Similar presentations:
Introductory/ Neuroimaging: What you need to know at 3 am And some cool stuff
1. Introductory Neuroimaging: What you need to know at 3 am And some cool stuff. . .
Kathleen Tozer, MD2. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
3. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
4. Which study? Acute change
• For acute mental status change, first study isALWAYS noncontrast head CT
• Brain MR:
– Stroke protocol (noncontrast)
– ICH protocol (with contrast)
– Tumor protocol (with contrast)
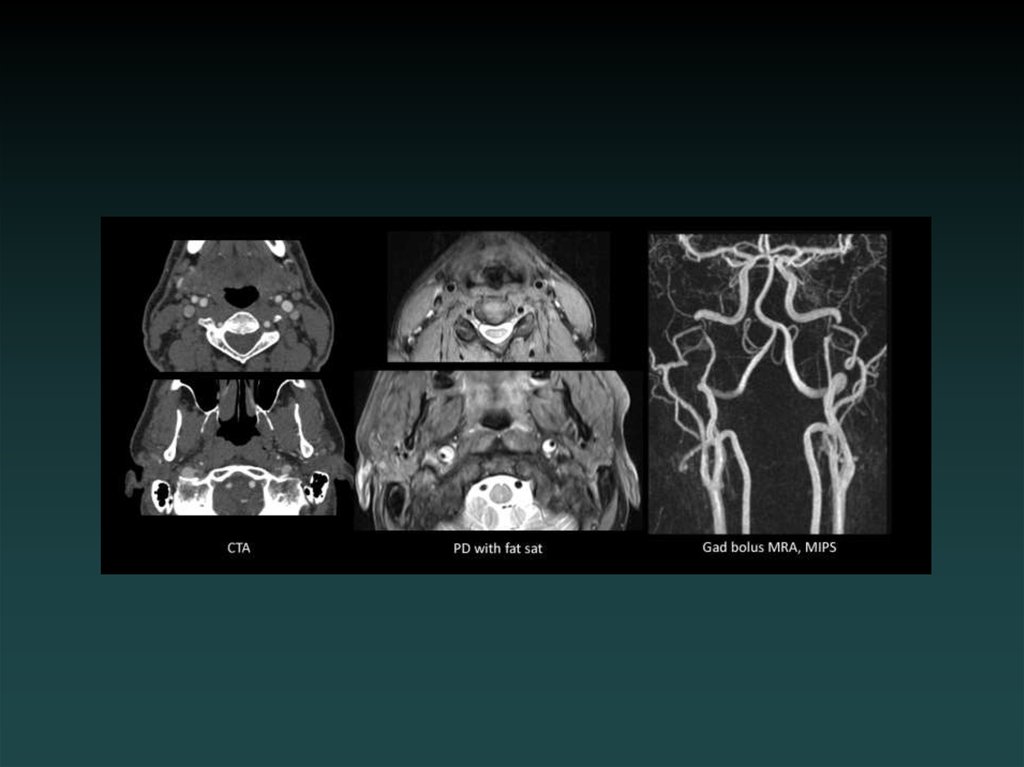
5. Which study? Vascular
• CTA:– Neck: Aortic arch through Circle of Willis.
– Head: Circle of Willis only
• MRA:
– Brain: noncontrast
– Neck: without and with contrast.
6. Regarding contrast:
• Iodinated contrast:– GFR > 60:
• in the clear
– GFR < 60:
• If acute, tread cautiously, especially if <30
• Hydration, mucomyst, Sodium bicarb protocol
• Decrease dose, Visipaque
– ESRD:
• Coordinate with hemodialysis
7. Regarding contrast:
• Gadolinium contrast:– GFR > 60:
• in the clear
– GFR 30-60:
• weigh risks.
• Consider noncontrast study first.
• Multihance
– GFR < 30:
• CONTRAINDICATED due to risk of NSF (nephrogenic systemic
fibrosis).
– Try noncontrast.
– Consult radiology for alternative studies.
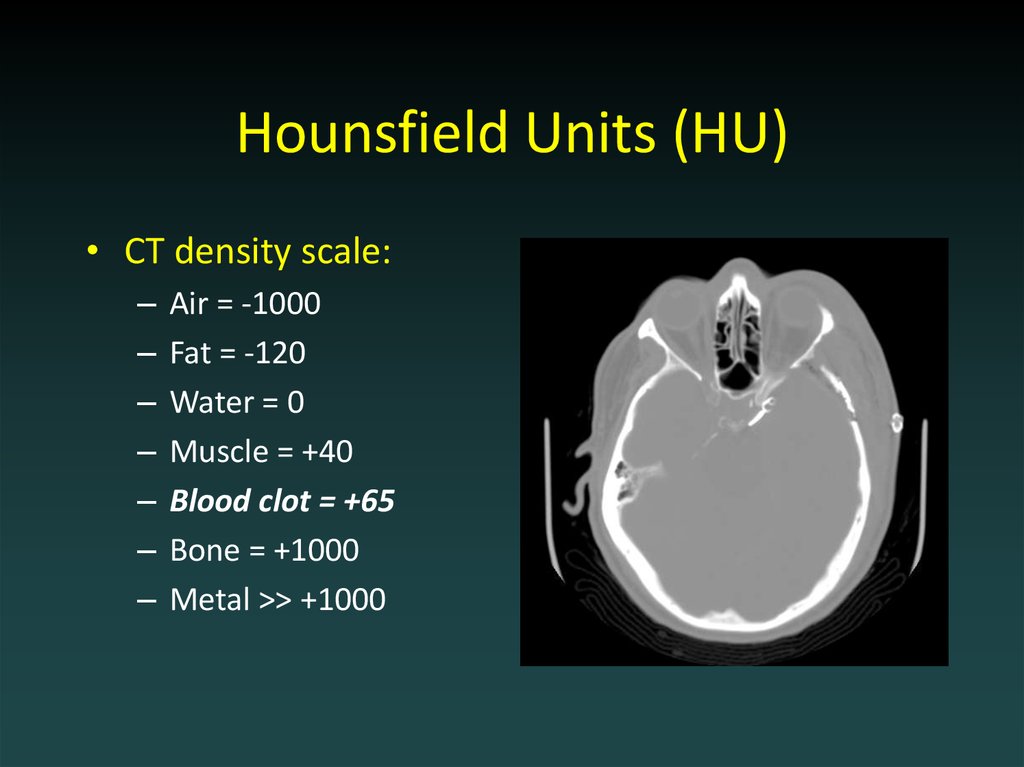
8. Hounsfield Units (HU)
• CT density scale:–
–
–
–
–
–
–
Air = -1000
Fat = -120
Water = 0
Muscle = +40
Blood clot = +65
Bone = +1000
Metal >> +1000
9. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
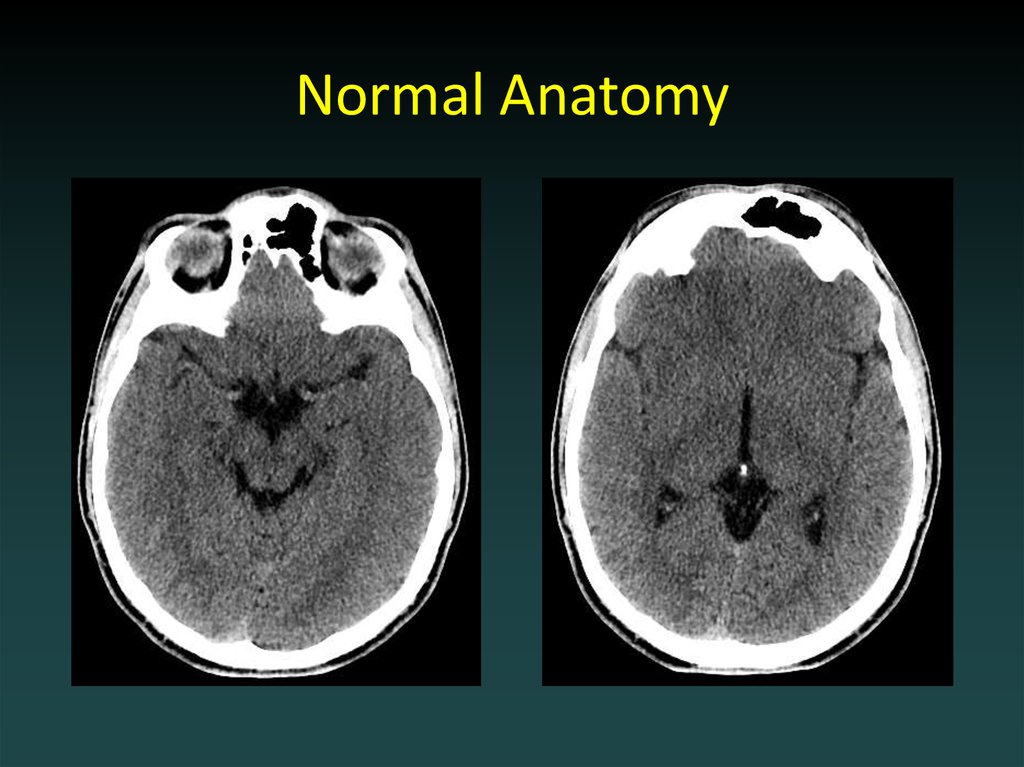
10. Normal Anatomy
11. Normal Anatomy
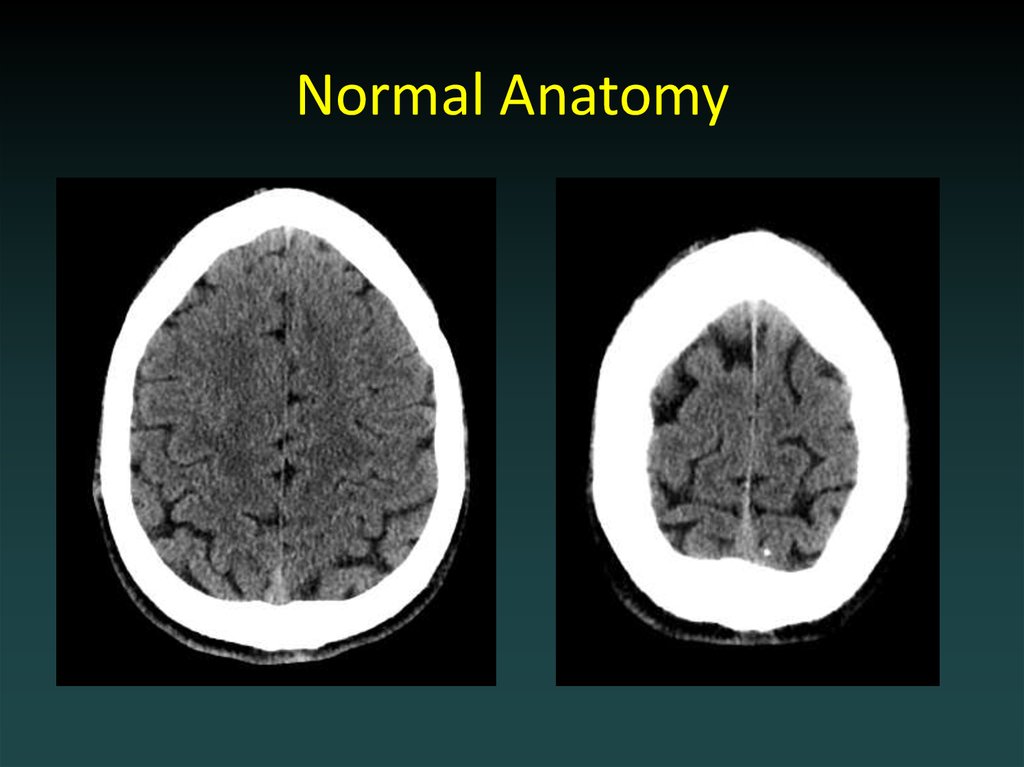
12. Normal Anatomy
13. Normal Anatomy
14. Acute Head CT Checklist
Midline Shift
Mass Effect
Density
CSF Spaces
Vascular Territories
Intra-/Extra-axial
Herniation
15. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
16.
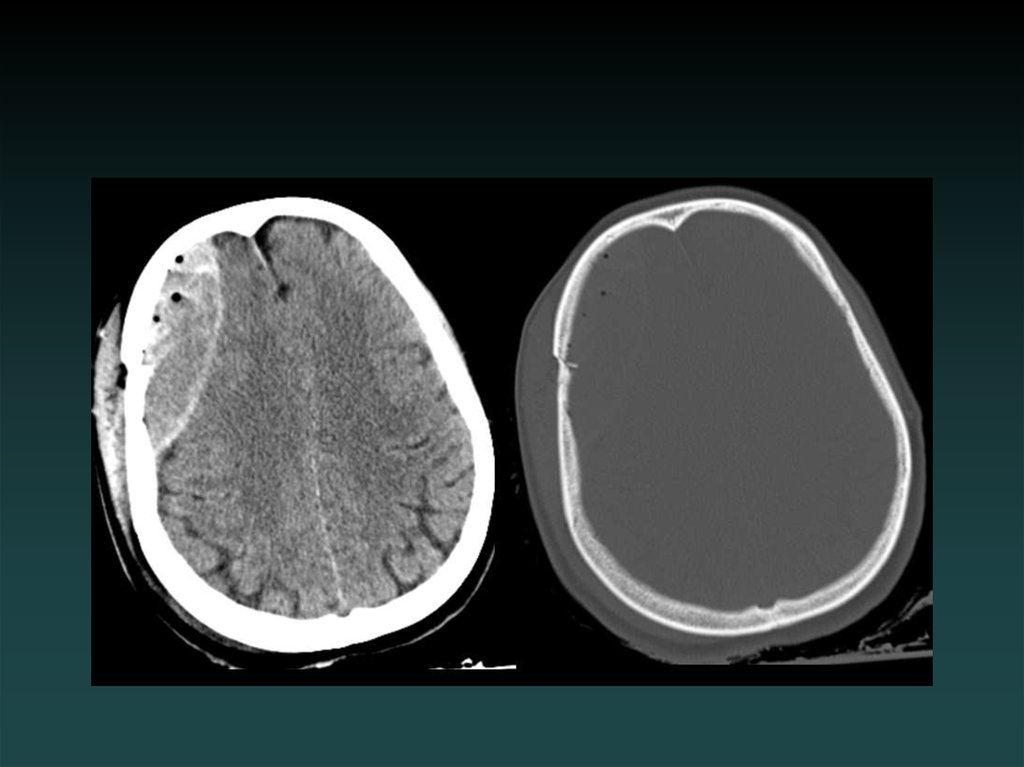
17. Epidural Hematoma
• Injury to epidural vessel– Arterial bleeding
• Lentiform shape
• Does not cross sutures
– May cross falx or tentorium
• Look for:
– FRACTURE
– RAPID EXPANSION
18.
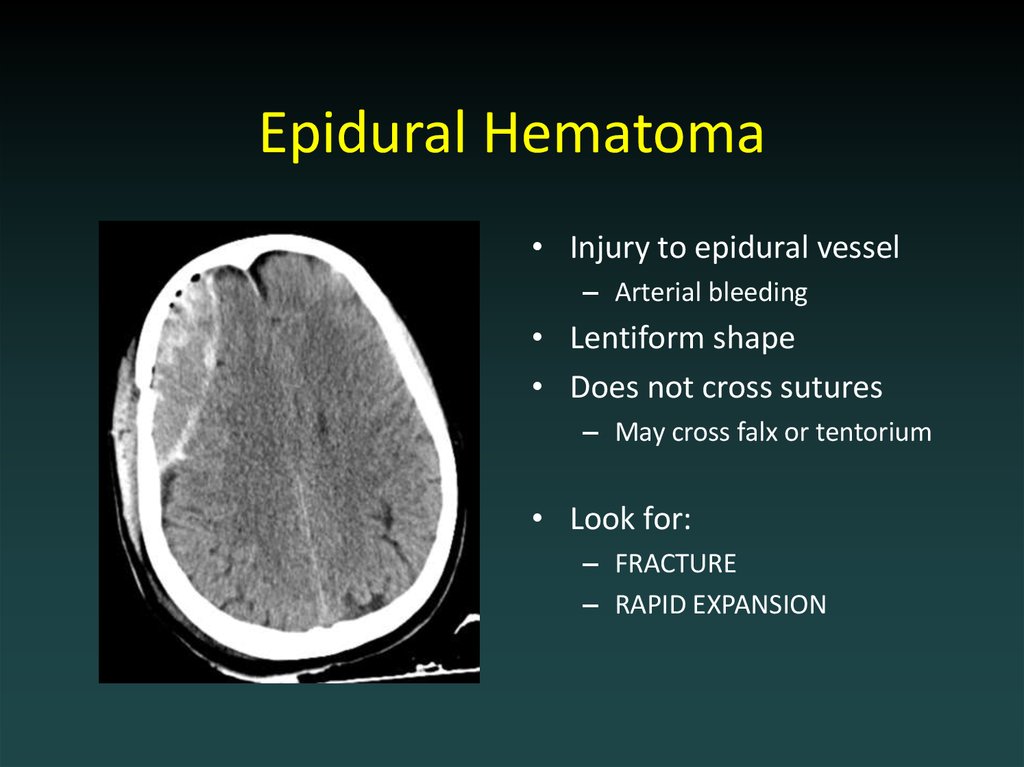
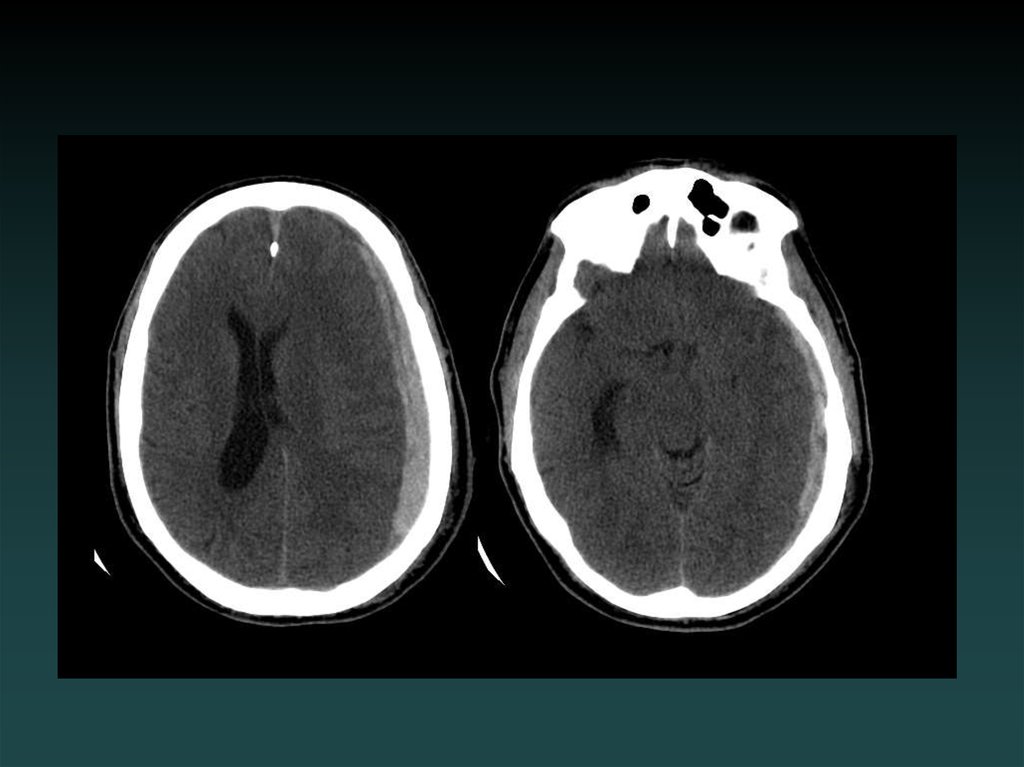
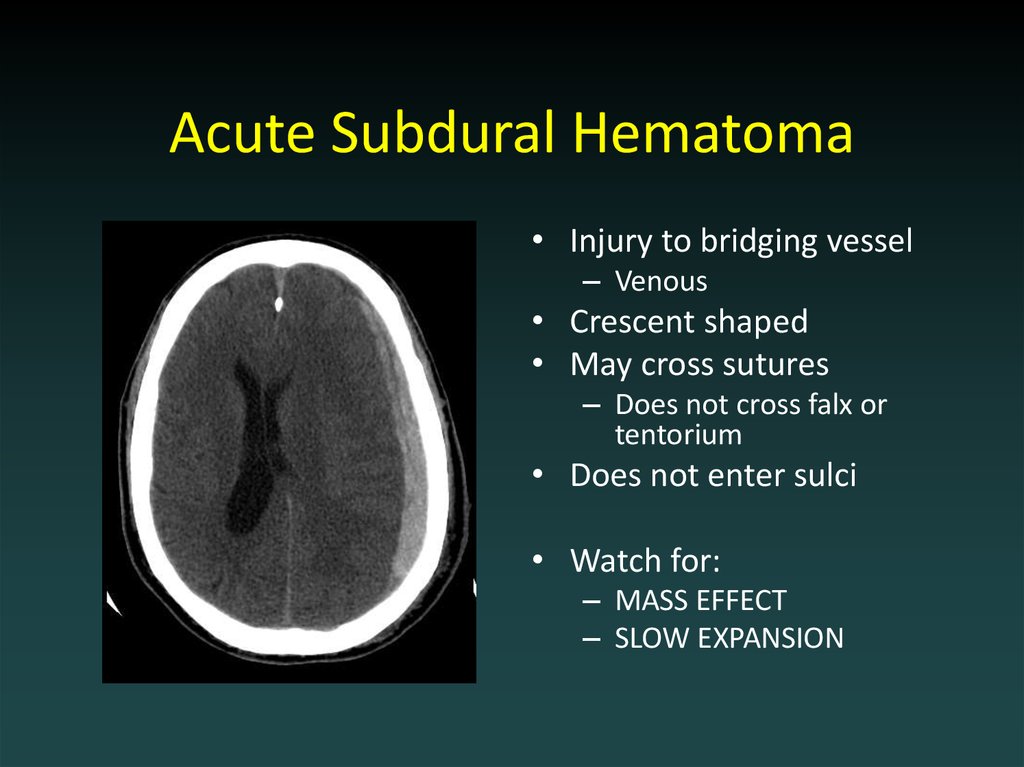
19. Acute Subdural Hematoma
• Injury to bridging vessel– Venous
• Crescent shaped
• May cross sutures
– Does not cross falx or
tentorium
• Does not enter sulci
• Watch for:
– MASS EFFECT
– SLOW EXPANSION
20.
21. Chronic Subdural Hematoma
• HYPODENSE– (blood degradation)
• MIXED
– (Acute-on-chronic)
22.
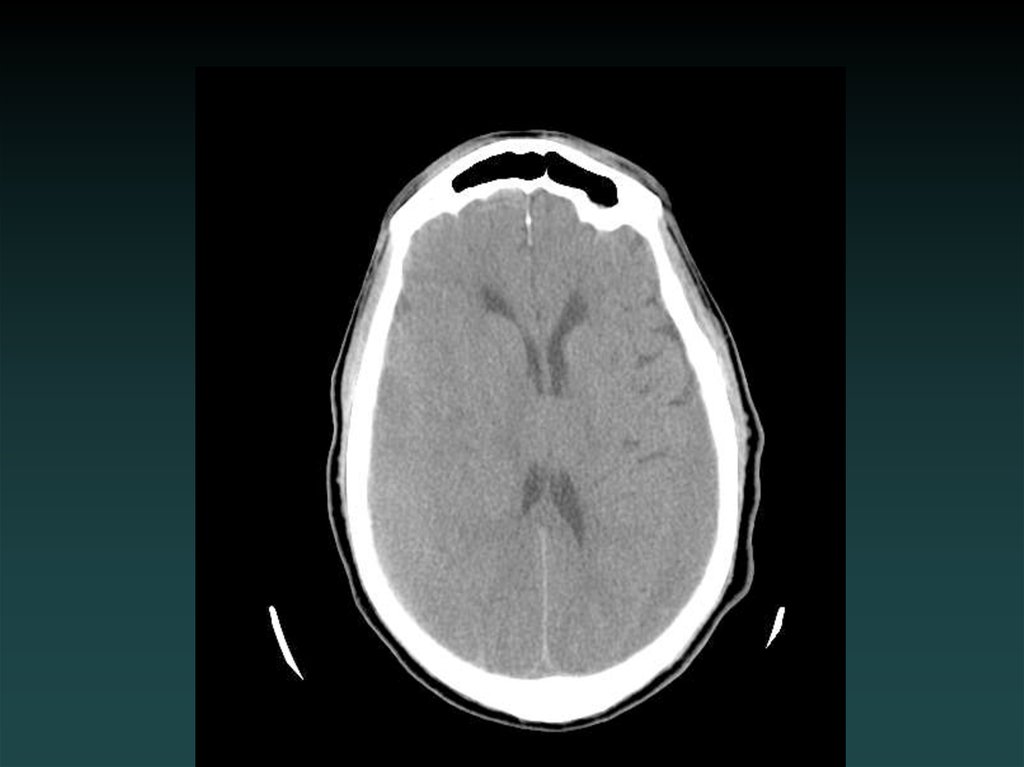
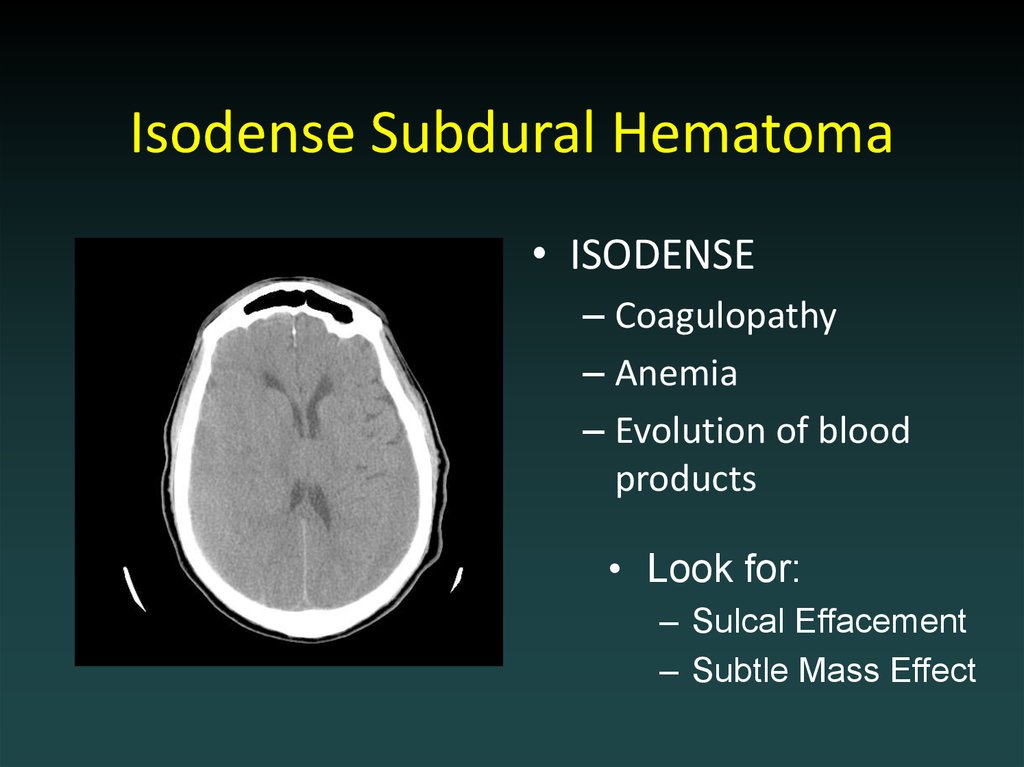
23. Isodense Subdural Hematoma
• ISODENSE– Coagulopathy
– Anemia
– Evolution of blood
products
• Look for:
– Sulcal Effacement
– Subtle Mass Effect
24.
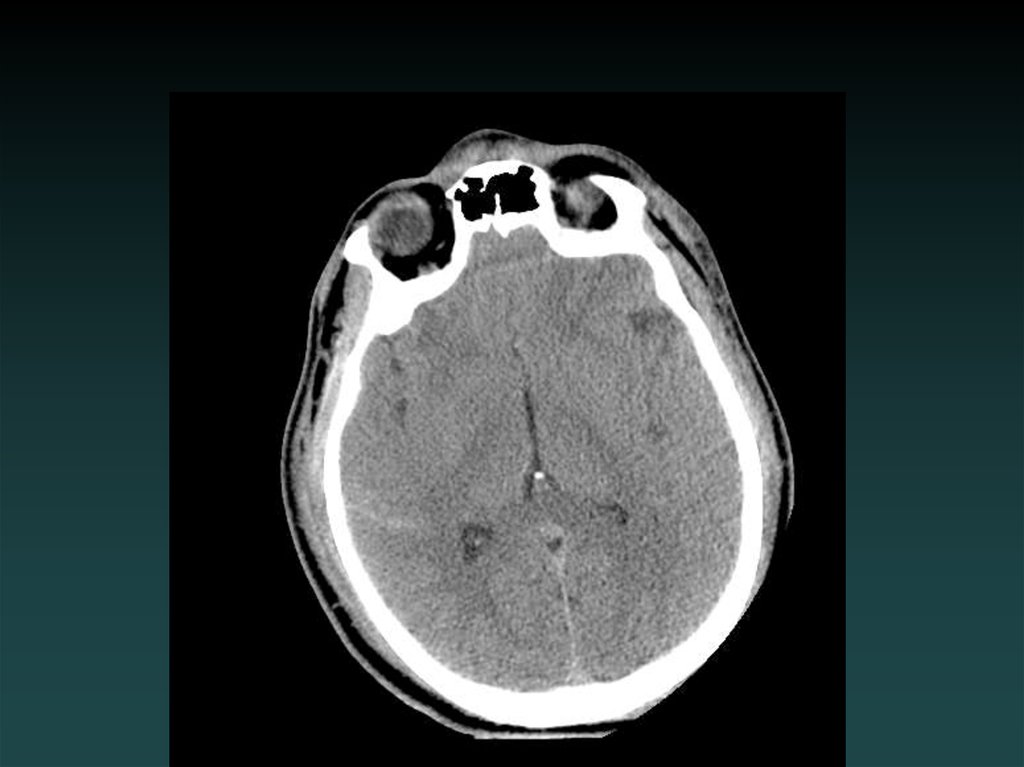
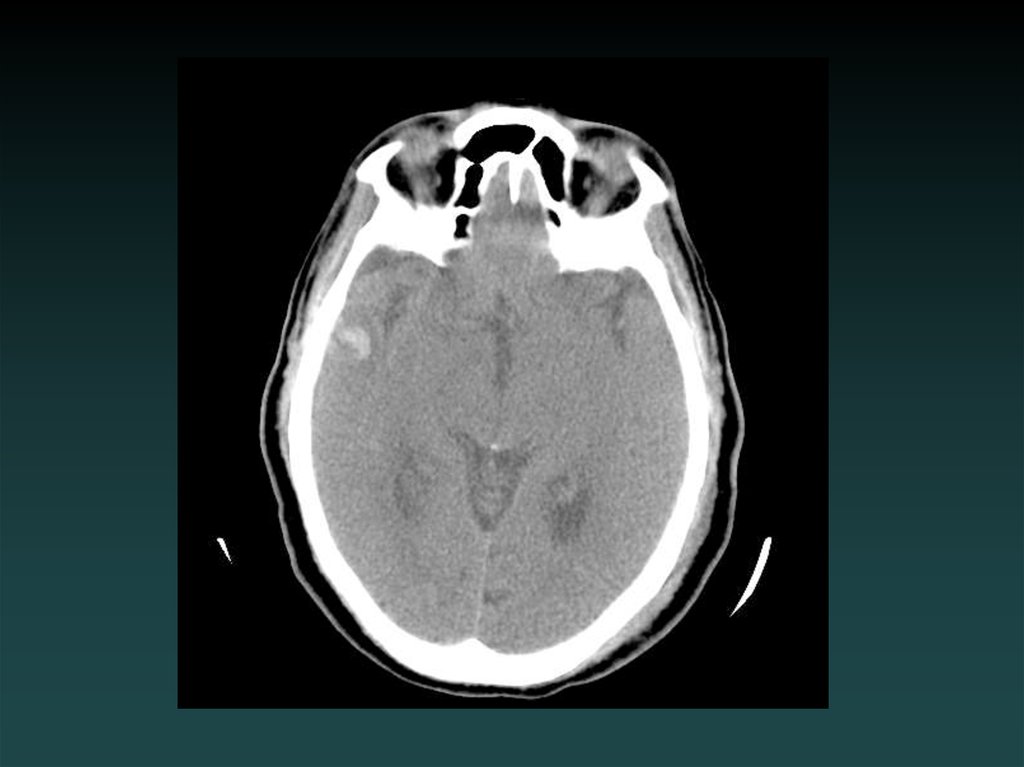
25. Subarachnoid Hemorrhage
• Subarachnoid– Sulci
– Cisterns
– Ventricles
• Trauma
– lateral convexities
• Aneurysm
– basal cisterns
• Interpeduncular Cistern
– most sensitive
26.
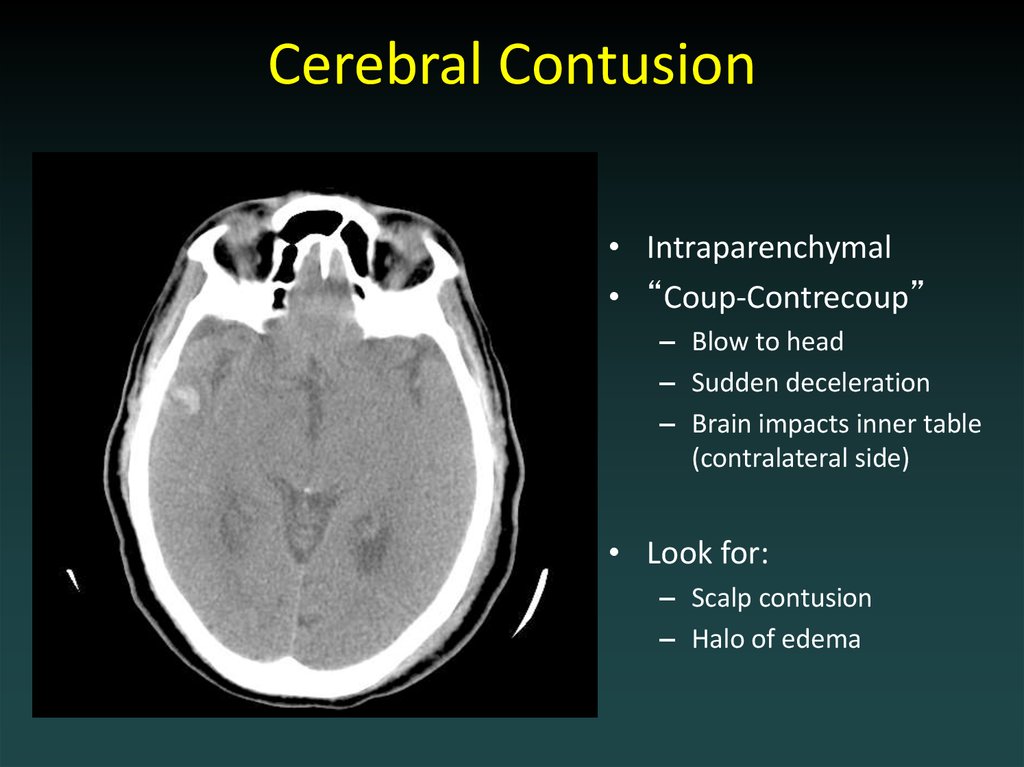
27. Cerebral Contusion
• Intraparenchymal• “Coup-Contrecoup”
– Blow to head
– Sudden deceleration
– Brain impacts inner table
(contralateral side)
• Look for:
– Scalp contusion
– Halo of edema
28.
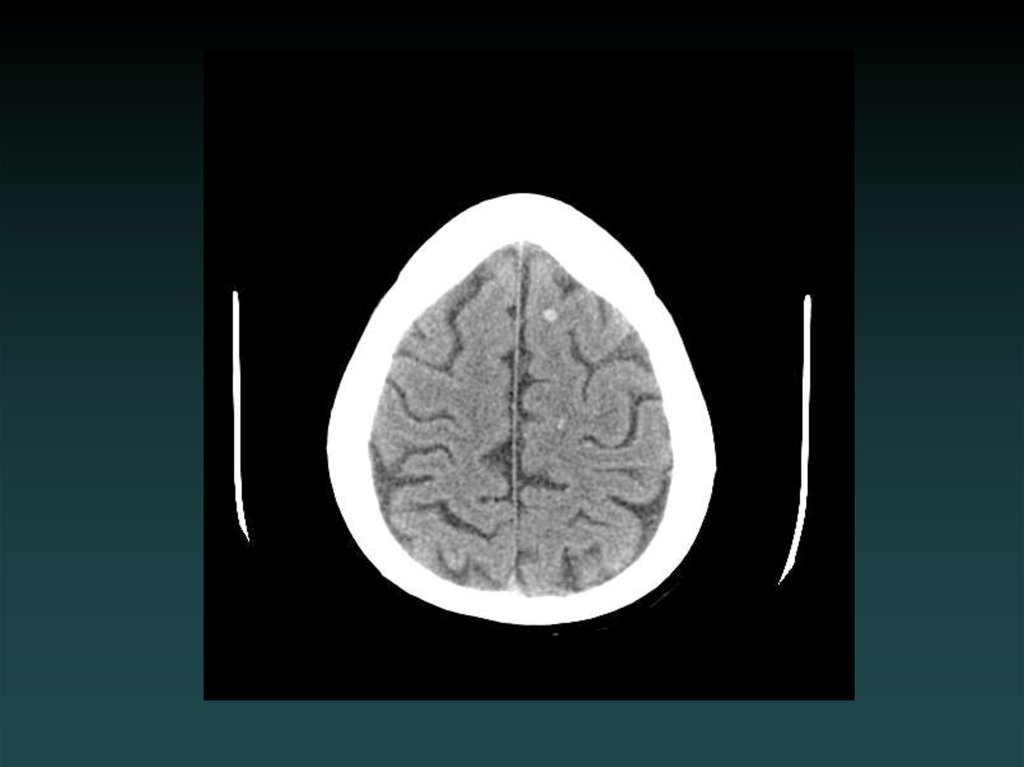
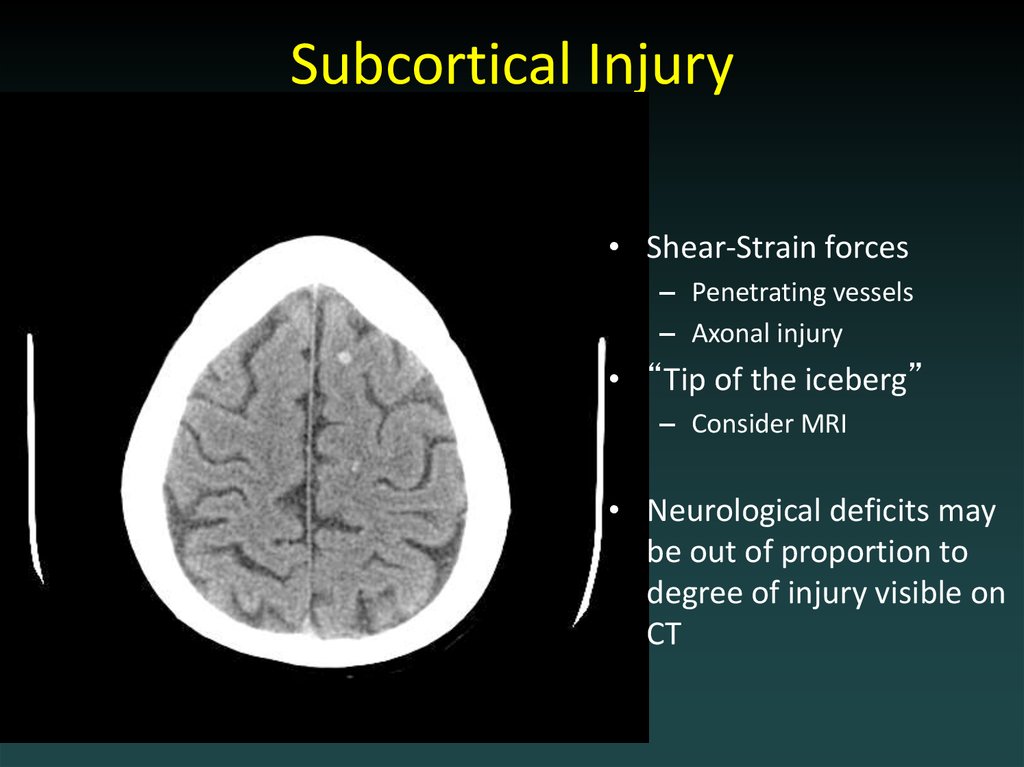
29. Subcortical Injury
• Shear-Strain forces– Penetrating vessels
– Axonal injury
• “Tip of the iceberg”
– Consider MRI
• Neurological deficits may
be out of proportion to
degree of injury visible on
CT
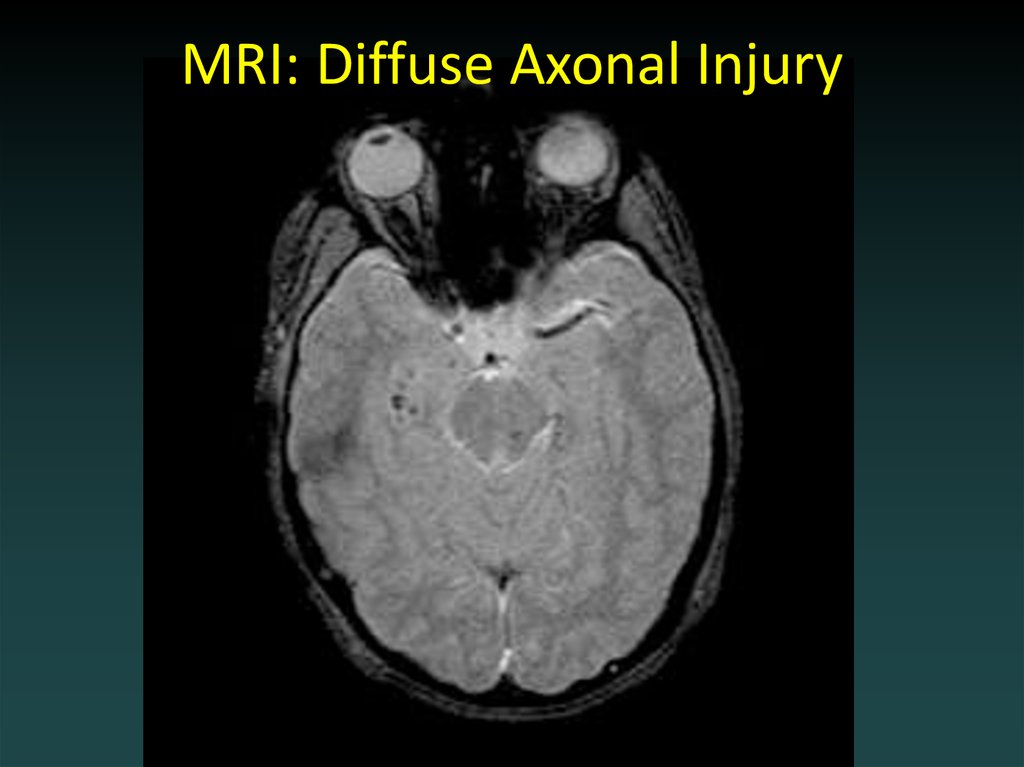
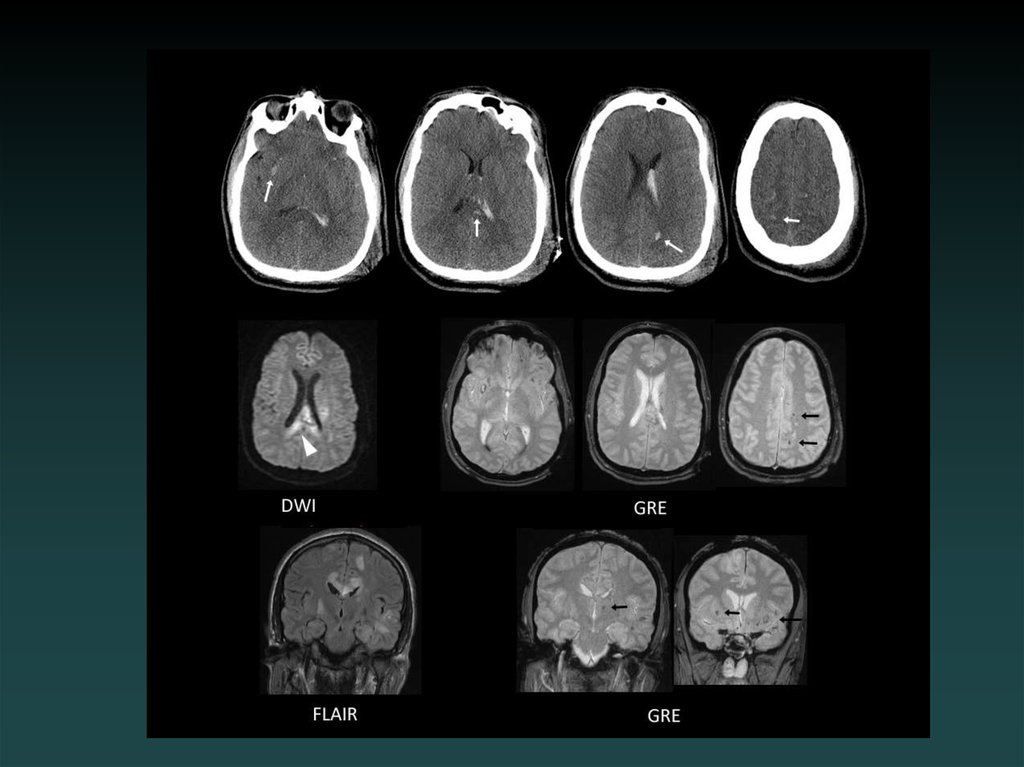
30. MRI: Diffuse Axonal Injury
31.
32.
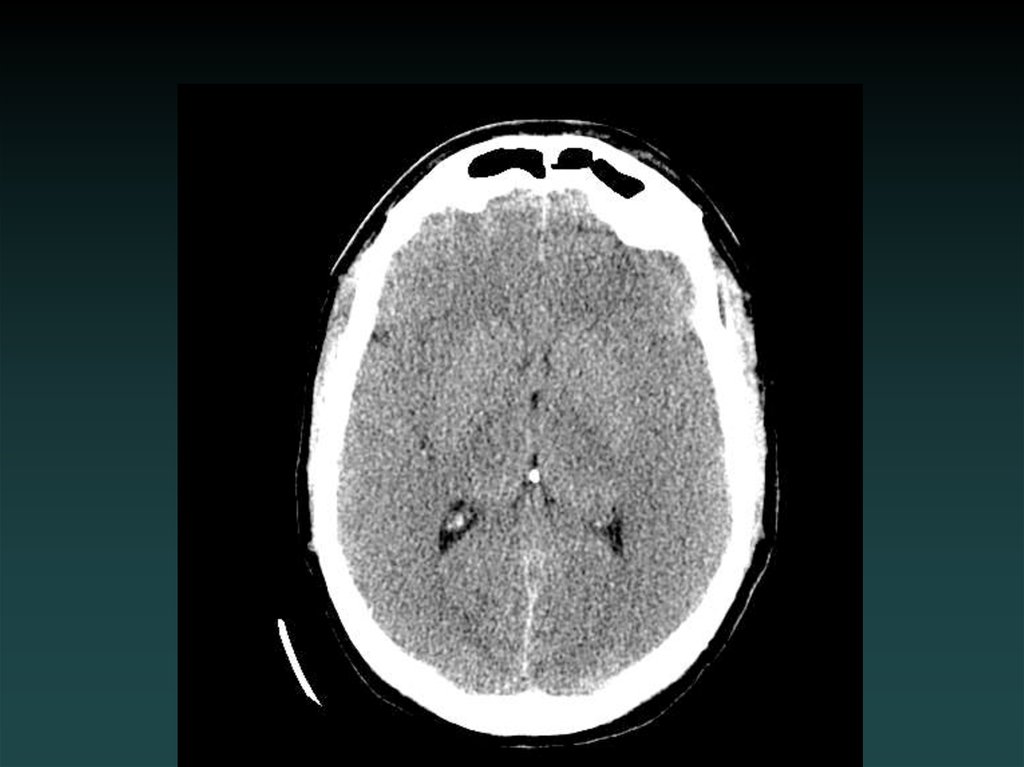
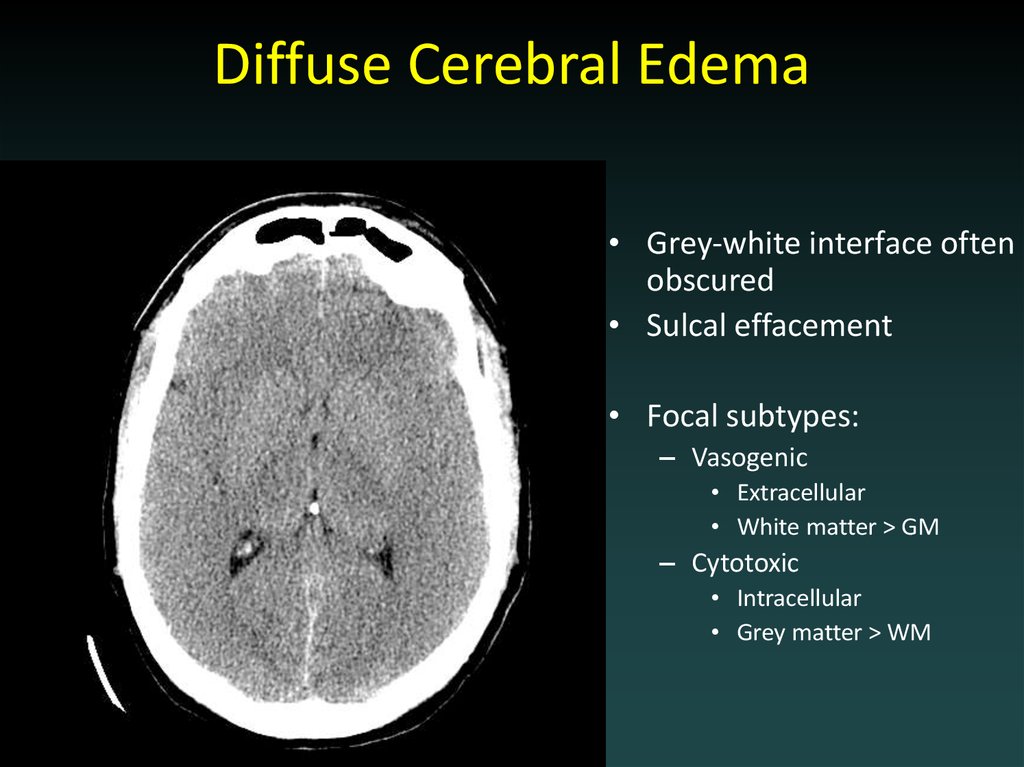
33. Diffuse Cerebral Edema
• Grey-white interface oftenobscured
• Sulcal effacement
• Focal subtypes:
– Vasogenic
• Extracellular
• White matter > GM
– Cytotoxic
• Intracellular
• Grey matter > WM
34. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
35. Stroke
36.
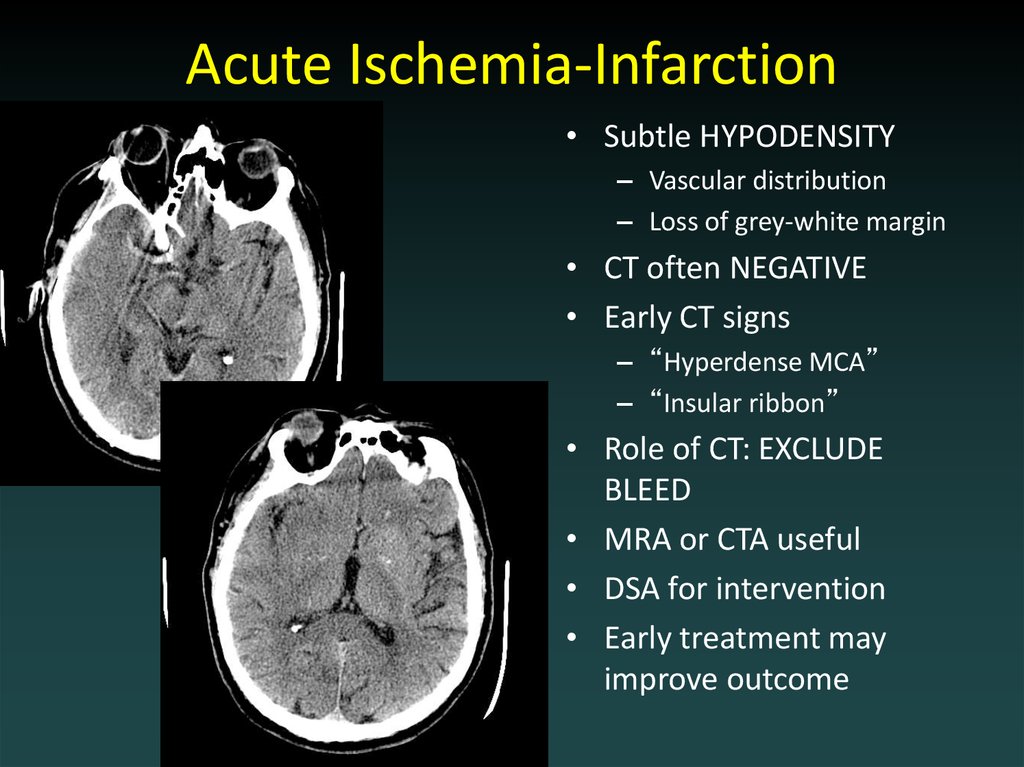
37. Acute Ischemia-Infarction
• Subtle HYPODENSITY– Vascular distribution
– Loss of grey-white margin
• CT often NEGATIVE
• Early CT signs
– “Hyperdense MCA”
– “Insular ribbon”
• Role of CT: EXCLUDE
BLEED
• MRA or CTA useful
• DSA for intervention
• Early treatment may
improve outcome
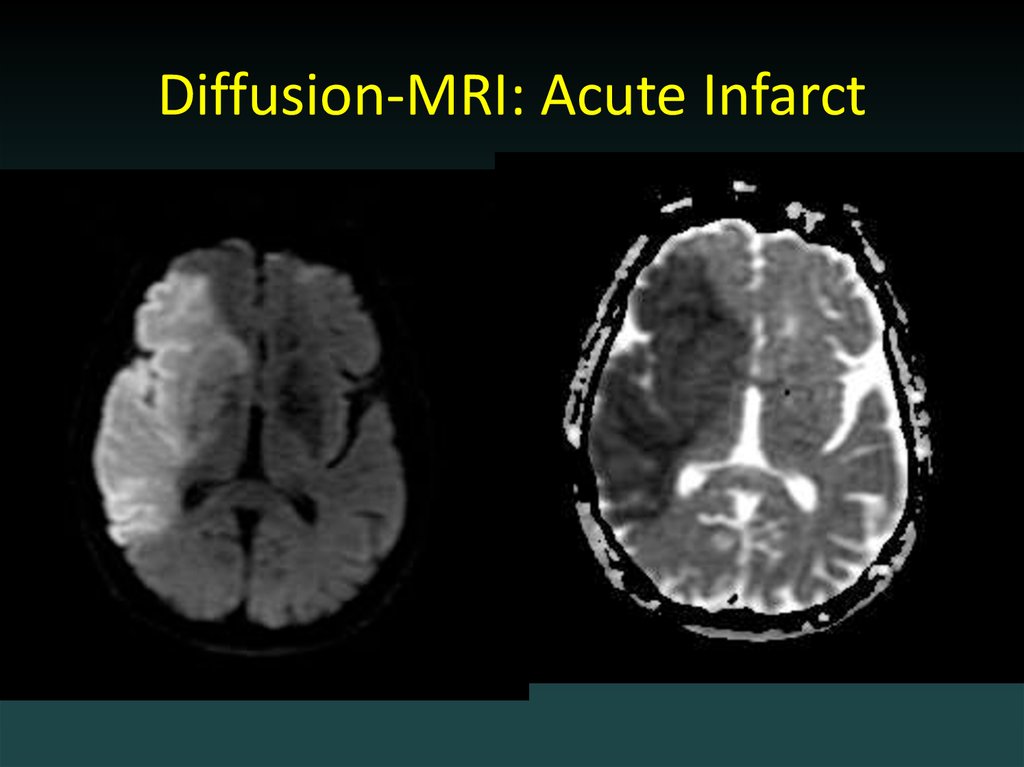
38. Diffusion-MRI: Acute Infarct
39.
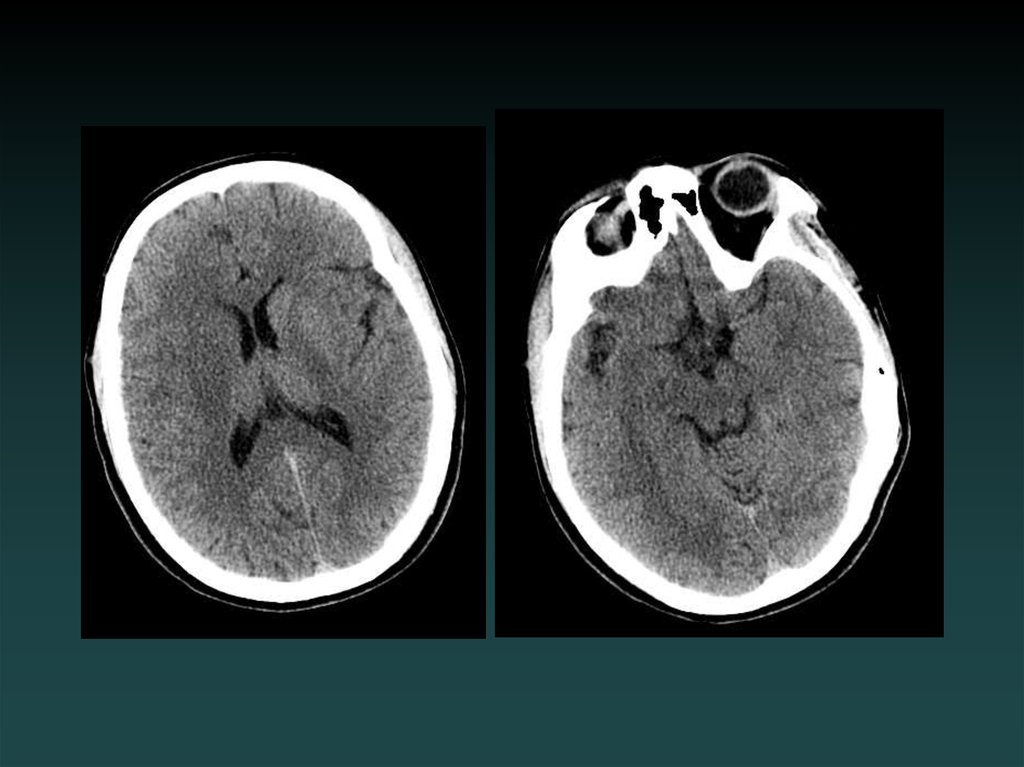
40. Acute facial droop, hemiparesis
41.
42.
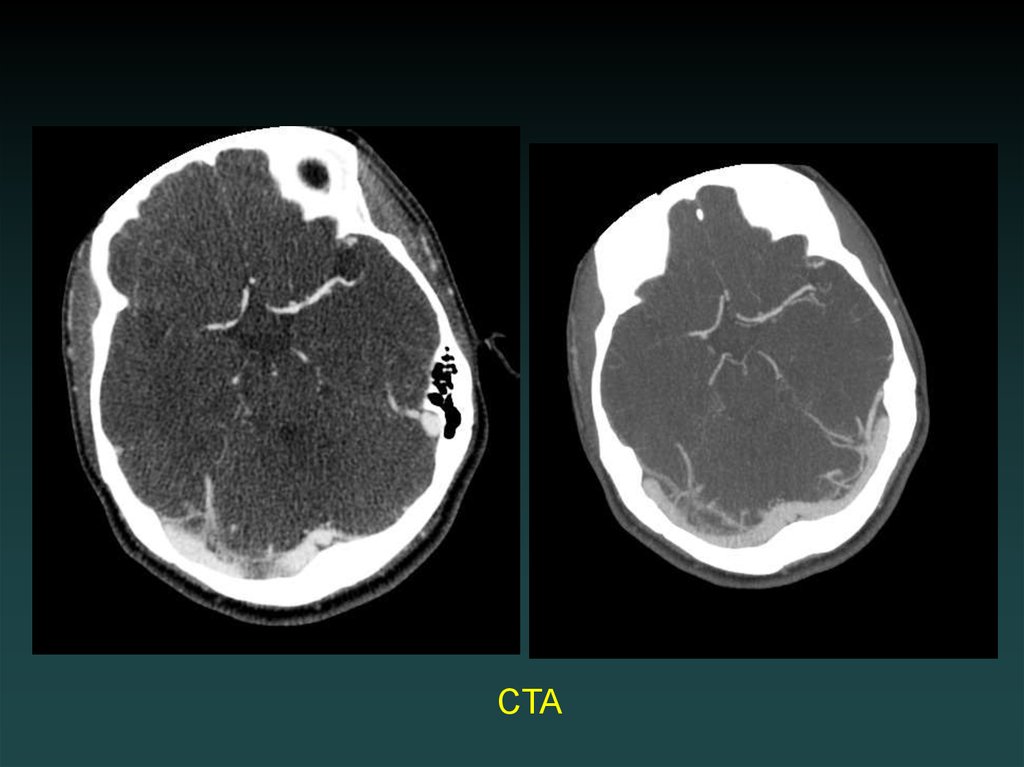
CTA43. Angio
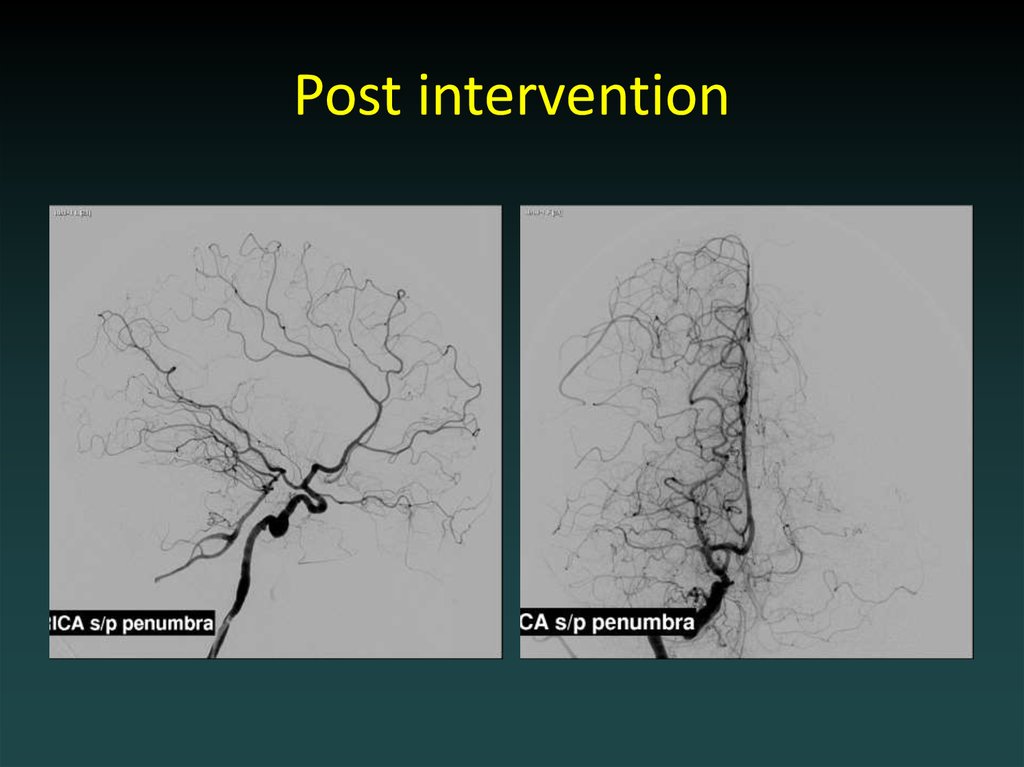
44. Post intervention
45. Watershed Infarction
46.
47.
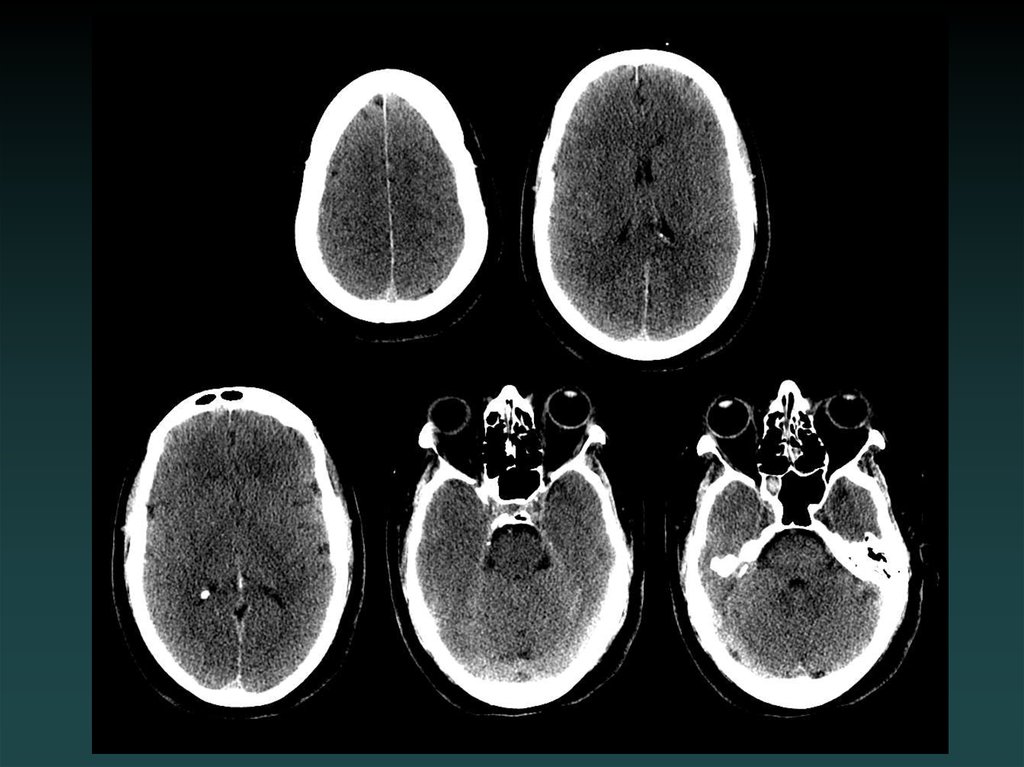
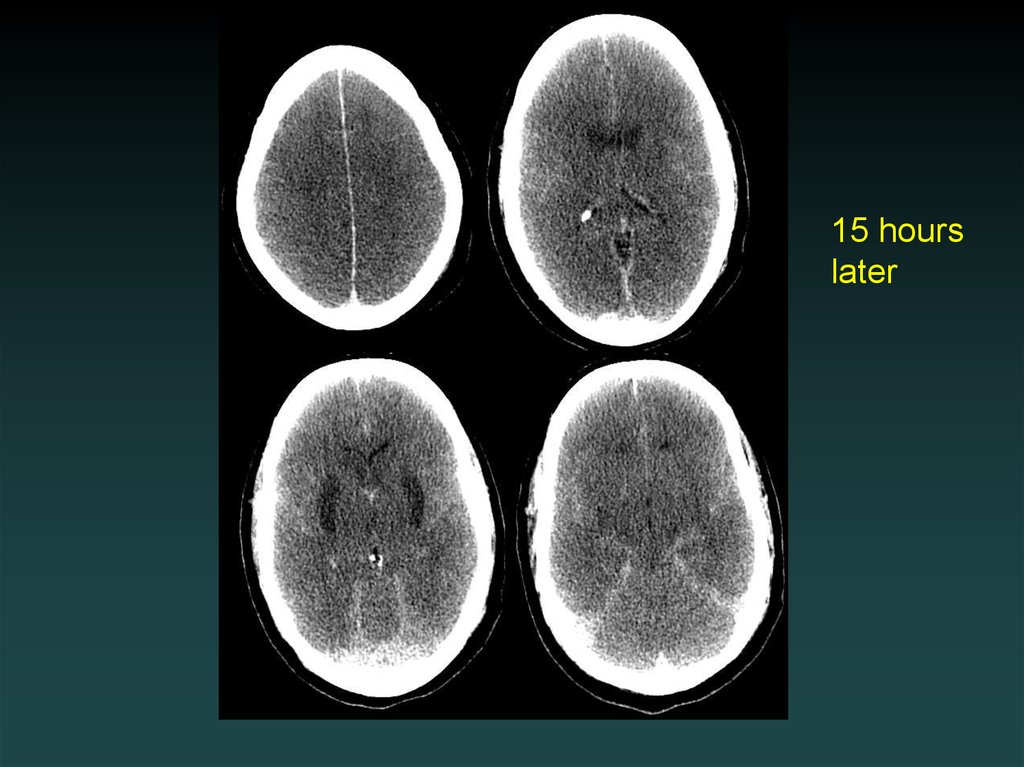
48.
15 hourslater
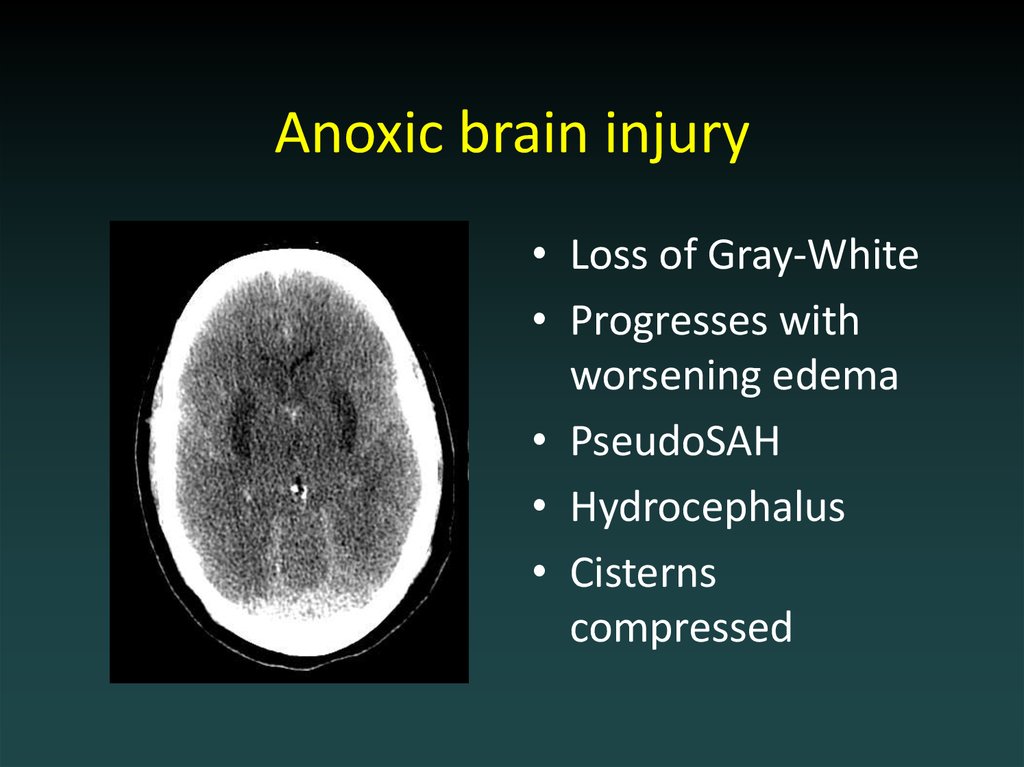
49. Anoxic brain injury
• Loss of Gray-White• Progresses with
worsening edema
• PseudoSAH
• Hydrocephalus
• Cisterns
compressed
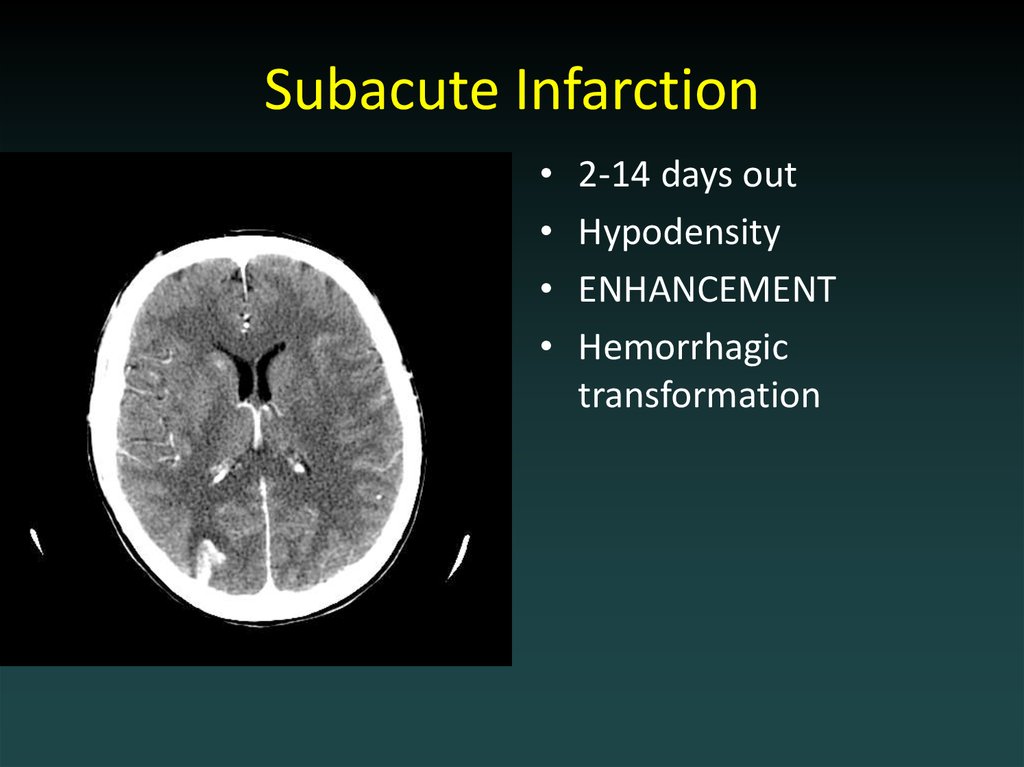
50. Subacute Infarction
2-14 days out
Hypodensity
ENHANCEMENT
Hemorrhagic
transformation
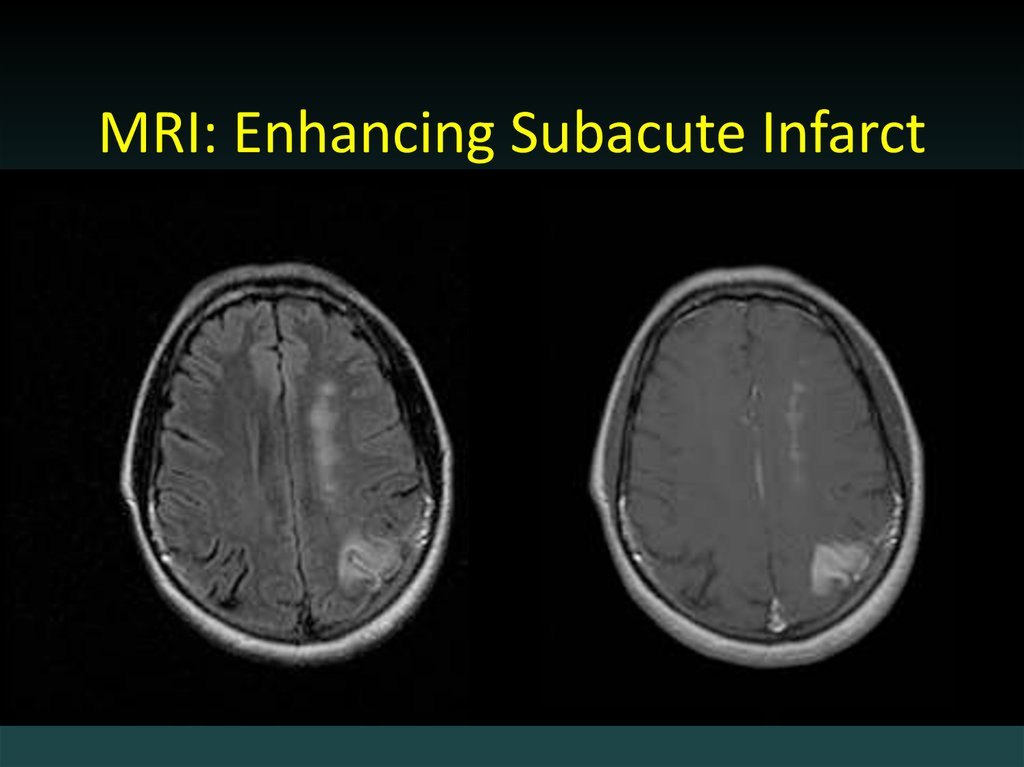
51. MRI: Enhancing Subacute Infarct
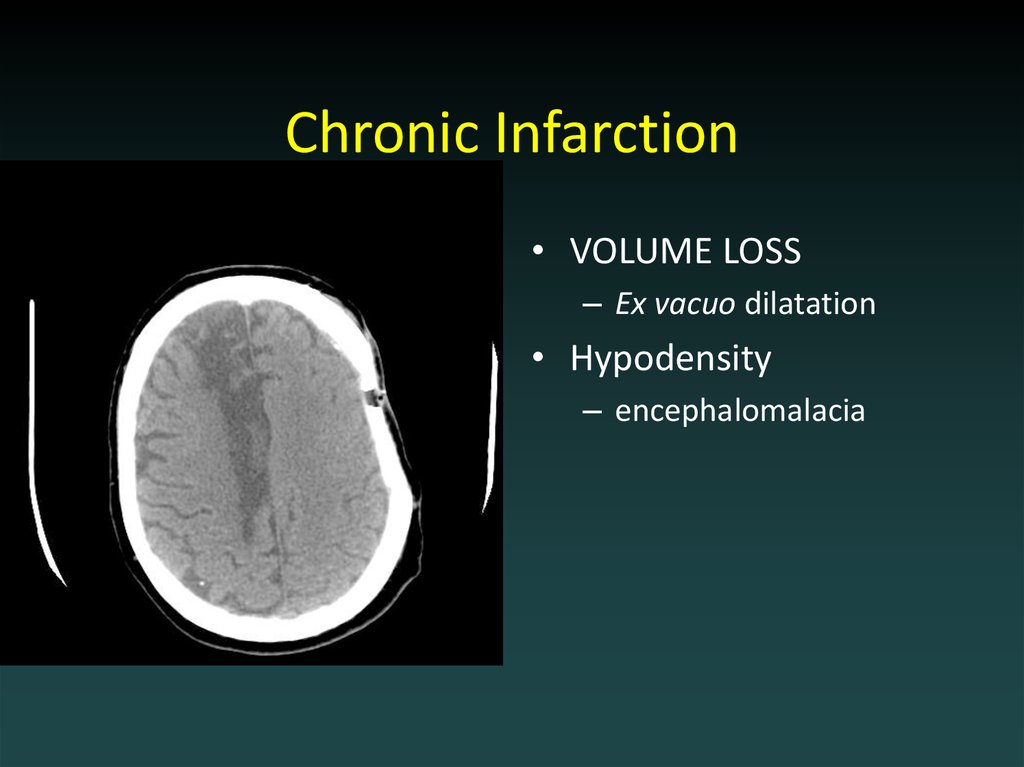
52. Chronic Infarction
• VOLUME LOSS– Ex vacuo dilatation
• Hypodensity
– encephalomalacia
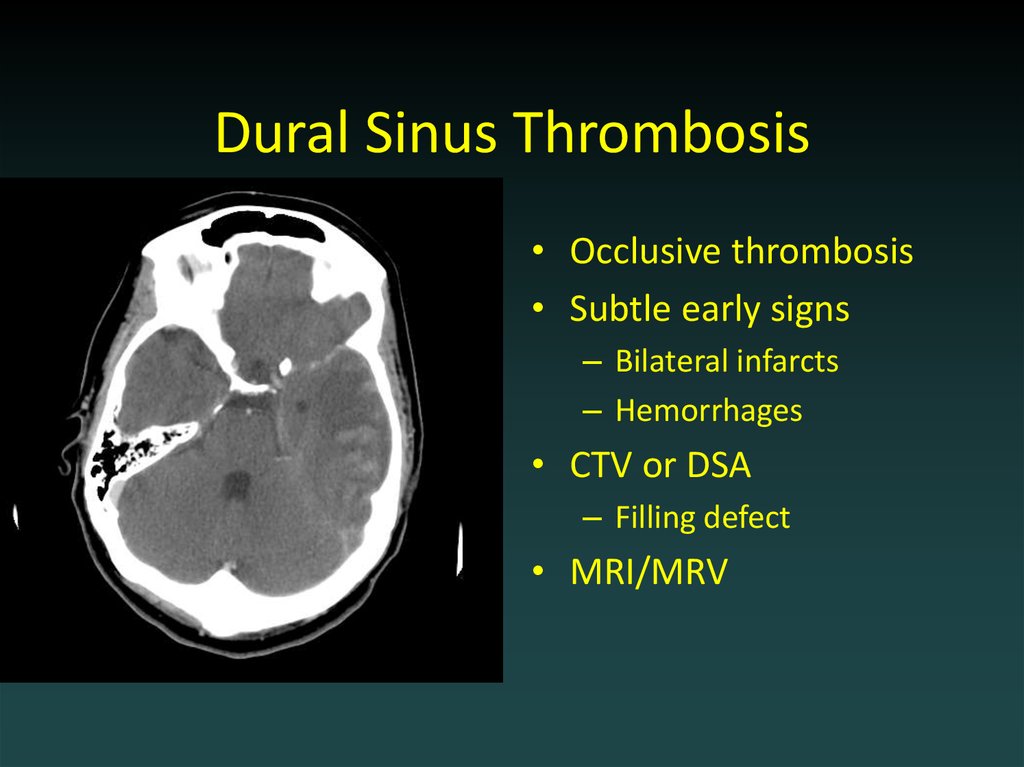
53. Dural Sinus Thrombosis
• Occlusive thrombosis• Subtle early signs
– Bilateral infarcts
– Hemorrhages
• CTV or DSA
– Filling defect
• MRI/MRV
54.
55. Outline
• Choosing a study• Normal anatomy
• Trauma
• Ischemic stroke
• Aneurysm
56.
57. Aneurysmal SAH
• Sudden severe headache• HYPERDENSE CSF spaces
• Location
– Interhemispheric: ACoA
– Sylvian: MCA
• HYDROCEPHALUS,
VASOSPASM and
ISCHEMIA
– MUST find the aneurysm!
• DSA, CTA and/or MRA
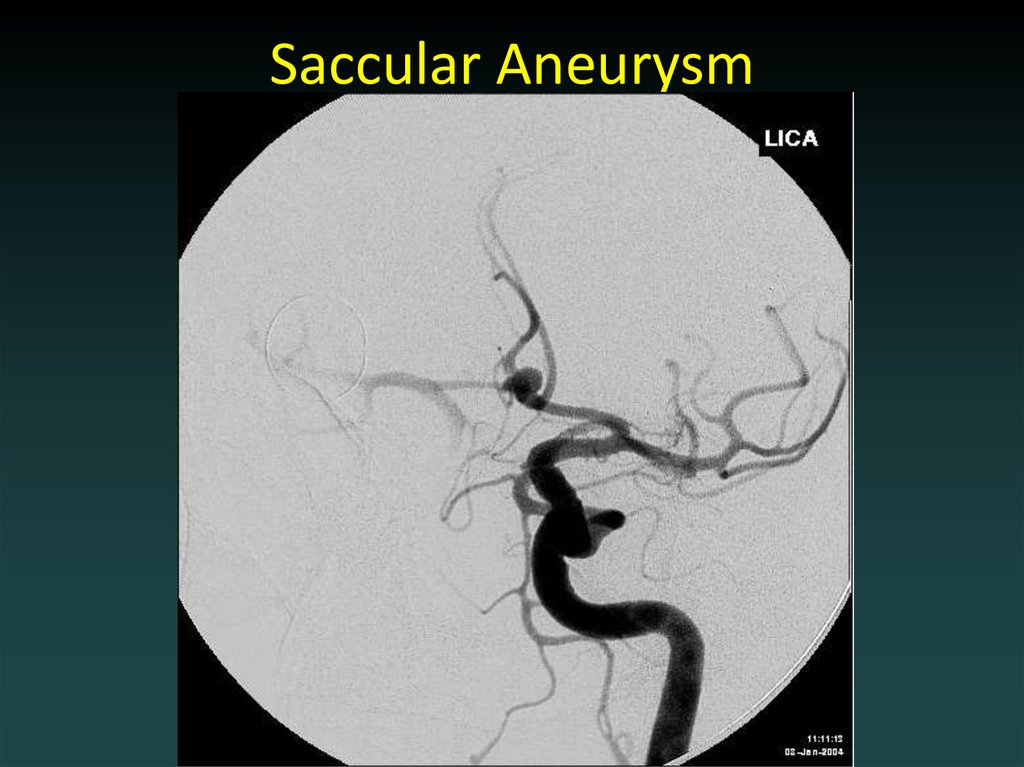
58. Saccular Aneurysm
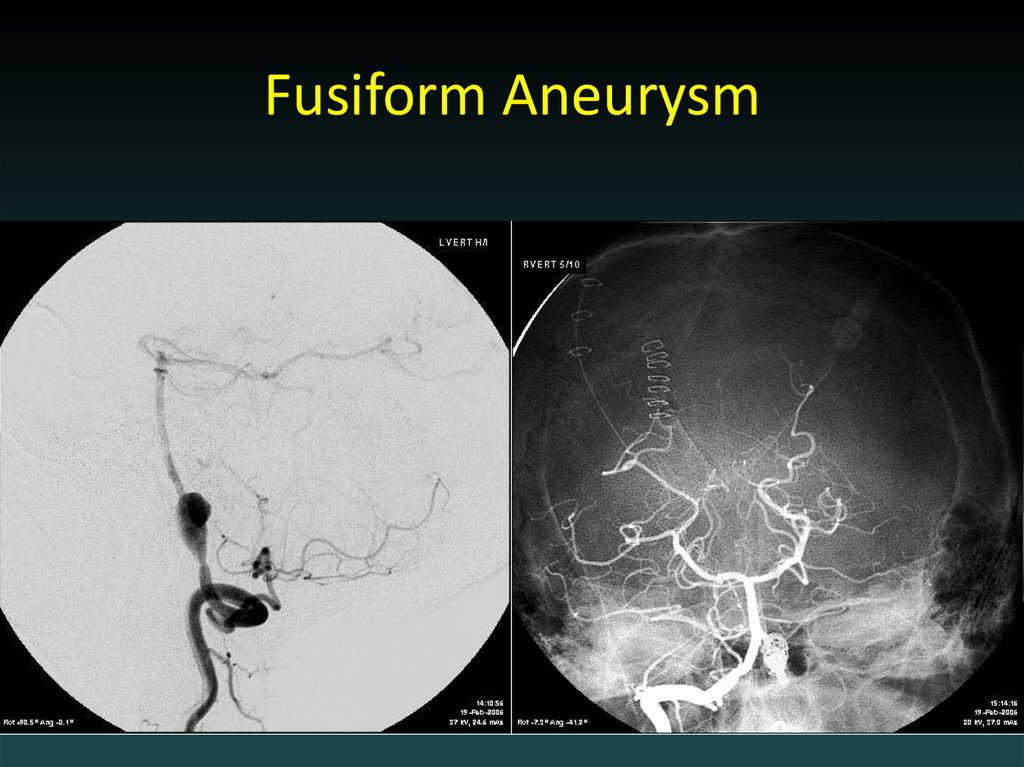
59. Fusiform Aneurysm
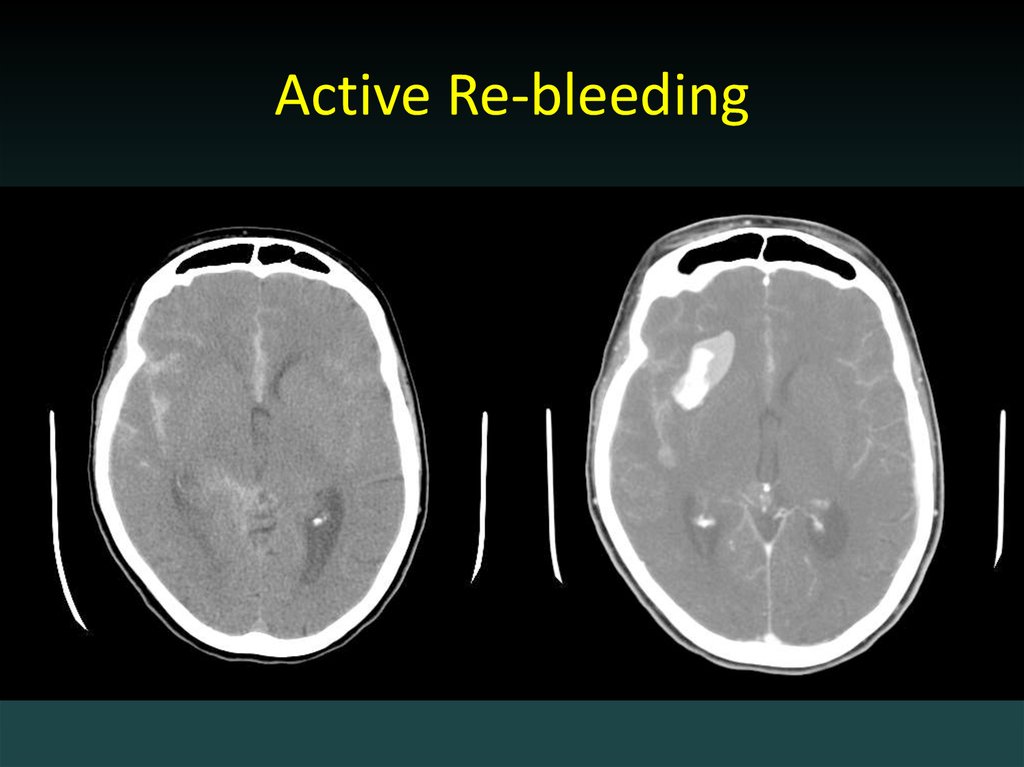
60. Active Re-bleeding
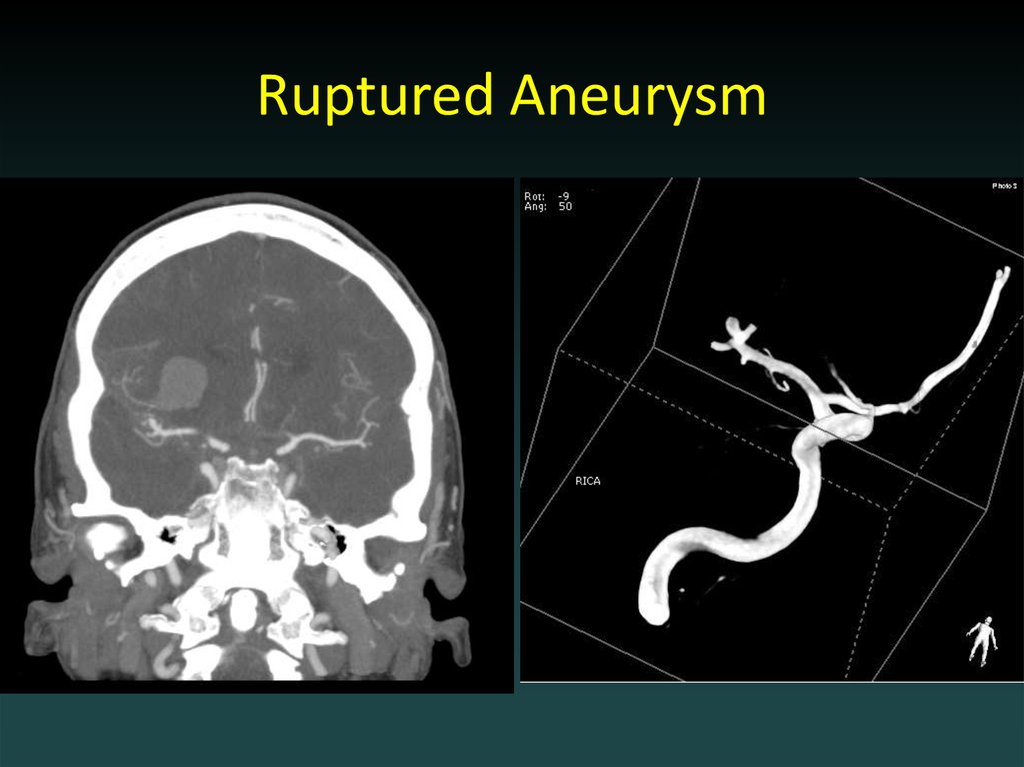
61. Ruptured Aneurysm
62.
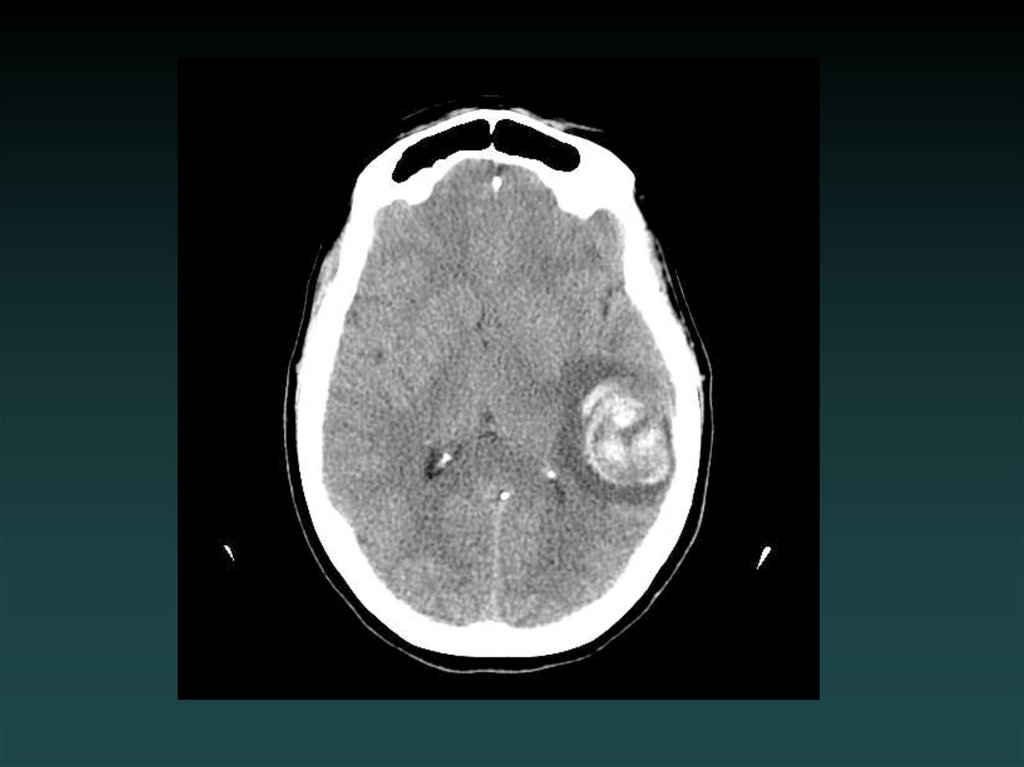
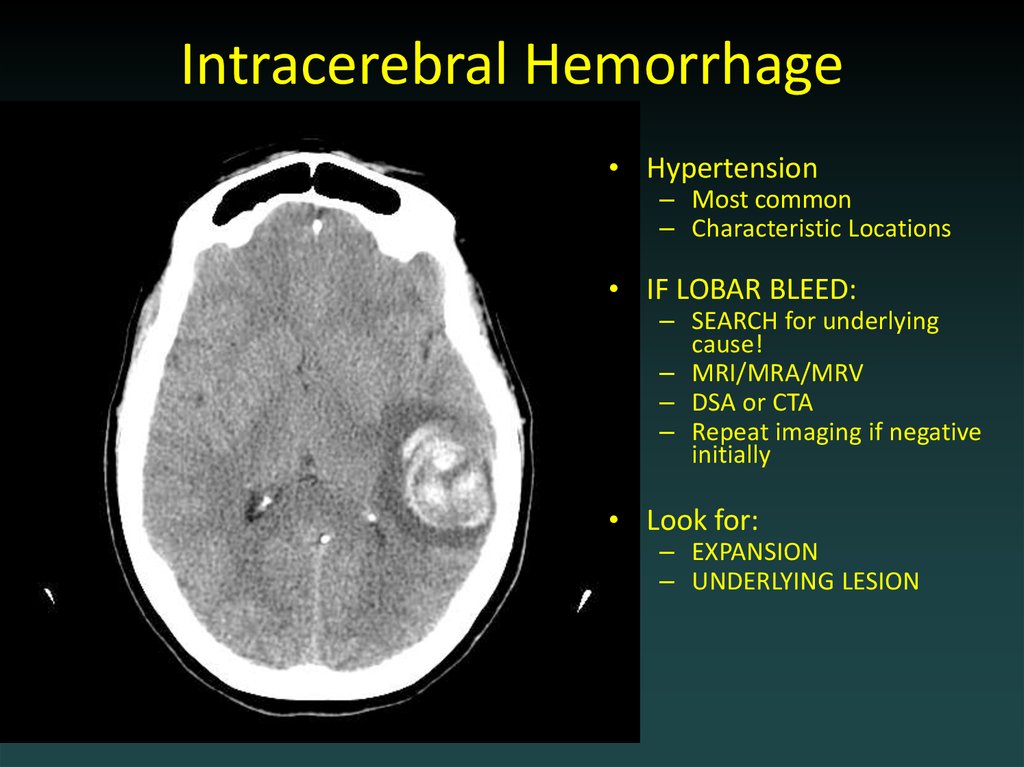
63. Intracerebral Hemorrhage
• Hypertension– Most common
– Characteristic Locations
• IF LOBAR BLEED:
– SEARCH for underlying
cause!
– MRI/MRA/MRV
– DSA or CTA
– Repeat imaging if negative
initially
• Look for:
– EXPANSION
– UNDERLYING LESION















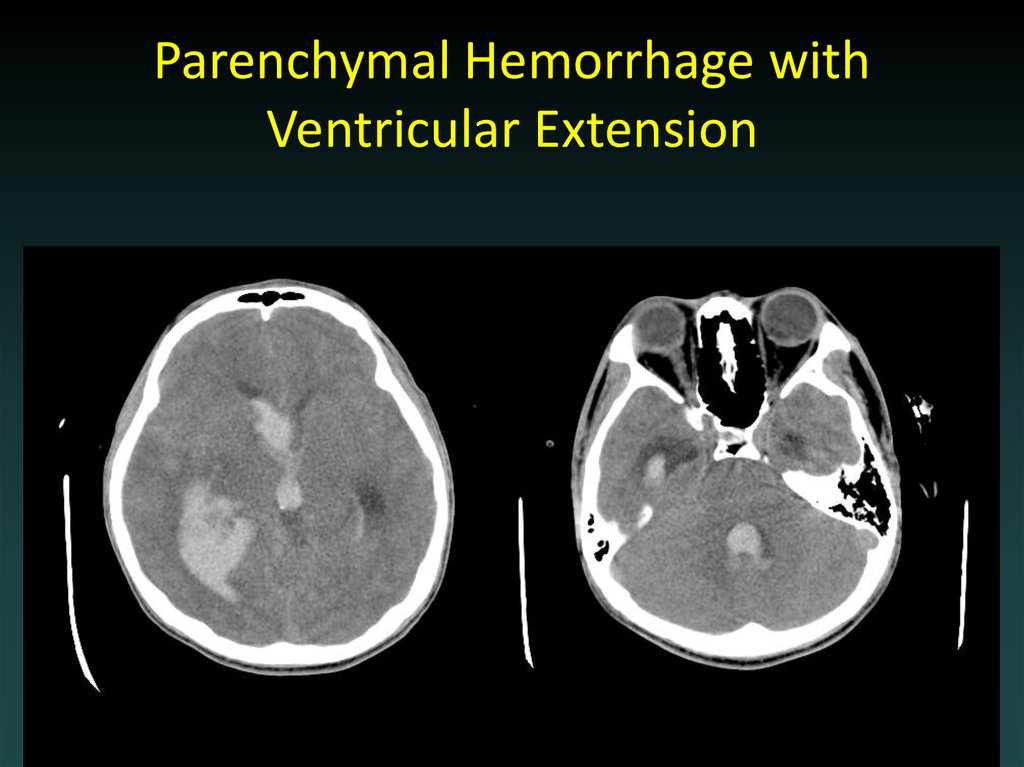
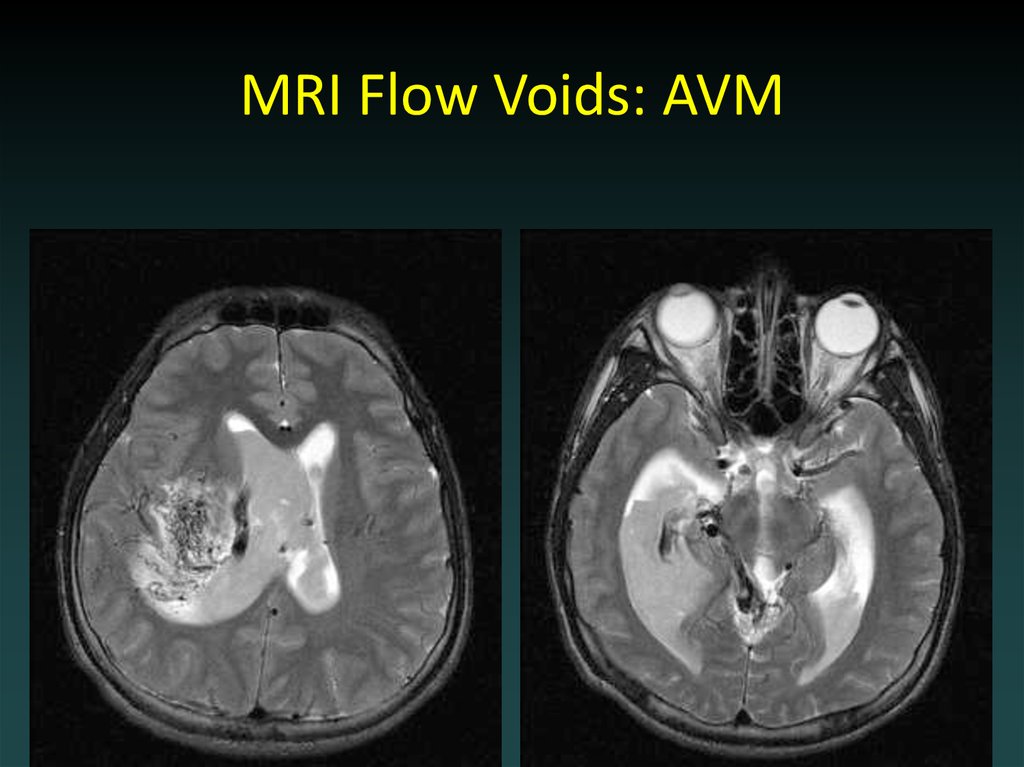
 medicine
medicine