Similar presentations:
Cardiovascular system. Systolic blood pressure
1. CARDIOVASCULAR SYSTEM
2. Plan of the lectures
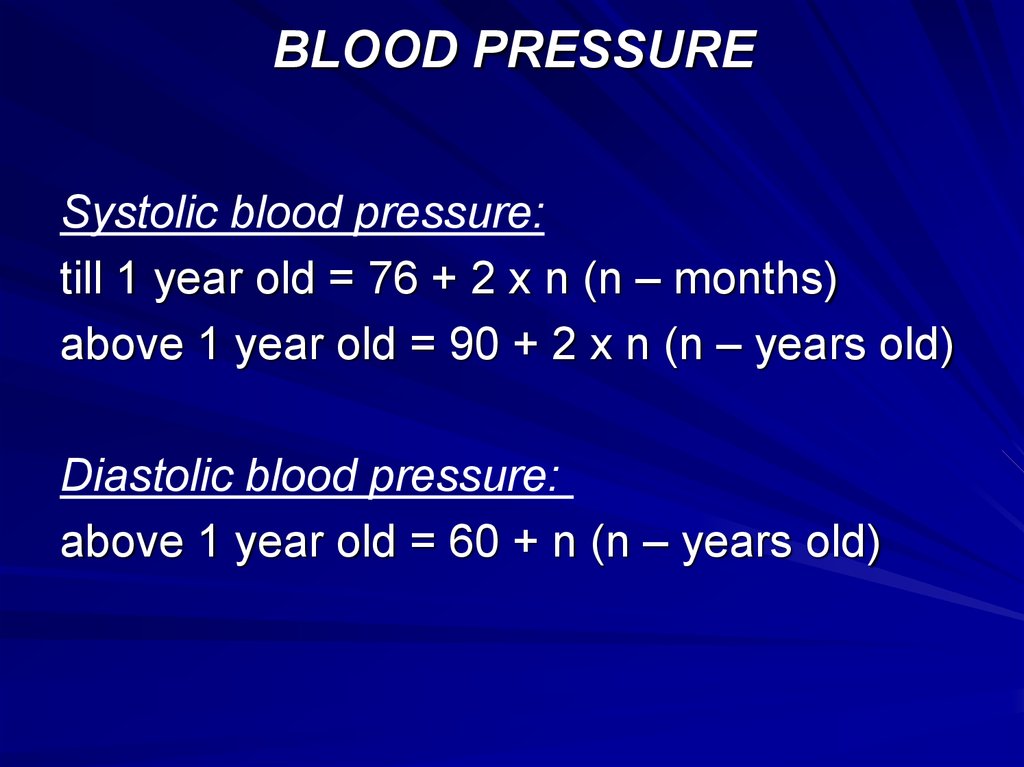
1. Semiotic of disorders of CVS.3. BLOOD PRESSURE
Systolic blood pressure:till 1 year old = 76 + 2 x n (n – months)
above 1 year old = 90 + 2 x n (n – years old)
Diastolic blood pressure:
above 1 year old = 60 + n (n – years old)
4. COMPLAINS
WeaknessFatigability
Disorders of appetite
Dyspnoea
Color of the skin: cyanosis or paleness
Pain of the heart region
Headache
Palpitation
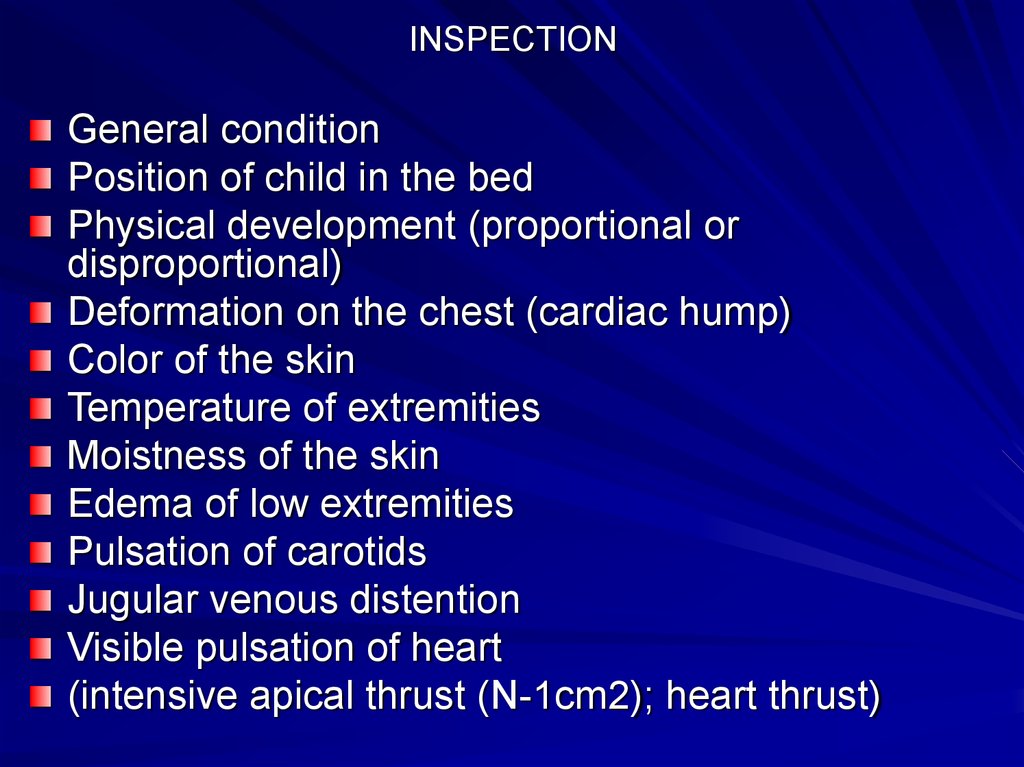
5. INSPECTION
General conditionPosition of child in the bed
Physical development (proportional or
disproportional)
Deformation on the chest (cardiac hump)
Color of the skin
Temperature of extremities
Moistness of the skin
Edema of low extremities
Pulsation of carotids
Jugular venous distention
Visible pulsation of heart
(intensive apical thrust (N-1cm2); heart thrust)
6. PALPATION
Localization of apical thrustCardiac thrust
Trembling above the mitral valve and it’s
characteristic
Presents of cat’s purr
7. Estimation of pulse:
Rhythm (N - respiratory arrhythmia revealsfrom 2 till 10 years old)
Rate
Symmetric
Synchronic
Tension
Size
8. PERCUSSION
Method of percussion of children over 4years old is same with adults.
Until 4 years old use modification.
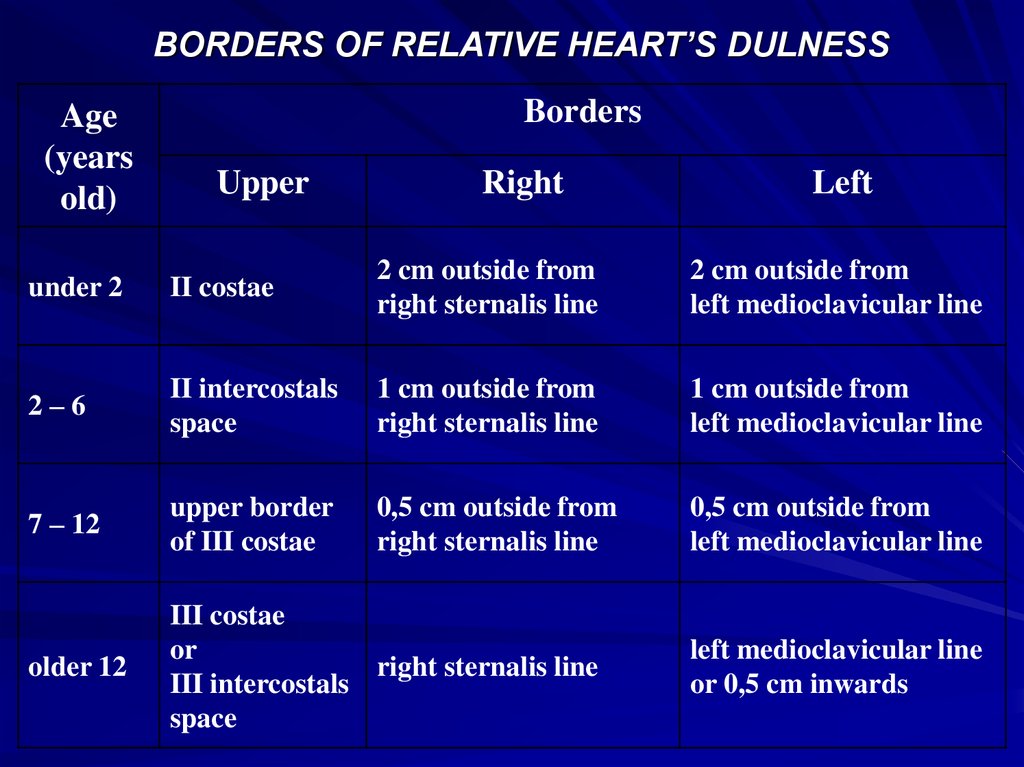
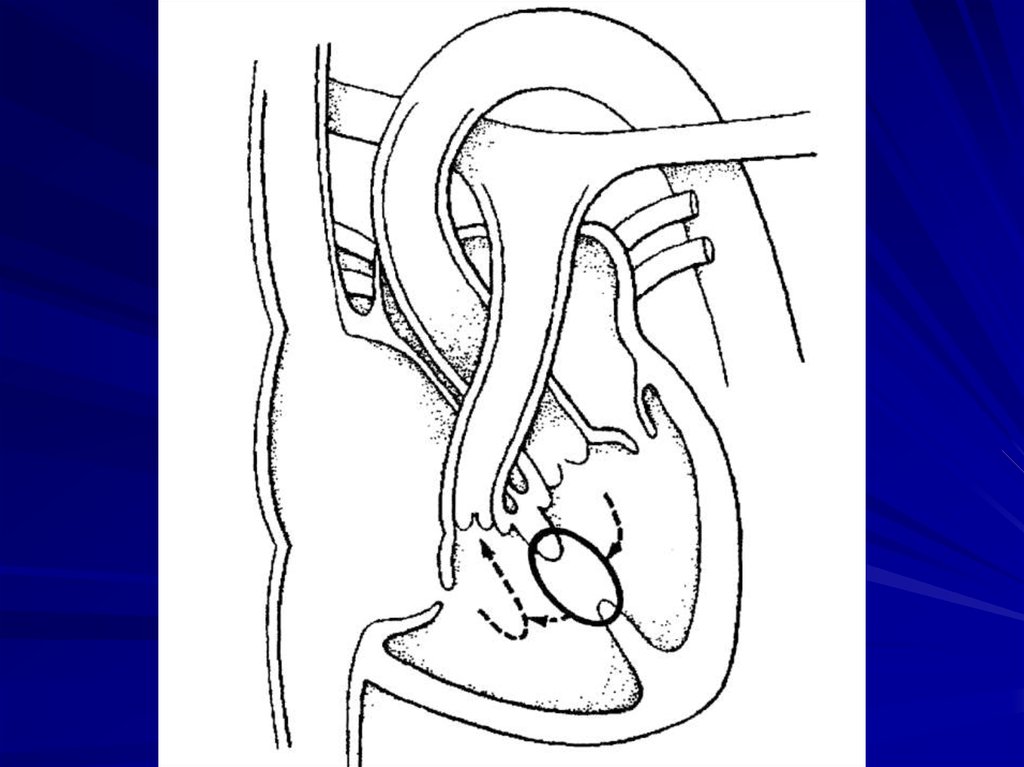
9. BORDERS OF RELATIVE HEART’S DULNESS
Age(years
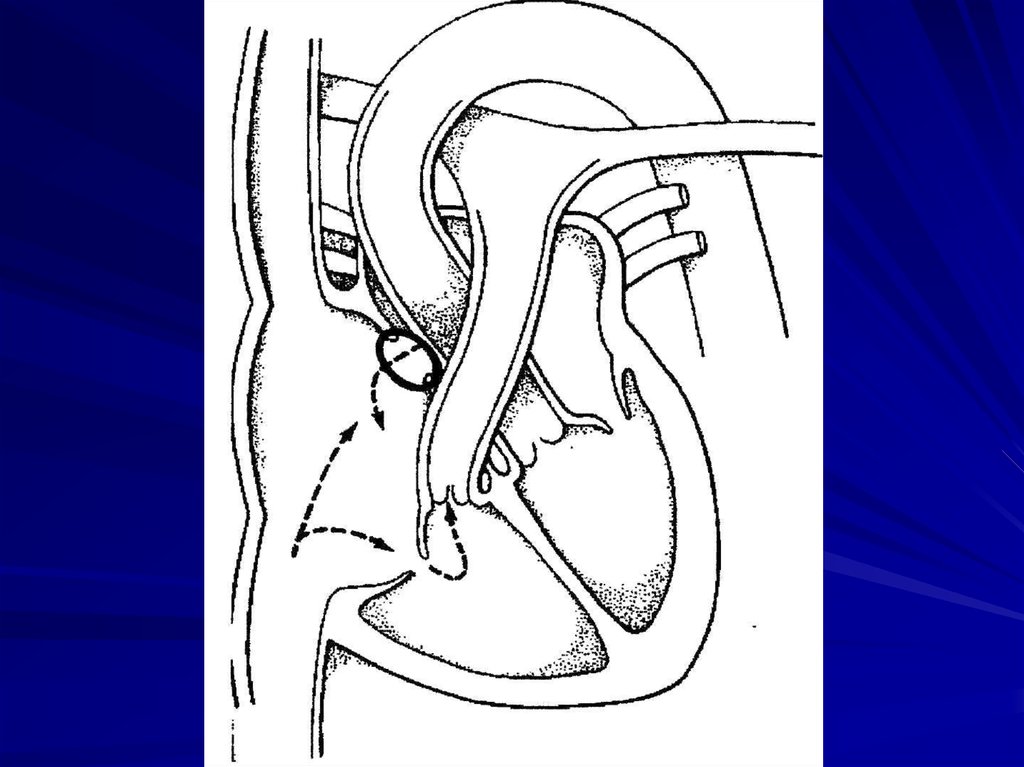
old)
Borders
Upper
Right
Left
under 2
II costae
2 cm outside from
right sternalis line
2 cm outside from
left medioclavicular line
2–6
II intercostals
space
1 cm outside from
right sternalis line
1 cm outside from
left medioclavicular line
7 – 12
upper border
of III costae
0,5 cm outside from
right sternalis line
0,5 cm outside from
left medioclavicular line
older 12
III costae
or
right sternalis line
III intercostals
space
left medioclavicular line
or 0,5 cm inwards
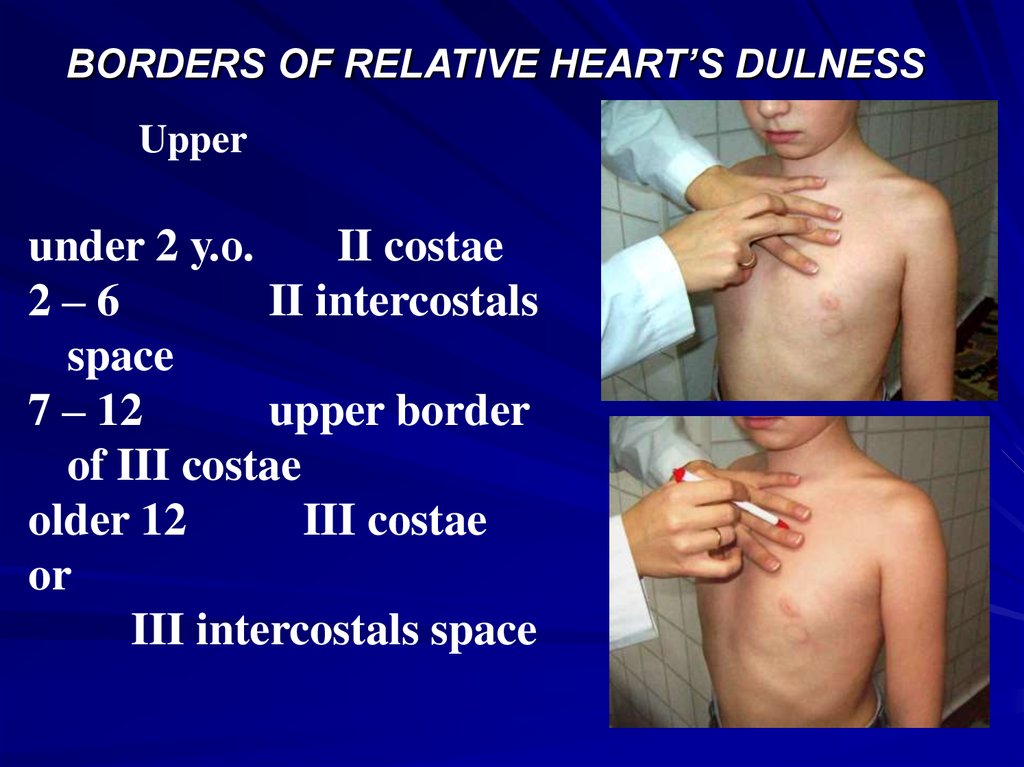
10. BORDERS OF RELATIVE HEART’S DULNESS
Upperunder 2 у.о.
II costae
2–6
II intercostals
space
7 – 12
upper border
of III costae
older 12
III costae
or
III intercostals space
11. Right
under 22 cm outside from
right sternalis line
2–6
1 cm outside from
right sternalis line
7 – 12
0,5 cm outside from
right sternalis line
older 12
right sternalis line
12. apical thrust
4 intercostals space to theleft of sternum (5) from left
medioclavicular line
13. Left
under 22 cm outside from
left medioclavicular line
2–6
1 cm outside from
left medioclavicular line
7 – 12
0,5 cm outside from
left medioclavicular line
older 12
or
left medioclavicular line
0,5 cm inwards
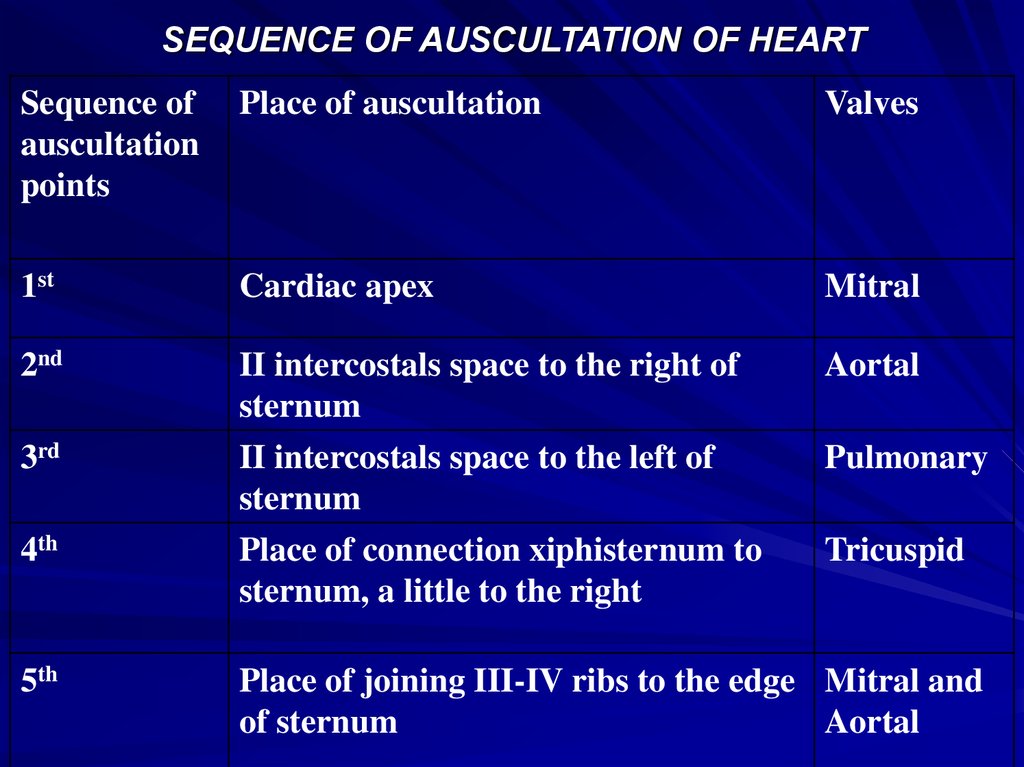
14. SEQUENCE OF AUSCULTATION OF HEART
Sequence ofauscultation
points
Place of auscultation
Valves
1st
Cardiac apex
Mitral
2nd
II intercostals space to the right of
sternum
II intercostals space to the left of
sternum
Place of connection xiphisternum to
sternum, a little to the right
Aortal
3rd
4th
5th
Pulmonary
Tricuspid
Place of joining III-IV ribs to the edge Mitral and
of sternum
Aortal
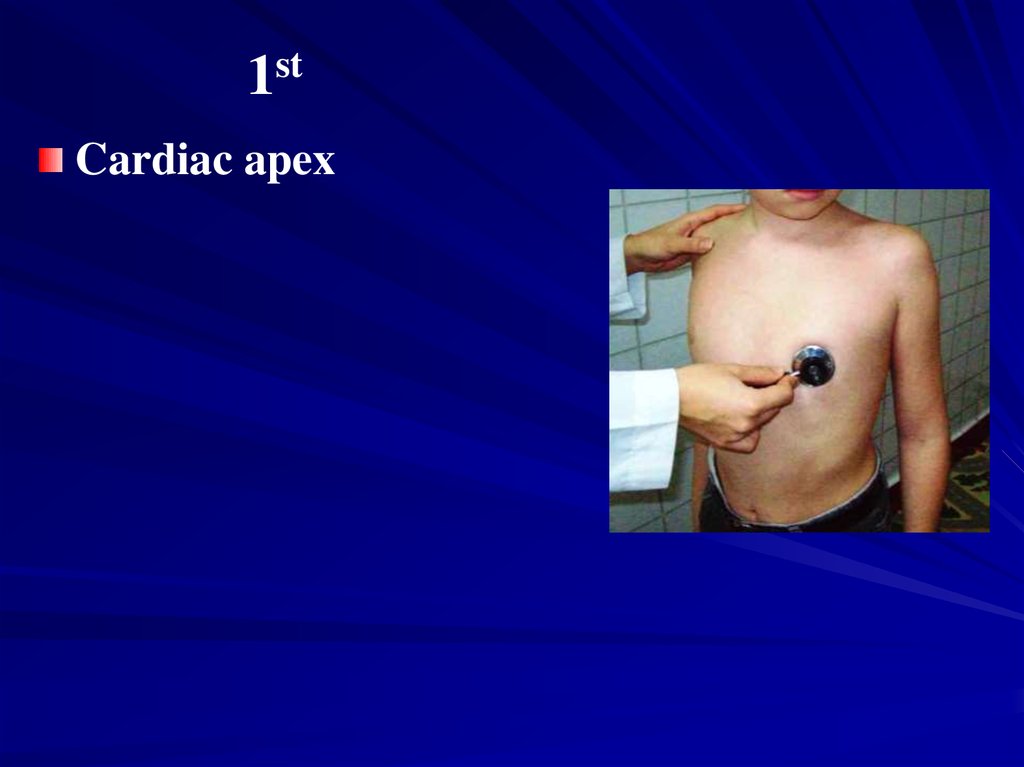
15. 1st
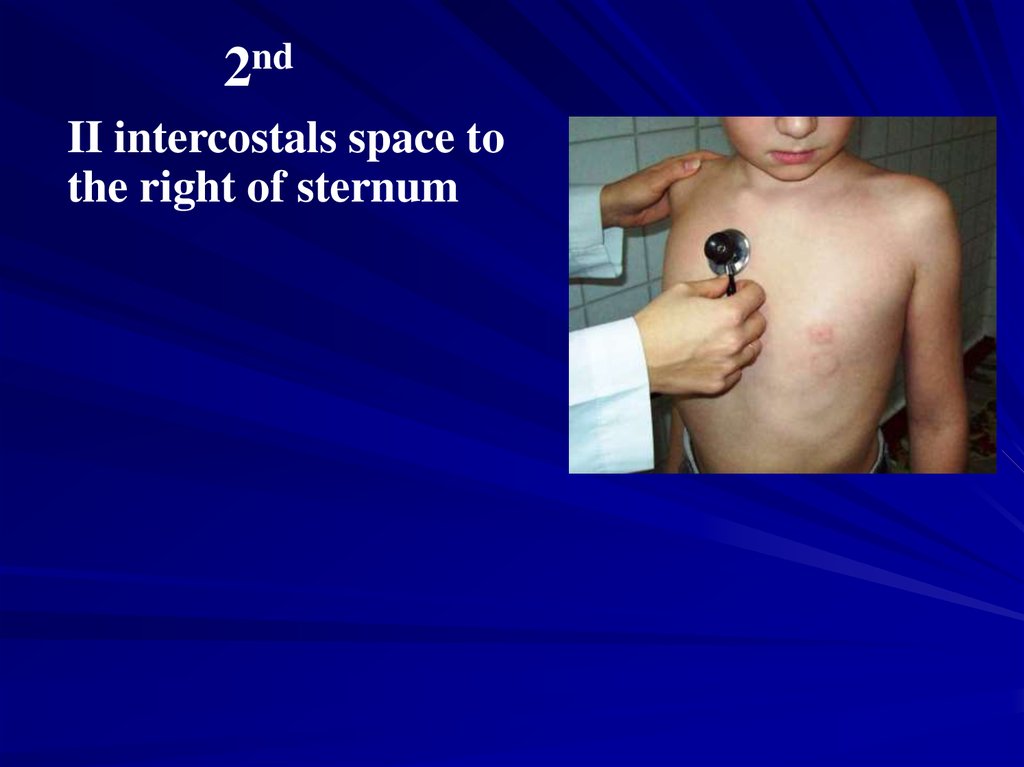
Cardiac apex16. 2nd
II intercostals space tothe right of sternum
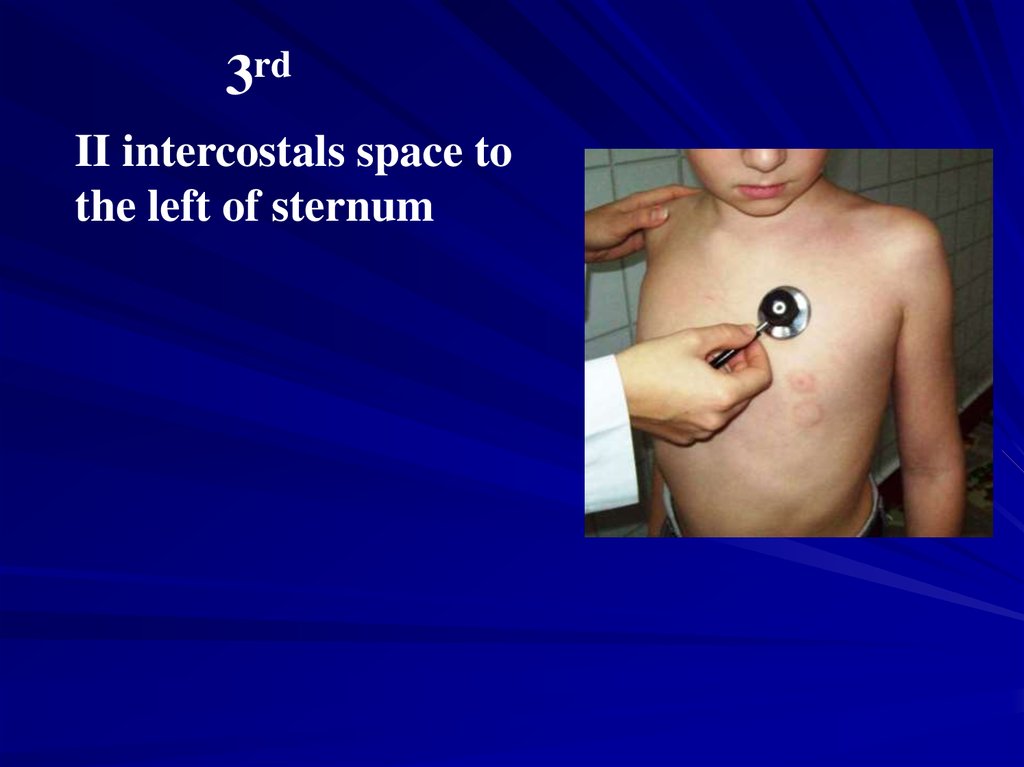
17. 3rd
II intercostals space tothe left of sternum
18. 4th
Place ofconnection
xiphisternum to
sternum, a little to
the right
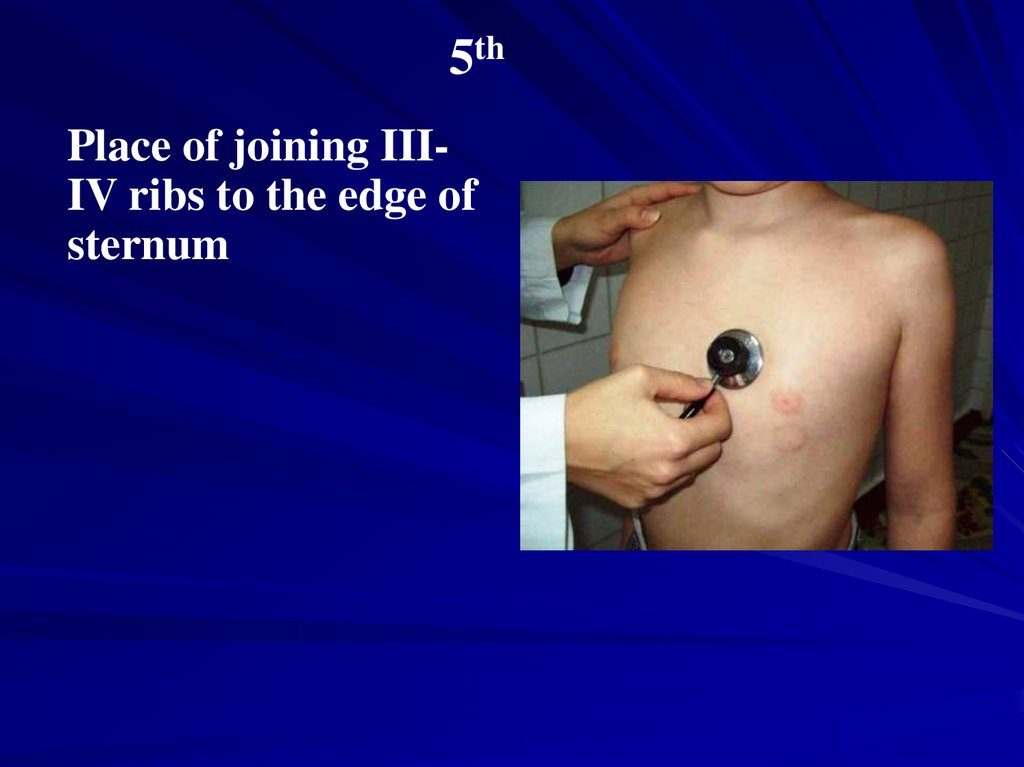
19. 5th
Place of joining IIIIV ribs to the edge ofsternum
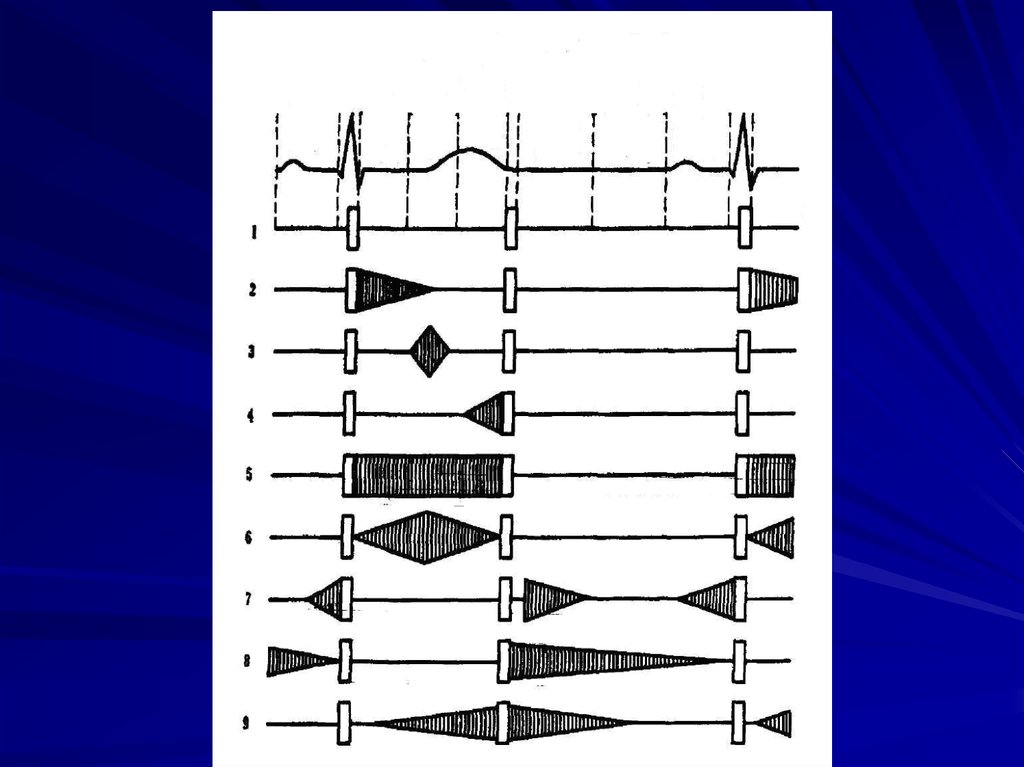
20. CARDIAC MURMURS
21. Cardiac murmurs – additional sounds heard during auscultation of the heart.
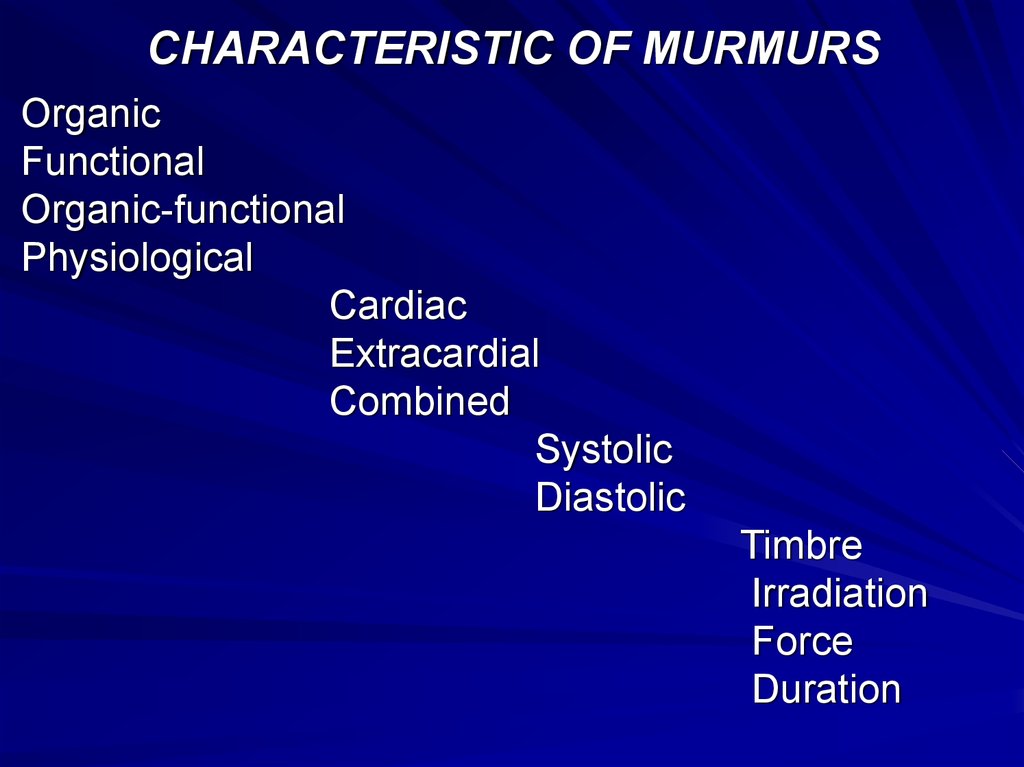
22. CHARACTERISTIC OF MURMURS
OrganicFunctional
Organic-functional
Physiological
Cardiac
Extracardial
Combined
Systolic
Diastolic
Timbre
Irradiation
Force
Duration
23.
24. RHEUMATIC FEVER (ACUTE RHEUMATIC HEART DISEASE)
Rheumatic heart disease (RHD) occurs afteracute rheumatic fever (ARF), which is a
postinfectious immune disease secondary
to a streptococcal infection.
RHD affects the valves of the heart, with the
mitral and aortic being the most commonly
affected valves. RHD is more likely to
occur with recurrent episodes.
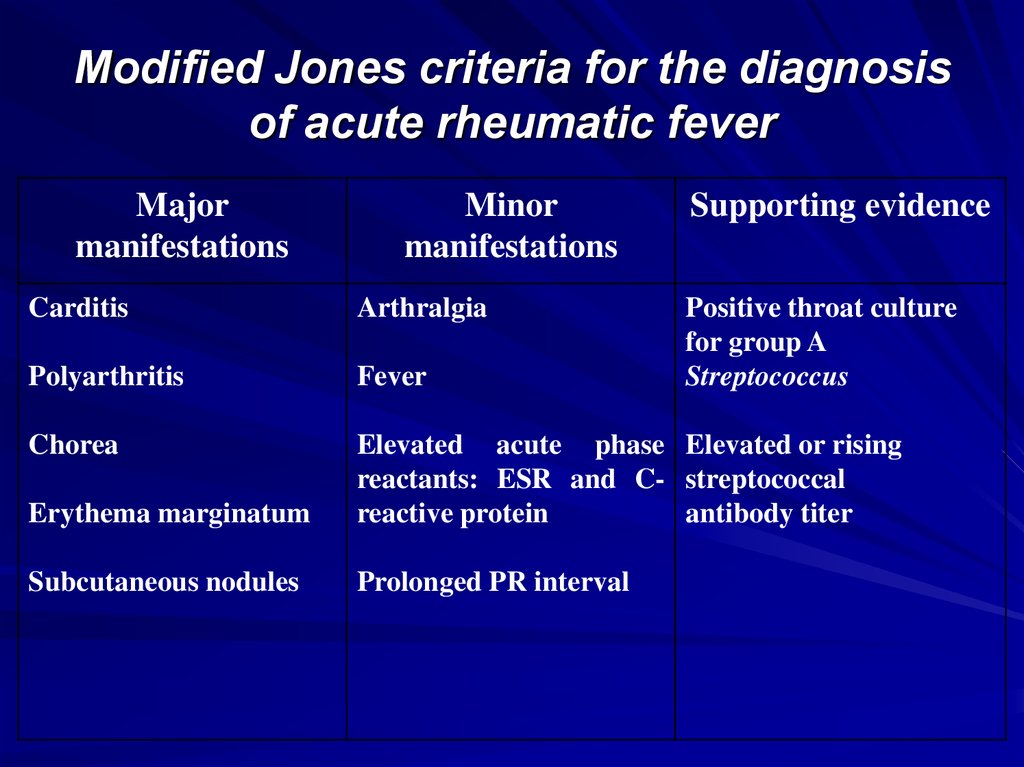
25. Diagnosis
Diagnosis of ARF is made from themodified Jones criteria, with a positive
diagnosis requiring two major or one
major and two minor criteria.
26. SYMPTOMS
Carditis: chest pain, shortness or breath, cough,palpitations with sensation of elevated or irregular
rate or rhythm, anorexia, fatigue, and exercise
intolerance.
Arthritis: occurs in 70% of patients with ARF;
symptoms include joint pain.
Sydenham’s chorea: affects 15% of patients with
ARF; reflects involvement of basal ganglia of central
nervous system; appears ~3 months after
streptococcal infection; symptoms include emotional
liability and loss of attention span.
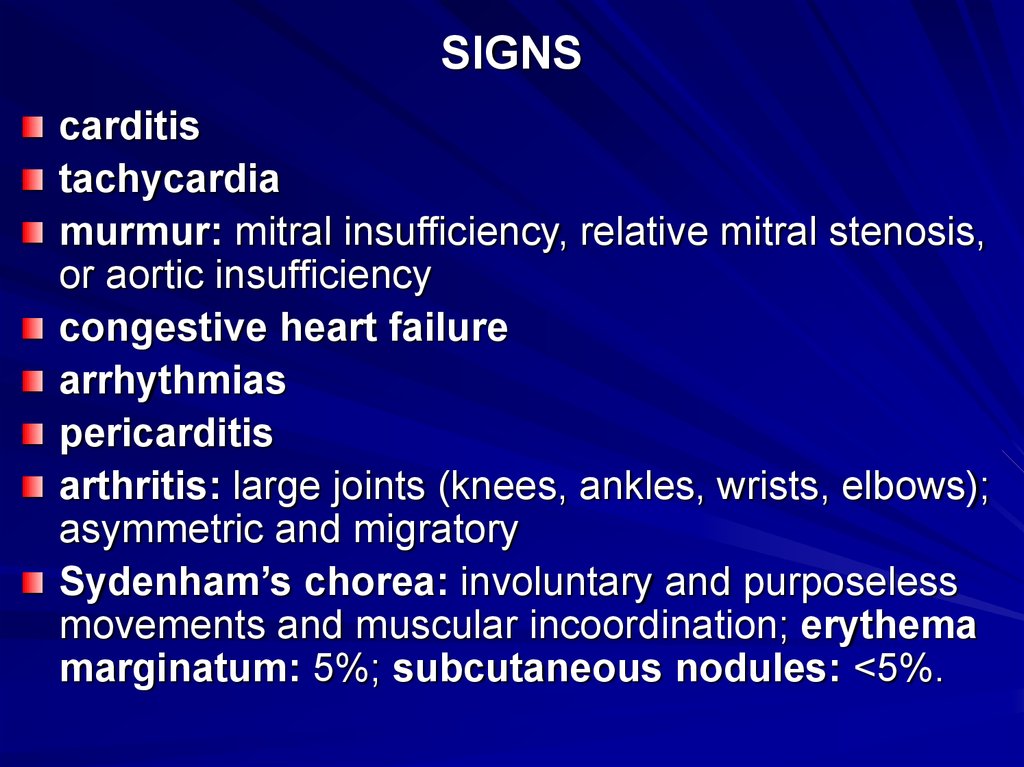
27. SIGNS
carditistachycardia
murmur: mitral insufficiency, relative mitral stenosis,
or aortic insufficiency
congestive heart failure
arrhythmias
pericarditis
arthritis: large joints (knees, ankles, wrists, elbows);
asymmetric and migratory
Sydenham’s chorea: involuntary and purposeless
movements and muscular incoordination; erythema
marginatum: 5%; subcutaneous nodules: <5%.
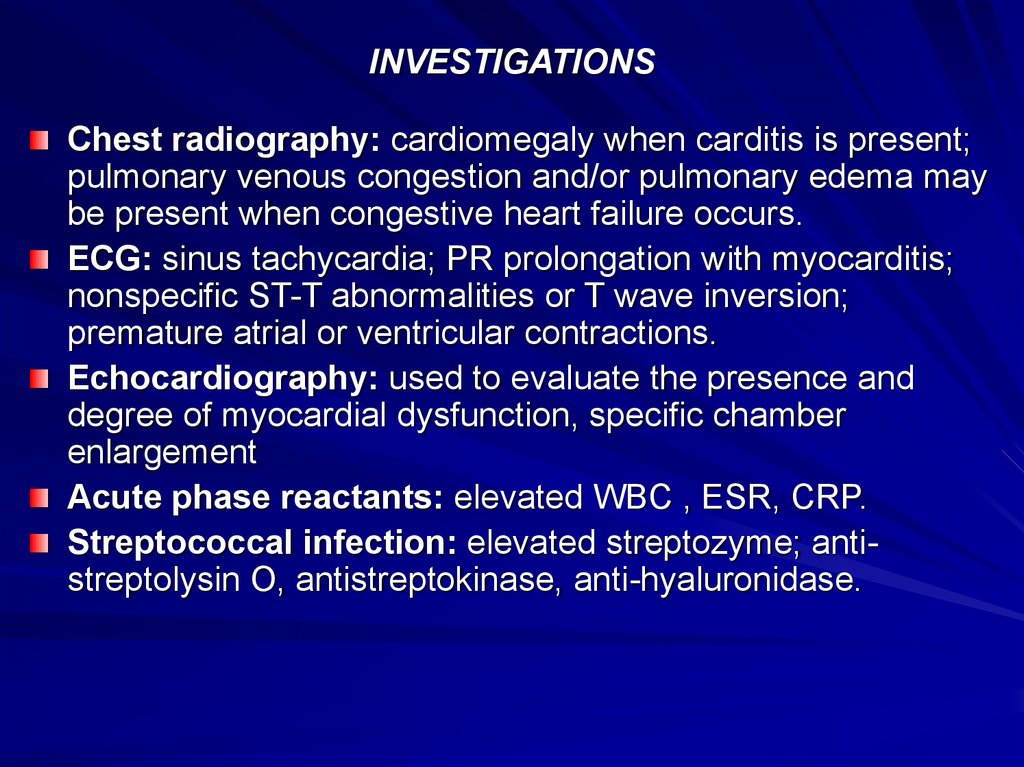
28. INVESTIGATIONS
Chest radiography: cardiomegaly when carditis is present;pulmonary venous congestion and/or pulmonary edema may
be present when congestive heart failure occurs.
ECG: sinus tachycardia; PR prolongation with myocarditis;
nonspecific ST-T abnormalities or T wave inversion;
premature atrial or ventricular contractions.
Echocardiography: used to evaluate the presence and
degree of myocardial dysfunction, specific chamber
enlargement
Acute phase reactants: elevated WBC , ESR, CRP.
Streptococcal infection: elevated streptozyme; antistreptolysin O, antistreptokinase, anti-hyaluronidase.
29. Modified Jones criteria for the diagnosis of acute rheumatic fever
Majormanifestations
Minor
manifestations
Supporting evidence
Carditis
Arthralgia
Positive throat culture
for group A
Streptococcus
Polyarthritis
Fever
Chorea
Erythema marginatum
Elevated acute phase Elevated or rising
reactants: ESR and C- streptococcal
reactive protein
antibody titer
Subcutaneous nodules
Prolonged PR interval
30. MYOCARDITIS
DefinitionInflammation of myocardium in association with
necrosis.
Presentation
Mild to moderate congestive heart failure
(CHF).
Severe CHF or shock.
Non-CHF: arrhythmia, sudden death.
History of prior gastrointestinal or flu-like
illness.
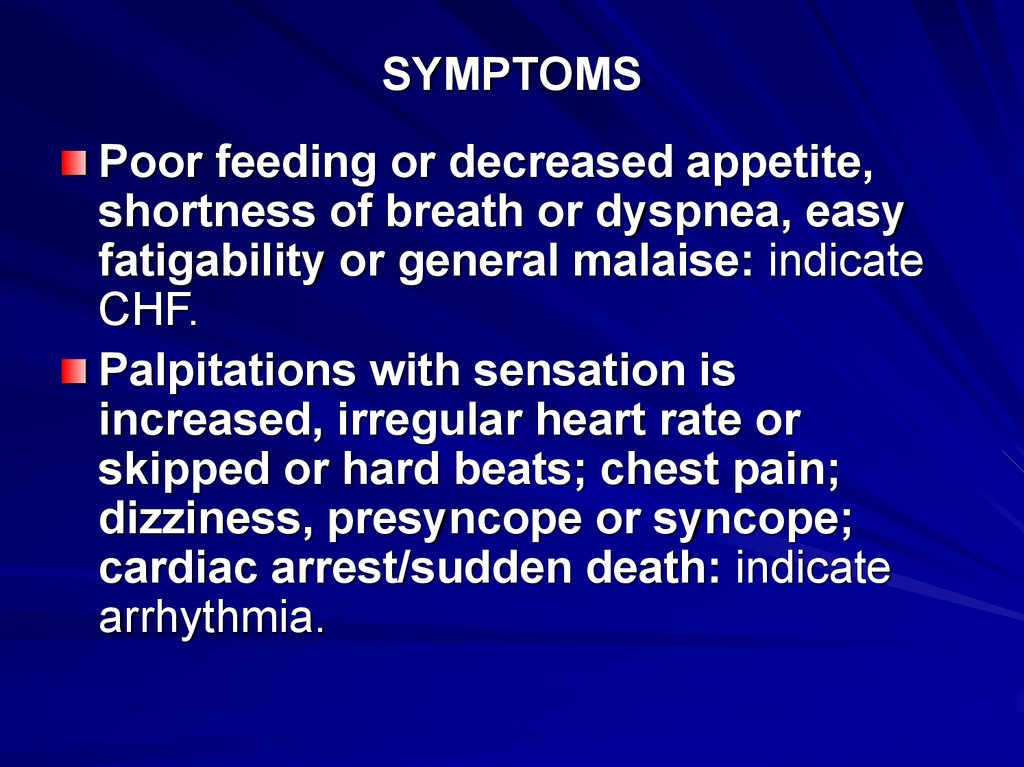
31. SYMPTOMS
Poor feeding or decreased appetite,shortness of breath or dyspnea, easy
fatigability or general malaise: indicate
CHF.
Palpitations with sensation is
increased, irregular heart rate or
skipped or hard beats; chest pain;
dizziness, presyncope or syncope;
cardiac arrest/sudden death: indicate
arrhythmia.
32. SIGNS
Tachycardia, irregular pulse.Soft, indistinct heart sounds.
Mitral or tricuspid regurgitation.
Systolic murmur of atrioventricular (AV) valve
regurgitation.
Tachypnea.
Rales: associated with pulmonary edema.
Hepatomegaly.
Hypotension: associated with shock.
Weak peripheral pulses.
Poor perfusion.
Jugular venous distention.
Pallor or cyanosis.
33. INVESTIGATIONS
ECGChest radiography
Echocardiography (ECHO)
Radionuclide studies
Laboratory studies
Endomyocardial biopsy
34. ENDOCARDITIS
35. SYMPTOMS
Fever and sweating.Easy fatiguability, malaise.
Palpitations.
Weight loss and anorexia.
Signs
Fever.
Tachycardia with new (or changing) cardiac
murmur(s).
Splenomegaly.
Embolic phenomena
36. INVESTIGATIONS
Laboratory testsBlood cultures.
Acute phase reactants
Complete blood count
Urinanalysis: hematuria.
Echocardiography!
37. COMPLICATIONS
Destruction of cardiac valve tissue: canresult in aortic, mitral, or tricuspid
insufficiency; resultant need for cardiac
valve replacement.
Congestive heart failure.
Myocardial abscesses with cardiac
arrhythmias and atrioventricular block.
Systemic embolization: potential for
stroke or cerebral mycotic aneurysm.
38. PERICARDITIS AND TAMPONADE
39. Pericarditis
SYMPTOMS AND SIGNSMild to severe pericardial pain on inspiration
or worse on inspiration: may radiate to neck
and shoulders; worse on coughing,
swallowing, or sneezing; improved by
leaning forward.
Fever.
Pericardial, often pleuropericardial, coarse
rub: best heard at left sternal edge with
patient leaning forward
Pericardial effusion: varies from small to
large.
40. Tamponade
Symptoms similar to pericarditis: pain, cough, hoarseness,tachypnea, dysphagia; malaise, cyanosis, dyspnea, sweating,
anxiety.
Tachycardias.
Low blood and pulse pressures.
Pulsus paradoxus: exaggerated reduction (>10 mm Hg) of
the normal inspiratory decrease in systolic blood pressure;
pulse may disappear on inspiration.
Hypotension: accompanied by signs of low cardiac output
(pallor, diaphoresis, poor perfusion with cool extremities).
Jugular venous distention: may increase on inspiration.
Hepatomegaly.
Muffled heart sounds.
Tachypnea.
Friction rub: heard with small to moderate effusions (may not
be present with
large effusions or tamponade).
41. INVESTIGATIONS
• For any pericardial disease, the underlyingcause must always be sought.
42. Pericarditis
Complete blood count, erythrocytesedimentation rate.
Antistreptolysin O titer, antineutrophil factor,
rheumatoid factor analysis.
Cardiac enzyme tests
Paired viral antibody screening:
Mantoux test.
ECG
Chest radiography.
43. Tamponade
Echocardiography.Complications -Relapsing or
constrictive pericarditis, pericardial
effusion, and tamponade,
Hypotension, renal failure
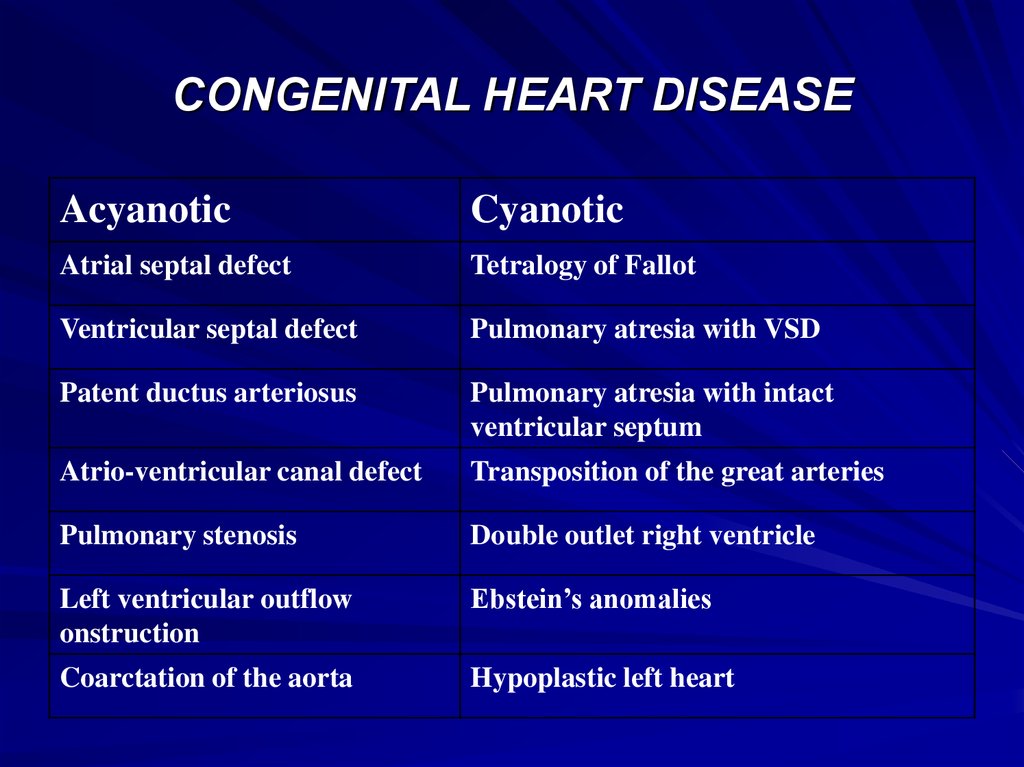
44. CONGENITAL HEART DISEASE
AcyanoticCyanotic
Atrial septal defect
Tetralogy of Fallot
Ventricular septal defect
Pulmonary atresia with VSD
Patent ductus arteriosus
Pulmonary atresia with intact
ventricular septum
Atrio-ventricular canal defect
Transposition of the great arteries
Pulmonary stenosis
Double outlet right ventricle
Left ventricular outflow
onstruction
Ebstein’s anomalies
Coarctation of the aorta
Hypoplastic left heart
45. A ventricular septal defect
Oxygenated blood is usually shunted fromthe left ventricle to the right ventricle.
Mixed blood then flows through the
pulmonary arteries. The incidence is from
1.5:1000 to 2.5:1000 live births.
46.
47. AN ATRIAL SEPTAL DEFECT
Oxygenated blood is usually shunted fromthe left atrium to the right atrium. Mixed
blood then flows to the right ventricle and
into the pulmonary arteries.
48.
49. A PATENT DUCTUS ARTERIOSUS
Oxygenated blood from the aorta flowsthrough the patent ductus arteriosus and
mixes with the unoxygenated blood
flowing to the lungs in the pulmonary
arteries. The incidence is 1:2000 live
births.
50.
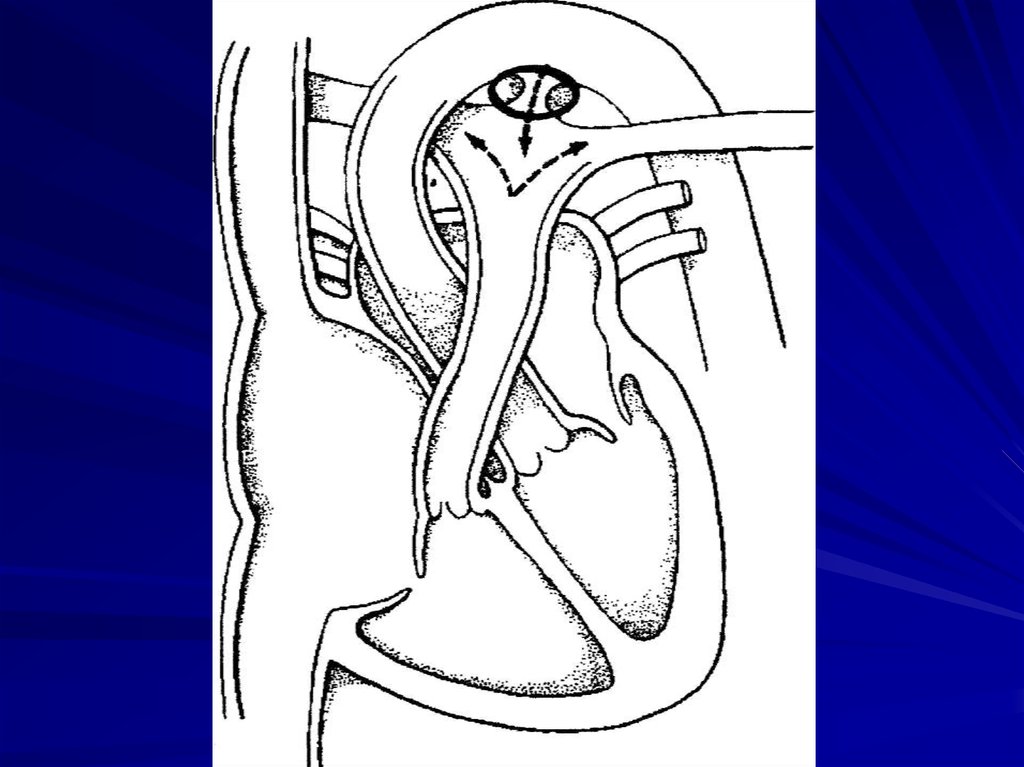
51. TETRALOGY OF FALLOT
(1) Right ventricular outflow obstruction,(2) Ventricular septal defect,
(3) The aorta overriding the ventricular
septal defect.
(4) Right ventricular hypertrophy. The
incidence is 1:2000 live births.
52.
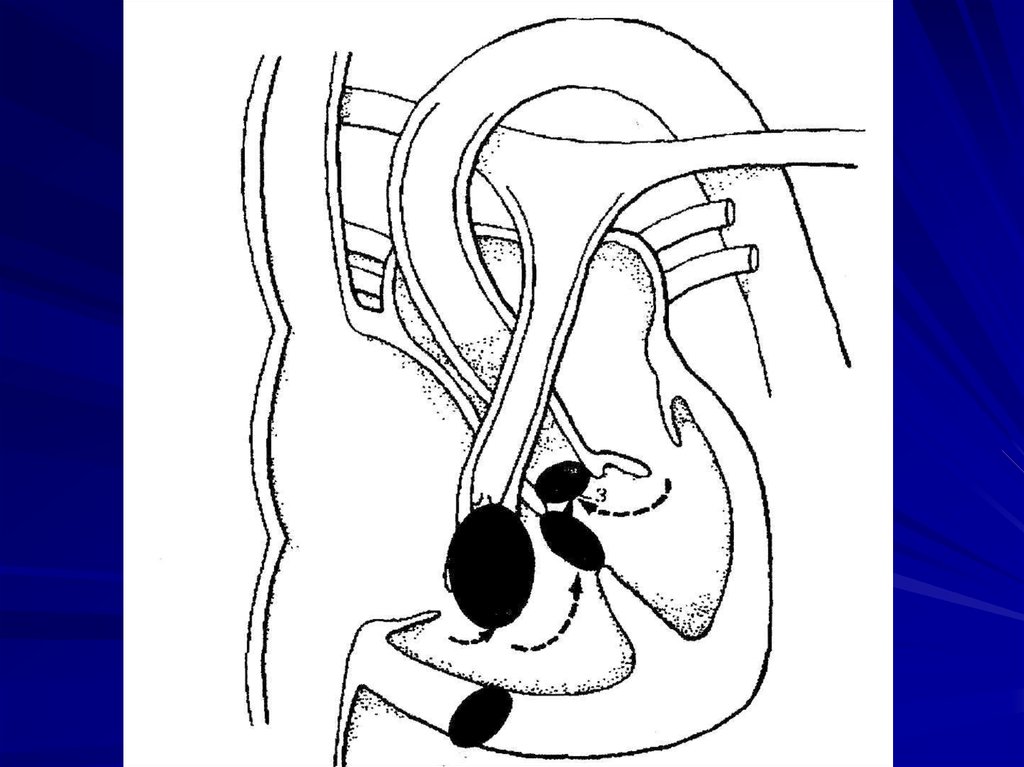
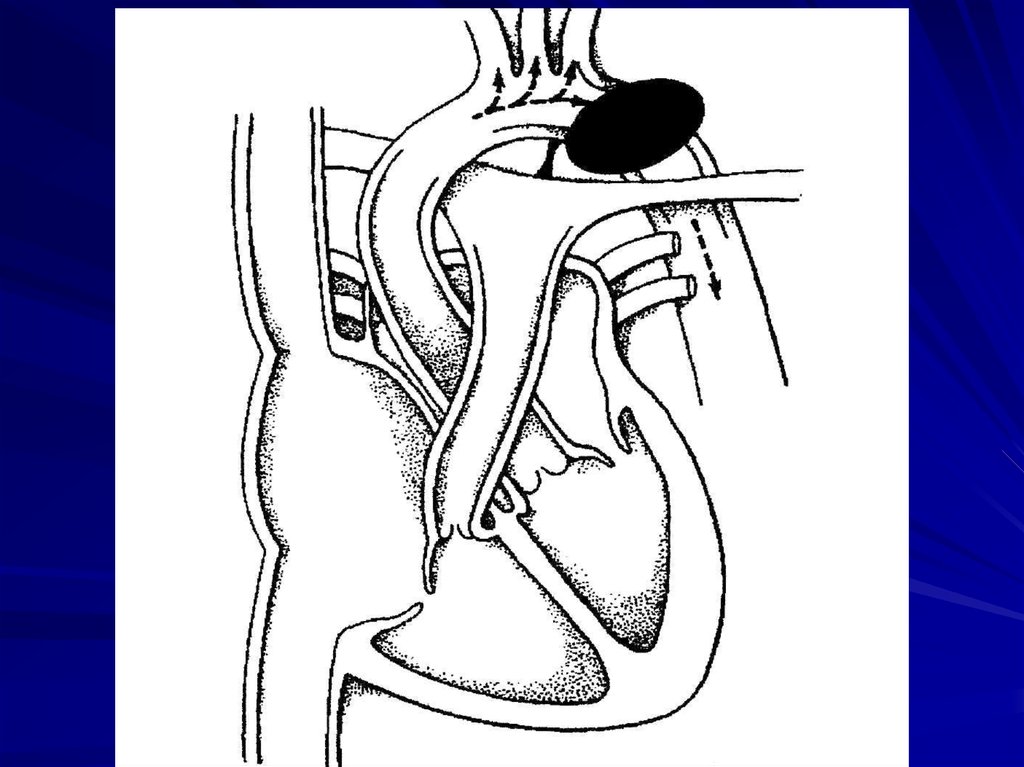
53. COARCTATION OF THE AORTA
Narrowing of the lumen results inincreased systolic blood pressure
proximal to the coarctation and
decreased systolic blood pressure distally.
The incidence is 1:13,000 live births.










 medicine
medicine