Similar presentations:
Cardiovascular disease In pregnancy
1. Cardiovascular Disease In Pregnancy
It is a relatively common in women of child bearingage, complicate about 1% of pregnancies
Maternal mortality related to heart disease has
decreased remarkably over the past 50 years (from 5.6
to 0.3/100 000 live birth)
Heart disease are still the second most common non
obstetrical cause of maternal mortality.
2. Cardiac Diseases
Rheumatic heart diseaseCongenital heart disease
Hypertensive heart disease
Coronary
Thyroid
Syphilitic
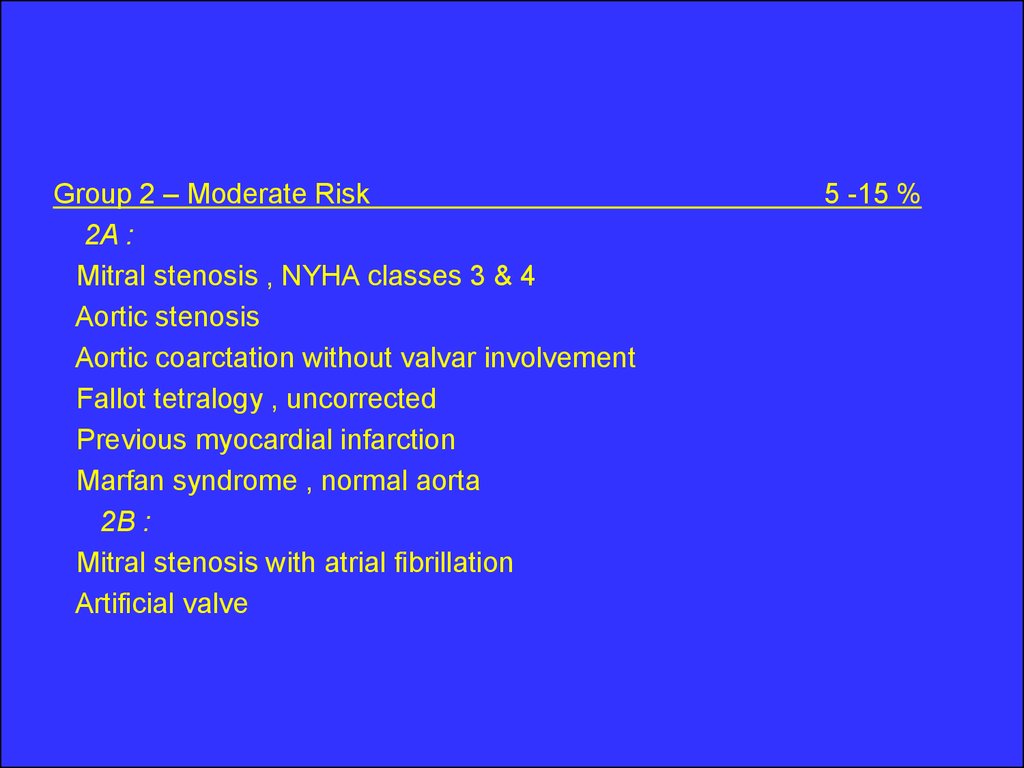
Kyphoscoliotic cardiac disease
Idiopathic cardiomyopathy
Corpulmonale
Constrictive pericarditis
Heart block
Isolated myocarditis
3. Physiological Consideration with Heart Disease In Pregnancy
The most important changes in cardiac function occurs inthe first 8 weeks of pregnancy with maximum changes at
28 weeks
↓
↓
↑
↑
Vascular resistance
Blood pressure
Heart rate
Blood volume
↑ Stroke volume
↑ COP
30% - 50%
Maternal weight and basal metabolic rate also affect COP
4.
cont…Later in pregnancy COP is higher when women is in the
lateral recumbent position than when she is in the supine
During labor COP increase moderately in the first stage
of labor and appreciably greater in the second stage
COP also increase in the immediate post partum period
5.
cont…Heart:
The heart is displaced upward and to the left with lateral
rotation on its long axis
Resting pulse increase by about 10 bpm
There is some changes in the cardiac sounds include:
An exaggerated splitting of the first heart sound with
increase loudness of both components, no definite
changes in the aortic and pulmonary elements of the
second sound, and aloud easily heard third sound
6.
conti….Systolic murmur is heard in 90 % of cases
Soft diastolic murmur transiently in 20 %
Continuous murmur arising from the breast vasculature
in10 % of cases
7. Diagnosis of Heart Disease
Some clinical indicators of heart disease duringPregnancy
Symptoms:
Progressive dyspnea or orthopnea
Nocturnal cough
Hemoptysis
Syncope
Chest pain
8.
Clinical findingsCyanosis
Clubbing of fingers
persistent neck vein distension
Systolic murmur grade 3/6 or greater
Diastolic murmur
Cardiomegaly
Persistent arrhythmia
Persistent split-second sound
Criteria for pulmonary hypertension
9. Diagnostic studies
ElectrocardiographyAn average 15 – degree left – axis deviation in the
ECG , and mild ST changes may be seen in the
inferior leads, Atrial and ventricular premature
contractions are relatively frequent
Chest x – ray:
Heart silhouette normally is larger in pregnancy,
however gross cardiomegaly can be excluded
10.
Echocardiography:Normal changes include : Tricuspid regurgitation ,
Significantly increase left atrial size and left
ventricular outflow cross sectional area.
11. Clinical clssification
The New York Heart Association’s FunctionalClassification [ NYHA] “ First published in 1928 “
Class 1 : Uncompromised , no limitation of physical
activity
Class 2 : Slightly compromised , slight limitation of
physical activity
Class 3 : Markedly compromised , marked limitation
of physical activity
Class 4 : Severely compromised , inability to perform
any physical activity without discomfort
12. Preconceptional counseling
Maternal mortality generally varies directly withfunctional classification at pregnancy onset;
However this relationship may change as pregnancy
progresses
Patient with pulmonary hypertension, primary or
secondary are in danger of undergoing decompensation
during pregnancy
13.
cont…Life threatening cardiac abnormalities can be reversed
by corrective surgery and subsequent pregnancy is
less dangerous
In other cases fetal consideration predominate, for
example the teratogenic effect of warfarin
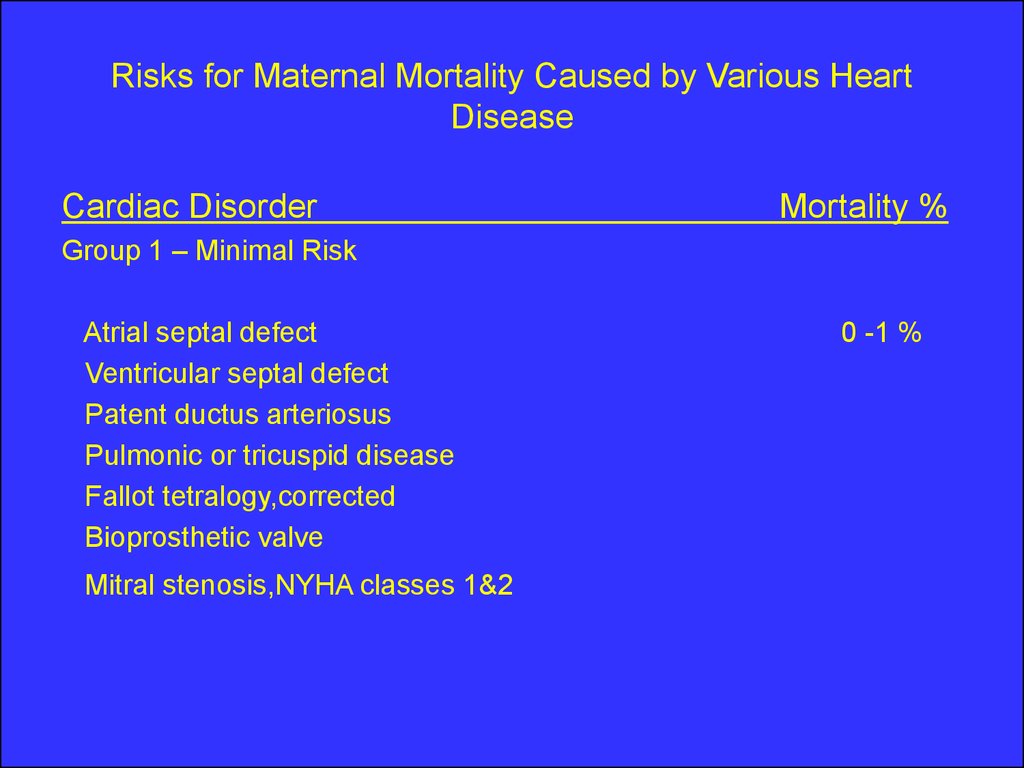
14. Risks for Maternal Mortality Caused by Various Heart Disease
Cardiac DisorderMortality %
Group 1 – Minimal Risk
Atrial septal defect
Ventricular septal defect
Patent ductus arteriosus
Pulmonic or tricuspid disease
Fallot tetralogy,corrected
Bioprosthetic valve
Mitral stenosis,NYHA classes 1&2
0 -1 %
15.
Group 2 – Moderate Risk2A :
Mitral stenosis , NYHA classes 3 & 4
Aortic stenosis
Aortic coarctation without valvar involvement
Fallot tetralogy , uncorrected
Previous myocardial infarction
Marfan syndrome , normal aorta
2B :
Mitral stenosis with atrial fibrillation
Artificial valve
5 -15 %
16.
Group 3 – Major RiskPulmonary hypertension
Aortic coarctation with valvar involvement
Marfan syndrome with aortic involvement
NYHA = New York Heart Association.
From the American College of Obstetrics and Gynecologists
(1992a ) , with permission .
25 -50 %
17. Management
In assuring an optimal outcome , management shouldbe a team approach involving ;obstetrician, cardiologist
and anesthesiologist
Risk to patient of : Heart failure, subacute bacterial
endocarditis, and thromboembolic disease will be
identified and minimized
18. Management
Four concepts that affect management are emphasizedby the American College of Obs /Gyn :1) the 50% increase in blood volume and COP by the
early 3rd trimester
2) further fluctuation in volume and COP in the
peripartum period
3) a decline in systemic vascular resistance, reaching
a nadir in the 2nd trimester, and then rising to 20%
below normal by late pregnancy
4) hyprcoagulability of special importance in women
requiring anticoagulation in the non pregnant state
19. Management of Class 1 & 2
Management of Class 1 & 2General measures:
_ avoid contact with persons who have respiratory
infection
_ pneumococcal and influenza vaccines are recommended
( patient with valvar heart disease)
_ cigarette smoking is prohibited
_ diet , avoidance of strenuous activity and avoidance of
anemia
20.
management cont…..sign’s of heart failure:
» persistent basilar rales
» nocturnal cough
» a sudden diminution in ability to carry
out usual duties
» increasing dyspnea on exertion
» attacks of smothering with cough
» hemoptysis, progressive edema and
tachycardia
21.
Management cont…..Labor and Delivery :
* vaginal delivery is preferred unless there is obstetrical
indication
* relief of pain with intravenous analgesics ,
continuous epidural analgesia is recommended for
most situation , but it’s contraindicated in patient with:
[ Intracardiac shunt , pulmonary hypertension , Aortic stenosis ] ,
to avoid the risk of maternal hypotension
22.
* fluid balance and antibiotic prophylactic* semi recumbent position with lateral tilt
* intensive medical management for any sign’s of
impending ventricular failure
[ pulse > 100 , RR > 24 , dyspnea ]
* expedite vaginal delivery
* close monitoring for the 3rd stage of labor
23.
puerperium* avoid complication of pph, anemia, infection
and thromboembolism
* delay the procedure of tubal sterilization until
it is obvious that the mother is a febrile, not
anemic and can ambulate without evidence
of distress
* option of contraceptive advise
24. Management of class 3&4
Management of class 3&4 ؟whether pregnancy should be undertaken
؟consider pregnancy interruption
؟prolonged hospitalization or bed rest
؟vaginal delivery is preferred
؟caesarian section delivery should be with the availability
of experience anesthetic support in a facility with
experience with complicated cardiac disease
25.
Most common lesions:_Rheumatic heart disease
Incidence of rheumatic fever is decreasing in developed
countries , It still remain the chief cause of serious mitral
valve disease in women,(3/4thof cases of mitral stenosis)
_Congenital Heart Disease:
many congenital heart lesions appear to be inherited as
polygenic characteristic , 10% of women with congenital
heart disease would give birth to similarly affected infants ,
50 % were concordant for the same anomaly
26.
Peripartum cardiomyopathy :this is a diagnosis of exclusion , it describe women
with peripartum heart failure with no apparent etiology,
symptoms of cardiac decompensation appear during
the last weeks of pregnancy or 1 to 6 months postpartum
obstetrical complications such as : preeclampsia, anemia
from blood loss , and infection either contribute or
precipitate heart failure
27.
Prognosis :favorable outcome for the mother with heart
disease depends upon the :
_ functional cardiac capacity
_ other complications that further increase cardiac load
_ quality of medical care provided
_ psychological and socioeconomical factors













 medicine
medicine