Similar presentations:
Deformation Polyosteoarthriosis
1.
deformationpolyosteoarthriosis
LECTURER: ALBERT ANTWI 1751
PROFESOR: DR.ELENA CHUGAY
2.
CONTENTSDefinition
.
Causes
Clinical pictures
Diagnosis
.
Treatment
3.
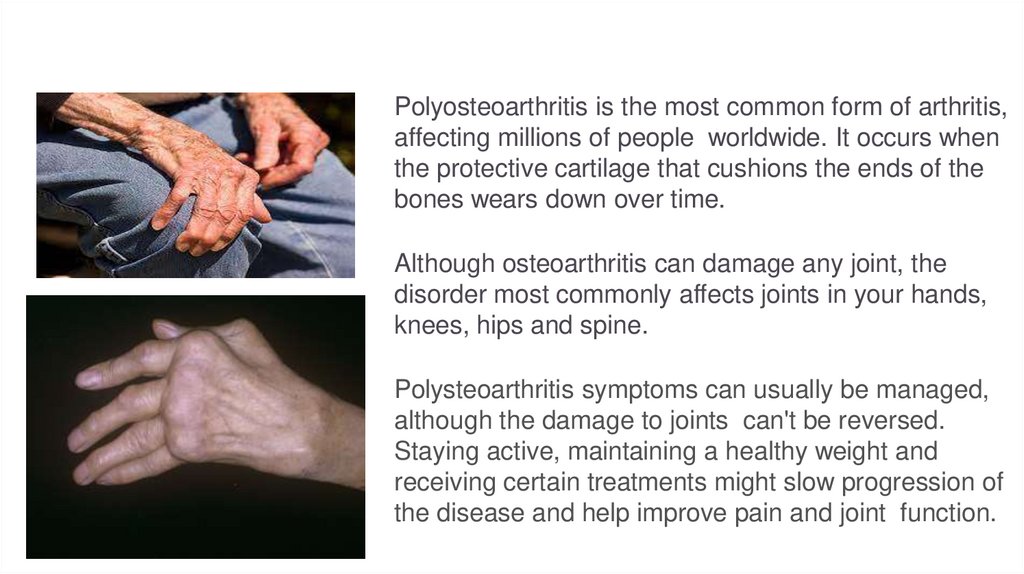
Polyosteoarthritis is the most common form of arthritis,affecting millions of people worldwide. It occurs when
the protective cartilage that cushions the ends of the
bones wears down over time.
Although osteoarthritis can damage any joint, the
disorder most commonly affects joints in your hands,
knees, hips and spine.
Polysteoarthritis symptoms can usually be managed,
although the damage to joints can't be reversed.
Staying active, maintaining a healthy weight and
receiving certain treatments might slow progression of
the disease and help improve pain and joint function.
4.
Polyosteoarthritis is a term used when five or more jointsare affected with joint pain. There are many potential
causes, so symptoms can vary widely from person to
person. Polyarthritis can present as acute episodes or it
may become chronic, lasting for more than six weeks.
5.
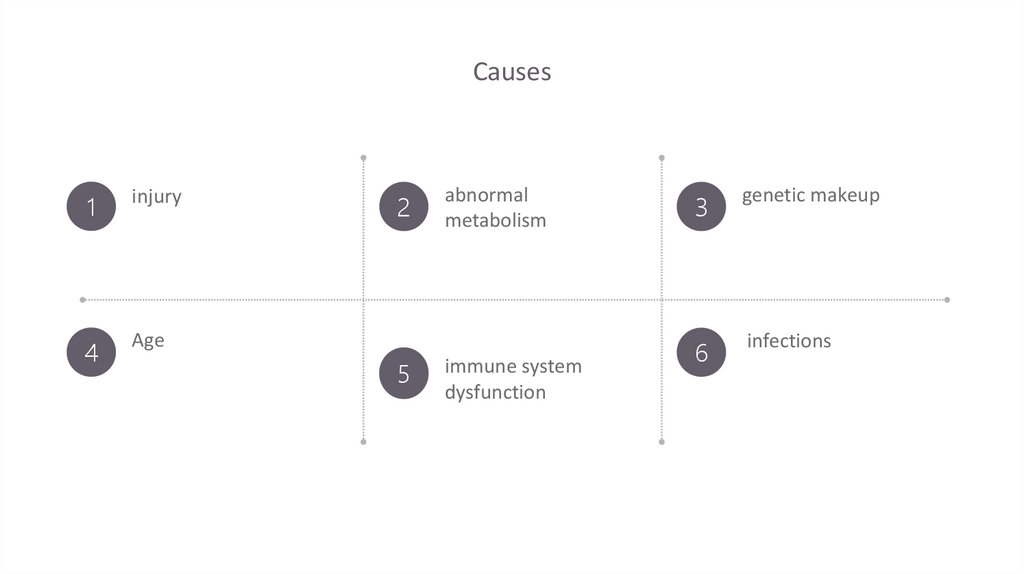
Causes1
injury
4
Age
2
5
abnormal
metabolism
immune system
dysfunction
3
genetic makeup
6
infections
6.
CLINICAL FEATURESPain. Affected joints of patient hurt during or after movement.
Stiffness. patient Joint stiffness is noticeable upon awakening or after being inactive.
Tenderness. patient joint might feel tender when you apply light pressure to or near it.
Loss of flexibility. patient might not be able to move joint through its full range of motion.
Grating sensation. patient feel a grating sensation when you use the joint, and you can hear popping.
Bone spurs. These extra bits of bone, which feel like hard lumps, can form around the affected joint.
Swelling. patient can have soft tissue inflammation around the joint.
7.
PART 01REPAIR OF SHOUIDER AND NECK
The user can perform the presentation on a projector or computer, and the powerpoint can be printed out and made into film.
Please enter title
PART 01
8.
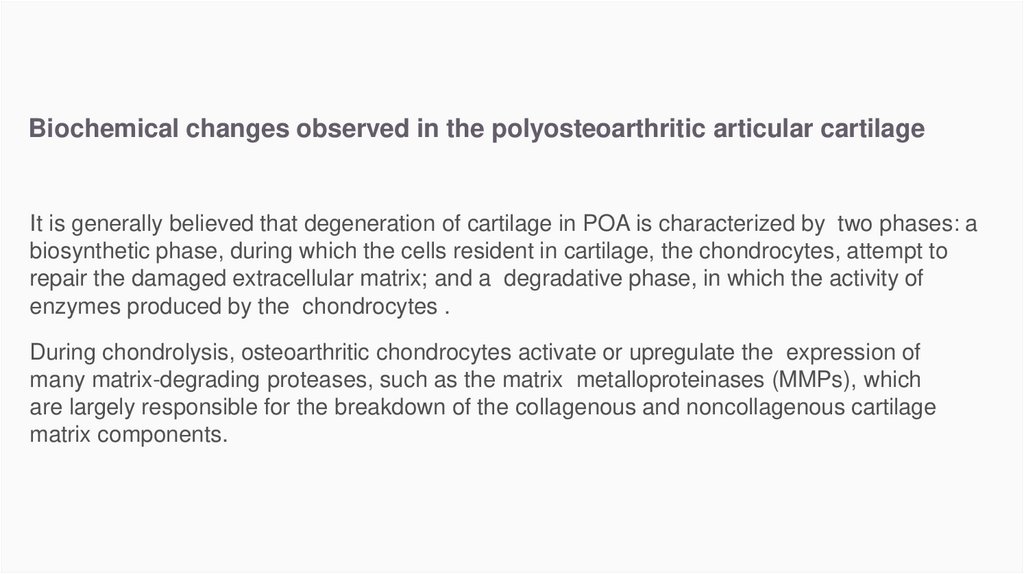
Biochemical changes observed in the polyosteoarthritic articular cartilageIt is generally believed that degeneration of cartilage in POA is characterized by two phases: a
biosynthetic phase, during which the cells resident in cartilage, the chondrocytes, attempt to
repair the damaged extracellular matrix; and a degradative phase, in which the activity of
enzymes produced by the chondrocytes .
During chondrolysis, osteoarthritic chondrocytes activate or upregulate the expression of
many matrix-degrading proteases, such as the matrix metalloproteinases (MMPs), which
are largely responsible for the breakdown of the collagenous and noncollagenous cartilage
matrix components.
9.
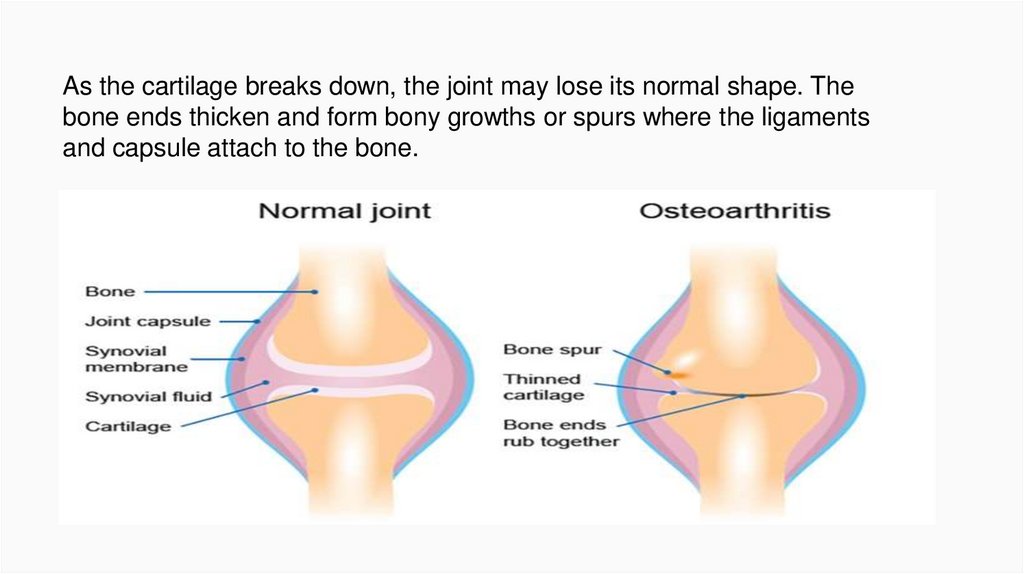
As the cartilage breaks down, the joint may lose its normal shape. Thebone ends thicken and form bony growths or spurs where the ligaments
and capsule attach to the bone.
10.
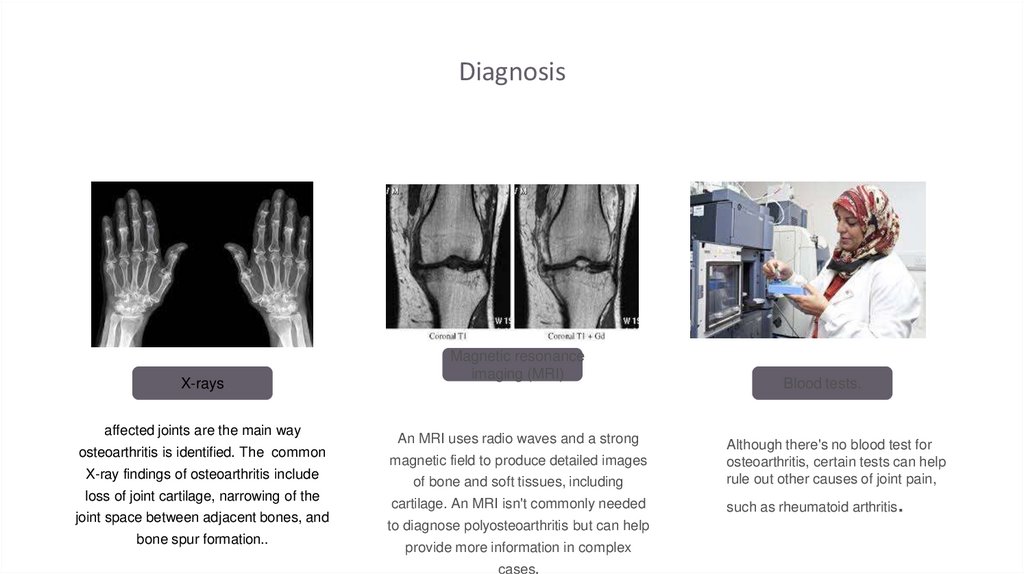
DiagnosisX-rays
affected joints are the main way
osteoarthritis is identified. The common
X-ray findings of osteoarthritis include
loss of joint cartilage, narrowing of the
joint space between adjacent bones, and
bone spur formation..
Magnetic resonance
imaging (MRI)
An MRI uses radio waves and a strong
magnetic field to produce detailed images
of bone and soft tissues, including
cartilage. An MRI isn't commonly needed
to diagnose polyosteoarthritis but can help
provide more information in complex
cases.
Blood tests.
Although there's no blood test for
osteoarthritis, certain tests can help
rule out other causes of joint pain,
.
such as rheumatoid arthritis
11.
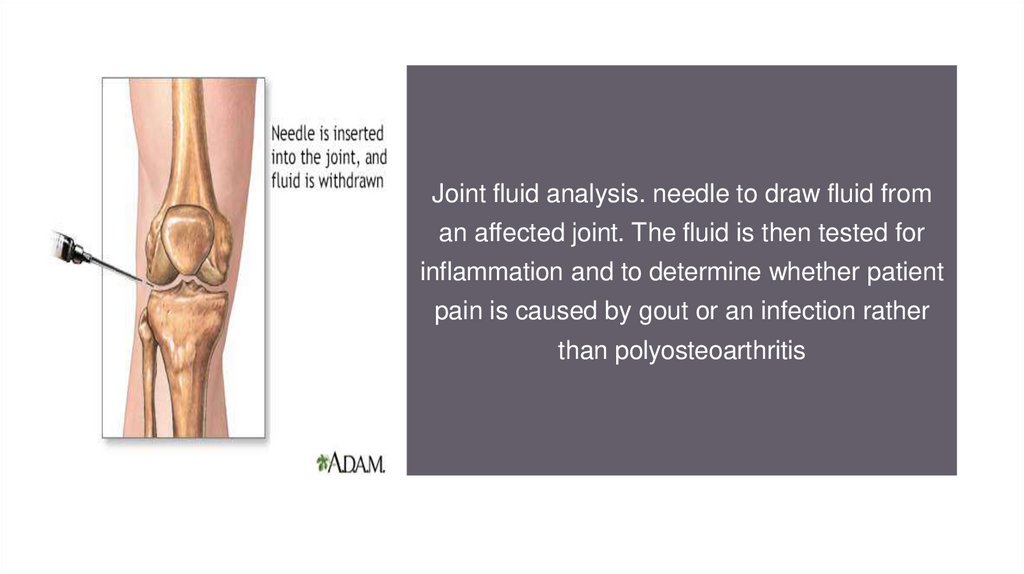
Joint fluid analysis. needle to draw fluid froman affected joint. The fluid is then tested for
inflammation and to determine whether patient
pain is caused by gout or an infection rather
than polyosteoarthritis
12.
TreatmentMedications that can help relieve polyosteoarthritis symptoms, primarily pain,
include:
Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help
patients with osteoarthritis who have mild to moderate pain. Taking more than
the recommended dose of acetaminophen can cause liver damage.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs, such
as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), taken at the
recommended doses, typically relieve osteoarthritis pain. Stronger NSAIDs are
available by prescription.
NSAIDs can cause stomach upset, cardiovascular problems, bleeding problems,
and liver and kidney damage. NSAIDs as gels, applied to the skin over the
affected joint, have fewer side effects and may relieve pain just as well.
13.
TherapyPhysical therapy. patient should exercise to strengthen the muscles around
their joint, increase flexibility and reduce pain. Regular gentle exercise on their
own, such as swimming or walking, can be equally effective.
Occupational therapy. patients should perform tasks without putting extra stress on
painful joints. For instance, a toothbrush with a large grip could make brushing
your teeth easier if you have osteoarthritis in your hands. A bench in your shower
could help relieve the pain of standing if you have knee osteoarthritis
14.
SurgeryLubrication injections. Injections of hyaluronic acid might relieve pain by
providing some cushioning in your knee, though some research suggests that
these injections offer no more relief than a placebo. Hyaluronic acid is similar
to a component normally found in your joint fluid.
Realigning bones. If polyosteoarthritis has damaged one side of your knee
more than the other, an osteotomy might be helpful. In a knee osteotomy, a
surgeon cuts across the bone either above or below the knee, and then
removes or adds a wedge of bone. This shifts your body weight away from the
worn-out part of your knee.
Joint replacement. In joint replacement surgery, your surgeon removes your
damaged joint surfaces and replaces them with plastic and metal parts.
Surgical risks include infections and blood clots. Artificial joints can wear out
or come loose and might eventually need to be replaced.
15.
PreventionKeep a healthy body weight. Extra weight puts stress on your joints. ...
Control your blood sugar. High blood sugar levels raise your risk of getting OA.
Be active every day. Exercise is a good way to prevent joint problems. ...
16.
PrognosisThe prognosis for osteoarthritis patients depends on which joints are affected and
the level of symptomatology and functional impairment. Some patients remain
relatively unaffected by polyosteoarthritis, while others can experience severe
disability.
17.
Referenceshttps://www.mayoclinic.org/diseases-conditions/osteoarthritis/diagnosistreatment/drc-20351930
https://www.aafp.org/afp/2012/0101/p49.html
https://en.wikipedia.org/wiki/Osteoarthritis


 medicine
medicine