Similar presentations:
Inflammation. Exudative inflammation
1.
INFLAMMATION.EXUDATIVE INFLAMMATION
Department of Histology, Embryology and Cytology of
Pirogov Russian National Research Medical University
2.
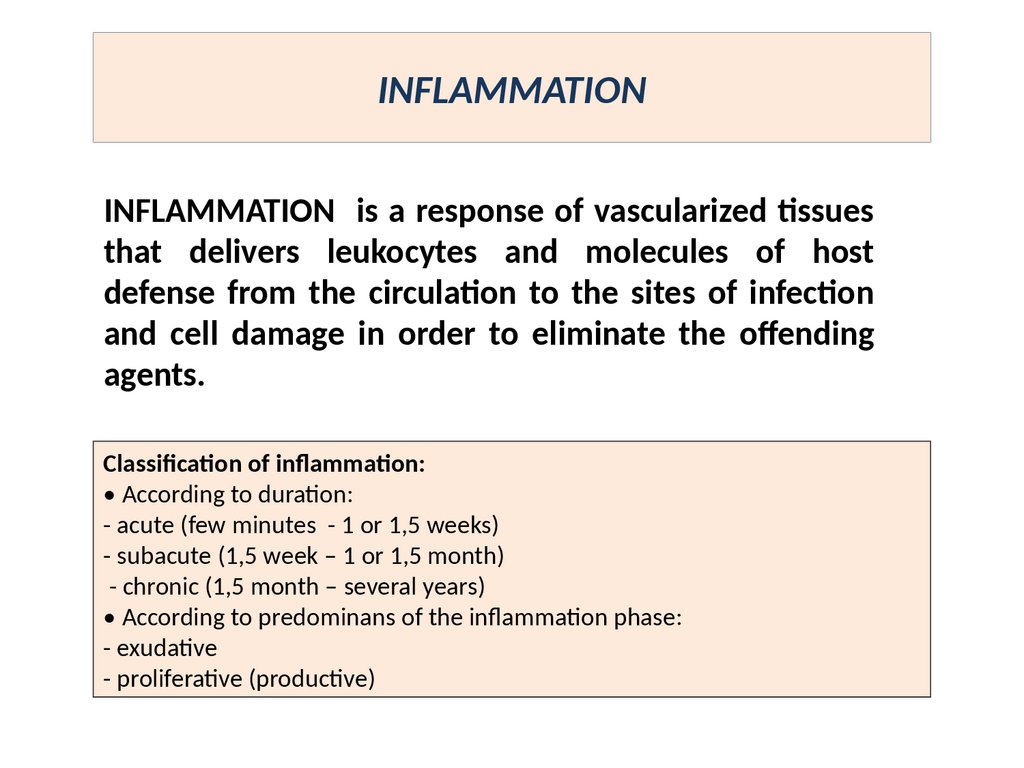
INFLAMMATIONINFLAMMATION is a response of vascularized tissues
that delivers leukocytes and molecules of host
defense from the circulation to the sites of infection
and cell damage in order to eliminate the offending
agents.
Classification of inflammation:
• According to duration:
- acute (few minutes - 1 or 1,5 weeks)
- subacute (1,5 week – 1 or 1,5 month)
- chronic (1,5 month – several years)
• According to predominans of the inflammation phase:
- exudative
- proliferative (productive)
3.
ETIOLOGY OFINFLAMMATION
Biologic agents: viruses, bacteria, fungi, parasites,
immunologic
factors
(antibodies,
immune
complexes, activated lymphocytes) & so on.
Physical agents: radiation, electricity, high & low
temperature, trauma, foreign body.
Chemical agents: endotoxins, exotoxins, poisons,
drags & so on.
Unknown factors
3
4.
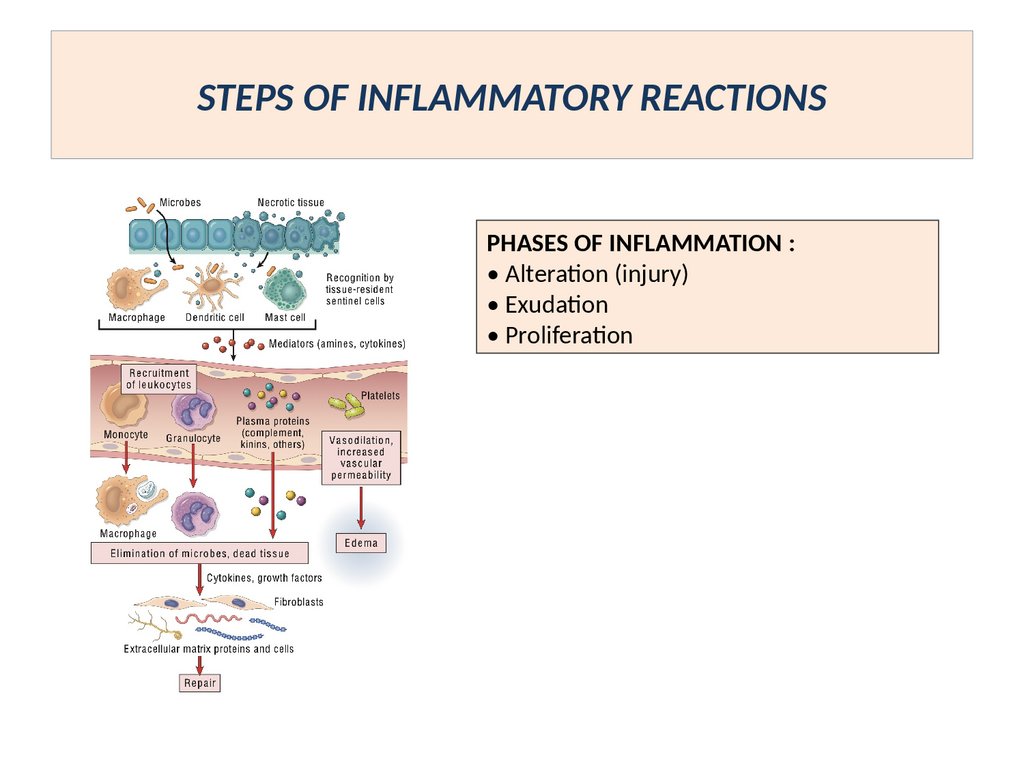
STEPS OF INFLAMMATORY REACTIONSPHASES OF INFLAMMATION :
• Alteration (injury)
• Exudation
• Proliferation
5.
EXUDATIVE INFLAMMATIONEXUDATIVE INFLAMMATION IS THE TYPE OF INFLAMMATION,
CHARACTERIZED BY PREDOMINANS OF EXUDATION OVER ALTERATION &
PROLIFERATION.
IT OCCURS AS A CONSEQUENCE OF SEVERE INJURIES, WITH RESULT TO
GREATER VASCULAR PERMEABILITY TO ALLOW LARGER MOLECULES
(SPECIFICALLY FIBRINOGEN) TO PASS THE ENDOTHELIAL BARRIER.
TYPES OF EXUDATIVE INFLAMMATION :
• SEROUS
• FIBRINOUS
• PURULENT
• HEMORRAGIC
• ROTTEN ( PUTRID )
• CATARRHAL
• MIXED
TYPE OF INFLAMMATION DEPENDS ON :
SEVERETY OF INJURY,
VASCULAR PERMEABILITY,
TYPE OF INJURING AGENT,
PROLONGATION OF ITS INFLUENCE.
EXUDATIVE INFLAMMATION USUALLY IS
ACUTE,
BUT PURULENT & CATARRHAL
INFLAMMATION MAY BE ACUTE OR CHRONIC.
6.
SEROUS INFLAMMATION• Exudate contains fluid, up to 2% proteins, a few cells (neutrophils,
macrophages, epithelium.
APPEARES:
on the serous membranes (rheumatic fever, uremia)
on the mucous membranes
skin
meninges
peripheral nerves
parenchymal organs
ETHIOLOGY
streptococcus (erysipelas)
viral infections (chicken pox, natural small pox, herpetic fever)
burn
7.
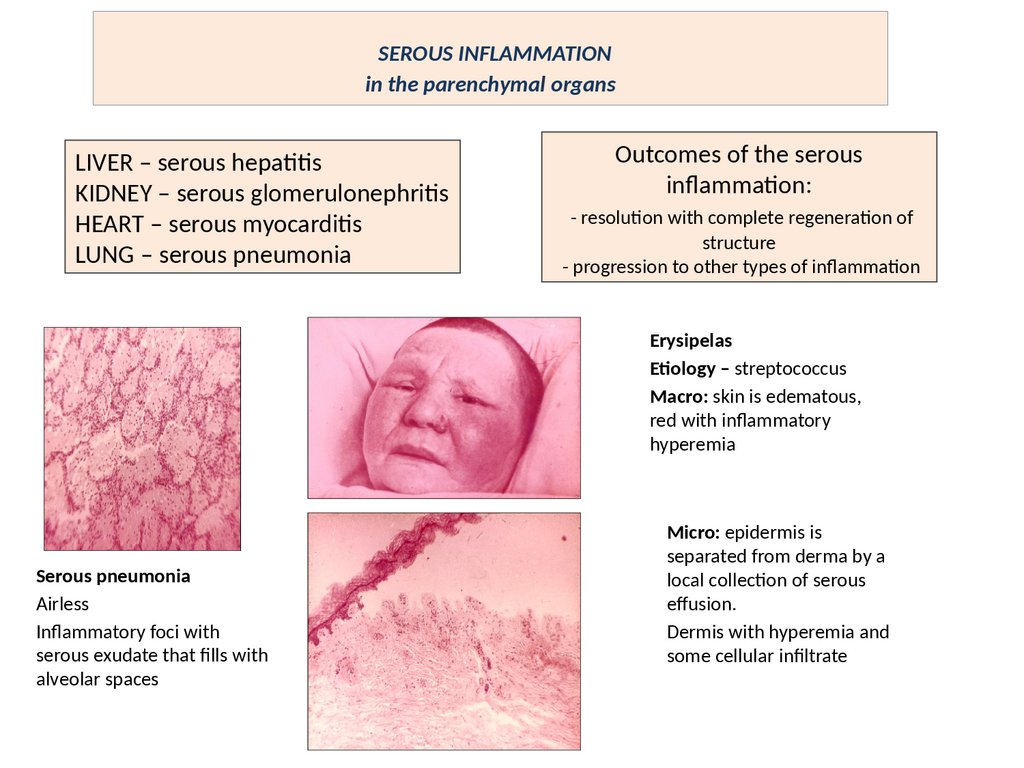
SEROUS INFLAMMATIONin the parenchymal organs
LIVER – serous hepatitis
KIDNEY – serous glomerulonephritis
HEART – serous myocarditis
LUNG – serous pneumonia
Outcomes of the serous
inflammation:
- resolution with complete regeneration of
structure
- progression to other types of inflammation
Erysipelas
Etiology – streptococcus
Macro: skin is edematous,
red with inflammatory
hyperemia
Serous pneumonia
Airless
Inflammatory foci with
serous exudate that fills with
alveolar spaces
Micro: epidermis is
separated from derma by a
local collection of serous
effusion.
Dermis with hyperemia and
some cellular infiltrate
8.
FIBRINOUS INFLAMMATION• It is the type of exudative inflammation, characterized by
exudation, which is reached by fibrin.
IT OCCURS AS A CONSEQUENCE OF SEVERE INJURIES, WITH RESULT TO
GREATER VASCULAR PERMEABILITY TO ALLOW LARGER MOLECULES
(SPECIFICALLY FIBRINOGEN) TO PASS THE ENDOTHELIAL BARRIER.
ETIOLOGY :
• TOXIC FACTORS (UREMIA)
• BACTERIAL INFECTIONS
• VIRUS INFECTIONS
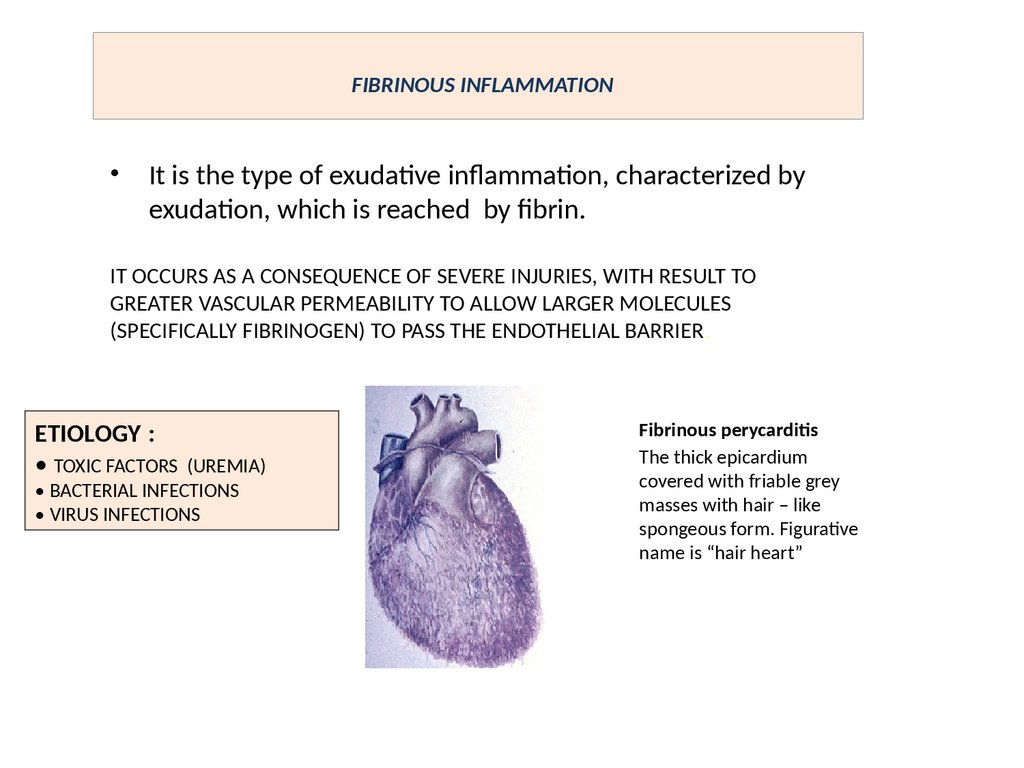
Fibrinous perycarditis
The thick epicardium
covered with friable grey
masses with hair – like
spongeous form. Figurative
name is “hair heart”
9.
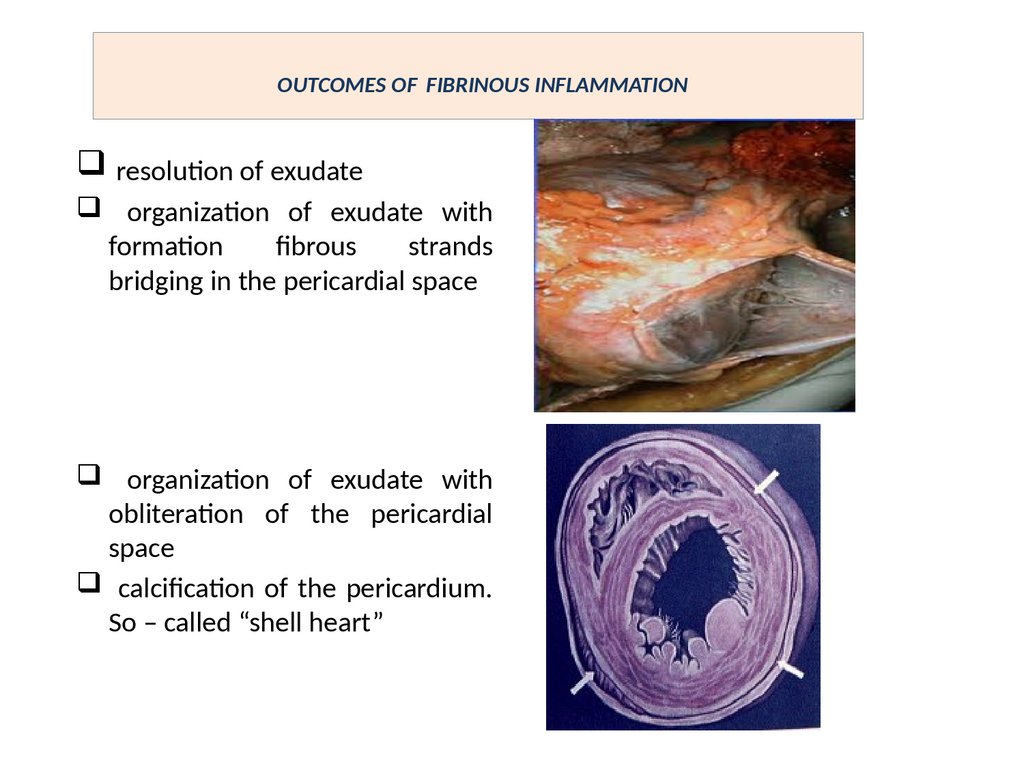
OUTCOMES OF FIBRINOUS INFLAMMATIONresolution of exudate
organization of exudate with
formation
fibrous
strands
bridging in the pericardial space
organization of exudate with
obliteration of the pericardial
space
calcification of the pericardium.
So – called “shell heart”
10.
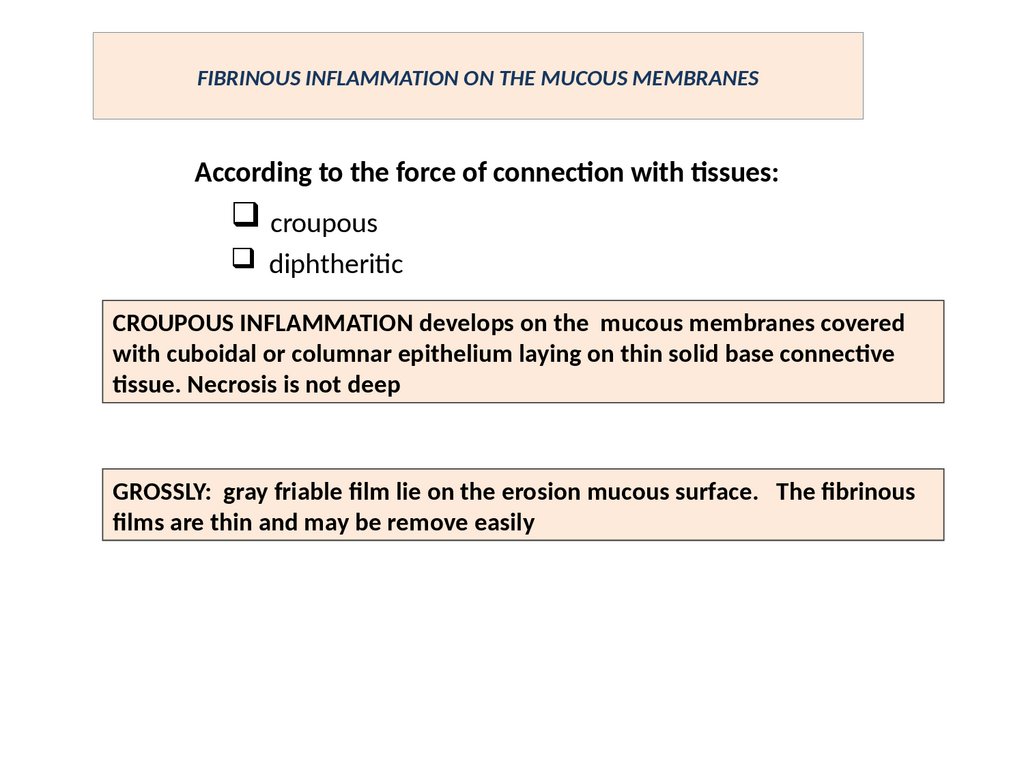
FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANESAccording to the force of connection with tissues:
croupous
diphtheritic
CROUPOUS INFLAMMATION develops on the mucous membranes covered
with cuboidal or columnar epithelium laying on thin solid base connective
tissue. Necrosis is not deep
GROSSLY: gray friable film lie on the erosion mucous surface. The fibrinous
films are thin and may be remove easily
11.
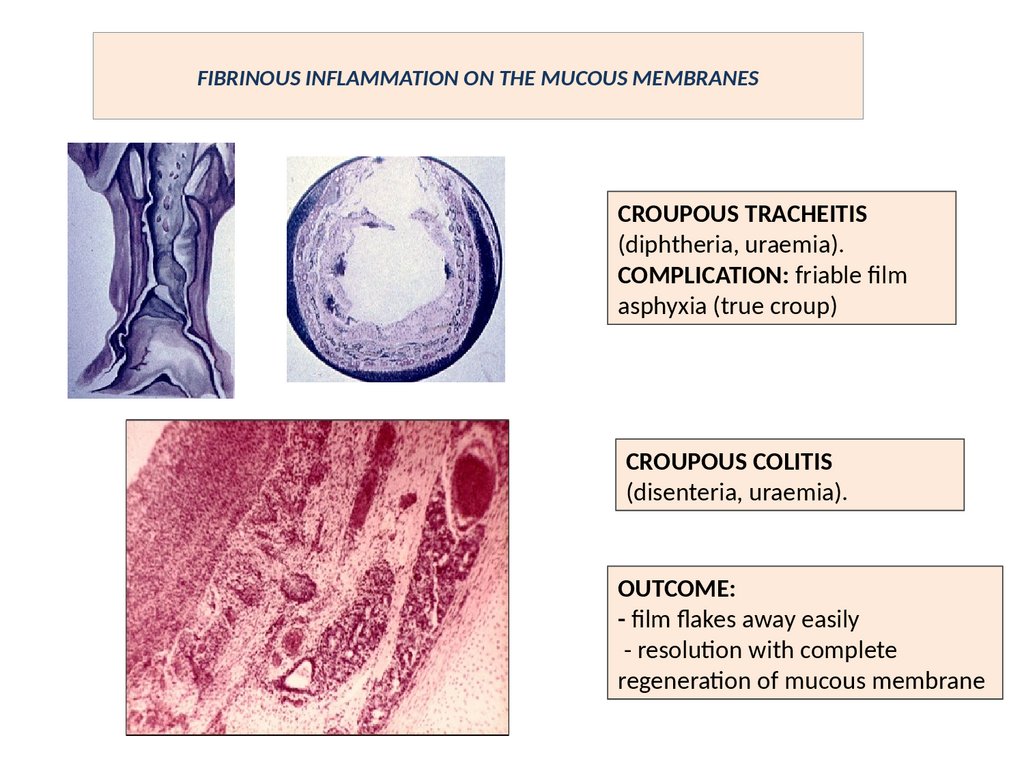
FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANESCROUPOUS TRACHEITIS
(diphtheria, uraemia).
COMPLICATION: friable film
asphyxia (true croup)
CROUPOUS COLITIS
(disenteria, uraemia).
OUTCOME:
- film flakes away easily
- resolution with complete
regeneration of mucous membrane
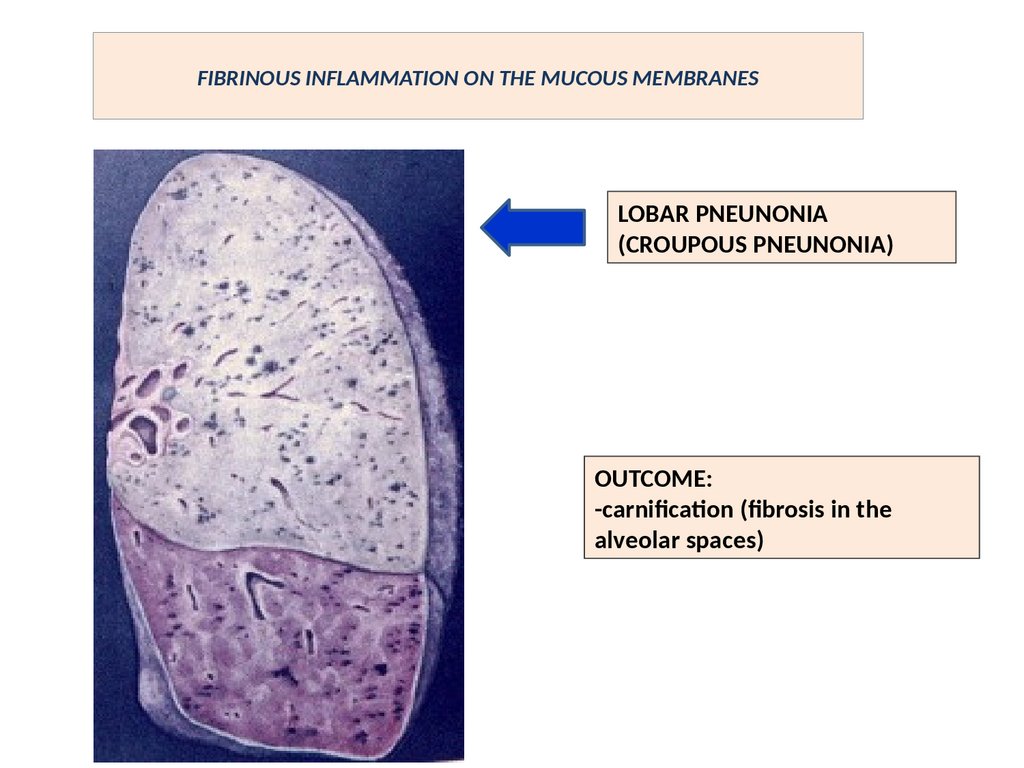
12.
FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANESLOBAR PNEUNONIA
(CROUPOUS PNEUNONIA)
OUTCOME:
-carnification (fibrosis in the
alveolar spaces)
13.
DIPHTHERITIC INFLAMMATIONIT develops on the mucous membranes covered with squamous or
transitional epithelium laying on thick friable base connective tissue.
Necrosis is deep
GROSSLY: The fibrinous films is thick, solid, connected strongly with injured
tissue. Removing of this cover leads to deep ulceration
ORGANS: pharynx, esophagus, uterus, vagina, intestine, stomach, urinary
bladder
14.
DIPHTHERITIC INFLAMMATIONIT develops on the mucous membranes covered with squamous or
transitional epithelium laying on thick friable base connective tissue.
Necrosis is deep
GROSSLY: The fibrinous films is thick, solid, connected strongly with injured
tissue. Removing of this cover leads to deep ulceration
ORGANS: pharynx, esophagus, uterus, vagina, intestine, stomach, urinary
bladder
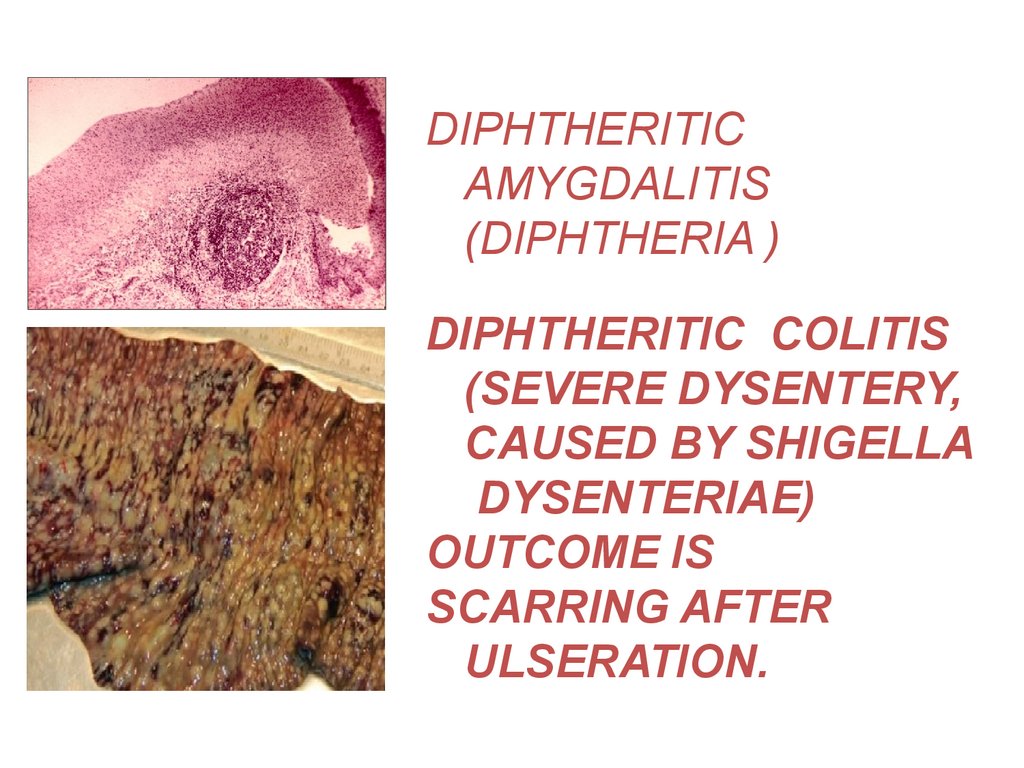
15.
DIPHTHERITICAMYGDALITIS
(DIPHTHERIA )
DIPHTHERITIC COLITIS
(SEVERE DYSENTERY,
CAUSED BY SHIGELLA
DYSENTERIAE)
OUTCOME IS
SCARRING AFTER
ULSERATION.
16.
HEMORRAGIC INFLAMMATIONCHARACTERIZED BY PRESENS OF NUMEROUS OF
ERYTHROCYTES IN THE EXUDATE.
ACCOMPANIED WITH SEVERE INFECTIONS SUCH
AS PESTILENCE, ANTHRAX.
IT IS VERY CHARACTERISTICALLY FOR
INFLUENZA
THIS TYPE OF INFLAMMATION ACCOMPANIED
WITH NEGATIVE (STOP) CHEMOTAXIS OF
NEUTROPHILS
17.
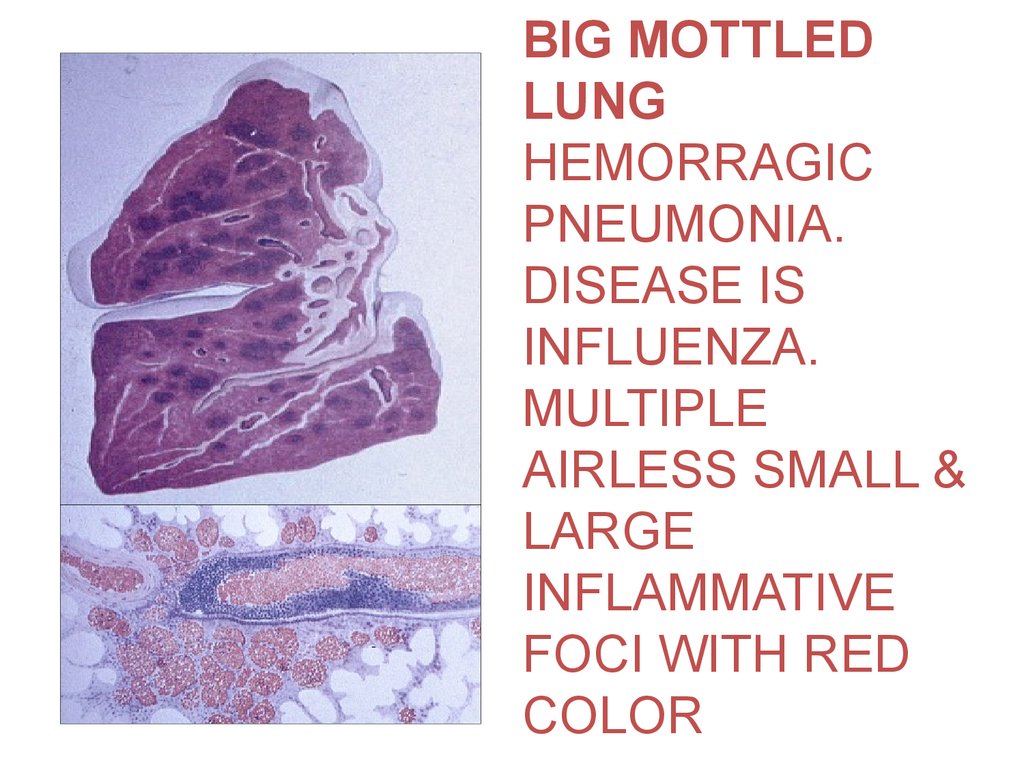
BIG MOTTLEDLUNG
HEMORRAGIC
PNEUMONIA.
DISEASE IS
INFLUENZA.
MULTIPLE
AIRLESS SMALL &
LARGE
INFLAMMATIVE
FOCI WITH RED
COLOR
18.
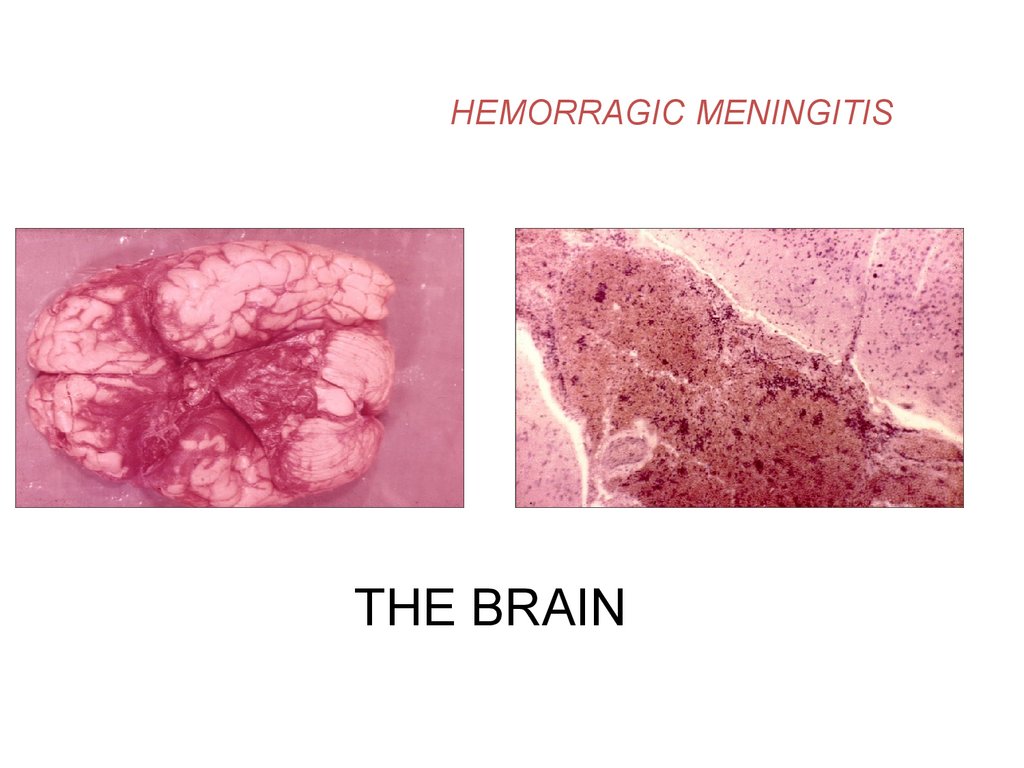
HEMORRAGIC MENINGITISTHE BRAIN
19.
PURULENT (SUPPURATIVE)INFLAMMATION
CHARACTERIZED BY A PURULENT EXUDATE
(PUS ) PRODACTION, CONSISTING OF
NEUTROPHILS, PARENCHYMAL CELL DEBRIS,
NEUTROPHILS DEBRIS ( PUS BODIES),
MICROORGANISMS.
IT IS ALWAYS ACCOMPAINED WITH
DESTRUCTION OF THE INFLAMMED TISSUE,
WHICH IS KNOWN AS PROTEOLYSIS.
20.
ETIOLOGIC FACTORS:1. PYOGENIC MICROORGANISMS
(STAPHYLOCOCCUS, STREPTOCOCCUS,
GONOCOCCUS, MENINGOCOCCUS , E.
COLI & OTHER ).
2. SOME CHEMICAL FACTORS
(TURPENIC, MUSTARD) AS ASEPTIC
PURULENT INFLAMMATION
21.
CLASSIFICATION :1. PHLEGMON – DIFFUSE PURULENT
INFLAMMATION
2. ABSCESS – LOCAL PURULENT INFLAMMATION
WITH BREAKDOWN OF THE TISSUE & FORMATION
OF A CAVITY WITH PUS ENCLOSED BY A PYOGENIC
MEMBRANE.
3. EMPYEMA – PURULENT INFLAMMATION OF THE
ANATOMIC CAVITY WALLS WITH THE
ACCUMULATION OF PUS IN THIS CAVITY.
22.
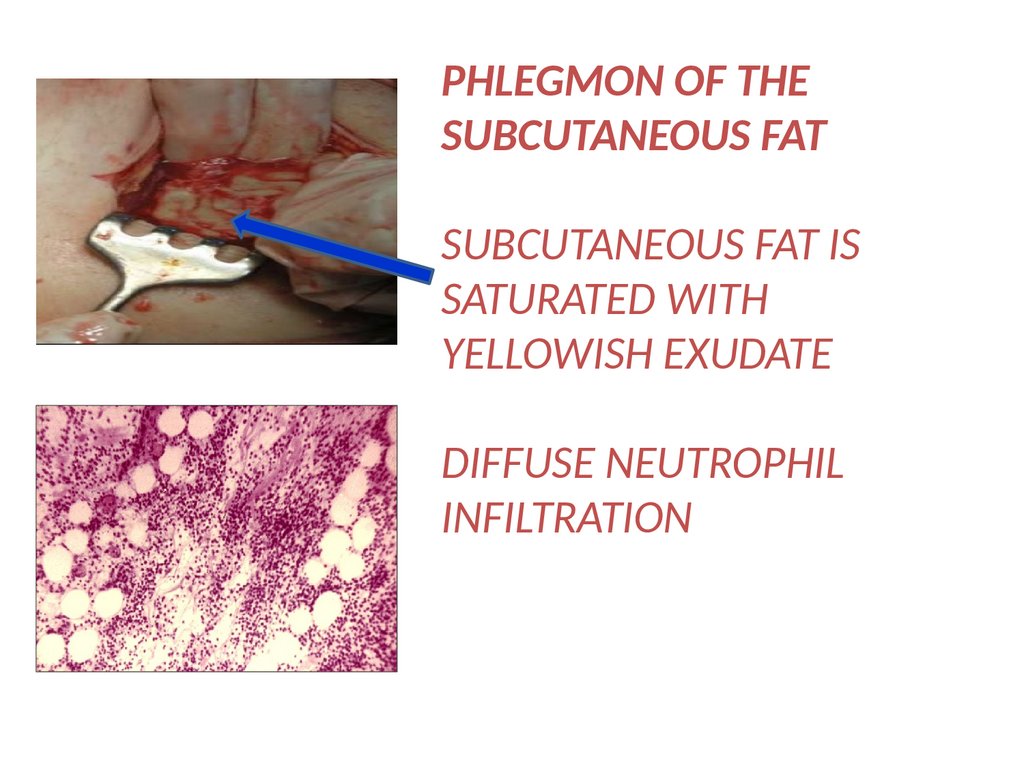
PHLEGMON OF THESUBCUTANEOUS FAT
SUBCUTANEOUS FAT IS
SATURATED WITH
YELLOWISH EXUDATE
DIFFUSE NEUTROPHIL
INFILTRATION
23.
PNEUMONIA WITHABSCESS
FORMATION
2
1
1.SUPPURATIVE
EXUDATE FILLS
WITH ALVEOLAR
SPACES.
2. DESTRUCTION OF
ALVEOLAR SEPTS
LEADS TO ABSCESS
FORMATION
24.
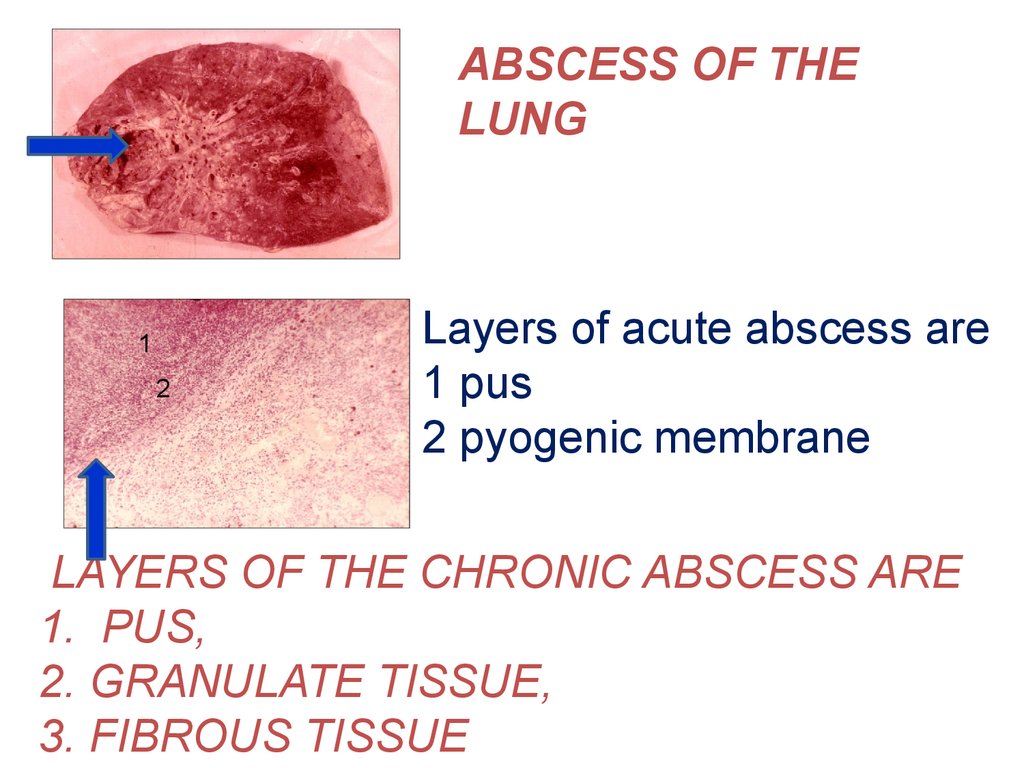
ABSCESS OF THELUNG
1
2
Layers of acute abscess are
1 pus
2 pyogenic membrane
LAYERS OF THE CHRONIC ABSCESS ARE
1. PUS,
2. GRANULATE TISSUE,
3. FIBROUS TISSUE
25.
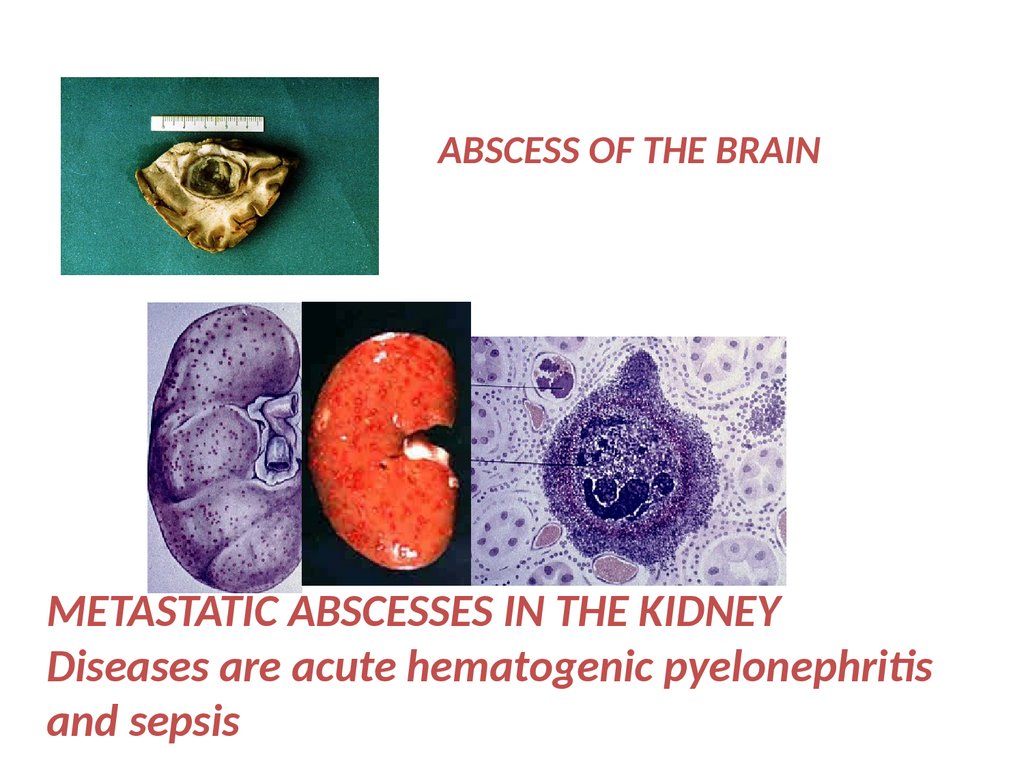
ABSCESS OF THE BRAINMETASTATIC ABSCESSES IN THE KIDNEY
Diseases are acute hematogenic pyelonephritis
and sepsis
26.
ROTTEN (PUTRID ) INFLAMMATIONAPPEARS AS USUAL IN WOUNDS
WITH SEVERY TISSUE DAMAGE
ACCOMPAINED WITH ANAEROBIC
BACTERIA.
SPREAD NECROSIS & ROTTEN SMELL
ARE CHARACTERISTICS
FOR THIS TYPE OF INFLAMMATION
27.
CATARRAL INFLAMMATIONAPPEARES ONLY ON THE MUCOUS
MEMBRANES, WITH PRODUCE MUCUS.
EXUDATE CONTAINS MUCUS
TYPES OF CATARRHAL INFLAMMATION occur
as
1. ACUTE
2.CHRONIC, WHICH MAY BE
atrophic, and hypertrophic
28.
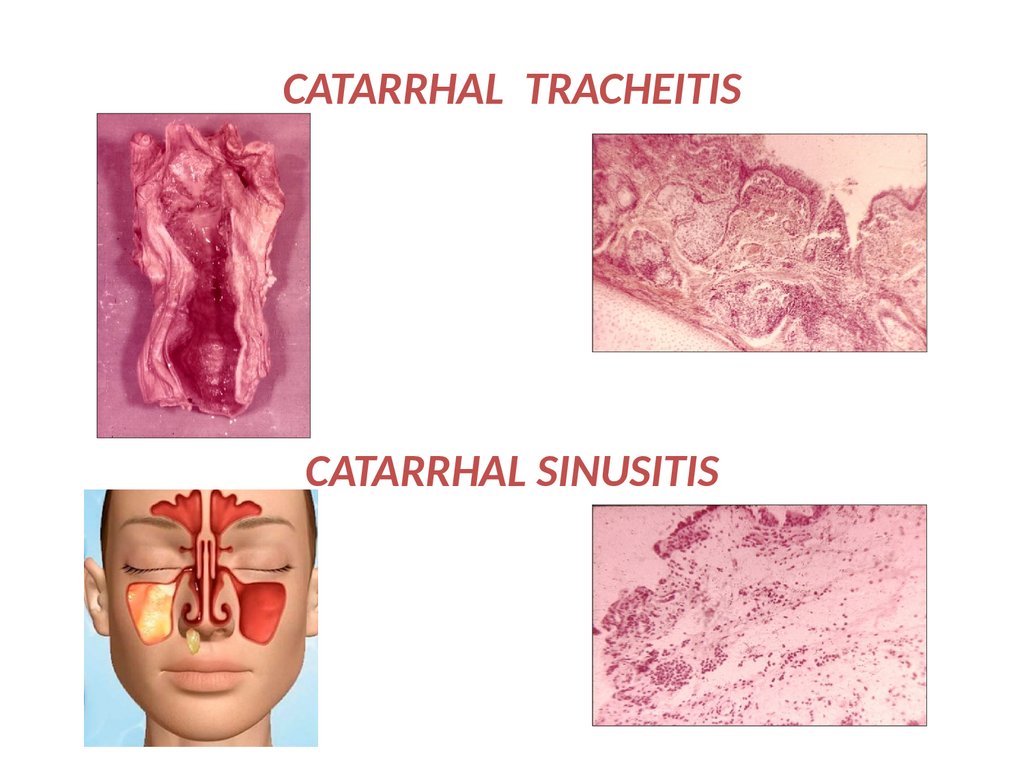
CATARRHAL TRACHEITISCATARRHAL SINUSITIS
29.
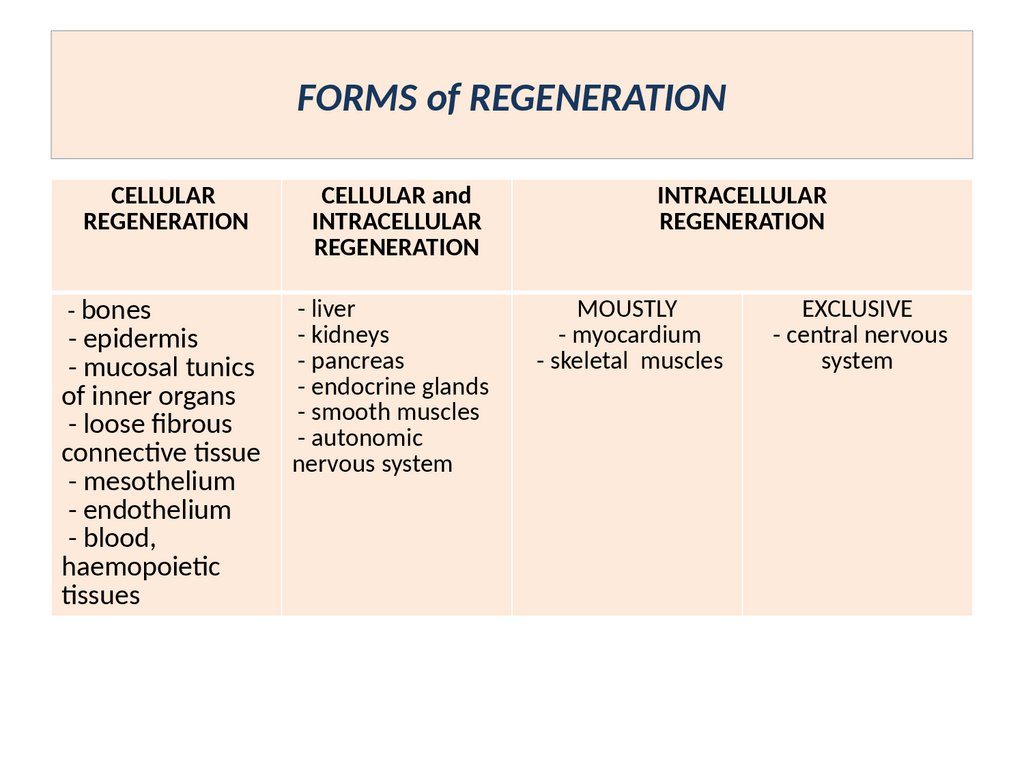
FORMS of REGENERATIONCELLULAR
REGENERATION
- bones
- epidermis
- mucosal tunics
of inner organs
- loose fibrous
connective tissue
- mesothelium
- endothelium
- blood,
haemopoietic
tissues
CELLULAR and
INTRACELLULAR
REGENERATION
- liver
- kidneys
- pancreas
- endocrine glands
- smooth muscles
- autonomic
nervous system
INTRACELLULAR
REGENERATION
MOUSTLY
- myocardium
- skeletal muscles
EXCLUSIVE
- central nervous
system
30.
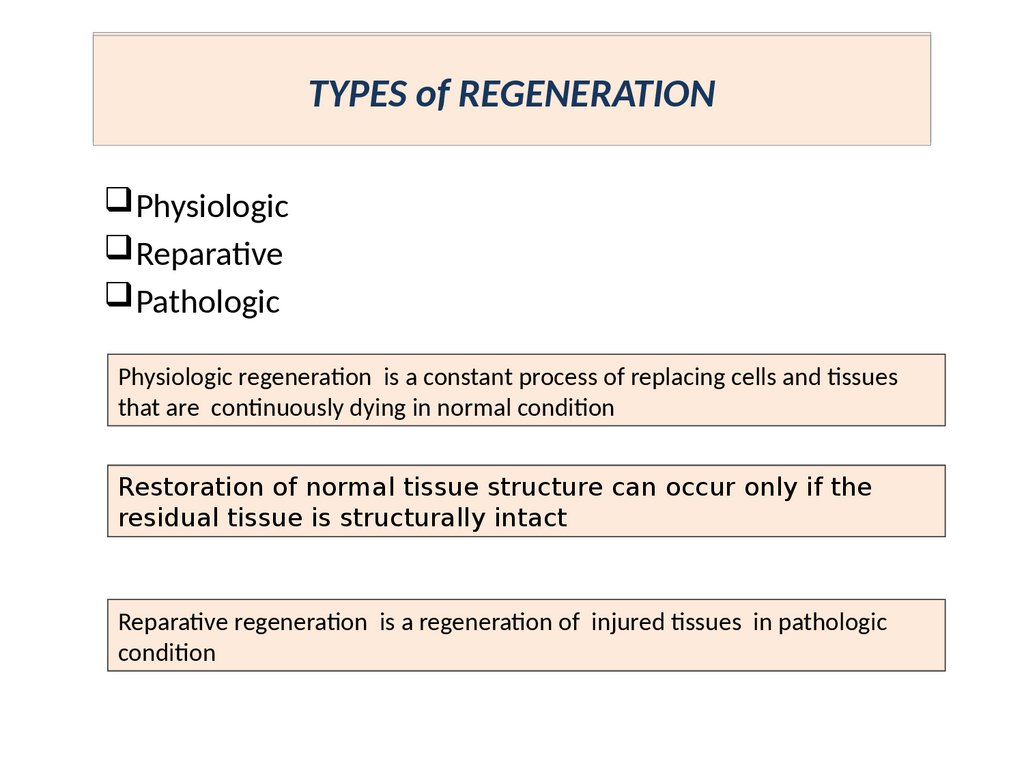
TYPES of REGENERATIONPhysiologic
Reparative
Pathologic
Physiologic regeneration is a constant process of replacing cells and tissues
that are continuously dying in normal condition
Restoration of normal tissue structure can occur only if the
residual tissue is structurally intact
Reparative regeneration is a regeneration of injured tissues in pathologic
condition
31.
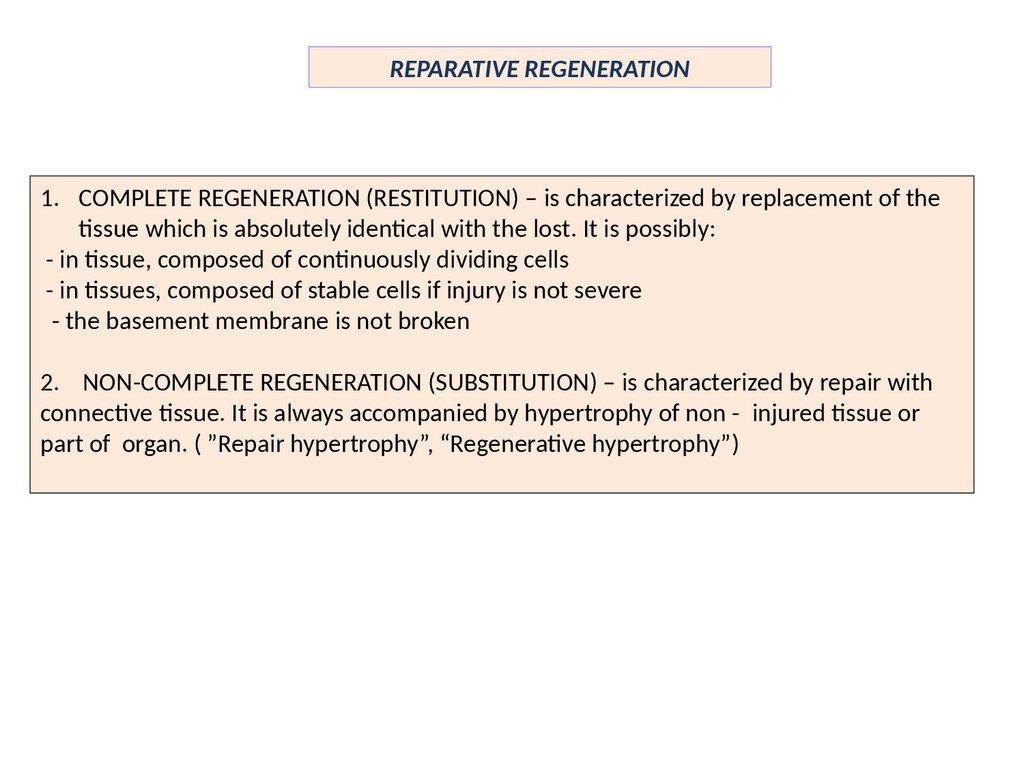
REPARATIVE REGENERATION1. COMPLETE REGENERATION (RESTITUTION) – is characterized by replacement of the
tissue which is absolutely identical with the lost. It is possibly:
- in tissue, composed of continuously dividing cells
- in tissues, composed of stable cells if injury is not severe
- the basement membrane is not broken
2. NON-COMPLETE REGENERATION (SUBSTITUTION) – is characterized by repair with
connective tissue. It is always accompanied by hypertrophy of non - injured tissue or
part of organ. ( ”Repair hypertrophy”, “Regenerative hypertrophy”)
32.
REPARATIVE REGENERATION1. REGENERATION of the mucous
membrane in the intestine.
Complete regeneration due to
proliferations of the columnar epithelial
cells
1. REPAIR REGENERATION (REPAIR
HYPERTROPHY) of the myocardium
with the connective tissue formation
33.
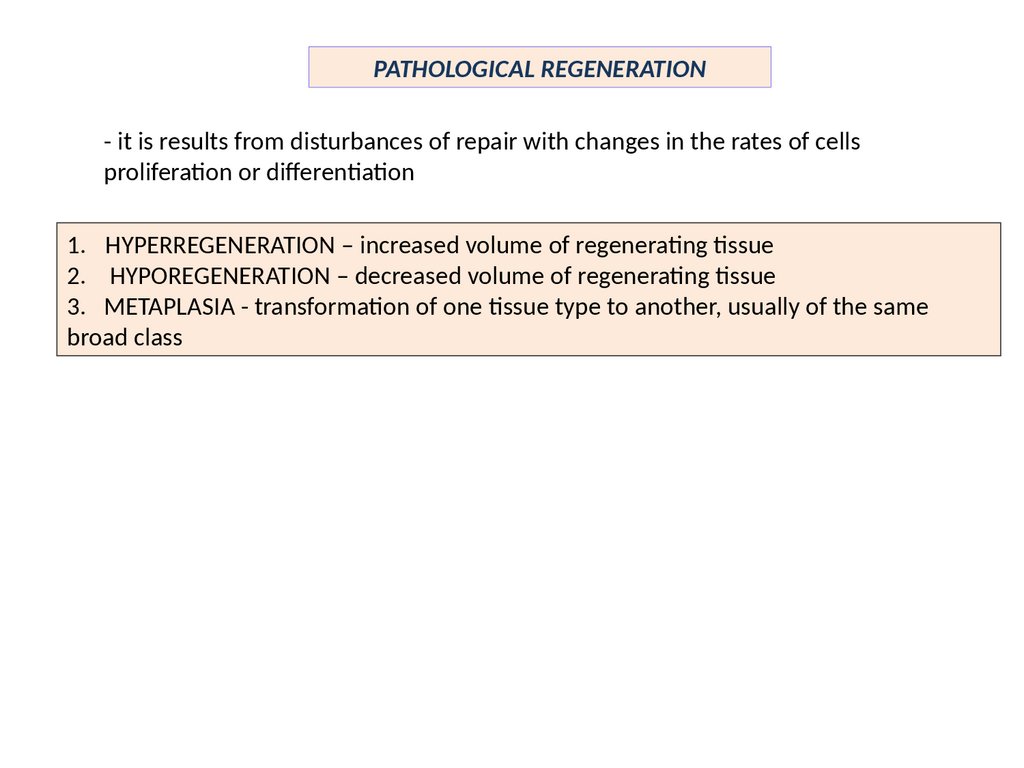
PATHOLOGICAL REGENERATION- it is results from disturbances of repair with changes in the rates of cells
proliferation or differentiation
1. HYPERREGENERATION – increased volume of regenerating tissue
2. HYPOREGENERATION – decreased volume of regenerating tissue
3. METAPLASIA - transformation of one tissue type to another, usually of the same
broad class
34.
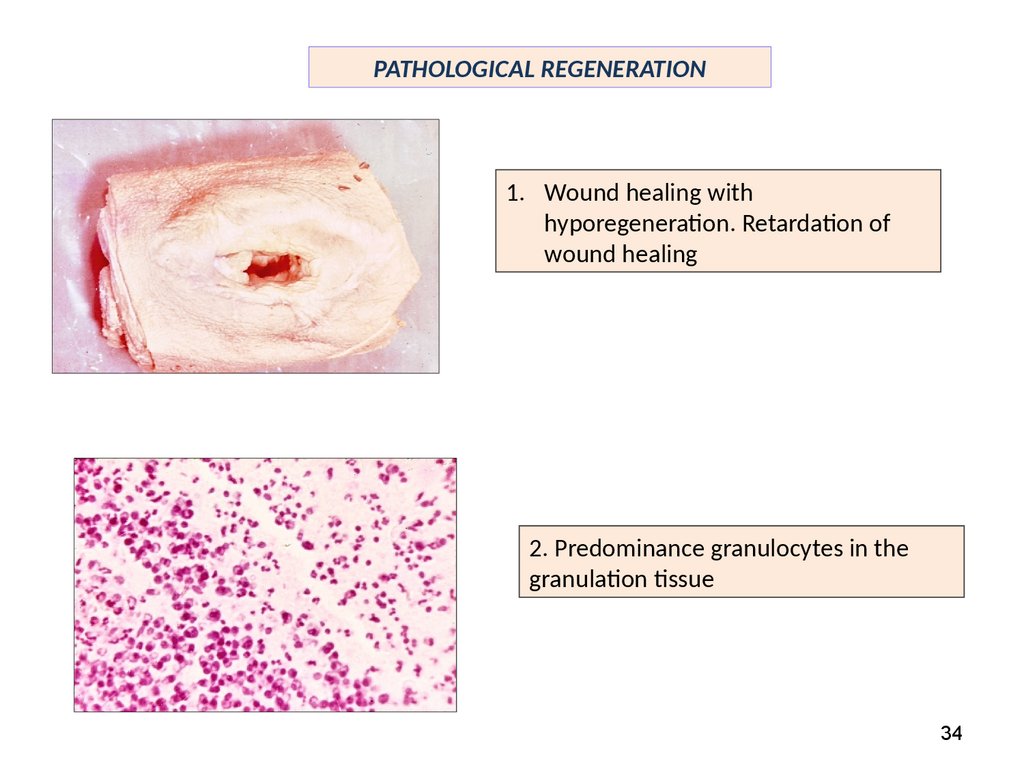
PATHOLOGICAL REGENERATION1. Wound healing with
hyporegeneration. Retardation of
wound healing
2. Predominance granulocytes in the
granulation tissue
34
35.
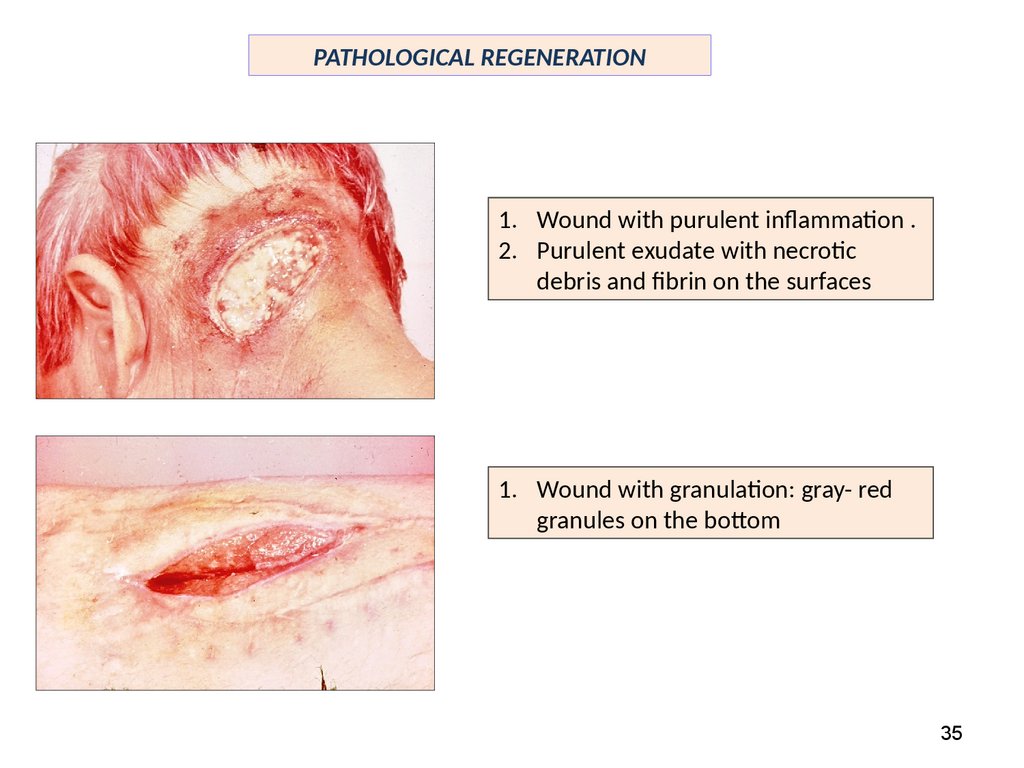
PATHOLOGICAL REGENERATION1. Wound with purulent inflammation .
2. Purulent exudate with necrotic
debris and fibrin on the surfaces
1. Wound with granulation: gray- red
granules on the bottom
35
36.
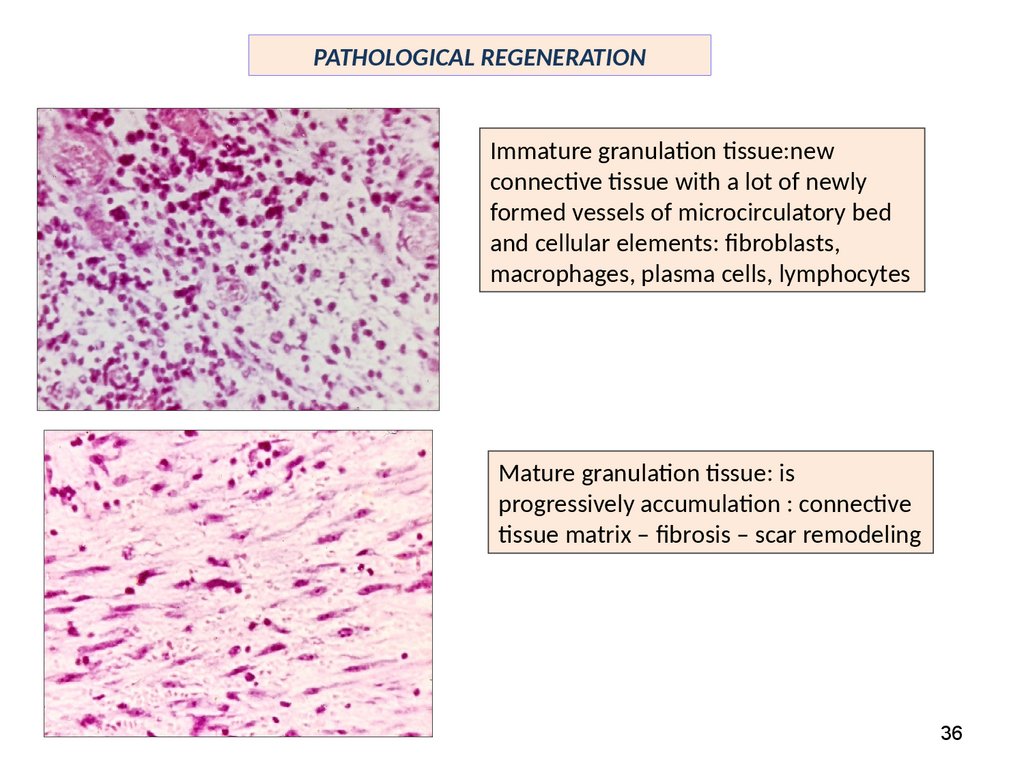
PATHOLOGICAL REGENERATIONImmature granulation tissue:new
connective tissue with a lot of newly
formed vessels of microcirculatory bed
and cellular elements: fibroblasts,
macrophages, plasma cells, lymphocytes
Mature granulation tissue: is
progressively accumulation : connective
tissue matrix – fibrosis – scar remodeling
36
37.
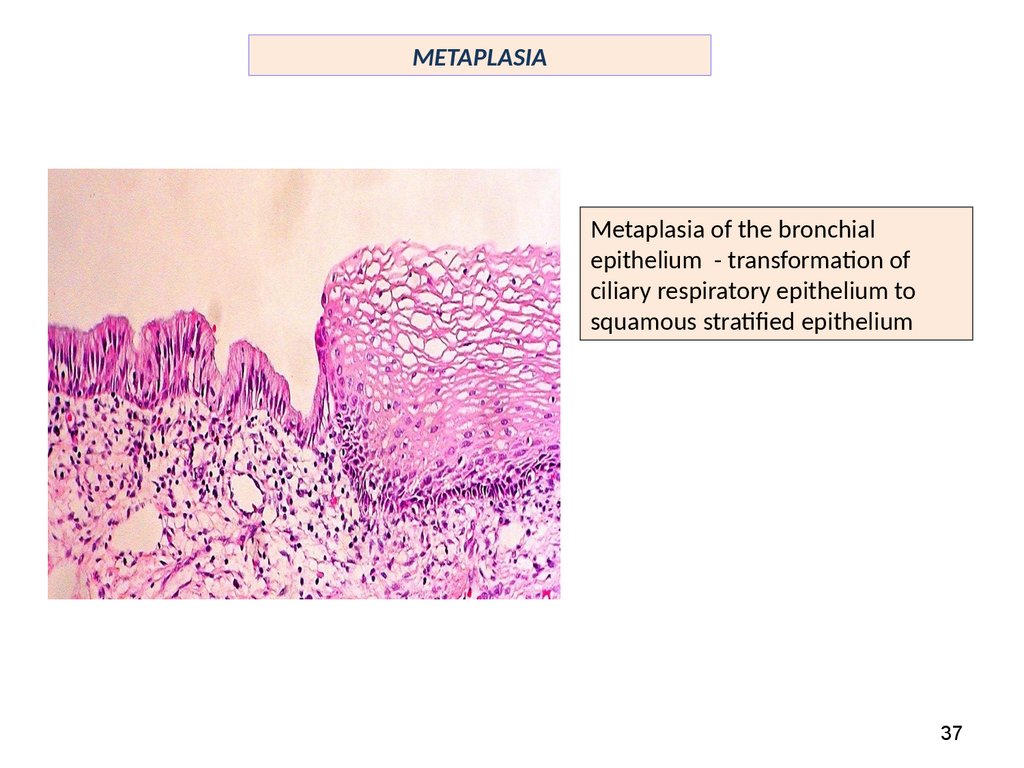
METAPLASIAMetaplasia of the bronchial
epithelium - transformation of
ciliary respiratory epithelium to
squamous stratified epithelium
37
38.
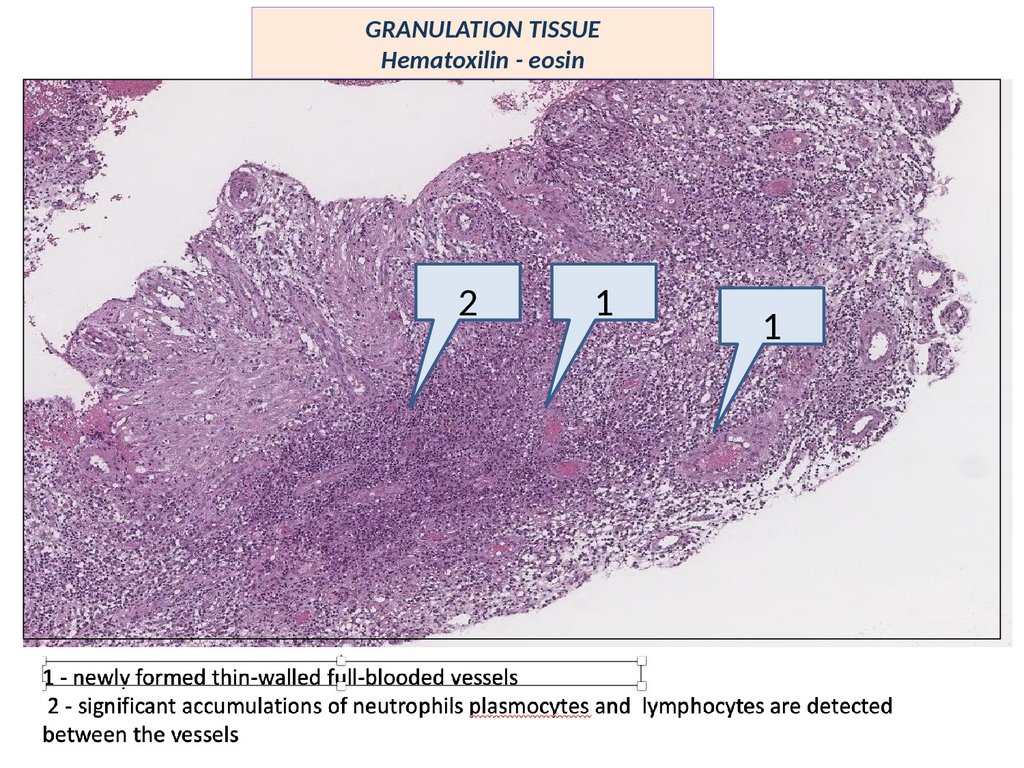
GRANULATION TISSUEHematoxilin - eosin
1
1
2
1 - newly formed thin-walled full-blooded vessels
2 - significant accumulations of neutrophils plasmocytes and lymphocytes are detected
between the vessels
39.
GRANULATION TISSUEHematoxilin - eosin
2
1
1
40.
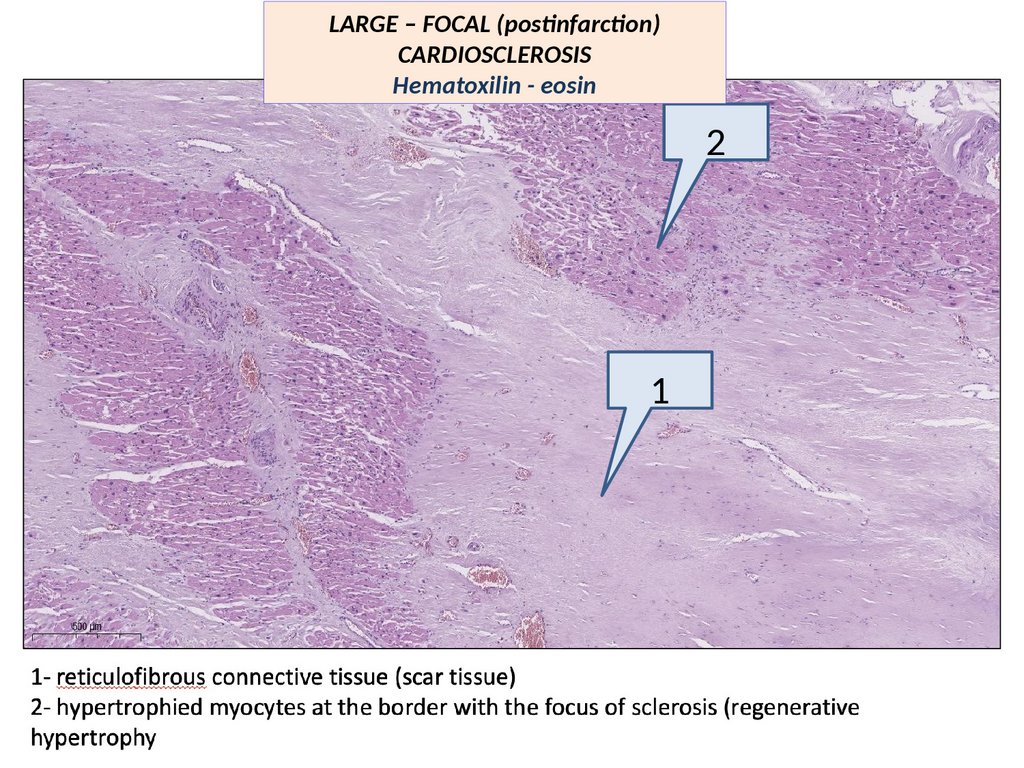
LARGE – FOCAL (postinfarction)CARDIOSCLEROSIS
Hematoxilin - eosin
2
1
41.
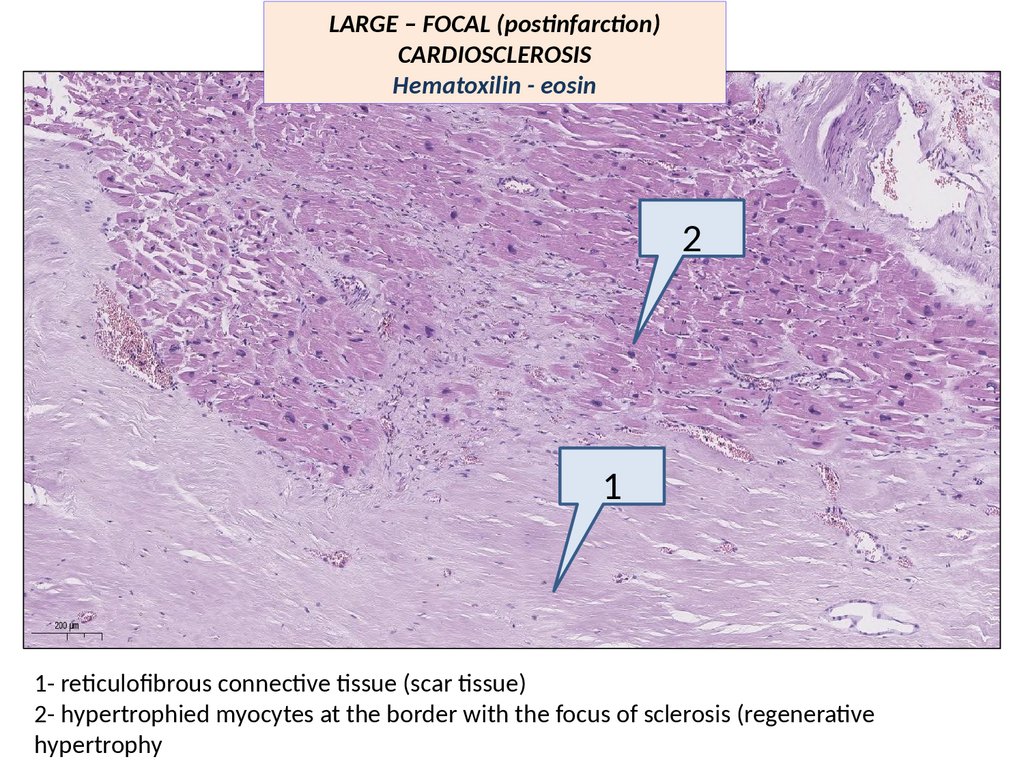
LARGE – FOCAL (postinfarction)CARDIOSCLEROSIS
Hematoxilin - eosin
2
1
1- reticulofibrous connective tissue (scar tissue)
2- hypertrophied myocytes at the border with the focus of sclerosis (regenerative
hypertrophy





 medicine
medicine