Similar presentations:
Physical examination of the genitourinary tract: Introduction
1.
Physical Examination ofthe Genitourinary Tract:
Introduction
2.
The history will suggest whether acomplete or partial examination is
indicated.
3. Examination of the Kidneys Inspection
4. Examination of the Kidneys Inspection
The presence and persistence ofindentations in the skin from lying on
wrinkled sheets suggest edema of the skin
secondary to perinephric abscess.
5. Palpation
The kidneys lie rather high under the diaphragmand lower ribs and are therefore well protected
from injury.
6. Palpation
Thekidney is lifted by one hand in the
costovertebral angle.
7. Palpation
On deep inspiration, the kidney movesdownward; when it is lowest, the other hand
is pushed firmly and deeply beneath the
costal margin in an effort to trap the kidney
below that point. If this is successful, the
anterior hand can palpate the size, shape,
and consistency of the organ as it slips back
into its normal position.
8. Palpation
The kidney sometimes can be palpated bestwith the examiner standing behind the
seated patient.
9. Palpation
Anomalies were found in 0.5% of 11,000newborns.
10. Palpation
An enlarged renal mass suggests compensatoryhypertrophy (if the other kidney is absent or
atrophic), hydronephrosis, tumor, cyst, or
polycystic disease.
11. Palpation
Tumors may have the consistency of normaltissue; they may also be nodular.
12. Palpation
This may be elicited by palpation or, moresharply, by percussion over that area.
13. Percussion
At times, a greatly enlarged kidney cannot be felton palpation, particularly if it is soft. This can be
true of hydronephrosis.
14. Transillumination
Transillumination may prove quite helpful inchildren under age 1 year who present with a
suprapubic or flank mass.
15. Transillumination
The fiberoptic light cord, used to illuminatevarious optical instruments, is an excellent
source of cold light.
16. Differentiation of Renal & Radicular Pain
Differentiation of Renal &Radicular Pain
Radicular pain is commonly felt in the
costovertebral and subcostal areas.
17. Differentiation of Renal & Radicular Pain
Differentiation of Renal &Radicular Pain
Frequent causes are poor posture (scoliosis,
kyphosis), arthritic changes in the
costovertebral or costotransverse joints,
impingement of a rib spur on a subcostal
nerve, hypertrophy of costovertebral
ligaments pressing on a nerve, and
intervertebral disk disease.
18. Differentiation of Renal & Radicular Pain
Differentiation of Renal &Radicular Pain
Radicular pain may be noted as an
aftermath of a flank incision wherein a rib
may become dislocated, causing the costal
nerve to impinge on the edge of a ligament.
19. Differentiation of Renal & Radicular Pain
Differentiation of Renal &Radicular Pain
Radiculitis usually causes hyperesthesia of the
area of skin served by the irritated peripheral
nerve.
20. Auscultation
Bruits over the femoral arteries may be found inassociation with Leriche syndrome, which may
be a cause of impotence.
21. Examination of the Bladder
The bladder cannot be felt unless it ismoderately distended. In adults, if it is
percussible, it contains at least 150 mL of urine.
22. Examination of the Bladder
A sliding inguinal hernia containing somebladder wall can be diagnosed (when the
bladder is full) by compression of the scrotal
mass. The bladder will be found to distend
additionally.
23. Examination of the Bladder
Bimanual (abdominorectal or abdominovaginal)palpation may reveal the extent of a vesical
tumor.
To be successful, it must be done under
anesthesia.
24.
Examination of theExternal Male Genitalia
Penis
Inspection
25.
If the patient has not been circumcised, theforeskin should be retracted. This may reveal
tumor or balanitis as the cause of a foul
discharge.
26.
The scars of healed syphilis may be animportant clue. An active ulcer requires
bacteriologic or pathologic study (eg,
syphilitic chancre, epithelioma).
27.
Meatal stenosis is a common causeof bloody spotting in male infants.
28.
The position of the meatus should be noted. Itmay be located proximal to the tip of the glans
on either the dorsum (epispadias) or the
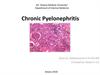
ventral surface (hypospadias).
29. Palpation
Palpation of the dorsal surface of the shaft mayreveal a fibrous plaque involving the fascial
covering of the corpora cavernosa.
30. Urethral Discharge
Urethral discharge is the most commoncomplaint referable to the male sex organ.
Gonococcal pus is usually profuse, thick, and
yellow or gray-brown.
31. Urethral Discharge
Although gonorrhea must be ruled out as thecause of a urethral discharge, a significant
percentage of such cases are found to be
caused by chlamydiae.
32. Urethral Discharge
Bloody discharge should suggestthe possibility of a foreign body in
the urethra (male or female),
urethral stricture, or tumor.
Urethral discharge must always be
sought before the patient is asked
to void.
33. Scrotum
Angioneurotic edema and infectionsand inflammations of the skin of the
scrotum are not common.
34.
Elephantiasis of the scrotum is caused byobstruction to lymphatic drainage. It is endemic
in the tropics and is due to filariasis.
35. Testis
The testes should be carefully palpated with thefingers of both hands.
36. Testis
A hydrocele will cause the intrascrotalmass to glow red.
37. Testis
About 10% of tumors are associated with asecondary hydrocele that may have to be
aspirated before definitive palpation can be
done.
38. Testis
The atrophic testis (followingpostoperative orchiopexy, mumps
orchitis, or torsion of the spermatic
cord) may be flabby and at times
hypersensitive but is usually firm and
hyposensitive.
39. Epididymis
The epididymis is sometimes ratherclosely attached to the posterior
surface of the testis, and at other
times it is quite free of it.
40. Epididymis
In the acute stage of epididymitis, the testisand epididymis are indistinguishable by
palpation; the testicle and epididymis may
be adherent to the scrotum, which is
usually quite red.
41. Epididymis
Chronic painless induration should suggesttuberculosis or schistosomiasis, although
nonspecific chronic epididymitis is also a
possibility.
42. Spermatic Cord & Vas Deferens
Spermatic Cord & Vas DeferensA swelling in the spermatic cord may be cystic
(e.g., hydrocele or hernia) or solid (e.g.,
connective tissue tumor).
43. Spermatic Cord & Vas Deferens
Spermatic Cord & Vas DeferensCareful palpation of the vas deferens
may reveal thickening (e.g., chronic
infection), fusiform enlargements (the
"beading" caused by tuberculosis), or
even absence of the vas.
44. Spermatic Cord & Vas Deferens
Spermatic Cord & Vas DeferensWhen a male patient stands, a mass
of dilated veins (varicocele) may be
noted behind and above the testis.
45. Testicular Tunics & Adnexa
Testicular Tunics & AdnexaHydroceles are usually cystic but on occasion
are so tense that they simulate solid tumors.
Transillumination makes the differential
diagnosis. They may develop secondary to
nonspecific acute or tuberculous epididymitis,
trauma, or tumor of the testis.
The latter is a distinct possibility if hydrocele
appears spontaneously between the ages of 18
and 35. It should be aspirated to permit careful
palpation of underlying structures.
46. Testicular Tunics & Adnexa
Testicular Tunics & AdnexaHydrocele usually surrounds the testis
completely.
47. Examination of the Female Genitalia
Vaginal ExaminationDiseases of the female genital tract may involve
the urinary organs secondarily, thereby making a
thorough gynecologic examination essential.
48. Inspection
In newborns and children especially, thevaginal vestibule should be inspected for a
single opening (common urogenital sinus),
labial fusion, split clitoris and lack of fusion
of the anterior fourchette (epispadias), or
hypertrophied clitoris and scrotalization of
the labia majora (adrenogenital syndrome).
49. Inspection
Biopsy is indicated if a malignant tumorcannot be ruled out.
50. Inspection
The diagnosis of senile vaginitis (and urethritis)is established by staining a smear of the vaginal
epithelium with Lugol's solution.
51. Inspection
Multiple painful small ulcers or blisterlike lesionsmay be noted; these probably represent herpes
virus type 2 infection, which may have serious
sequels.
52. Inspection
The presence of skenitis and bartholinitis mayreveal the source of persistent urethritis or
cystitis.
The condition of the vaginal wall should be
observed.
Bacteriologic study of the secretions may be
helpful.
Urethrocele and cystocele may cause residual
urine and lead to persistent infection of the
bladder.
53. Inspection
They are often found in association with stressincontinence.
54. Palpation
A soft mass found in this area could be aurethral diverticulum.
Pressure on such a lesion may cause pus to
extrude from the urethra.
55. Palpation
A stone in the lower ureter may bepalpable. Evidence of enlargement of the
uterus (e.g., pregnancy, myomas) or
diseases or inflammations of the colon or
adnexa may afford a clue to the cause of
urinary symptoms (e.g., compression of a
ureter by a malignant ovarian tumor,
endometriosis, or diverticulitis of the
sigmoid colon adherent to the bladder).
56. Palpation
Rectal examination may afford furtherinformation and is the obvious route of
examination in children and virgins.
57. Rectal Examination in Males
Sphincter & Lower RectumThe estimation of sphincter tone is of great
importance.
58.
The same is true for a spastic analsphincter.
59. Prostate
A specimen of urine for routine analysis shouldbe collected before the rectal examination is
made.
60. Size
The average prostate is about 4 cm in length andwidth. It is widest superiorly at the bladder neck.
61. Consistency
Normally, the consistency of the gland is similarto that of the contracted thenar eminence of the
thumb (with the thumb completely opposed to
the little finger).
62. Consistency
Generally speaking, nodules caused byinfection are raised above the surface of
the gland.
63. Consistency
At their edges, the induration graduallyfades to the normal softness of surrounding
tissue.
64.
The prostate-specific antigen (PSA) level can behelpful if elevated. Transrectal ultrasound-guided
biopsy can be diagnostic.
65. Mobility
The prostate should be routinelymassaged in adults and its secretion
examined microscopically.
66. Mobility
It should not be massaged, however, in thepresence of an acute urethral discharge, acute
prostatitis, or acute prostatocystitis; in men near
the stage of complete urinary retention (because
it may precipitate complete retention); or in men
suffering from obvious cancer of the gland.
Even without symptoms, massage is necessary,
for prostatitis is commonly asymptomatic.
Diagnosis and treatment of such silent disease
is important in preventing cystitis and
epididymitis.
67. Massage & Prostatic Smear
Massage & Prostatic SmearCopious amounts of secretion may be obtained
from some prostate glands and little or none
from others.
68. Massage & Prostatic Smear
Massage & Prostatic SmearMicroscopic examination of the secretion is
done under low-power magnification. Normal
secretion contains numerous lecithin bodies,
which are refractile, like red cells, but much
smaller than red cells.
69. Massage & Prostatic Smear
Massage & Prostatic SmearThe presence of large numbers of pus cells is
pathologic and suggests the diagnosis of
prostatitis.
70. Massage & Prostatic Smear
Massage & Prostatic SmearOn occasion, it may be necessary to obtain
cultures of prostatic secretion in order to
demonstrate nonspecific organisms, tubercle
bacilli, gonococci, or chlamydiae.
71. Seminal Vesicles
Palpation of the seminal vesicles should beattempted. The vesicles are situated under the
base of the bladder and diverge from below
upward.
72. Seminal Vesicles
Stripping of the seminal vesicles should be donein association with prostatic massage, for the
vesicles are usually infected when prostatitis is
present.
73. Lymph Nodes
It should be remembered thatgeneralized lymphadenopathy
usually occurs early in human
immunodeficiency syndrome (HIV).
74. Inguinal & Subinguinal Lymph Nodes
Inguinal & Subinguinal LymphNodes
Such diseases include chancroid,
syphilitic chancre, lymphogranuloma
venereum, and, on occasion,
gonorrhea.
75. Inguinal & Subinguinal Lymph Nodes
Inguinal & Subinguinal LymphNodes
Malignant tumors (squamous cell
carcinoma) involving the penis, glans,
scrotal skin, or distal urethra in women
metastasize to the inguinal and
subinguinal nodes.
76. Other Lymph Nodes
Tumors of the testis and prostate may involvethe left supraclavicular nodes. Tumors of the
bladder and prostate typically metastasize to the
internal iliac, external iliac, and preaortic nodes,
although only occasionally are they so large as
to be palpable.
77. Neurologic Examination
A careful neurologic survey may uncoversensory or motor impairment that will account for
residual urine (neuropathic bladder) or
incontinence.
78. Neurologic Examination
The bulbocavernosus reflex is elicited byplacing a finger in the patient's rectum and
squeezing the glans penis or clitoris or by
jerking on an indwelling Foley catheter.
The normal reflex is contraction of the anal
sphincter and bulbocavernosus muscles in
response to these maneuvers.
79. Neurologic Examination
It is wise, particularly in children, to seek adimple over the lumbosacral area.
80. NONSPECIFIC INFLAMMATORY DISEASES OF GENITOURINARY ORGANS
81. Nonspecific inflammatory diseases of genitourinary organs:
Acutepyelonephritis
Chronic pyelonephritis
82. Nonspecific inflammatory diseases of genitourinary organs:
CystitisParacystitis
Urethritis
83. Nonspecific inflammatory diseases of genitourinary organs:
ProstatitisVesiculitis
84. Pyelonephritis
is nonspecific inflammatoryinfectious process, in which the
parenchyma and pelvis of the
kidney simultaneously or
sequentially are affected.
85. Pyelonephritis
Patients with acute pyelonephritispresent with chills, fever, and
costovertebral angle tenderness.
They often have accompanying
lower-tract symptoms such as
dysuria, frequency, and urgency.
86. Pyelonephritis
Sepsis may occur, with 20–30% of allsystemic sepsis resulting from a urine
infection.
87. Pyelonephritis
Bacteriaare cultured from the urine when the
culture is obtained before antibiotic treatment is
instituted.
88. Pyelonephritis
The infection penetrates into thekidney by two routes:
-
Hematogenous
89. Pyelonephritis
Of the local factors contributing toorigination pyelonephritis most
often is the disturbance of outflow
of urine (reason – different
anomalies of the kidneys and
urinary paths)
90. Factors, which promote development of acute pyelonephritis
Stonesof the kidney
Ureter and urethra
91. The triad of symptoms of acute pyelonephritis
Highbody temperature
Pain in the lumbar area
92. Acute Pyelonephritis
Of great value for diagnostics arethe laboratory methods of
investigations
93. Acute Pyelonephritis
Radiological researches in patientswith AP are necessary to exclude
accompanying diseases, which
promote development of infectious
process, and to specify the character
of pathological changes in serious
cases
94. Acute Pyelonephritis
Treatmentof primary AP in most cases is
conservative
95. Acute Pyelonephritis treatment
The management of acutepyelonephritis depends on the
severity of the infection.
96. Acute Pyelonephritis treatment
Empiric therapy with intravenousampicillin and aminoglycosides is
effective against a broad range of
uropathogens, including enterococci
and Pseudomonas species.
Alternatively, amoxicillin with clavulanic
acid or a third-generation
cephalosporin can be used.
97. Acute Pyelonephritis treatment
Fever from acute pyelonephritis may persistfor several days despite appropriate
therapy.
98. Acute Pyelonephritis treatment
In patients who are not severely ill, outpatienttreatment with oral antibiotics is appropriate. For
adults, treatment with fluoroquinolones or TMPSMX is well tolerated and effective.
99. Vesicoureteral Reflux
Approximately 50% of patientswith the infection of urinary paths
have
Vesicoureteral Reflux – is a
backflow of urine from the bladder
to the ureter and kidney
100. Classification of Vesicoureteral Reflux according to its grades:
GradeI: a contrast drug fills the ureter, but
does not get into the renal pelvis.
101. Classification of Vesicoureteral Reflux according to its grades:
GradeIV: moderate dilatation and/or
tortuousity of the ureter with moderate
dilatation of the renal pelvis and calyces
102. Treatment of Vesicoureteral Reflux
Antibacterial treatment is directed toprevention of development infection
of the urinary paths. Routinely
Sulphonamides and Nitrofurans are
prescribed.
103. Treatment of Vesicoureteral Reflux
-Indications for operative treatment:
Inefficient conservative treatment
104. Secondary Acute Pyelonephritis
Differs from primary in a clinicalpicture by its greater expressivness of
sings of local nature that allows faster
and easier to recognize acute
pyelonephritis
105. Cause of Secondary Acute Pyelonephritis
Stonesof the kidney and ureter
106. Chronic Pyelonephritis
The diagnosis is made by radiologicor pathologic examination rather than
from clinical presentation.
107. Chronic Pyelonephritis
Many individuals with chronic pyelonephritishave no symptoms, but they may have a
history of frequent UTIs.
108. Chronic Pyelonephritis
Main X-ray signs are:-
Deformations of the pyelocaliceal system
109. Chronic Pyelonephritis
-Main X-ray signs are:
Changes of dimensions and contours of
the kidneys
110. Chronic Pyelonephritis
Renal scarring induced by UTIs is rarely seenin adult kidneys.
111. Chronic Pyelonephritis
In these patients, urinalysis may showleukocytes or proteinuria but is likely to
be normal.
112. Treatment of Chronic Pyelonephritis
Removalof causes produsing the
disturbance of urine passage of renal
circuation, venous in particular
113. Chronic Pyelonephritis management
The management of chronic pyelonephritisis somewhat limited because renal
damage incurred by chronic pyelonephritis
is not reversible.
114. Chronic Pyelonephritis management
Long-term use of continuous prophylacticantibiotic therapy may be required to limit
recurrent UTIs and renal scarring.
115. Chronic Pyelonephritis management
Rarely, removal of theaffected kidney may be
necessary due to
hypertension or having a
large stone burden in a
nonfunctioning kidney.
116. Necrosis of Renal Papillae
117. Bacteriemic Shock
118. Pyonephrosis
means the final stage of specific ornonspecific purulent-destructive
inflammatory lesion of the kidney. The
pyonephrotic kidney represents the organ,
exposed to purulent destruction, consisting
of separate cavities, filled with pus, urine
and products of nephrolysis.
119. Apostematous Pyelonephritis
represents a purulentinflammatory process with theformation of numerous, smallsized pustules (apostemas)
predominantly in the renal cortex.
120. Renal Abscesses
Renal abscesses result from a severeinfection that leads to liquefaction of
renal tissue; this area is subsequently
sequestered, forming an abscess.
They can rupture out into the
perinephric space, forming
perinephric abscesses.
121. Renal Abscesses
When the abscesses extend beyond theGerota's fascia, paranephric abscesses
develop.
122. Renal Abscesses
With the development of effectiveantibiotics and better management of
diseases such as diabetes and renal
failure, renal/perinephric abscesses
due to gram-positive bacteria are less
prevalent; those caused by E coli or
Proteus species are becoming more
common.
123. Renal Abscesses
Abscesses that form in the renal cortexare likely to arise from hematogenous
spread, whereas those in the
corticomedullary junction are caused
from gram-negative bacteria in
conjunction with some other underlying
urinary tract abnormalities, such as
stones or obstruction.
124. Renal Abscesses management
The appropriate management of renal abscessfirst must include appropriate antibiotic therapy.
125. Renal Abscesses management
The drained fluid should be culturedfor the causative organisms.
126. Renal Abscesses management
If the abscess still does not resolve, then opensurgical drainage or nephrectomy may be
necessary.
127. Pyonephrosis
Pyonephrosis refers to bacterial infection ofa hydronephrotic, obstructed kidney, which
leads to suppurative destruction of the renal
parenchyma and potential loss of renal
function. Because of the extent of the
infection and the presence of urinary
obstruction, sepsis may rapidly ensue,
requiring rapid diagnosis and management.
128. Pyonephrosis
Patients with pyonephrosis are usuallyvery ill, with high fever, chills, and flank
pain.
129. Pyonephrosis management
Management of pyonephrosis includesimmediate institution of antibiotic therapy
and drainage of the infected collecting
system.
130. Pyonephrosis management
Extensive manipulation may rapidlyinduce sepsis and toxemia.
131. Pyonephrosis management
In the ill patient, drainage of the collectingsystem with a percutaneous nephrostomy
tube is preferable.
132. Acute Cystitis
The most common causative agent ofcystitis is E.Coli, then
Staphylococcus, Enterococcus,
Proteus, Streptococcus, etc.
133. Acute Cystitis
Acute cystitis refers to urinary infectionof the lower urinary tract, principally the
bladder.
134. Acute Cystitis
The diagnosis is made clinically. Inchildren, the distinction between upper and
lower UTI is important.
135. Acute Cystitis
Patients with acute cystitis present withirritative voiding symptoms such as dysuria,
frequency, and urgency.
136. Acute Cystitis
Urine culture is required to confirmthe diagnosis and identify the
causative organism.
137. Acute Cystitis
E coli causes most of the acutecystitis. Other gram-negative
(Klebsiella and Proteus spp.) and
gram-positive (Staphylococcus
saprophyticus and enterococci)
bacteria are uncommon
pathogens.
138. Acute Cystitis Management
Trimethoprim-sulfamethoxazole andnitrofurantoin are less expensive and thus
are recommended for the treatment of
uncomplicated cystitis
139. Acute Cystitis Management
In adults and children, the duration oftreatment is usually limited to 3–5 days.
Longer therapy is not indicated.
140. Acute Cystitis Management
Resistance to penicillins andaminopenicillins is high and thus they are
not recommended for treatment.





















 medicine
medicine