Similar presentations:
Acute Pancreatitis
1.
Acute PancreatitisDr. Eddie Koifman
Gastroenterology Dpt.
RAMBAM
2.
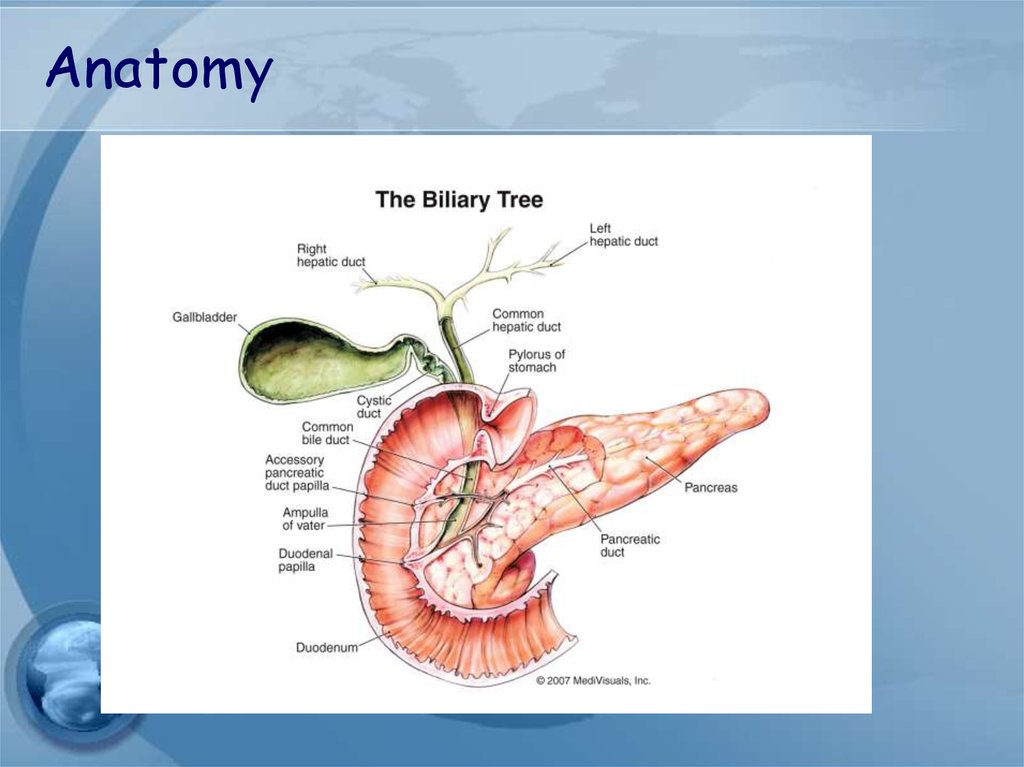
Anatomy3.
4.
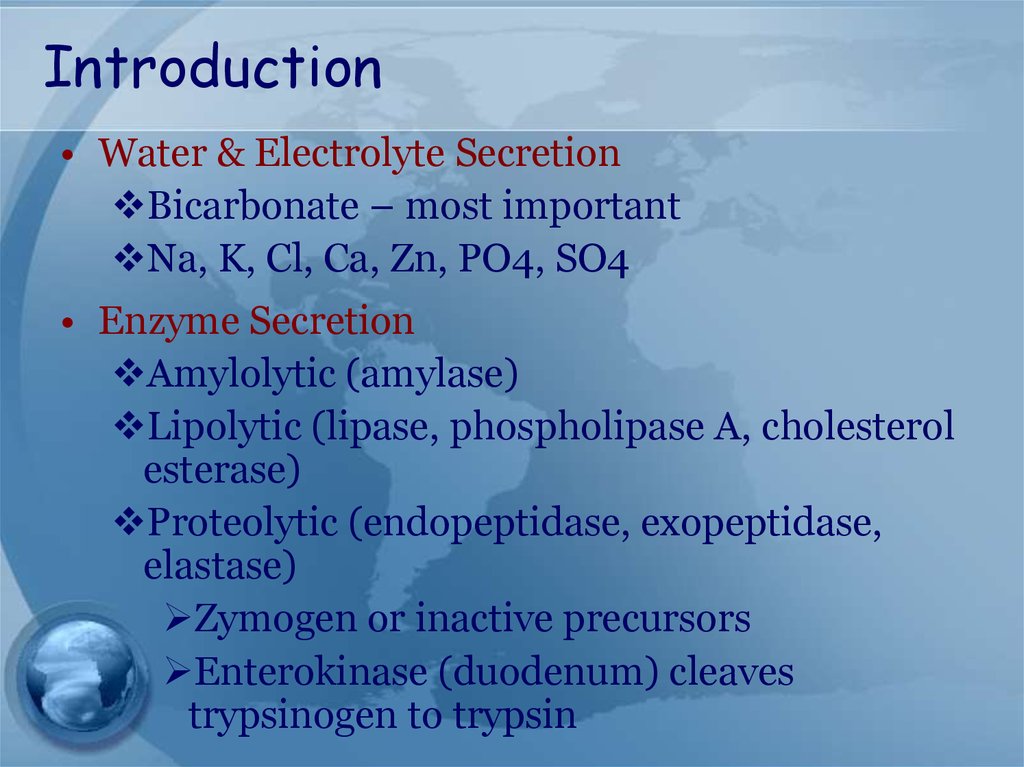
Introduction• Water & Electrolyte Secretion
Bicarbonate – most important
Na, K, Cl, Ca, Zn, PO4, SO4
• Enzyme Secretion
Amylolytic (amylase)
Lipolytic (lipase, phospholipase A, cholesterol
esterase)
Proteolytic (endopeptidase, exopeptidase,
elastase)
Zymogen or inactive precursors
Enterokinase (duodenum) cleaves
trypsinogen to trypsin
5.
What are the two most commonetiologies for acute pancreatitis
in the western civilization?
1.
2.
3.
4.
5.
Drugs and alcohol
Neoplastic and metabolic
Bile stones and alcohol
Structural and drugs
Toxic and idiopathic
6.
Etiology7.
8.
Gallstone pancreatitis• Mechanism is not entirely clear
• Common-channel theory
“Blockage below junction of biliary and
pancreatic duct cause bile flow into
pancreas”
BUT…
– short channel that stone located would
block both biliary and pancreatic duct
– Hydrostatic pressure in biliary<pancreatic
duct
9.
Mechanism???• Ductal hypertension
– Cause rupture of small ducts and
leakage of pancreatic juice
– pH in pancreatic tissue ↓
– activation of protease
– “Colocalization”
10.
Alcoholic pancreatitisCommon in pt. alcohol drinking > 2yr.
Often much longer up to 10 yr.
Sphincter spasm
Decrease pancreatic blood flow
11.
12.
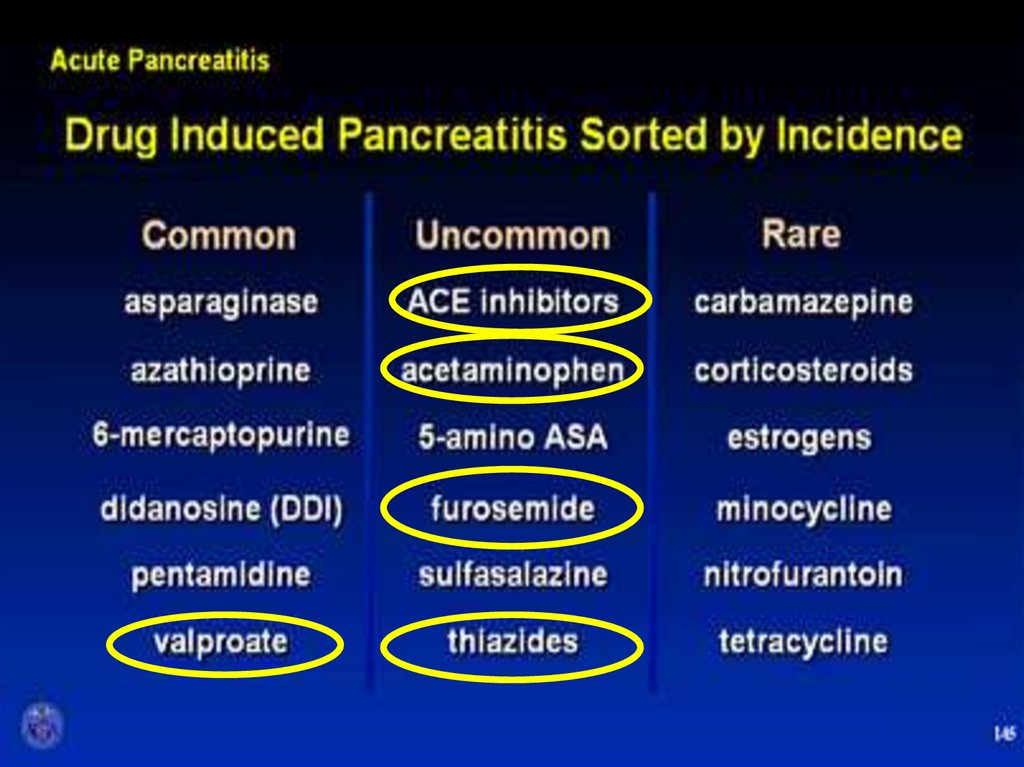
Which of the following drugs iswell known for it’s ability to
induce pancreatitis?
1.
2.
3.
4.
Propranolol
Erythromycin
Azathioprin
Codein
13.
14.
AGA Institute15.
Diagnosis16.
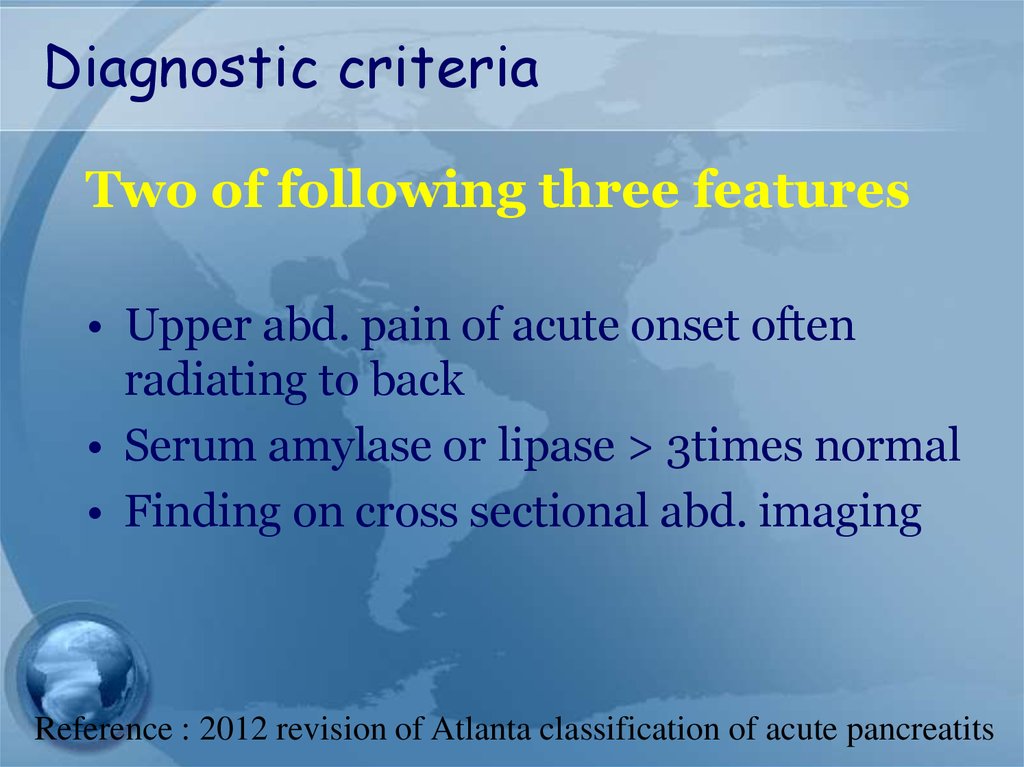
Diagnostic criteriaTwo of following three features
• Upper abd. pain of acute onset often
radiating to back
• Serum amylase or lipase > 3times normal
• Finding on cross sectional abd. imaging
Reference : 2012 revision of Atlanta classification of acute pancreatits
17.
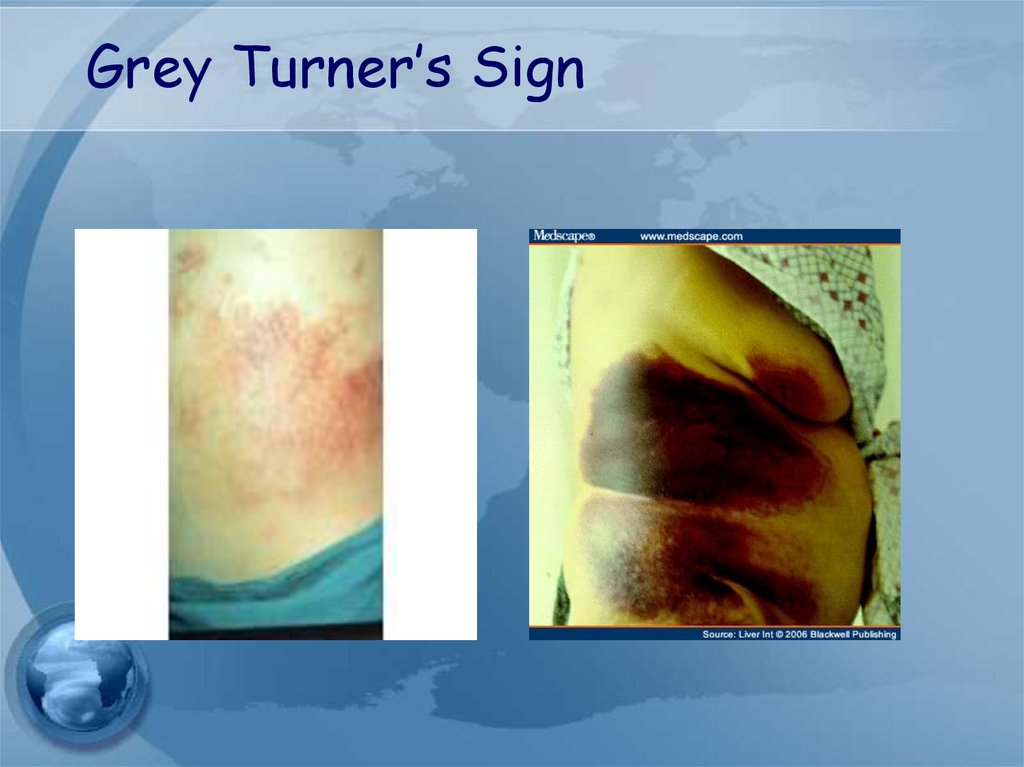
Physical exam• Grey Turner’s Sign
- ecchymosis in 1 or both flanks
• Cullen’s sign
- ecchymosis in periumbilical area
• Associated with Necrotizing pancreatitis
• poor prognosis occurs in 1% of cases
18.
Grey Turner’s Sign19.
Cullen’s Sign20.
Serum markers21.
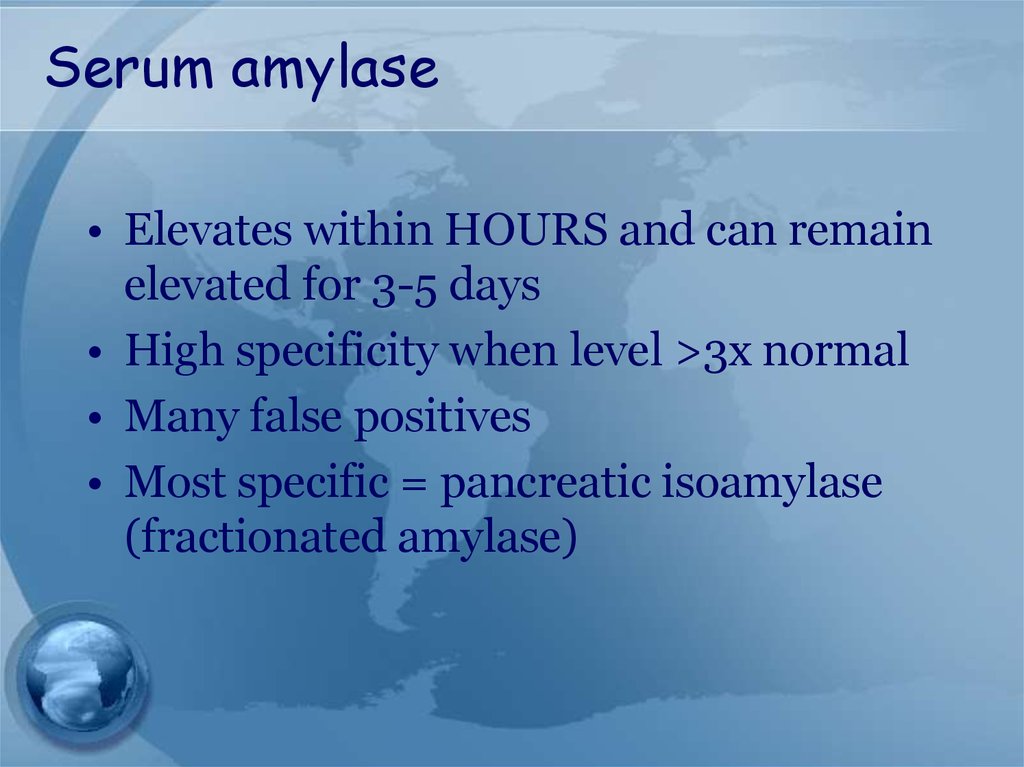
Serum amylase• Elevates within HOURS and can remain
elevated for 3-5 days
• High specificity when level >3x normal
• Many false positives
• Most specific = pancreatic isoamylase
(fractionated amylase)
22.
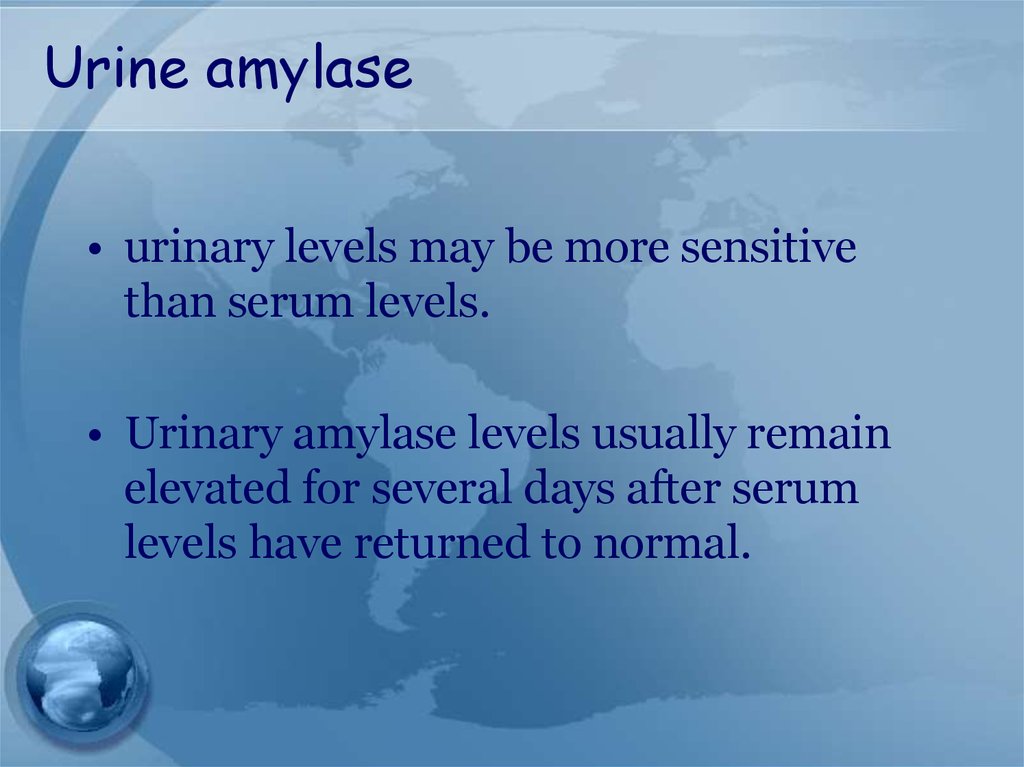
Urine amylase• urinary levels may be more sensitive
than serum levels.
• Urinary amylase levels usually remain
elevated for several days after serum
levels have returned to normal.
23.
Serum lipase• The preferred test for diagnosis
• Begins to increase 4-8H after onset of
symptoms and peaks at 24H
• Remains elevated for days
• Sensitivity 86-100% and Specificity 6099%
• >3X normal S&S ~100%
24.
Slide 18925.
Plain Abdominal Radiograph26.
Plain Abdominal RadiographBowel ileus
“Sentinel Loop”
“Colon cut off sign”
Loss of psoas shadow
• Helps exclude other causes of
abdominal pain: bowel obstruction and
perforation
27.
Radiologic Findings• Plain radiographs contribute little
• Ultrasound may show the pancreas in
only 25-50%
• CT scan provides better information
–Severity and prognosis
–Exclusion of other diseases
• EUS & MRI with MRCP – cause of
pancreatitis
28.
Assessment of severity29.
Classification of severity- Mild : lack of organ failure or
systemic complications
- Moderate : transient organ failure
and/or complications < 48hr
- Severe : persistent organ failure and
systemic complications
Reference : 2012 revision of Atlanta classification of acute pancreatitis
30.
Complication31.
Which of the following is notconsidered adverse prognostic
feature in acute pancreatitis?
1. WBC> 16,000
2. Amylase> 1000
3. Glucose> 200
4. PaO2< 60
5. Age> 55
32.
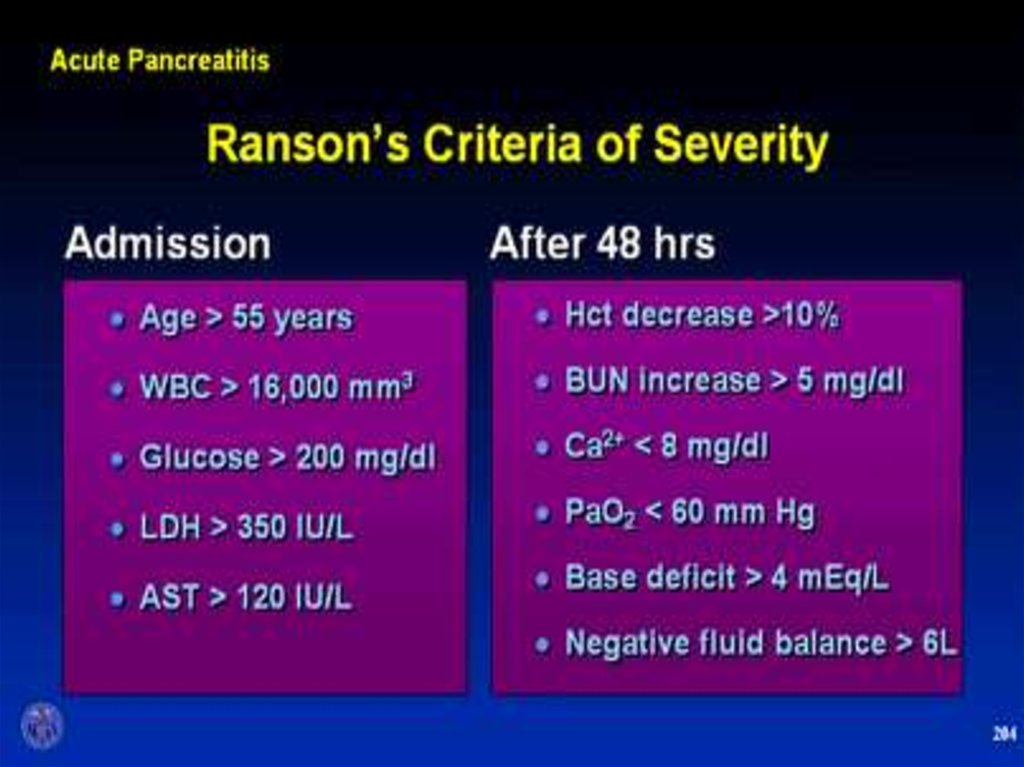
Early prognostic signs• Ranson’s score
• APACHE II
33.
34.
Ranson’s Criteria (GB Pancreatitis)• At Admission
Age > 70 yr
WBC > 18,000/mm3
Blood glucose > 220 mg/dL
Serum lactate dehydrogenase > 400IU/L
Serum aspartate aminotransferase >250IU/L
• During Initial 48 hr
Hematocrit decrease of > 10%
BUN increase of >2 mg/dL
Serum calcium <8mg/dL
Arterial pO2 NA
Serum base deficit > 5 mEq/Lio
Fluid sequestration > 4L
35.
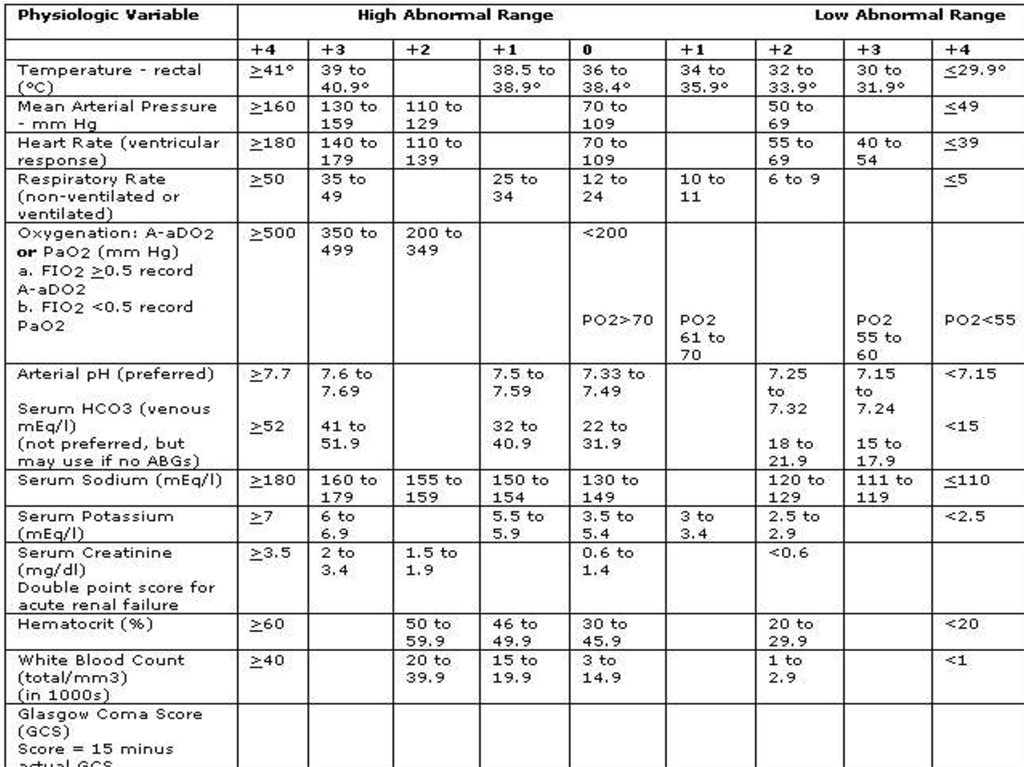
APACHE II• Measure at during the first 24 hours
after admission
• Using a cutoff of ≥8
• The American Gastroenterological
Association (AGA) recommends:
Prediction of severe disease by the
APACHE II system
36.
APACHE II37.
Biochemical marker• CRP at 48hr
– cutoff 150mg/L
– Sens. 80%
– Spec. 76%
• TAP
• Interleukins
• ???
38.
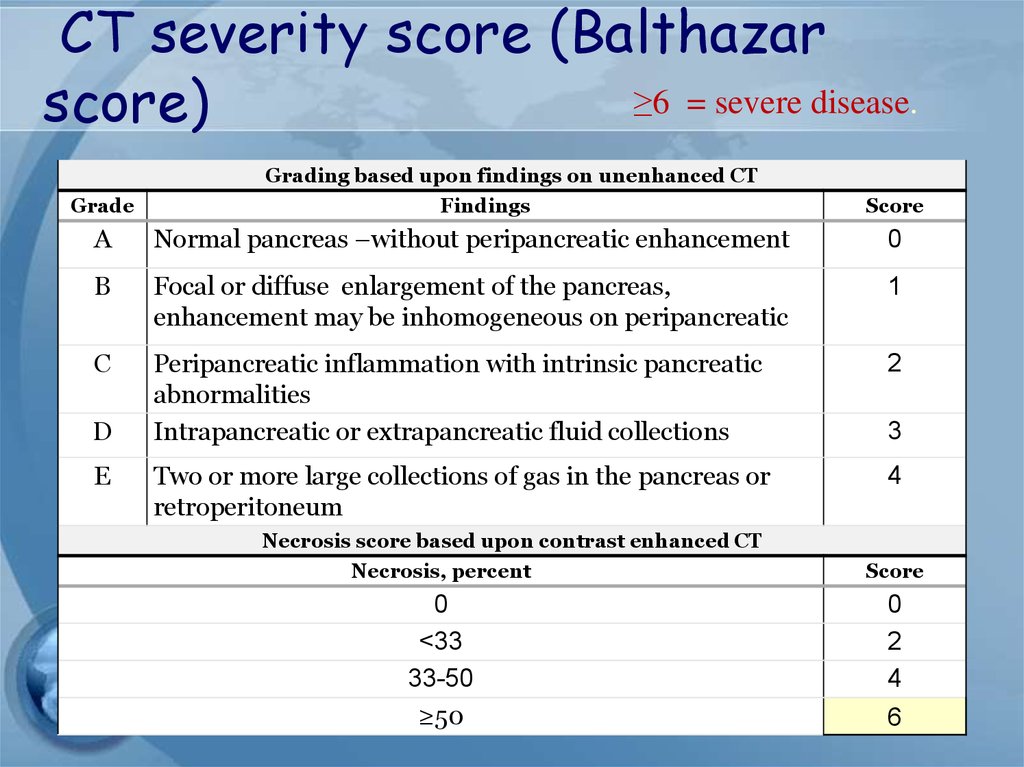
CT severity score (Balthazar≥6 = severe disease.
score)
Grading based upon findings on unenhanced CT
Grade
Findings
Score
A
Normal pancreas –without peripancreatic enhancement
0
B
Focal or diffuse enlargement of the pancreas,
enhancement may be inhomogeneous on peripancreatic
1
C
Peripancreatic inflammation with intrinsic pancreatic
abnormalities
Intrapancreatic or extrapancreatic fluid collections
2
Two or more large collections of gas in the pancreas or
retroperitoneum
4
D
E
3
Necrosis score based upon contrast enhanced CT
Necrosis, percent
Score
0
<33
33-50
≥50
0
2
4
6
39.
40.
Treatment41.
Treatment• General Considerations
- adequate IV hydration and analgesia
- NPO
- NG tube: not routinely used
* But may be used in patients with ileus or intractable N/V
• Nutrition
• Early enteral feeding
• Nasojejunal tube feeding
• PPN,TPN
42.
Treatment• Metabolic Complications
- Correction of electrolyte imbalance - Ca,Mg
- Cautiously for hyperglycemia
• Cardiovascular Care
• Respiratory Care
• Deep vein thrombosis prophylaxis
43.
Prophylactic antibiotics–Although this is still an area of debate
–Not indicated for mild attack
–suggest imipenem or meropenem
for 14 days for patients with proven
necrosis
44.
TREATMENT OFASSOCIATED CONDITIONS
• Gallstone pancreatitis
– ERCP should be performed within 72
hours in those with a high suspicion of
persistent bile duct stones
– EUS & MRCP should be considered in case
that clinical is not improving sufficiently
– Cholecystectomy +/- IOC
45.
Cholecystectomy??• should be performed after recovery in all
patient with gallstone pancreatitis
• Failure to perform a cholecystectomy
is associated with a 25-30% risk of recurrent
acute pancreatitis, cholecystitis, or cholangitis
within 6-18 weeks
46.
Cholecystectomy• In mild pancreatitis case, can usually be
performed safely within 7 days after recovery
• In severe pancreatitis case ,delaying for at
least 3 wks may be reasonable
• If high suspicion of CBD stones, preoperative
ERCP is the best test that therapeutic
intervention will be required
• If low suspicion,intraoperative cholangiogram
during cholecystectomy may be preferable to
avoid the morbidity associated with ERCP
47.
Complications48.
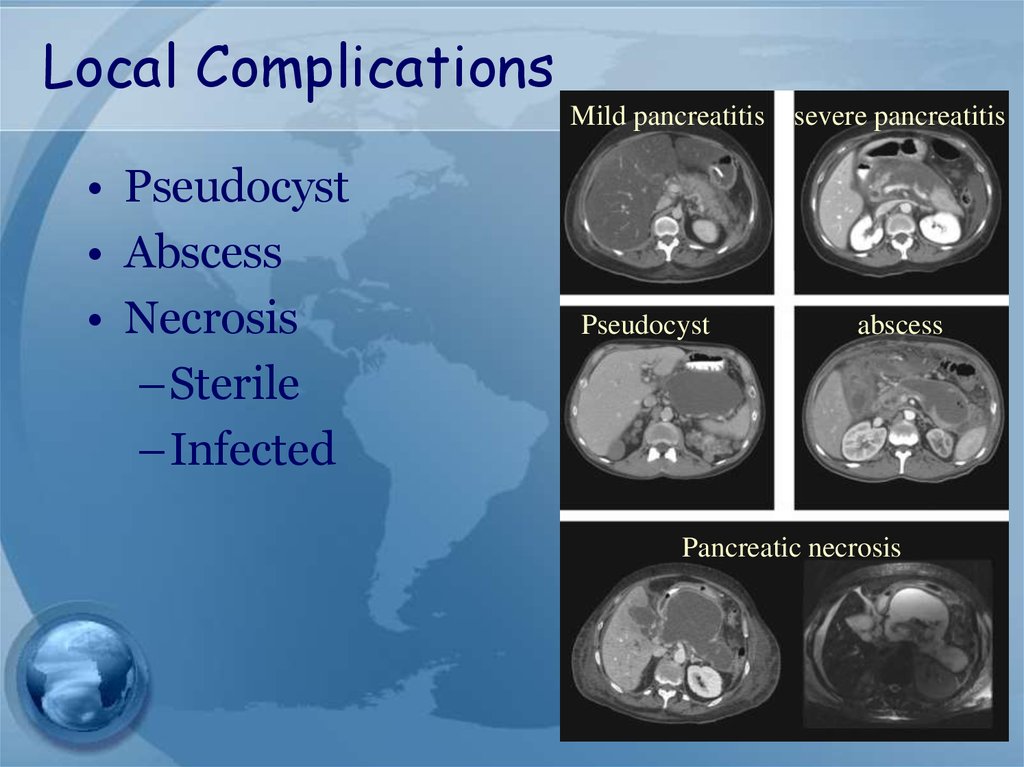
Local ComplicationsMild pancreatitis
• Pseudocyst
• Abscess
• Necrosis
–Sterile
–Infected
Pseudocyst
severe pancreatitis
abscess
Pancreatic necrosis
49.
Infected pancreatic necrosis.• The most common organisms include E.coli,
Pseudomonas, Klebsiella, and Enterococcus
50.
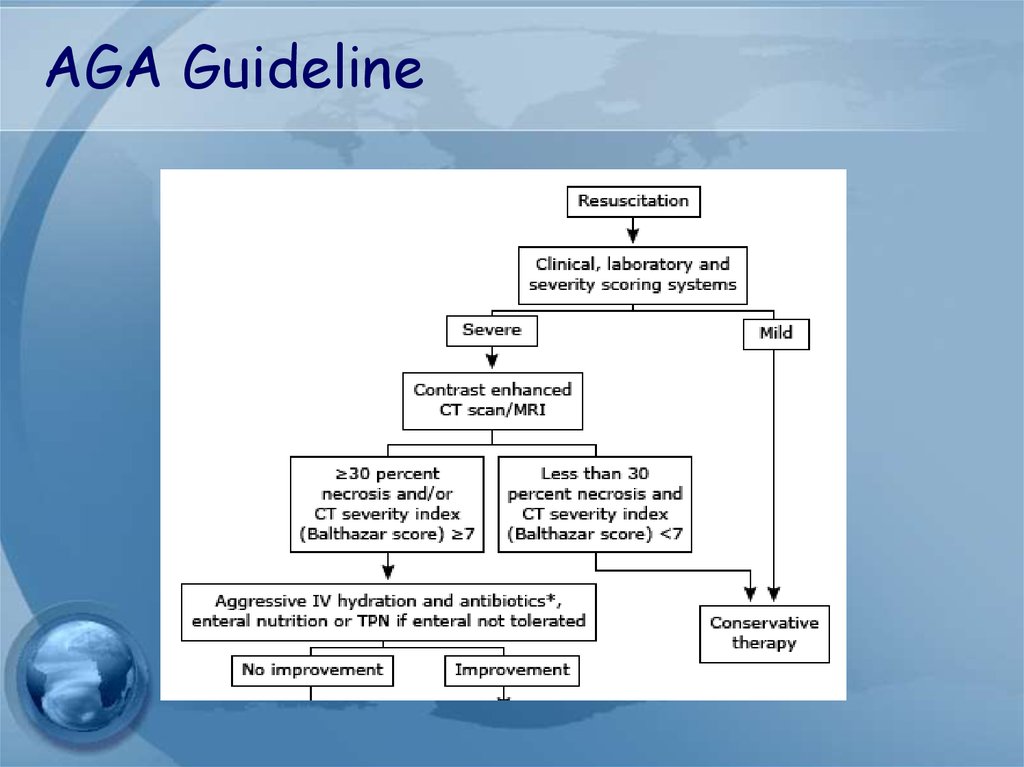
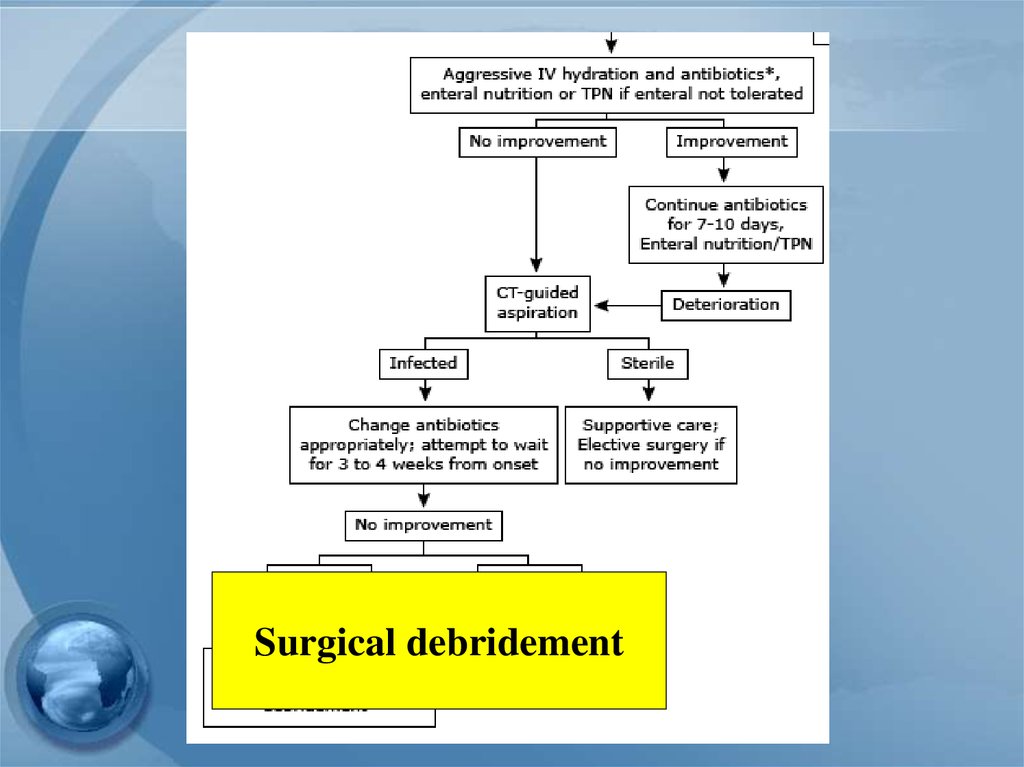
Guideline management ofsevere pancreatitis
51.
AGA Guideline52.
Surgical debridement53.
Management of pseudocyst54.
Management of pseudocyst• Watchful waiting:
- Operative intervention was recommended
following an observation period of 6 wks
- However, there are some reports support
more conservative approach
55.
Management of pseudocyst• Surgical drainage – gold standard
Open vs endoscopic
–cystgastrostomy
–Cystenterostomy
–Cystojejunostomy, Cystoduodenostomy
–Ressection
56.
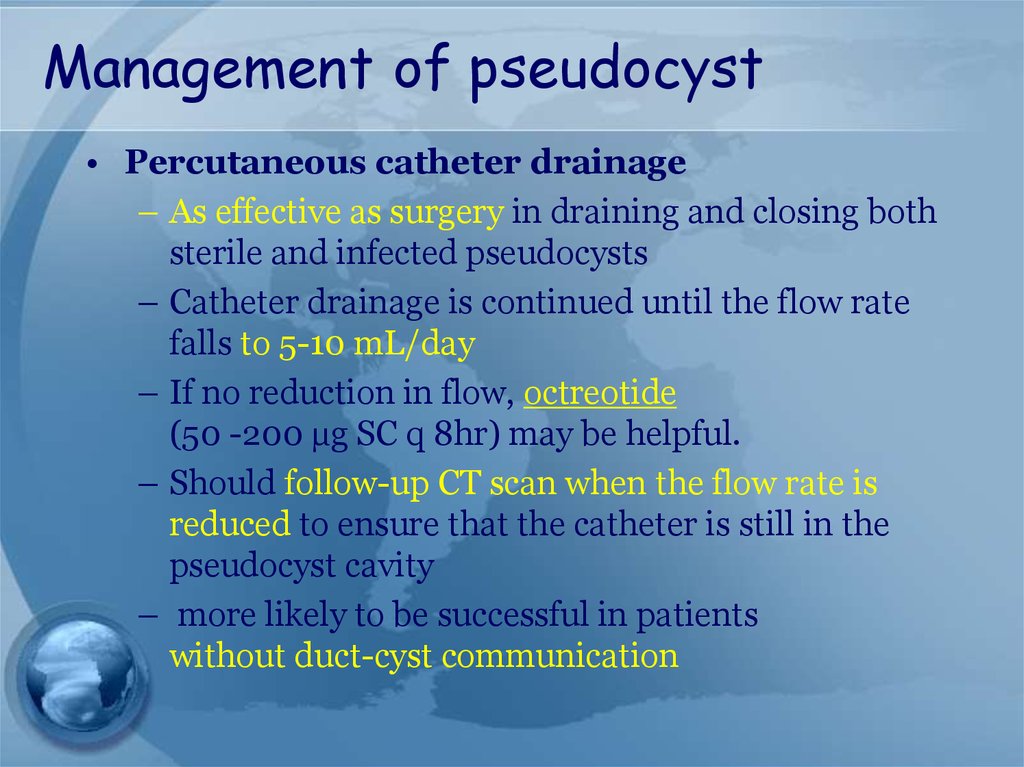
Management of pseudocyst• Percutaneous catheter drainage
– As effective as surgery in draining and closing both
sterile and infected pseudocysts
– Catheter drainage is continued until the flow rate
falls to 5-10 mL/day
– If no reduction in flow, octreotide
(50 -200 µg SC q 8hr) may be helpful.
– Should follow-up CT scan when the flow rate is
reduced to ensure that the catheter is still in the
pseudocyst cavity
– more likely to be successful in patients
without duct-cyst communication
57.
Management of localcomplication of pancreatitis
58.
Indication forpancreatic debridement
• Infected pancreatic necrosis
• Symptomatic sterile pancreatic necrosis
• chronic low grade fever
• Nausea
• Lethargy
• Inability to eat
• * Fail medical treatment
59.
Timing of debridement• The optimal timing is at least 3-4wks
following the onset of acute pancreatitis.
• Delayed debridement allows
– clinical stabilization of the patient
– resolution of early organ failure
– decreased inflammatory reaction, and
necrotic areas are demarcated
































 medicine
medicine