Similar presentations:
Leishmaniasis
1.
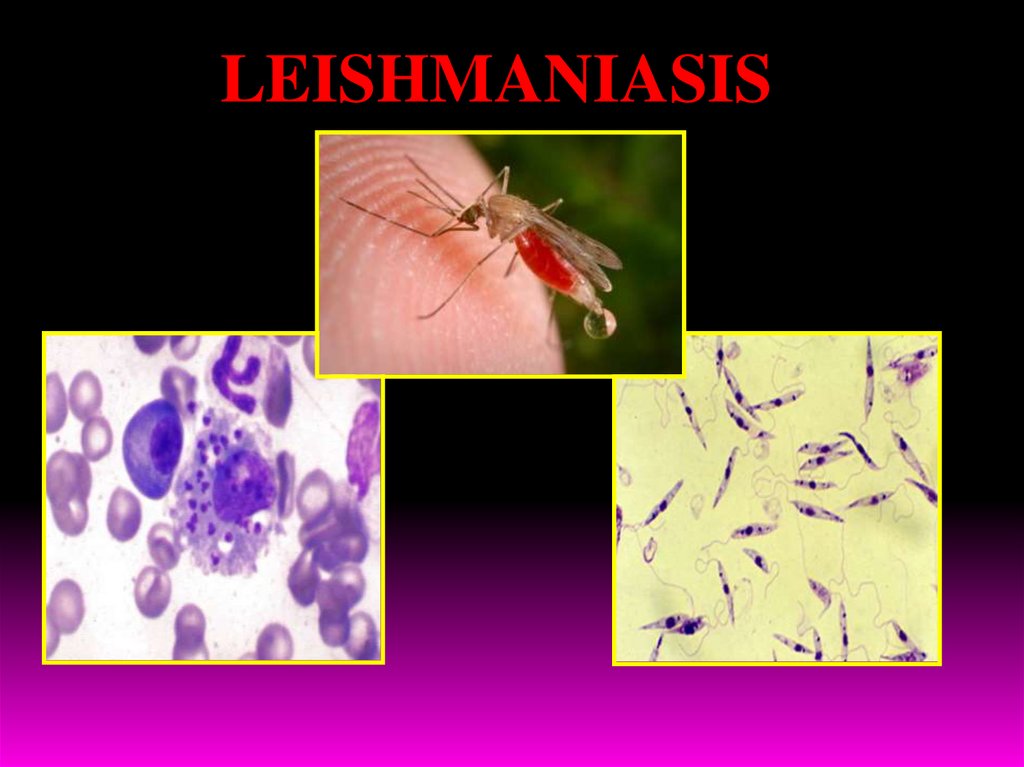
LEISHMANIASIS2.
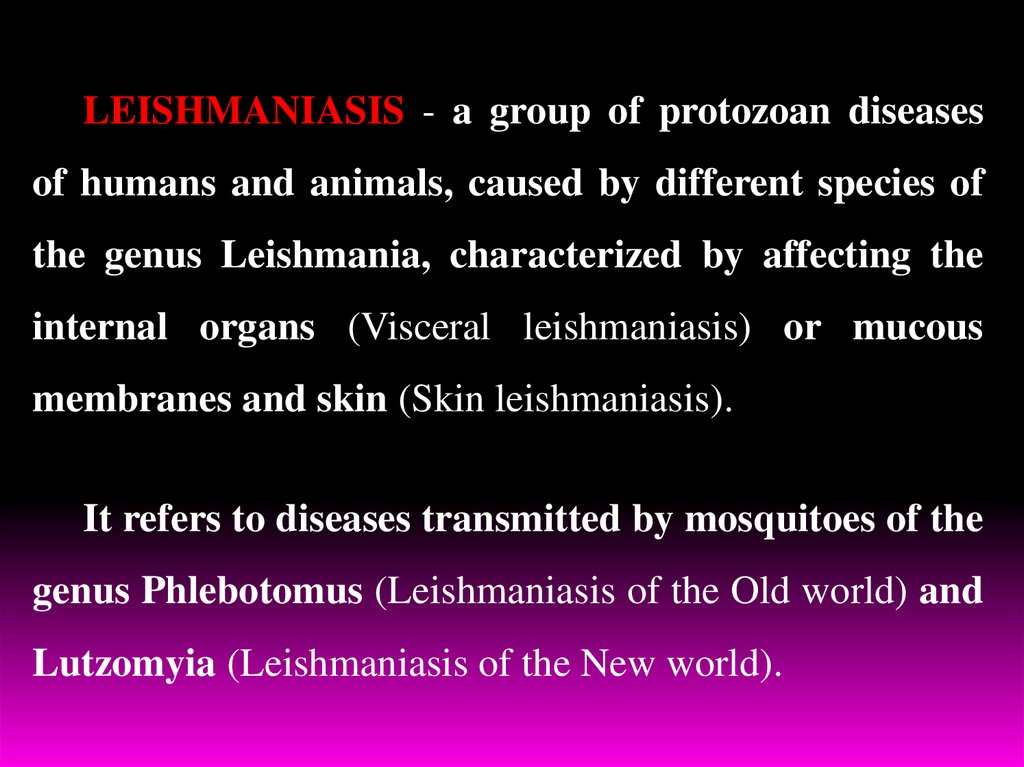
LEISHMANIASIS - a group of protozoan diseasesof humans and animals, caused by different species of
the genus Leishmania, characterized by affecting the
internal organs (Visceral leishmaniasis) or mucous
membranes and skin (Skin leishmaniasis).
It refers to diseases transmitted by mosquitoes of the
genus Phlebotomus (Leishmaniasis of the Old world) and
Lutzomyia (Leishmaniasis of the New world).
3.
1. Leishmaniasis takes an important place in tropical pathology.2. According to WHO, leishmaniasis common in 88 countries of the
world, in 32 countries – it is subject of obligatory registration.
3. According to expert estimates, the number of patients with
Leishmaniasis in the world - more than 12 million people. There
are 2million new cases annually.
4. Approximately 350 million people live in endemic area.
5. Leishmaniasis included in the special program of
WHO «Study and struggle with tropical diseases».
6. Leishmaniases is one of the most actual problems due to its ability
to suppress immune system, especially in persons with HIV or
AIDS.
4.
ClassificationВ55 Leishmaniasis
В55.0 Visceral Leishmaniasis (Leishmaniosis visceralis).
By type:
- anthroponotic - Indian VL (Kala-Azar);
- zoonotic - Mediterranean, Central Asia
visceral leishmaniasis (children's Kala Azar),
- the East African leishmaniasis,
- visceral leishmaniasis of New world.
By duration: acute, subacute, chronic, latent, subclinical.
By periods: initial, climax, terminal (cachexia).
By severity: mild, moderate, severe.
Leading syndromes: exanthema, fever, polilymphadenopathy,
hepatosplenomegaly, haemorragic syndrom, cachexia
5.
В55. Dermal leishmaniasisВ55. Mucocutaneous leishmaniasis
By type: - leishmaniasis of the Old World (Borovski disease):
a) anthponotic subtype;
b) zoonotic subtype (Pendjdeh ulcer):
- primary leishmanioma
(stage tubercle, ulcer, scarring),
- sequential leishmanioma, diffuse-infiltrative
leishmanioma,
- tuberculoid (lupoid) leishmaniasis.
- leishmaniasis of New World: American, Mexican, Amazon,
diffused, Panaman, Peru, Venezuelian.
В55.9 Leishmaniasis of unknown origin.
Example of formulation of diagnosis:
Indian VL, chronic form, moderate severity, manifest period with hepatolienal
syndrome.
6.
7.
8.
9.
10.
11.
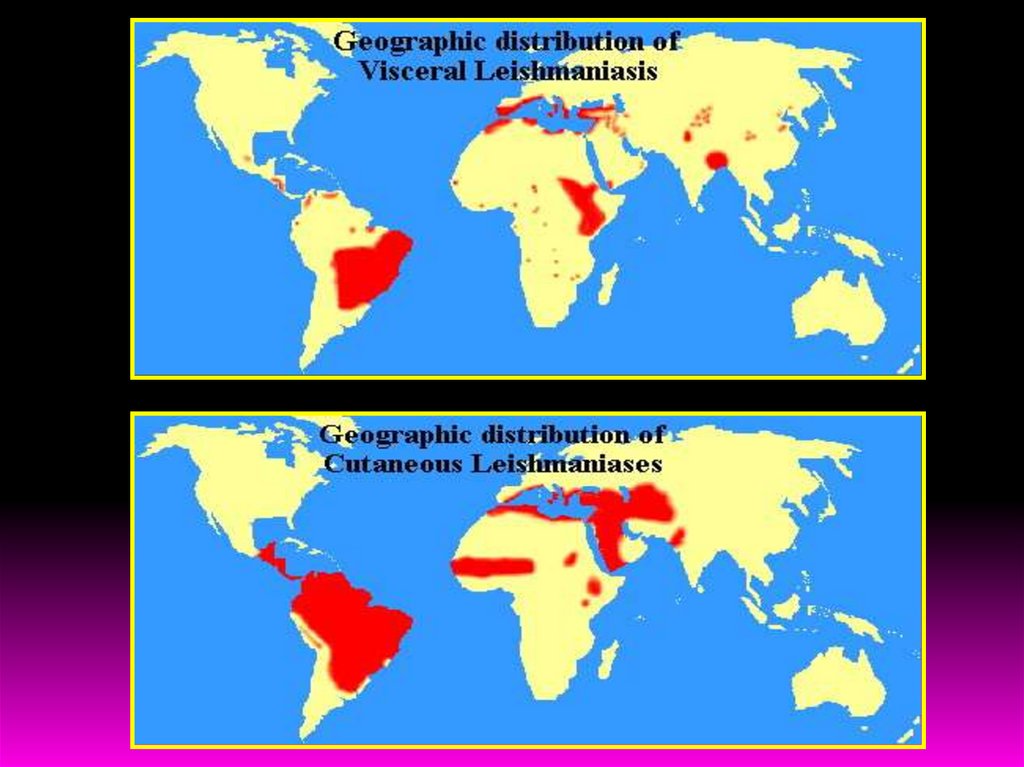
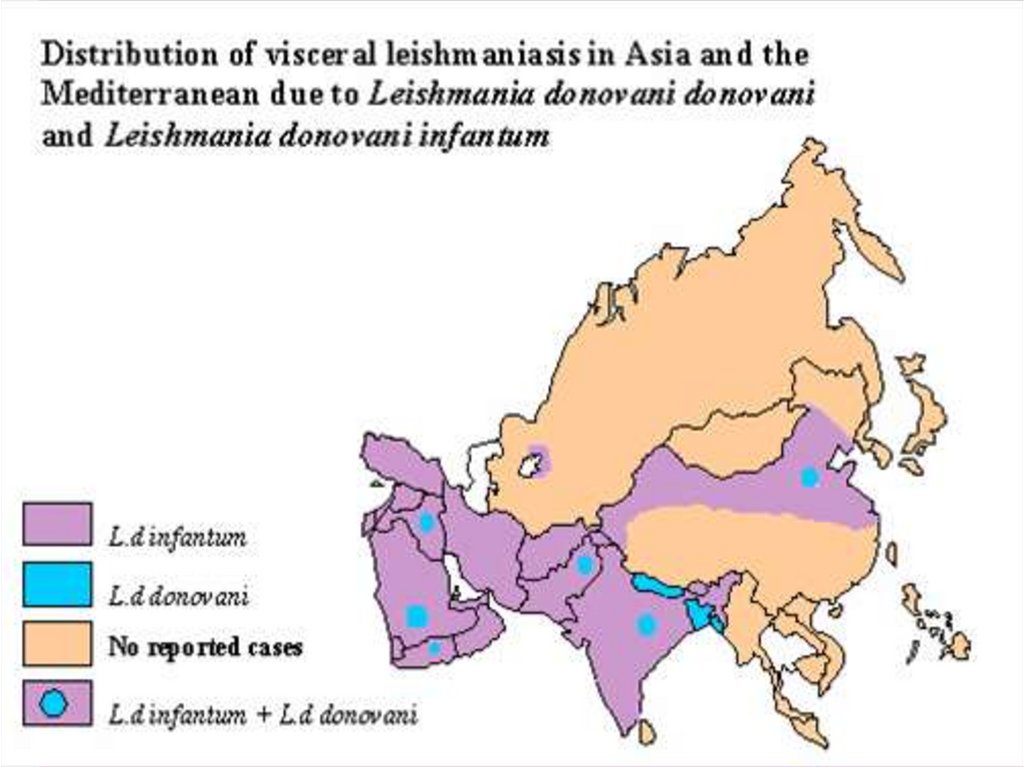
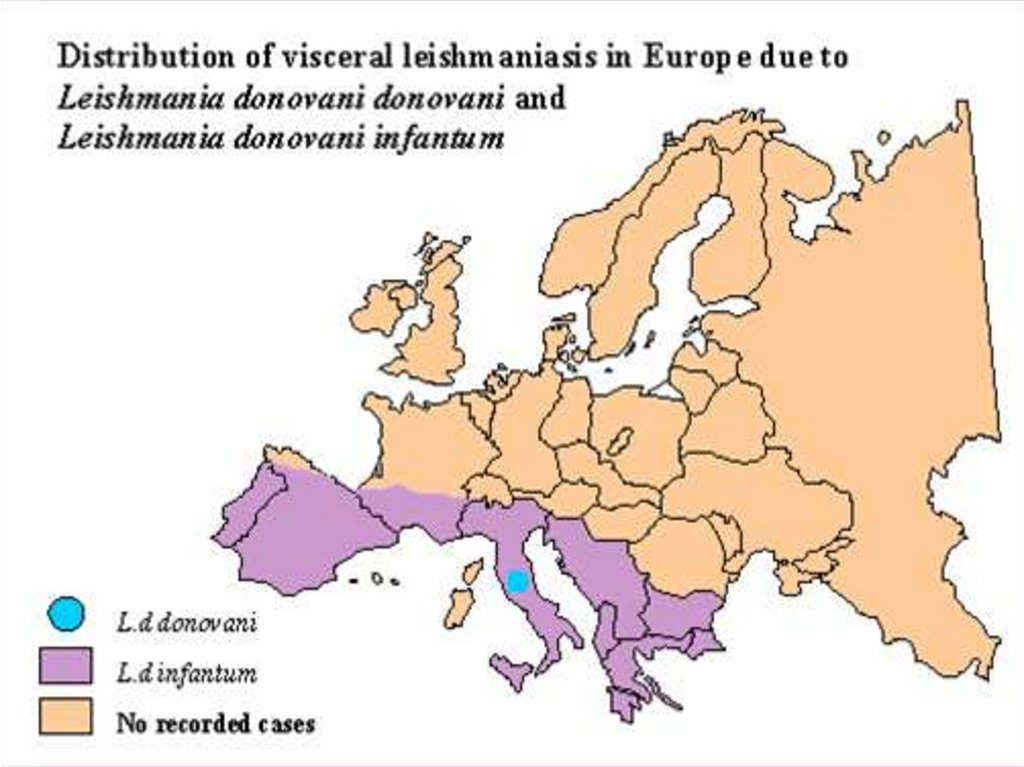
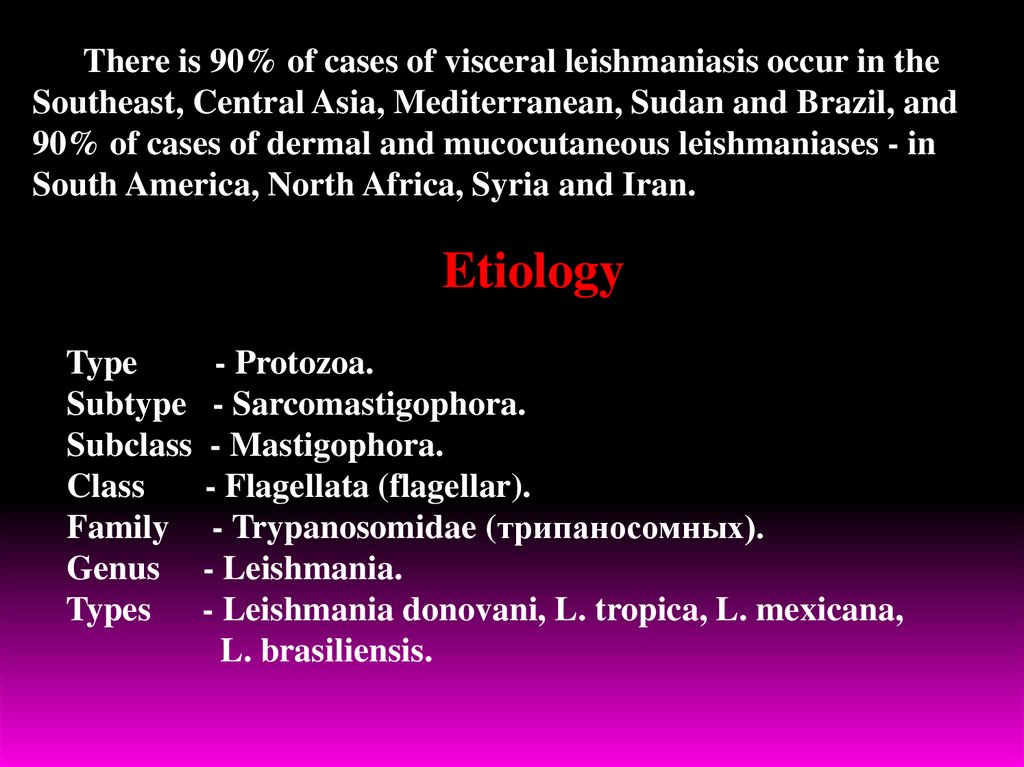
There is 90% of cases of visceral leishmaniasis occur in theSoutheast, Central Asia, Mediterranean, Sudan and Brazil, and
90% of cases of dermal and mucocutaneous leishmaniases - in
South America, North Africa, Syria and Iran.
Etiology
Type
- Protozoa.
Subtype - Sarcomastigophora.
Subclass - Mastigophora.
Class
- Flagellata (flagellar).
Family - Trypanosomidae (трипаносомных).
Genus - Leishmania.
Types
- Leishmania donovani, L. tropica, L. mexicana,
L. brasiliensis.
12.
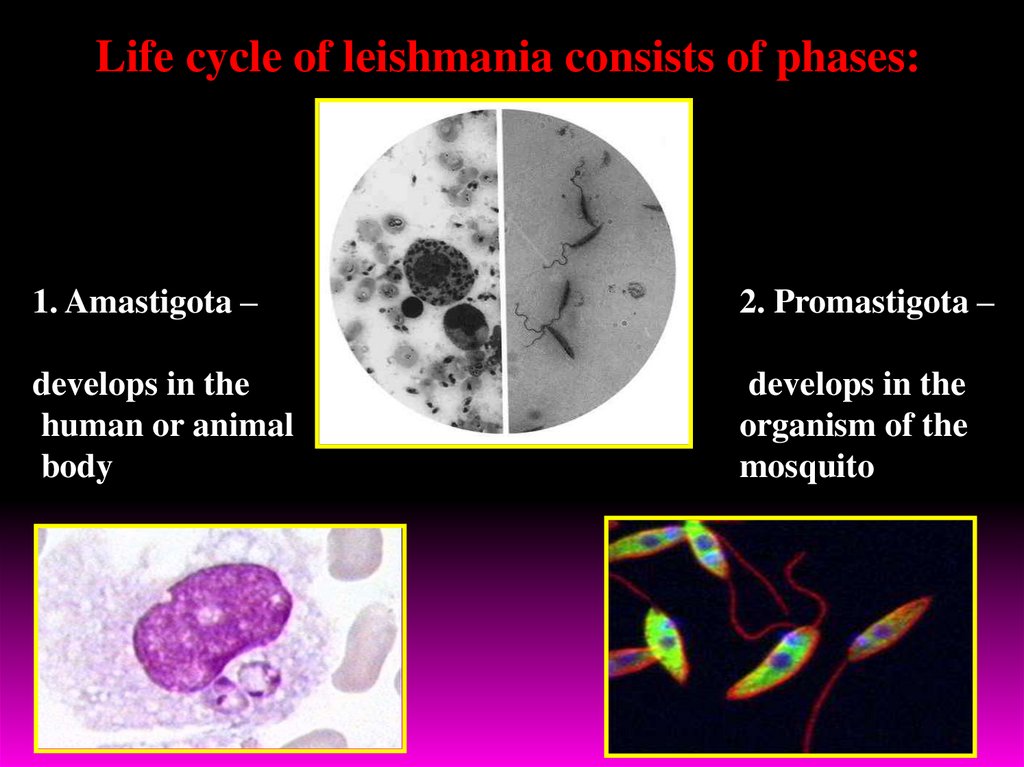
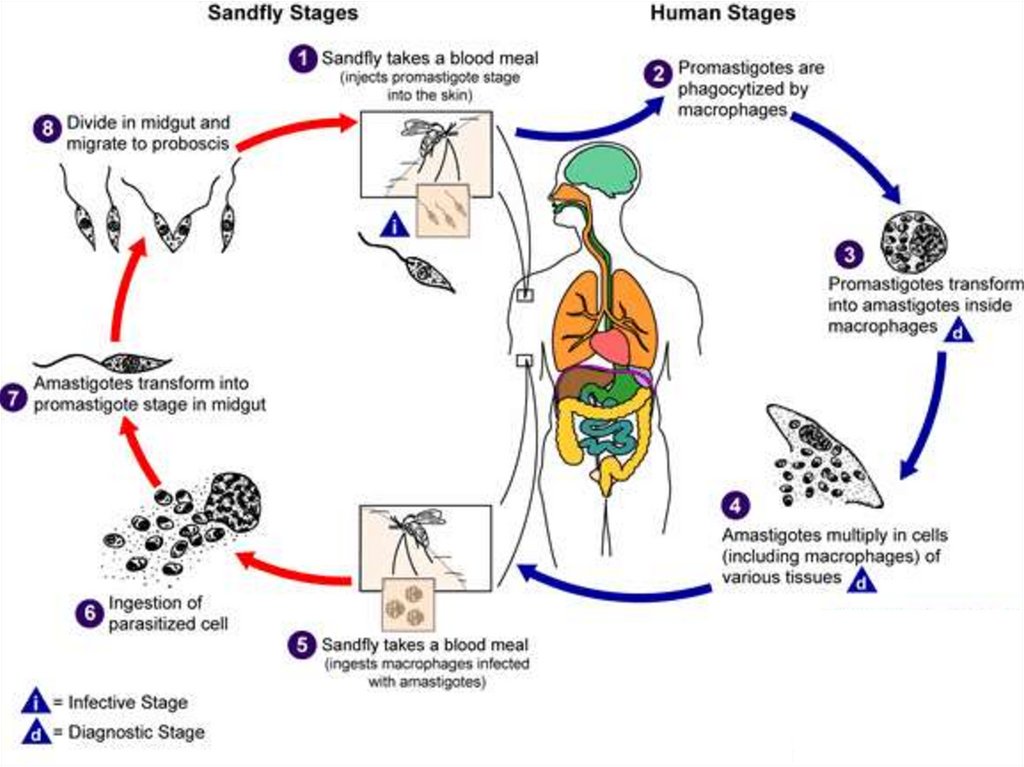
Life cycle of leishmania consists of phases:1. Amastigota –
2. Promastigota –
develops in the
human or animal
body
develops in the
organism of the
mosquito
13.
14.
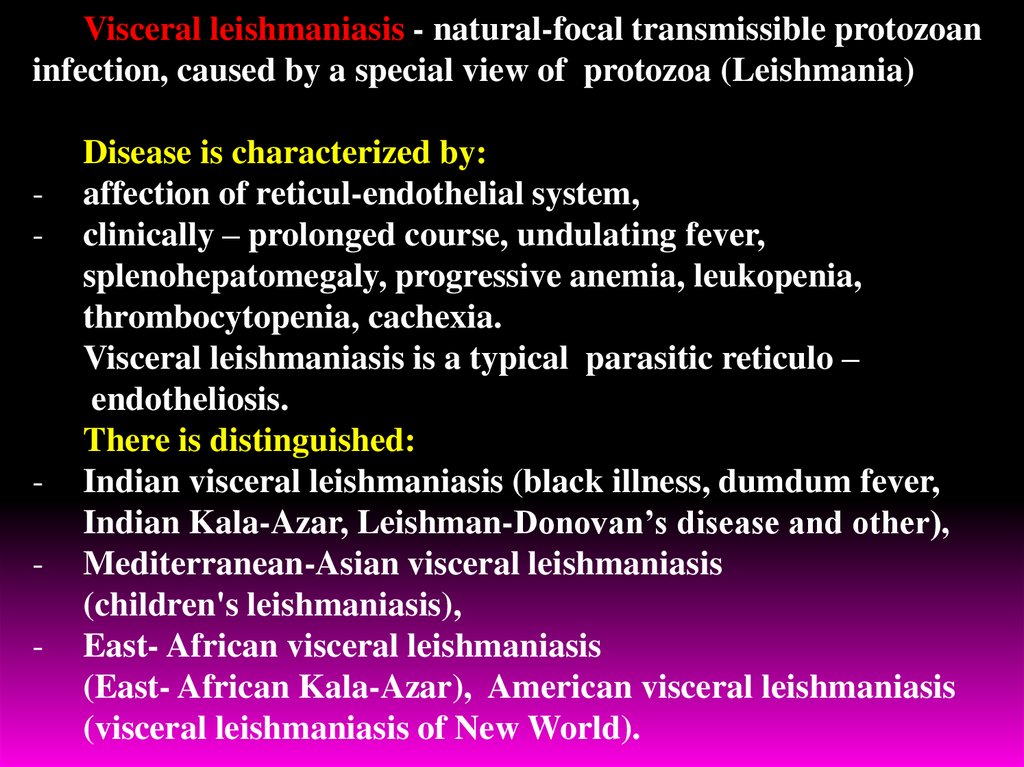
Visceral leishmaniasis - natural-focal transmissible protozoaninfection, caused by a special view of protozoa (Leishmania)
-
-
Disease is characterized by:
affection of reticul-endothelial system,
clinically – prolonged course, undulating fever,
splenohepatomegaly, progressive anemia, leukopenia,
thrombocytopenia, cachexia.
Visceral leishmaniasis is a typical parasitic reticulo –
endotheliosis.
There is distinguished:
Indian visceral leishmaniasis (black illness, dumdum fever,
Indian Kala-Azar, Leishman-Donovan’s disease and other),
Mediterranean-Asian visceral leishmaniasis
(children's leishmaniasis),
East- African visceral leishmaniasis
(East- African Kala-Azar), American visceral leishmaniasis
(visceral leishmaniasis of New World).
15.
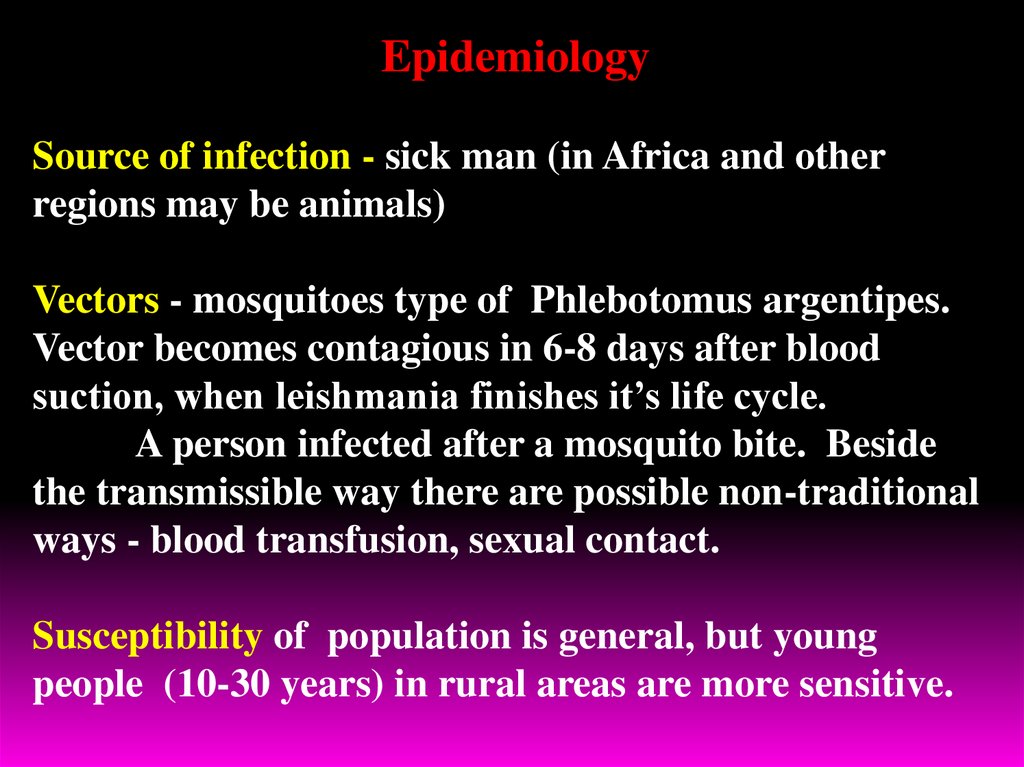
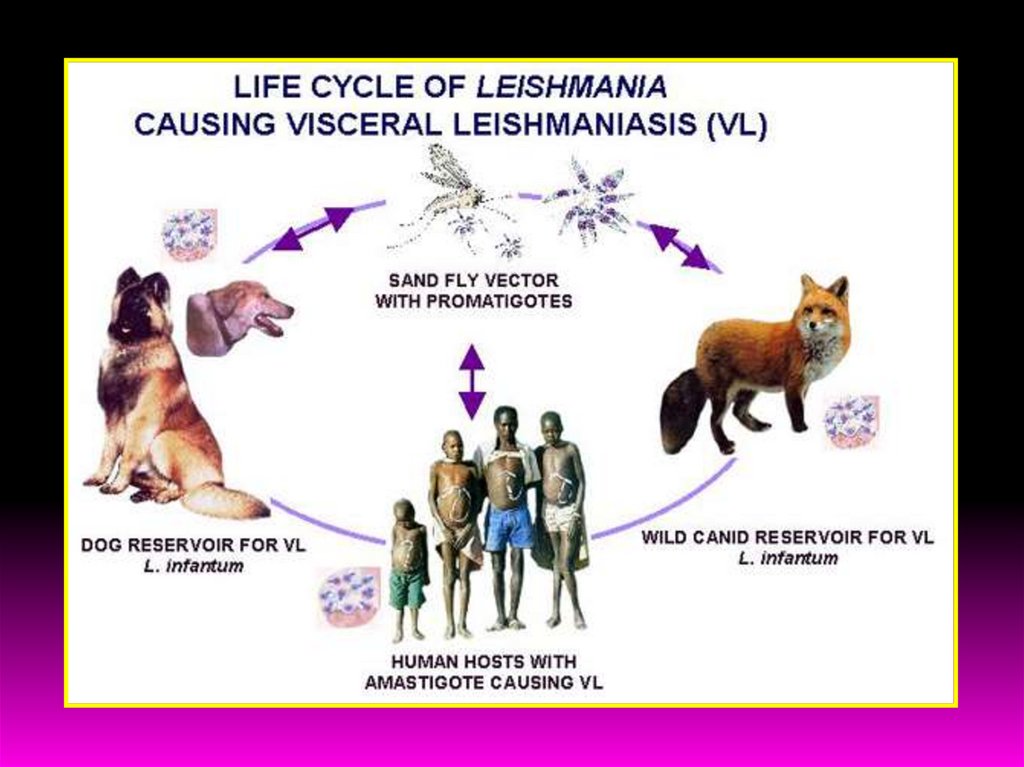
EpidemiologySource of infection - sick man (in Africa and other
regions may be animals)
Vectors - mosquitoes type of Phlebotomus argentipes.
Vector becomes contagious in 6-8 days after blood
suction, when leishmania finishes it’s life cycle.
A person infected after a mosquito bite. Beside
the transmissible way there are possible non-traditional
ways - blood transfusion, sexual contact.
Susceptibility of population is general, but young
people (10-30 years) in rural areas are more sensitive.
16.
17.
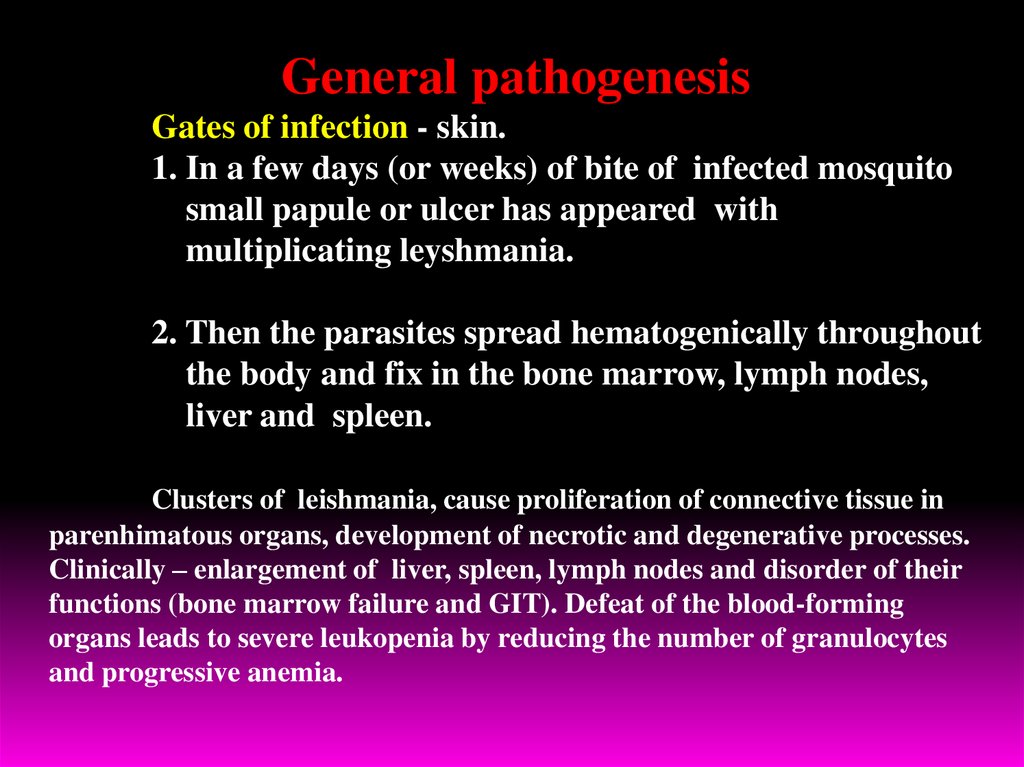
General pathogenesisGates of infection - skin.
1. In a few days (or weeks) of bite of infected mosquito
small papule or ulcer has appeared with
multiplicating leyshmania.
2. Then the parasites spread hematogenically throughout
the body and fix in the bone marrow, lymph nodes,
liver and spleen.
Clusters of leishmania, cause proliferation of connective tissue in
parenhimatous organs, development of necrotic and degenerative processes.
Clinically – enlargement of liver, spleen, lymph nodes and disorder of their
functions (bone marrow failure and GIT). Defeat of the blood-forming
organs leads to severe leukopenia by reducing the number of granulocytes
and progressive anemia.
18.
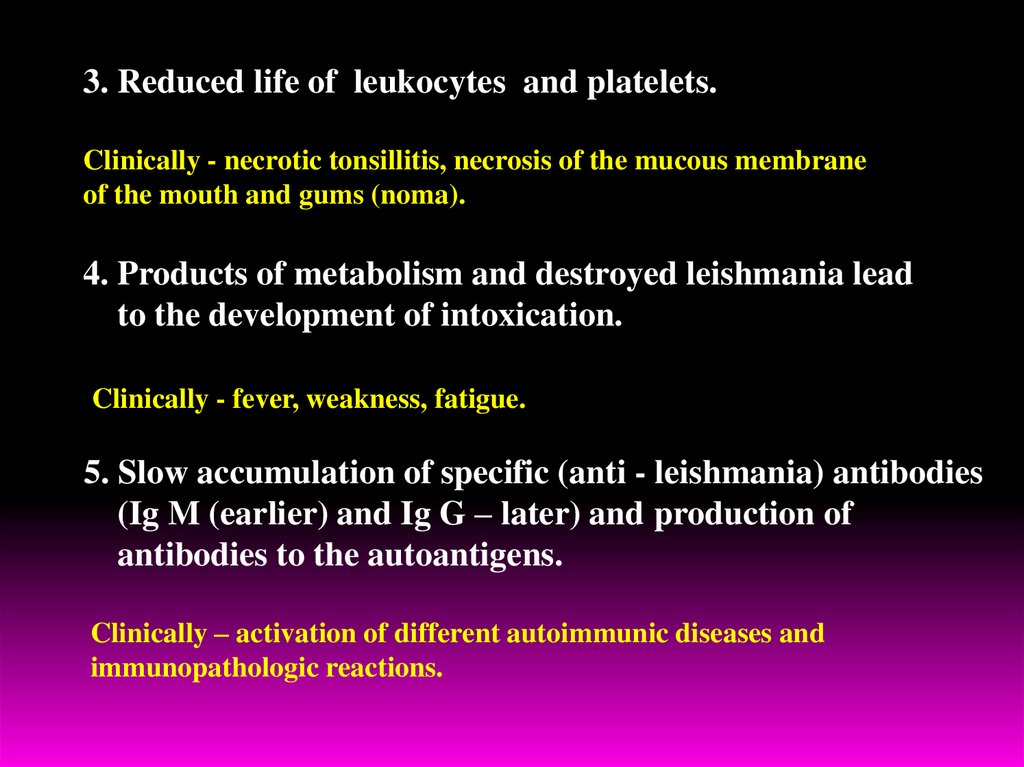
3. Reduced life of leukocytes and platelets.Clinically - necrotic tonsillitis, necrosis of the mucous membrane
of the mouth and gums (noma).
4. Products of metabolism and destroyed leishmania lead
to the development of intoxication.
Clinically - fever, weakness, fatigue.
5. Slow accumulation of specific (anti - leishmania) antibodies
(Ig M (earlier) and Ig G – later) and production of
antibodies to the autoantigens.
Clinically – activation of different autoimmunic diseases and
immunopathologic reactions.
19.
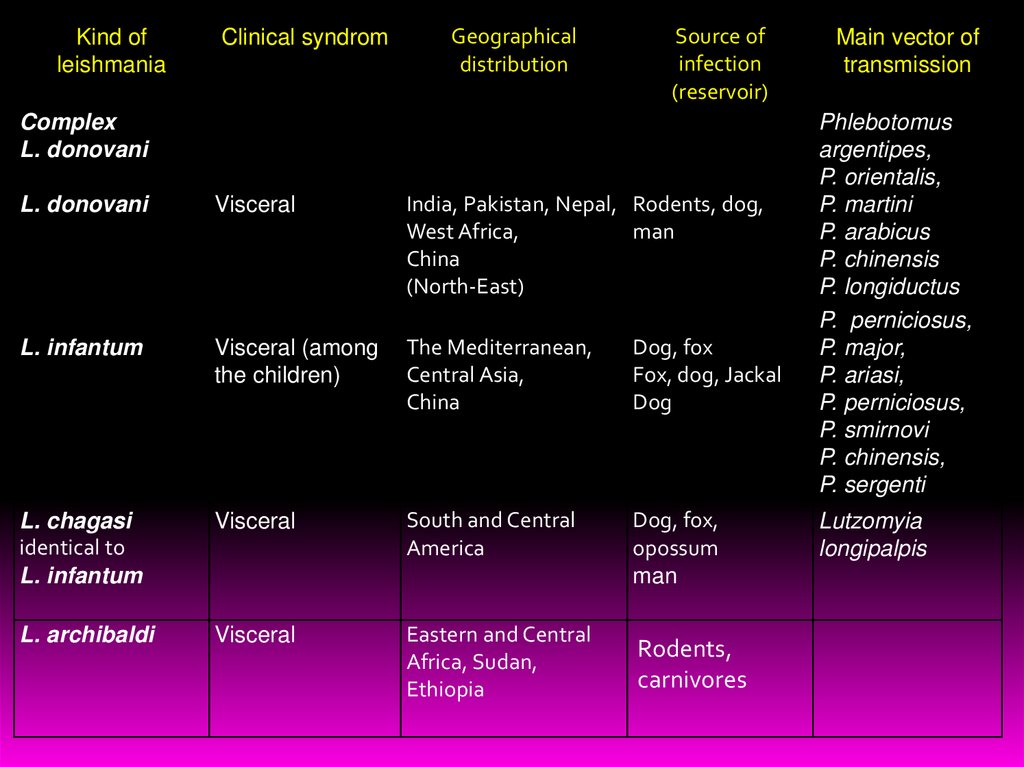
Kind ofleishmania
Clinical syndrom
Geographical
distribution
Source of
infection
(reservoir)
Complex
L. donovani
L. donovani
Visceral
India, Pakistan, Nepal, Rodents, dog,
West Africa,
man
China
(North-East)
L. infantum
Visceral (among
the children)
The Mediterranean,
Central Asia,
China
Dog, fox
Fox, dog, Jackal
Dog
L. chagasi
identical to
L. infantum
Visceral
South and Central
America
Dog, fox,
opossum
man
L. archibaldi
Visceral
Eastern and Central
Africa, Sudan,
Ethiopia
Rodents,
carnivores
Main vector of
transmission
Phlebotomus
argentipes,
P. orientalis,
P. martini
P. arabicus
P. chinensis
P. longiductus
P. perniciosus,
P. major,
P. ariasi,
P. perniciosus,
P. smirnovi
P. chinensis,
P. sergenti
Lutzomyia
longipalpis
20.
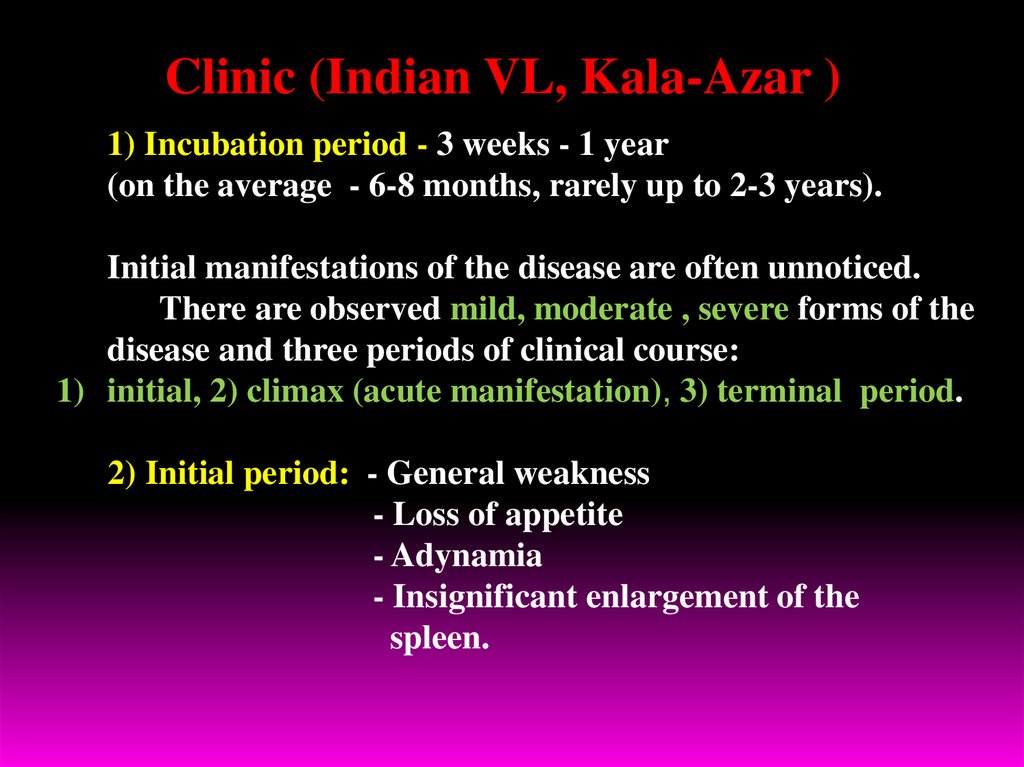
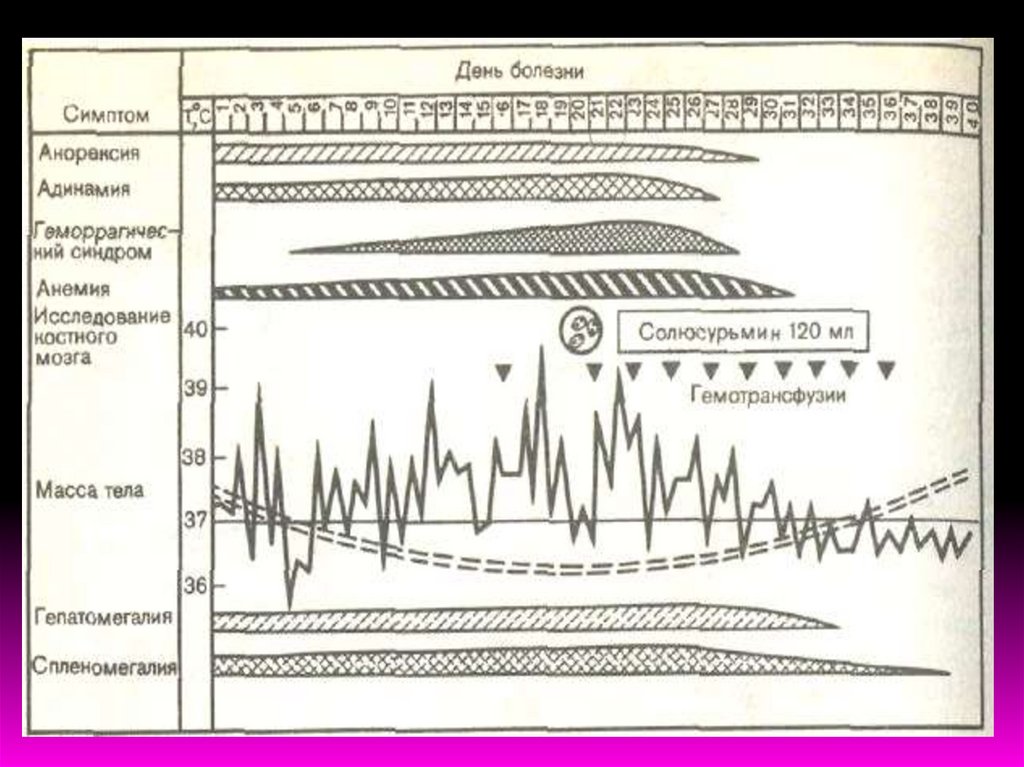
Clinic (Indian VL, Kala-Azar )1) Incubation period - 3 weeks - 1 year
(on the average - 6-8 months, rarely up to 2-3 years).
Initial manifestations of the disease are often unnoticed.
There are observed mild, moderate , severe forms of the
disease and three periods of clinical course:
1) initial, 2) climax (acute manifestation), 3) terminal period.
2) Initial period: - General weakness
- Loss of appetite
- Adynamia
- Insignificant enlargement of the
spleen.
21.
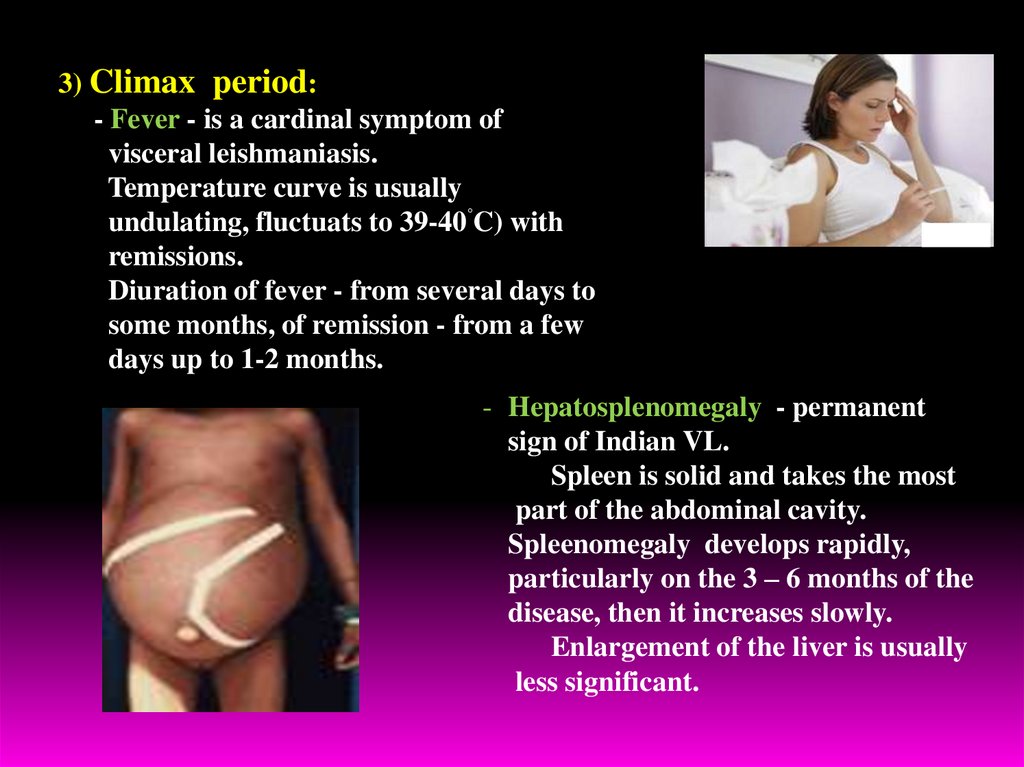
3) Climax period:- Fever - is a cardinal symptom of
visceral leishmaniasis.
Temperature curve is usually
undulating, fluctuats to 39-40˚C) with
remissions.
Diuration of fever - from several days to
some months, of remission - from a few
days up to 1-2 months.
- Hepatosplenomegaly - permanent
sign of Indian VL.
Spleen is solid and takes the most
part of the abdominal cavity.
Spleenomegaly develops rapidly,
particularly on the 3 – 6 months of the
disease, then it increases slowly.
Enlargement of the liver is usually
less significant.
22.
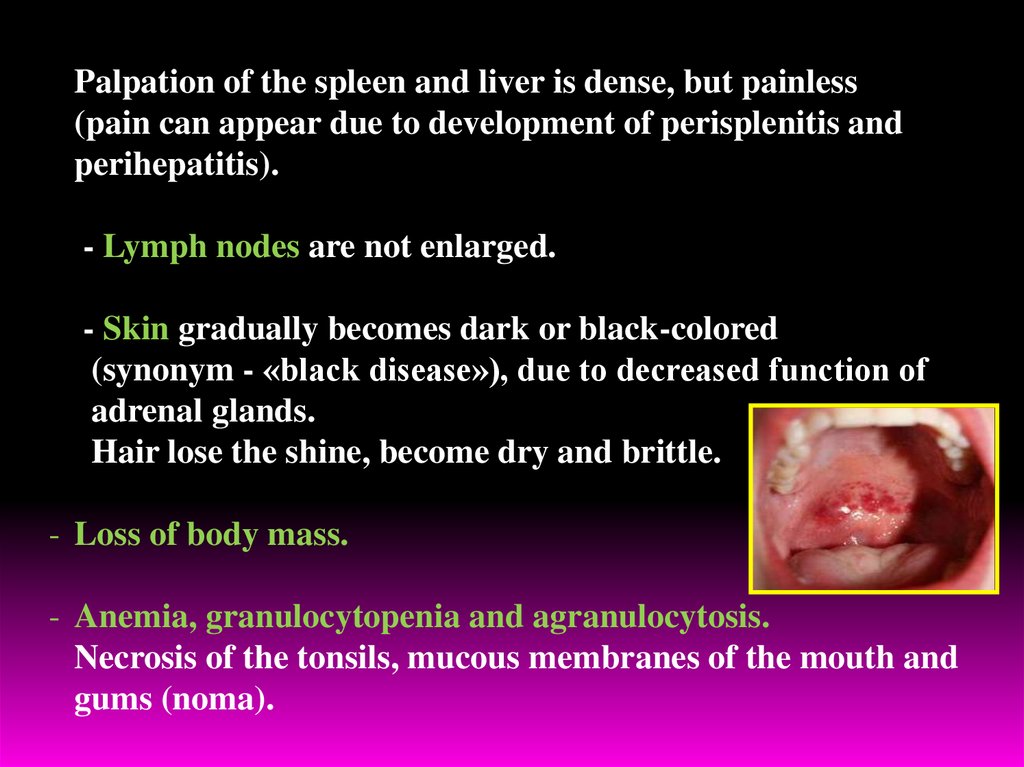
Palpation of the spleen and liver is dense, but painless(pain can appear due to development of perisplenitis and
perihepatitis).
- Lymph nodes are not enlarged.
- Skin gradually becomes dark or black-colored
(synonym - «black disease»), due to decreased function of
adrenal glands.
Hair lose the shine, become dry and brittle.
- Loss of body mass.
- Anemia, granulocytopenia and agranulocytosis.
Necrosis of the tonsils, mucous membranes of the mouth and
gums (noma).
23.
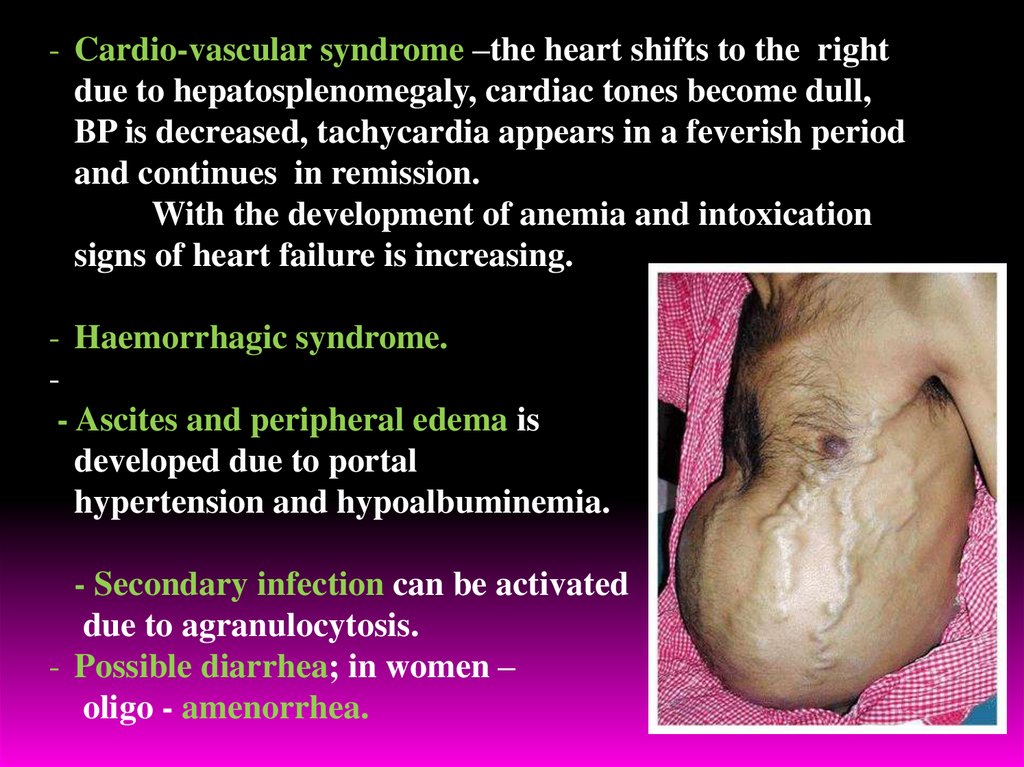
- Cardio-vascular syndrome –the heart shifts to the rightdue to hepatosplenomegaly, cardiac tones become dull,
BP is decreased, tachycardia appears in a feverish period
and continues in remission.
With the development of anemia and intoxication
signs of heart failure is increasing.
- Haemorrhagic syndrome.
- Ascites and peripheral edema is
developed due to portal
hypertension and hypoalbuminemia.
- Secondary infection can be activated
due to agranulocytosis.
- Possible diarrhea; in women –
oligo - amenorrhea.
24.
4) Terminal period:- cachexia
- sharp hypotonia of muscles
- skin is thin, through the abdominal wall can see the
border of enlarged spleen and liver.
Prognosis of mild forms of VL is favorable, but in severe
and complicated forms – serious.
In HIV-patients VL has malignant character and is
accompanied by resistance to specific therapy.
25.
In CBC: anemia (Hb – up to 40—50 g/l),leukopenia to 2—2,5х109/l and less, neutropenia
at relative lymphocytosis.
Uneosinophilia – constant sign.
Coagulation of blood and erythrocyte resistance is decreased,
ESR sharply increased (till 90 mm/h).
5-10% of patients have skin leishmanoid, wich develops
in 1-2 years of effective treatment and consist of macula,
nodulus papilloma. Leishmania contained in leishmanoid
can survive many years.
Thus, a patient with skin leishmanoid – reservoir of the agent
and the source of invasion of mosquitoes for many years.
26.
27.
Mediterranean Kala – Azar- Most cases of co-infection are registered among men,
aged 20-40 years.
- 25-75% of HIV-infected and 1,5-9% of AIDS-patients
suffers from visceral leishmaniasis. That why VL in
HIV-infected - the most frequent cause of opportunistic
infections.
- Hematogenic (syringe) way is easier realized due to high
concentration of leyshmania in the blood of HIV-patients
28.
The most significant features of Mediterranean-Asianvisceral leishmaniasis are:
1) incubation period - within 1 month to 1 year (on an average 3-5 months);
2) skin leishmanoid is absent;
3) involvment in pathological process peripheral and visceral lymph nodes
with the development of mesadenitis;
4) frequent development of hemorrhages and bacterial pneumonia;
5) hyperpigmentation of skin is absent , skin is pale, grey-colored;
6) primary affect as papules, sometimes covered with scale before the
manifestation of the disease;
7) the disease may occur in acute, subacute and chronic forms.
29.
30.
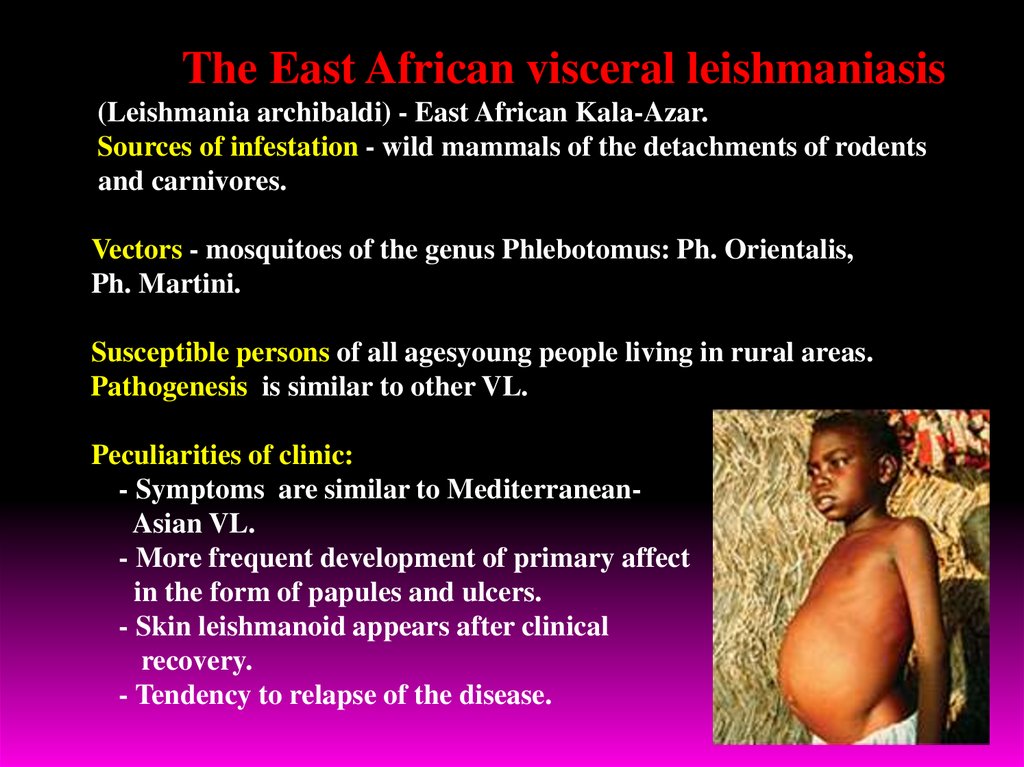
The East African visceral leishmaniasis(Leishmania archibaldi) - East African Kala-Azar.
Sources of infestation - wild mammals of the detachments of rodents
and carnivores.
Vectors - mosquitoes of the genus Phlebotomus: Ph. Orientalis,
Ph. Martini.
Susceptible persons of all agesyoung people living in rural areas.
Pathogenesis is similar to other VL.
Peculiarities of clinic:
- Symptoms are similar to MediterraneanAsian VL.
- More frequent development of primary affect
in the form of papules and ulcers.
- Skin leishmanoid appears after clinical
recovery.
- Tendency to relapse of the disease.
31.
Visceral leishmaniasis of New WorldAmerican (South American) visceral leishmaniasis (Leishmania chagasi,
identical L. infantum)
1) Epidemiology is similar to the VL of Old World, called by Leishmania
infantum. The causative agent of American visceral leishmaniasis has
tropisity to the canids. Is registered in the Central, South America, Mexico.
2) Vector - mosquito Lutzomyia longipalpis, which
actively attacking dogs than people.
3) Pathogenesis, clinical symptoms, complications,
diagnostics, treatment are the similar to other forms
of visceral leishmaniasis.
4) Prognosis in symptomatic cases is serious.
5) There is large number of asymptomatic disease
with praesence of leishmania in the skin.
6) Prevention is the same, includes active detection
and treatment of patients, the destruction of sick dogs, fight against
mosquitoes
32.
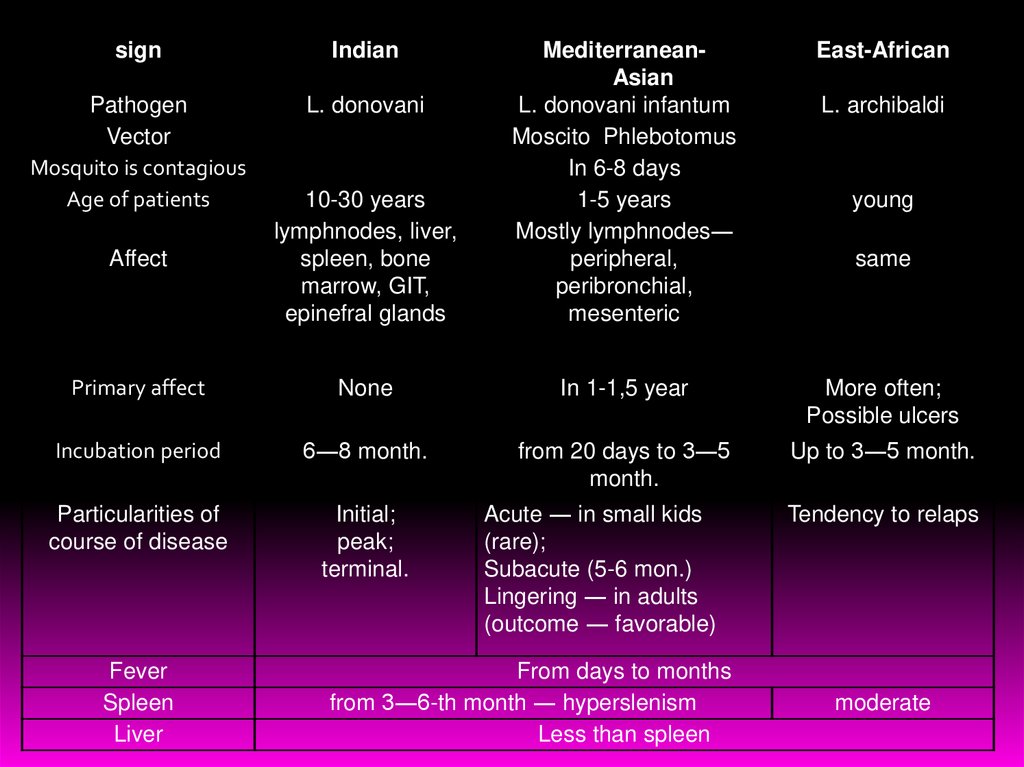
signIndian
East-African
Affect
10-30 years
lymphnodes, liver,
spleen, bone
marrow, GIT,
epinefral glands
MediterraneanAsian
L. donovani infantum
Moscito Phlebotomus
In 6-8 days
1-5 years
Mostly lymphnodes―
peripheral,
peribronchial,
mesenteric
Pathogen
Vector
Mosquito is contagious
Age of patients
L. donovani
Primary affect
None
In 1-1,5 year
More often;
Possible ulcers
Incubation period
6―8 month.
from 20 days to 3―5
month.
Up to 3―5 month.
Particularities of
course of disease
Initial;
peak;
terminal.
Fever
Spleen
Liver
Acute ― in small kids
(rare);
Subacute (5-6 mon.)
Lingering ― in adults
(outcome ― favorable)
From days to months
from 3―6-th month ― hyperslenism
Less than spleen
L. archibaldi
young
same
Tendency to relaps
moderate
33.
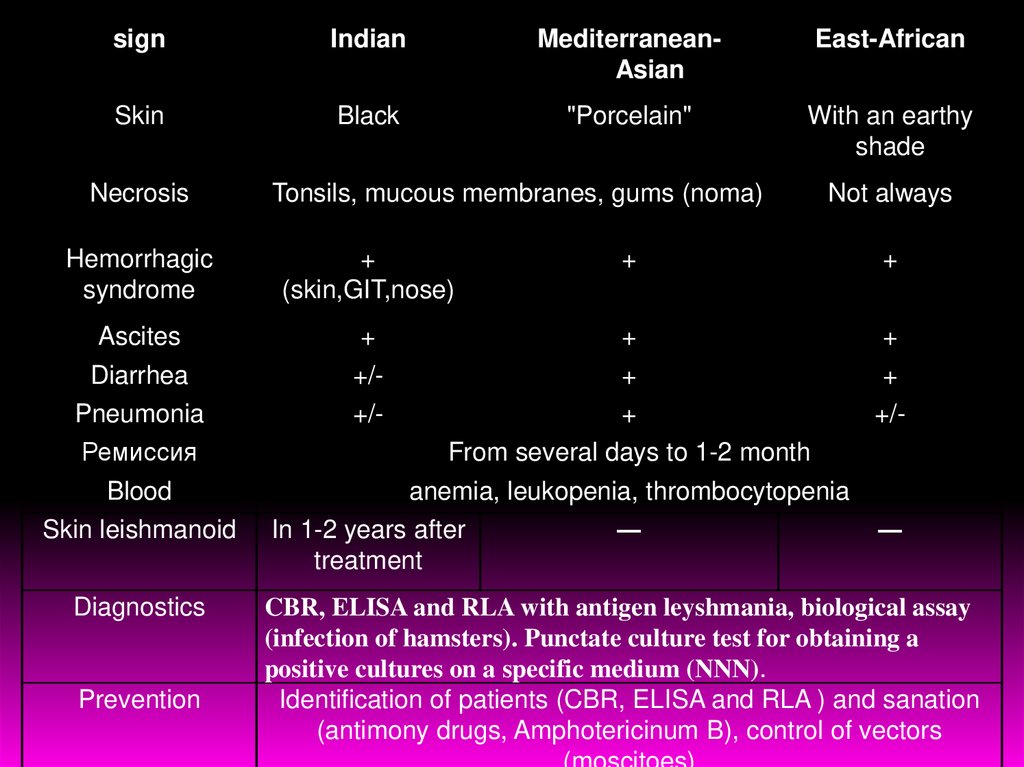
signIndian
MediterraneanAsian
East-African
Skin
Black
"Porcelain"
With an earthy
shade
Necrosis
Tonsils, mucous membranes, gums (noma)
Not always
Hemorrhagic
syndrome
+
(skin,GIT,nose)
+
+
Ascites
+
+
+
Diarrhea
+/-
+
+
Pneumonia
+/-
+
+/-
Ремиссия
From several days to 1-2 month
Blood
anemia, leukopenia, thrombocytopenia
Skin leishmanoid
Diagnostics
Prevention
In 1-2 years after
treatment
―
―
CBR, ELISA and RLA with antigen leyshmania, biological assay
(infection of hamsters). Punctate culture test for obtaining a
positive cultures on a specific medium (NNN).
Identification of patients (CBR, ELISA and RLA ) and sanation
(antimony drugs, Amphotericinum B), control of vectors
34.
Diagnostics1) Parasitological method: revealing of leishmania in the blood
smear and thick drop).
2) Biopsy (puncture) of bone marrow where leishmania easily
detectable. Sometimes trepanobiopsy of iliac bone or biopsy
of the lymph nodes, rarely – of spleen and liver can give
positive result.
3) Punctate culture test for obtaining a positive cultures on a
specific medium (NNN).
4) Serological investigation: CBR, ELISA and RLA with
antigen leyshmania, biological assay (infection of hamsters).
5) PCR and express method (immunochromatographic) –
detection of recombinant clone – antigen К39.
35.
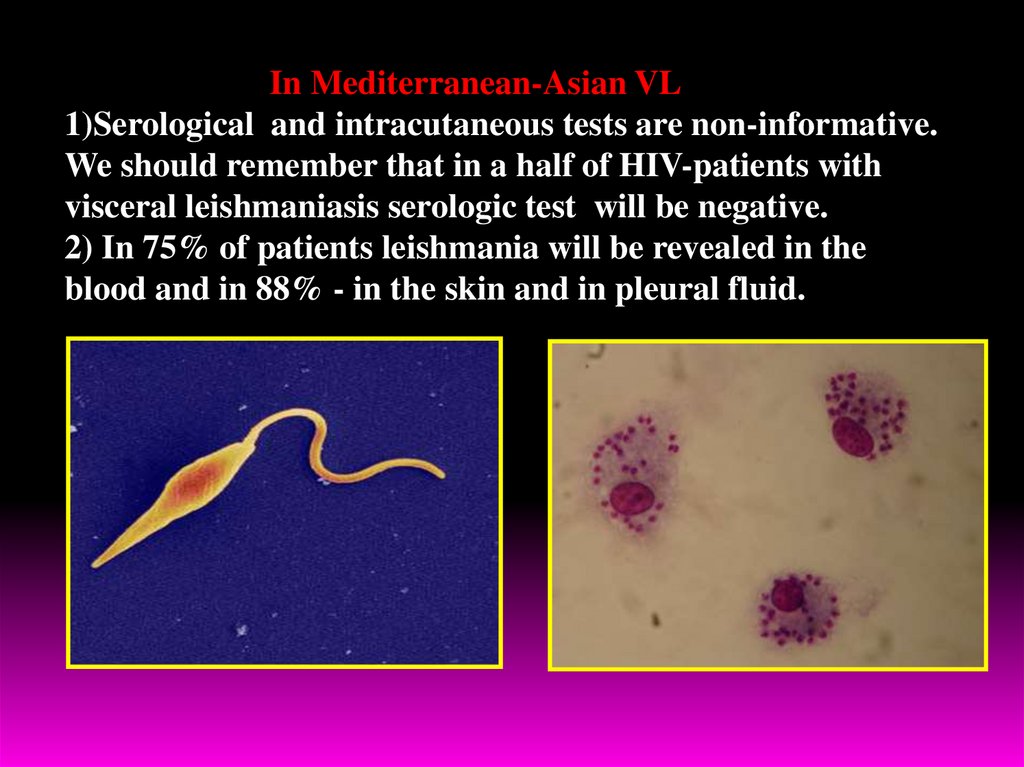
In Mediterranean-Asian VL1)Serological and intracutaneous tests are non-informative.
We should remember that in a half of HIV-patients with
visceral leishmaniasis serologic test will be negative.
2) In 75% of patients leishmania will be revealed in the
blood and in 88% - in the skin and in pleural fluid.
36.
TreatmentFor the treatment of visceral leishmaniasis,
used drugs of 5-valent antimony:
1. Solusurmine
2. Pentostame – sodium stibogluconatis
3.Glucantime - synonyms: Meglumini stibias
Contraindications: pneumonic tuberculosis, severe violations of the liver
and kidney function.
Side-reactions: fever, cough, vomiting, polyneuritis, myocarditis.
Intradaction: Intramuscularly deeply.
Daily dose - 0,06 g/kg of body mass.
On the first day ¼ of necessary dose, on the second – a half of necessary
dose, on the 3rd day - ¾ of daily dose, 4-day - full dose.
The course of treatment is 10-15 injection.
Repeat a course through the 4-6 weeks.
At non effective therapy with antimony drugs appoint Amphotericin B and
paromicyne!
Aminozidine can be administered simultaneously with drugs 5-valent
antimony in two syringes in different places.
37.
For the treatment of VL also can be applied:-
Pentamidine - 4 mg/kg/day – during 11 weeks
Amphotericin B, full dose for a course –
20-30 mg/kg – during 10-20 days.
In addition to specific treatment, is necessary
pathogenic therapy and prevention of secondary
bacterial infection.
It is necessary to widely use restorative therapy, drugs iron and phosphorus
(per os), vitamin B12, diet, rich in animal proteins and vitamins.
- Treatment of post-Kala-Azar skin leishmanoid is the same as visceral
leishmaniasis, but the course of treatment continuances to 4 months.
The first oral medication for the treatment of VL – miltefosine had been
registered in India.
It is suggested that miltefosine will replace drugs of 5-valent antimony
and amphotericin as the drugs of first line.
38.
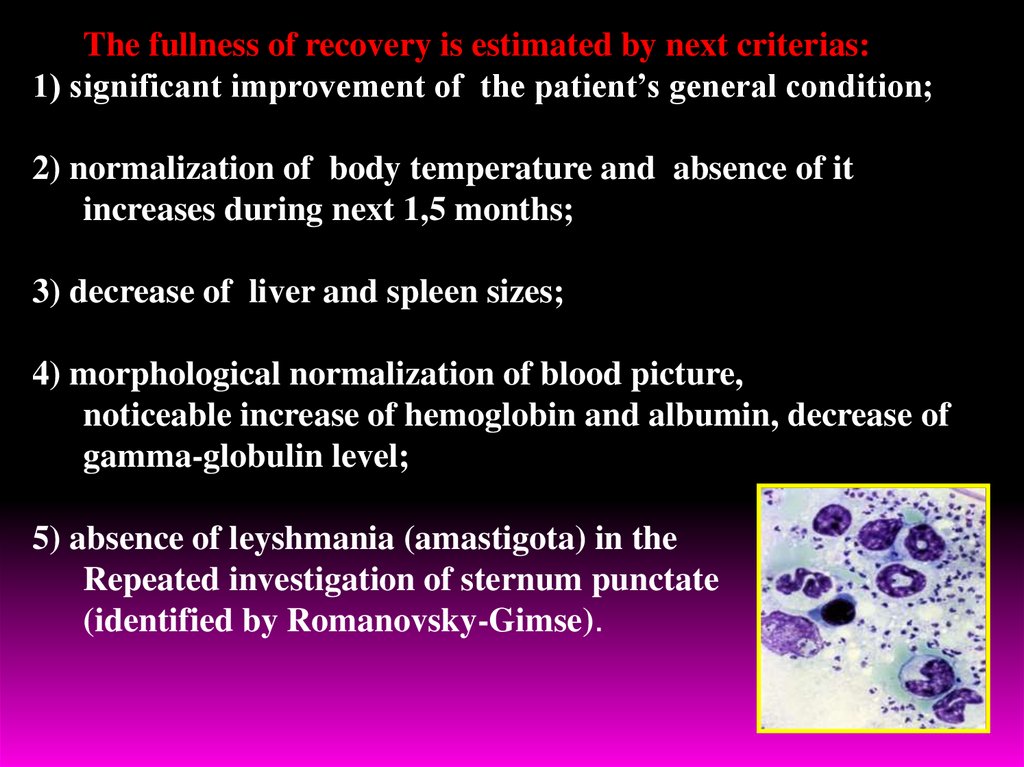
The fullness of recovery is estimated by next criterias:1) significant improvement of the patient’s general condition;
2) normalization of body temperature and absence of it
increases during next 1,5 months;
3) decrease of liver and spleen sizes;
4) morphological normalization of blood picture,
noticeable increase of hemoglobin and albumin, decrease of
gamma-globulin level;
5) absence of leyshmania (amastigota) in the
Repeated investigation of sternum punctate
(identified by Romanovsky-Gimse).





 medicine
medicine