Similar presentations:
Antifungal agents are used for superficial and deep (systemic) fungal infections
1. Antifungal agents are used for superficial and deep (systemic) fungal infections.
2.
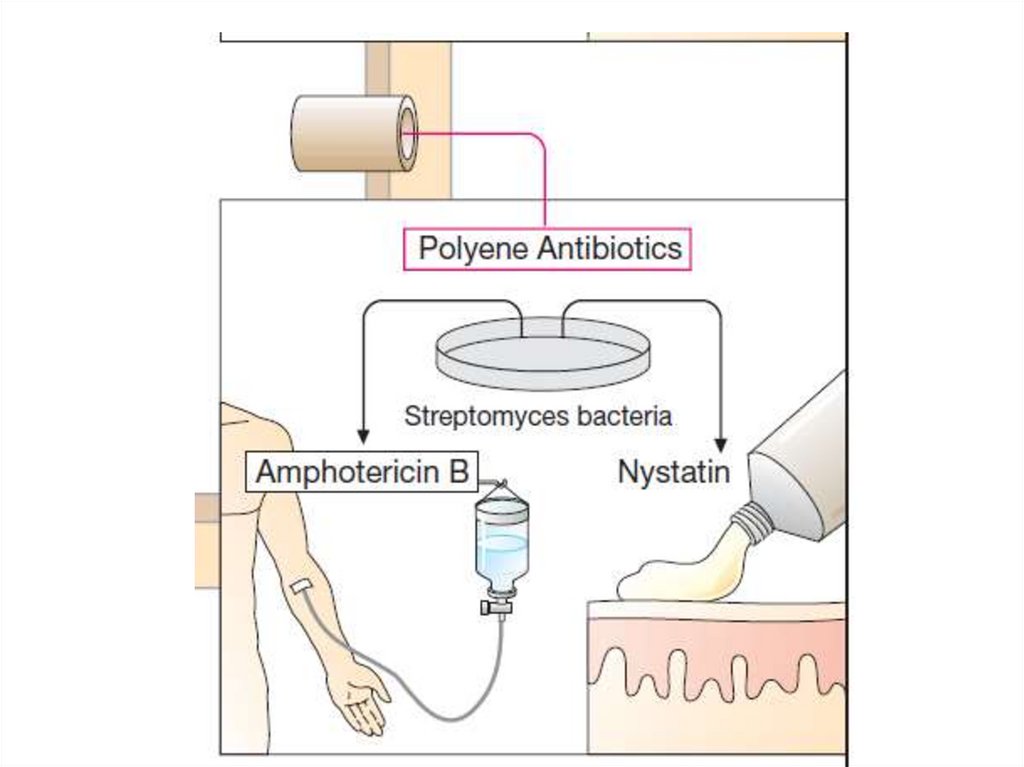
Antibiotics• Polyenes: Amphotericin B (AMB), Nystatin,
Hamycin
• Echinocandins: Caspofungin, Micafungin
• Heterocyclic benzofuran: Griseofulvin
Synthetic drugs:
Antimetabolite - Flucytosine (5-FC)
Azoles:
• Imidazoles
1.Topical: Clotrimazole, Miconazole, Oxiconazole
2.Systemic: Ketoconazole
• Triazoles: Fluconazole (systemic), Intraconazole
Allylamine - Terbinafine
3.
4.
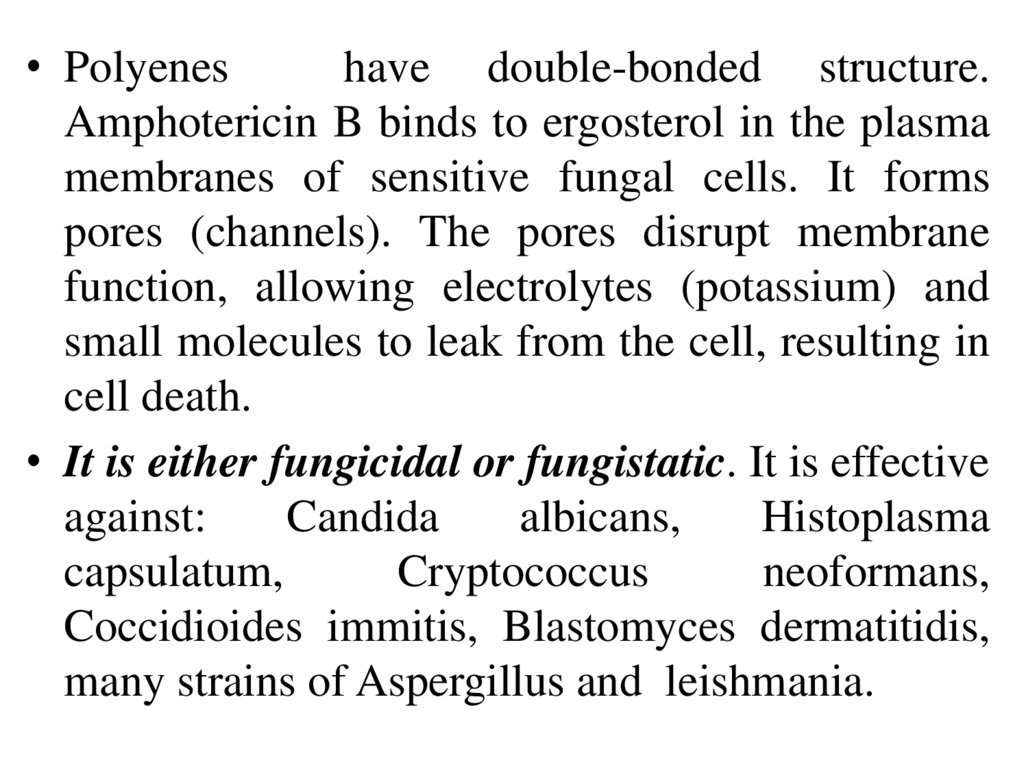
• Polyeneshave double-bonded structure.
Amphotericin B binds to ergosterol in the plasma
membranes of sensitive fungal cells. It forms
pores (channels). The pores disrupt membrane
function, allowing electrolytes (potassium) and
small molecules to leak from the cell, resulting in
cell death.
• It is either fungicidal or fungistatic. It is effective
against:
Candida
albicans,
Histoplasma
capsulatum,
Cryptococcus
neoformans,
Coccidioides immitis, Blastomyces dermatitidis,
many strains of Aspergillus and leishmania.
5.
6.
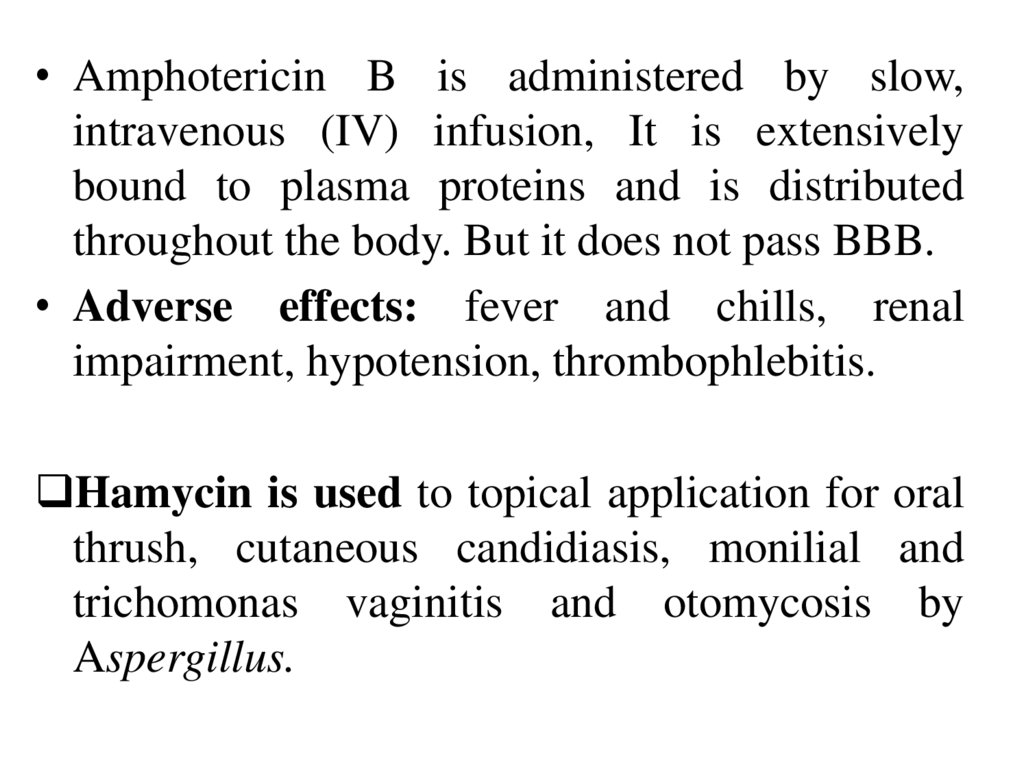
• Amphotericin B is administered by slow,intravenous (IV) infusion, It is extensively
bound to plasma proteins and is distributed
throughout the body. But it does not pass BBB.
• Adverse effects: fever and chills, renal
impairment, hypotension, thrombophlebitis.
Hamycin is used to topical application for oral
thrush, cutaneous candidiasis, monilial and
trichomonas vaginitis and otomycosis by
Aspergillus.
7.
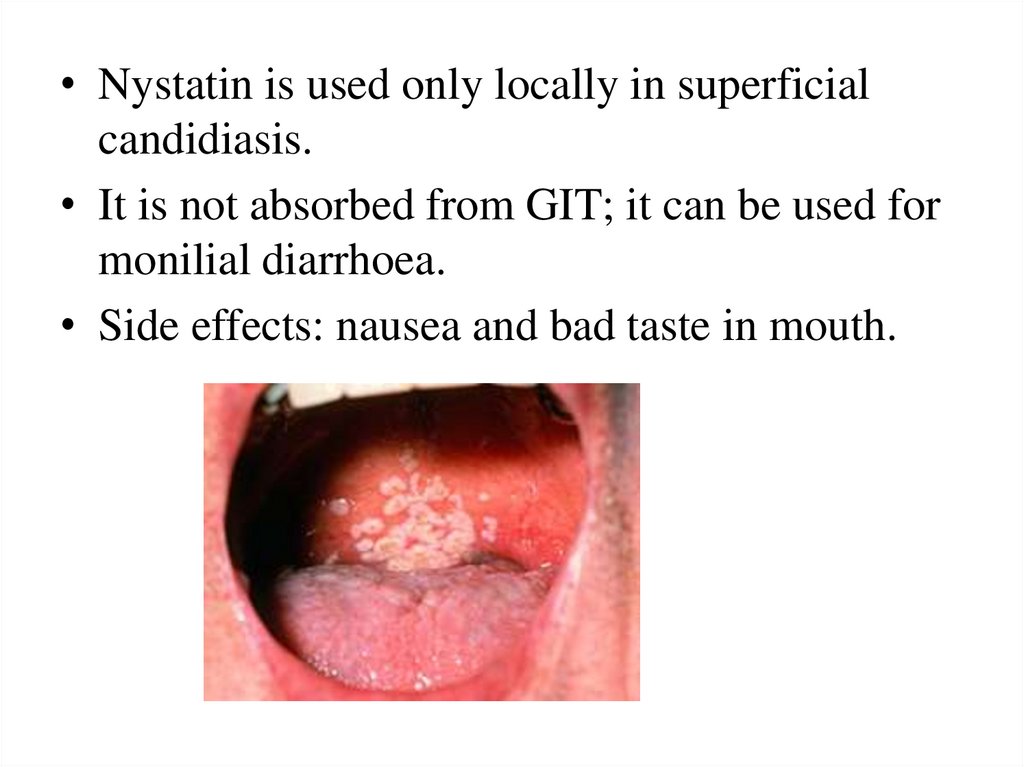
• Nystatin is used only locally in superficialcandidiasis.
• It is not absorbed from GIT; it can be used for
monilial diarrhoea.
• Side effects: nausea and bad taste in mouth.
8.
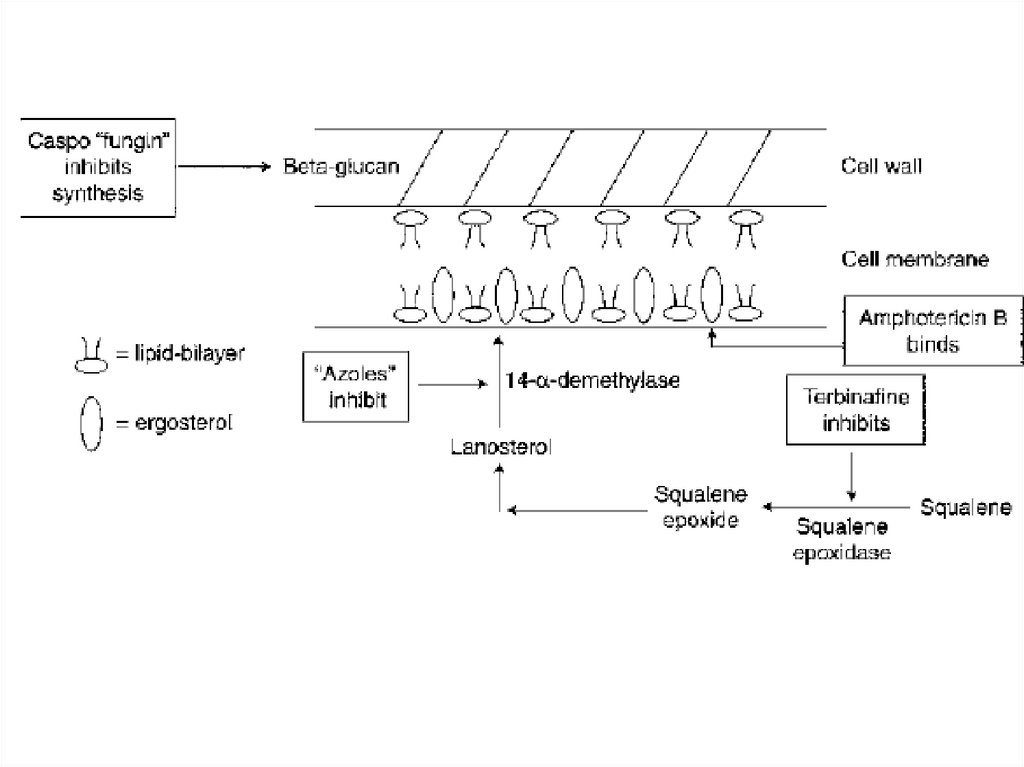
Caspofungin inhibits the synthesis of β-1,3-glucan (a unique component of the fungal
cell wall. It is active mainly against Candida
and Aspergillus.
Uses: deep and invasive candidiasis, invasive
aspergillosis.
It is infused i.v., distributed into tissues, but
does not enter CSF.
Adverse effects: rash, vomiting, dyspnoea,
hypokalemia and joint pain, acute febrile
reaction.
9.
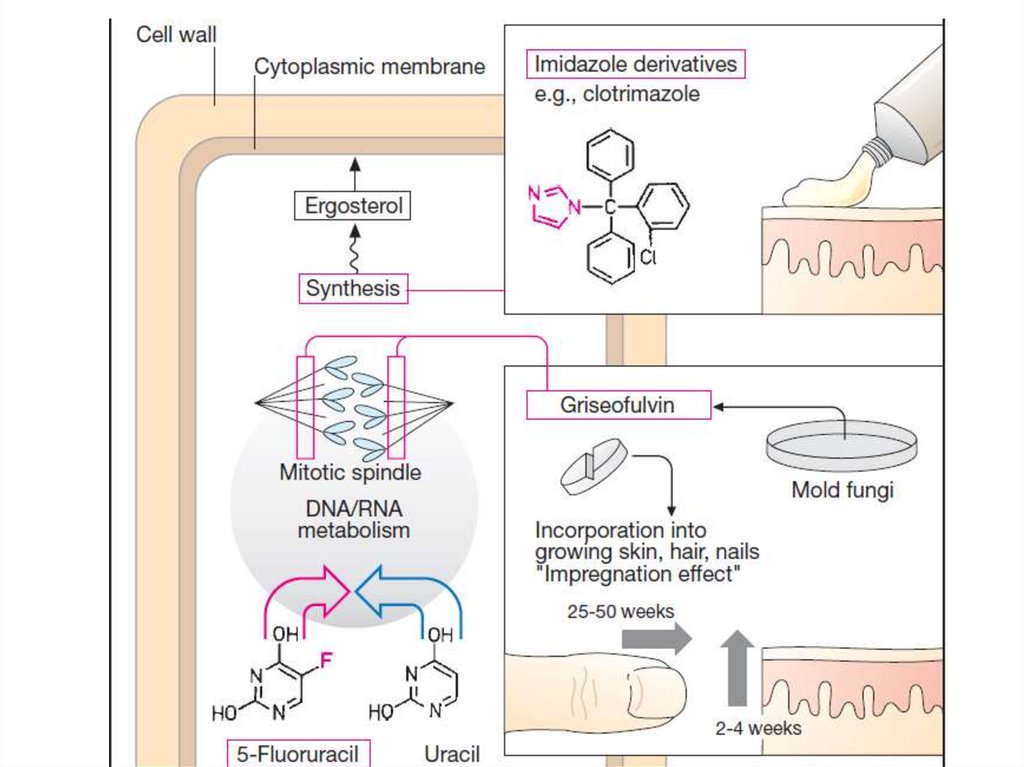
• Azoles are predominantly fungistatic, but maybe fungicidal.
• Mechanism of action: They inhibit C-14 αdemethylase,
block the demethylation of
lanosterol to ergosterol, the principal sterol of
fungal membranes.
• The inhibition of ergosterol biosynthesis disrupts
membrane structure and function, inhibits fungal
cell growth.
• They have broad-spectrum antifungal activity
covering dermatophytes, Candida, other fungi
involved in deep mycosis, Nocardia and
Leishmania
10.
• Clotrimazole is effective in the topicaltreatment. Uses: tinea infections, ringworm,
Athletes’ foot, otomycosis, oropharyngeal
candidiasis, vaginal candidiasis.
• Adverse effects: local irritation with stinging.
Ketoconazole is the broad-spectrum antifungal
drug, useful in both dermatophytosis and deep
mycosis.
Adverse effects: nausea and vomiting; loss of
appetite, headache, paresthesia, rashes and hair
loss.
11.
• Fluconazole is well absorbed after oraladministration and distributes widely to body fluids
and tissues. The majority of the drug is excreted
unchanged via the urine. It is used orally, IV .
• It is highly active against Cryptococcus neoformans
and certain species of Candida, including C.
albicans
• Uses: deep fungal infections (including meningitis),
ringworm, mucocutaneous candidiasis (the oral
cavity, gastrointestinal tract, vagina).
• Side effects: dyspepsia, liver dysfunction, skin rash.
12.
• Griseofulvinis
fungistatic
for
most
dermatophytes, including Epidermophyton,
Trichophyton, Microsporum.
• Griseofulvin interferes with microtubule
function in dermatophytes and may also inhibit
the synthesis and polymerization of nucleic
acids.
• Griseofulvin is fungistatic.
• The oral formulation of the drug is indicated for
dermatophytoses of the skin and hair.
• Adverse effects: headaches, mental confusion,
gastrointestinal irritation, photosensitivity and
changes in liver function.
13.
14.
• Terbinafine inhibits a fungal enzyme squaleneepoxidase. It causes accumulation of toxic
levels of squalene, which can interfere with
ergosterol synthesis.
• Terbinafine is fungicidal.
• Terbinafine is available in both oral and topical
forms. It accumulates in keratin, but it is much
more effective than griseofulvin in
onychomycosis.
• Adverse effects include gastrointestinal upsets,
rash, headache, and taste disturbances.
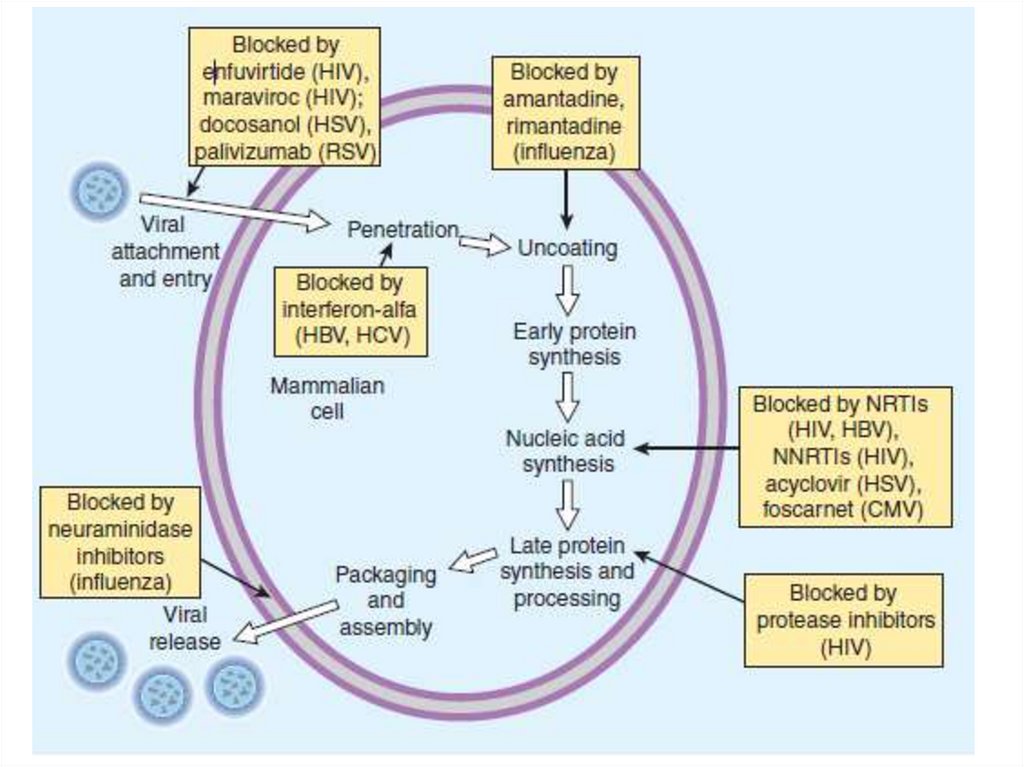
15. Antiviral Chemotherapy Prophylaxis
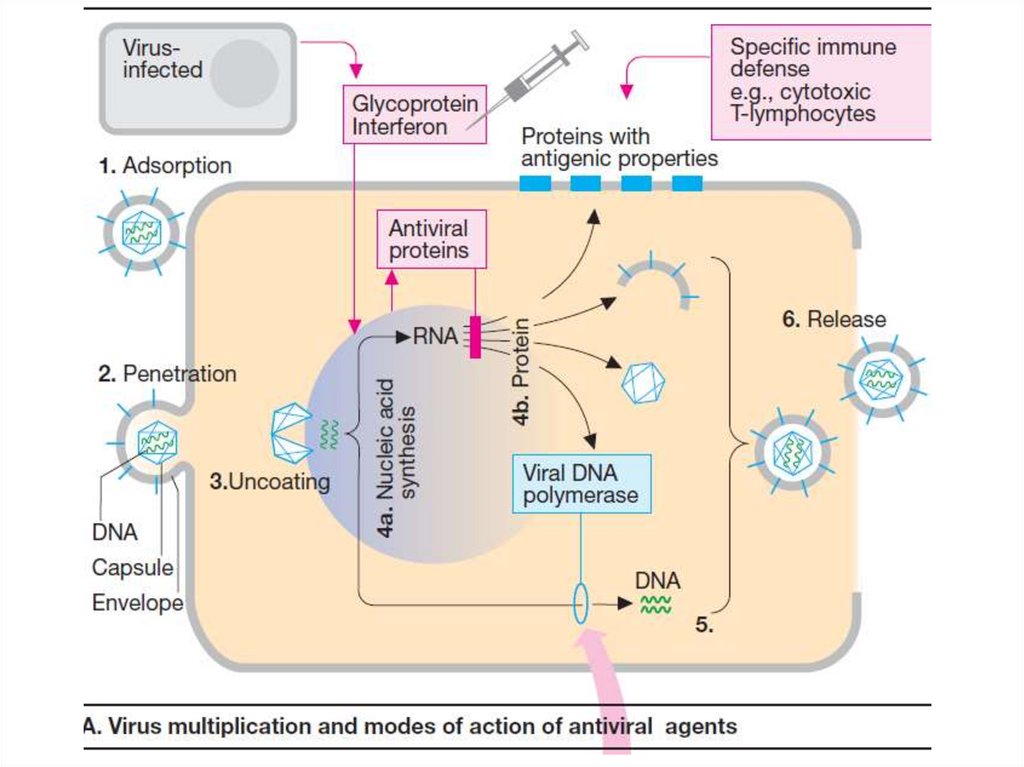
• As obligate intracellular parasites, thereplication of viruses depends on synthetic
processes of the host cell.
• Antiviral drugs can exert their actions at
several stages of viral replication including
viral entry, nucleic acid synthesis, late protein
synthesis and processing, and in the final
stages of viral packaging and virion release.
16.
17.
18.
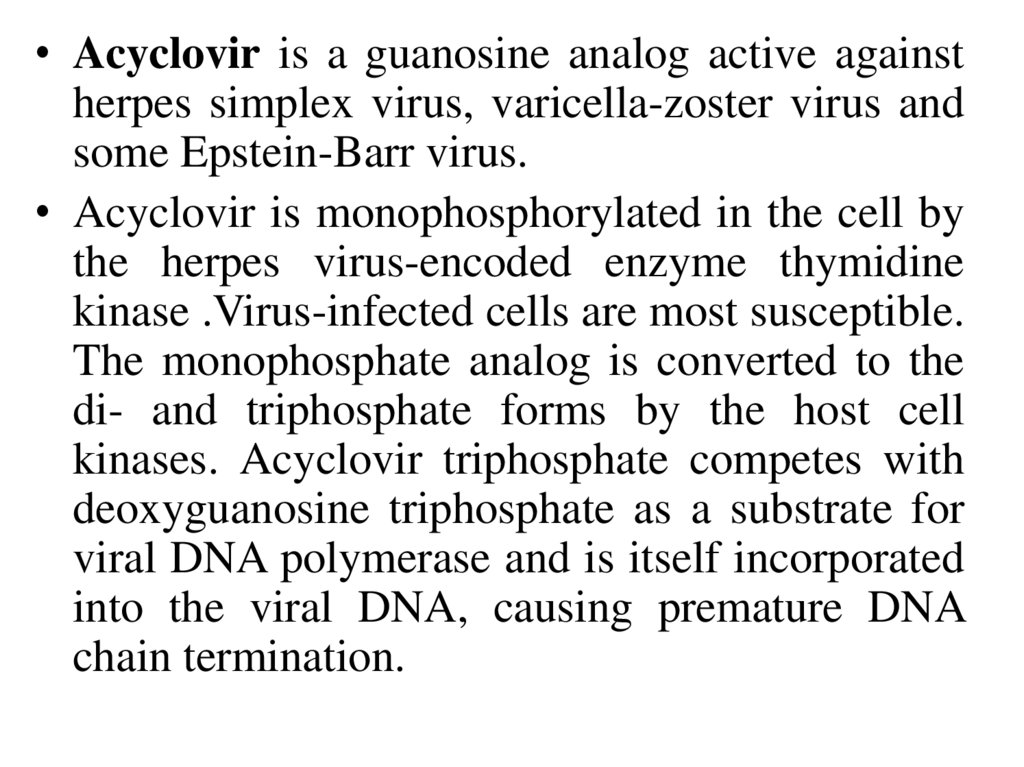
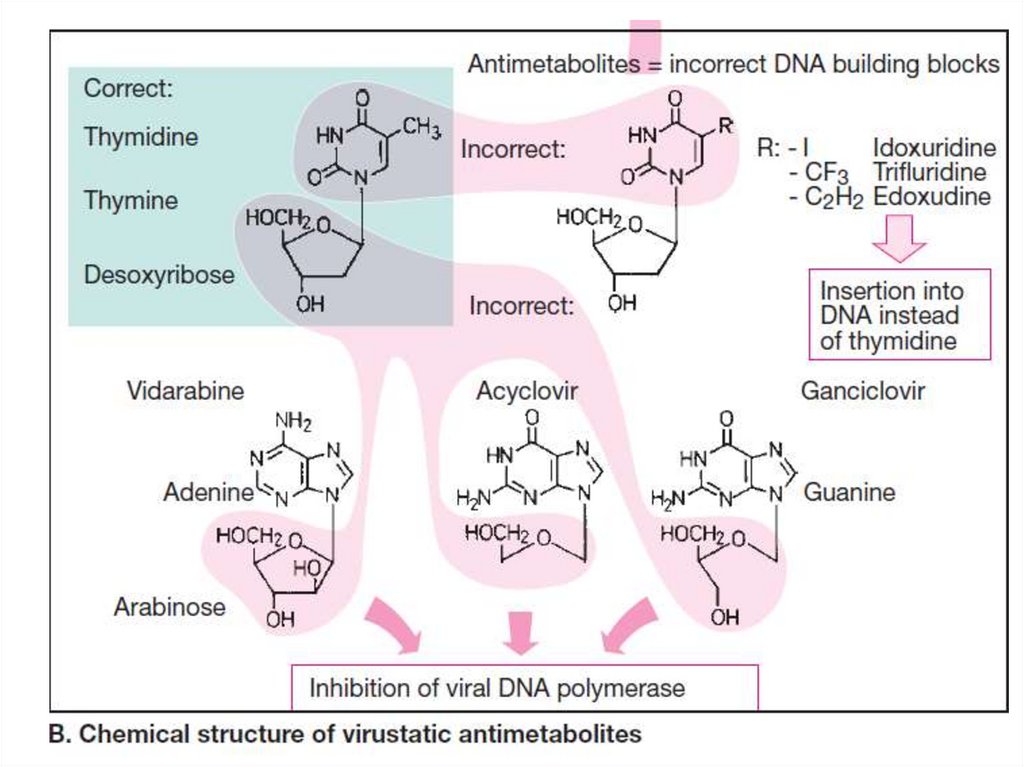
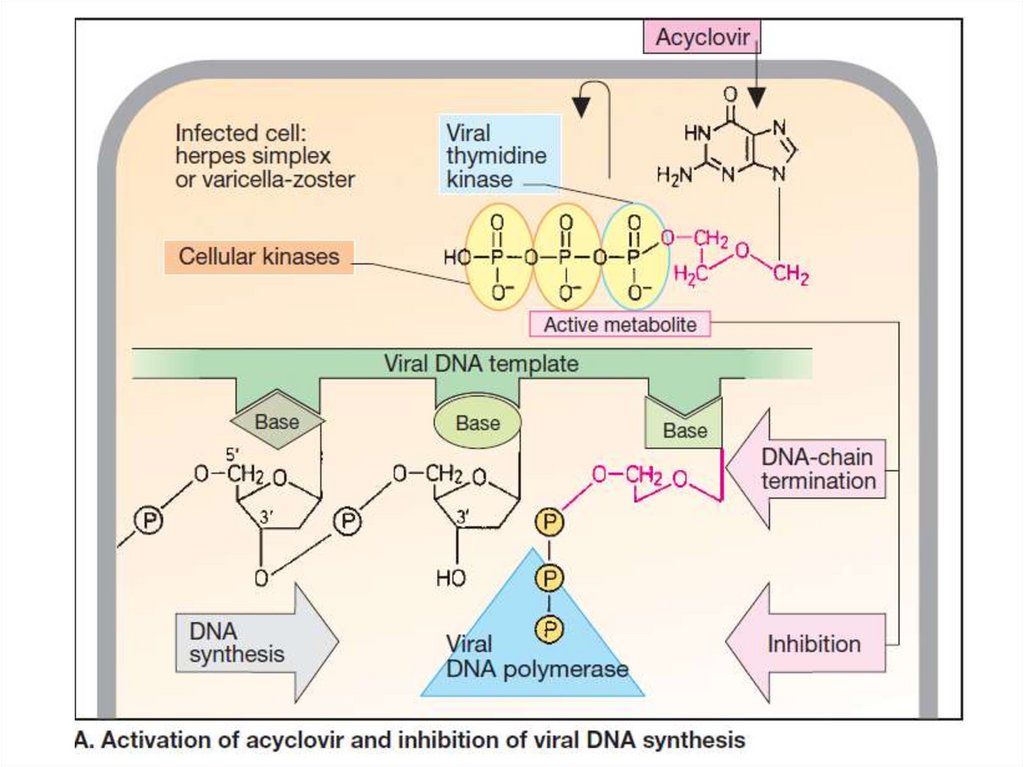
• Acyclovir is a guanosine analog active againstherpes simplex virus, varicella-zoster virus and
some Epstein-Barr virus.
• Acyclovir is monophosphorylated in the cell by
the herpes virus-encoded enzyme thymidine
kinase .Virus-infected cells are most susceptible.
The monophosphate analog is converted to the
di- and triphosphate forms by the host cell
kinases. Acyclovir triphosphate competes with
deoxyguanosine triphosphate as a substrate for
viral DNA polymerase and is itself incorporated
into the viral DNA, causing premature DNA
chain termination.
19.
20.
21.
• Acyclovir can be administered by the topical,and oral routes for the treatment of
mucocutaneous and genital herpes lesions.
• The oral drug is well tolerated but may cause
gastrointestinal distress and headache.
• Intravenous administration is used for severe
herpes disease, including encephalitis, and for
neonatal HSV infection.
• Toxic effects with parenteral administration
include delirium, tremor, seizures, hypotension
and nephrotoxicity
22.
• Ribavirin is an analogue of guanosine. It isphosphorylated in monophosphate, reduces the
synthesis of nucleotides.
• It turns into triphosphate, inhibits viral
dehydrogenase, disrupts the formation of
RNA, proteins and virus replication.
• It is used for influenza, herpes.
• It can cause allergic reactions.
• It is contraindicated in pregnancy.
23.
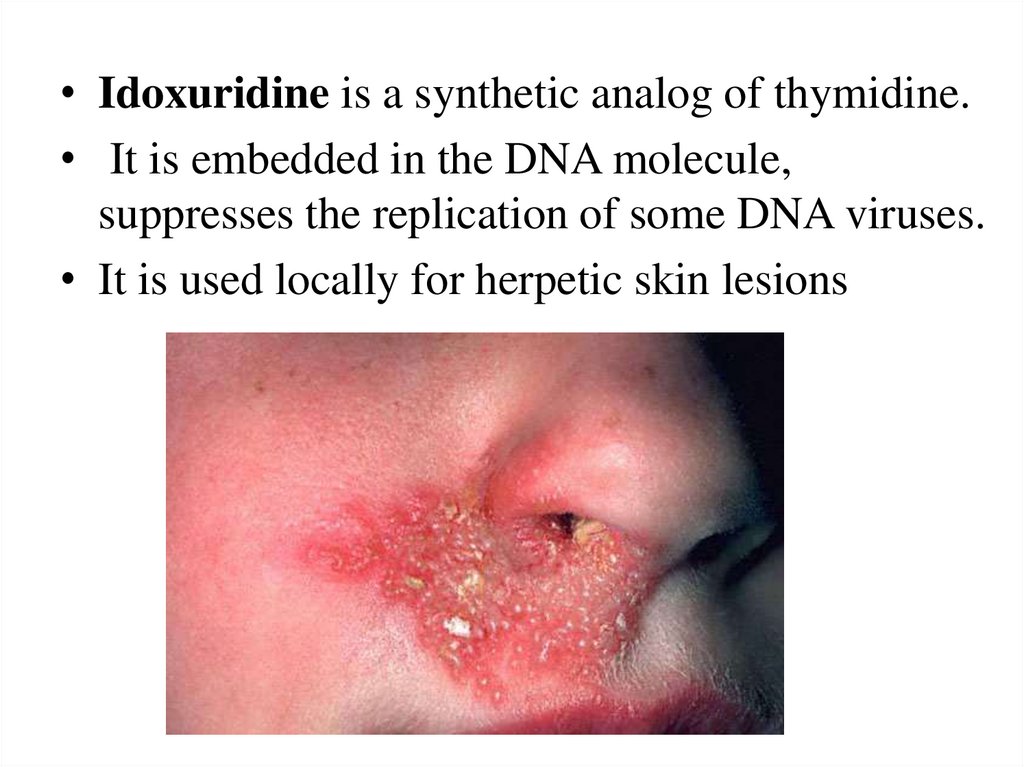
• Idoxuridine is a synthetic analog of thymidine.• It is embedded in the DNA molecule,
suppresses the replication of some DNA viruses.
• It is used locally for herpetic skin lesions
24.
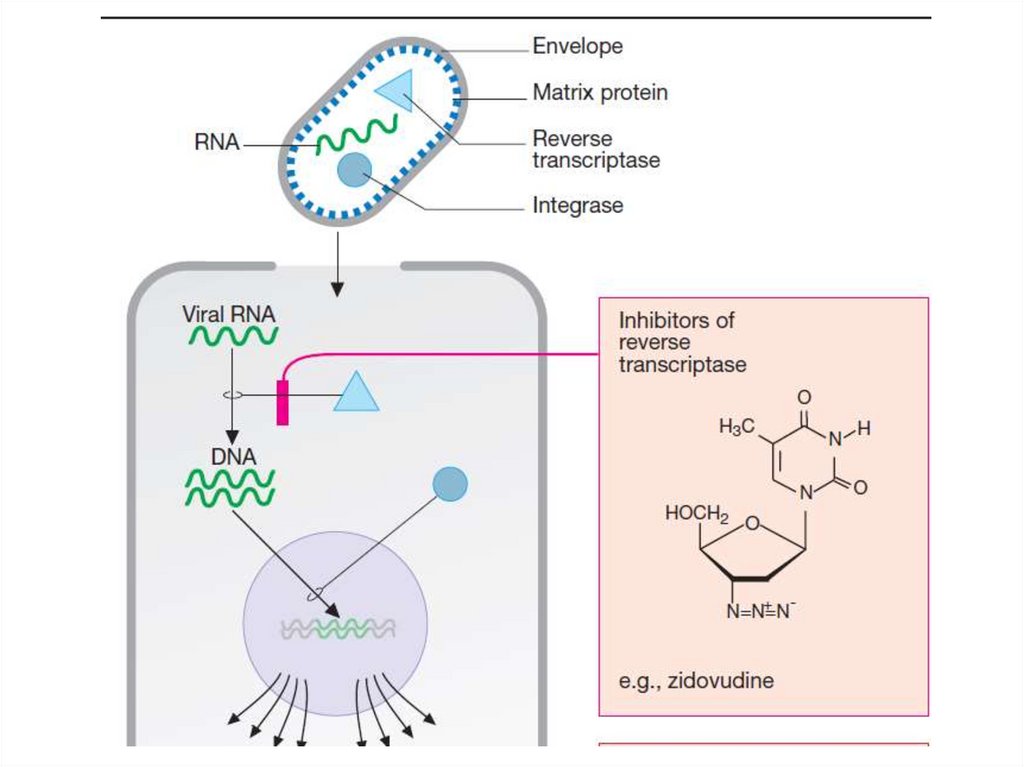
• Zidovudine is a nucleoside derivative. It isphosphorylated in the cells and is converted to
thymidine triphosphate. It inhibits the reverse
transcriptase of virion, prevents the formation of
DNA from viral RNA.
• This DNA can be stored in human cells and
become a source of RNA virus synthesis.
• Zidovudine inhibits the synthesis of mRNA and
viral proteins.
• HIV reverse transcriptase is 20-30 times more
sensitive to the inhibitory effect of the drug than
DNA polymerase of macroorganism cells.
25.
• It is used for the treatment of HIV infection.• It is effective during the first 6 to 8 months
from the start of disease and it delays the
development of the disease.
• It is used orally and IV, passes well into the
tissue, through the BBB. It is excreted by the
kidneys in the active form and in the form of
metabolites.
• Side
effects:
anemia,
neutropenia,
thrombocytopenia,
headache,
insomnia,
myalgia, renal dysfunction, dyspepsia.
26.
27.
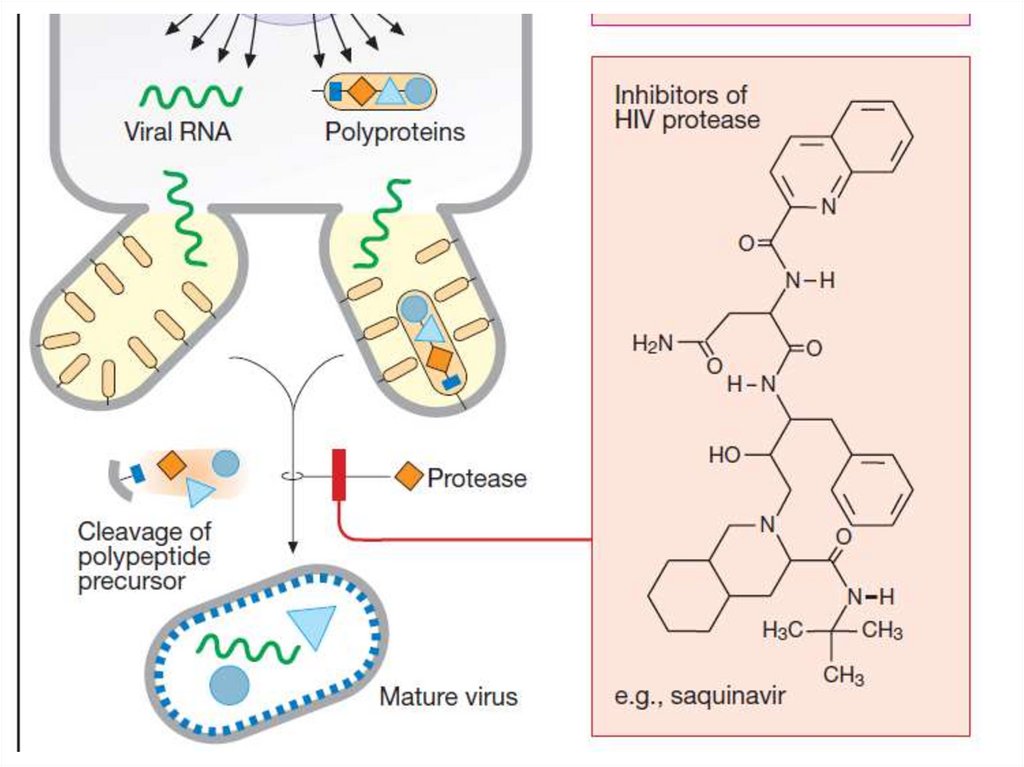
• Saquinavir selectively inhibits the HIVprotease. It disrupts the formation of structural
proteins and enzymes of HIV virions, which are
necessary for reproduction.
• Immature virion precursors are formed. The
development of infection is delayed.
• Saquinavir is used orally for HIV-1 infection
(causes HIV infection and AIDS) and HIV-2.
• Side effects: dyspepsia, increased activity of
liver enzymes, lipid metabolism disorders,
hyperglycemia.
28.
29.
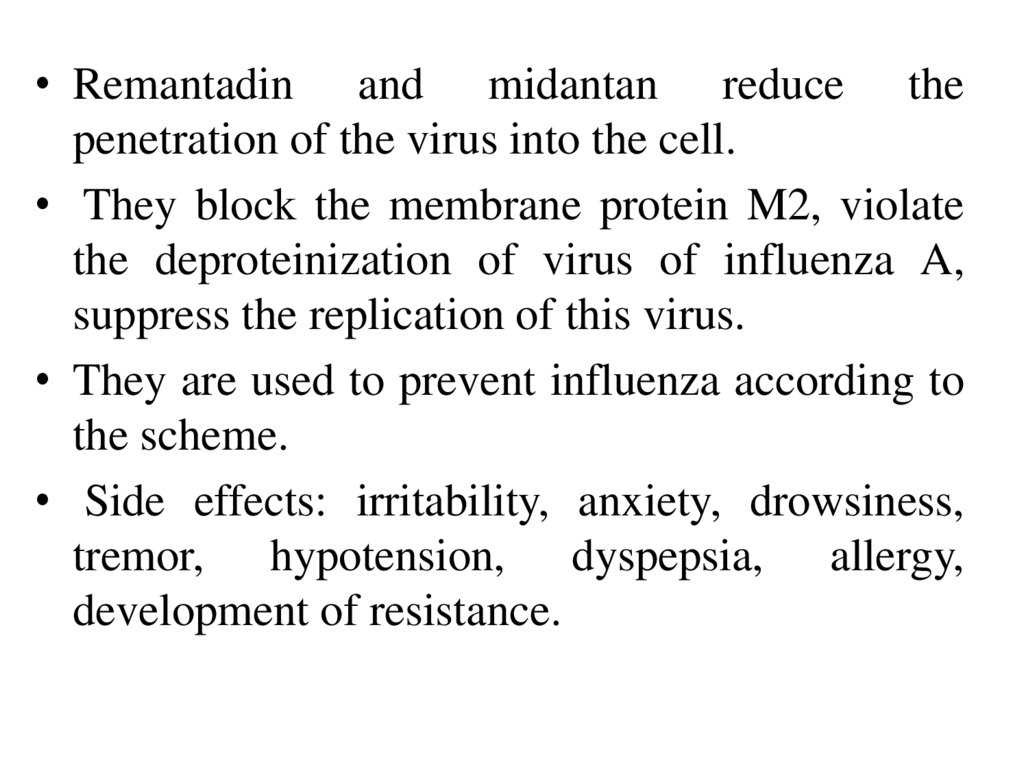
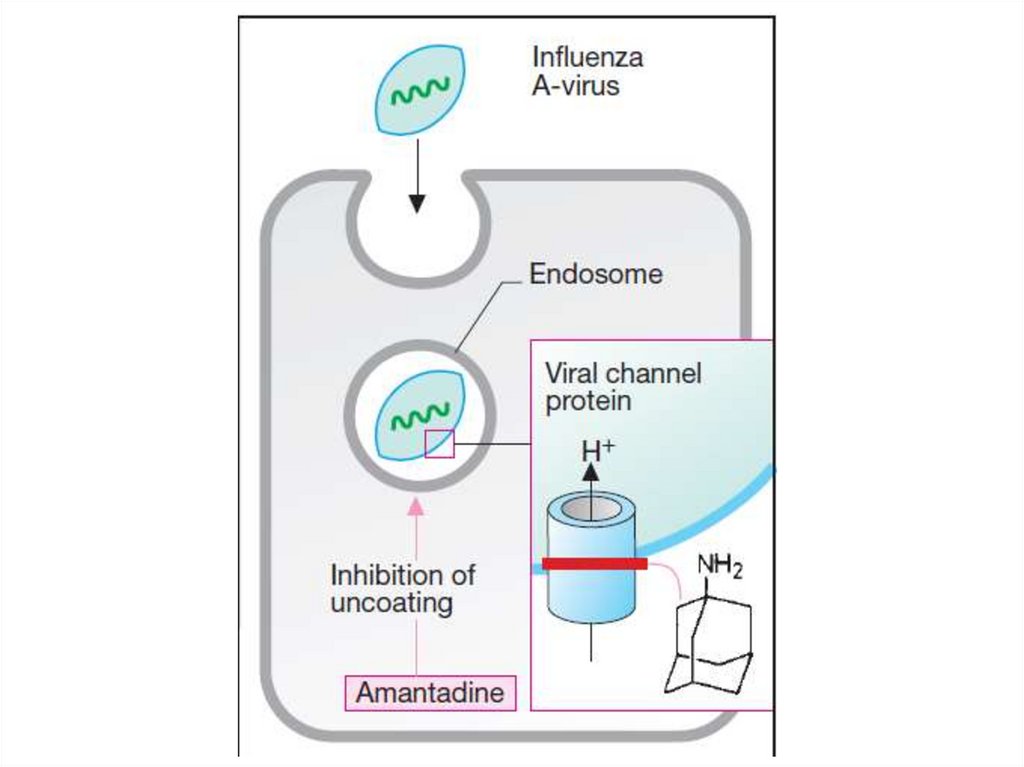
• Remantadin and midantan reduce thepenetration of the virus into the cell.
• They block the membrane protein M2, violate
the deproteinization of virus of influenza A,
suppress the replication of this virus.
• They are used to prevent influenza according to
the scheme.
• Side effects: irritability, anxiety, drowsiness,
tremor, hypotension, dyspepsia, allergy,
development of resistance.
30.
31.
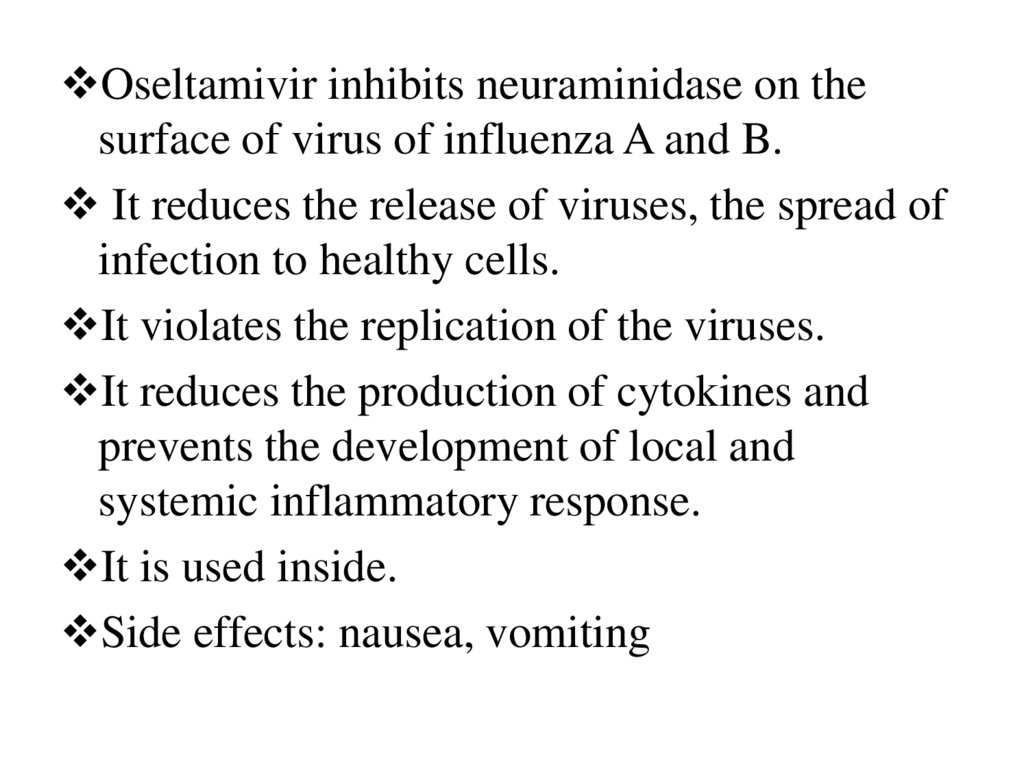
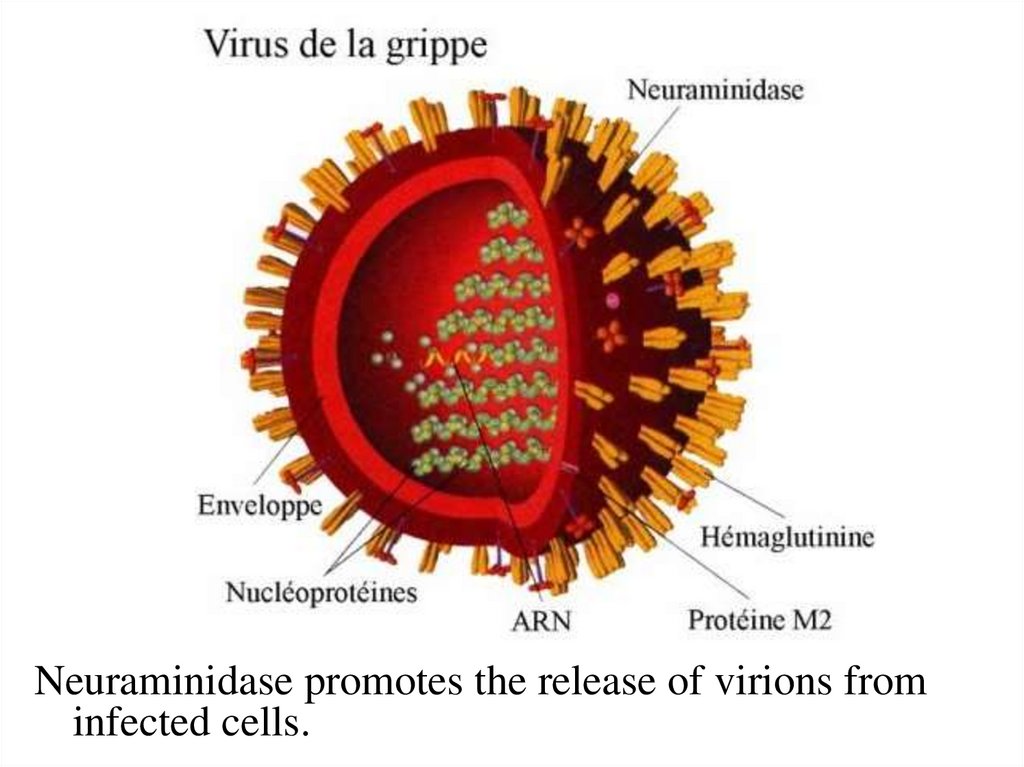
Oseltamivir inhibits neuraminidase on thesurface of virus of influenza A and B.
It reduces the release of viruses, the spread of
infection to healthy cells.
It violates the replication of the viruses.
It reduces the production of cytokines and
prevents the development of local and
systemic inflammatory response.
It is used inside.
Side effects: nausea, vomiting
32.
Neuraminidase promotes the release of virions frominfected cells.
33.
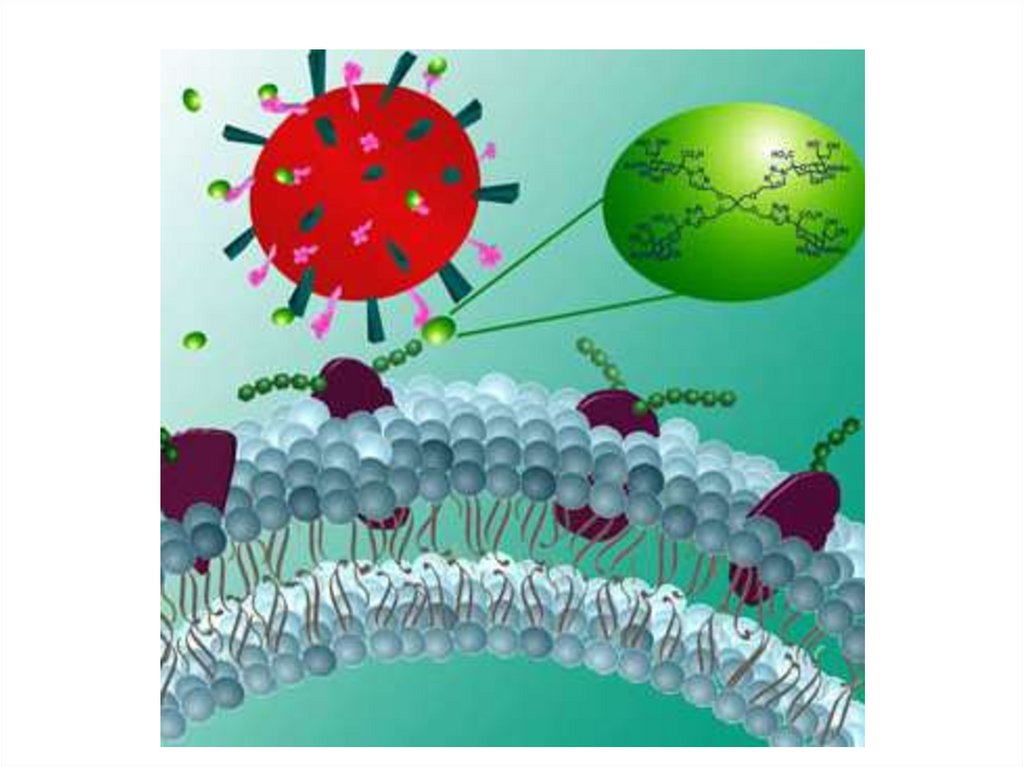
• Arbidol and oxoline reduce the penetration ofthe virus into the cells.
• Arbidol is active in influenza A and B,
adenovirus infection. It increases humoral and
cellular immunity, resistance to infections.
• It is used orally.
• Oxoline is used in drops or ointments for
prevention of influenza, herpetic, adenovirus
infection.
• It can cause irritating effect.
34.
35.
• Interferons-glycopeptides, which are producedby leukocytes (α), fibroblasts (β), lymphocytes
(γ).
• They bind to specific receptors on the surface of
cells infected with the virus, activate protein
kinases. They increase the synthesis of
endonucleases that destroy RNA of viruses.
• They reduce virus replication.
• Interferons increase immunity, macrophage
activity, cytotoxicity of T-killers.
• They are used in viral diseases: hepatitis,
encephalitis, rabies, herpes, influenza, adenovirus
infections, etc. They reduce the risk of cancer.
36.
• Drugs are obtained from cells and by geneticengineering.
• Preparations of α-interferon: Reaferon, Viferon
• β-interferon: Betaferon
• γ-interferon: Gammaferon.
• They are used locally for the treatment and
prevention of influenza, adenovirus infection,
herpes.
• They are administered IV, IM, SC in severe
forms of influenza, viral hepatitis, measles,
herpes, multiple sclerosis.
• They penetrate into the tissues poorly, they
quickly collapse.
37.
• Side effects of interferon: fever, chills,headache, soreness, hyperemia at the injection
site, tachycardia, hypotension, dyspepsia,
muscle pain.
• In very high doses, they cause violation of
hematopoiesis,
paresis,
paralysis,
hepatotoxicity
38.
39.
40.
• Amixin has an immunostimulatory effect, itincreases the production of α, β, γ interferons.
• It is used for influenza, acute respiratory viral
infections, hepatitis, neuroinfection, herpes,
cytomegalovirus infection.
• It can cause dyspepsia, chills, intermittent
fever, allergic reactions.
41. Literature
1. Tripathi K.D. Essentials of Medical Pharmacology. Eighth Edition. -2019.- Jaypee
Brothers Medical Publishers. The Health Sciences Publisher. -New Delhi. London.
Panama
2. D.A.Kharkevich. Pharmacology. Textbook for medical students. Translation of 12th
edition of Russion textbook “Pharmacology” (2017). – М., ГЭОТАР-Медиа, 2017.
3. Review of pharmacology. Gobind Rai Garg, Sparsh Gupta. 13th edition. - 2019.Jaypee Brothers Medical Publishers. The Health Sciences Publisher. -New Delhi.
London. Panama
4. Whalen Karen. Lippincott Illustrated Reviews: Pharmacology. Sixth Edition. Wolters Kluwer. - 2015.-Philadelphia
5. Color Atlas of Pharmacology. 2nd edition, revised and expanded. Heinz Lüllmann.2000 Thieme
6. Pharmacology Examination & Board Review. Tenth Edition. Trevor Anthony J.,
Katzung Bertram G., Kruidering-Hall Marieke, Susan B. Masters. - a LANGE medical
book. - 2013.-New York
7. Medical Pharmacology at a Glance. Eighth Edition. Neal Michael J. – 2016. John
Wiley & Sons, Ltd.
8. USMLE Step 1. Lecture Notes. Pharmacology. Lionel P.Raymon and others.Kaplan Medical.Inc. -2009



 medicine
medicine