Similar presentations:
Antimicrobial agents
1. ANTIMICROBIAL AGENTS
2.
ANTIBIOTICSANTIMICROBIAL AGENTS
CHEMOTHERAPEUTIC AGENTS
3. ANTIBIOTICS
Natural substances produced by variousspecies of microorganisms
bacteria
fungi
actinomycetes
suppress growth / kill other
microorganisms
4. ANTIMICROBIAL AGENTS
Synthetic analoguesANTIMICROBIAL AGENTS :
includes synthetic as well as naturally
obtained drugs that attenuate
microorganisms
5. CHEMOTHERAPEUTIC AGENTS
Drugs in this class differ from all othersin that they are
Designed to inhibit/kill the infecting
organism and have no/minimal effect
on the recipient.
6.
ClassificationOf AMA’s
7.
Microorganisms of medical impotance fallinto four categories
Bacteria
Viruses
Fungi
Parasites
8.
Anti-bacterialAnti-viral
Anti-fungal
Anti-parasitic agents
9. Mechanism of Action
Agents that inhibit synthesis ofbacterial cell walls
Penicillins & cephalosporins
Cycloserine,
Vancomycin
Bacitracin
Azole antifungal agents (clotrimazole,
fluconazole, itraconazole)
10.
Agents that act directly on the cellmembranes of the microorganisms
Polymixin
Polyene antifungal agents
(Nystatin, Amphotericin B)
Alter cell memb. Permeability,
leakage of intracellular comp.
11.
Agents that affect the function of 30Sor 50S ribosomal subunits to cause a
reversible inhibition of protein
synthesis
Bacteriostatic drugs
Chloramphenicol, Tetracyclines,
Erythromycin, Clindamycin,
Pristinamycins
12.
Agents that bind to 30S ribosomalsubunit & alter protein synthesis,
which eventually leads to cell death
Aminoglycosides
13.
Agents that affect bacterial nucleicacid metabolism.
Rifamycins which inhibit RNA
polymerase
Quinolones which inhibit topoisomerases
14.
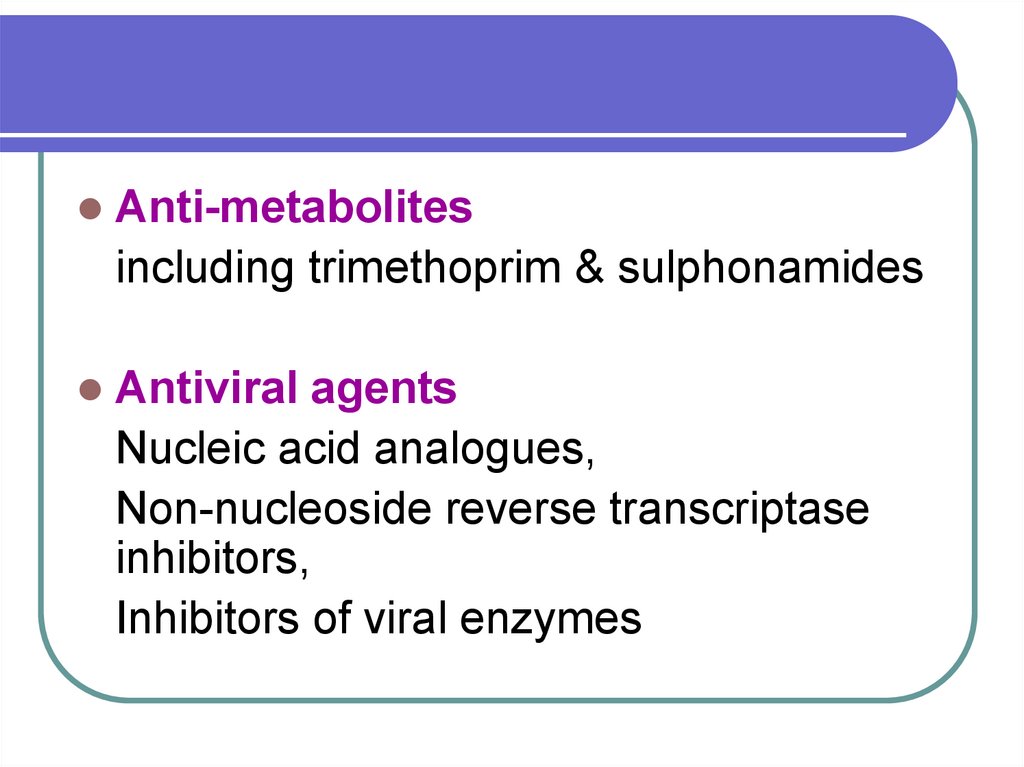
Anti-metabolitesincluding trimethoprim & sulphonamides
Antiviral agents
Nucleic acid analogues,
Non-nucleoside reverse transcriptase
inhibitors,
Inhibitors of viral enzymes
15.
16. TYPE OF ACTION
Bacteriostatic AgentsBactericidal Agents
17.
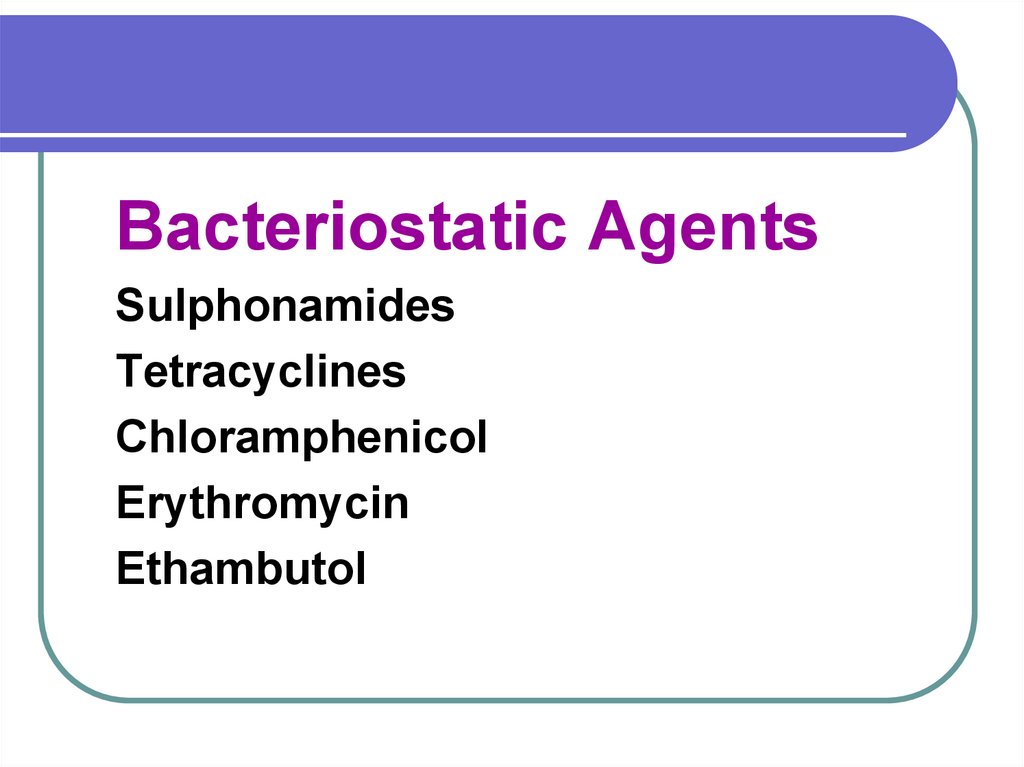
Bacteriostatic AgentsSulphonamides
Tetracyclines
Chloramphenicol
Erythromycin
Ethambutol
18.
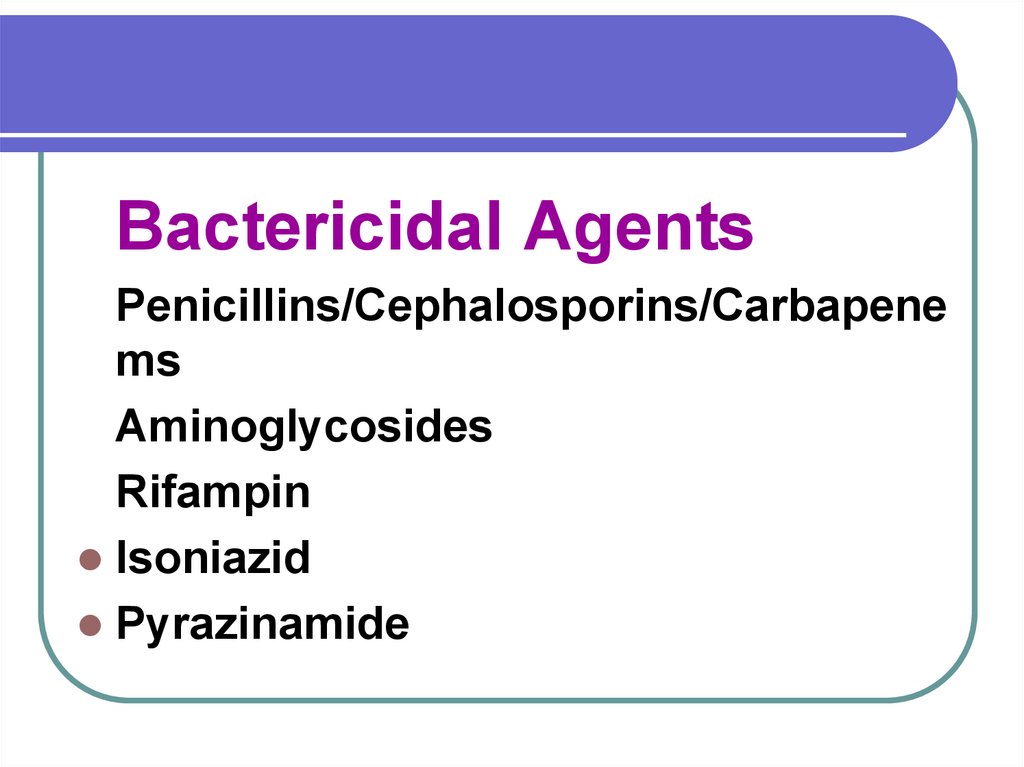
Bactericidal AgentsPenicillins/Cephalosporins/Carbapene
ms
Aminoglycosides
Rifampin
Isoniazid
Pyrazinamide
19.
CephalosporinsVancomycin
Nalidixic acid
Ciprofloxacin
Metronidazole
& Cotrimoxazole
20.
Some primarily static drugs may becomecidal at higher concentrations (as
attained in the urinary tract) & vice-versa.
21. SPECTRUM Of ACTIVITY
Narrow spectrumBroad spectrum
22. SPECTRUM Of ACTIVITY
Narrow spectrumPenicillin G
Streptomycin
Broad spectrum
Tetracyclines
Chloramphenicol
23. Successful Antimicrobial Therapy
Concentration: site of infectionConcentration should inhibit
microorganisms
simultaneously it should be below the
level toxic to human beings.
Host Defences
Immunity intact - Bacteriostatic Agents
Impaired immunity - Bactericidal Agents
24. Source of antibiotics
FungiBacteria
Actinomycetes.
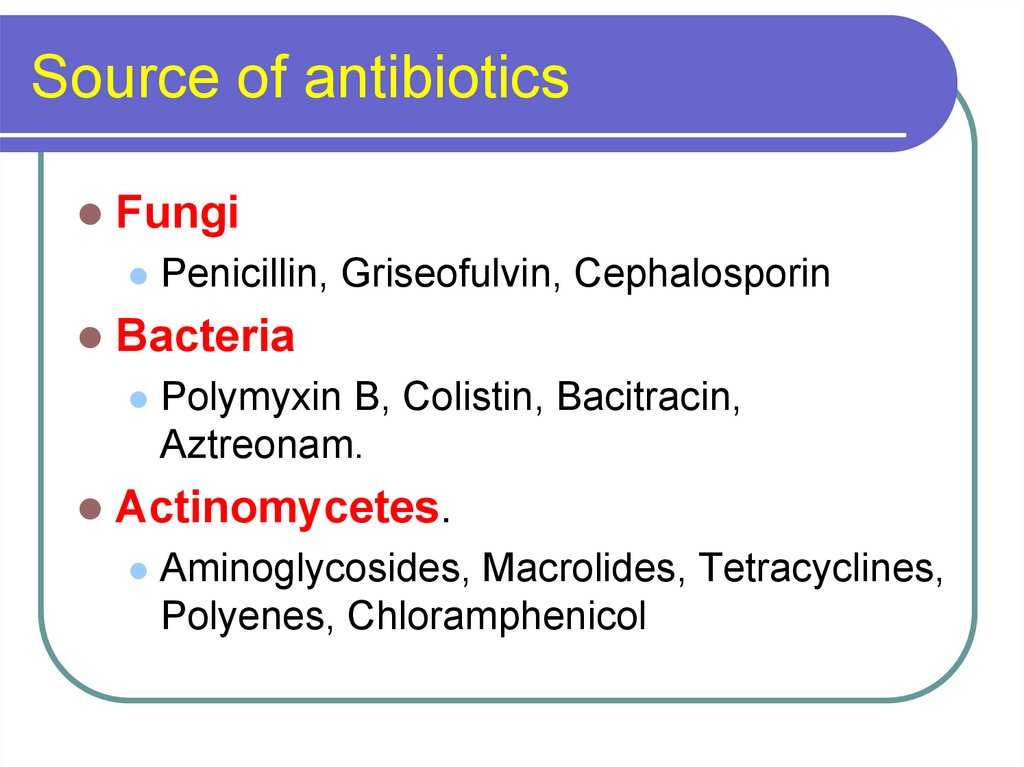
25. Source of antibiotics
FungiPenicillin, Griseofulvin, Cephalosporin
Bacteria
Polymyxin B, Colistin, Bacitracin,
Aztreonam.
Actinomycetes.
Aminoglycosides, Macrolides, Tetracyclines,
Polyenes, Chloramphenicol
26.
Resistance27. Bacterial resistance to ANTIMICROBIAL AGENTS
3 general categoriesDrug does not reach its target
Drug is not active
Target is altered
28. Drug does not reach its target
PorinsAbsence/mutation
Reduce drug entry
Reduced effective drug concentration at the
target site.
Efflux pumps
Transport drugs out of the cell
Resistance to tetracyclines & β-lactam antib
29. Inactivation of Drug
Second general mechanism of drugresistance
β-lactam antibiotics - β-lactamase
Aminoglycosides - Aminoglycoside
modifying enzymes
Variant: failure of bacterial cell to
convert an inactive drug to its active
metabolite. Resistance to INH in
mycobacterium TB
30. Alteration of the Target
Mutation of natural targetTarget modification
The new target does not bind the drug
for native target
Resulting in resistance to antibiotic.
31.
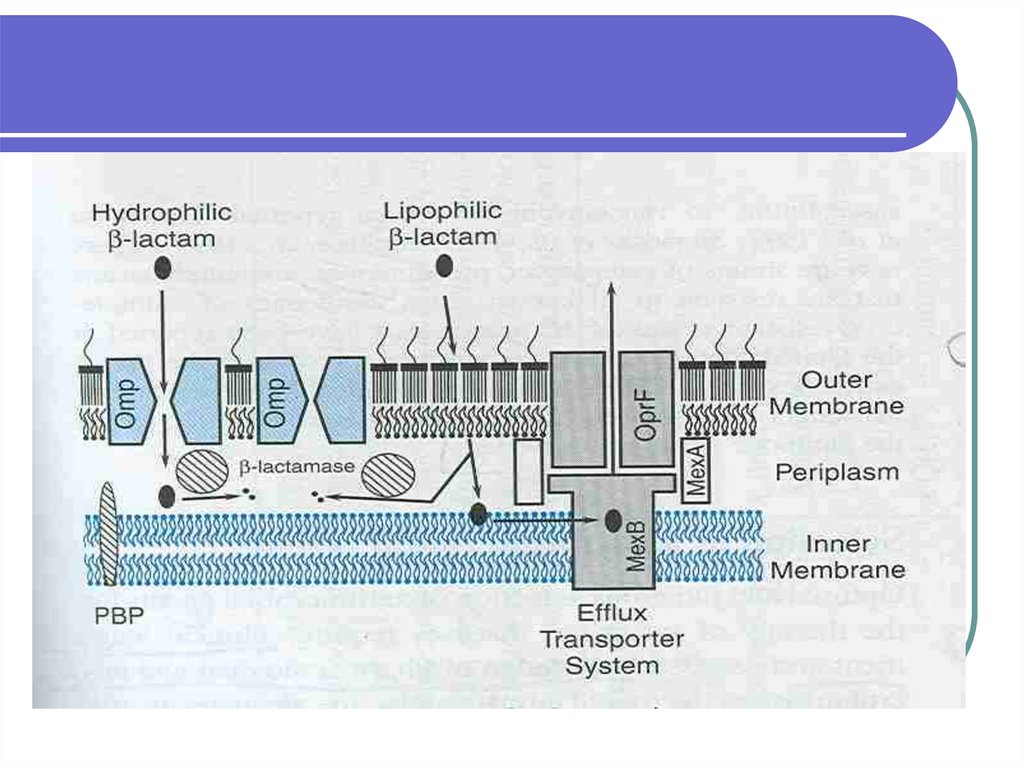
Components mediating resistance to β –lactam antibiotics in psuedomonas aeruginosa
32.
33.
β –lactam antibiotics hydrophilicMust cross outer membrane barrier of
the cell via outer membrane protein
(Omp) channel or porins
Mutation/missing/deleted
Drug entry slow or prevented.
34.
β - lactamase concentrated between theinner & outer membrane in the
periplasmic space
constitutes an enzymatic barrier
Drug destroyed
Effective concentration not achieved
35.
Target: PBP penicillin binding proteinLow affinity for drug
Altered
36.
Efflux transporterMex A, Mex B & Opr F
Pumps the antibiotic across the outer
membrane
Reduced intracellular concentration of
active drug
RESISTANCE
37. Mutations
May occur inTarget protein
Drug transport protein
Protein important for drug activation
Random events
Survival advantage upon re-exposure
to the drug
38.
Resistance is acquired by horizontaltransfer of resistance determinants from
a donor cell, often of another bacterial
species by
Transduction
Transformation
Conjugation
39.
Insatiable need for newantibiotics
40.
Emergence of antibiotic resistance inbacterial pathogens both nosocomially &
in the community setting is a very
serious development that threatens the
end of antibiotic era.
41.
Responsible approach to the use ofantibiotics
That are now available & new agents
that might be developed in future
Is essential
If the end of antibiotic era is to be
averted.
42.
CROSS RESISTANCE43. CROSS RESISTANCE
Acquisition of resistance to one AMAconferring resistance to another
antimicrobial agent to which the
organism has not been exposed,is called
cross resistance
Seen b/w chemically or mechanistically
related drugs.
44.
Resistance to one sulphonamidemeans resistance to all others
Resistance to one tetracyclines
means insenstivity to all others
Complete cross resistance
45.
Resistance to one aminoglycosidemay not extend to others,
Gentamycin resistant strains may
respond to amikacin.
partial cross resistance
46.
Sometimes unrelated drugs show partialcross resistance,
e.g. Tetracyclines
& Chloramphenicol
47.
PREVENTIONDRUG
RESISTANCE
48. Prevention DRUG RESISTANCE
Use of AMAs should not be:indiscriminate
inadequate
unduly prolonged
Use rapidly acting & narrow spectrum
(Selective) AMA whenever possible.
49. Prevention DRUG RESISTANCE
Combination AMAwhenever prolonged therapy is undertaken.
Tuberculosis, SABE
Infection by organism notorious for
developing resistance Staph, E. Coli, M.
Tuberculosis must be treated intensively.

 medicine
medicine biology
biology