Similar presentations:
Acute and Chronic pyelonephritis
1. JSC “Astana Medical University” Department of Internal Diseases №1 IWS Acute and Chronic pyelonephritis
Checked by: Baydurin S.A.Prepared by: Issabayeva A.
463 GM
Astana, 2018
2.
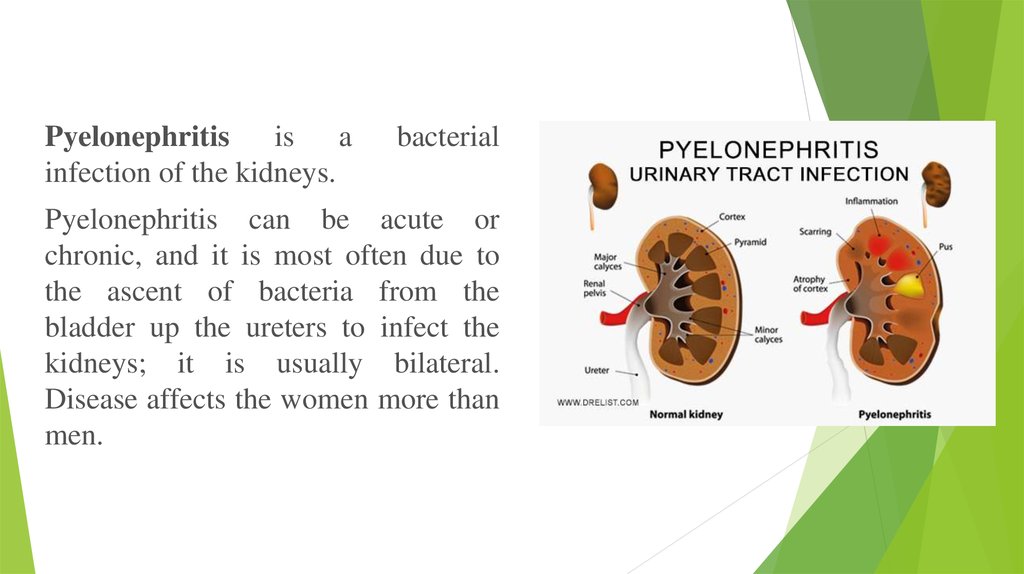
Pyelonephritis is ainfection of the kidneys.
bacterial
Pyelonephritis can be acute or
chronic, and it is most often due to
the ascent of bacteria from the
bladder up the ureters to infect the
kidneys; it is usually bilateral.
Disease affects the women more than
men.
3.
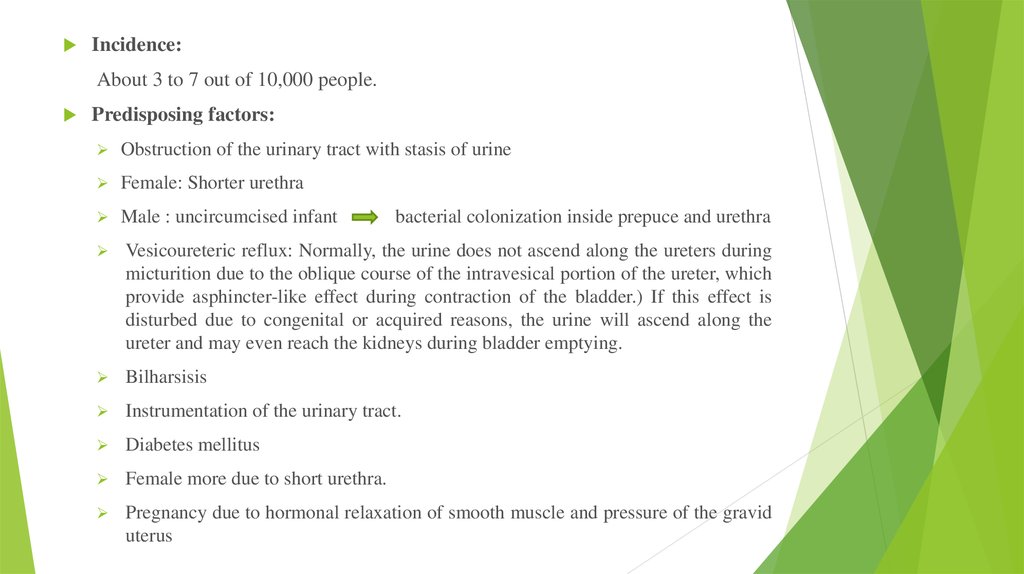
Incidence:About 3 to 7 out of 10,000 people.
Predisposing factors:
Obstruction of the urinary tract with stasis of urine
Female: Shorter urethra
Male : uncircumcised infant
bacterial colonization inside prepuce and urethra
Vesicoureteric reflux: Normally, the urine does not ascend along the ureters during
micturition due to the oblique course of the intravesical portion of the ureter, which
provide asphincter-like effect during contraction of the bladder.) If this effect is
disturbed due to congenital or acquired reasons, the urine will ascend along the
ureter and may even reach the kidneys during bladder emptying.
Bilharsisis
Instrumentation of the urinary tract.
Diabetes mellitus
Female more due to short urethra.
Pregnancy due to hormonal relaxation of smooth muscle and pressure of the gravid
uterus
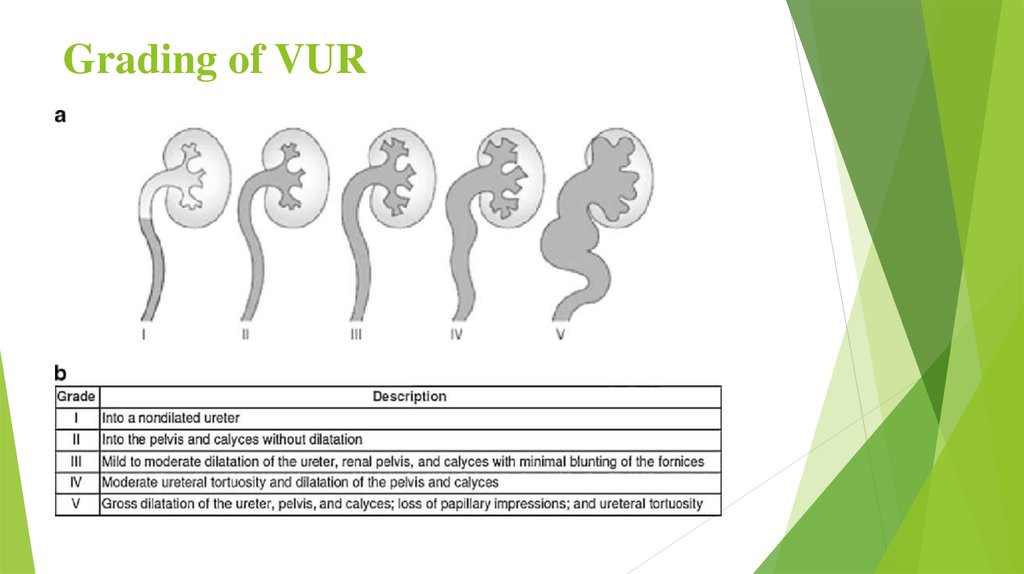
4. Grading of VUR
5.
Causative organisms:Gram negative organism: E.coli (common), Proteus mirabilis,
Citrobacter, klebsiella, enterobacter, proteus pseudomonas
aeruginosa;
Gram positive organism, Staph.saprophyticus, Staph.epidermidis
enterococcus, Corynebacteria and lactobacilli.
Routes of infection:
Ascending infection from the lower urinary tract.
Lymphatic spread from the intestinal tract.
Blood borne infection complicating boils or carbuncles.
Pathology:
Acute pyelonephritis
Chronic pyelonephritis
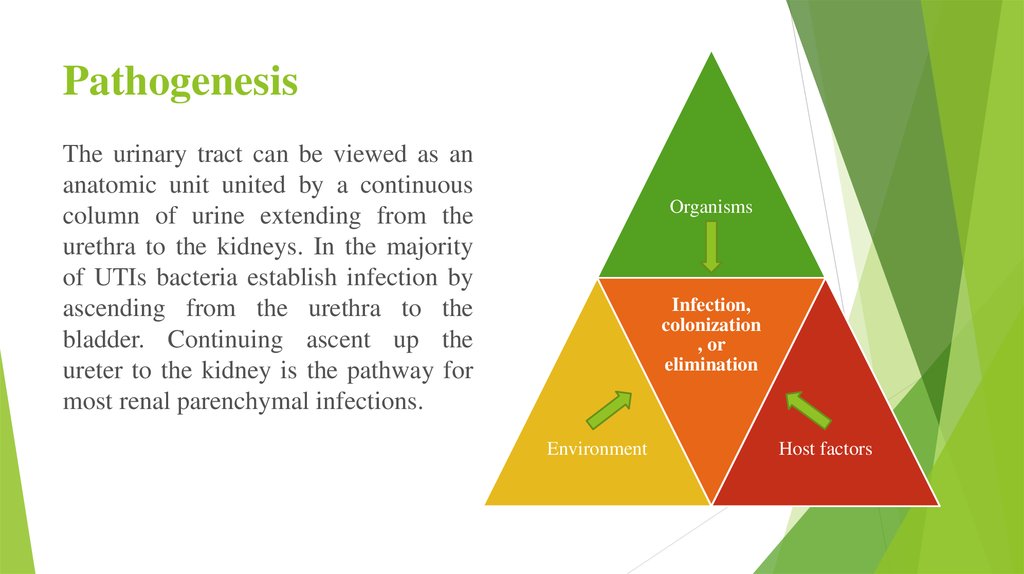
6. Pathogenesis
The urinary tract can be viewed as ananatomic unit united by a continuous
column of urine extending from the
urethra to the kidneys. In the majority
of UTIs bacteria establish infection by
ascending from the urethra to the
bladder. Continuing ascent up the
ureter to the kidney is the pathway for
most renal parenchymal infections.
Organisms
Infection,
colonization
, or
elimination
Environment
Host factors
7.
8. Signs and symptoms
Signs and symptoms of a kidney infection might include:Fever
Chills
Back, side (flank) or groin pain
Abdominal pain
Frequent urination
Strong, persistent urge to urinate
Burning sensation or pain when urinating
Nausea and vomiting
Pus or blood in your urine (hematuria)
Urine that smells bad or is cloudy
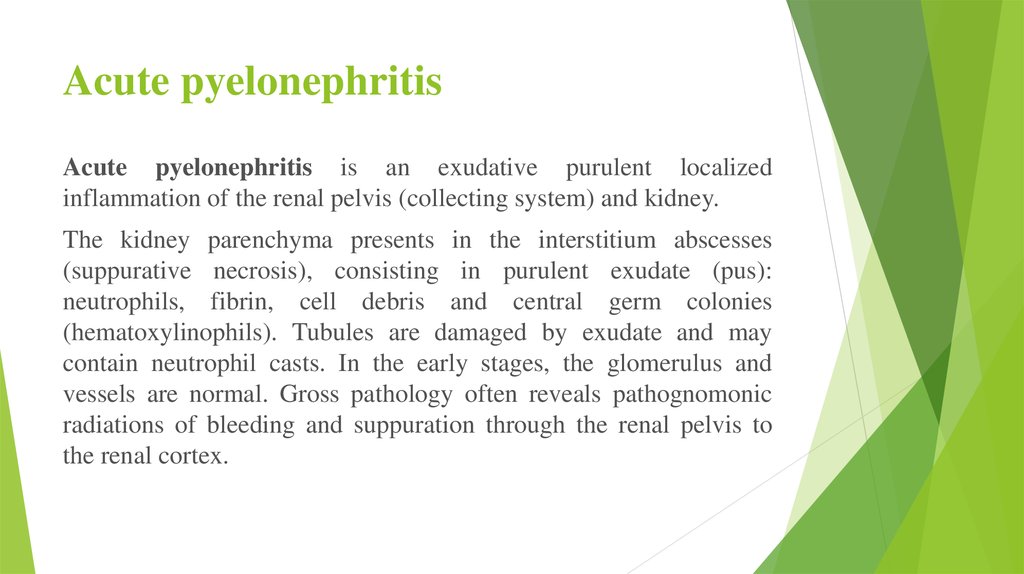
9. Acute pyelonephritis
Acute pyelonephritis is an exudative purulent localizedinflammation of the renal pelvis (collecting system) and kidney.
The kidney parenchyma presents in the interstitium abscesses
(suppurative necrosis), consisting in purulent exudate (pus):
neutrophils, fibrin, cell debris and central germ colonies
(hematoxylinophils). Tubules are damaged by exudate and may
contain neutrophil casts. In the early stages, the glomerulus and
vessels are normal. Gross pathology often reveals pathognomonic
radiations of bleeding and suppuration through the renal pelvis to
the renal cortex.
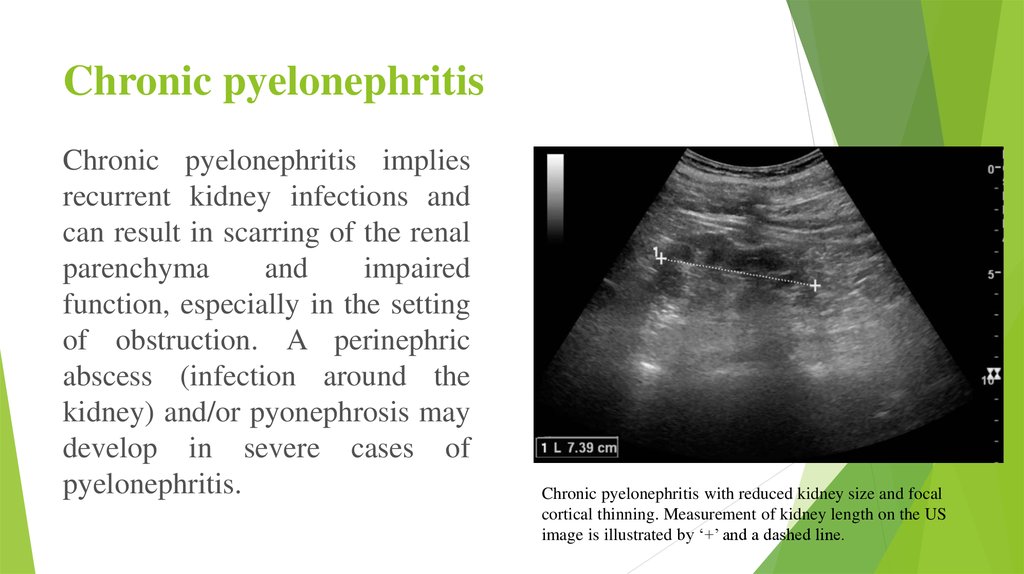
10. Chronic pyelonephritis
Chronic pyelonephritis impliesrecurrent kidney infections and
can result in scarring of the renal
parenchyma
and
impaired
function, especially in the setting
of obstruction. A perinephric
abscess (infection around the
kidney) and/or pyonephrosis may
develop in severe cases of
pyelonephritis.
Chronic pyelonephritis with reduced kidney size and focal
cortical thinning. Measurement of kidney length on the US
image is illustrated by ‘+’ and a dashed line.
11.
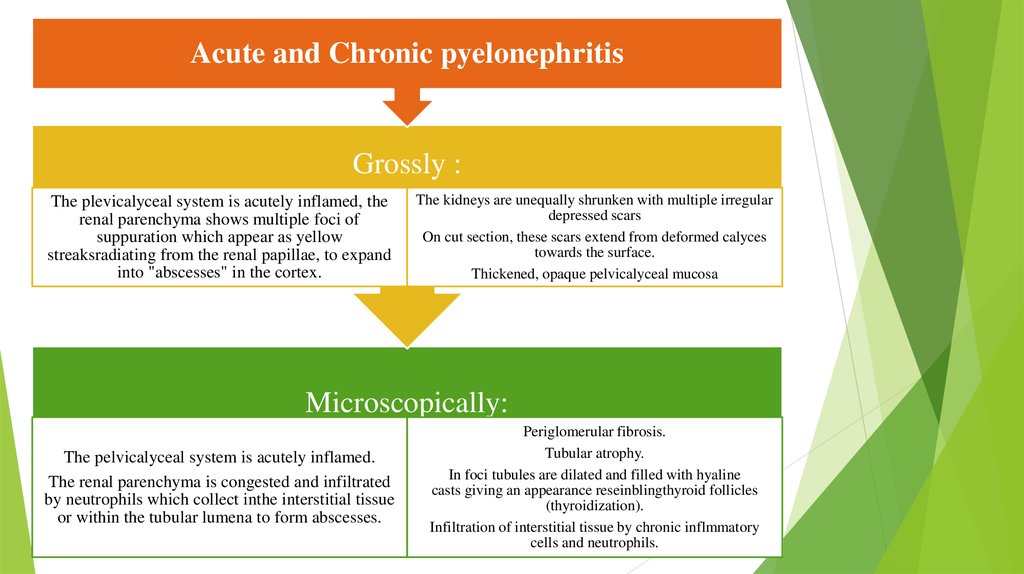
Acute and Chronic pyelonephritisGrossly :
The plevicalyceal system is acutely inflamed, the
renal parenchyma shows multiple foci of
suppuration which appear as yellow
streaksradiating from the renal papillae, to expand
into "abscesses" in the cortex.
The kidneys are unequally shrunken with multiple irregular
depressed scars
On cut section, these scars extend from deformed calyces
towards the surface.
Thickened, opaque pelvicalyceal mucosa
Microscopically:
The pelvicalyceal system is acutely inflamed.
The renal parenchyma is congested and infiltrated
by neutrophils which collect inthe interstitial tissue
or within the tubular lumena to form abscesses.
Periglomerular fibrosis.
Tubular atrophy.
In foci tubules are dilated and filled with hyaline
casts giving an appearance reseinblingthyroid follicles
(thyroidization).
Infiltration of interstitial tissue by chronic inflmmatory
cells and neutrophils.
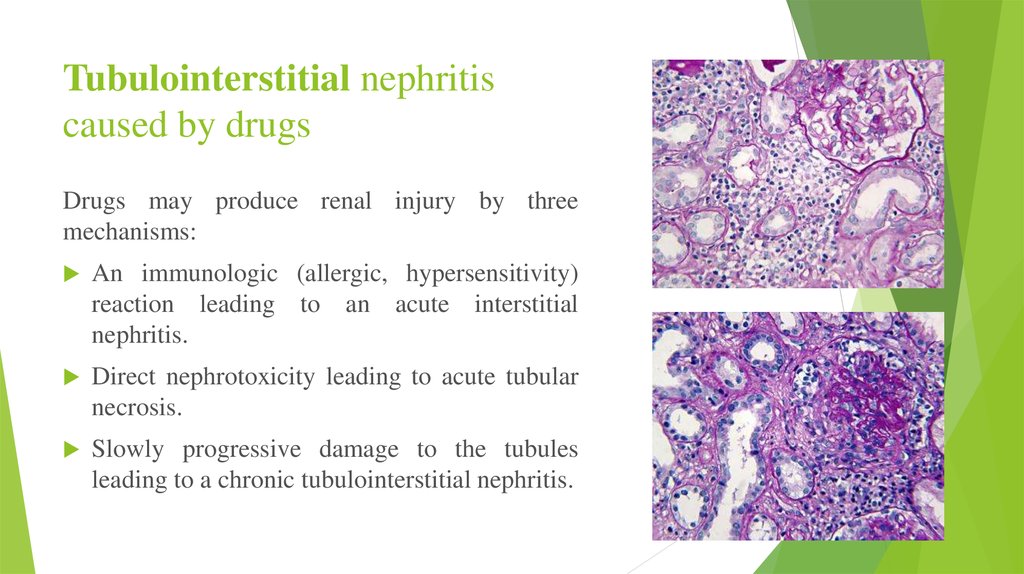
12. Tubulointerstitial nephritis caused by drugs
Drugs may produce renal injury by threemechanisms:
An immunologic (allergic, hypersensitivity)
reaction leading to an acute interstitial
nephritis.
Direct nephrotoxicity leading to acute tubular
necrosis.
Slowly progressive damage to the tubules
leading to a chronic tubulointerstitial nephritis.
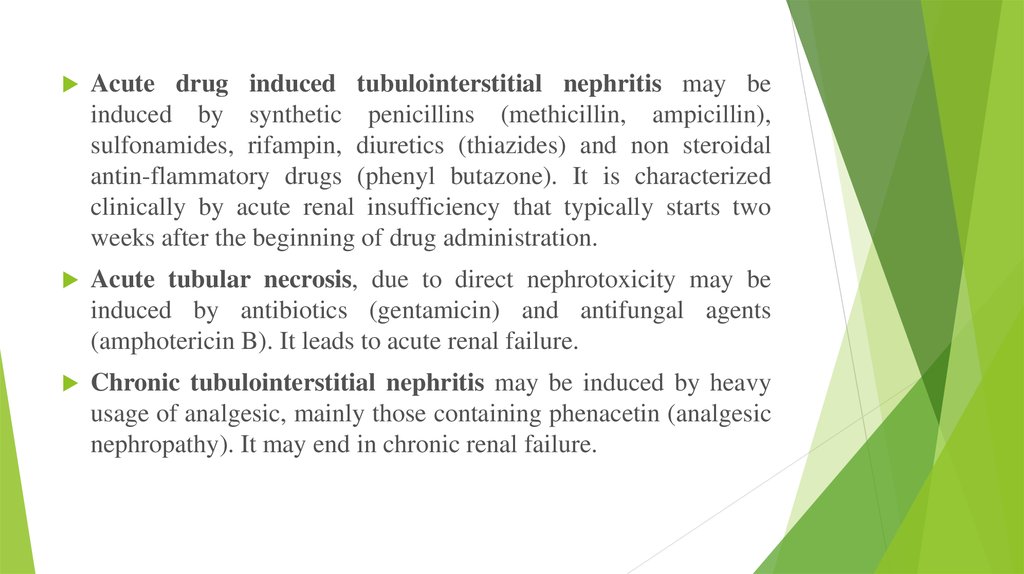
13.
Acute drug induced tubulointerstitial nephritis may beinduced by synthetic penicillins (methicillin, ampicillin),
sulfonamides, rifampin, diuretics (thiazides) and non steroidal
antin-flammatory drugs (phenyl butazone). It is characterized
clinically by acute renal insufficiency that typically starts two
weeks after the beginning of drug administration.
Acute tubular necrosis, due to direct nephrotoxicity may be
induced by antibiotics (gentamicin) and antifungal agents
(amphotericin B). It leads to acute renal failure.
Chronic tubulointerstitial nephritis may be induced by heavy
usage of analgesic, mainly those containing phenacetin (analgesic
nephropathy). It may end in chronic renal failure.
14. Diagnostics
Physical examination:- soreness in palpation in the area of the projection of the kidneys;
- arterial hypertension.
Laboratory research:
- bacteriuria 105;
- leukocyturia;
- erythrocyturia;
- proteinuria (β2-microglobulin);
- reduction of the concentration function;
- GFR;
- anemia
15. Imaging studies
If a kidney stone is suspected (e.g. on the basis of characteristic colicky pain or the presence of adisproportionate amount of blood in the urine), a kidneys, ureters, and bladder x-ray may assist in
identifying radioopaque stones. Where available, a noncontrast helical CT scan with 5 millimeter
sections is the diagnostic modality of choice in the radiographic evaluation of suspected
nephrolithiasis. All stones are detectable on CT scans except very rare stones composed of certain
drug residues in the urine. In patients with recurrent ascending urinary tract infections, it may be
necessary to exclude an anatomical abnormality, such as vesicoureteral reflux or polycystic kidney
disease. Investigations used in this setting include kidney ultrasonography or voiding
cystourethrography. CT scan or kidney ultrasonography is useful in the diagnosis of
xanthogranulomatous pyelonephritis; serial imaging may be useful for differentiating this
condition from kidney cancer.
Ultrasound findings that indicate pyelonephritis are enlargement of the kidney, edema in the renal
sinus or parenchyma, bleeding, loss of corticomedullary differentiation, abscess formation, or an
areas of poor blood flow on doppler ultrasound. However, ultrasound findings are seen in only
20% to 24% of people with pyelonephritis.
A DMSA scan is a radionuclide scan that uses dimercaptosuccinic acid in assessing the kidney
morphology. It is now the most reliable test for the diagnosis of acute pyelonephritis.
16.
Purpose of treatment: consists in elimination of infectious and inflammatory process,possible only at restoration of outflow of urine and sanitation of urinary tract.
Indications for hospitalization: In acute secondary pyelonephritis, urgent hospitalization
is necessary in the urological department in connection with the possible need for an
urgent open surgery to prevent severe, life-threatening complications (toxic shock). In
acute primary pyelonephritis, hospitalization is also desirable, since a concealed violation
is possible outflow of urine. In addition, with this form of the disease, the serous phase can
quickly progress to purulent, requiring urgent surgical treatment. In extreme cases, with
confidence in the diagnosis of acute primary pyelonephritis, antibiotic therapy can also be
started on an outpatient basis.
Unambiguously patients need the emergency hospitalization:
▪ with acute pyelonephritis of a single or only functioning kidney;
▪ exacerbation of chronic pyelonephritis and signs of renal insufficiency;
▪ acute pyelonephritis on the background of diabetes mellitus or immunodeficiency;
▪ suspected purulent process in the kidney;
▪ acute pyelonephritis with ineffective antibiotic therapy.
17.
Detoxification therapy:plentiful drink;
parenteral infusion therapy in the form of solutions of glucose 5-10% and NaCl 0.45% is indicated only
for dyspepsia (nausea, vomiting, diarrhea).
Antibiotic therapy: The basic principle is the early and long-term appointment of antimicrobial agents in
strict accordance with the sensitivity to them microflora inoculated from the urine, the alternation of
antimicrobials or their combined use.
1. Gram-positive: semi-synthetic penicillins (ampicillin, amoxicillin + clavulanic acid).
2. Gram-negative: co-trimoxazole + fluoroquine (ciprofloxacin, ofloxacin, norfloxacin).
3. Nosocomial infection: aminoglycosides (gentamicin) + cephalosporins (ceftriaxone, cefotaxime,
ceftazidime).
4. Reserve antibiotics: imipenem, amikacin.
5. Uroantiseptics: nitrofurans (furagin).
The duration of antibiotic therapy is determined by the severity of the infection process, the presence of
complications.
In some cases, supportive therapy with other antibacterial agents - uroseptics (furagin 1-2 mg / kg / night, cotrimoxazole - 120-240 mg per night) is necessary.
In parallel, it is necessary to carry out antifungal therapy (itraconazole), correction of intestinal microflora,
immunostimulant therapy.
18. The list of basic medicines:
1. Amoxicillin + clavulanic acid, coated tablets 250 mg / 125 mg, 500 mg / 125 mg, 875mg / 125 mg, powder for the preparation of a solution for intravenous administration in
vials 500 mg / 100 mg
2. Ampicillin - 500 mg, fl.
3. Ceftriaxone 500 mg, 1 g, fl.
4. Imipenems
5. Fluoroquine (ciprofloxacin, ofloxacin, norfloxacin)
6. Co-trimoxazole - 120 mg, 480 mg, tab.
7. Cefuroxime axetil - 125 mg, 250 mg, tablets, suspensions
8. Gentamicin 40 mg, 80 mg, fl.
9. Furagin 50 mg, tab.
10. Enalapril 5 mg, 10 mg, tab.
19. Complications
If left untreated, a kidney infection can lead to potentially seriouscomplications, such as:
Kidney scarring. This can lead to chronic kidney disease, high blood
pressure and kidney failure.
Blood poisoning (septicemia). Your kidneys filter waste from your blood
and return your filtered blood to the rest of your body. Having a kidney
infection can cause the bacteria to spread through your bloodstream.
Pregnancy complications. Women who develop a kidney infection during
pregnancy may have an increased risk of delivering low birth weight
babies.




 medicine
medicine