Similar presentations:
The pharmacology of inflammatory mediators
1. The pharmacology of inflammatory mediators
Allison Granta.w.grant@gcu.ac.uk
2. The inflammatory response
• Non-adaptive (innate)• Macroscopic signs:
– Redness
– Pain
– Swelling
– Heat
– Loss of function
3. Cells of the inflammatory response
• Macrophages-PAMPs andcytokines, e.g. interleukins
• Vascular endothelial cells and
adhesion molecules
• Mast cells and histamine
• Polymorphonuclear leukocytes –
ROS, cytokines
• Damaged local tissues-eicosanoids,
bradykinin
• Platelets-serotonin
• Nerves-substance P
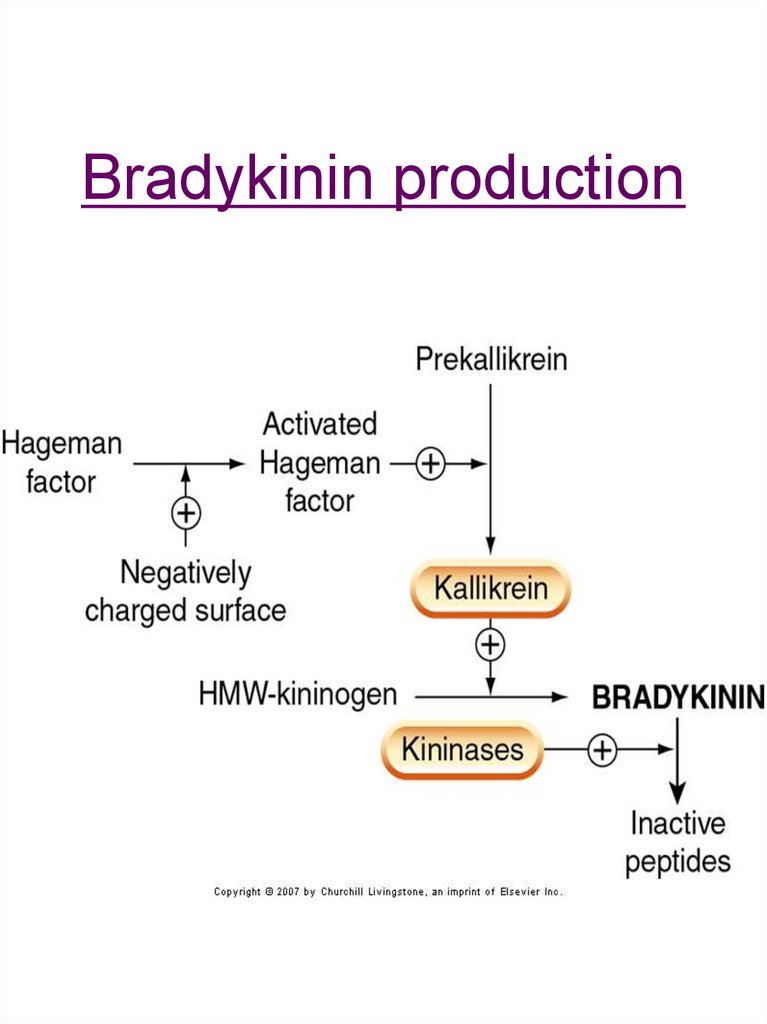
4. Bradykinin production
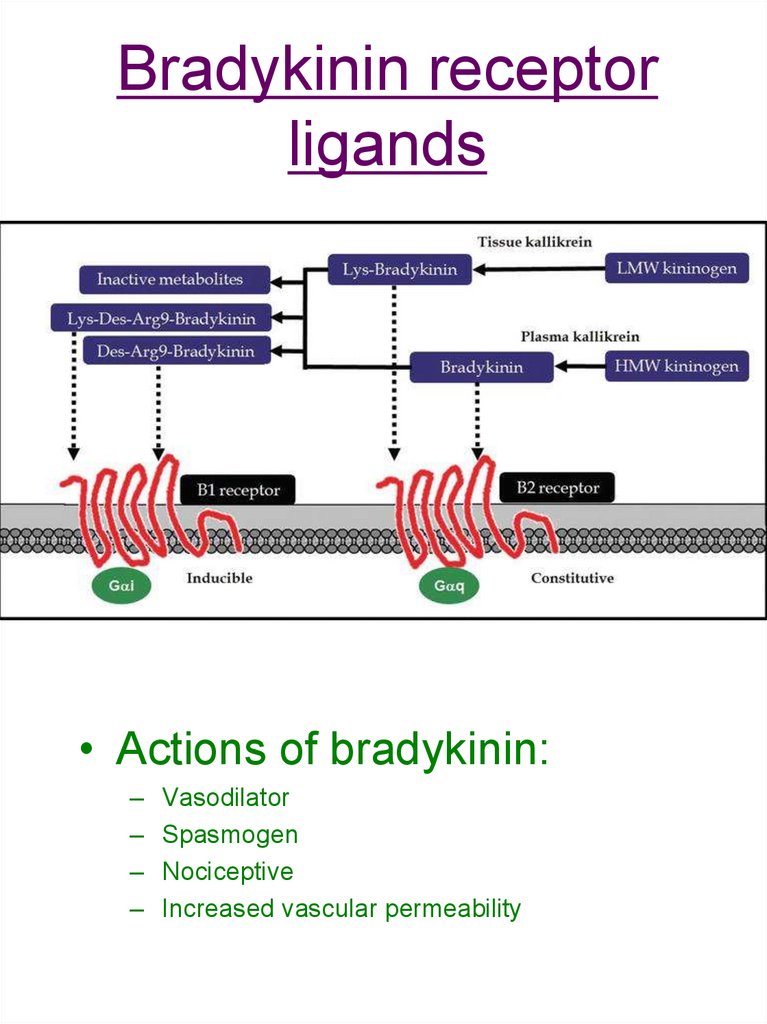
5. Bradykinin receptor ligands
• Actions of bradykinin:– Vasodilator
– Spasmogen
– Nociceptive
– Increased vascular permeability
6. Bradykinin receptors and cell signalling
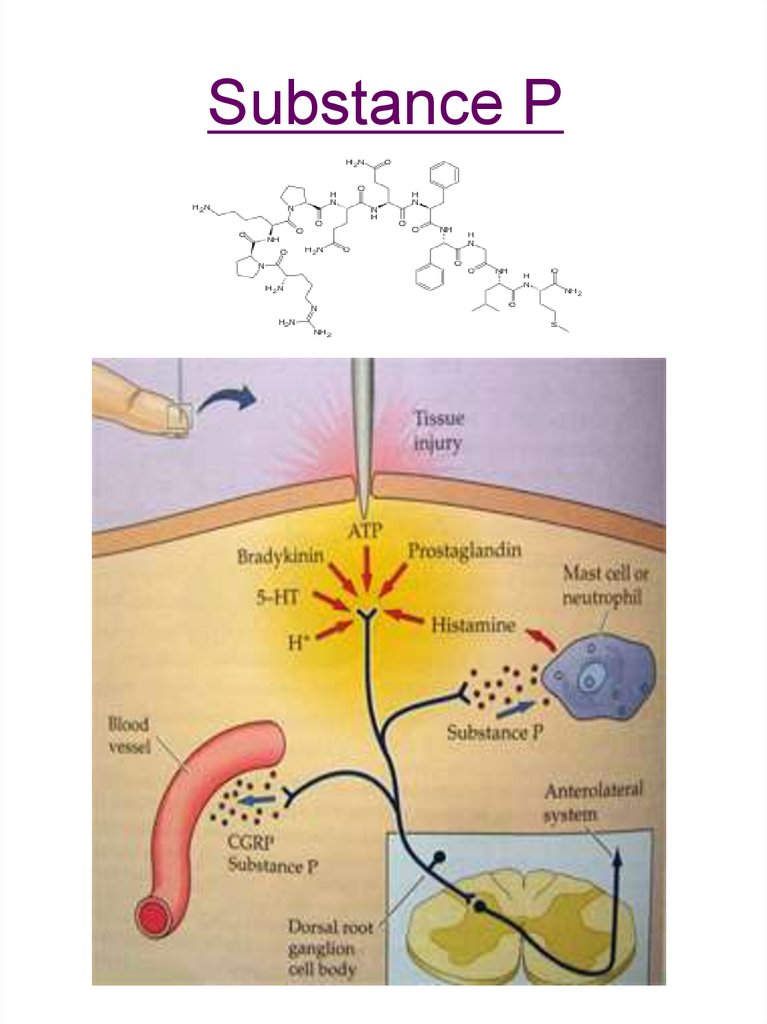
7. Substance P
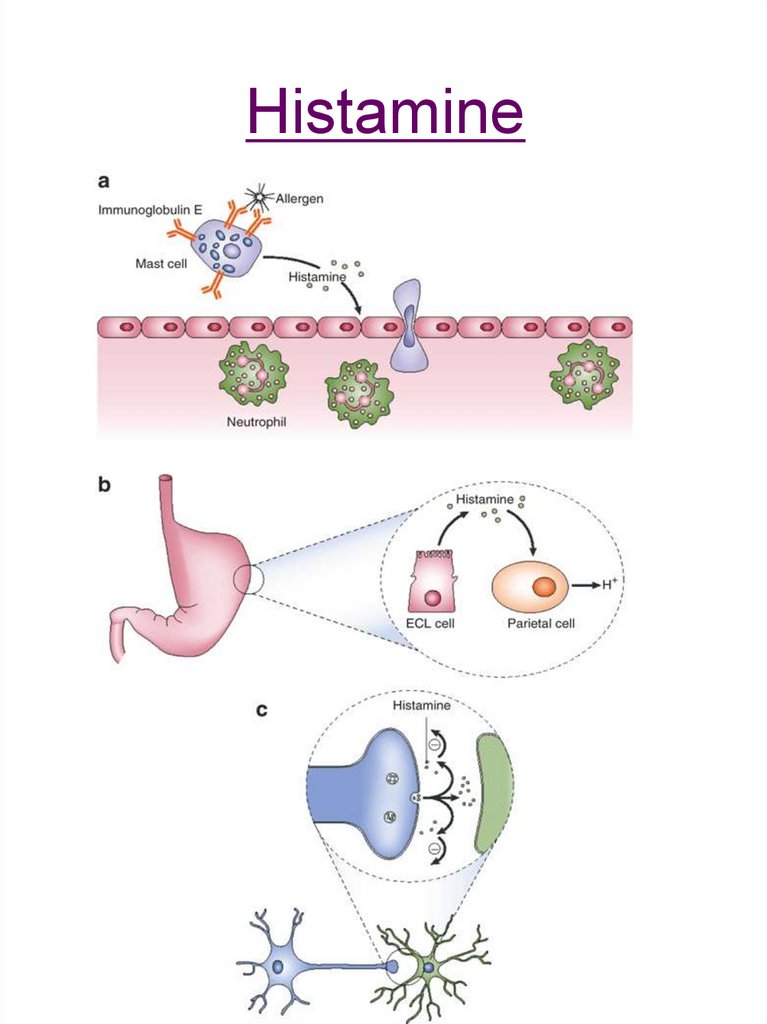
8. Histamine
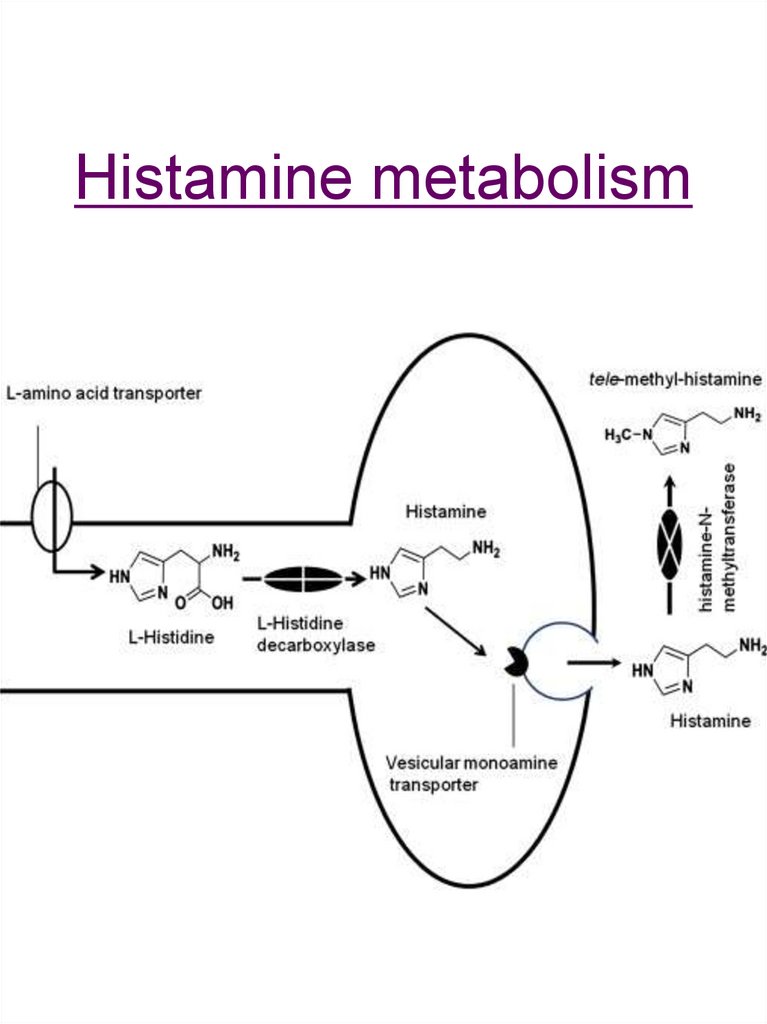
9. Histamine metabolism
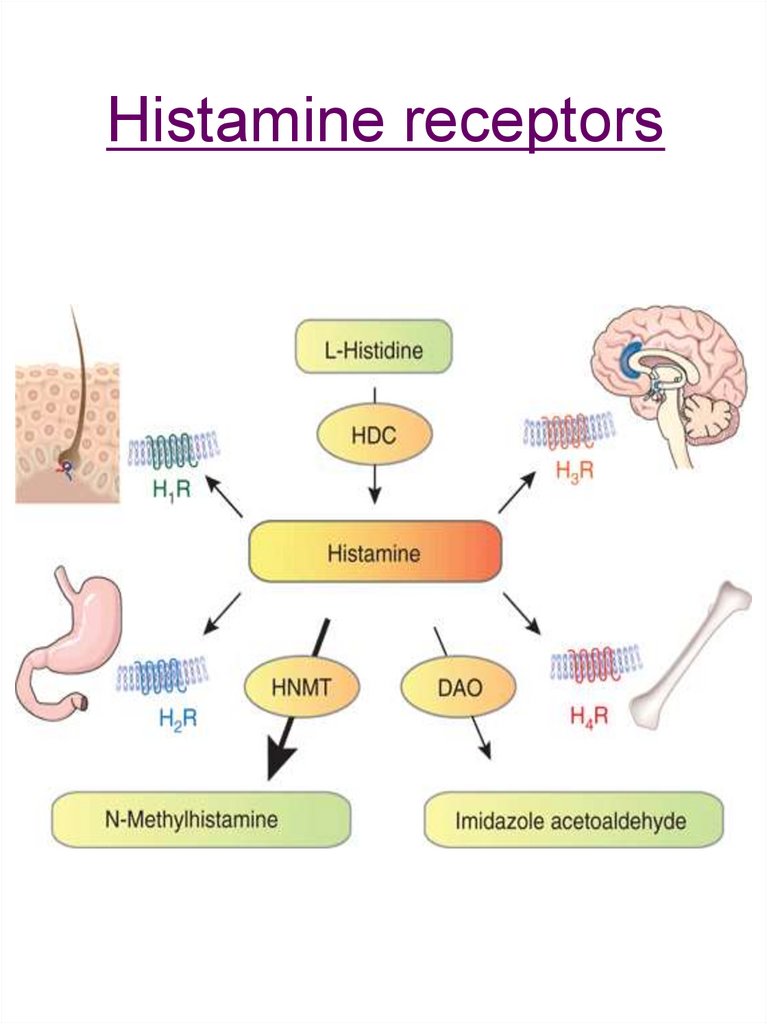
10. Histamine receptors
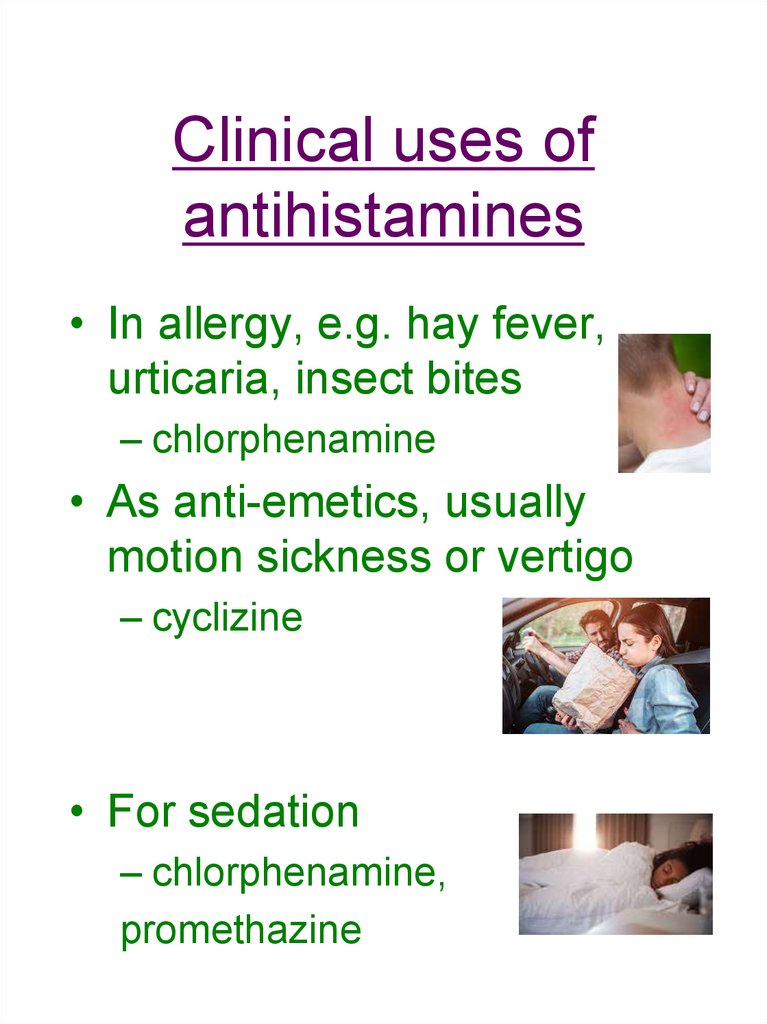
11. Clinical uses of antihistamines
• In allergy, e.g. hay fever,urticaria, insect bites
– chlorphenamine
• As anti-emetics, usually
motion sickness or vertigo
– cyclizine
• For sedation
– chlorphenamine,
promethazine
12. Clinical aspects of antihistamines
• Many non-specific: act on 1,muscarinic, 5-HT receptors
• Sedative and non-sedative• Usually given orally, well
absorbed, metabolised in
liver and excreted by kidney
• Side-effects
13. Non-steroidal anti-inflammatory drugs
Non-steroidal antiinflammatory drugs• Include:
– Aspirin
– Ibuprofen
– Mefenamic acid
– Indomethacin
– Diclofenac
– Celecoxib
• Reduce production of proinflammatory prostaglandins
by blocking cyclo-oxygenase
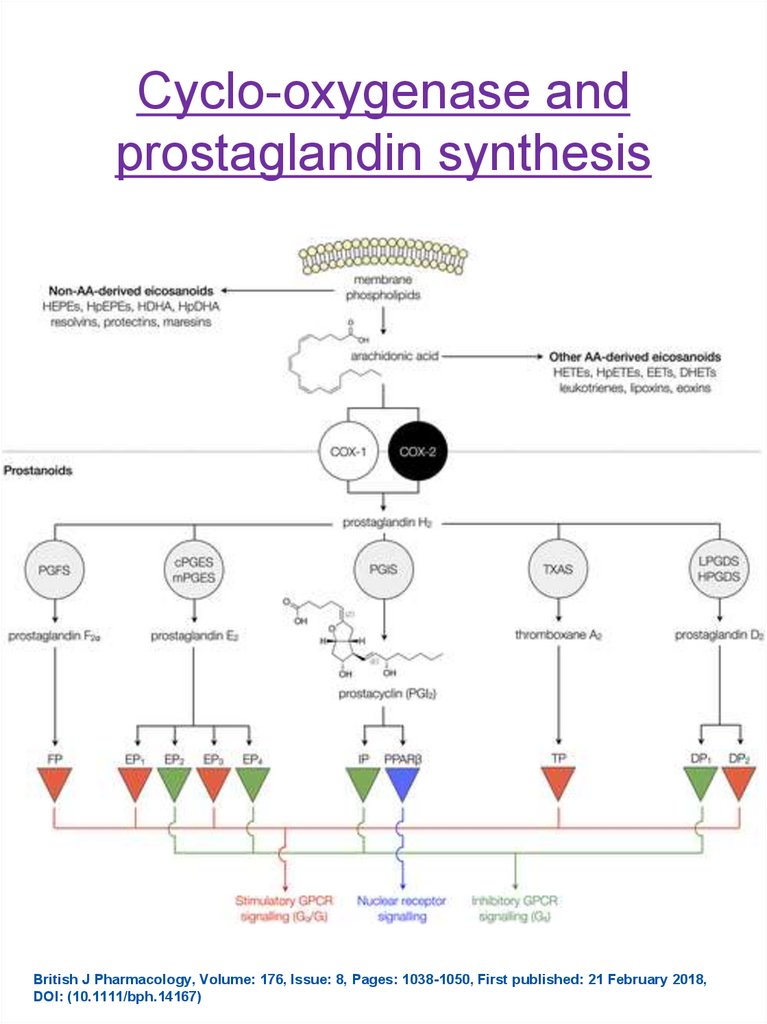
14. Cyclo-oxygenase and prostaglandin synthesis
British J Pharmacology, Volume: 176, Issue: 8, Pages: 1038-1050, First published: 21 February 2018,DOI: (10.1111/bph.14167)
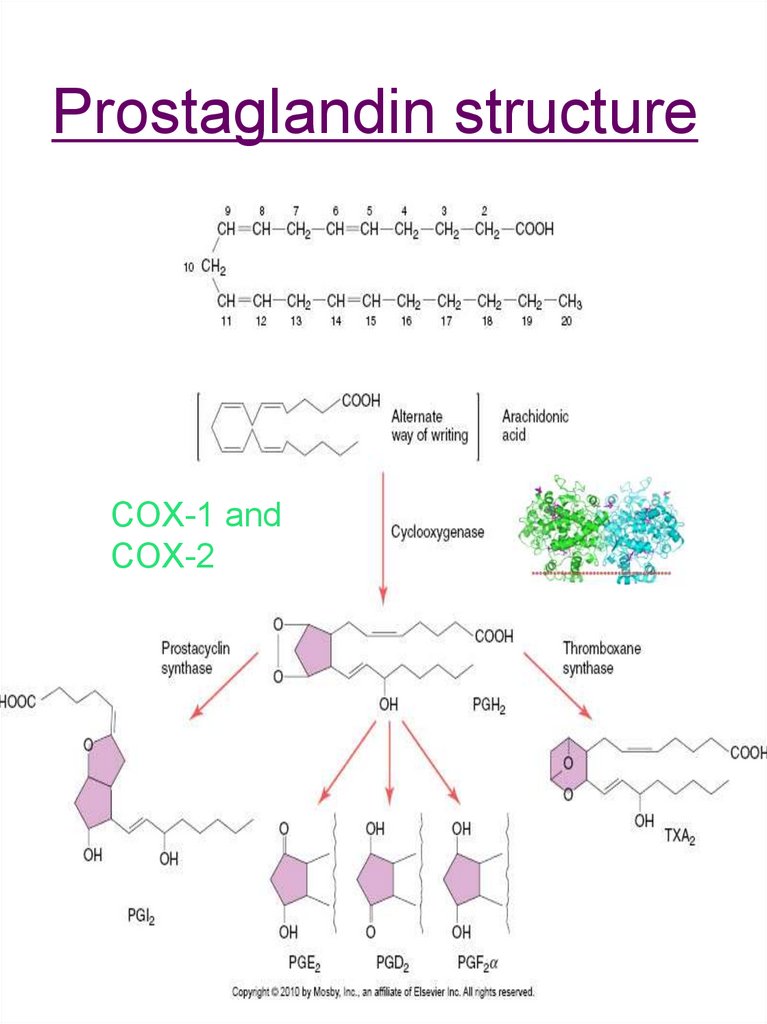
15. Prostaglandin structure
COX-1 andCOX-2
16. Prostaglandins
• Multiple physiologicalfunctions:
– Vasoactive, including
protection of renal blood flow
– Smooth muscle contraction
– Regulation of clotting
– Gastric mucosal protection
– Tumour progression
– Pro-inflammatory
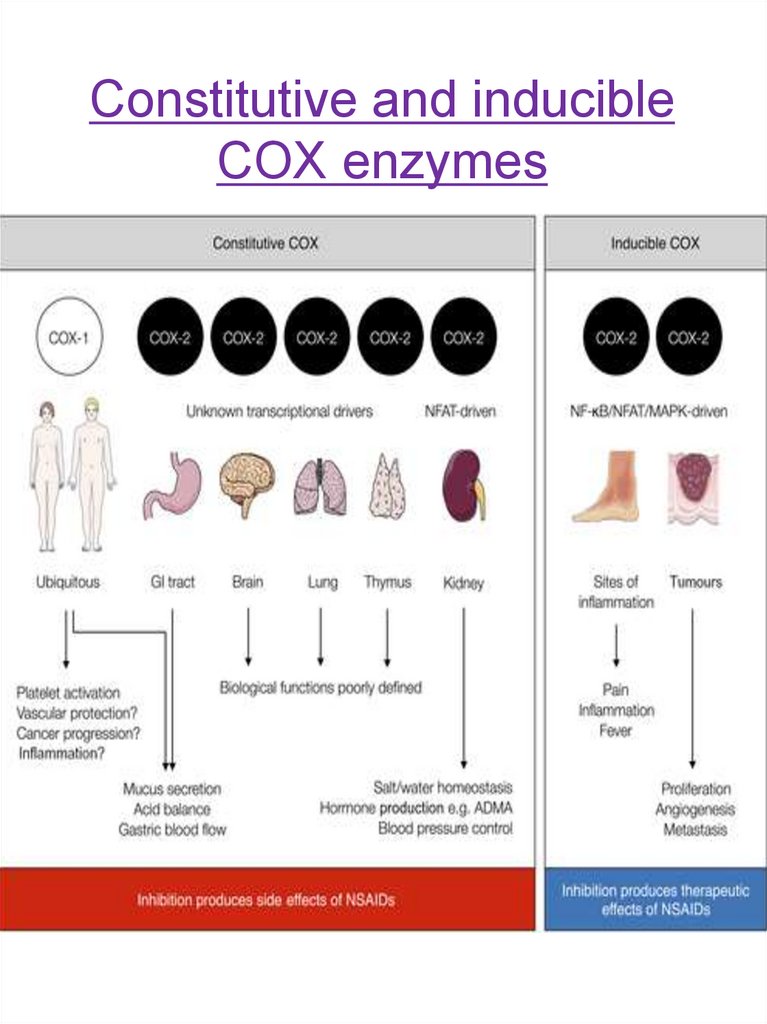
17. Constitutive and inducible COX enzymes
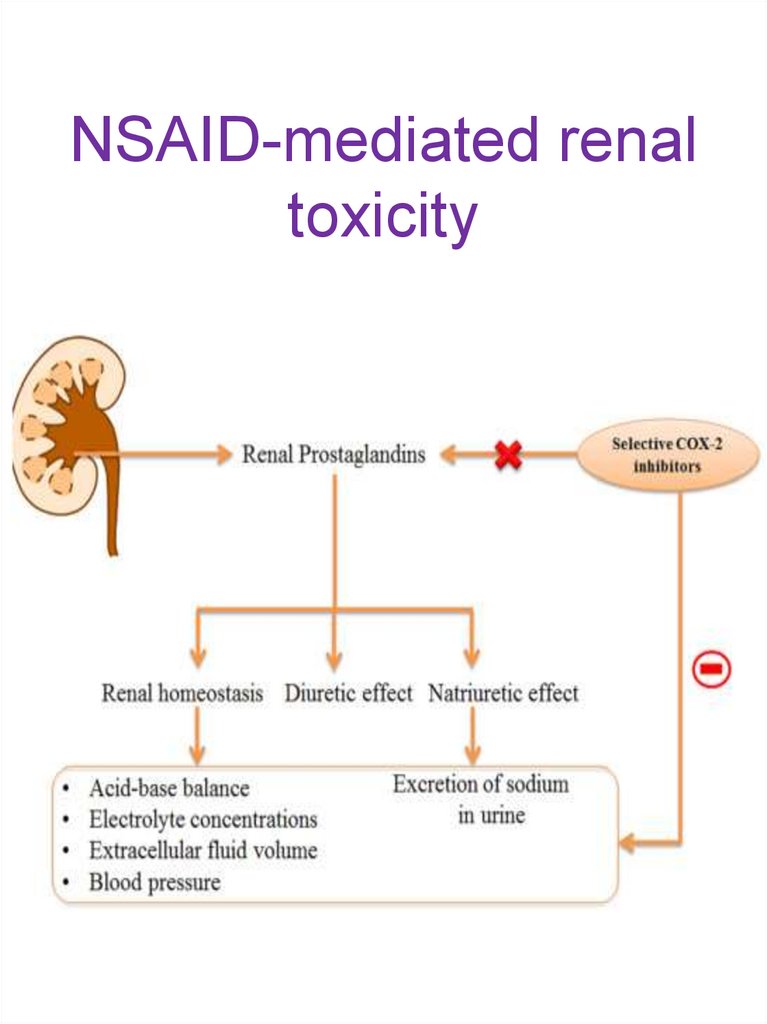
18. NSAID-mediated renal toxicity
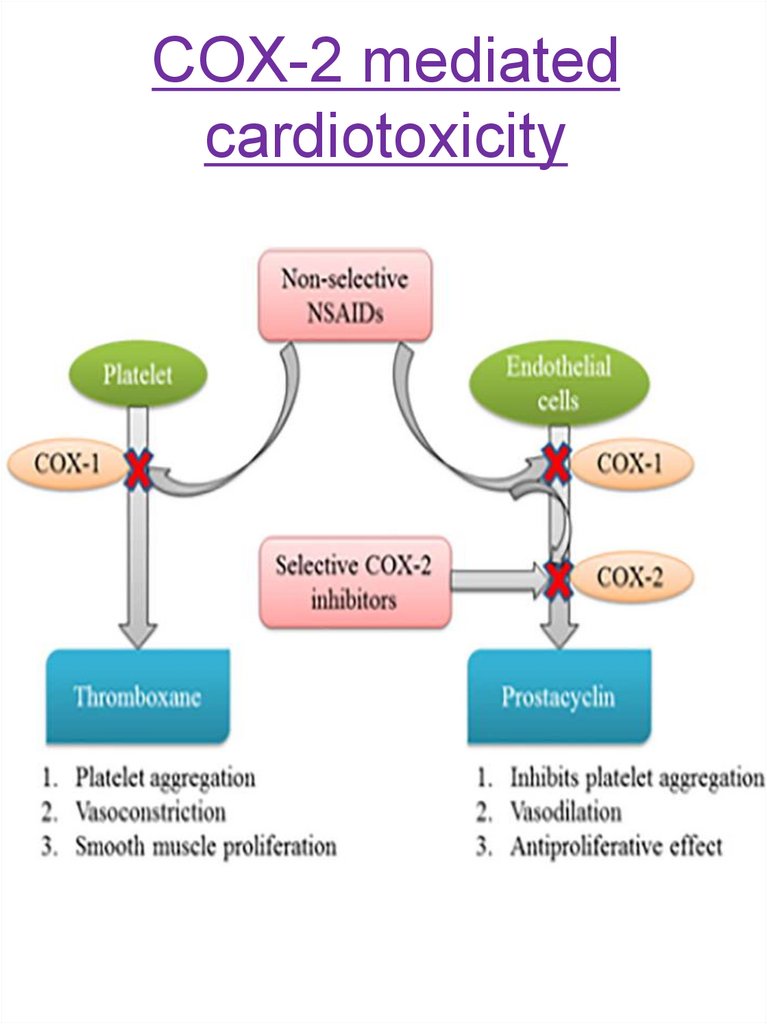
19. COX-2 mediated cardiotoxicity
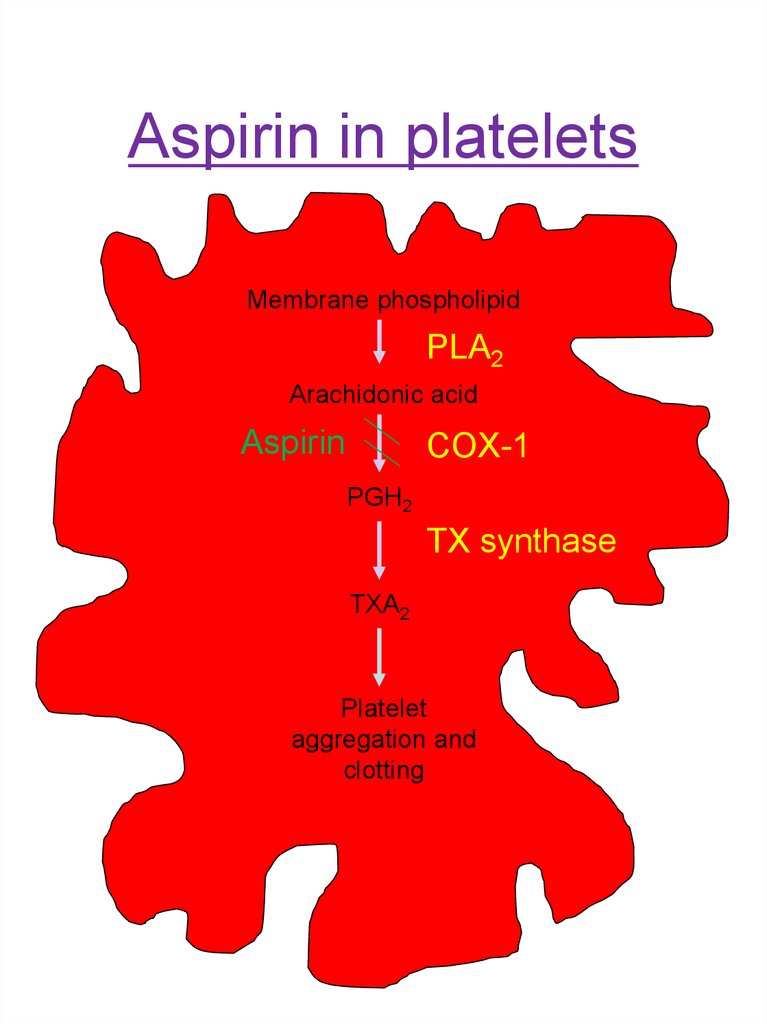
20. Aspirin in platelets
Membrane phospholipidPLA2
Arachidonic acid
Aspirin
COX-1
PGH2
TX synthase
TXA2
Platelet
aggregation and
clotting
21. Aspirin
• Aspirin in plasma salicylic acid• Effects of aspirin
– Good anti-inflammatory
– Mild analgesic
– Potent antiplatelet
– Antipyretic
• Well abs. orally; t1/2 4h
• Adverse effects
– GI irritation
– Decreased renal function
– Asthma
– Reye’s syndrome-rare
– Allergy
– Salicylism
• Newer agents e.g. ibuprofen
22. Celecoxib
• Selective COX-2 inhibitor• Less GI irritation than nonselective agents
• Other COX-2 inhibitors have
been withdrawn from use
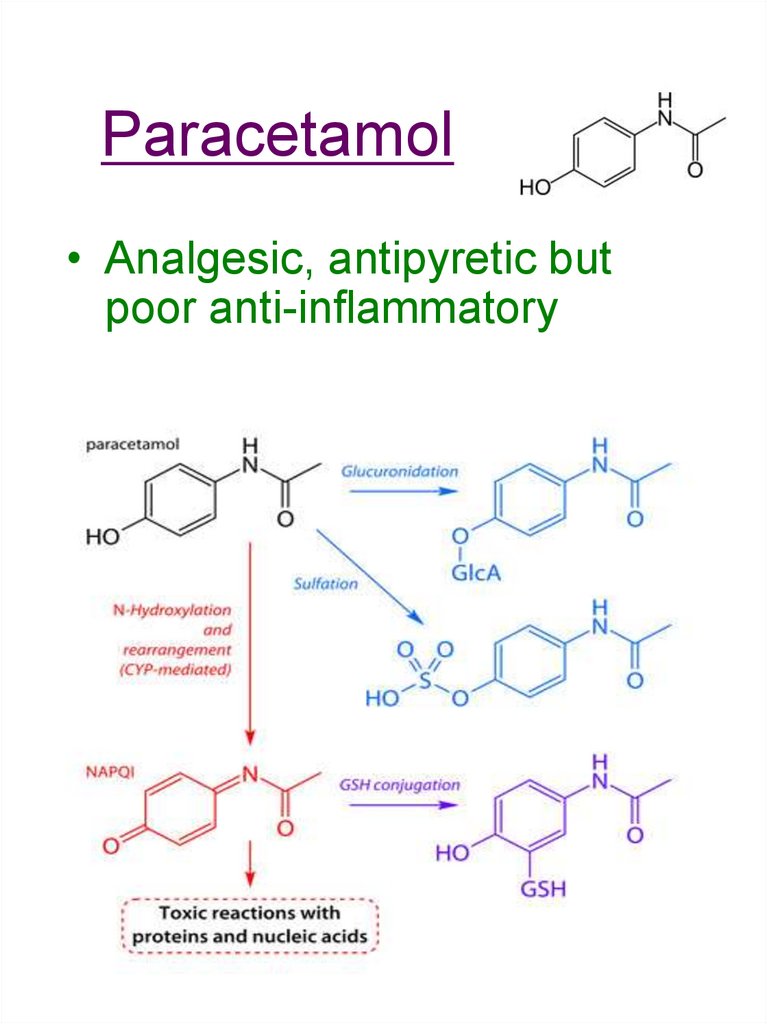
23. Paracetamol
• Analgesic, antipyretic butpoor anti-inflammatory
24. Leukotrienes
• Produced by lipoxygenases• Main LTs:
• LTB4
• Cysteinyl-LTs
• LTs in inflammation• Psoriasis
• UC
• RA
• Asthma
25. LT antagonists
• Zafirlukast and montelukast• Used in asthma, usually as
part of therapy
• Given orally
• Side-effects: Churg-Strauss
syndrome, GI effects,
hypersensitivity
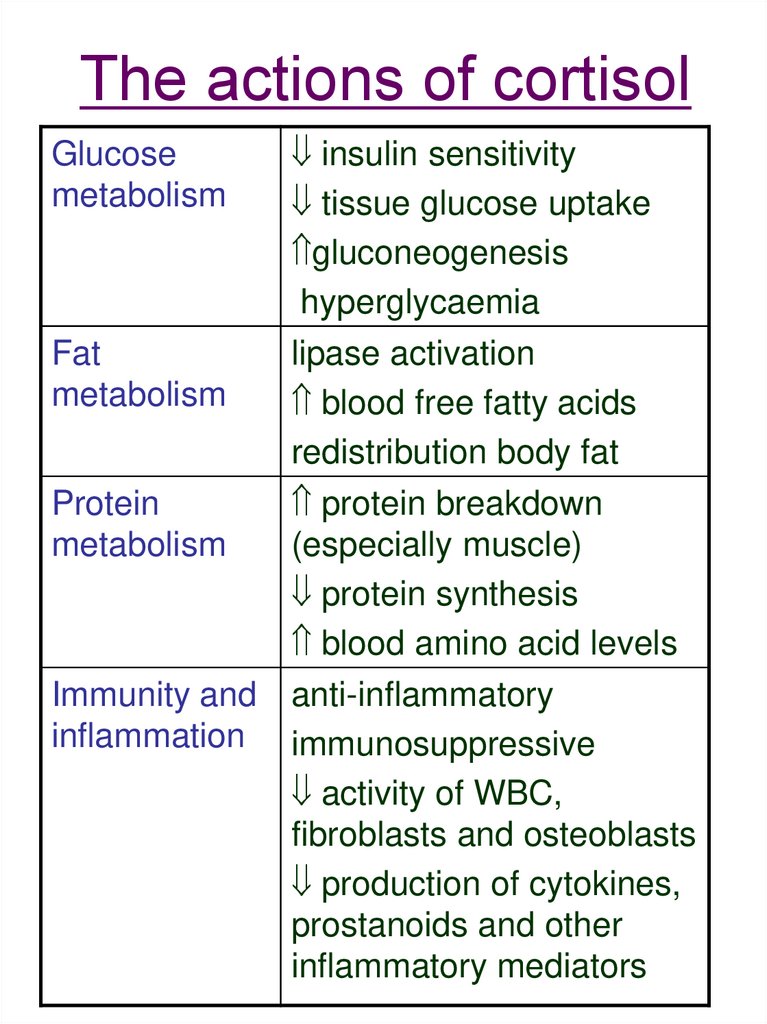
26. The actions of cortisol
insulin sensitivitytissue glucose uptake
gluconeogenesis
hyperglycaemia
Fat
lipase activation
metabolism
blood free fatty acids
redistribution body fat
Protein
protein breakdown
metabolism
(especially muscle)
protein synthesis
blood amino acid levels
Immunity and anti-inflammatory
inflammation immunosuppressive
activity of WBC,
fibroblasts and osteoblasts
production of cytokines,
prostanoids and other
inflammatory mediators
Glucose
metabolism
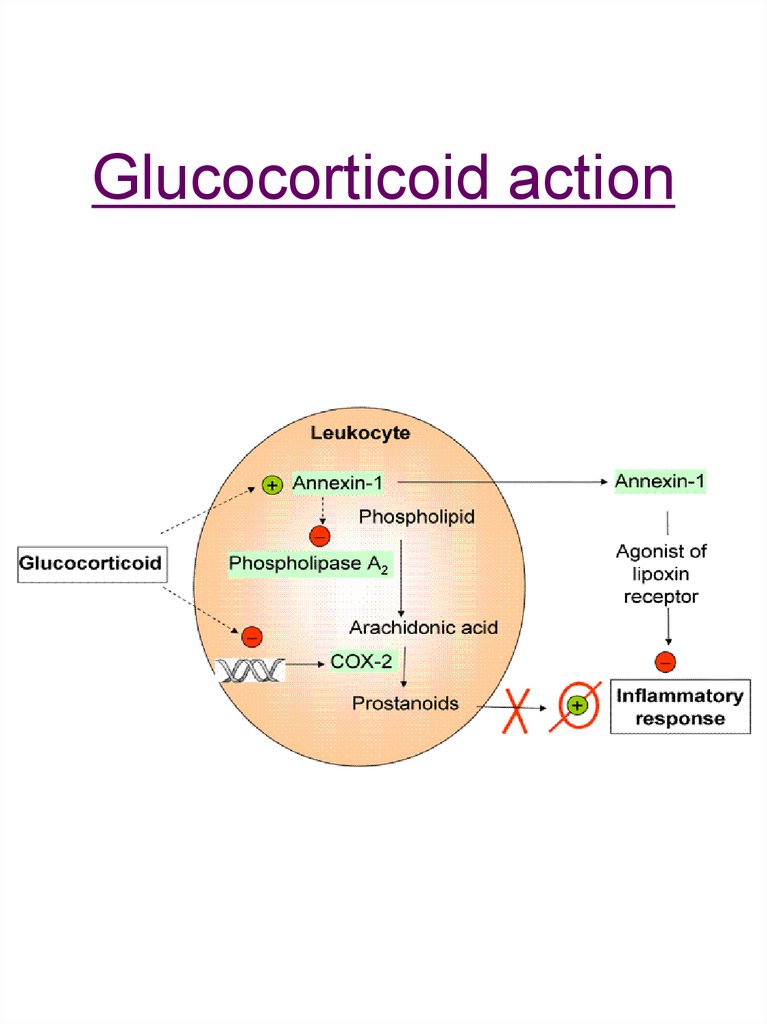
27. Glucocorticoid action
28. Uses of glucocorticoids
• Replacement therapy– e.g. Addison’s disease
• Reduced mineralocorticoids and
glucocorticoids
• Anti-inflammatory therapy
– Asthma
– IBD
– Arthritis
• Immunosuppressive therapy
– e.g. leukaemia, Hodgkin’s
disease
29. Steroid therapy
• Topical preferred-creams,ointments, lotions
• Oral
• Intravenous
• Inhaled
• Body cavities, e.g. into joints
30. Hydrocortisone
• Low potency• High mineralocorticoid
activity
• Used in:
– Replacement therapy
– Hypersensitivity
– Topical anti-inflammatory (1%)
31. Other topical steroids
• Betamethasone 0.1%• Clobetasol proprionate
0.05%
• Care needed as potency
• Adverse effects
– Loss of pigmentation
– Skin atrophy
– Striae
– Absorption
32. Cytokine inhibitors
• Used in e.g. severe arthritis,psoriasis
• e.g. adalimumab blocks
TNF and anakinra blocks
IL-1
33. Refer to your textbook..
…and here are some additional resources:https://bpspubs.onlinelibrary.wiley.com/doi/full/10.
1111/bph.14167
Useful review article on the cardiovascular
pharmacology of eicosanoids, prostacyclin and
COX
https://pdb101.rcsb.org/motm/17
Short article on COX








 medicine
medicine








