Similar presentations:
Antihistamine agents. Immunopharmacology
1.
ZSMU Pharmacology DepartmentLecture № 6
ANTIHISTAMINE AGENTS.
IMMUNOPHARMACOLOGY
1
2.
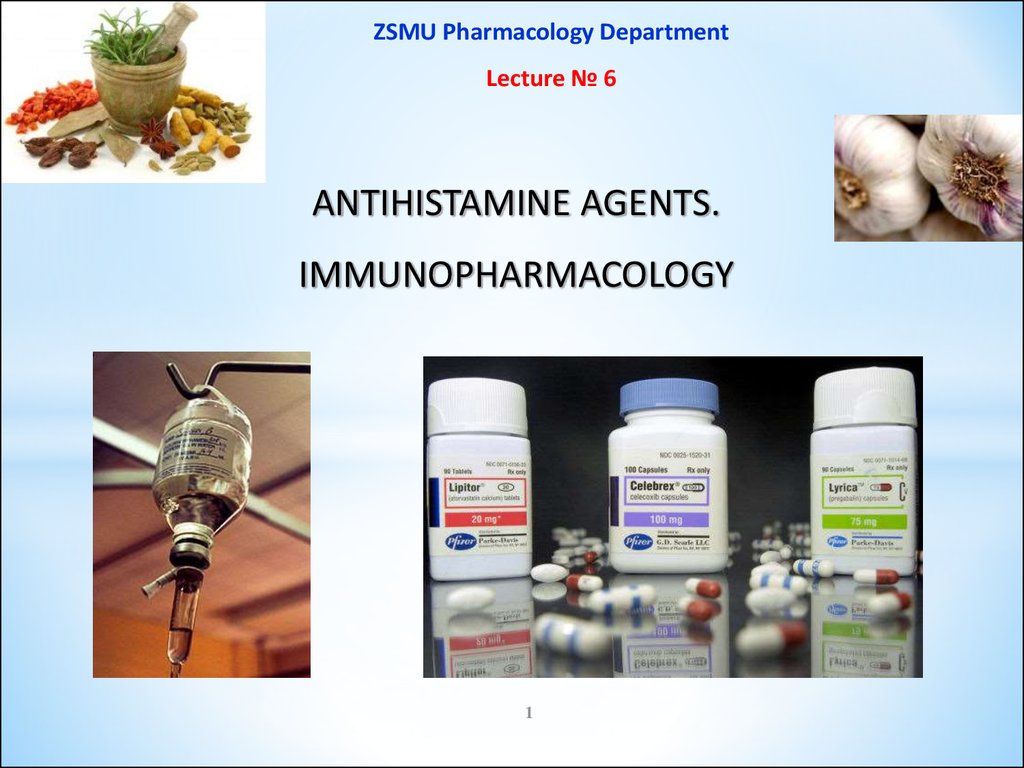
Allergic Reactions on Drugs include4 types of Hypersensitivity Reactions:
A. Humoral type:
Type I : Anaphylactic reactions
Type II : Cytolytic reactions
Type III : Retarded reactions
B. Cell mediated (Ig-mediated):
Type IV : Delayed reactions
2
3.
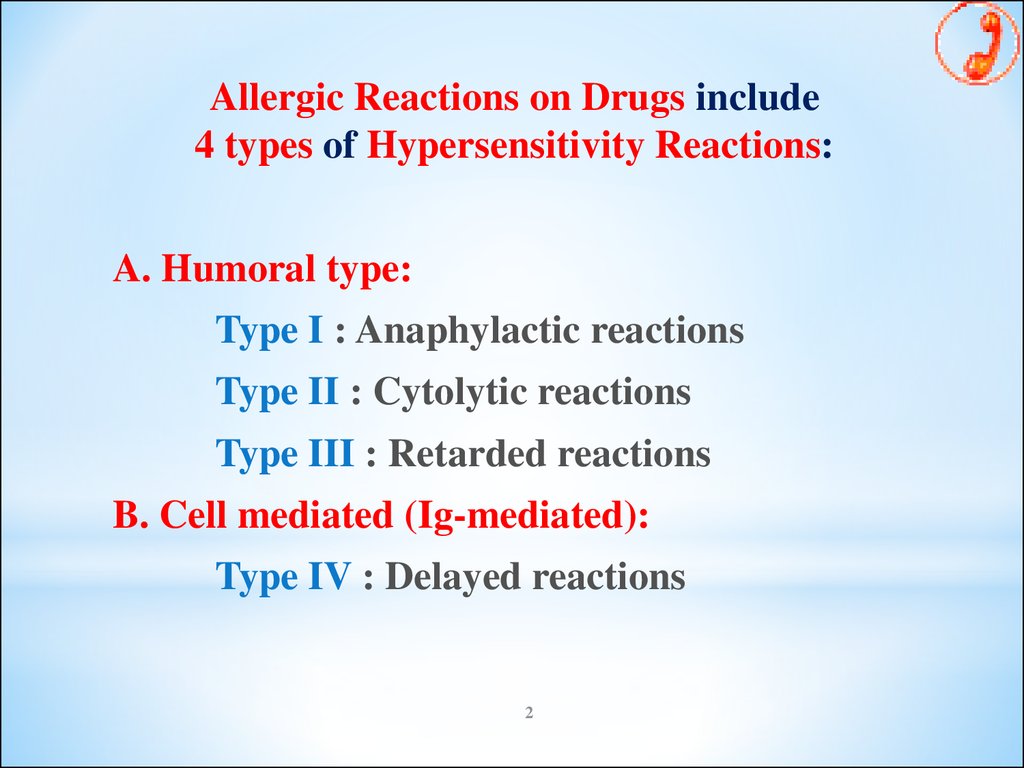
ANTIALLERGIC DRUGS1. Drugs Stabilizing Mast Cell Membrane:
Glucocorticoids: Prednisolone, Hydrocortisone
Antihistamine H1 : Ketotifen
Mast cell stabilizers: Cromolyn, Nedocromil
β-adrenomimetics: Adrenaline, Ephedrine
Methylxanthines: Euphylline (Aminophylline)
2. Antihistamine H1 agents: Dimedrol, Diprazine, Loratadine
3. Agents eliminating generalized symptoms of immediate allergic reactions:
Adrenomimetics: Adrenaline
Methylxanthines: Euphylline, Theophylline
Ca2+ preparations: Calcium chloride, Calcium gluconate
4. Agents decreasing tissue damage: Glucocorticoids
3
4.
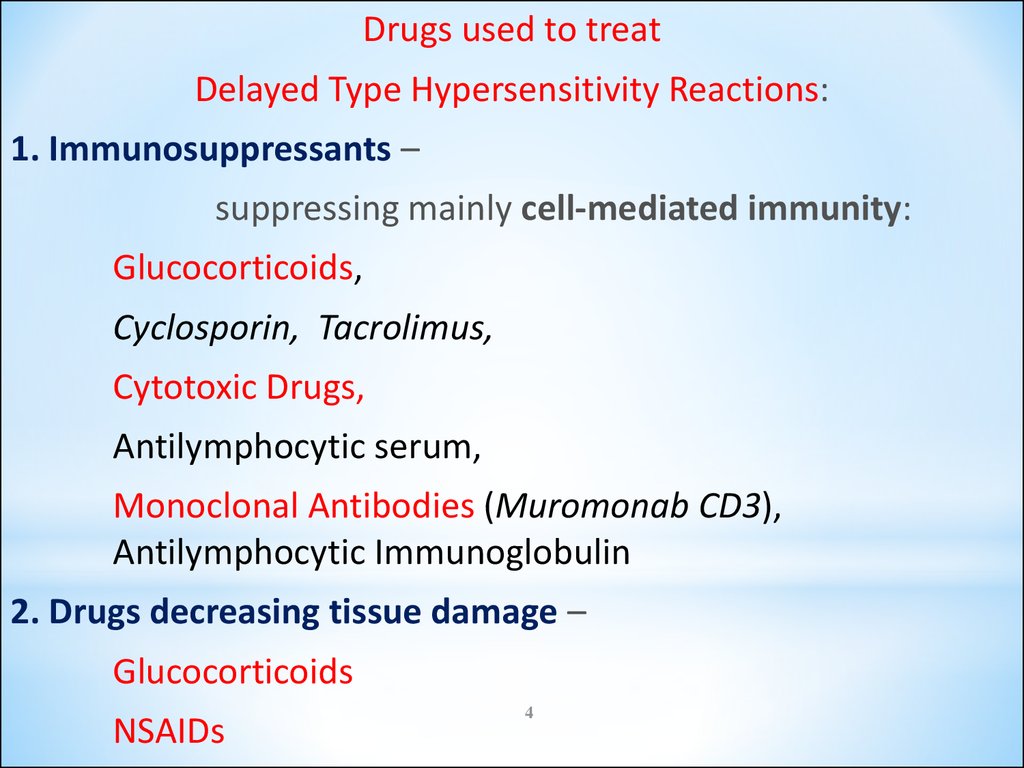
Drugs used to treatDelayed Type Hypersensitivity Reactions:
1. Immunosuppressants –
suppressing mainly cell-mediated immunity:
Glucocorticoids,
Cyclosporin, Tacrolimus,
Cytotoxic Drugs,
Antilymphocytic serum,
Monoclonal Antibodies (Muromonab CD3),
Antilymphocytic Immunoglobulin
2. Drugs decreasing tissue damage –
Glucocorticoids
NSAIDs
4
5.
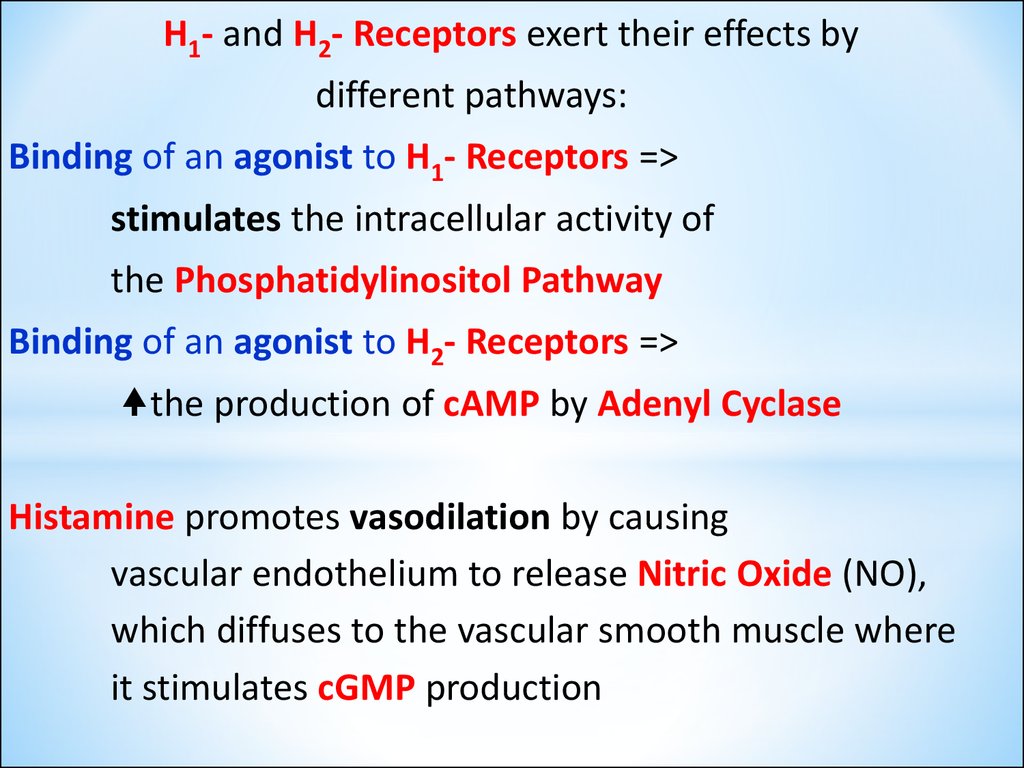
H1- and H2- Receptors exert their effects bydifferent pathways:
Binding of an agonist to H1- Receptors =>
stimulates the intracellular activity of
the Phosphatidylinositol Pathway
Binding of an agonist to H2- Receptors =>
the production of cAMP by Adenyl Cyclase
Histamine promotes vasodilation by causing
vascular endothelium to release Nitric Oxide (NO),
which diffuses to the vascular smooth muscle where
it stimulates cGMP production
6.
67.
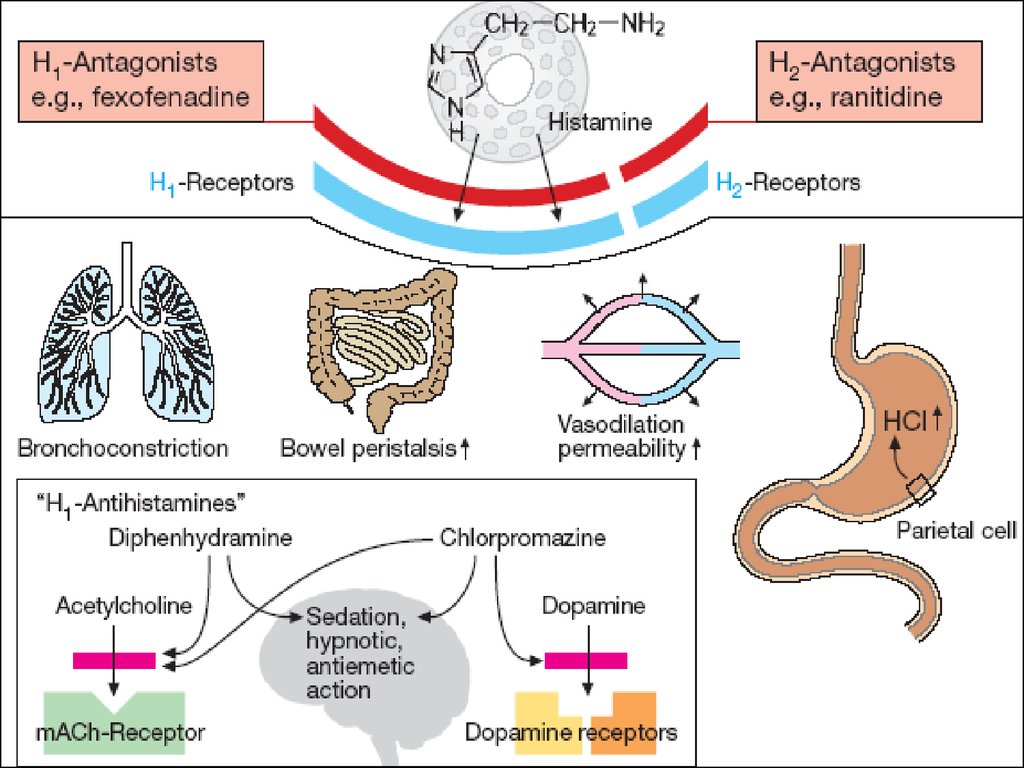
H1-Receptor AntagonistsI GENERATION (SEDATIVE):
Dimedrol (Diphenhydramine)
Diprazine (Promethazine)
Suprastine (Chloropyramine)
Diazoline
Tavegyl (Clemastin)
II GENERATION (NON-SEDATIVE):
Loratadine (Claritin)
Terfenadine
Astemizole
Phencarol (Quifenadine)
III GENERATION (ACTIVE METABOLITES):
Telfast (Fexofenadine)
Zirtek (Cetirizine)
7
8.
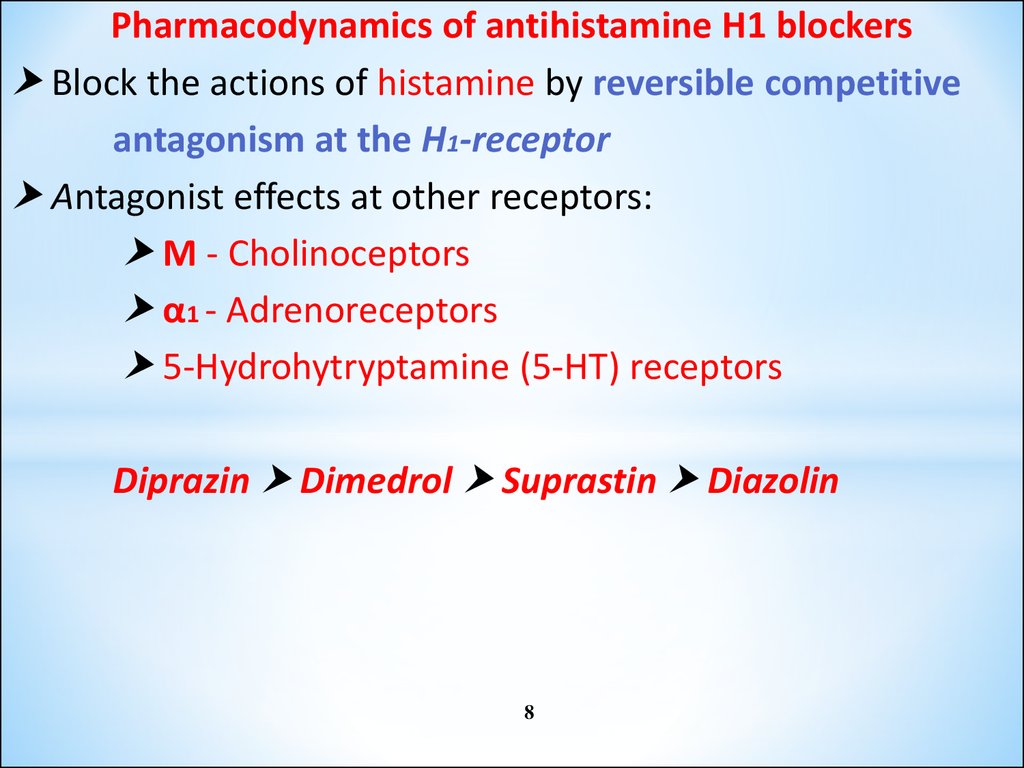
Pharmacodynamics of antihistamine H1 blockersBlock the actions of histamine by reversible competitive
antagonism at the H1-receptor
Antagonist effects at other receptors:
M - Cholinoceptors
α1 - Adrenoreceptors
5-Hydrohytryptamine (5-HT) receptors
Diprazin Dimedrol Suprastin Diazolin
8
9.
Dimedrol (Diphenhydramine)-Tab 0.05 g, amp 1%-1 mlcompetes to H1 receptors on the smooth muscle of
the bronchi, GIT, uterus, and large blood vessels.
By binding to receptors, suppresses histamine-induced
allergic symptoms, even though it does not prevent its
release.
Central antimuscarinic actions is responsible for antivertigo,
antiemetic, and antidyskinetic action.
Clinical uses:
Allergy symptoms
Motion sickness
Parkinson’s disease
Nonproductive cough
Insomnia
9
10.
Suprastine (Chloropyramine)-Tab. 0.025 g, amp. 2% - 2 ml H1 receptor antagonist of I generation.It competes to histamine H1 receptor sites on the smooth
muscle of the bronchi, GIT, uterus, and large blood
vessels.
It has less expressed antihistamine, M-cholinoblocker and
sedative effects than Dimedrol.
Clinical uses:
Allergic dermatosis
Allergic rhinitis
Conjunctivitis
Quincke’s edema
Medicamental allergy
Hay (pollen) fever
10
11.
Terfenadine (Claritin)-.blocks cardiac K+ channels, prolongs Q-T and
has occasionally produced Polymorphic Ventricular Tachycardia.
The risk is increased in liver disease or when inhibitors of CYP3A4 are
administered concurrently – because larger amounts of unchanged drug
reach systemic circulation.
Erythromycin, Clarithromycin, Ketoconazole and Itraconazole
are the drugs precipitating their
cardiotoxicity as they block
microsomal CYP-450 enzymes.
Because of this risk,
Terfenadine has been withdrawn
by most manufactures.
Clinical use: allergic rhinitis
11
12.
Telfast (Fexofenadine) and Zirtek (Cetirizine)non-toxic metabolites of Terfenadine
that do not block K+ channels in the heart –
does not prolong Q-T interval.
Telfast has plasma T1/2 11-16 hours and duration
of action 24 hours.
12
13.
Drugs used to treat Delayed Type Hypersensitivity Reactions:I. IMMUNOSUPRESSANTS - suppressing mainly
cell-mediated immunity:
1.Inhibitors of IL-2 production or action:
Cyclosporine (Sandimmune)
Tacrolimus
2.Inhibitors of cytokine gene expression:
Glucocorticoids: Prednisolone
3. Antitumor Cytotoxic Agents:
a) Alkylating agents: Cyclophosphan
b) Antimetabolites: Azathioprine, Mercaptopurine,
Methotrexate
4.Blockers of the T-cell surface molecules involved in signaling Monoclonal Antibodies: Basiliximab
and Daclizumab
13
14. Clinical uses of immunosupressants:
to suppress rejection of transplanted organsto suppress graft-versus-host disease
to treat diseases that are believed to have
autoimmune component in their pathogenesis:
● Idiopathic thrombocytopenic purpura
● Hemolytic anemia
● Glomerulonephritis
● Myasthenia gravis
● Systemic lupus erythematosus
● Rheumatoid arthritis
● Psoriasis
14
15.
Cyclosporine amp.5% - 1 ml, caps. 50 mg –a polypeptide antibiotic with immunosuppressive activity but no effect
on the acute inflammatory reaction per se.
The main action is a relatively selective inhibitory effect on
IL-2 gene transcription, though an effect on
the transcription of the genes for IFN-γ and IL-3
has also been reported:
IL-2 Release and
IL-2 Receptors Expression =>
Clonal Proliferation of T-cells
Transcription of the genes for interferon-γ
Clonal Proliferation of cytotoxic T-cells from
CD8+ precursor T-cells
15
16.
2.GlucocorticoidsPrednisolone
Beclomethasone
Hydrocortisone
Betamethasone
Triamcinolone
Fluocinolone (Flucinar)
Dexamethasone
Fluomethasone (Lorinden)
Decrease Transcription of Genes for
IL-2
TNF-α
IFNγ
IL-1
and many other INTERLEUKINS in both the INDUCTION and
EFFECTOR PHASES of the immune response =>
Restrain the clonal proliferation of Th cells
17.
3. Antitumor Cytotoxic DrugsCyclophosphan (Cyclophosphamide)
Tab. 0.05 g, amp. 0.2 and 0.5 g
is cytotoxic only after generation of
its alkylating species, following
their hydroxylation by CYP-450.
Exerts its cytotoxic effects by
covalently binding to nucleophylic groups
on various cell constituents
Destroys proliferating lymphoid cells
but also appears to alkylate
some resting cells.
17
18.
1819.
Methotrexate – the folate analogue –acts as a false substrate,
inhibits enzyme activity of dihydrofolate reductase =>
Tetrahydrofolic acid required for the synthesis of
Purine Bases and Thymidine =>
=> Synthesis of DNA and RNA building blocks ceases.
The effect of these antimetabolites can be reversed by
administration of Folic acid.
19
20.
Azathioprine – Tab. 50 mg - interferes with purine synthesis.a prodrug metabolized to give
the antimetabolite 6-mercaptopurine,
a purine analogue that inhibits DNA synthesis.
Both cell-mediated and antibody-mediated
immune reactions are depressed by azathioprine since
it inhibits clonal proliferation in the induction phase of
the Immune response by a cytotoxic action on dividing cells.
Clinical uses:
Control of tissue rejection in TRANSPLANT SURGERY
Autoimmune diseases: systemic lupus erythematosus,
rheumatoid arthritis.
Adverse effects:
bone marrow depression
skin eruptions, hepatotoxicity.
21.
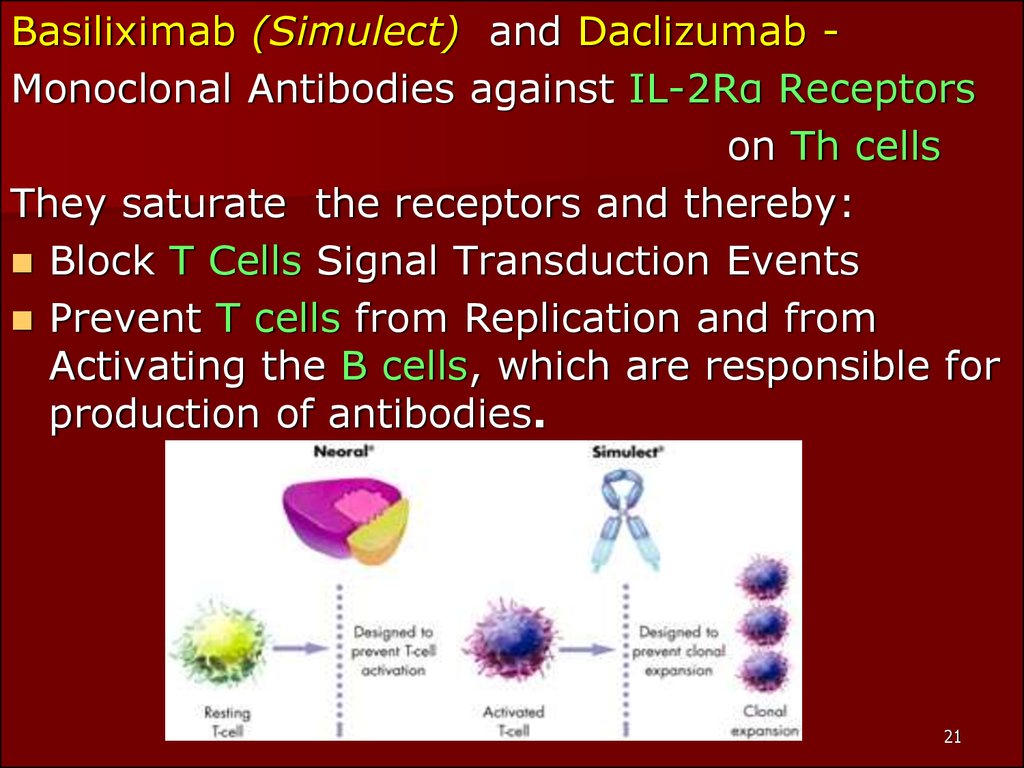
Basiliximab (Simulect) and Daclizumab Monoclonal Antibodies against IL-2Rα Receptorson Th cells
They saturate the receptors and thereby:
Block T Cells Signal Transduction Events
Prevent T cells from Replication and from
Activating the B cells, which are responsible for
production of antibodies.
21
22.
2223. IMMUNOMODULATING AGENTS
I. Biogenic substances:1. Preparations of the Thymus:
Thymosin
Thymalin
Tactivine
2. Peptides:
Thymogen
3. Inductor of Interferon:
Cycloferon
23
24.
4. Interferons:Interferon – α: amp. 1 and 3 million IU, SC
amp. 100,000 IU – intranasally
Interferon - β: IFN β-1a, IFN β-1b
Interferon - γ 1b
5. Inerleukin-2
6. BCG
II. Synthetic compounds:
Levamisol (Decaris) – Tab. 50 mg and 150 mg
24
25.
Cycloferon (amp 12.5%-2 ml, Tab 0.15 )- low-molecular inductor of interferon
(Acridone-Acetic Acid)
Immunomodulating
Antiviral
Antinflammatory effects
Clinical uses:
Viral Hepatitis
Herpetic and Cytomegalovirus Infections
Chlamidiosis
HIV-infection (AIDS, stage IIA-IIIB)
Immunodeficiency conditions
25
26.
Inerferon-α (Laferon) – amp. 1 and 3 million IU or SC,amp. 100,000 IU – intranasally
Mechanism of action:
direct antiproliferative action against tumor cells or
viral cells to inhibit replication and modulation of
host immune response by:
enhancing phagocytic activity of macrophages
augmenting specific cytotoxicity of
lymphocytes for target cells.
26
27.
Clinical uses:Neoplasms
Chronic Myelogenous Leukemia
Malignant Melanoma and Kaposi’s Sarcoma
Renal Cell Carcinoma
T-cell Leukemia
Hepatitis B and C
Multiplied Sclerosis
Acute Respiratory Virus Infection
27
28.
BCG (Bacille Calmette-Guerin) vaccine-viable strain of Mycobacterium bovis
-nonspecific immunostimulant
-has been successful only in intravesical therapy for
Superficial Bladder Cancer.
BCG appears to act via activation of macrophages
to make them more effective killer cells
28










 medicine
medicine