Similar presentations:
Ovarian tumors and cysts
1. Radynova S.B. Ph.D. Medicine, Associated Professor of Chair of Obstetrics and Gynecology
Ovarian tumors and cysts2. Relevance
occur at any agereduce a woman's reproductive potential
an indication for surgical treatment
the risk of malignancy is high
the treatment is often in the advanced
stage
3. Epidemiology
One out of 70 newborn girls will get an ovarian tumor duringtheir lifetime, and one out of 100 will die from ovarian
cancer.
Tumors and tumorous formations of the ovaries account for
up to 14% of tumors of the female genital organs.
Benign ovarian tumors account for up to 80% of all ovarian
tumors.
Almost every woman during her life is faced with one or
another disease accompanied by an increase in the ovary.
Benign tumors account for 85% of all tumors, and the chance
that a patient under the age of 45 will have a malignant tumor
is 1 in 15.
4. Classification of benign ovarian tumors
I. Tumors of the superficial epithelium and ovarian stroma(cystadenomas).
А. Serous tumors:
simple serous cystadenoma;
papillary (coarse-grained) serous cystadenoma;
papillary cystadenoma.
B. Mucinous tumors:
pseudomucinous cystadenoma.
C. Endometrioid tumors.
D. Brenner 's tumors.
E. Ovarian cancer.
5. Classification of benign ovarian tumors
II. Tumors of the genital cord and ovarian stroma.А. Granulosostromal cell tumors:
granulocellular tumor;
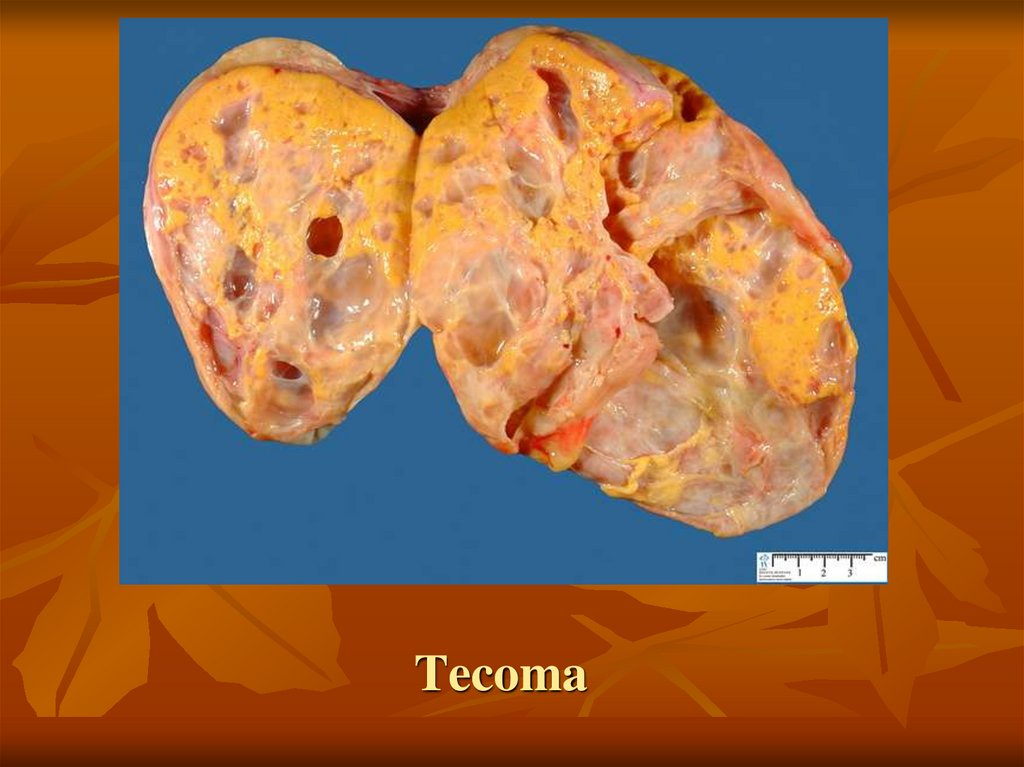
tecoma;
fibroma.
B. Androblastomas.
III. Germinogenic tumors.
A. Dysgerminoma.
B. Teratomas:
mature;
immature.
6.
CLASSIFICATION OF OVARIANCYSTS
1. Follicular cyst.
2. Corpus lu-teum cyst.
3. Teka-luteal cysts.
4. Paraovarial cyst.
5. Endometrioid cyst.
7. Etiology
1. Hormonal disorders2. Inflammation of the internal genitals
8. Risk factors:
- early menarche, late menopause;- violation of reproductive function;
- a high-calorie diet with a high content of saturated fatty acids;
- genetic predisposition;
- infertility;
- smoking;
- neuroendocrine disorders;
- late toxicosis in the mother;
- zero and second blood group;
- frequent acute respiratory infections and other viral diseases in childhood;
- the duration of the menstrual cycle is less than 24 days;
- recurrent abdominal pain syndrome;
- ovarian tumors at the mother;
- chronic stress;
- increased radiation background;
- a group of women who have no sexual life, haven’t become pregnant and/or haven’t given
birth;
- treatment for breast cancer;
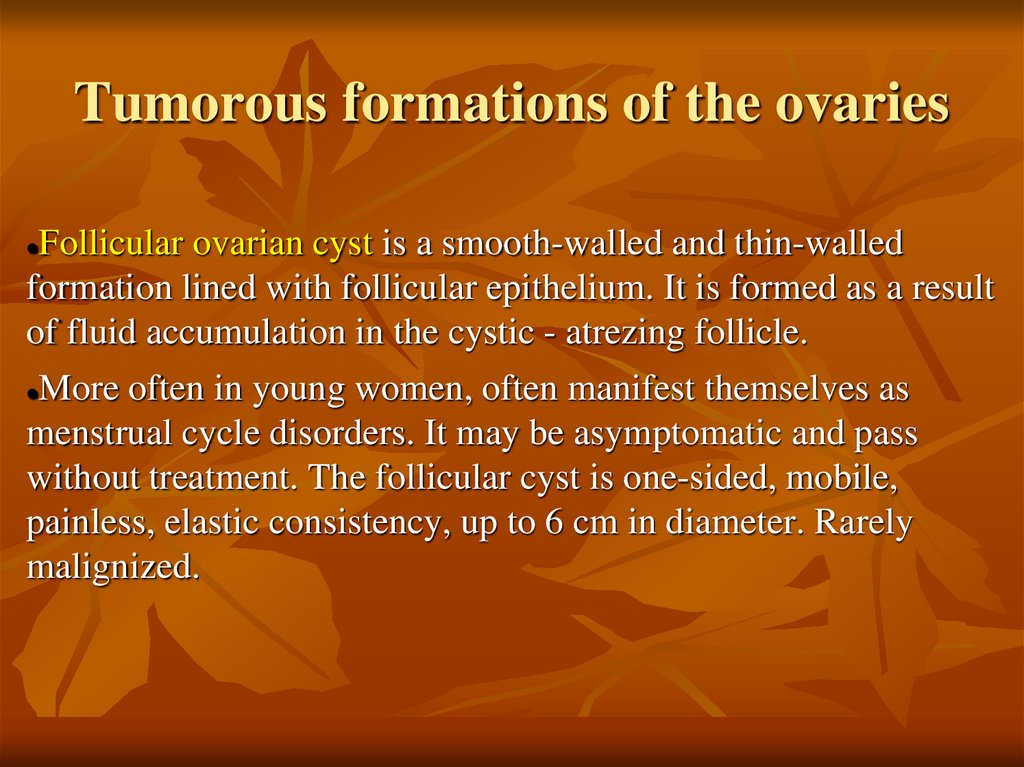
9. Tumorous formations of the ovaries
Follicular ovarian cyst is a smooth-walled and thin-walledformation lined with follicular epithelium. It is formed as a result
of fluid accumulation in the cystic - atrezing follicle.
More often in young women, often manifest themselves as
menstrual cycle disorders. It may be asymptomatic and pass
without treatment. The follicular cyst is one-sided, mobile,
painless, elastic consistency, up to 6 cm in diameter. Rarely
malignized.
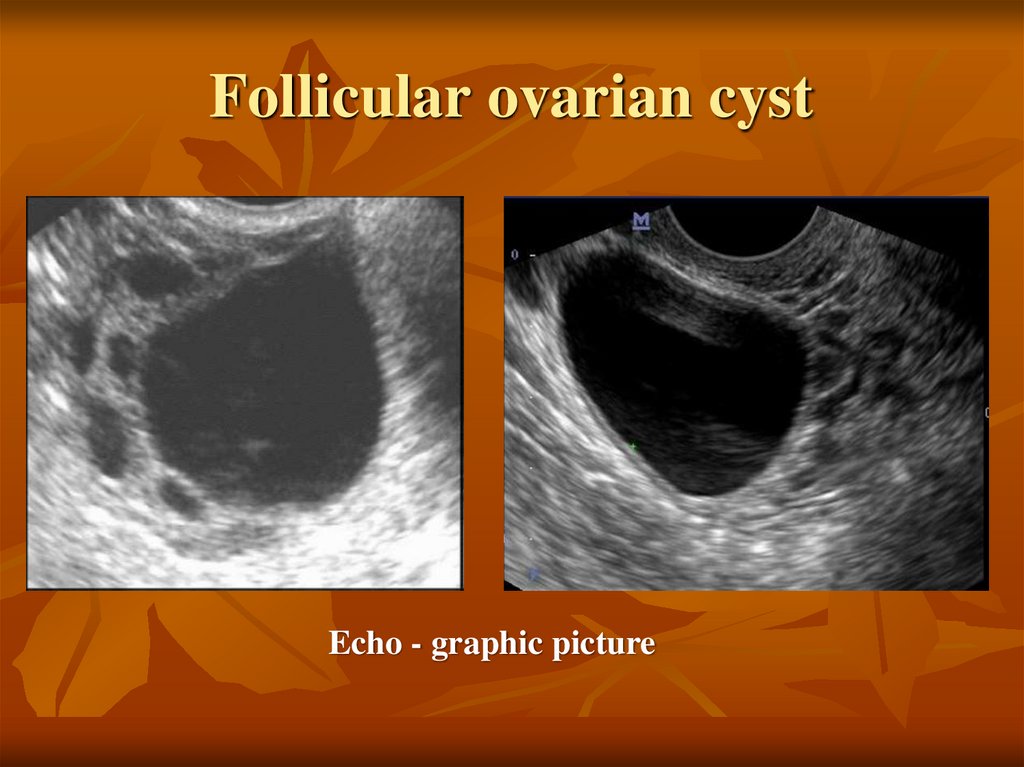
10. Follicular ovarian cyst
Echo - graphic picture11. Follicular ovarian cyst
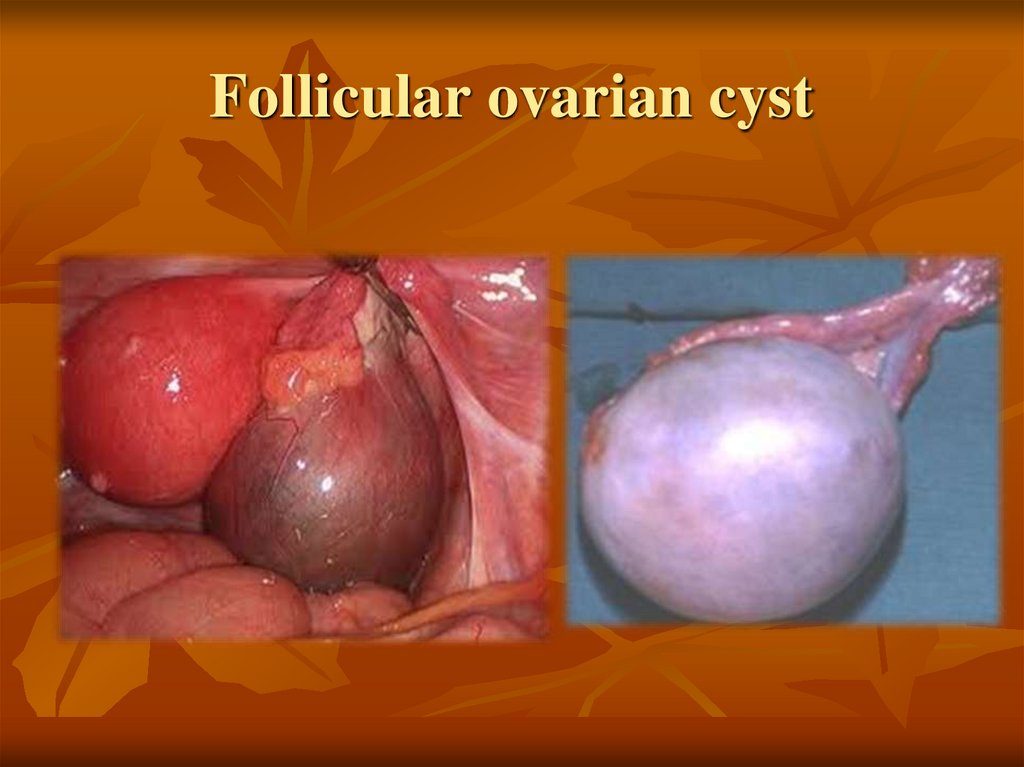
12. Follicular ovarian cyst
13.
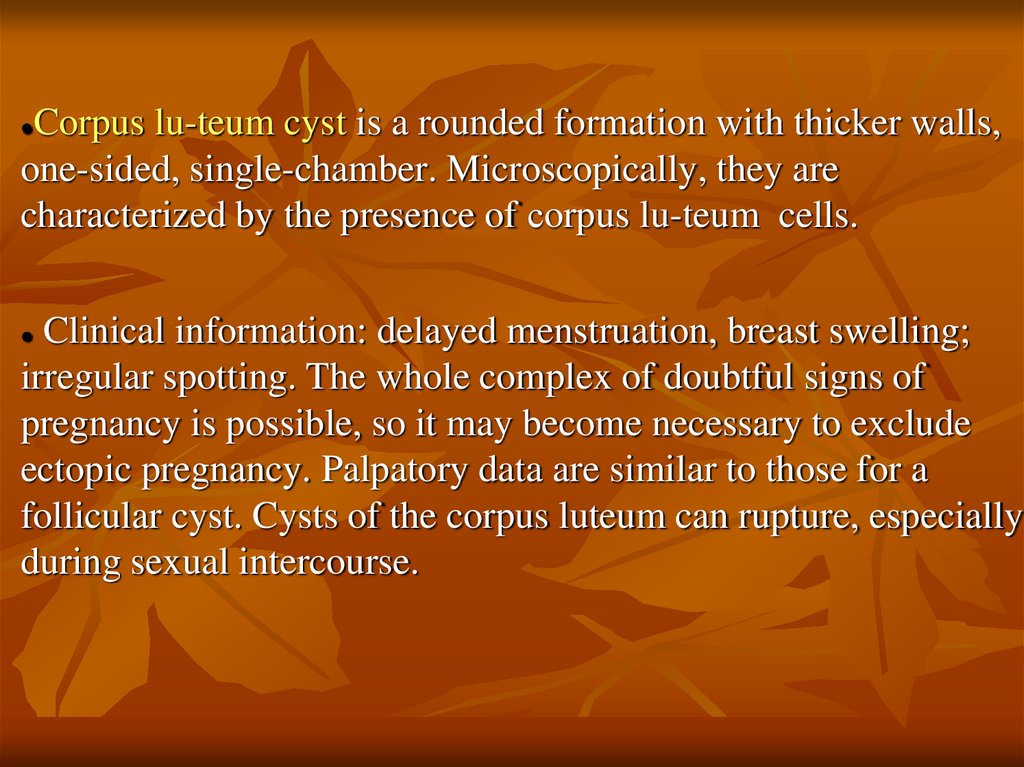
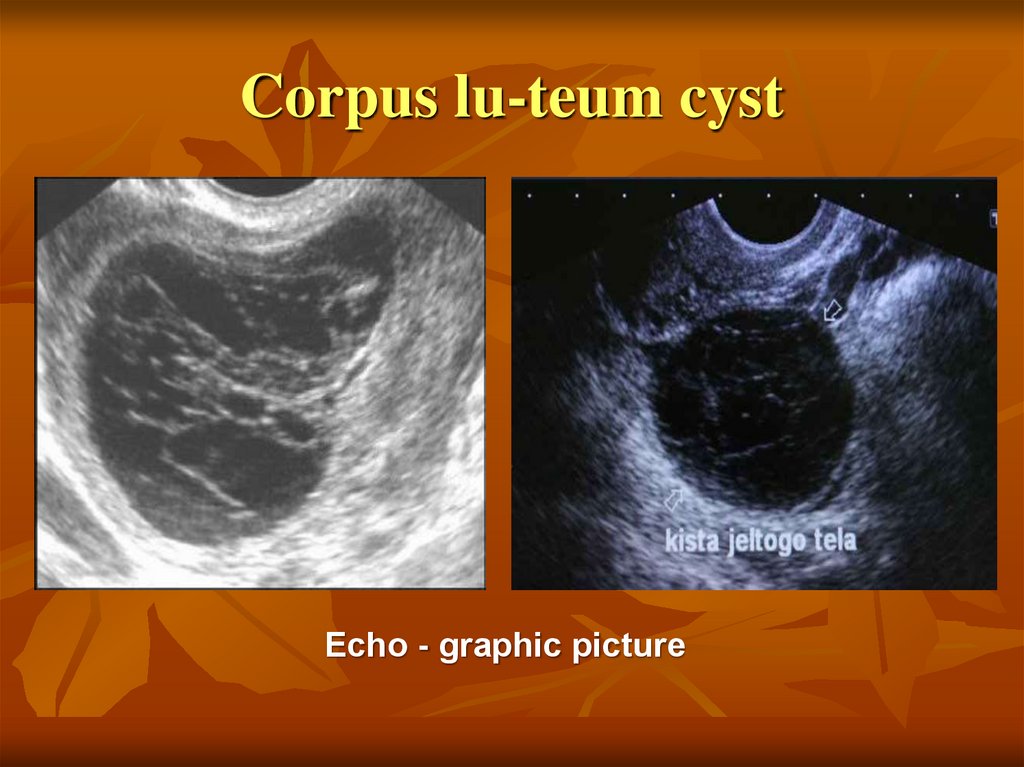
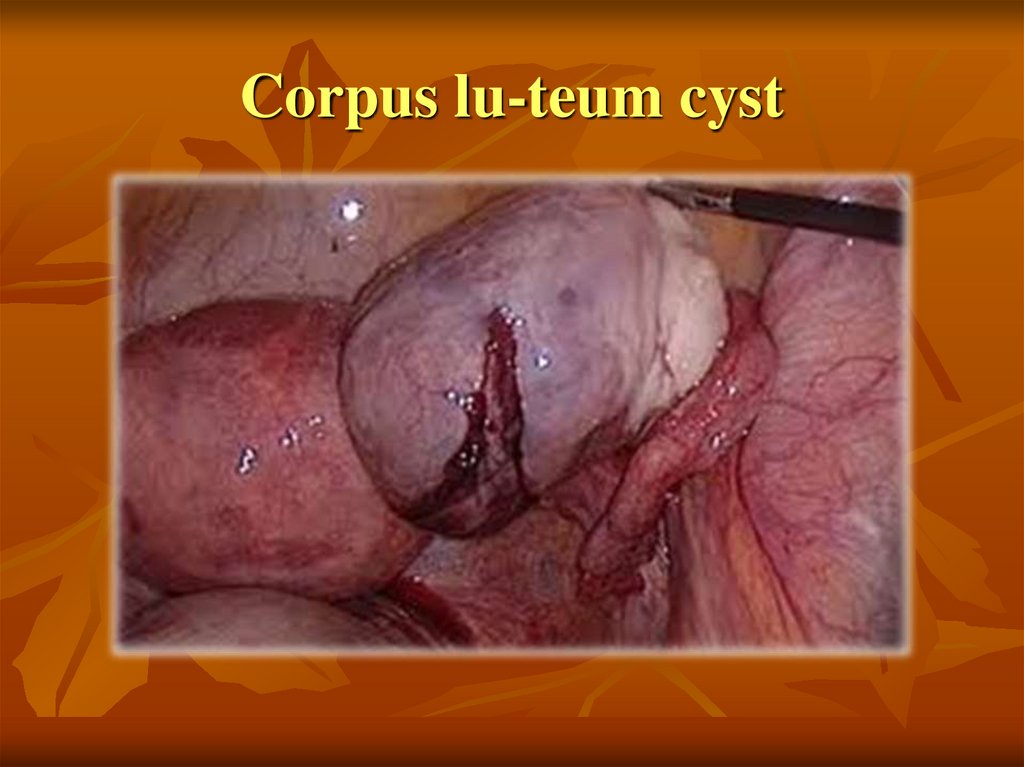
Corpus lu-teum cyst is a rounded formation with thicker walls,one-sided, single-chamber. Microscopically, they are
characterized by the presence of сorpus lu-teum cells.
Clinical information: delayed menstruation, breast swelling;
irregular spotting. The whole complex of doubtful signs of
pregnancy is possible, so it may become necessary to exclude
ectopic pregnancy. Palpatory data are similar to those for a
follicular cyst. Cysts of the corpus luteum can rupture, especially
during sexual intercourse.
14. Corpus lu-teum cyst
Echo - graphic picture15. Corpus lu-teum cyst
16.
A simple (serous) ovarian cyst is clinically andvisually resembles a follicular cyst.
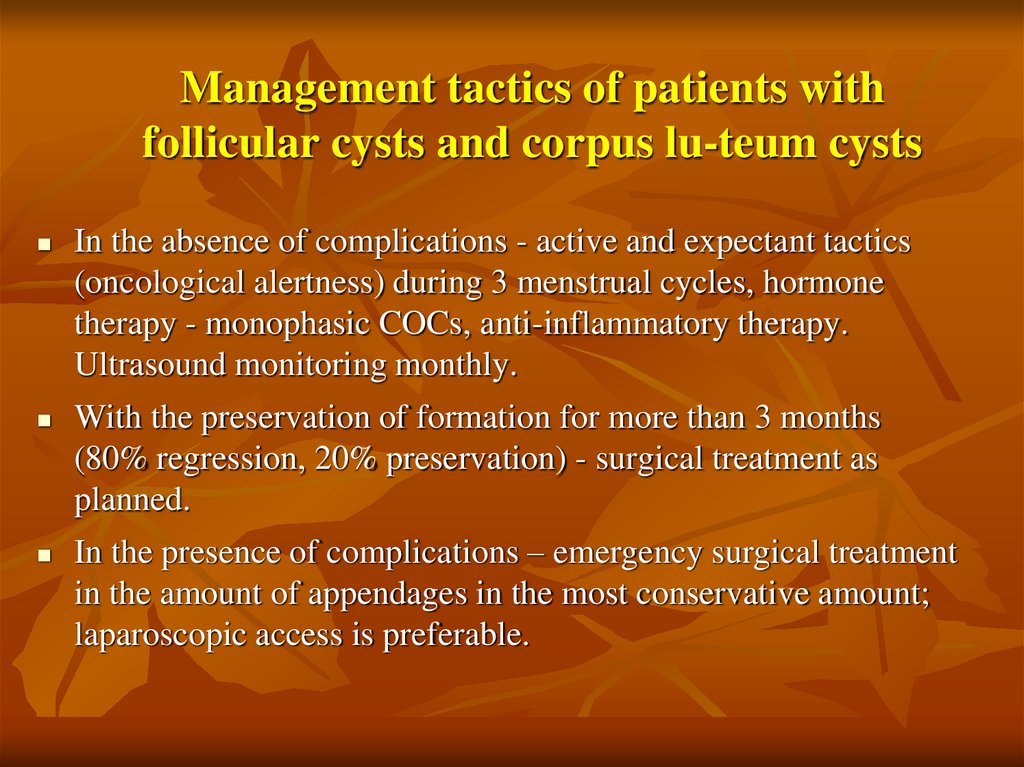
17. Management tactics of patients with follicular cysts and corpus lu-teum cysts
In the absence of complications - active and expectant tactics(oncological alertness) during 3 menstrual cycles, hormone
therapy - monophasic COCs, anti-inflammatory therapy.
Ultrasound monitoring monthly.
With the preservation of formation for more than 3 months
(80% regression, 20% preservation) - surgical treatment as
planned.
In the presence of complications – emergency surgical treatment
in the amount of appendages in the most conservative amount;
laparoscopic access is preferable.
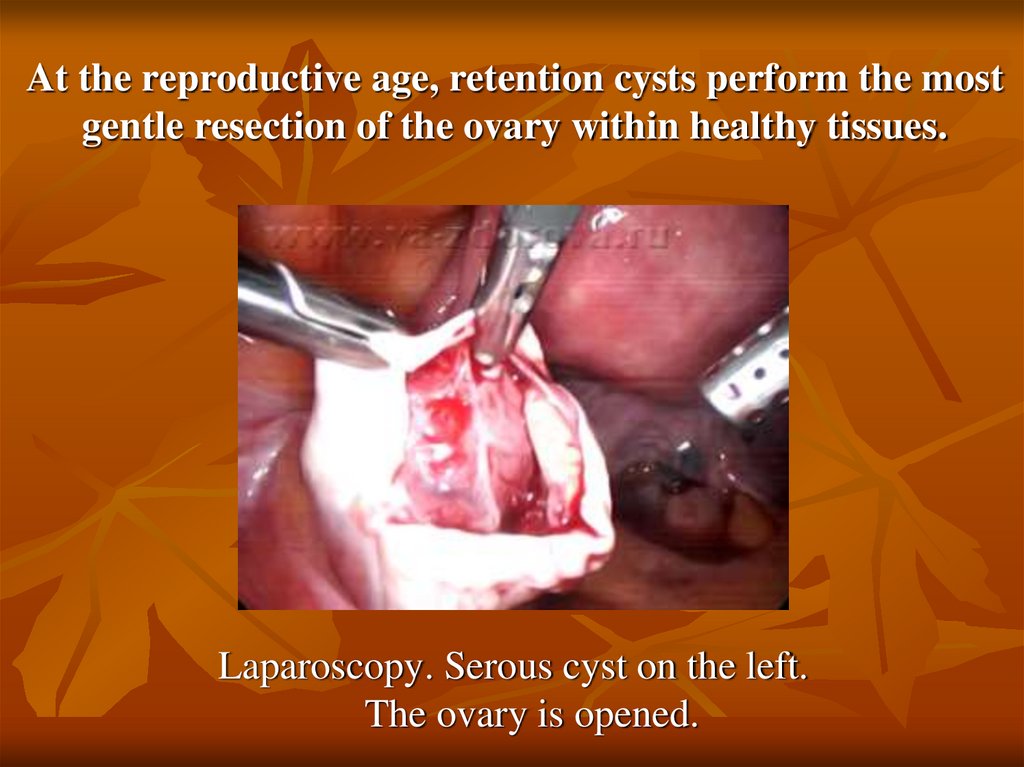
18. At the reproductive age, retention cysts perform the most gentle resection of the ovary within healthy tissues.
Laparoscopy. Serous cyst on the left.The ovary is opened.
19.
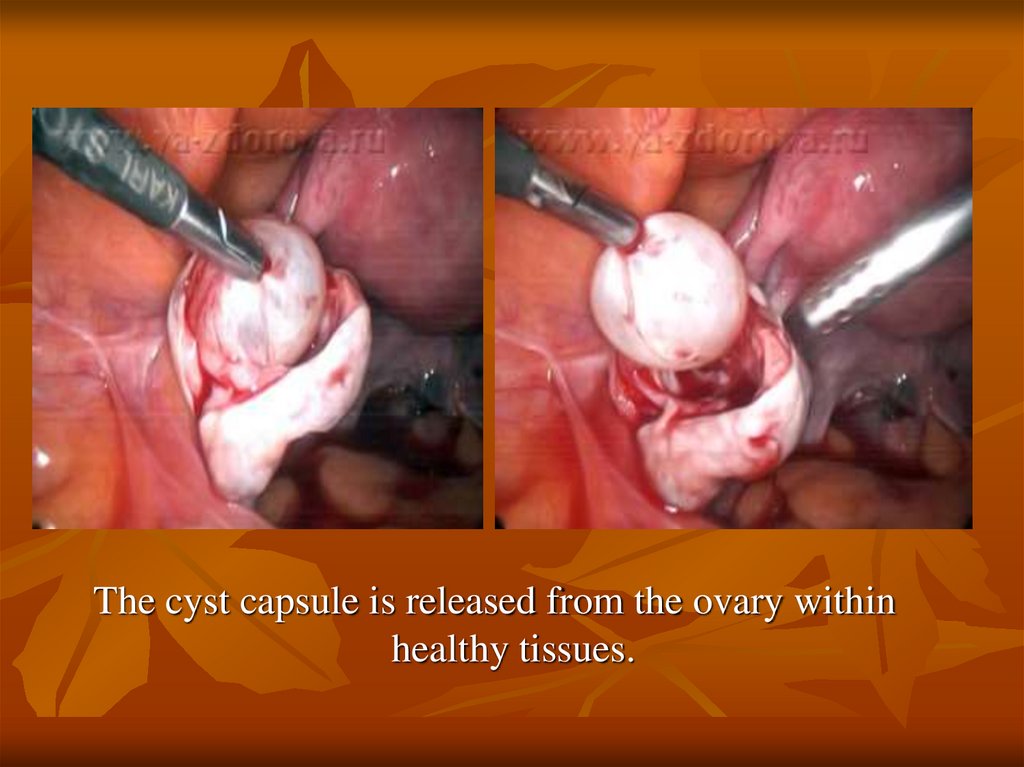
The cyst capsule is released from the ovary withinhealthy tissues.
20.
Ovarian cyst isolated, not opened during surgery. On the left healthy ovarian tissue.21.
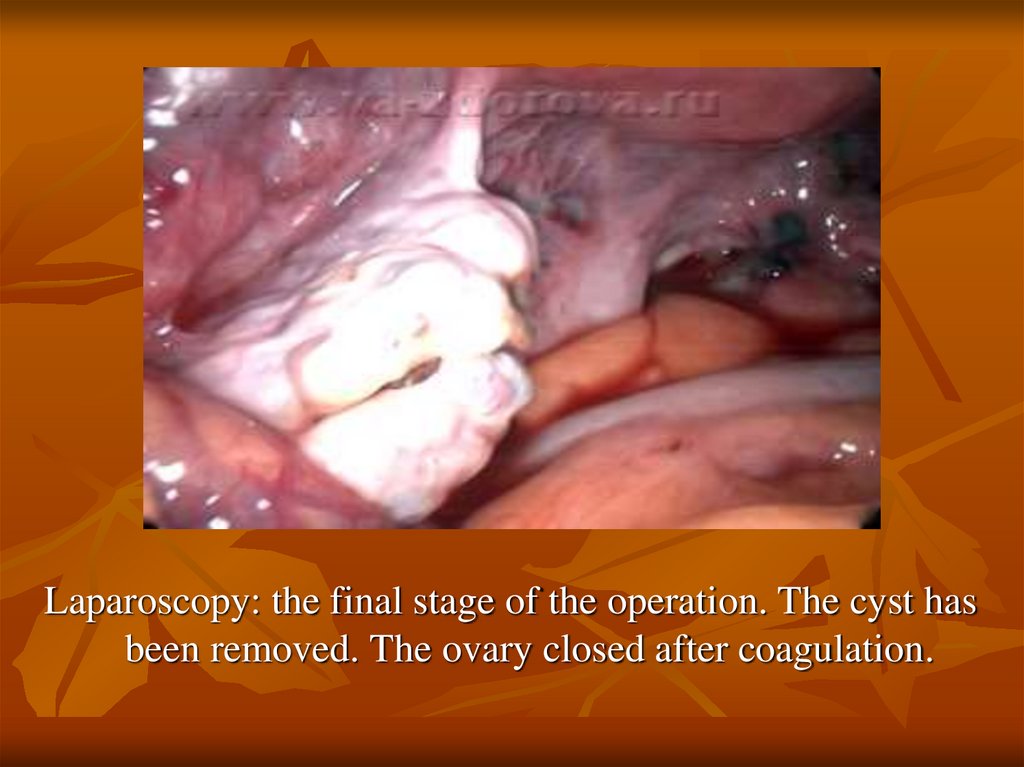
Laparoscopy: the final stage of the operation. The cyst hasbeen removed. The ovary closed after coagulation.
22.
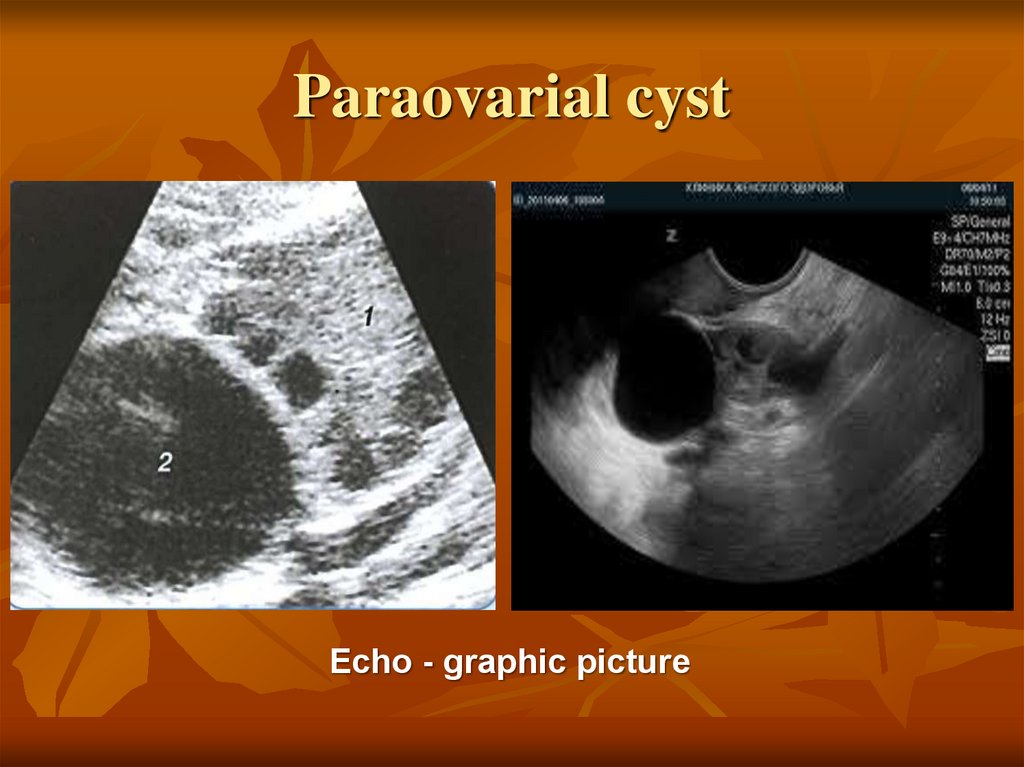
A paraovarial cyst is considered as a cyst formedfrom a mesosalpinx. Arises from the residues of
mesonephros. More often, it does not manifest
itself clinically in any way, but with large sizes,
there may be a violation of nutrition (twisting of
the leg) and rupture of the cyst. One-sided,
mobile, of a tight elastic consistency. With
ultrasound, the ovary is usually visualized
separately next to the cyst.
23. Paraovarial cyst
Echo - graphic picture24. Paraovarial cyst
25. Management tactics of a patient with a paraovarial cyst
Surgical treatment in a planned manner in thevolume of cyst exfoliation.
The access - laparoscopy, laparotomy.
26.
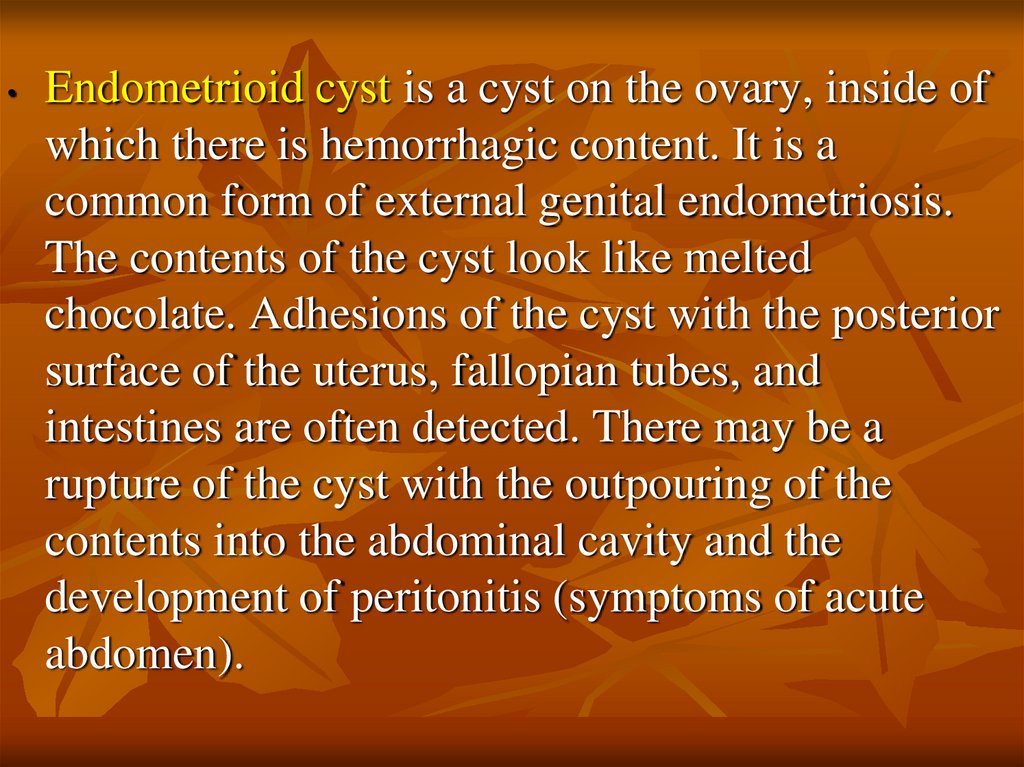
Endometrioid cyst is a cyst on the ovary, inside of
which there is hemorrhagic content. It is a
common form of external genital endometriosis.
The contents of the cyst look like melted
chocolate. Adhesions of the cyst with the posterior
surface of the uterus, fallopian tubes, and
intestines are often detected. There may be a
rupture of the cyst with the outpouring of the
contents into the abdominal cavity and the
development of peritonitis (symptoms of acute
abdomen).
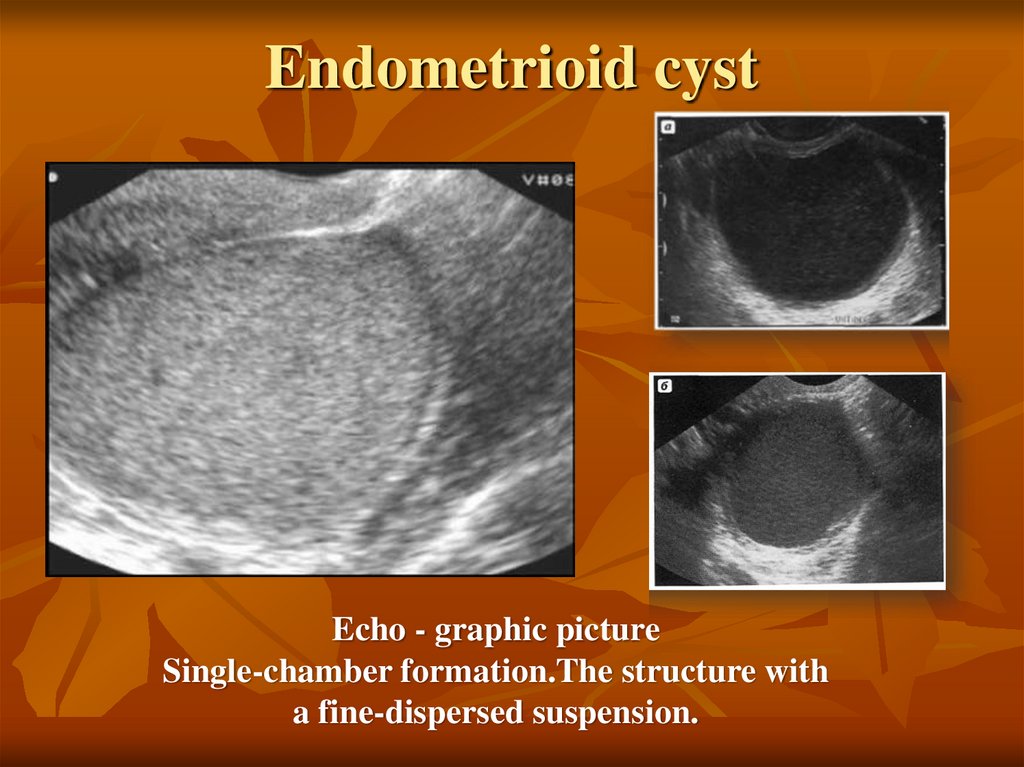
27. Endometrioid cyst
Echo - graphic pictureSingle-chamber formation.The structure with
a fine-dispersed suspension.
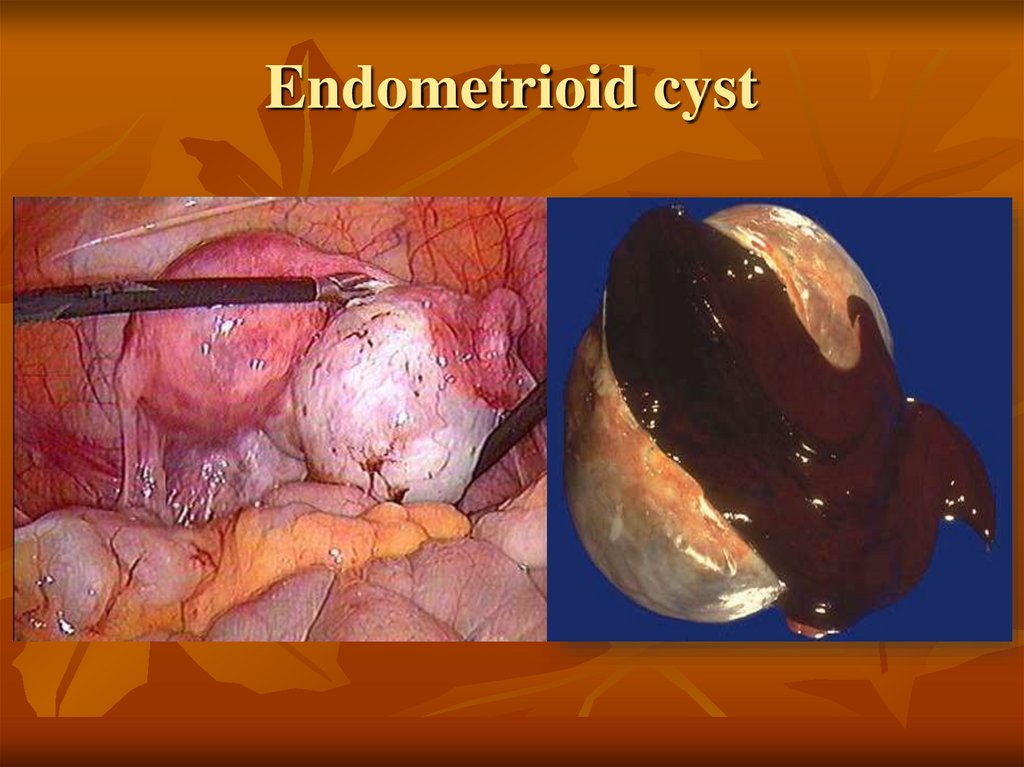
28. Endometrioid cyst
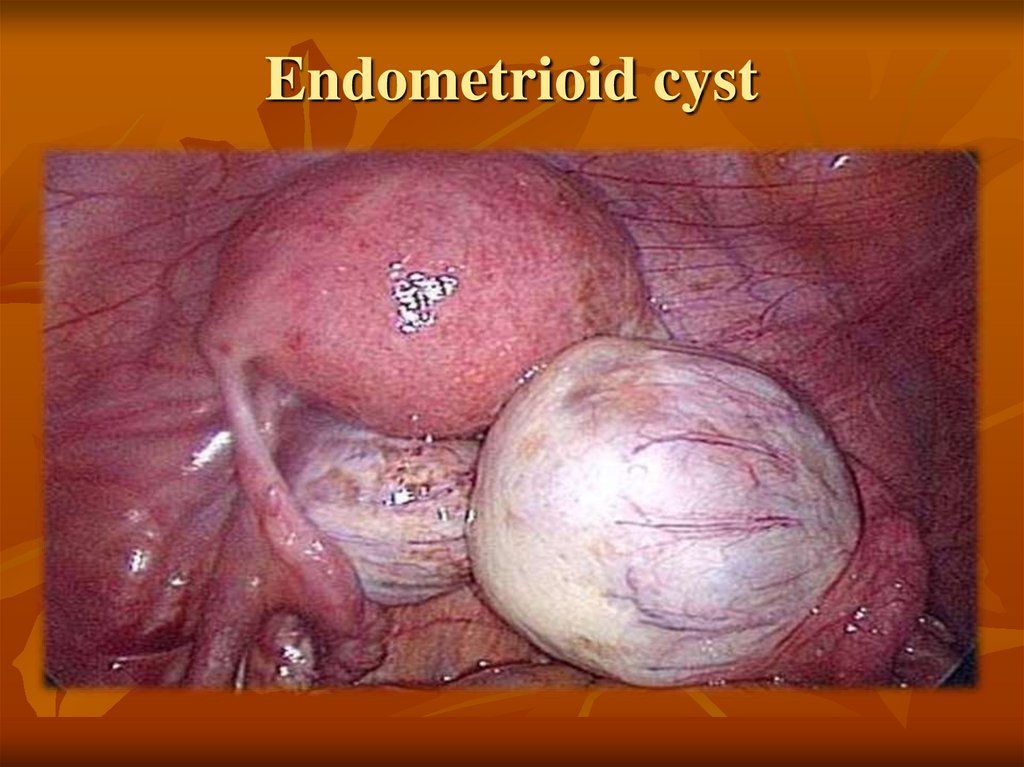
29. Endometrioid cyst
30. Management tactics of a patient with an endometrioid cyst
Two-stage management of the patient:Stage I - planned surgical treatment in the volume of
organ-preserving surgery (separation of adhesions,
cyst exfoliation, coagulation of cyst capsule, rarely
ovarian resection).
Stage II - drug hormone therapy in continuous mode
for up to 6 months.
In the presence of complications - cyst rupture emergency surgical treatment in volume of organpreserving surgery.
31. Benign ovarian tumors
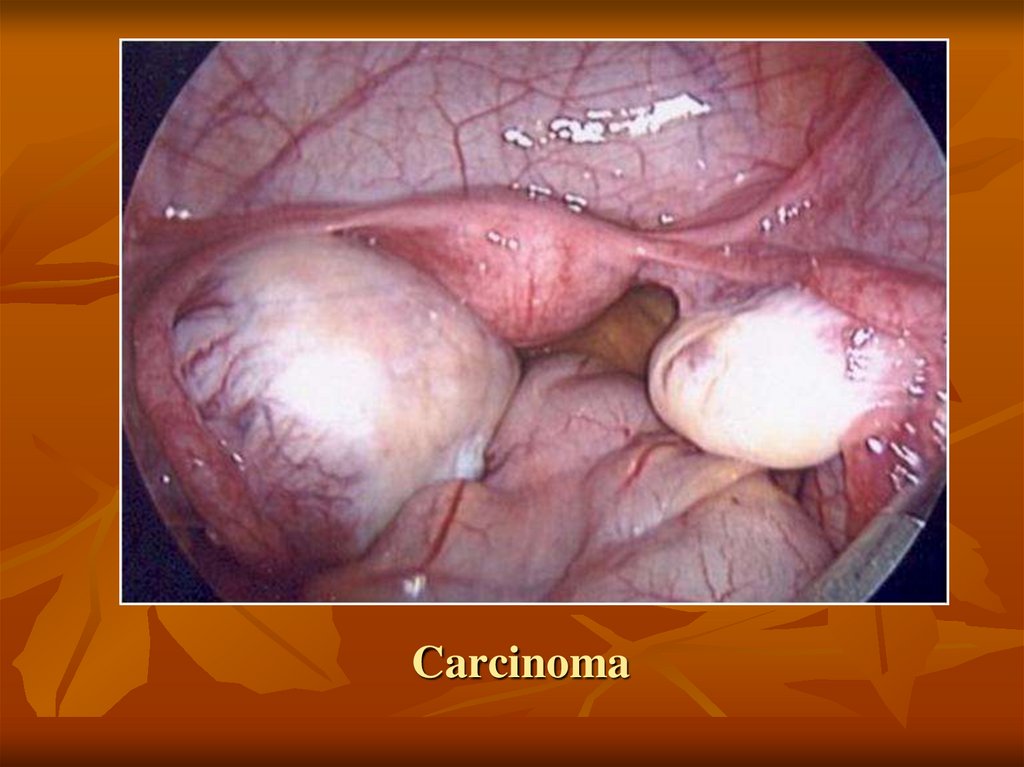
Epithelial ovarian tumors have no specific clinicalpicture. Tumors are one-sided, mobile, painless, up
to 10-15 cm, of a tight elastic consistency. Bilateral
tumors should be considered as a suspicion of
malignancy.
32. Benign ovarian tumors
Tumors of the genital cord and stromal cell. In 10-14%are hormone-producing. Tumors are one-sided, dense,
painless, small in size. There may be malignant variants.
Masculinizing tumors (Sertoli - Leydig) are rare. Causes
signs of virilization.
33. Benign ovarian tumors
Germinogenic tumors. The most commonly diagnosedbenign germinogenic tumor is a mature teratoma. As a
rule, the tumor is one-sided, in 15-25% of patients it can
be bilateral, mobile, uneven consistency, up to 15 cm in
diameter. In a mature teratoma, you can find the
beginnings of any tissue: hair, fatty inclusions,
rudiments of teeth.
34. Dagnostics
1. Laboratory testsTumor markers:
* oncophetal and oncoplacental Antigens (cancer-embryonic antigen, alphafetoprotein, HCG) have diagnostic value in germinogenic tumors.
* tumor associated Antigen (CA 125, CA 19-9). CA 125 may increase with
inflammation, endometriosis, pregnancy.
* growth factor (VEGF - vascular endothelial growth factor)
* oncogen products (BRCA1,2)
35. Dagnostics:
2. instrumental examination- ultrasound examination;
- CT, MRI scan;
- - endoscopic methods:
a)
FGDS – for examination of the stomach in order to exclude metastases
to the ovaries (Krukenberg tumor).
b)
Colonoscopy - to exclude involvement in cancer process the colon.
c)
Laparoscopy - visualization of metastases in salpinx, intra-abdominal
fluid sampling for the presence of cancer cells.
An operative biopsy is possible.
36. Differential diagnostics
First of all, it is carried out withtumorous formations of the ovaries,
because this is important for choosing
the tactics of management and
preservation of reproductive function.
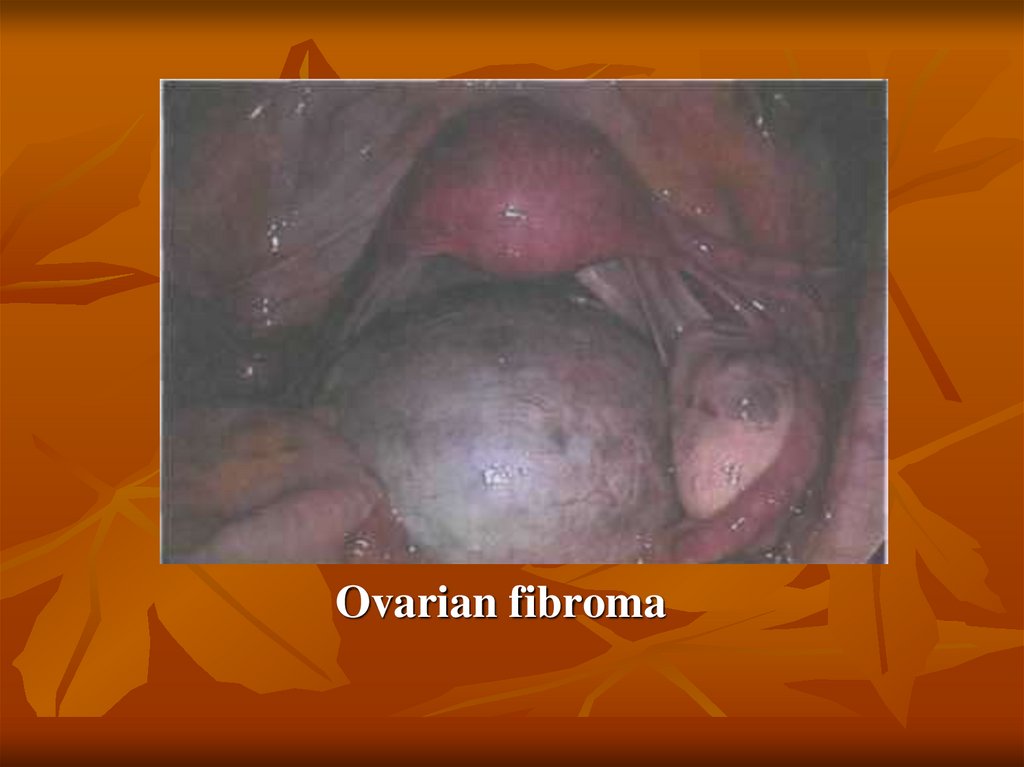
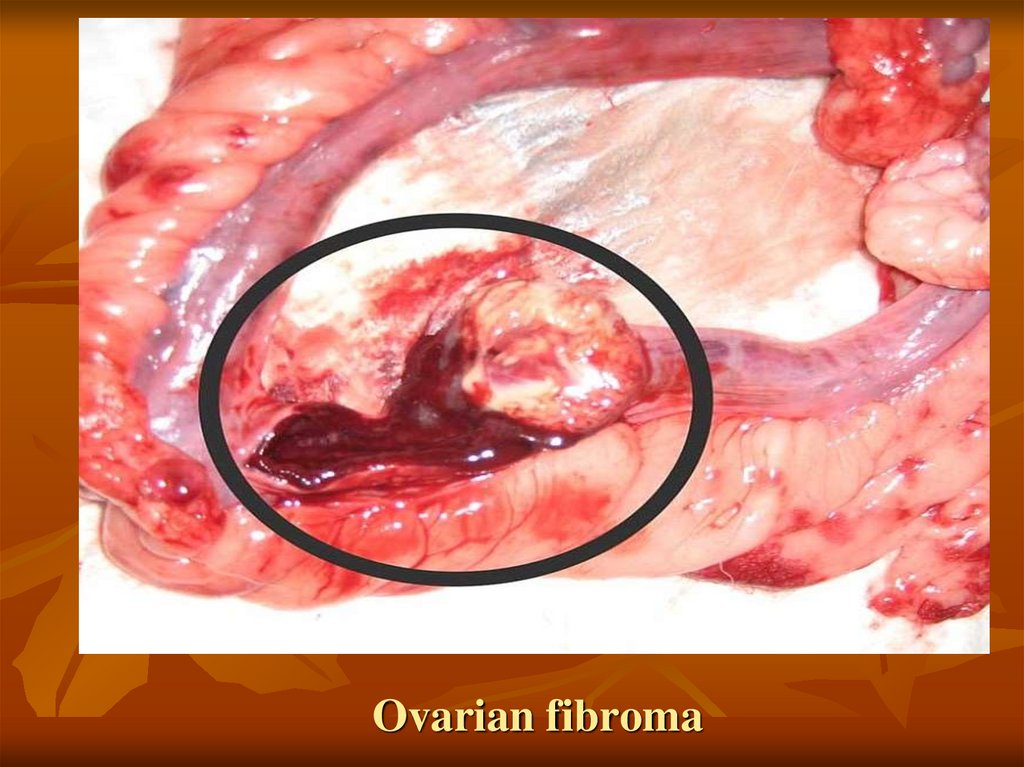
37. Ovarian fibroma
38. Brenner's tumor
39. Tecoma
40. Carcinoma
41. Mucinous cystadenoma
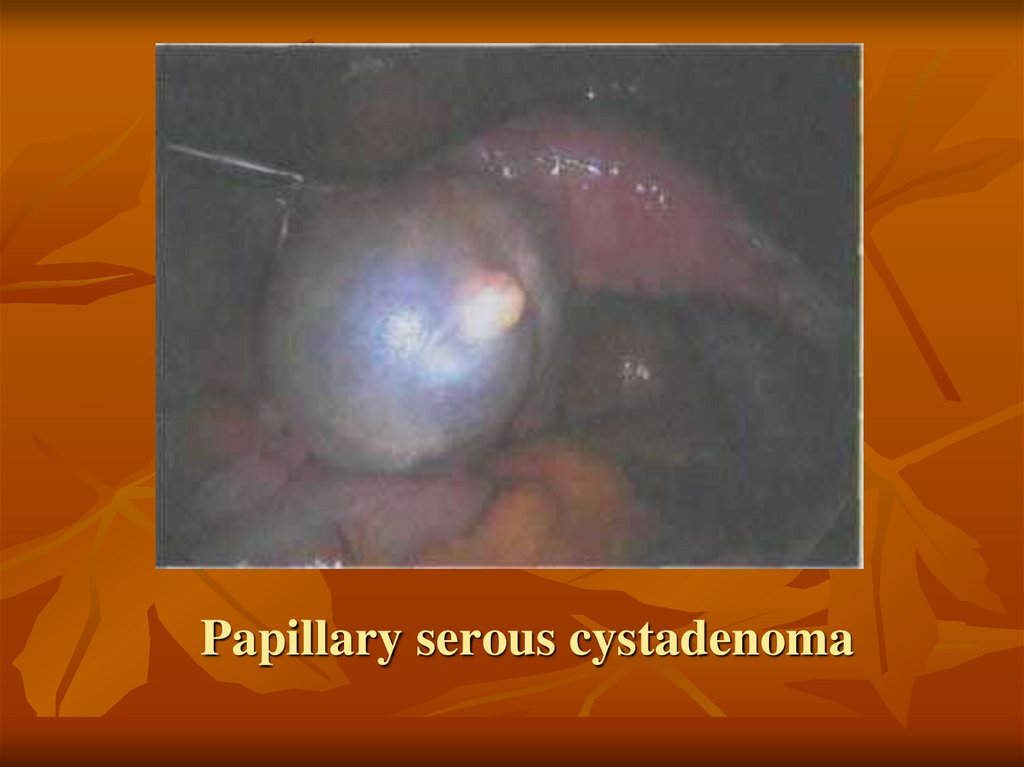
42. Papillary serous cystadenoma
43. Teca-cellular tumor
44. Germinogenic tumors
Mature teratoma45. Ovarian fibroma
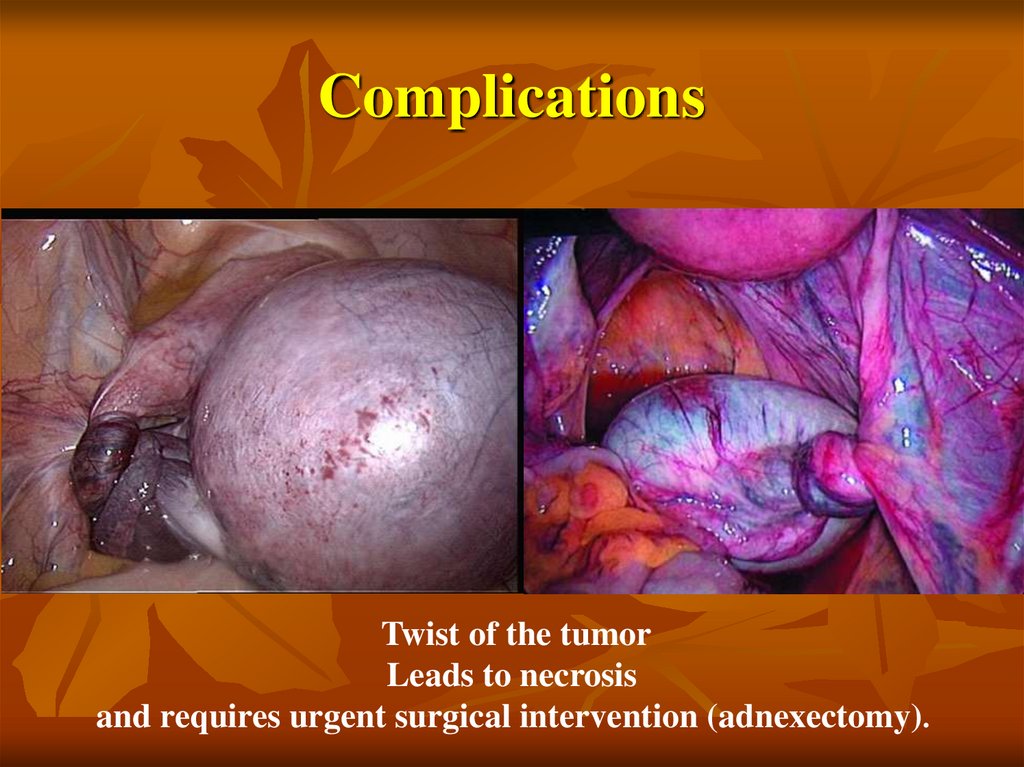
46. Complications
Twist of the tumorLeads to necrosis
and requires urgent surgical intervention (adnexectomy).
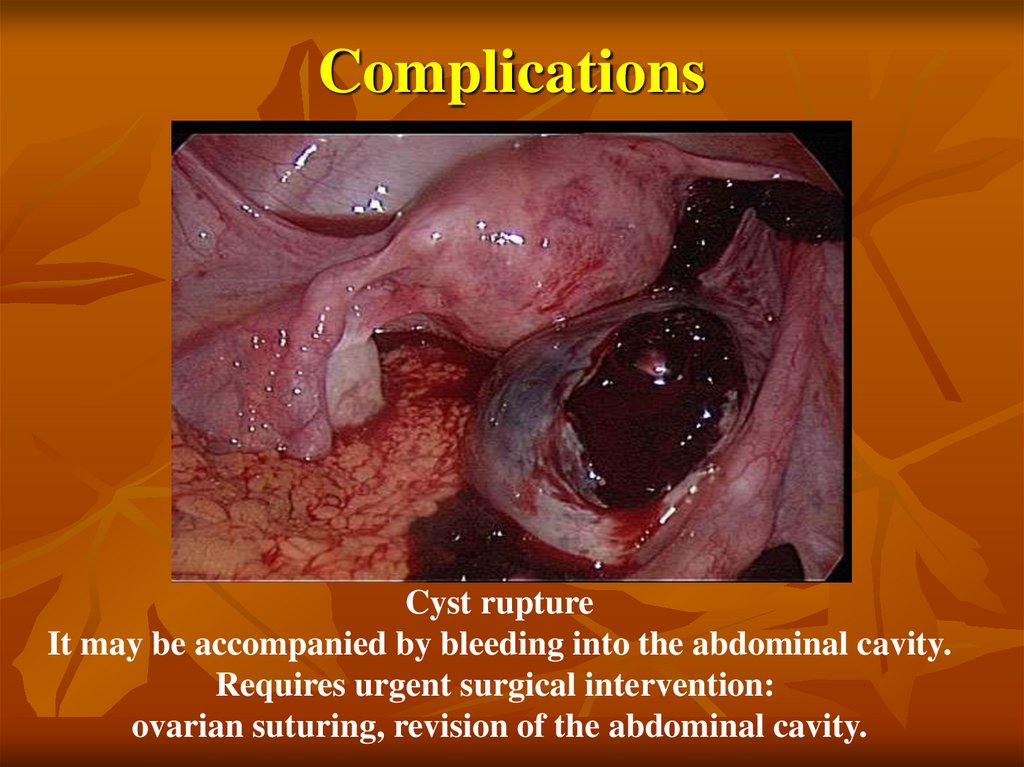
47. Complications
Cyst ruptureIt may be accompanied by bleeding into the abdominal cavity.
Requires urgent surgical intervention:
ovarian suturing, revision of the abdominal cavity.
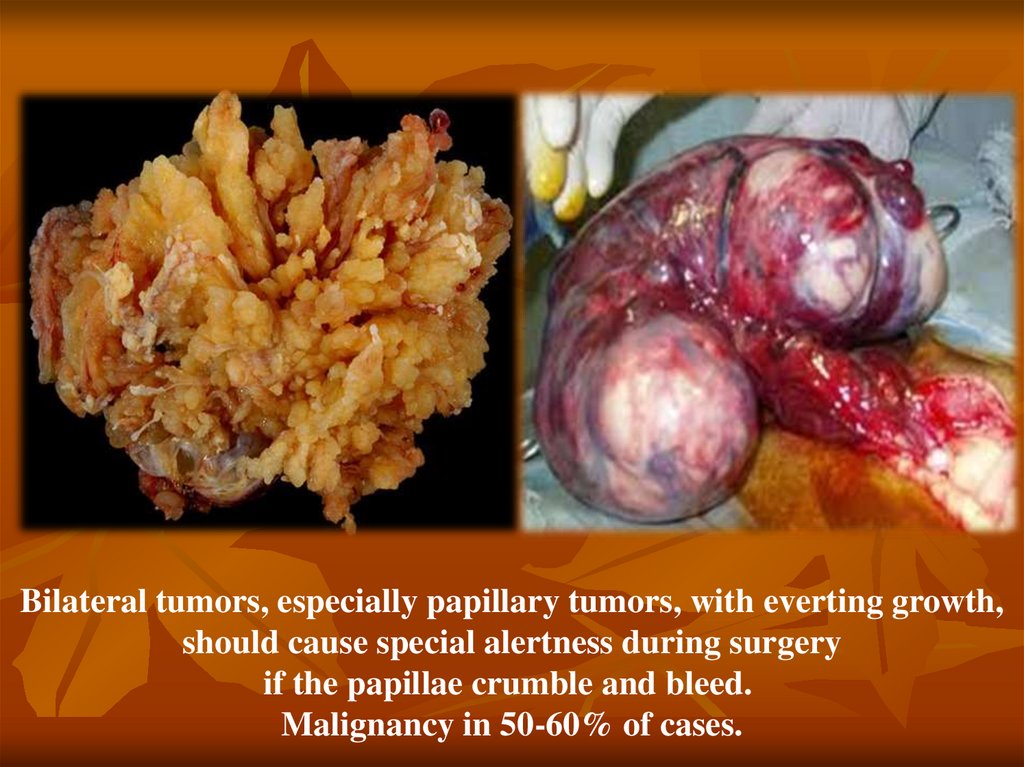
48.
Bilateral tumors, especially papillary tumors, with everting growth,should cause special alertness during surgery
if the papillae crumble and bleed.
Malignancy in 50-60% of cases.
49. Treatment:
Operational only. Any true tumor is an absolute indication forsurgical treatment, adnexectomy is performed at the
reproductive age, and hysterectomy with appendages is
performed at perimenopause. Currently, laparoscopic access is
chosen. If malignancy is suspected and if the emergency
histological examination data are questionable, an adnexectomy
is performed from the affected side, a sectoral biopsy of the
contralateral ovary, an omentectomy, flushes from the lateral
canals, pelvis and subdiaphragmatic space. The final
management tactics are determined after receiving the data of a
planned histological examination and verification of the
morphological diagnosis.















 medicine
medicine