Similar presentations:
Gastric and duodenal ulcers
1. Gastric and duodenal ulcers
С.Ж.АСФЕНДИЯРОВ АТЫНДАҒЫҚАЗАҚ ҰЛТТЫҚ МЕДИЦИНА УНИВЕРСИТЕТІ
KAZAKH NATIONAL MEDICAL UNIVERSITY
NAMED AFTER S.J.ASFENDIYAROV
DEPARTMENT OF FOREIGN LANGUAGES
GASTRIC AND DUODENAL ULCERS
Checked by:Sainova M.B
Prepared by:Beken O.SH
Faculty:GM
Course:2
Group:027-2
Almaty,2017
2. Plan:
PLAN:I.Introduction
What is an ulcer?
II.Main section
Diagnosis
Causes & Risk Factors
Why are they important?
Consequences
III.Conclusion
IV.Used books
3. What is an ulcer?
WHAT IS AN ULCER?• Acid breaks through protective
substances on gut wall
• Duodenum (1st part small intestine) –
most common site
• “Gastric” ulcers – in stomach
Pain, bloating, nausea, “fullness”,
weight loss, tiredness
Complications: bleeding,
perforation, obstruction
4. Diagnosis
DIAGNOSISEndoscopy (>55yrs, first time). Capture all cases?
Faecal / breath tests for H. pylori
GI series (rare)
False positive tests
Missed cases? – risk of transmission / disease progression
5. Why are they important?
WHY ARE THEY IMPORTANT?HPA – “infectious disease” but main effects are from
chronic burden
Potential “medical emergency”
Chronic symptoms – health and economic costs
H. pylori also linked to:
Functional dypepsia
Cancer (2-6x more likely, though still rare)
Differential clinical outcome - interaction between bacterial
properties (phenotypic variation), genetics and
environmental / behavioural factors
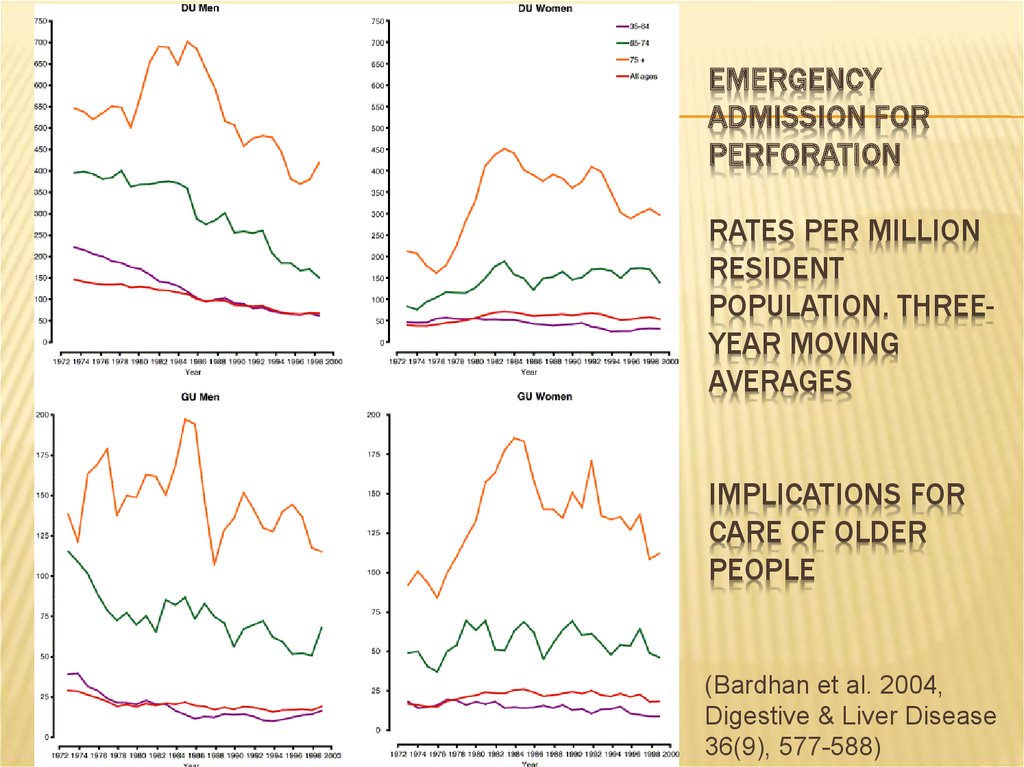
6. Emergency admission for perforation Rates per million resident population. Three-year moving averages Implications for care of
EMERGENCYADMISSION FOR
PERFORATION
RATES PER MILLION
RESIDENT
POPULATION. THREEYEAR MOVING
AVERAGES
IMPLICATIONS FOR
CARE OF OLDER
PEOPLE
(Bardhan et al. 2004,
Digestive & Liver Disease
36(9), 577-588)
7. Causes?
CAUSES?Ulcers are only found in white people,
usually in long thin types given to worry
and irritability (Robinson & Bruce 1940)
8. Causes & Risk Factors
CAUSES & RISK FACTORSHelicobacter pylori
90% duodenal ulcers
70-75% gastric ulcers
NSAIDs
Lifestyle factors increase risk – smoking, physical stress, salt
(GU)
Genetic susceptibility / protection against H. pylori infection
(twin studies, mouse models)
Rarely…Zollinger-Ellison syndrome & others
9. Treatment & Outcome (NICE)
TREATMENT & OUTCOME (NICE)10% cases fail treatment (HPA)
1 course of combination therapy clears most cases (74%
duodenal ulcers)
Relapse greater for gastric ulcers (affected by lifestyle
factors). At 3-12 months:
Duodenal ulcers: 39% clear (acid suppression only); 91%
(combination therapy)
Gastric ulcers: 45% clear (acid suppression only); 77%
(combination therapy)
10. Consequences
CONSEQUENCESPrimary care – GP consultations, drug costs (increasing
resistance)
Secondary care – complications, surgery
Tertiary care – rarely needed
Socio-economic cost: Standardised average annual years of
life lost (up to age 75) = 2.6 (per 10,000) (Females=1.8;
Males=3.5) (1999 & 2001 pooled data, ONS)
11. Consequences…
CONSEQUENCES…“Mass eradication of H pylori is impractical because
of…generating antibiotic resistance, so we need to know
how to target prophylaxis.” (Calam & Baron 2001)
Ulcers occurring in absence of H. pylori or NSAIDs / aspirin.
Combination therapies less effective in absence of H. pylori
– data needed
Screening? Cost-effective cost/LYS < £10,000 over 80yrs.
But effects of eradication on morbidity / mortality?
12.
UK Incidence & Prevalence (Time)Increases due to:
• Increase in H.pylori?
• Different strain of H.
pylori?
• Another concurrent gut
infection?
But what about differing
temporal changes of CU
and DU and between men
and women?
Barron & Sonnenberg (2002)
13. UK Incidence & Prevalence (Time)
UK INCIDENCE & PREVALENCE (TIME)Evidence of cohort effect 1970-1986: (Primatesta et al. 1994)
Decreased hospitalized morbidity and mortality
Related more to changes in risk factors (e.g. smoking) in
different cohorts than new pharmacological treatments? implications for public health!
OR: Genetic factors may be more important (Malaty et al.
1994)
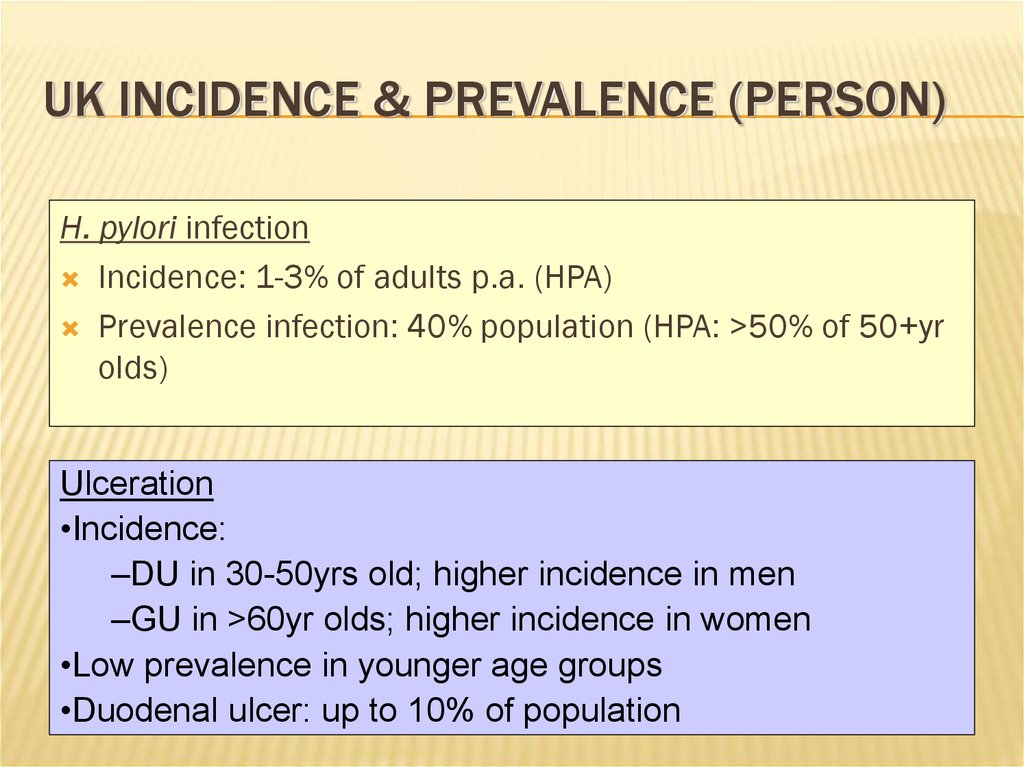
14. UK Incidence & Prevalence (Person)
UK INCIDENCE & PREVALENCE (PERSON)H. pylori infection
Incidence: 1-3% of adults p.a. (HPA)
Prevalence infection: 40% population (HPA: >50% of 50+yr
olds)
Ulceration
•Incidence:
–DU in 30-50yrs old; higher incidence in men
–GU in >60yr olds; higher incidence in women
•Low prevalence in younger age groups
•Duodenal ulcer: up to 10% of population
15. UK Incidence & Prevalence (Person)
UK INCIDENCE & PREVALENCE (PERSON)Current trends:
Annual age-standardized period prevalence decreased 19941998, particularly deprived areas (men 3.3/1000 - 1.5/1000; women
1.8/1000 - 0.9/1000)
Sex incidence evening out – decreasing incidence in young
men; increasing in older women
But emergency admission rates for complications unchanged
in last 30yrs
Kang et al. (2006) – increase in case fatality for DU. Due to
concomitant comorbidity / increasing ulceration (NSAIDs) /
H.pylori (i.e. changing natural history)?
Future decrease in prevalence?
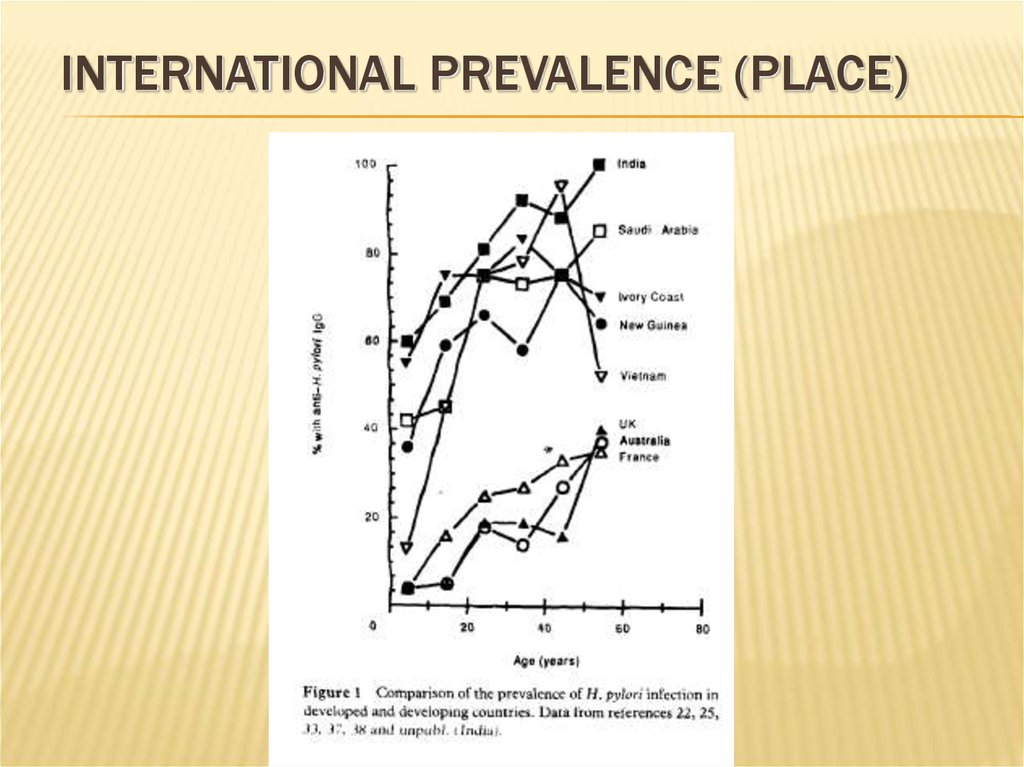
16. International prevalence (Place)
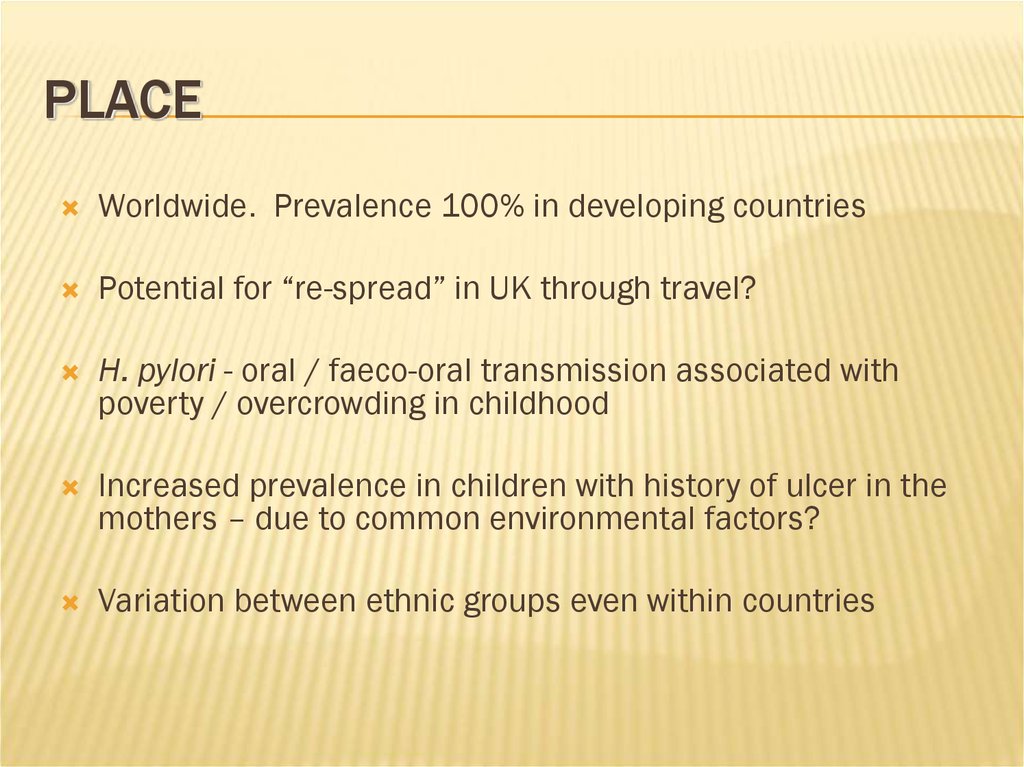
INTERNATIONAL PREVALENCE (PLACE)17. Place
PLACEWorldwide. Prevalence 100% in developing countries
Potential for “re-spread” in UK through travel?
H. pylori - oral / faeco-oral transmission associated with
poverty / overcrowding in childhood
Increased prevalence in children with history of ulcer in the
mothers – due to common environmental factors?
Variation between ethnic groups even within countries
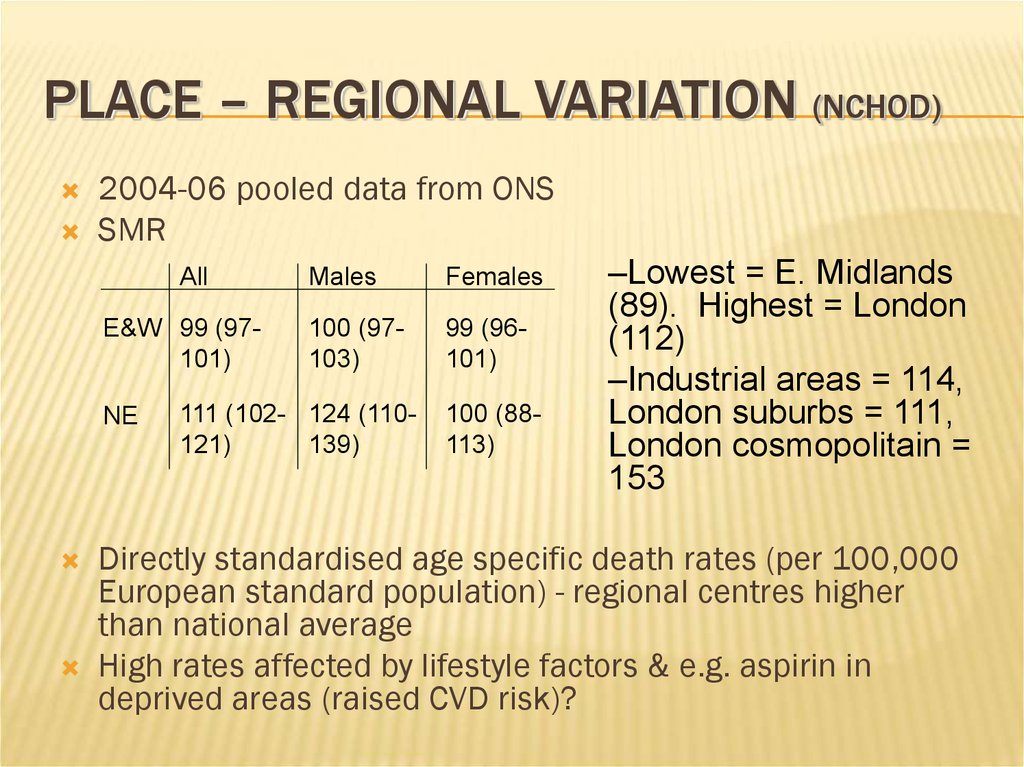
18. Place – Regional variation (NCHOD)
PLACE – REGIONAL VARIATION (NCHOD)2004-06 pooled data from ONS
SMR
All
E&W 99 (97101)
NE
Males
Females
100 (97103)
99 (96101)
111 (102- 124 (110121)
139)
100 (88113)
–Lowest = E. Midlands
(89). Highest = London
(112)
–Industrial areas = 114,
London suburbs = 111,
London cosmopolitain =
153
Directly standardised age specific death rates (per 100,000
European standard population) - regional centres higher
than national average
High rates affected by lifestyle factors & e.g. aspirin in
deprived areas (raised CVD risk)?
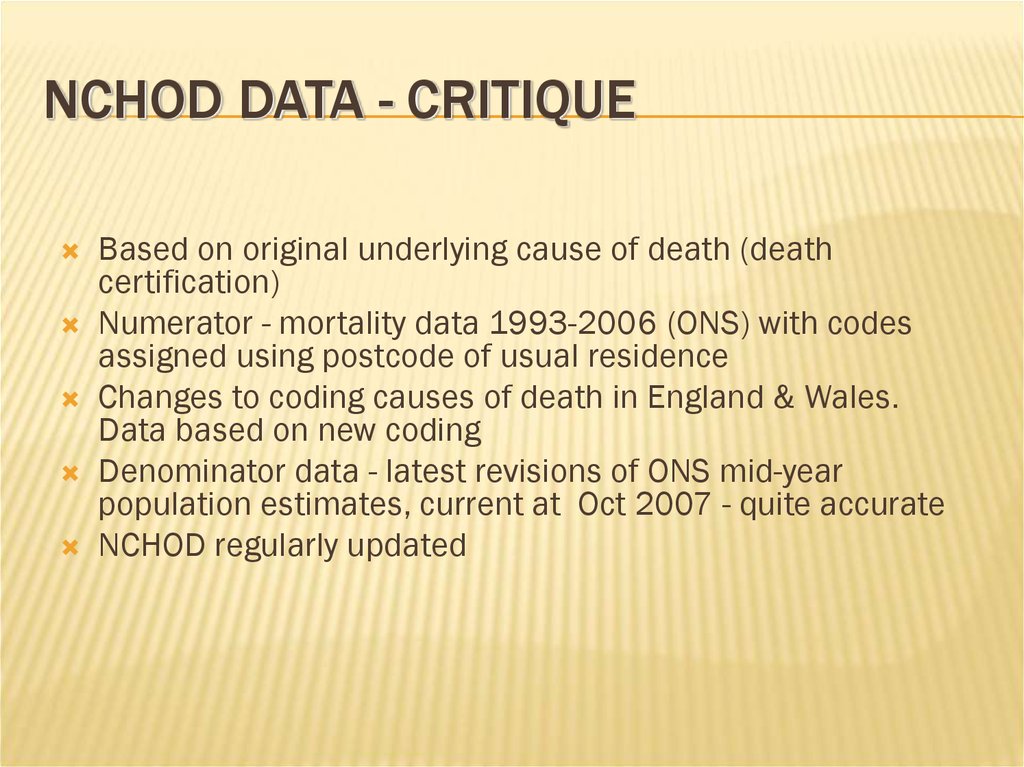
19. NCHOD data - critique
NCHOD DATA - CRITIQUEBased on original underlying cause of death (death
certification)
Numerator - mortality data 1993-2006 (ONS) with codes
assigned using postcode of usual residence
Changes to coding causes of death in England & Wales.
Data based on new coding
Denominator data - latest revisions of ONS mid-year
population estimates, current at Oct 2007 - quite accurate
NCHOD regularly updated
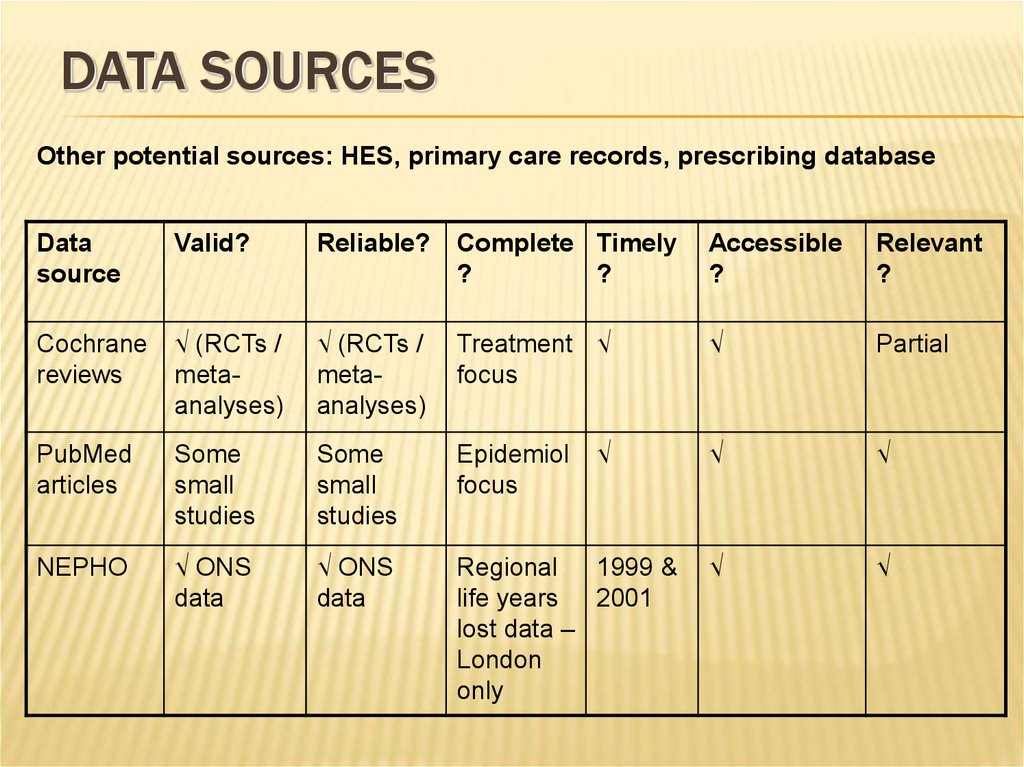
20. Data sources
DATA SOURCESOther potential sources: HES, primary care records, prescribing database
Data
source
Valid?
Reliable?
Complete Timely
?
?
Accessible
?
Relevant
?
Cochrane
reviews
√ (RCTs /
metaanalyses)
√ (RCTs /
metaanalyses)
Treatment √
focus
√
Partial
PubMed
articles
Some
small
studies
Some
small
studies
Epidemiol
focus
√
√
√
NEPHO
√ ONS
data
√ ONS
data
Regional
1999 &
life years 2001
lost data –
London
only
√
√
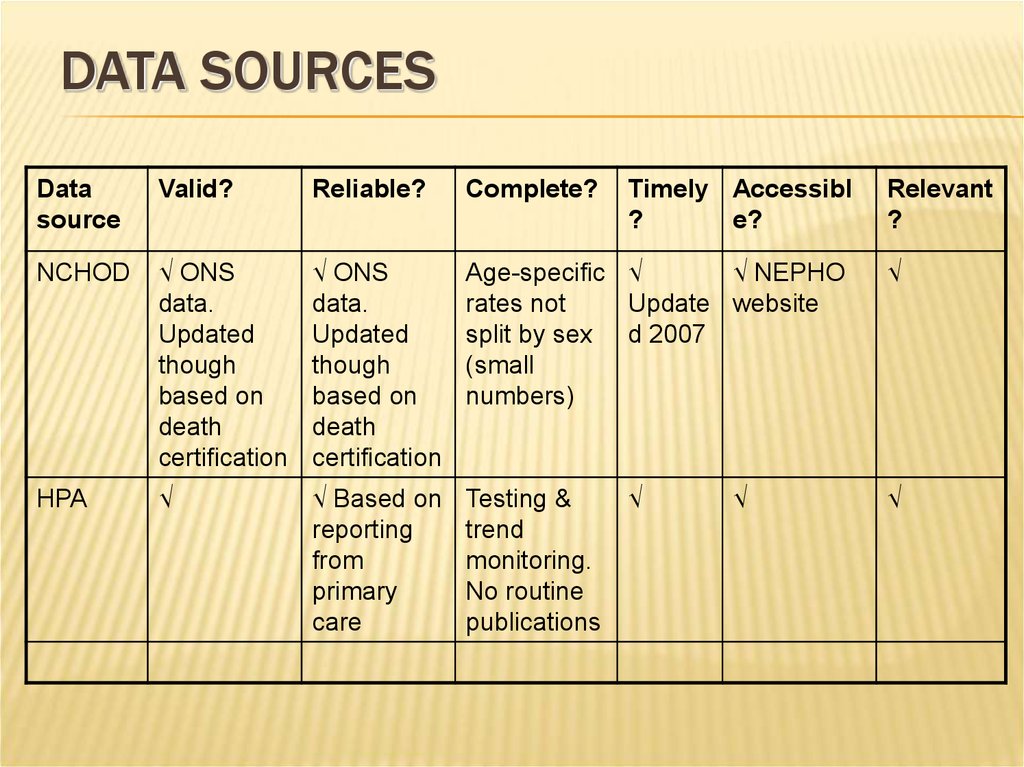
21. Data sources
DATA SOURCESData
source
Valid?
Reliable?
Complete?
Timely Accessibl
?
e?
NCHOD
√ ONS
data.
Updated
though
based on
death
certification
√ ONS
data.
Updated
though
based on
death
certification
Age-specific √
√ NEPHO
rates not
Update website
split by sex d 2007
(small
numbers)
HPA
√
√ Based on
reporting
from
primary
care
Testing &
trend
monitoring.
No routine
publications
√
√
Relevant
?
√
√
22. Data sources
DATA SOURCESData
Valid?
source
Reliable?
Complete Timely?
?
Accessible
?
Relevant
?
Patient √ NICE
UK
guidance &
review
articles.
Written by
clinicians.
Reviewed
18monthly
√ NICE
guidance
& review
articles.
Written by
clinicians.
Reviewed
18monthly
Patient
info.
√ Based
on recent
guidance
& articles
√
√
Patient √ Peer
Plus
reviewed.
Based on
NICE
guidance &
review
articles.
Written by
clinicians.
√ Peer
reviewed.
Based on
NICE
guidance
& review
articles.
Written by
clinicians.
Clinical
focus –
diagnosis
and
managem
ent
√ Based
on recent
guidance
& articles
√
Partial
23. Conclusion
CONCLUSIONDisease mechanism / transmission poorly understood
Risk factors multiple & interacting
H. pylori is main cause but has changing natural history
“Each generation has carried its own particular risk of bearing
ulcers throughout adult life” (Susser & Stein 1962)
Current pattern = exposure to H. pylori + genetics + exposure to
drugs + environmental / behavioural factors
DU / GU likely to continue causing significant chronic disease
burden and personal / societal cost. Predicting future pattern
difficult
24.
Used books• Tuberculosis Fact sheet N°104". WHO.
October 2015. Retrieved 11 February 2016.
• "Basic TB Facts". CDC. March 13, 2012.
Retrieved 11 February 2016
• Medical Laboratory Science: Theory and
Practice. New Delhi: Tata McGraw-Hill. 2000.
p. 473
• "Acid-Fast Stain Protocols". 21 August 2013.
Retrieved 26 March 2016.
• Wkipedia.org






 medicine
medicine