Similar presentations:
Clinical pathological anatomy Les1 Biopsy Autopsy
1.
LESSON 1Research Methods and Objectives of
Pathological Anatomy in Clinic
2.
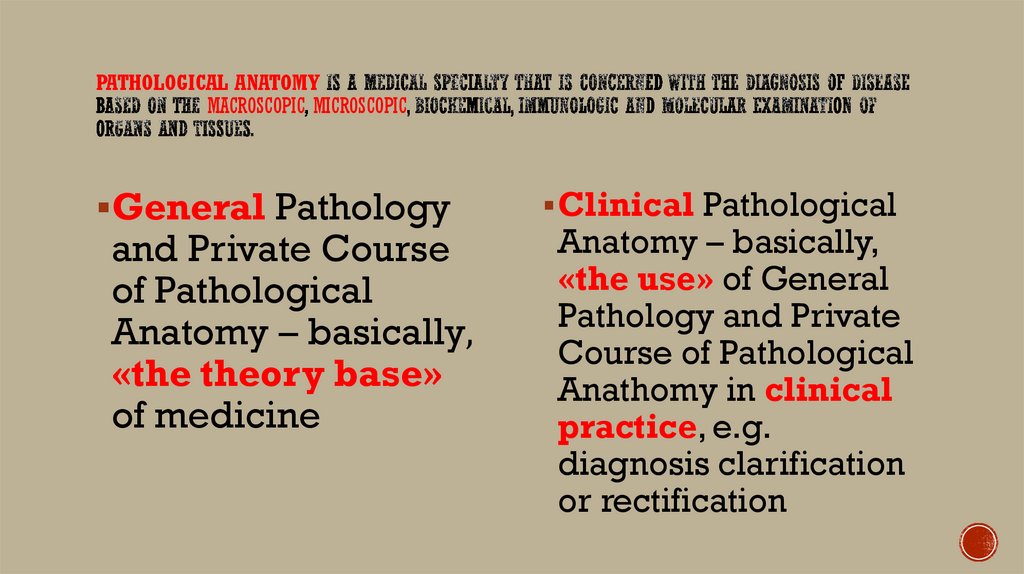
PATHOLOGICAL ANATOMYMACROSCOPIC MICROSCOPIC
General Pathology
and Private Course
of Pathological
Anatomy – basically,
«the theory base»
of medicine
Clinical Pathological
Anatomy – basically,
«the use» of General
Pathology and Private
Course of Pathological
Anathomy in clinical
practice, e.g.
diagnosis clarification
or rectification
3.
4.
1. CONTROL OFCORRECT AND
TIMELY MAKING OF
DIAGNOSIS
This is provided
by the
COMPARSION of
clinical and postmortem
diagnoses. The
DISCREPANCY
RATE in Russia is
about 12-19%.
5.
2. PATHOLOGISTPARTICIPATION IN
TREATING PROCESS
This is
provided by
intravital
microscopic
diagnostic of
patients’
samples.
6.
3. DETECTION OFINFECTIOUS
DISEASES
Some infectious
diseases could
be suspected
(and confirmed)
during the
autopsy, so the
spread of the
disease can be
stopped in the
morgue.
7.
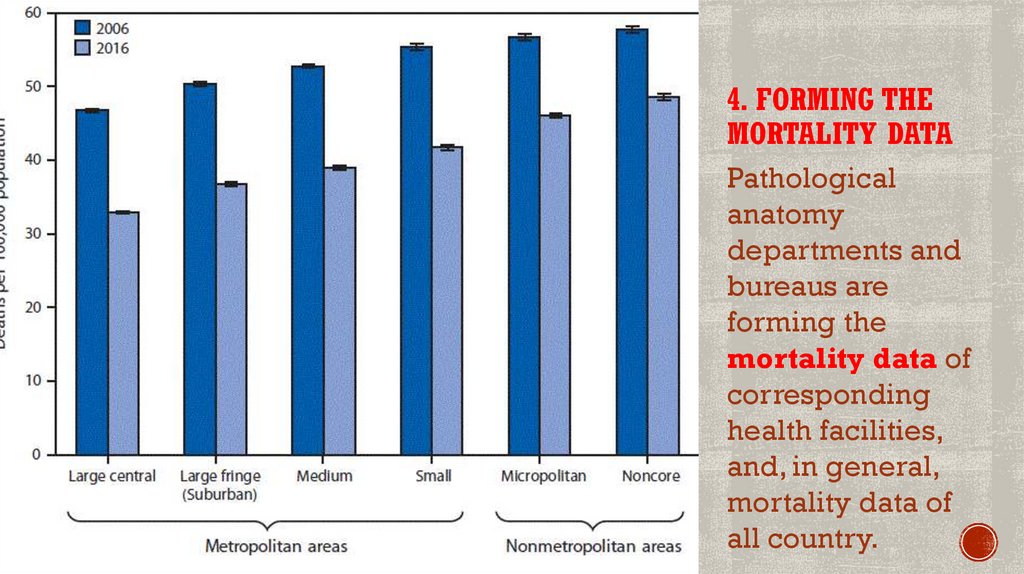
4. FORMING THEMORTALITY DATA
Pathological
anatomy
departments and
bureaus are
forming the
mortality data of
corresponding
health facilities,
and, in general,
mortality data of
all country.
8.
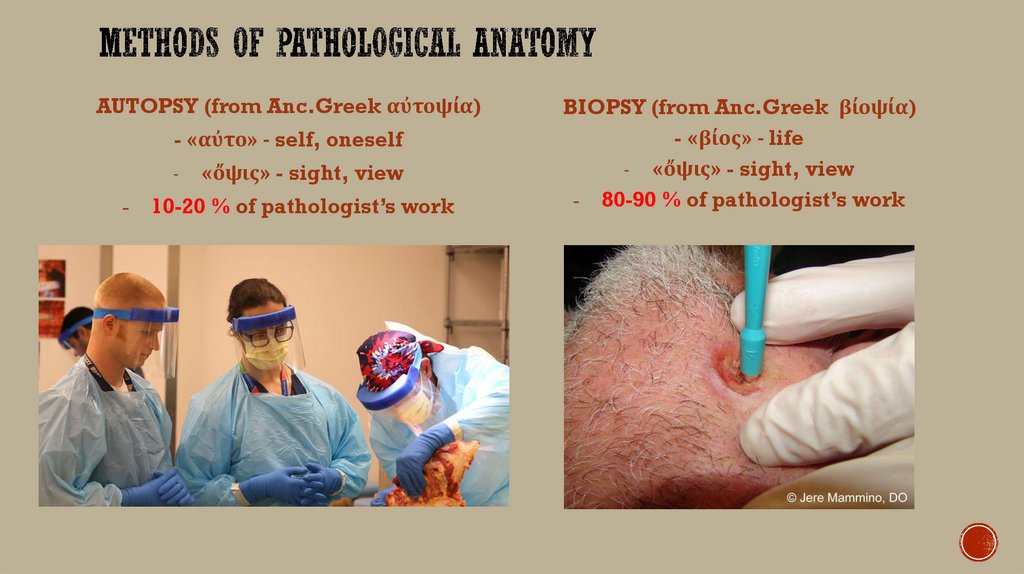
AUTOPSY (from Anc.Greek αὐτοψία)- «αὐτο» - self, oneself
-
-
«ὄψις» - sight, view
10-20 % of pathologist’s work
BIOPSY (from Anc.Greek βίοψία)
- «βίος» - life
- «ὄψις» - sight, view
- 80-90 % of pathologist’s work
9.
BIOPSY is an EXTRACTION of sample cells or tissues from theLIVING patient for MICROSCOPIC examination to determine the
presence or extent of a pathological process.
The biopsy is one of the most PRECISE and RELIABLE diagnostic
methods.
The biopsy can make a diagnosis on the EARLY stages of disease
(most often in ONCOLOGY) and, by that, allows to start the specific
treatment EARLY and raises the SURVIVAL RATE.
The early detection of disease can also RELIEVE the patient from the
long and expensive diagnostic methods.
The intrasurgical express-biopsy determines the EXTENT of
surgical operation in general surgery, surgical oncology and
gynecology surgery.
10.
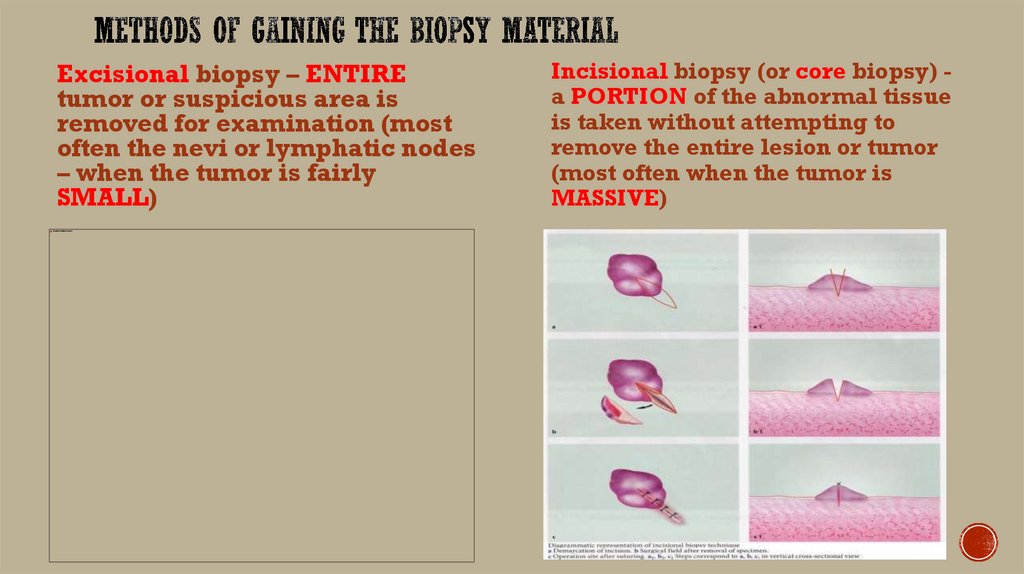
Excisional biopsy – ENTIREtumor or suspicious area is
removed for examination (most
often the nevi or lymphatic nodes
– when the tumor is fairly
SMALL)
Incisional biopsy (or core biopsy) a PORTION of the abnormal tissue
is taken without attempting to
remove the entire lesion or tumor
(most often when the tumor is
MASSIVE)
11.
Punch biopsy – small roundpiece of tissue about the size of a
pencil eraser is removed using a
sharp, hollow, circular
instrument
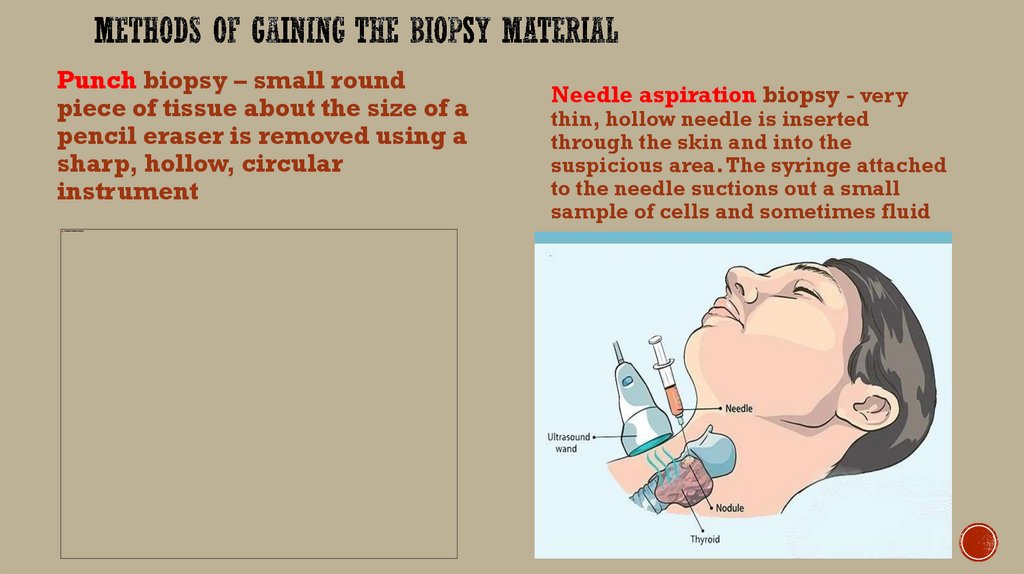
Needle aspiration biopsy - very
thin, hollow needle is inserted
through the skin and into the
suspicious area.The syringe attached
to the needle suctions out a small
sample of cells and sometimes fluid
12.
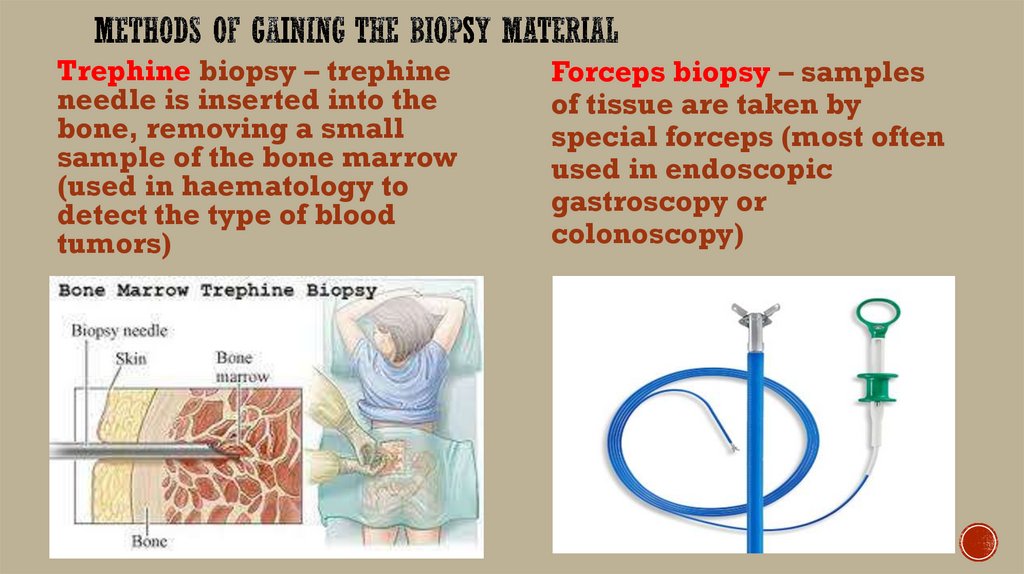
Trephine biopsy – trephineneedle is inserted into the
bone, removing a small
sample of the bone marrow
(used in haematology to
detect the type of blood
tumors)
Forceps biopsy – samples
of tissue are taken by
special forceps (most often
used in endoscopic
gastroscopy or
colonoscopy)
13.
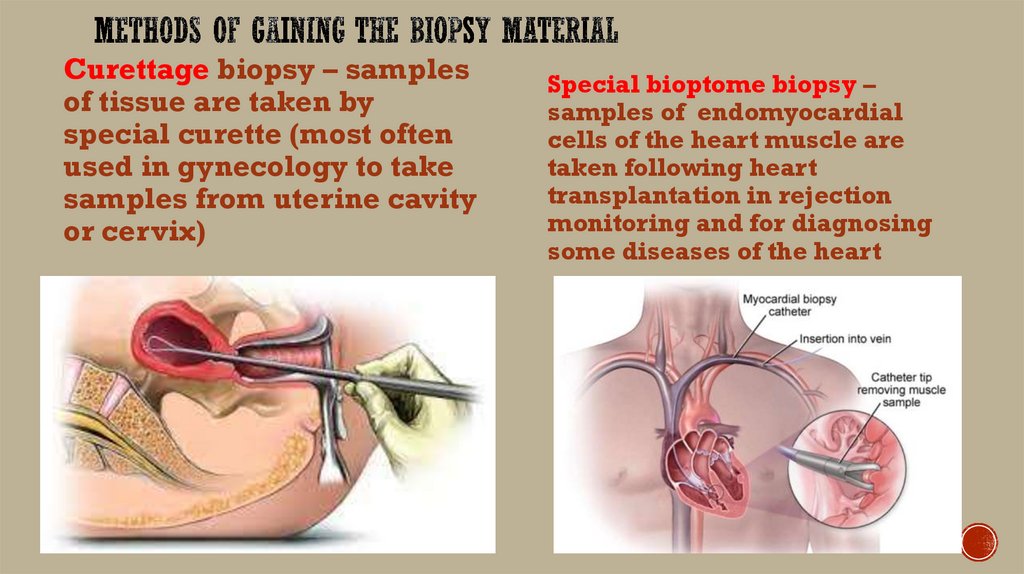
Curettage biopsy – samplesof tissue are taken by
special curette (most often
used in gynecology to take
samples from uterine cavity
or cervix)
Special bioptome biopsy –
samples of endomyocardial
cells of the heart muscle are
taken following heart
transplantation in rejection
monitoring and for diagnosing
some diseases of the heart
14.
During all the ENDOSCOPIC DIAGNOSTICPROCEDURES in gastroenterology and gynecology
Mandatory TUMOR VERIFICATION in oncology –
determination of histological types of tumors and
differentiation grade (well-, moderately-, poorly- or
undifferentiated tumors)
During all the SURGICAL OPERATIONS, where the
samples of tissue or even the whole organ are removed
In obstetrics after the delivery all the PLACENTAS are
mandatory examined to determine the risk rate of
newborn’s several diseases
15.
16.
1. THE BIOPSYSAMPLES ARE
PLACED IN BIOPSY
JARS
The medical personnel
of the clinic put the
samples in special
sterilized jars with tight
cap. The jar must be
properly marked with
the patients personal
data (name, surname,
patronymic, date of
birth, clinic
department).
17.
2. THE BIOPSY JARSARE FILLED WITH
STABILIZING
LIQUIDS
The 10% aqueous
solution of
formaldehyde
(FORMALIN) is
most commonly
used. Formalin
prevents the
degradation of
biopsy samples.
18.
The samples must be put in formalin AS FAST AS POSSIBLE. Insome cases (high summer temperature, high moisture) the samples
can degrade even after a few minutes
The volume of formalin taken must be at least 10 TIMES MORE than
the volume of samples
The thickness of sliced samples must not exceed 4-5
MILLIMETERS
The samples of walls of the hollow organs (e.g. stomach, esophagus,
intestines, urine bladder) must be stretched of a little piece of
cardboard or thin wooden plank
The formalin from the jar MUST NOT BE USED the second time
The ideal temperature of storing the biopsy jars is about 37-40 C, but
most often the jars are stored at room temperature
The time of stabilization in formalin must not exceed 48 HOURS
19.
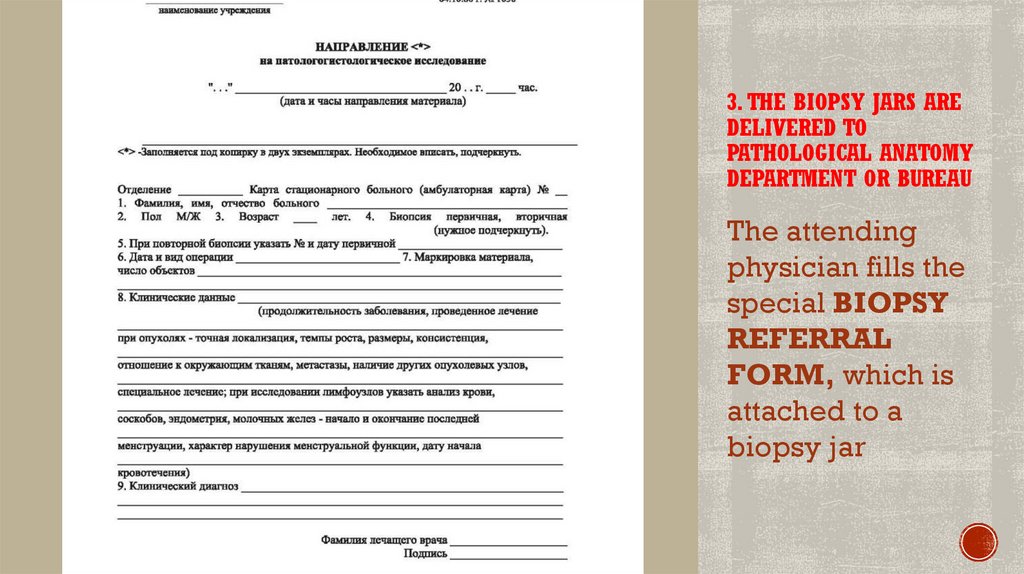
3. THE BIOPSY JARS AREDELIVERED TO
PATHOLOGICAL ANATOMY
DEPARTMENT OR BUREAU
The attending
physician fills the
special BIOPSY
REFERRAL
FORM, which is
attached to a
biopsy jar
20.
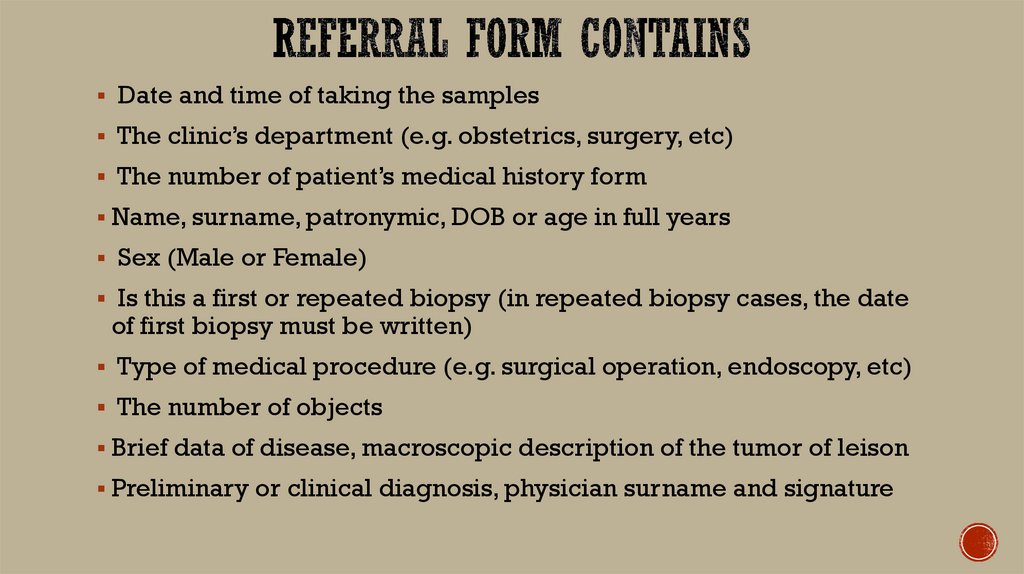
Date and time of taking the samplesThe clinic’s department (e.g. obstetrics, surgery, etc)
The number of patient’s medical history form
Name, surname, patronymic, DOB or age in full years
Sex (Male or Female)
Is this a first or repeated biopsy (in repeated biopsy cases, the date
of first biopsy must be written)
Type of medical procedure (e.g. surgical operation, endoscopy, etc)
The number of objects
Brief data of disease, macroscopic description of the tumor of leison
Preliminary or clinical diagnosis, physician surname and signature
21.
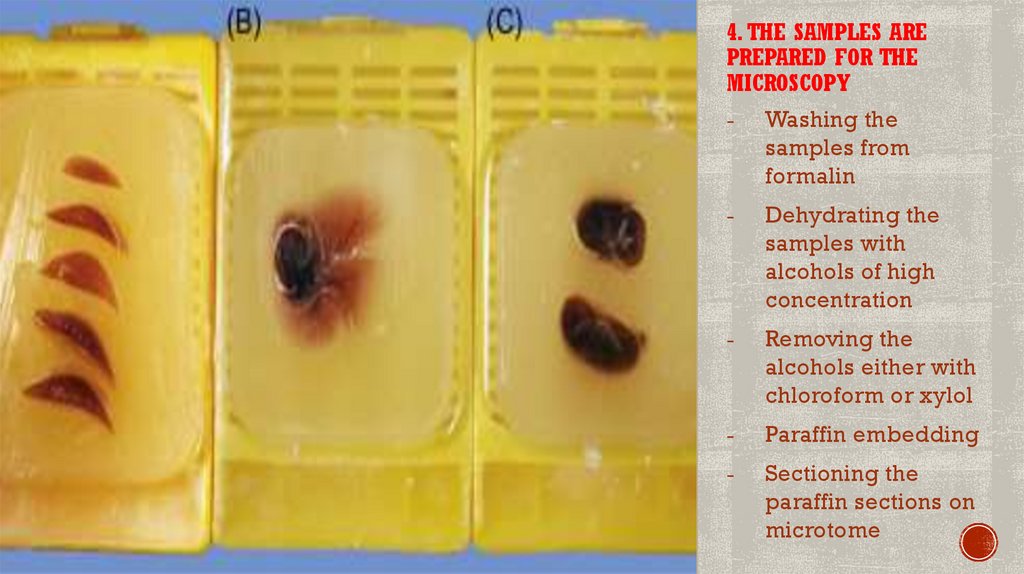
4. THE SAMPLES AREPREPARED FOR THE
MICROSCOPY
-
Washing the
samples from
formalin
-
Dehydrating the
samples with
alcohols of high
concentration
-
Removing the
alcohols either with
chloroform or xylol
-
Paraffin embedding
-
Sectioning the
paraffin sections on
microtome
22.
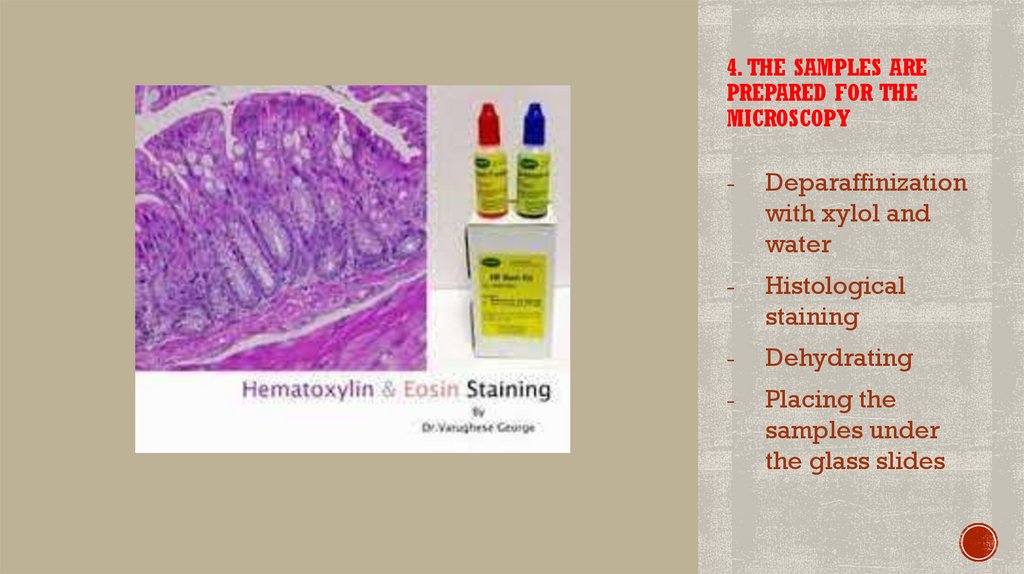
4. THE SAMPLES AREPREPARED FOR THE
MICROSCOPY
-
Deparaffinization
with xylol and
water
-
Histological
staining
-
Dehydrating
-
Placing the
samples under
the glass slides
23.
24.
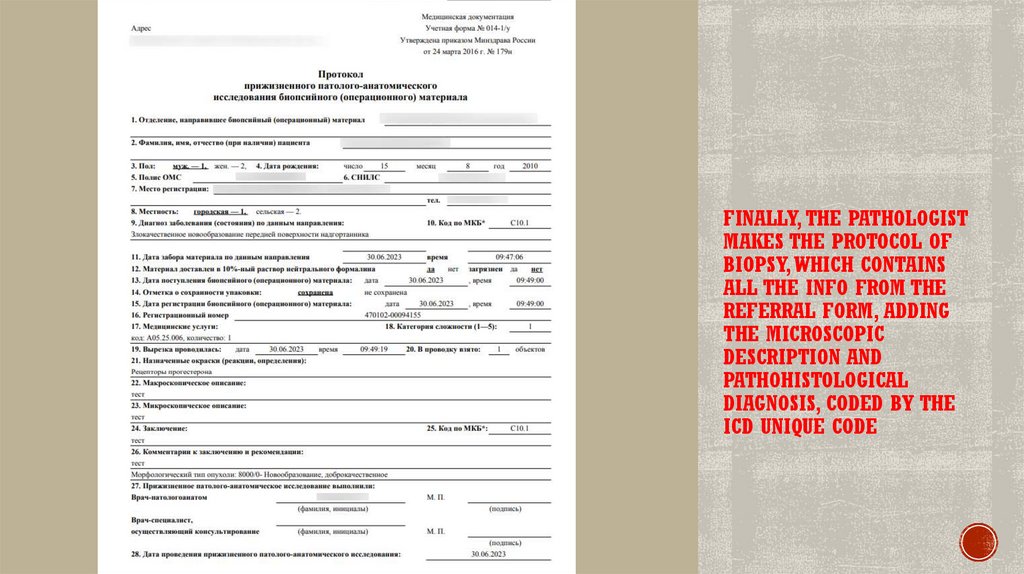
FINALLY, THE PATHOLOGISTMAKES THE PROTOCOL OF
BIOPSY, WHICH CONTAINS
ALL THE INFO FROM THE
REFERRAL FORM, ADDING
THE MICROSCOPIC
DESCRIPTION AND
PATHOHISTOLOGICAL
DIAGNOSIS, CODED BY THE
ICD UNIQUE CODE


 medicine
medicine