Similar presentations:
Non-narcotic analgesics (NNA). Non-steroidal anti-inflammatory drugs (NSAID)
1. Non-narcotic analgesics (NNA) Non-steroidal anti-inflammatory drugs (NSAID)
2.
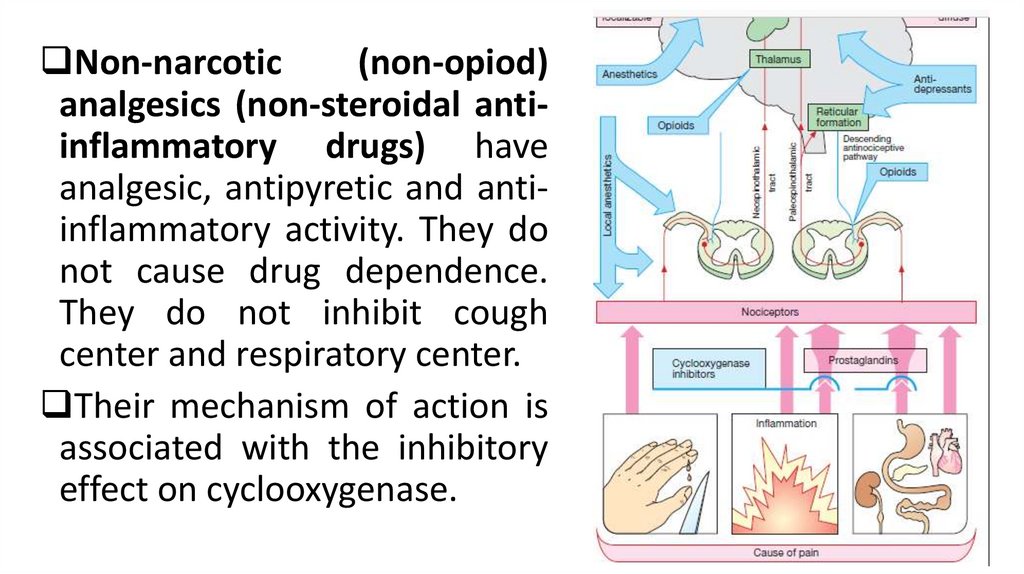
Non-narcotic(non-opiod)
analgesics (non-steroidal antiinflammatory drugs) have
analgesic, antipyretic and antiinflammatory activity. They do
not cause drug dependence.
They do not inhibit cough
center and respiratory center.
Their mechanism of action is
associated with the inhibitory
effect on cyclooxygenase.
3.
Arachidonic acid is formed under the influence ofphospholipase A2 from membrane phospholipids of the
cells.
Cyclic endoperoxides are formed from arachidonic acid
under the influence of cyclooxygenase. There are such
metabolites of arachidonic acid as prostaglandins (PGE2,
PGF2α, PGD2), prostacyclin (PGI2), thromboxane A2 (TXA2).
Leukotrienes are formed from arachidonic acid under the
influence of 5-Lipoxygenase. Leukotrienes are the main
components of SRSA – slow-reacting substance of
anaphylaxis.
4.
5.
6.
SubstanceEffects
PGE2
Inflammation, pain, fever, stimulation of the myometrium,
decrease in the tone of bronchi and peripheral vessels
PGF2Α
Stimulation of the myometrium, increase in the tone of
smooth muscles of bronchi, gastrointestinal tract
PGD2
PGI2
Decrease in the tone of mesenteric, coronary, renal
vessels, increase in the tone of pulmonary vessels;
decrease in platelet aggregation
Decrease in platelet aggregation, vasodilation
TXA2
Increase in platelet aggregation, vasoconstriction
7.
8.
There are 3 variants of cyclooxygenase: type 1,2,3.Cyclooxygenase 1 (COX1) is produced in the absence of any
pathology. It influences on the synthesis of prostaglandins,
which regulates functions of organism: platelet aggregation,
tone of vessels, tone of uterus.
In the stomach COX1 provides protective effect because
prostaglandins dilates mesenteric vessels and increases the
production of protective mucus.
in the kidneys prostaglandins increase filtration and
enhance diuresis.
9.
10.
COX2 production is, to a large extent, induced by theinflammatory process. Prostaglandins enhance the
inflammatory process and pain.
COX 3 is synthesized in the CNS. Prostaglandins are
involved in the formation and transmission of pain
impulse; and they play a role in the development of
fever also.
It is necessary to reduce the activity of Cox 2 and 3.
We should not reduce the activity of Cox 1.
11.
Classification of non-narcotic analgesics (NSAID)according to the chemical structure. Derivative of:
salicylic acid: acetylsalicylic acid (aspirin)
pyrazolone: metamizole
paraaminophenol: paracetamol
indolacetic acid: indomethacin
phenylacetic acid: diclofenac
heteroarylacetic acid: ketorolac
12.
phenylpropionic acid: ibuprofennaphthylpropionic acid: naproxen
anthranilic acid: mefenamic acid, flufenamic acid
oxicams: pyroxicam, lornoxicam, meloxicam
sulfonamides:nimesulide
coxibs: celecoxib
13.
It is important to block COX2 and COX3. And it isreasonable to classify NSAIDs in the following way:
1. Inhibitor of COX1: Acetylsalicylic acid in
small doses
2. Non-selective inhibitors of COX1 and 2: Most of
the NSAIDs
3. Selective inhibitors of COX2: Meloxicam,
Nimesulide, Celecoxib
4. Inhibitor of COX3 in the CNS: Paracetamol
14.
15.
Localization and mechanism of analgesic action NSAIDSAt the site of the inflammation:
NSAIDs block COX-2 and decrease the synthesis of PGE2.
Suppression of prostaglandins synthesis reduces sensitivity
of nociceptors; hyperalgesia disappears; the threshold of
sensitivity to pain increases.
The stabilization of membranes of mast cells is
accompanied by decreased synthesis, release and activation
of mediators of pain and inflammation (histamine,
serotonin, bradykinin). Their effects on the nociceptors are
decreased. Analgesic effect is especially prominent in the
presence of inflammation.
16.
NSAIDS cause pain reliefdue to purely mechanical
factors
as
well.
The
elimination of edema and
tissue infiltration leads to a
decrease in pressure on
nerve
endings,
thus
contributing
to
the
elimination of pain.
17.
B. The central component :NSAIDS block COX-3 and decrease synthesis of PG E2 in
thalamic synapses.
They reduce transmission of pain signal from 2 to 3
neuron of pain afferent pathway.
Paracetamol does not have peripheral anti-inflammatory
effect, but its analgesic effect is quite significant.
Ketorolac is the most effective pain-relieving drug among
NSAIDS.
Metamizole has weak anti-inflammatory effect, but its
analgesics effect is significant also.
18.
Indications for NNA (NSAIDS)Headache, toothache
Neuralgia, sciatica, myositis, arthritis (pain associated
with inflammation)
Pain in the case of bruises, sprains and torn ligaments,
fractured bones
Acute gout
Postoperative pain
Colics (Maxigan)
Algodismenorrhea
19.
The routes of administration (dosage forms)Enteral
1. Oral: tablets, pills (dragee), suspensions, capsules,
capsules-retard (sustained-release)
2. Rectal – suppositories
Parenteral
1. Local application of ointments, creams (diclofenac,
indomethacin, piroxicam, ketoprofen)
2. Intramuscular, intravenous injection (metamizole,
diclofenac, ketorolac, piroxicam, meloxicam)
It is impossible to inject more than 2-3 days (necrosis)!!!
20.
21.
22. The mechanism of antipyretic action
NormalFever
pyrogens ↑
PGЕ2 ↑
NNA
PGЕ2 ↓
HYPOTHALAMUS
HEAT
HEAT LOSS
PRODUCTION
HYPOTHALAMUS
HEAT
PRODUCTION
HEAT LOSS
HYPOTHALAMUS
HEAT
PRODUCTION
HEAT LOSS
23.
NSAIDS have characteristic antipyretic effect. They suppressprostaglandin synthesis and decrease their pyrogenic effect
on the thermoregulating center in the hypothalamus.
Prostaglandin E2 is the most active pyrogen.
A fall of body temperature is caused by an increase in heat
loss: skin vessels are dilated, perspiration is increased.
Antipyretic effect of NSADS is apparent only in the presence
of fever.
In normothermia they do not change body temperature.
We can use paracetamol, ibuprofen, acetylsalicylic
acid (aspirin), metamizole.
24.
25.
The mechanism of anti-inflammatory effect of NSAIDsNSAIDs inhibit COX (cyclooxygenase enzyme) and
synthesis of prostaglandins, decrease hyperemia, edema
and pain.
The phase of alteration. Their effect is weak.
They stabilize membranes of lysosomes, ↓the release
of lysosomal enzymes.
They inhibit lipid peroxidation, ↓the release of free
radicals.
26.
27.
The phase of exudation.NSAIDs :
↓ formation of histamine, serotonin, bradykinin;
Stabilize the membranes of mast cells;
↓ release of inflammatory mediators;
Block hyaluronidase, ↑ accumulation of hyaluronic
acid;
↓the formation of thromboxane and prostacyclin;
↓ energy supply of inflammation.
28.
The phase of proliferationThe drugs:
• ↓energy supply of inflammation;
• ↓ migration of leucocytes;
• ↓the concentration of inflammatory mediators in tissues;
• ↓ the division of fibroblasts, synthesis of collagen and
other fibers of connective tissue;
• ↓ formation of connective tissue, the formation of scars
and adhesions.
29.
The use of NSAIDsMyositis, radiculitis;
Acute gout attack;
The collagen diseases: rheumatism, rheumatoid
polyarthritis, lupus erythematosus, scleroderma;
Diseases of the spine: ankylosing spondylitis;
Vascular disease: periarteritis nodosa;
Glomerulonephritis.
Drugs: piroxicam, meloxicam, lornoxicam, diclofenac,
indomethacin, nimesulide, celecoxib.
30.
Features of the pharmacokinetics of NSAIDsThey are absorbed from the gastrointestinal tract
well.
They bind with blood proteins, and they may
displace sugar-lowering drugs, indirect
anticoagulants from compounds with protein.
NSAIDs penetrate well into sites of inflammation,
where they are delayed for a long time.
The drugs are metabolized in the liver, they are
excreted by the kidneys.
31.
The rate of application:Piroxicam, meloxicam 1 time a day,
Celecoxib, naproxen, nimesulide 2 times a day.
Diclofenac, indomethacin, ibuprofen 3-4 times a day.
32.
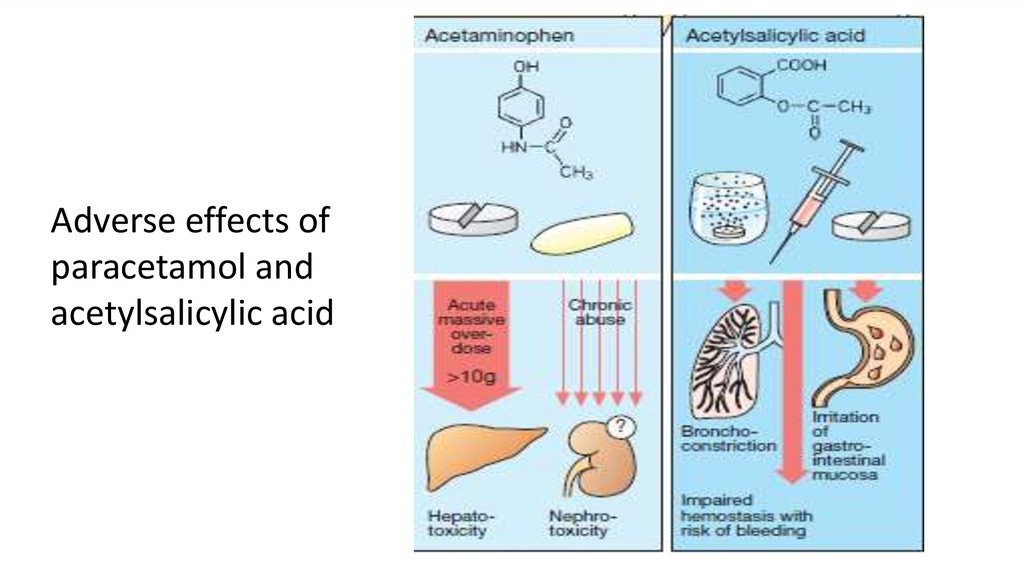
• Acetylsalicylic aciddecreases the platelet
aggregation because it
inhibits COX1 and decreases
the synthesis of
thromboxane.
• Hypoprothrombinemia may
occur usually as a result of
a high-dose treatment.
33.
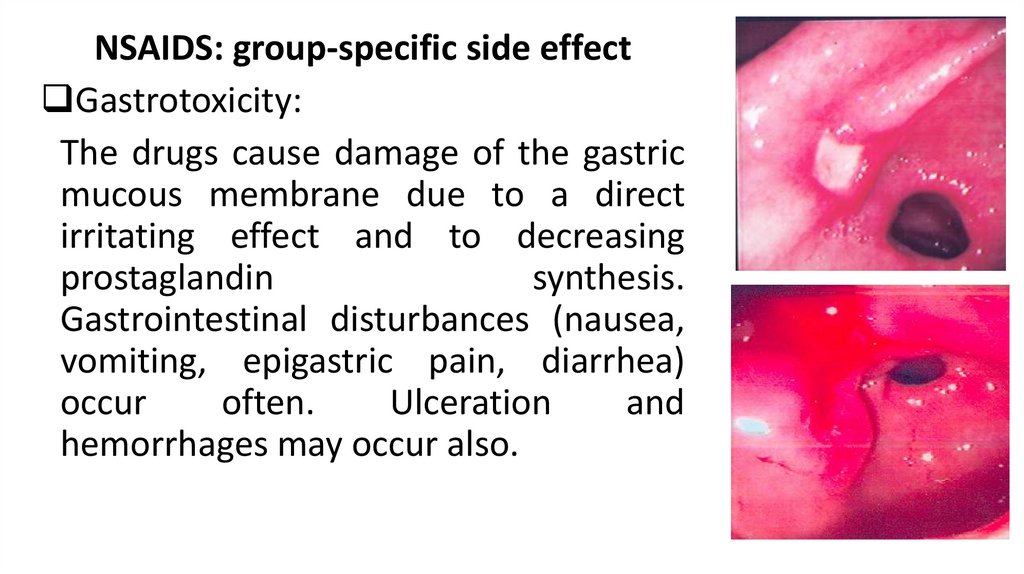
NSAIDS: group-specific side effectGastrotoxicity:
The drugs cause damage of the gastric
mucous membrane due to a direct
irritating effect and to decreasing
prostaglandin
synthesis.
Gastrointestinal disturbances (nausea,
vomiting, epigastric pain, diarrhea)
occur
often.
Ulceration
and
hemorrhages may occur also.
34.
35.
Allergic reaction: NSAIDs inhibit prostaglandinsynthesis, but do not reduce the synthesis of
leukotrienes. This can lead to the development of
asthma, skin rash, urticaria, angioneurotic edema.
Reduced filtration in the kidneys, retention of water,
edema.
Impaired synthesis of prothrombin in the liver.
36.
Salicylates stimulate respiration. They directly stimulate therespiratory center and increase formation of carbonic acid in
tissues. A rise in respiratory rate and respiratory amplitude
may lead to respiratory alkalosis.
They enhance bile excretion in the liver.
They can increase reabsorption of urates and phosphates.
The other side effects are: ringing in the ears, decreasing
hearing, headache, hemorrhages, teratogenicity,
The Reye's syndrome (in children with viral infections –
hepatitis + encephalopathy).
37.
• Paracetamol inhibits COX only in the CNS, so it does notcause gastrointestinal disturbances. But its therapeutic
window is small. Toxic doses exceed the maximal
therapeutic ones by just 2-3 times. In acute poisoning of
paracetamol severe hepatic and renal failure may occur.
These complications are also associated with the
accumulation of the toxic metabolite, which inactivated due
to its conjugation with glutathione. In toxic doses full
inactivation of this metabolite does not occur. It is
necessary to take acetylcycteine or methionine in order to
treat the paracetamol poisoning.
38.
Adverse effects ofparacetamol and
acetylsalicylic acid
39.
Indometacin causes gastrointestinal disturbances,CNS disorders (headache, dizziness, depression,
hallucinations, visual impairment),
Teratogenic effect.
It can inhibits hematopoiesis (leukopenia, aplastic
anemia).
Metamizole can cause leukopenia or agranulocytosis
also.
40.
The selective inhibitors of COX2 (meloxicam, nimesulid,celecoxib) do not suppress the activity of enzyme COX1.
They suppress the enzyme only in a focus of inflammation.
They cause gastrointestinal disturbances (ulceration or
bleeding), altered renal functions (decrease in glomerular
filtration, sodium and water retention) rarely. But they have
analgesic, anti-inflammatory and antipyretic activity.
Celecoxib was shown to be able to prevent the
development of cancer and polyposis of the colon and
rectum.
41.
Drugs used for the treatment of goutGout is a condition which is characterized by an increased
level of uric acid in the blood, storage of urate crystals in the
joints or soft tissues, and the formation of uric calculi (urates)
in the urinary ducts.
Uric acid is a final product of purine base metabolism. It is
eliminated from the body by the kidneys. Filtration of uric
acid takes place in the renal glomeruli, its reabsorption and
secretion takes place in the proximal renal tubules.
42.
43.
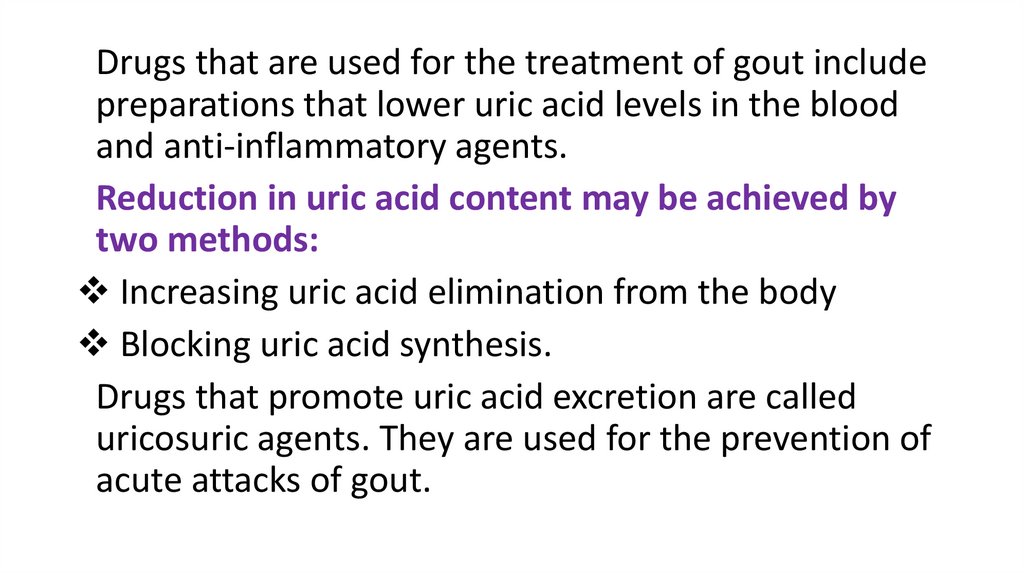
Drugs that are used for the treatment of gout includepreparations that lower uric acid levels in the blood
and anti-inflammatory agents.
Reduction in uric acid content may be achieved by
two methods:
Increasing uric acid elimination from the body
Blocking uric acid synthesis.
Drugs that promote uric acid excretion are called
uricosuric agents. They are used for the prevention of
acute attacks of gout.
44.
Sulfinpyrazone inhibits uric acidreabsorption in the proximal
renal tubules thus enhancing
its excretion from the body. It
also
decreases
platelet
aggregation.
Adverse
effects:
irritating
influence on gastrointestinal
mucosa, allergic reactions,
renal calculi formation, bone
marrow suppression.
45.
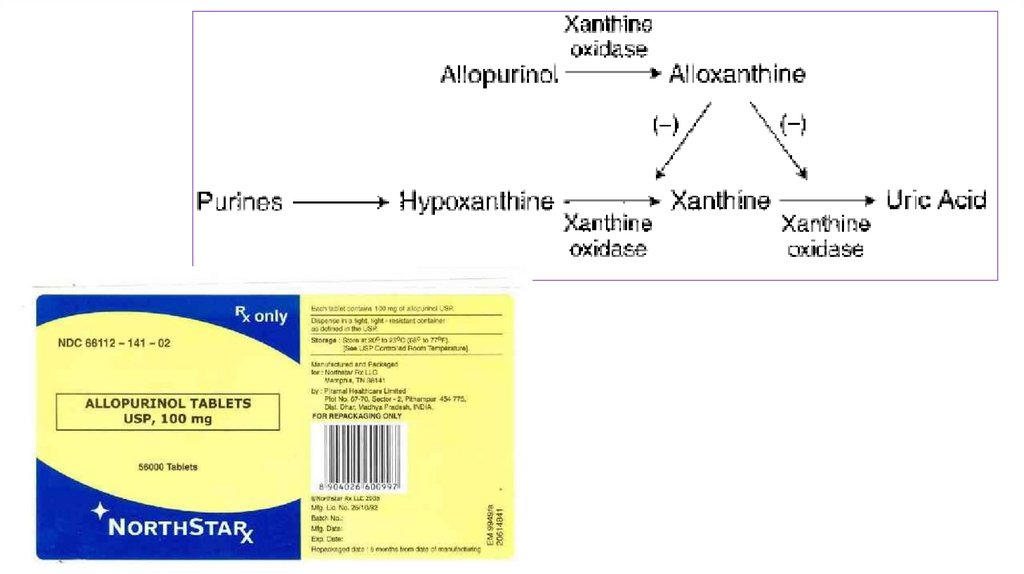
Allopurinol inhibits uric acid formation in the body. Itschemical structure is similar to that of hypoxanthine.
In the body allopurinol is converted into alloxanthine which
interferes with uric acid formation. Allopurinol inhibits
xanthine oxidase. This prevent hypoxanthine and xanthine
from the transformation into uric acid. Allopurinol treatment
leads to the formation of more easily-soluble hypoxanthine
and xanthine that are excreted with urine instead of uric
acid.
Adverse effects: allergic reactions, dyspeptic disorders,
gout exacerbation, leucopenia, anemia.
46.
47.
Colchicine blocks mitotic activity of granulocytes. Itsuppresses granulocyte migration to the focus of
inflammation.
The drug lowers the production of glycoprotein, lactic acid
and a number of enzymes which accompany phagocytosis of
uric acid crystals by granulocytes and promote the
development of inflammation.
It impedes storage of uric acid microcrystals in tissues. This
anti-inflammatory effect occurs relatively quickly with gout
attack being resolved within a few hours.
48.
Colchicine decreases body temperature, elevates arterialblood pressure, suppresses respiratory center, impairs
neuromuscular transmission.
Adverse effects: nausea, vomiting, diarrhea, abdominal pain,
leucopenia, aplastic anemia, alopecia.
It is used mainly to relief of acute gout attacks and some
times to prevent them.
49. Literature
1. Tripathi K.D. Essentials of Medical Pharmacology. Eighth Edition. -2019.- Jaypee Brothers MedicalPublishers. The Health Sciences Publisher. -New Delhi. London. Panama
2. D.A.Kharkevich. Pharmacology. Textbook for medical students. Translation of 12th edition of Russion
textbook “Pharmacology” (2017). – М., ГЭОТАР-Медиa, 2017.
3. Review of pharmacology. Gobind Rai Garg, Sparsh Gupta. 13th edition. - 2019.- Jaypee Brothers
Medical Publishers. The Health Sciences Publisher. -New Delhi. London. Panama
4. Whalen Karen. Lippincott Illustrated Reviews: Pharmacology. Sixth Edition. - Wolters Kluwer. - 2015.Philadelphia
5. Color Atlas of Pharmacology. 2nd edition, revised and expanded. Heinz Lüllmann.- 2000 Thieme
6. Pharmacology Examination & Board Review. Tenth Edition. Trevor Anthony J., Katzung Bertram G.,
Kruidering-Hall Marieke, Susan B. Masters. - a LANGE medical book. - 2013.-New York
7. Medical Pharmacology at a Glance. Eighth Edition. Neal Michael J. – 2016. John Wiley & Sons, Ltd.
8. USMLE Step 1. Lecture Notes. Pharmacology. Lionel P.Raymon and others.- Kaplan Medical.Inc. -2009





































 medicine
medicine