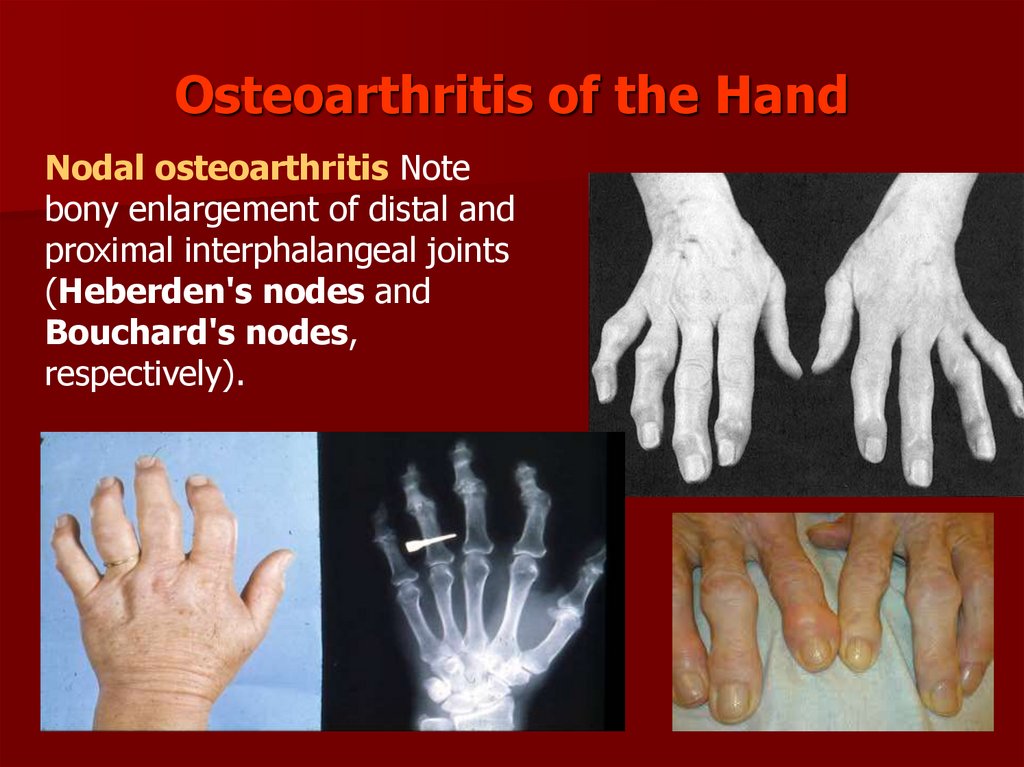
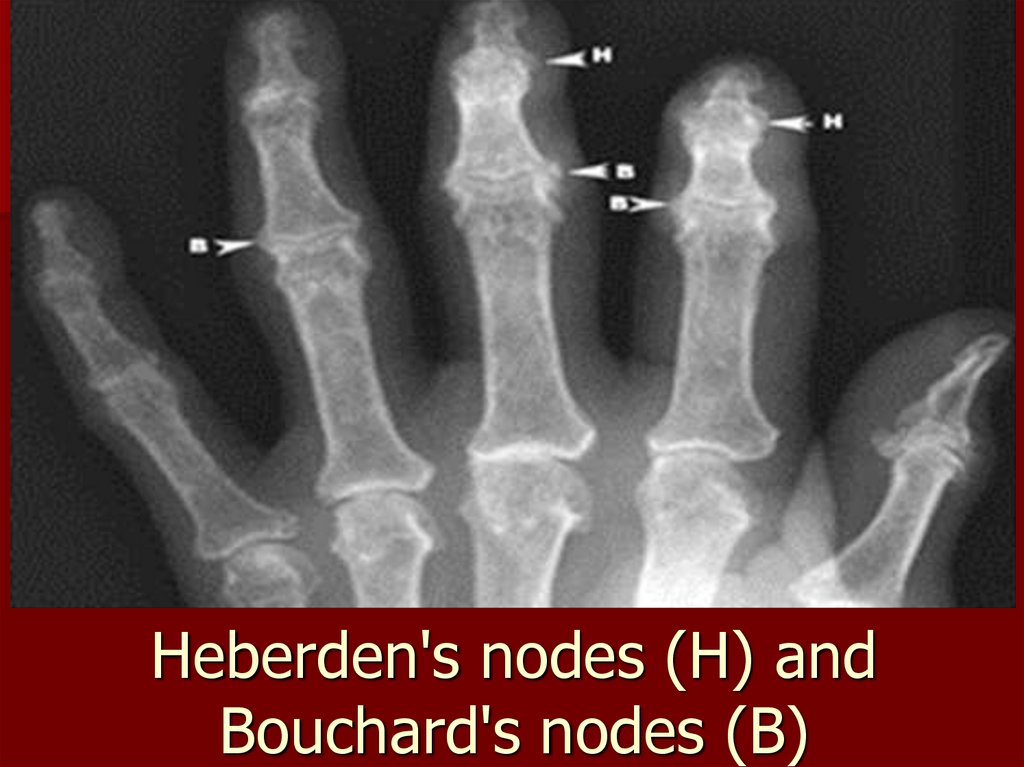
99. Osteoarthritis of the Hand
Nodal osteoarthritis Notebony enlargement of distal and
proximal interphalangeal joints
(Heberden's nodes and
Bouchard's nodes,
respectively).
100. WOMAC OA index
Western Ontario and Mc-MasterUniversity (WOMAC) osteoarthritis
index to determine function, quality
of life, and joint pain.
on a scale that ranges from 0 (no
pain or stiffness) to 500 (extreme
pain, stiffness, and impaired
function).
101. Laboratory findings
No specific testESR normal or slightly elevated
Rheumatoid factor negative
Haematological and biochemical
surveys usually normal
No systemic manifestations
102. Radiological findings
Early in disease• X-ray changes often absent
Progression of OA
• Narrowing or complete loss of joint
space
• Sclerosis and cysts in adjacent bones
• Osteophytes: bony overgrowth
Late OA
• Effusions, abnormal alignment
103. Kellgren-Lawrence Score
A score of 0 (none)– no osteoarthritic features
A score of 1 (doubtful)
– single osteophytes of doubtful importance.
A score of 2 (minimal)
– definite osteophytes without reduction of the joint
space.
A score of 3 (moderate)
– decreased joint space, osteophytes
A score of 4 (severe)
– greatly reduced joint space and sclerosis of the
subchondral bone; ankylosis.
104.
105.
Osteoarthritis –radiographicdiagnosis
•Asymmetrical
joint space
narrowing
•Periarticular
sclerosis
•Osteophytes
•Subchrondral
bone cysts
106.
107.
108. Heberden's nodes (Н) and Bouchard's nodes (В)
109.
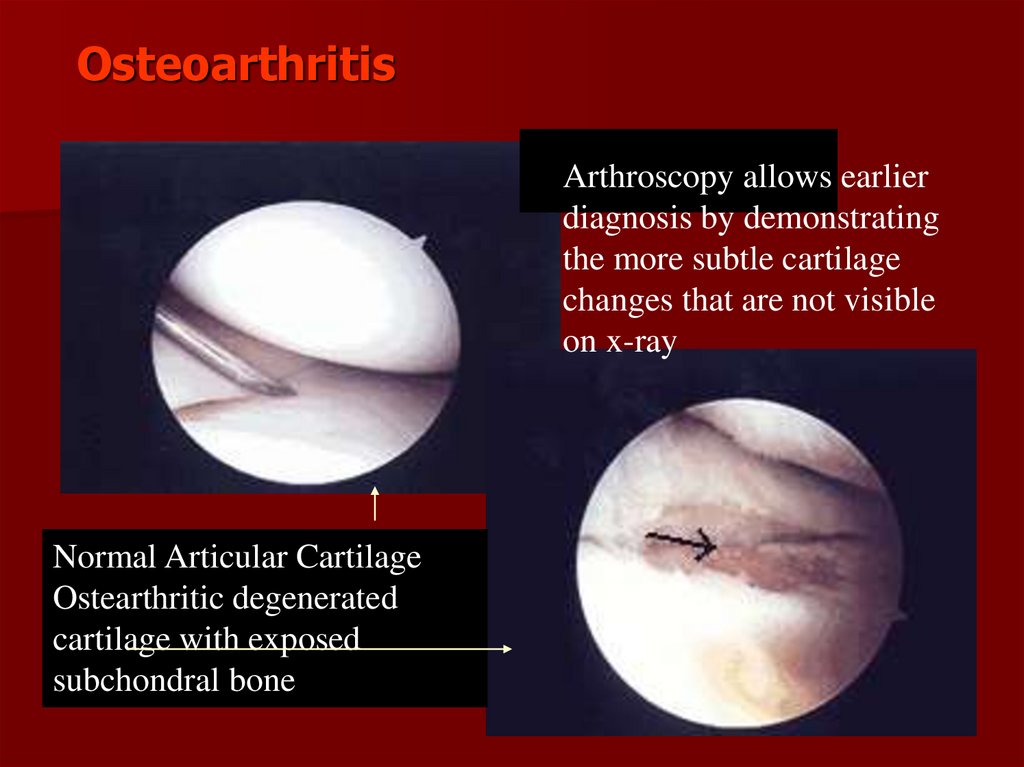
OsteoarthritisArthroscopy allows earlier
diagnosis by demonstrating
the more subtle cartilage
changes that are not visible
on x-ray
Normal Articular Cartilage
Ostearthritic degenerated
cartilage with exposed
subchondral bone
110. American College of Rheumatology Guidelines
“Thegoals of osteoarthritis (OA)
management are to control pain and
other symptoms, minimise disability,
and educate the patient about the
disease and its therapy.”
111. How we achieve the goals…
1.2.
3.
4.
5.
6.
Treatment approach individualised to
include:
Patient education
Physiotherapy
Occupational therapy
Dietary considerations
Pharmacological therapy
Surgery
112.
113. PHARMACOLOGIC NONPHARMACOLOGIC
TREATMENTPHARMACOLOGIC
NONPHARMACOLOGIC
114.
115. Patient education
Education for patient’s family, friends,other carers
Arthritis Foundation Self-Management
Programs
Decreased joint pain
Frequency of arthritis-related visits to the
doctor
Increases in physical activity and overall
improvement in quality of life
116.
Education117.
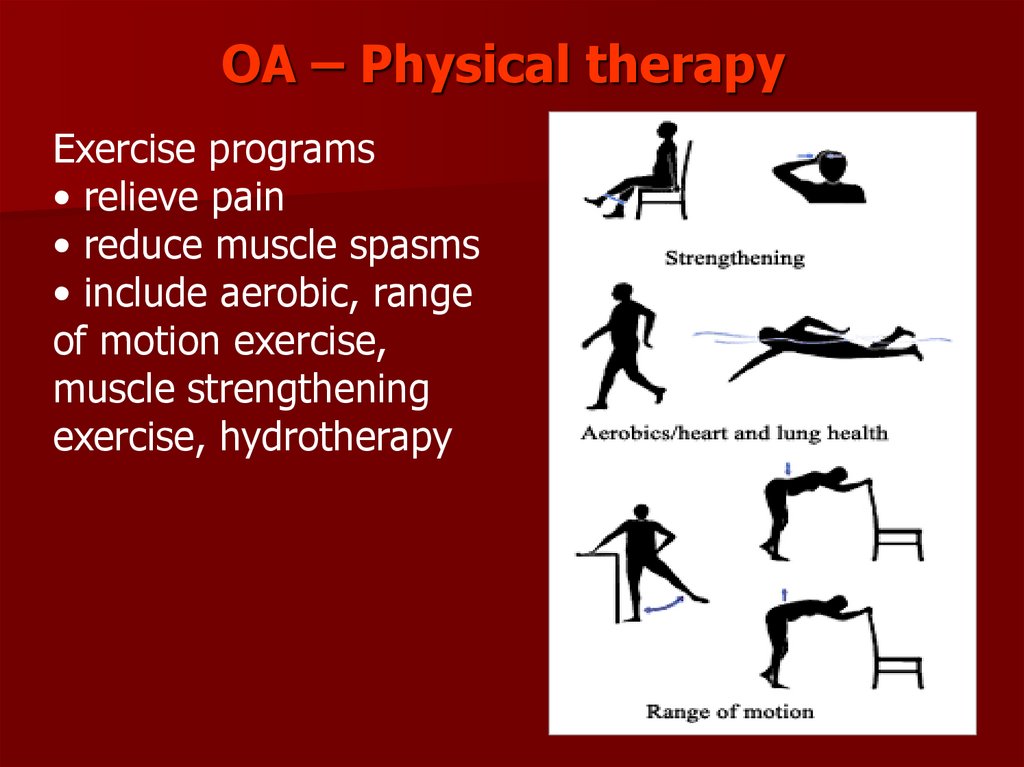
OA – Physical therapyExercise programs
• relieve pain
• reduce muscle spasms
• include aerobic, range
of motion exercise,
muscle strengthening
exercise, hydrotherapy
118. Occupational Therapy
Patellar taping (for knee OA),appropriate footwear and bracing
Assistive devices for activities of daily
living
119. American College of Rheumatology 2012 Guidelines for OA of the Knee
Nonpharmacologic ModalitiesAcetaminophen
At increased risk
for an upper GI adverse event
Not at risk
for an upper GI adverse event
Viscosupplements
COX-2–specific inhibitor
NSAID and GI-protective agent
Glucocorticoid injection
Surgery
Viscosupplements
COX-2–specific inhibitor
Low-dose NSAID
Glucocorticoid injection
120. Pharmacological therapy
Considered an addition tononpharmacological measures
Paracetamol (2g/day, could be increase to
4g/day not more 5 days)
NSAIDs and COX-2 selective agents
Glucosamine and chondroitin
Intra-articular corticosteroids and
hyaluronan
Opioid analgesia
121. Management: Medical
Acetaminophen–
–
–
–
Indication: mild-moderate pain
1000 mg Q6h PRN
Better than placebo but less efficacious than NSAIDs
Caution in advanced hepatic disease
NSAIDs
–
–
–
–
Indication: moderate-severe pain, failed acetaminophen
GI/renal/hepatic toxicity, fluid retention
If risk of GIB, use anti-ulcer agents concurrently
Agents have highly variable efficacy and toxicity
122. Management: Medical
Cox-2 inhibitors–
–
–
–
–
–
Indication: mod-severe pain, failed NSAID, risk of GIB
OA pain relief similar to NSAIDs
Fewer GI events e.g. symptomatic ulcers, GIB
Celecoxib 200 mg daily
GI/renal toxicity, fluid retention
Increased risk of CV events?
APC Trial: 700 pts each assigned to placebo, 200 BID, 400 BID
– Increased risk at higher doses
CLASS Trial: 8,000 pts compared Celecoxib vs Ibuprofen
– Similar risk to Ibuprofen
123. Glucosamine and chondroitin
Naturally occurring components of jointcartilage
Glucosamine and chondroitin: proposed to
stop and possibly reverse degenerative
process in OA
– Glucosamine: may stimulate proteoglycan
synthesis or inhibit degradation of existing
cartilage 1500 mg/day
– Chondroitin: may stimulate cartilage
synthesis or inhibit enzymes that degrade
cartilage 800 mg/day
124. Intraarticular corticosteroids
effective if 1 or 2 joints affectedup to 6 wks decreased pain, increased
function
Generally not monotherapy
Low risks if appropriate sterile technique
applied
Effective short-term treatment
125. Intraarticular Injections
Glucocorticoids– Indication: pain persists despite oral analgesics
– 40 mg/mL triamcinolone (kenalog-40)
– Solution: 5 mL (lidocaine 4 mL + kenalog 1 mL)
– Limit to Q3months, up to 2 yrs
– Effective for short-term pain relief < 12 wks
– Acute flare w/in 48 hrs post-injection
126.
Intraarticular injection127.
Intraarticular injection128. ORTHOPEDIC TREATMENT
129. Surgery use to treat Osteoarthritis
Surgical treatment of osteoarthritis may include thereplacement of a damaged joint with an artificial part
or appliance; surgical fusion of spinal bones; scraping
or removal of damaged bone from the joint; or the
removal of a piece of bone in order to realign the
bone.
arthroplasty (total or partial replacement of the deteriorated
joint with an artificial joint
arthroscopic surgery to trim torn and damaged cartilage and
wash out the joint
osteotomy (change in the alignment of a bone to relieve
stress on the bone or joint)
arthrodesis (surgical fusion of bones, usually in the spine)
130.
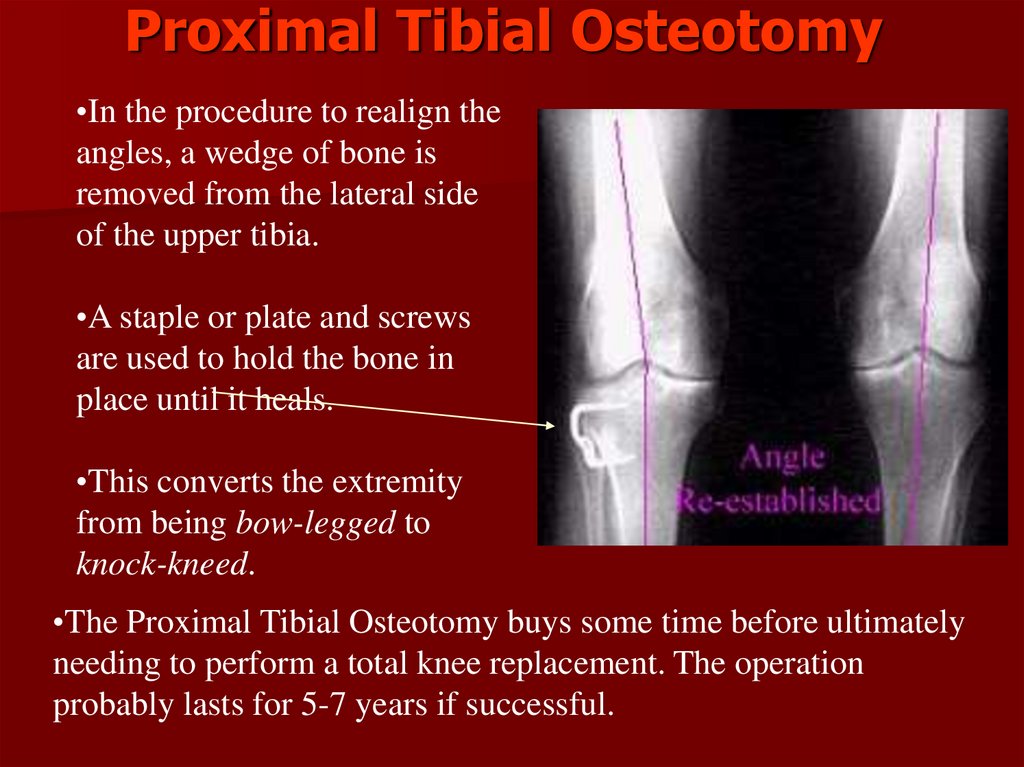
Proximal Tibial Osteotomy•In the procedure to realign the
angles, a wedge of bone is
removed from the lateral side
of the upper tibia.
•A staple or plate and screws
are used to hold the bone in
place until it heals.
•This converts the extremity
from being bow-legged to
knock-kneed.
•The Proximal Tibial Osteotomy buys some time before ultimately
needing to perform a total knee replacement. The operation
probably lasts for 5-7 years if successful.
131.
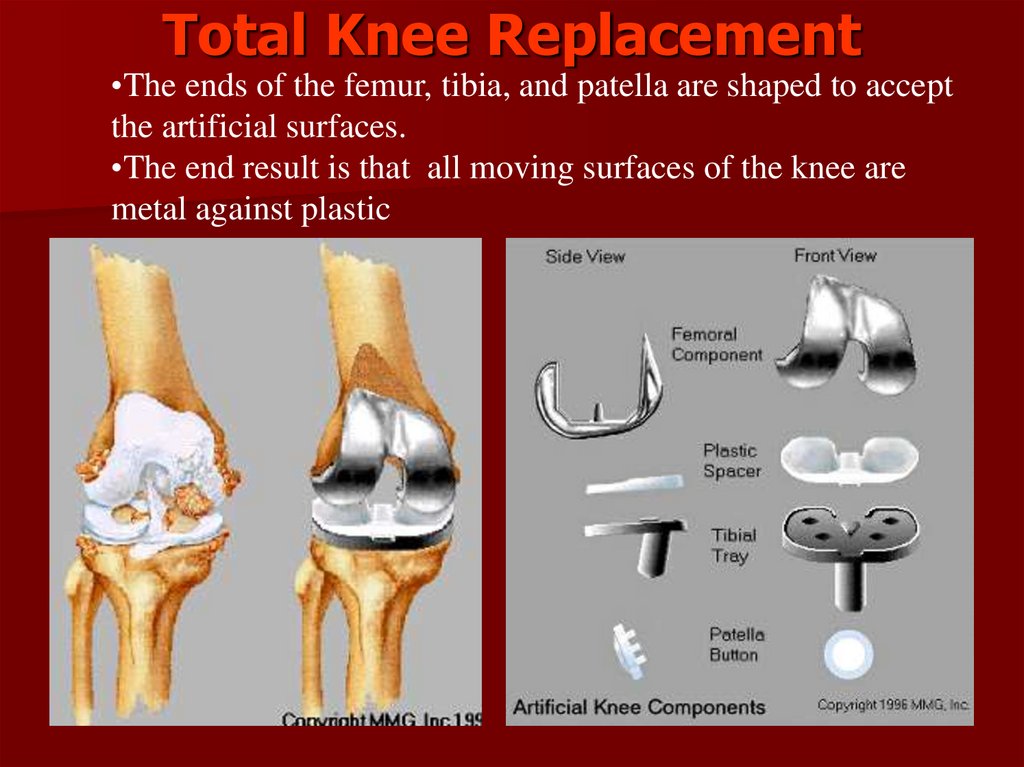
Total Knee Replacement•The ends of the femur, tibia, and patella are shaped to accept
the artificial surfaces.
•The end result is that all moving surfaces of the knee are
metal against plastic
132.
Total Knee ReplacementPhotographs of total knee
components on model
bone



































































 medicine
medicine