Similar presentations:
Vestibular schwannoma
1.
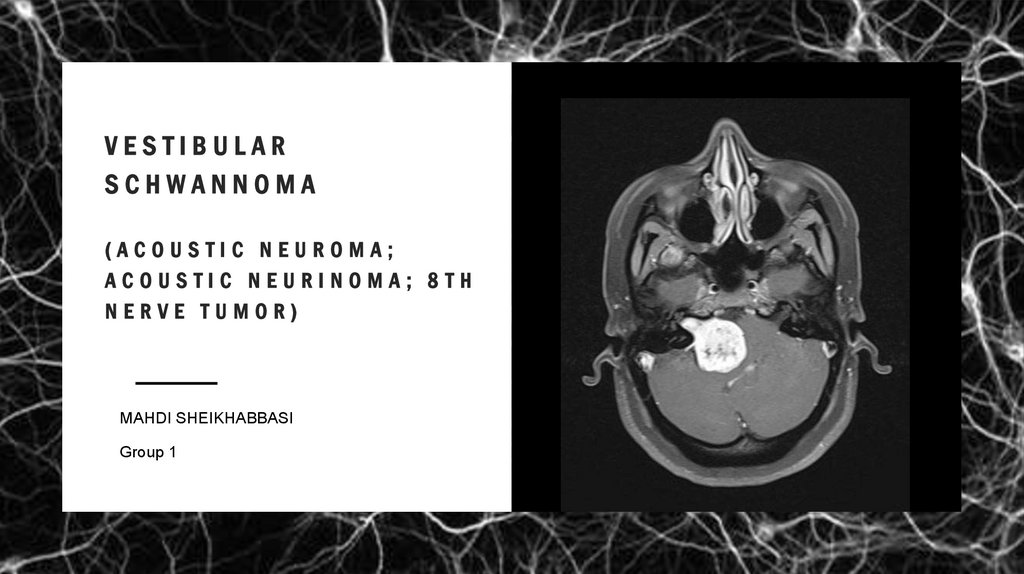
VESTIBULARSCHWANNOMA
(ACOUSTIC NEUROMA;
ACOUSTIC NEURINOMA; 8TH
NERVE TUMOR)
MAHDI SHEIKHABBASI
Group 1
2.
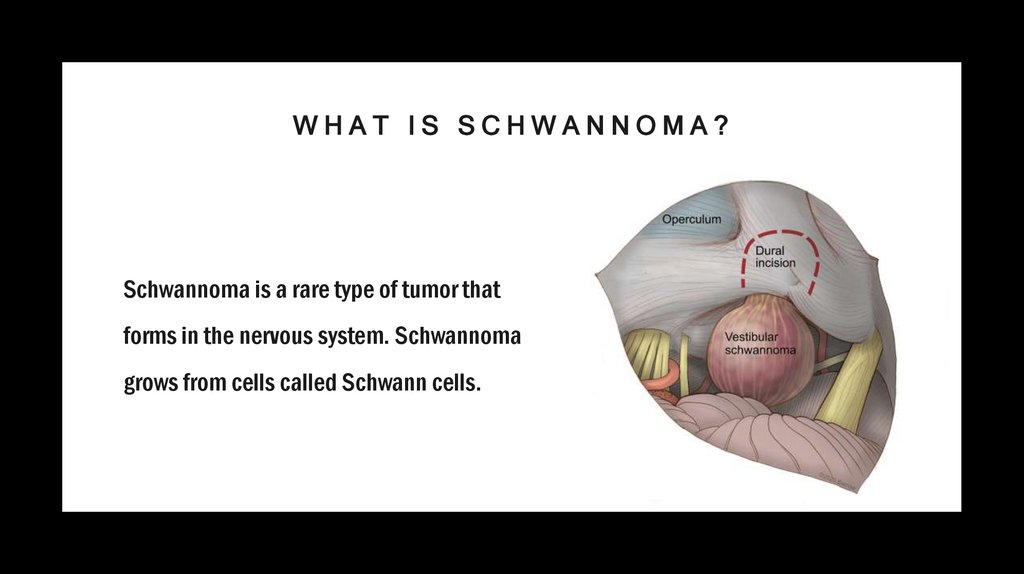
WHAT IS SCHWANNOMA?Schwannoma is a rare type of tumor that
forms in the nervous system. Schwannoma
grows from cells called Schwann cells.
3.
4.
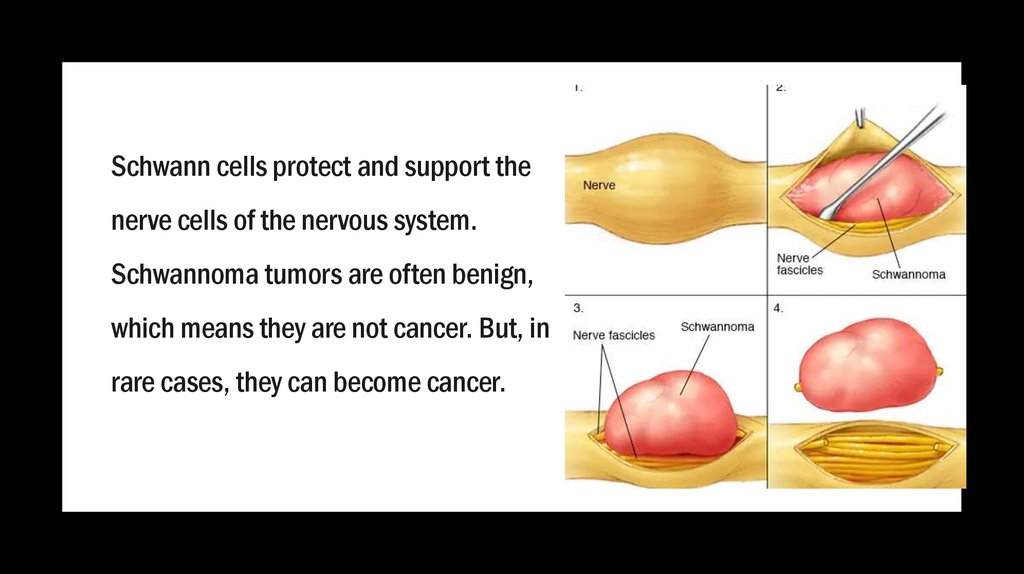
Schwann cells protect and support thenerve cells of the nervous system.
Schwannoma tumors are often benign,
which means they are not cancer. But, in
rare cases, they can become cancer.
5.
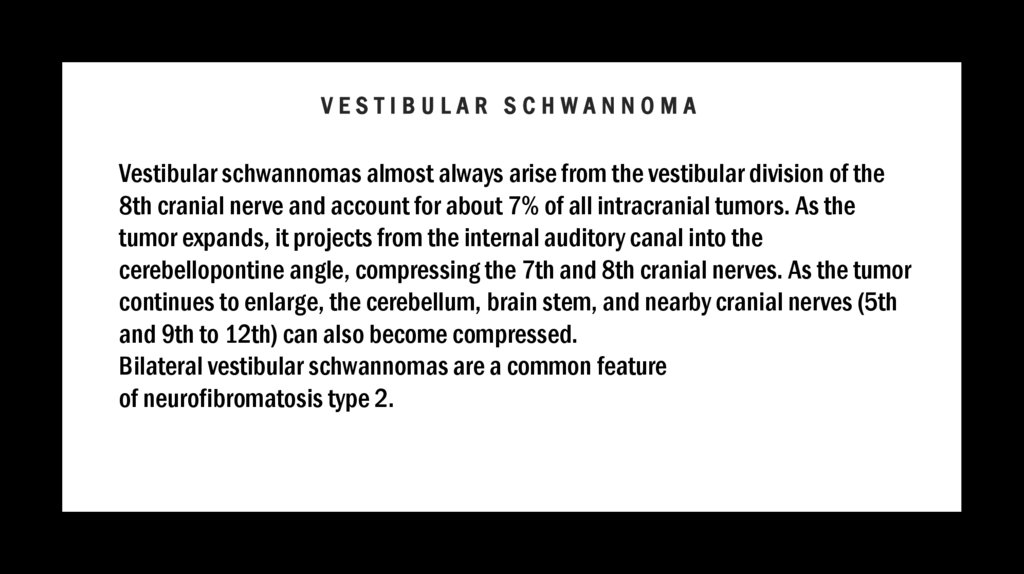
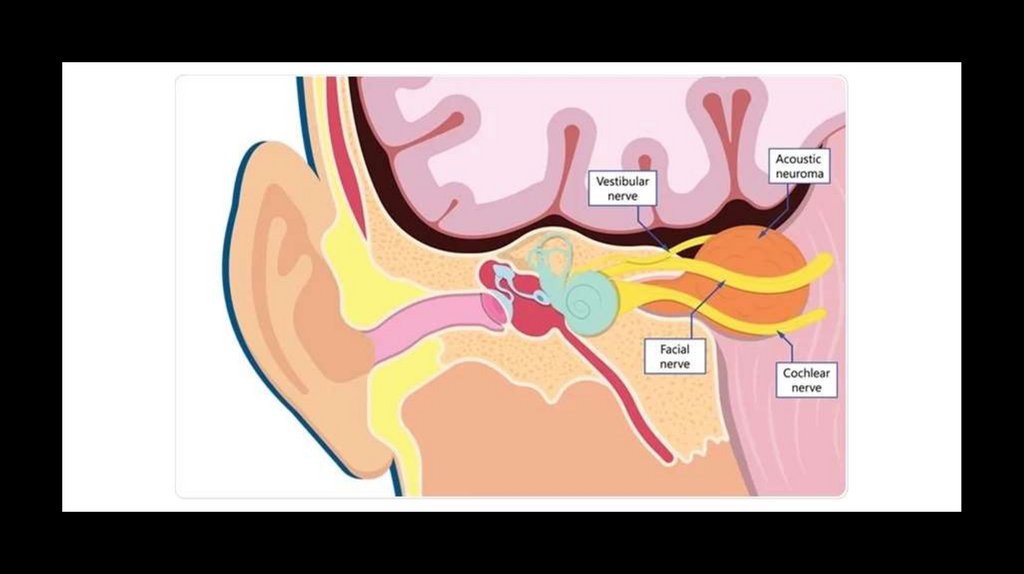
VESTIBULAR SCHWANNOMAVestibular schwannomas almost always arise from the vestibular division of the
8th cranial nerve and account for about 7% of all intracranial tumors. As the
tumor expands, it projects from the internal auditory canal into the
cerebellopontine angle, compressing the 7th and 8th cranial nerves. As the tumor
continues to enlarge, the cerebellum, brain stem, and nearby cranial nerves (5th
and 9th to 12th) can also become compressed.
Bilateral vestibular schwannomas are a common feature
of neurofibromatosis type 2.
6.
7.
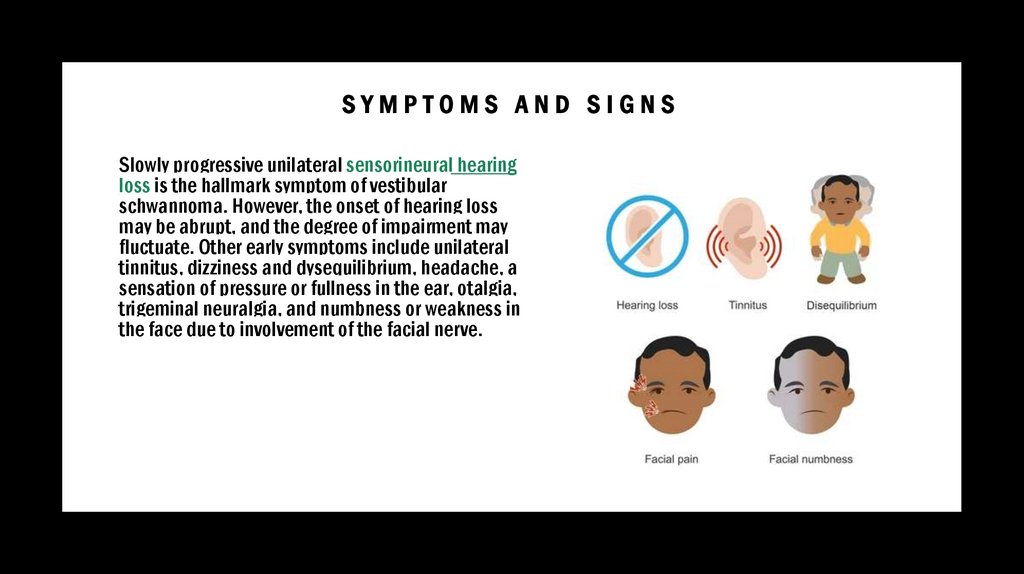
SYMPTOMS AND SIGNSSlowly progressive unilateral sensorineural hearing
loss is the hallmark symptom of vestibular
schwannoma. However, the onset of hearing loss
may be abrupt, and the degree of impairment may
fluctuate. Other early symptoms include unilateral
tinnitus, dizziness and dysequilibrium, headache, a
sensation of pressure or fullness in the ear, otalgia,
trigeminal neuralgia, and numbness or weakness in
the face due to involvement of the facial nerve.
8.
DIAGNOSISI. Audiogram
II. Gadolinium-enhanced MRI
Most commonly, an audiogram is the first test done to diagnose vestibular schwannoma. It usually detects an
asymmetric sensorineural hearing loss and a greater impairment of speech discrimination than would be
expected for the degree of hearing loss. Such findings indicate the need for imaging tests, preferably
gadolinium-enhanced MRI. However, some tumors are found incidentally when brain imaging is done for
another reason.
Other findings include presence of acoustic reflex decay on tympanometry. Auditory brain stem response
testing may show the absence of waveforms and/or increased latency of the 5th waveform.
Although not usually required in the routine evaluation of a patient with asymmetric sensorineural hearing
loss, caloric testing shows marked vestibular hypoactivity (canal paresis) on the affected side.
9.
PRINCIPLES OF TREATMENTI.
Observation
II.
Sometimes surgical removal or stereotactic radiation therapy in selected cases
Small, asymptomatic (ie, discovered incidentally), and nongrowing vestibular schwannomas do not
require treatment; such tumors may be observed with serial MRI scans and treated if they begin
growing or cause symptoms. Whether to use stereotactic radiation therapy (eg, gamma knife or
cyberknife radiation therapy) or conventional microsurgery depends on many factors including the
amount of residual hearing, tumor size, and patient age and health. Stereotactic radiation therapy
tends to be used for older patients, those with smaller tumors, or those who cannot have surgery for
medical reasons. Microsurgery can involve a hearing-preservation approach (middle cranial fossa
or retrosigmoid approach) or a translabyrinthine approach if there is no useful residual hearing.
10.
EVOLUTION IN SURGICAL TREATMENT OF VESTIBULARSCHWANNOMAS
Preoperative Management
there is a standardized preoperative assessment of VS patients. Every VS patient
undergoes a MRI of the head (with and without contrast enhancement) and a
bone window CT scan of the skull base. Tumor sizes were classified according to
Koos system into T1 to T4. Additionally, a transesophageal echocardiography (TEE)
is requested to rule out a patent foramen ovale in patients selected for surgery in
semi-sitting position. Pure tone audiography with speech discrimination and
auditory evoked potentials are performed to classify hearing according to Gardner
and Robertson grading. Facial nerve function is photo-documented and graded
according to the House and Brackmann grading scale.
11.
I N T R A O P E R AT I V E M O N I TO R I N GVS surgeries are generally performed under continuous intraoperative
neuromonitoring (IONM). IONM encompass the somatosensory- (SSEP) and
motor-evoked potentials (MEPs) to the upper and lower extremities, corticobulbar
motor-evoked potentials (CoMEPs), and free-running electromyography (EMG) of
the affected cranial nerves (CN VII, XI, XII) as well as the brainstem auditory-evoked
potentials (BAEPs). To avoid any damage to the cervical spinal cord during the
positioning maneuver, particularly for the semi-sitting position, SSEPS are recorded
before and immediately after the patient has been seated and the head fixed with
the head clamp. Any significant drop on the SSEP may indicate major spine cord
compression that demands positioning adjustments.
12.
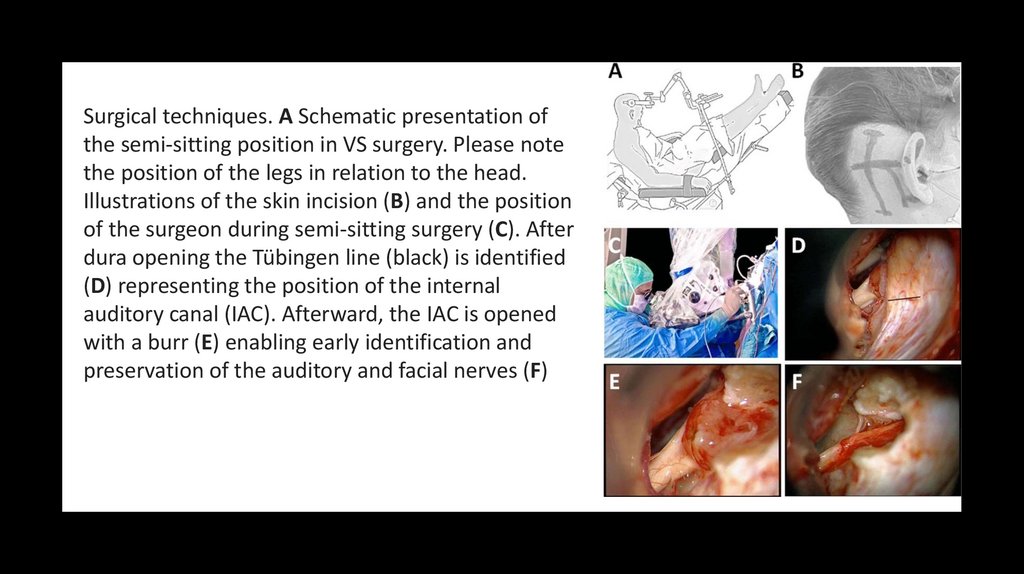
Surgical techniques. A Schematic presentation ofthe semi-sitting position in VS surgery. Please note
the position of the legs in relation to the head.
Illustrations of the skin incision (B) and the position
of the surgeon during semi-sitting surgery (C). After
dura opening the Tübingen line (black) is identified
(D) representing the position of the internal
auditory canal (IAC). Afterward, the IAC is opened
with a burr (E) enabling early identification and
preservation of the auditory and facial nerves (F)
13.
MICROSURGICAL TECHNIQUEVS surgery is performed either in a supine (SP) or a semi-sitting position (SSP)
depending on tumor size and risk profile of the patient. A slightly curved skin
incision is planned approximately 3–4 cm behind the ear, above the asterion from
the level of the tip of the ear down to the level of the mastoid tip. The
retrosigmoid approach allows removal of tumors of all sizes; it is compatible with
hearing and facial nerve preservation, and it permits in large tumors an excellent
control of the lower cranial nerves at the very early beginning of the exposure at
the CPA. In young patients, a bone flap is cut and detached along the transversal
and sigmoid sinus; in older patients, a craniectomy is done after piecemeal bone
removal, to avoid dura or sinus wall laceration, since dura adherence is common in
elderly patients.
14.
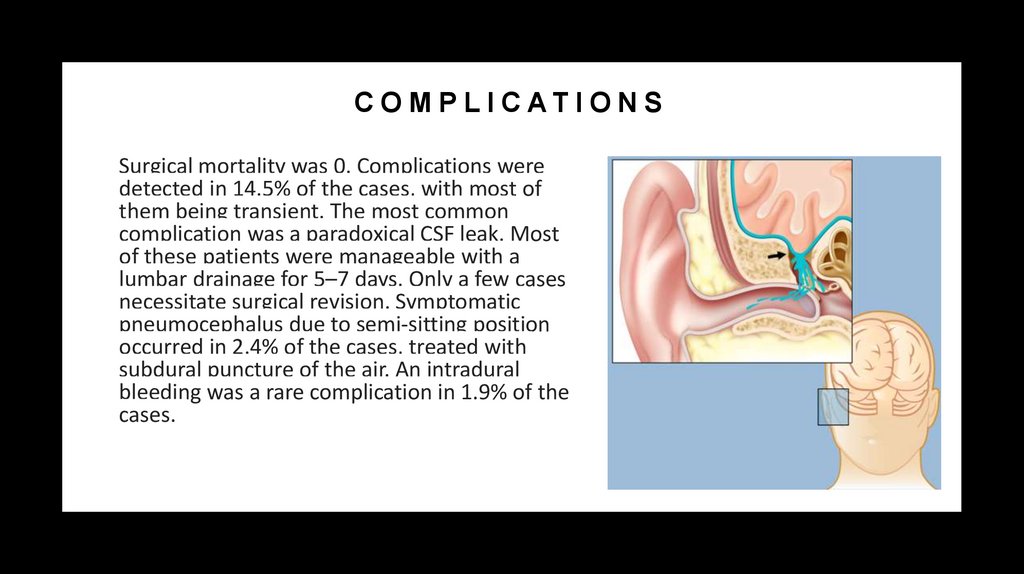
C O M P L I C AT I O N SSurgical mortality was 0. Complications were
detected in 14.5% of the cases, with most of
them being transient. The most common
complication was a paradoxical CSF leak. Most
of these patients were manageable with a
lumbar drainage for 5–7 days. Only a few cases
necessitate surgical revision. Symptomatic
pneumocephalus due to semi-sitting position
occurred in 2.4% of the cases, treated with
subdural puncture of the air. An intradural
bleeding was a rare complication in 1.9% of the
cases.
15.
CONCLUSIONIn conclusion, surgery of VS has been refined and
represents a powerful tool for treatment of the
disease. In our opinion surgery is mostly indicated in
large VS but also in small VS in young patients and in
female patients in whom pregnancy is expected.
16.
REFERENCEShttps://www.msdmanuals.com/professional/ear,-nose,-and-throatdisorders/inner-ear-disorders/vestibular-schwannoma?query=schwannoma
https://neurosurgery.weillcornell.org/condition/csf-leaks/symptoms-cranial-csf-leak
https://link.springer.com/article/10.1007/s40136-021-00366-2
https://thejns.org/view/journals/j-neurosurg/105/4/article-p527.xml

 medicine
medicine