Similar presentations:
Injury of the vision organ
1.
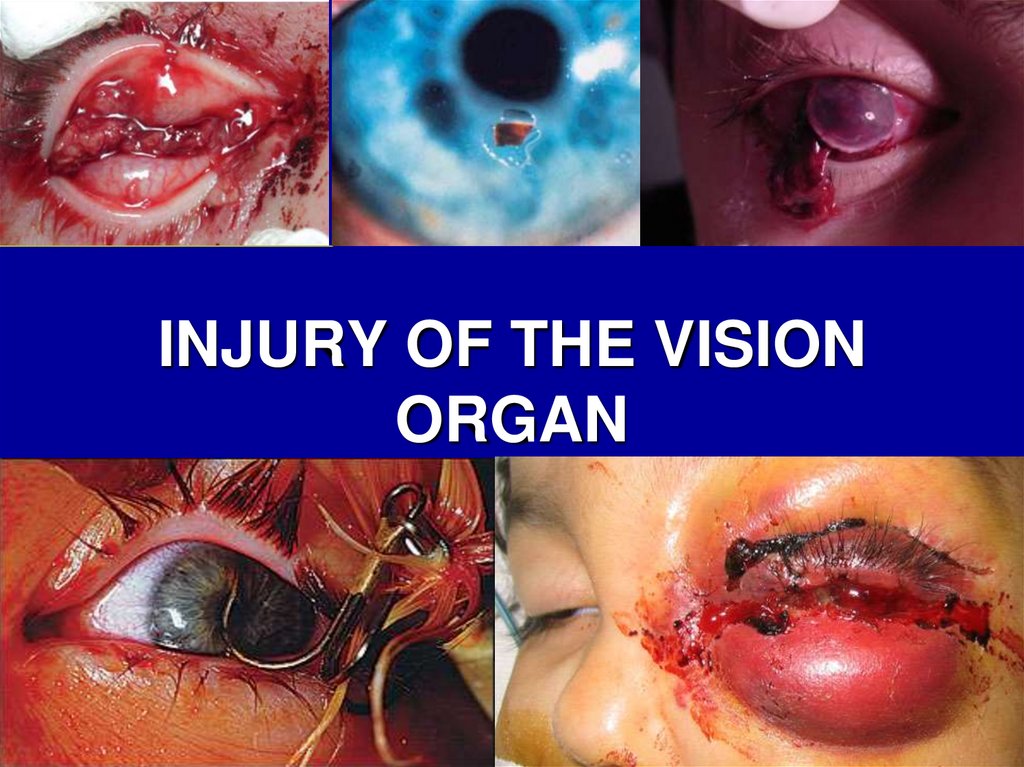
INJURY OF THE VISIONORGAN
2.
• An injury to the eye or its surroundingtissues is the most common cause for
attendance at an eye hospital emergency
department.
• The resultant ocular damage may be
minor or severe with loss of vision or even
the eye
• Globally, more than 500 000 blinding
injuries occur every year.
3.
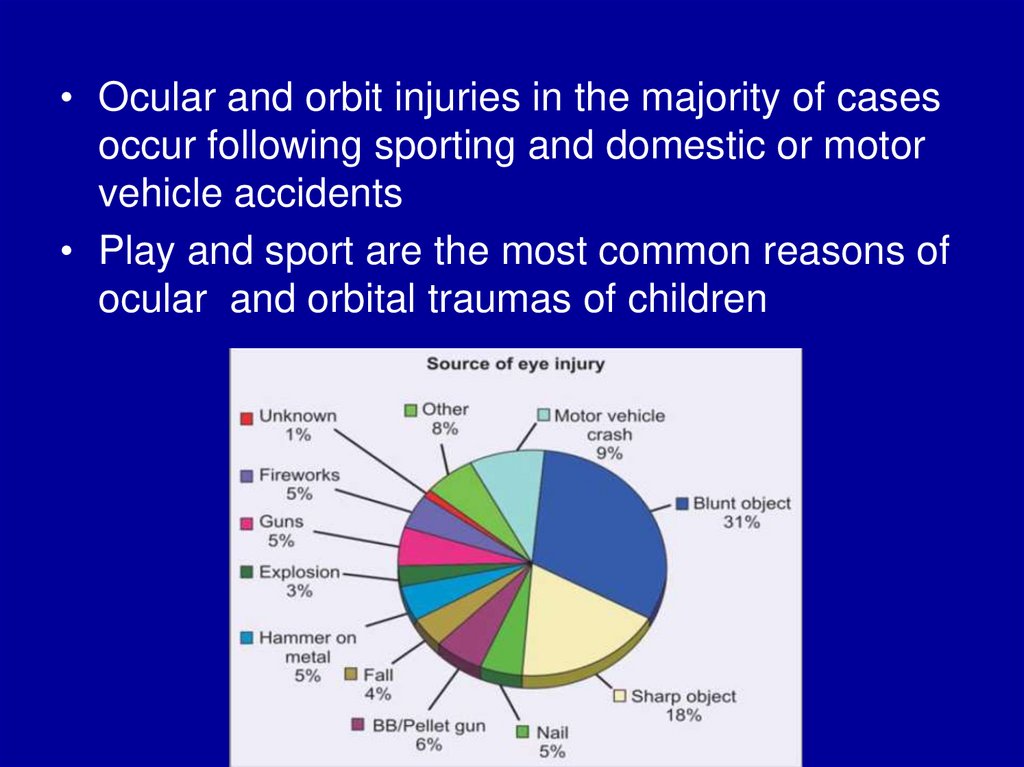
• Ocular and orbit injuries in the majority of casesoccur following sporting and domestic or motor
vehicle accidents
• Play and sport are the most common reasons of
ocular and orbital traumas of children
4.
5.
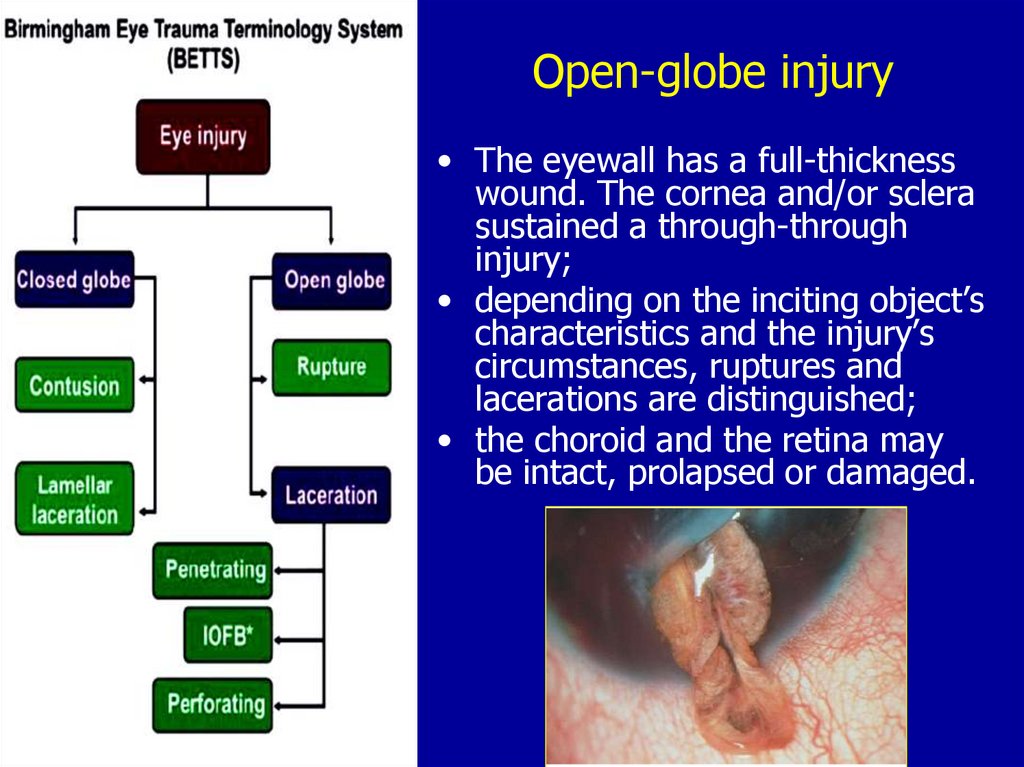
Classification.Birmingham Eye Trauma Terminology System
The double-framed boxes show the diagnoses that are used in clinical practice
6.
Closed-globe injuryThe eyewall does not have a fullthickness wound. Either there is
no corneal or scleral wound at
all (contusion) or is it only
partial thickness (lamellar
laceration).
Extraocular foreign bodies, abrasions,
burns, chemical injuries - close-globe
injury with lamellar laceration
7.
Open-globe injury• The eyewall has a full-thickness
wound. The cornea and/or sclera
sustained a through-through
injury;
• depending on the inciting object’s
characteristics and the injury’s
circumstances, ruptures and
lacerations are distinguished;
• the choroid and the retina may
be intact, prolapsed or damaged.
8.
Open-globe injuryRupture
• Full-thickness wound of the
eyewall, caused by a blunt object;
• the impact results in momentary
increase of the intraocular
pressure.
• The eyewall gives way at its
weakest point (at the impact site
or elsewhere; example: an old
cataract wound dehisces even
though the impact occurred
elsewhere);
• the actual wound is produced by
an inside-out mechanism.
9.
Open-globe injuryLaceration
• Full-thickness wound of the eyewall,
usually caused by a sharp object: needle,
knife, scissors or flying metallic foreign
bodies; the wound occurs at the impact
site by an outside-in mechanism.
• Penetrating injury. Single laceration of
the eyewall, usually caused by a sharp
object. No exit wound has occurred; if
more than one entrance wound is present,
each must have been caused by a
different agent.
• Intraocular foreign body injury
(IOFB).
• Perforating injury. Two full-thickness
lacerations (entrance and exit) of the
eyewall, usually caused by a sharp object
or missile. The two wounds must have
been caused by the same agent.
10.
Open-globe injuryLaceration
Penetrating injury.
IOFB
Perforating injury.
11.
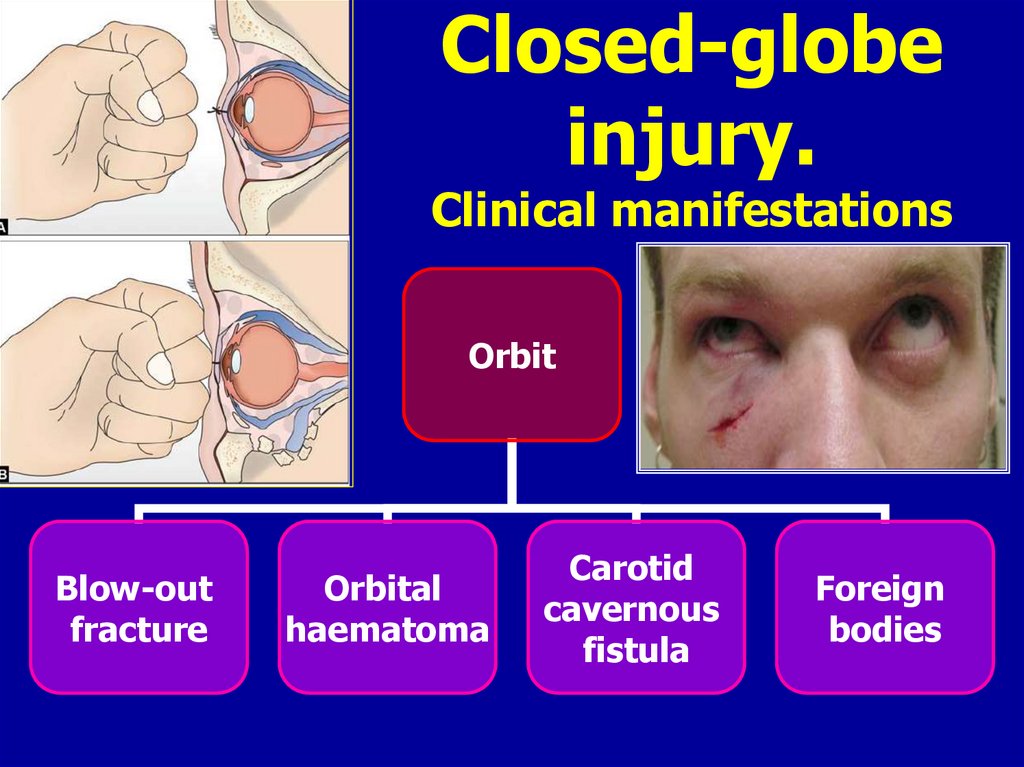
Closed-globeinjury.
Clinical manifestations
Orbit
Blow-out
fracture
Orbital
haematoma
Carotid
cavernous
fistula
Foreign
bodies
12.
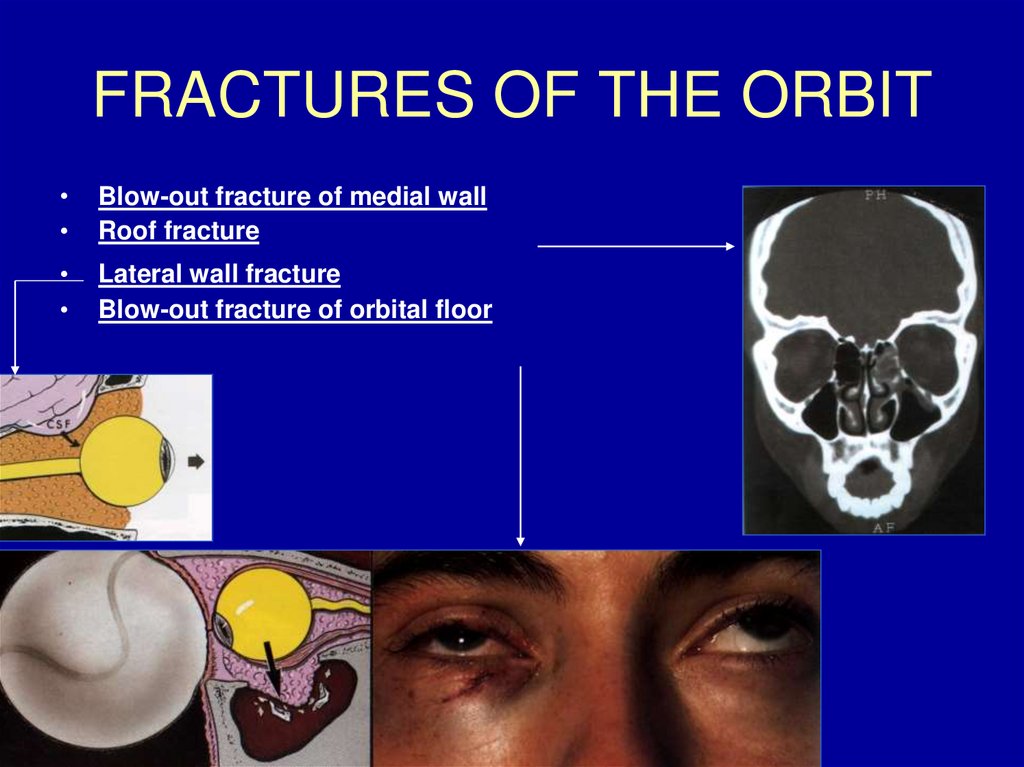
FRACTURES OF THE ORBITBlow-out fracture of medial wall
Roof fracture
Lateral wall fracture
Blow-out fracture of orbital floor
13.
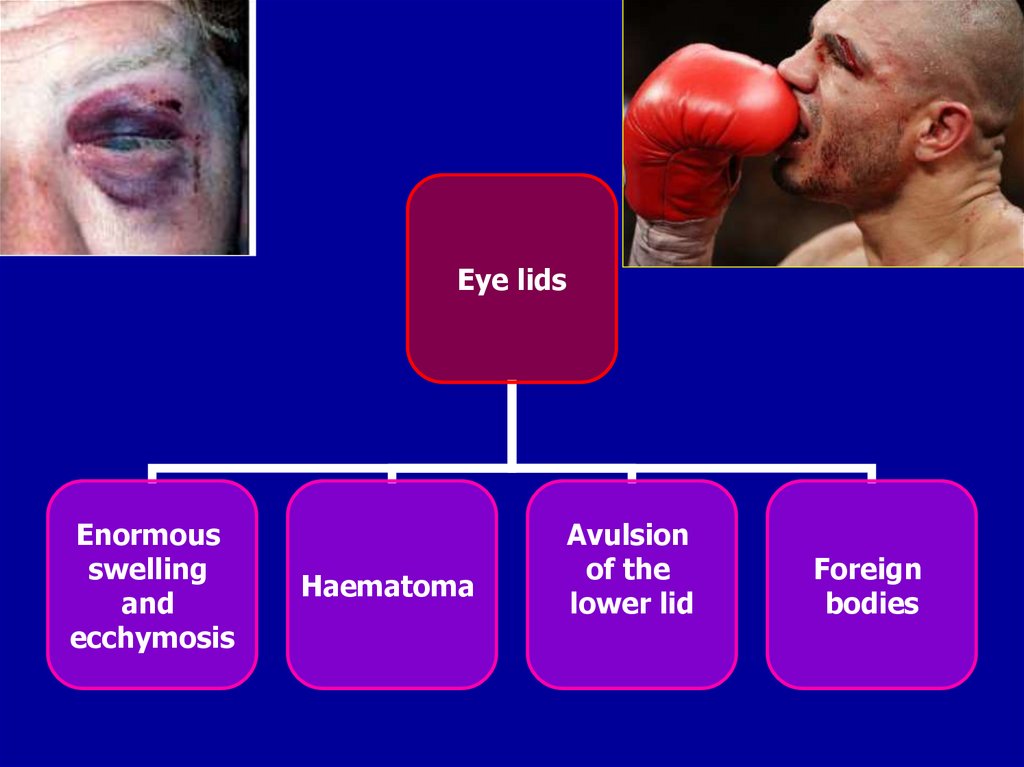
Eye lidsEnormous
swelling
and
ecchymosis
Haematoma
Avulsion
of the
lower lid
Foreign
bodies
14.
ConjunctivaSubconjunctival
haemorrhage
Conjunctival
laceration
Conjunctival
foreign bodies
15.
CorneaAbrasions
Stromal
oedema
partial
rupture
blood
staining
of cornea
foreign
bodies
16.
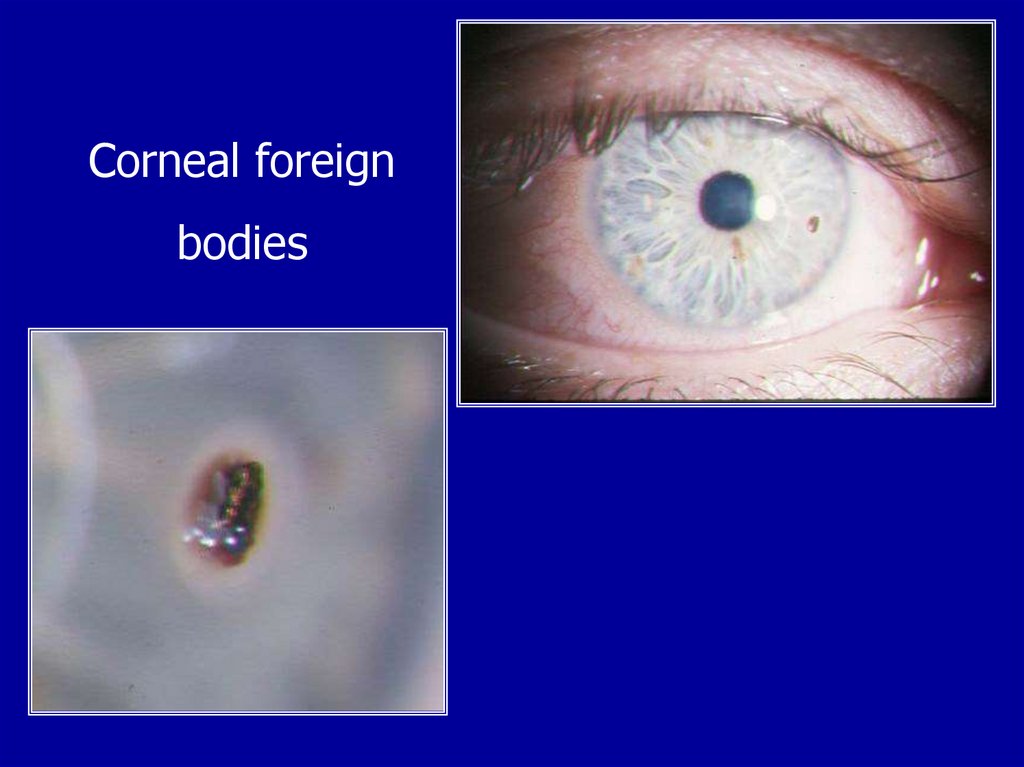
Corneal foreignbodies
17.
To Remove a Corneal FB Using aNeedle
18.
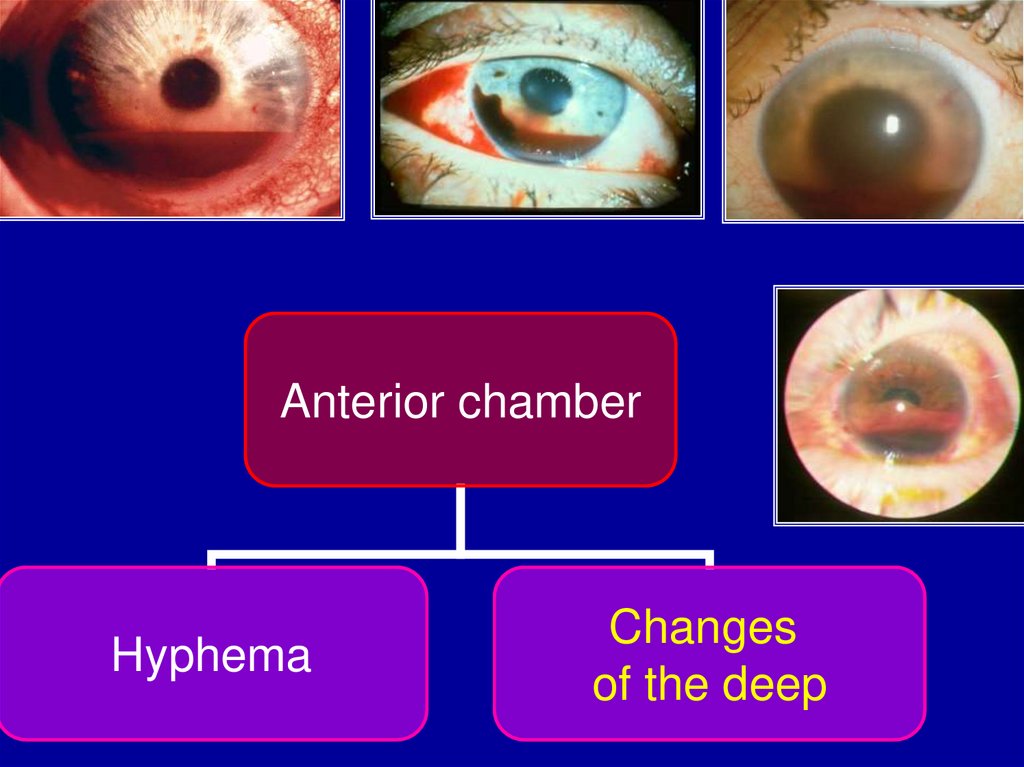
Anterior chamberHyphema
Changes
of the deep
19.
Anterior uveaIridodialysis
Tear
of the
iris sphincter
Iridoschisis
angle
recession
20.
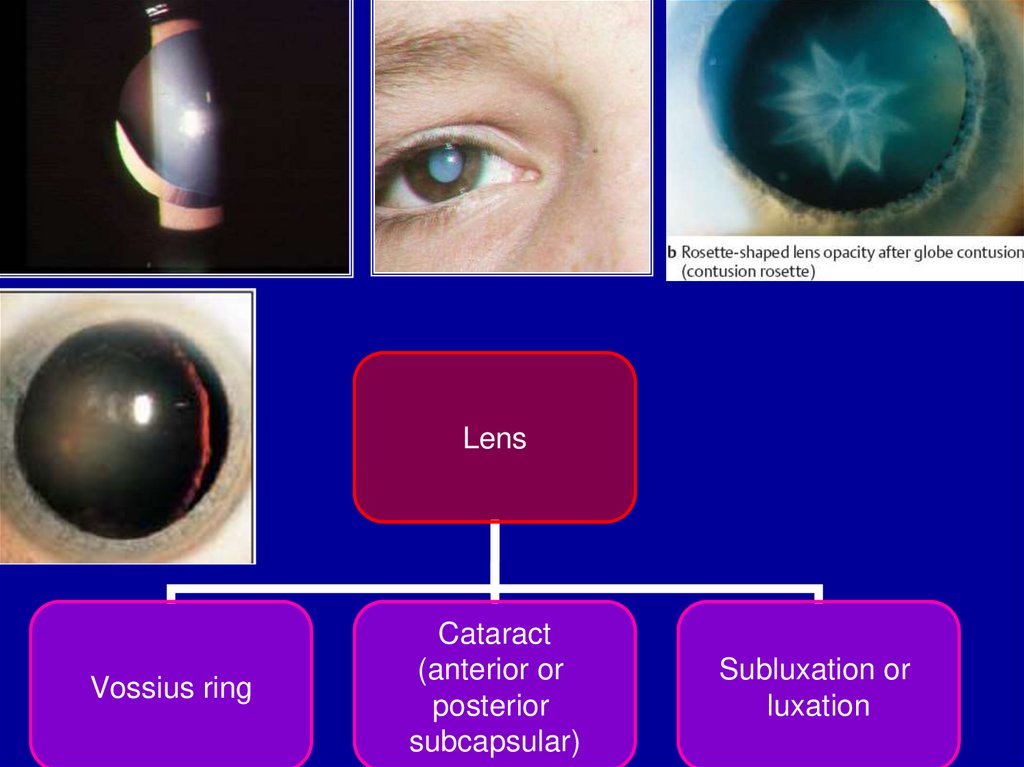
LensVossius ring
Cataract
(anterior or
posterior
subcapsular)
Subluxation or
luxation
21.
Vitreousposterior
vitreous
detachment
hemorrhage
22.
Retinaehemorrhages
Berlin’s oedema
Macular oedema
or holes
Retinal dialysis
23.
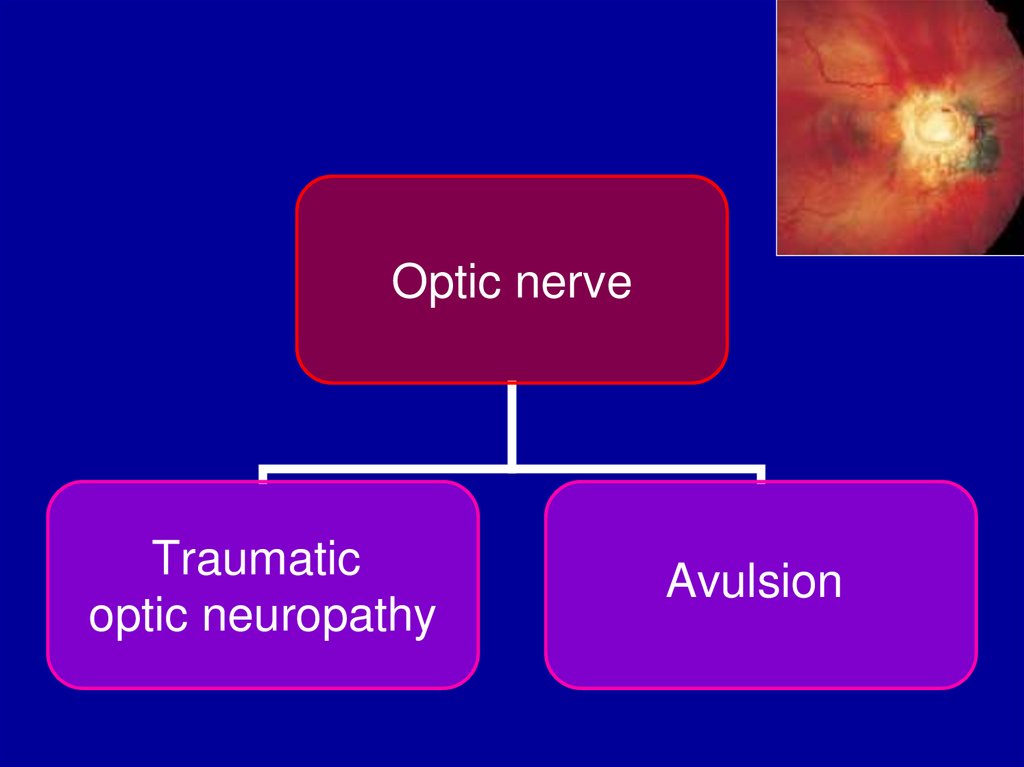
Optic nerveTraumatic
optic neuropathy
Avulsion
24.
BurnsThermal
Chemical
Alkaly
Acid
UV burns
25.
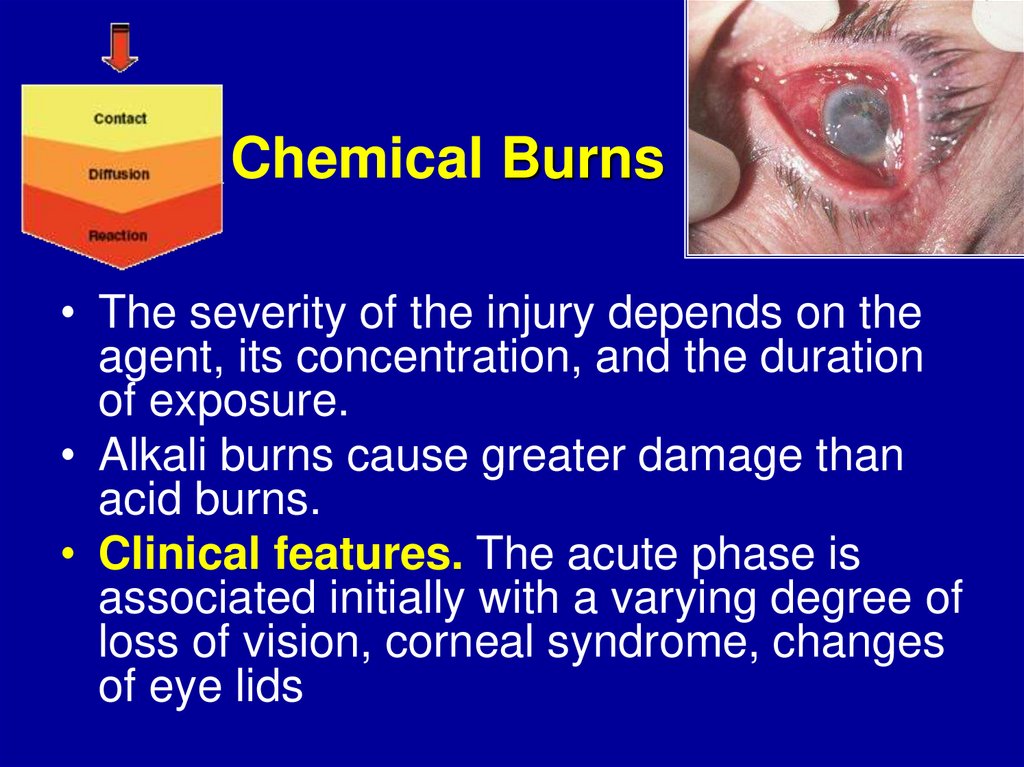
Chemical Burns• The severity of the injury depends on the
agent, its concentration, and the duration
of exposure.
• Alkali burns cause greater damage than
acid burns.
• Clinical features. The acute phase is
associated initially with a varying degree of
loss of vision, corneal syndrome, changes
of eye lids
26.
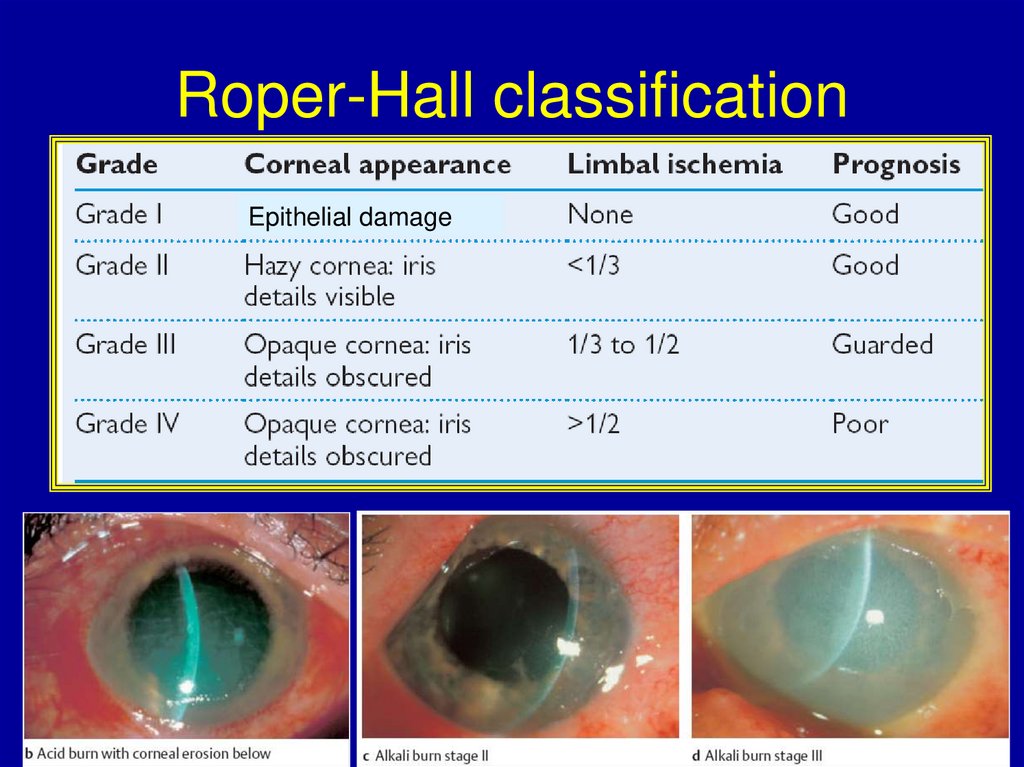
Roper-Hall classificationEpithelial damage
27.
Treatment of chemicalburns
• Prophylaxis of shock - local and systemic
analgesia.
• Mechanical removing the pieces of
damage matter with turning out of upper
lid
• Profuse irrigation with water, BSS and
antiseptic solutions
• Local and systemic antibacterial drugs
• Tetanus prophylaxis
• Ointment or oil for prophylaxis of
symblepharon
• The skin is treated with spray (Panthenol,
Levamisol, etc.).
28.
ComplicationsCorneal opacity
Symblepharon
Recurrent corneal ulceration
Complicated cataract
Secondary glaucoma
29.
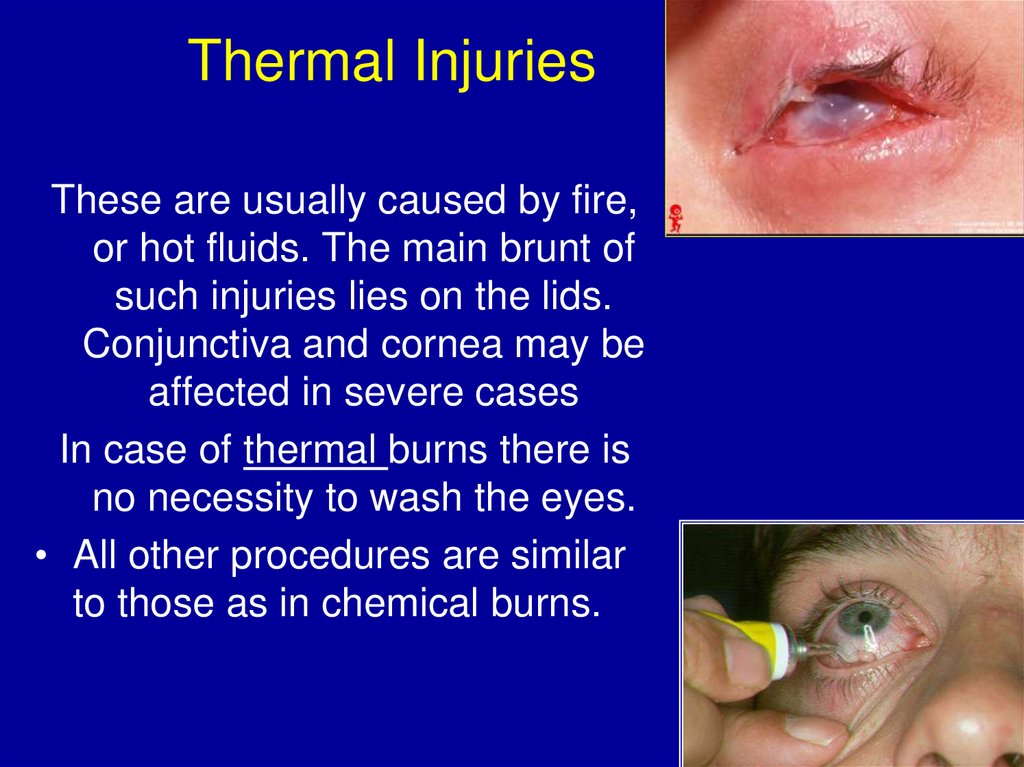
Thermal InjuriesThese are usually caused by fire,
or hot fluids. The main brunt of
such injuries lies on the lids.
Conjunctiva and cornea may be
affected in severe cases
In case of thermal burns there is
no necessity to wash the eyes.
• All other procedures are similar
to those as in chemical burns.
30.
Ultraviolet (UV) burnsEtiology:
• welding without proper eye protection,
• exposure to high-altitude sunlight,
• sunlight reflected of snow when skiing at high altitudes on a
sunny day.
• Symptoms typically manifest themselves after a latency
period of six to eight hours. This causes patients to seek the
aid of an ophthalmologist or eye clinic in the middle of the
night, complaining of “acute blindness” accompanied by
corneal syndrom.
• examination will reveal epithelial edema and superficial
punctate keratitis or erosion in the palpebral fissure.
31.
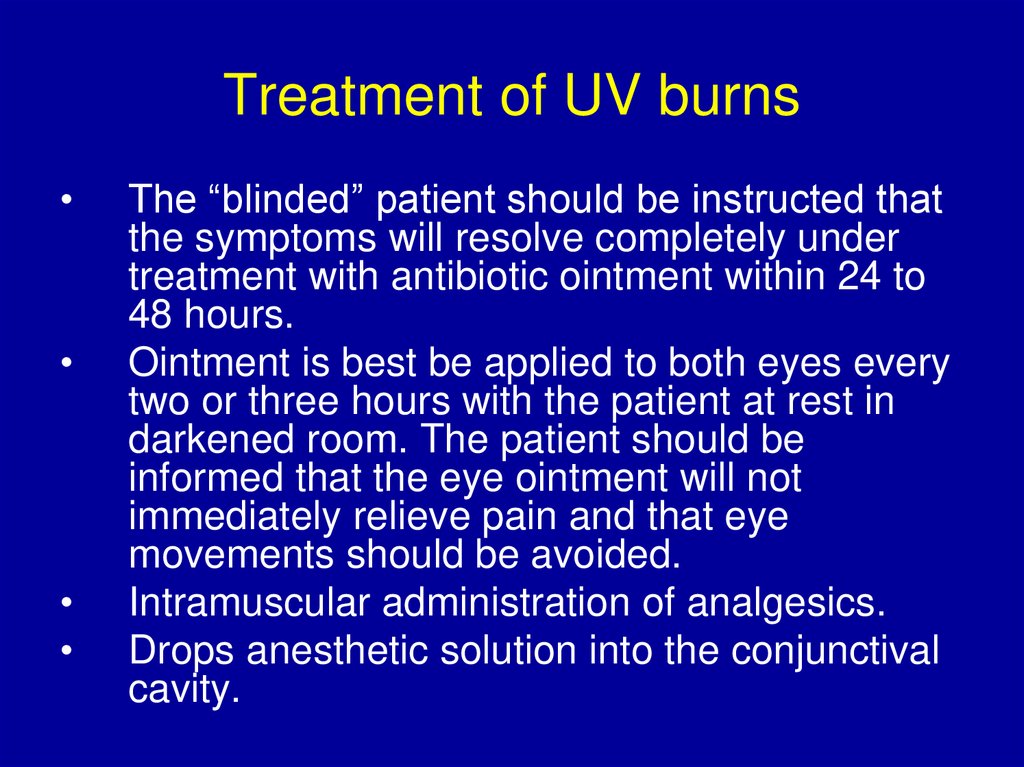
Treatment of UV burnsThe “blinded” patient should be instructed that
the symptoms will resolve completely under
treatment with antibiotic ointment within 24 to
48 hours.
Ointment is best be applied to both eyes every
two or three hours with the patient at rest in
darkened room. The patient should be
informed that the eye ointment will not
immediately relieve pain and that eye
movements should be avoided.
Intramuscular administration of analgesics.
Drops anesthetic solution into the conjunctival
cavity.
32.
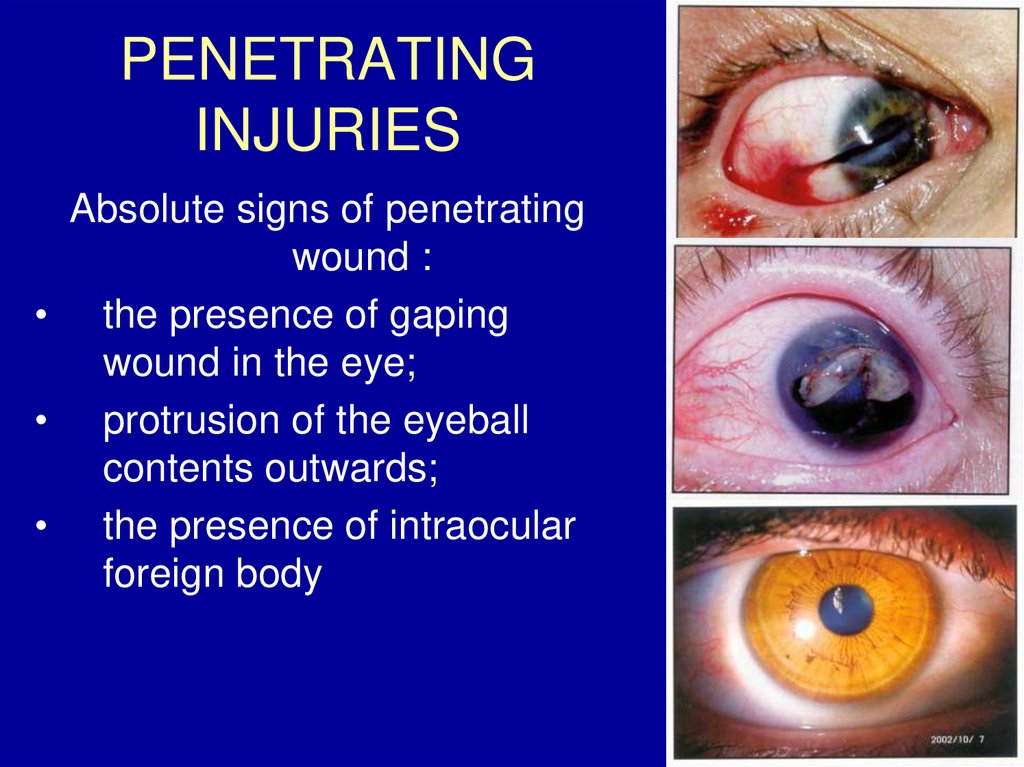
PENETRATINGINJURIES
Absolute signs of penetrating
wound :
• the presence of gaping
wound in the eye;
• protrusion of the eyeball
contents outwards;
• the presence of intraocular
foreign body
33.
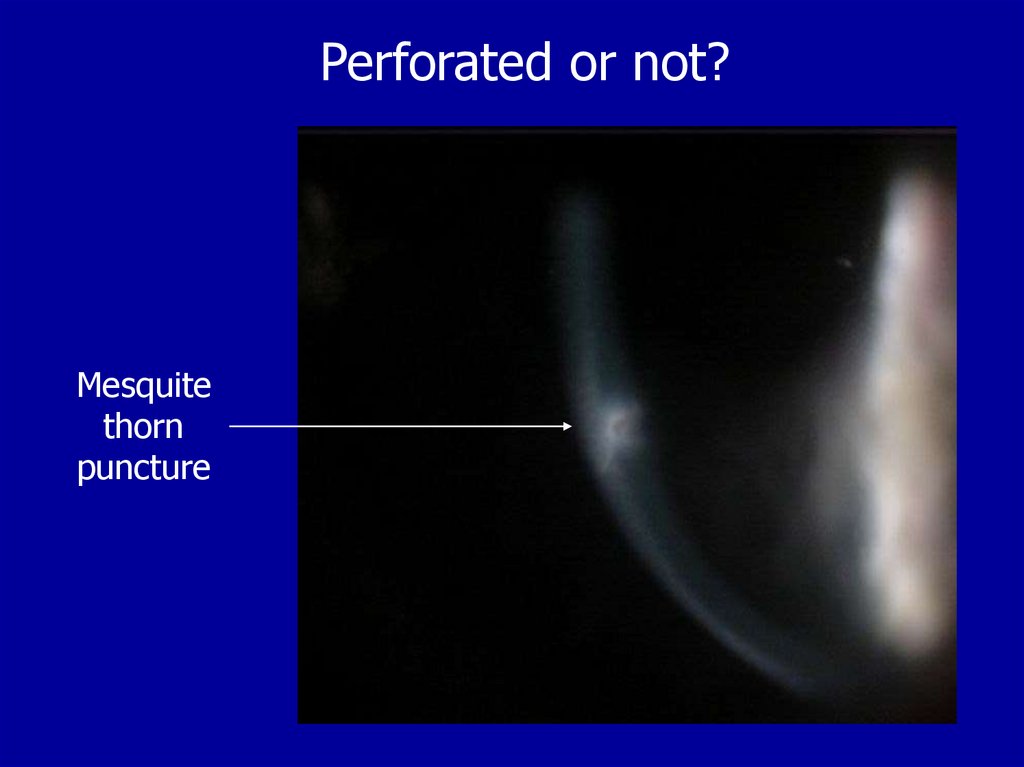
Perforated or not?Mesquite
thorn
puncture
34.
Seidel test: Use concentrated fluorescein35.
P0SITIVE SEIDELPinpoint perforation
Leaking bleb
36.
37.
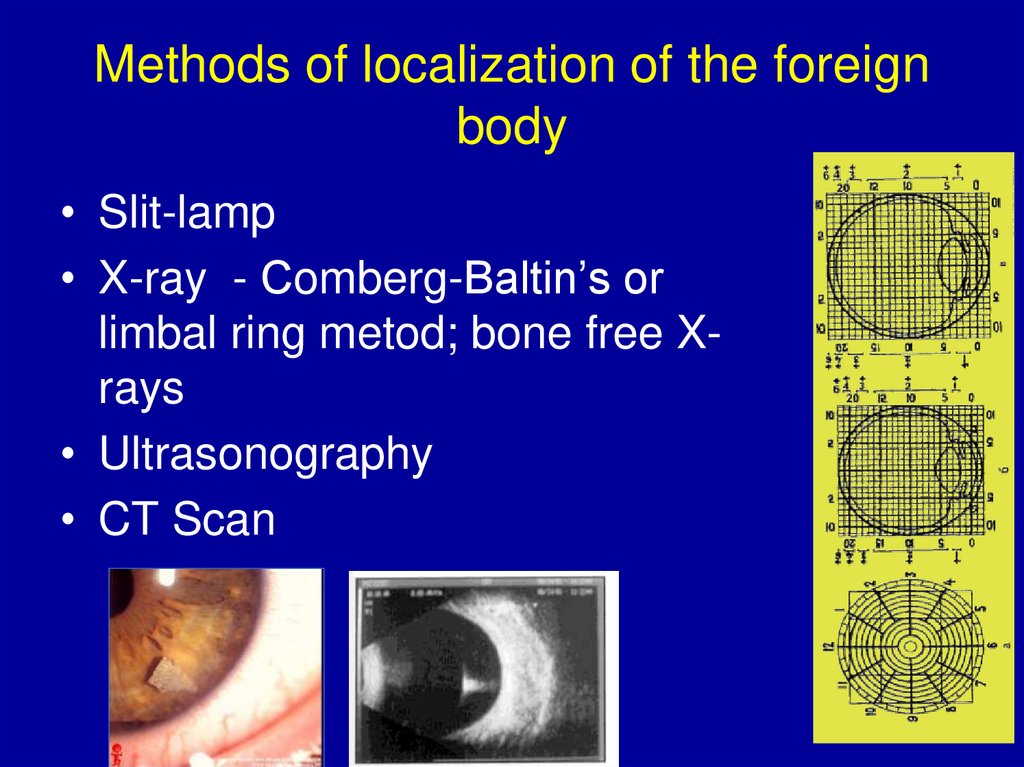
Methods of localization of the foreignbody
• Slit-lamp
• X-ray - Сomberg-Baltin’s or
limbal ring metod; bone free Xrays
• Ultrasonography
• CT Scan
38.
First aid in case of penetratingwound of the cornea
• Prophylaxis of shock - local and systemic
analgesia.
• Prophylaxis of tetanus
• Prophylaxis of infection – local and
systemic antibiotics of broad spectrum
• Binocular bandage
39.
First aid in case of penetratingwound of the sclera
• Prophylaxis of shock - local and systemic
analgesia.
• Prophylaxis of hemorrhages - local and
systemic stopping of bleeding.
• Prophylaxis of tetanus
• Prophylaxis of infection – local and
systemic antibiotics of broad spectrum
• Binocular bandage
40.
The surgical managementof such injuries is directed
primarily at the restoration
of normal ocular anatomy;
the ultimate goal is to
prevent secondary
complications and
maximize the patient’s
visual prognosis.
41.
indications for enucleation ofwounded eye
• Primary enucleation is
performed in case of:
– crushing of the eyeball;
– when a half or more of the vitreous
body is lost.
• Later on an eye is enucleated in
case of:
• Recurrence sympathetic
inflammation of healthy eye;
• painful secondary glaucoma on
the blind eye;
• atrophy of the eyeball.
42.
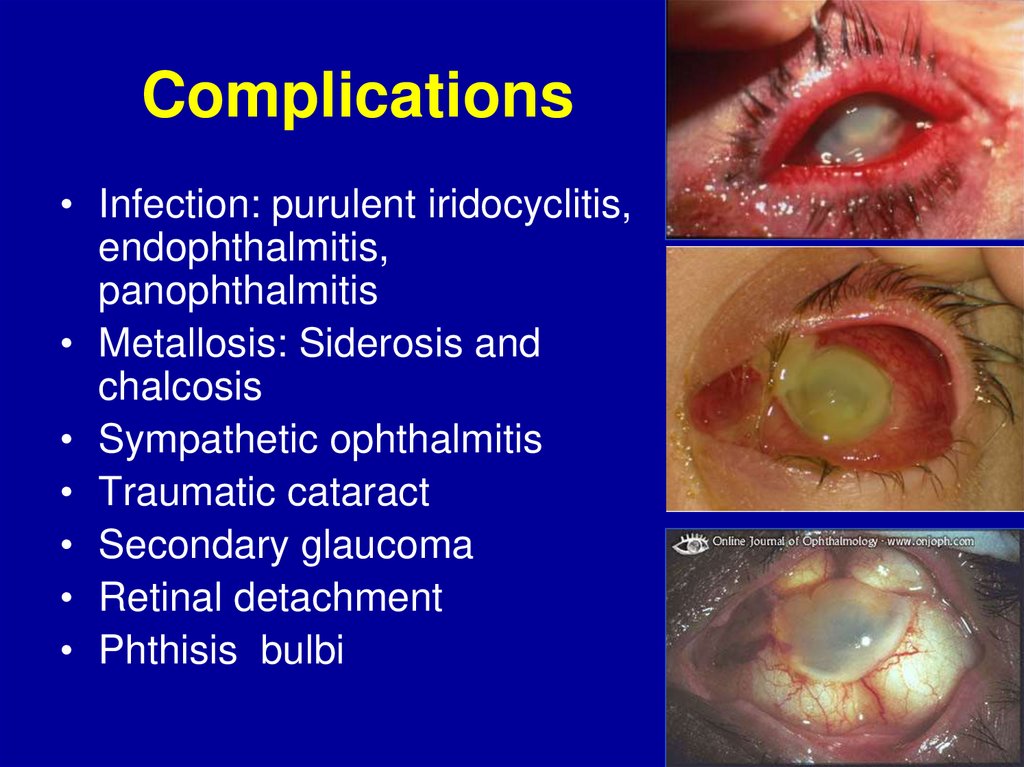
Complications• Infection: purulent iridocyclitis,
endophthalmitis,
panophthalmitis
• Metallosis: Siderosis and
chalcosis
• Sympathetic ophthalmitis
• Traumatic cataract
• Secondary glaucoma
• Retinal detachment
• Phthisis bulbi
43.
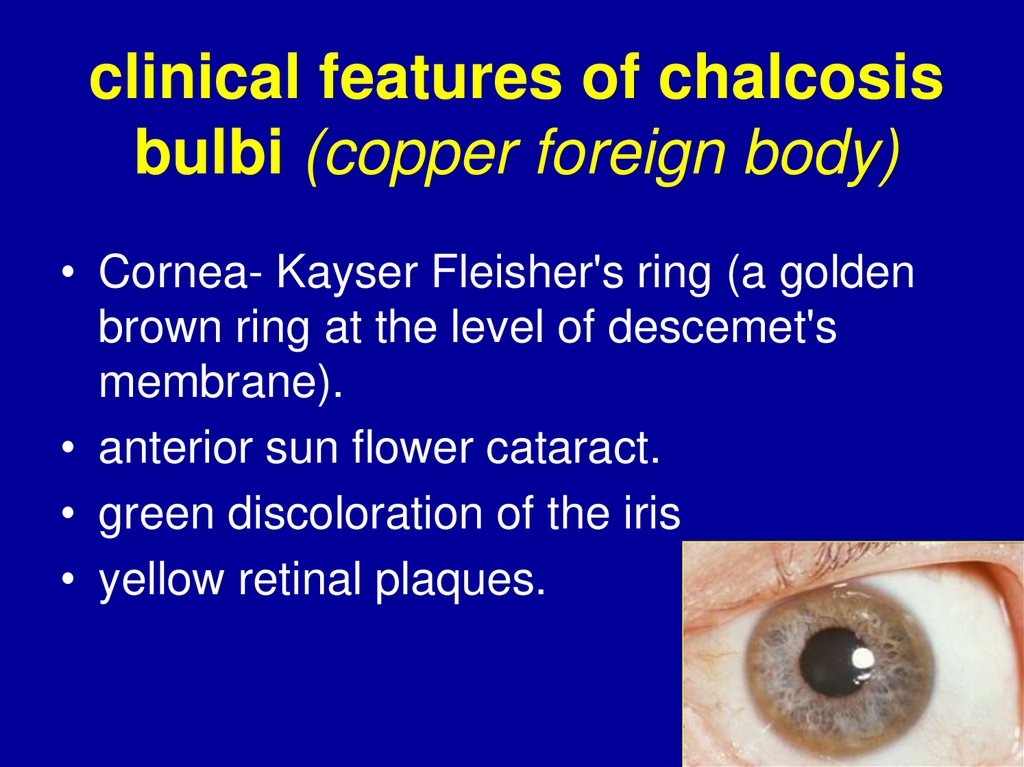
clinical features of chalcosisbulbi (copper foreign body)
• Cornea- Kayser Fleisher's ring (a golden
brown ring at the level of descemet's
membrane).
• anterior sun flower cataract.
• green discoloration of the iris
• yellow retinal plaques.
44.
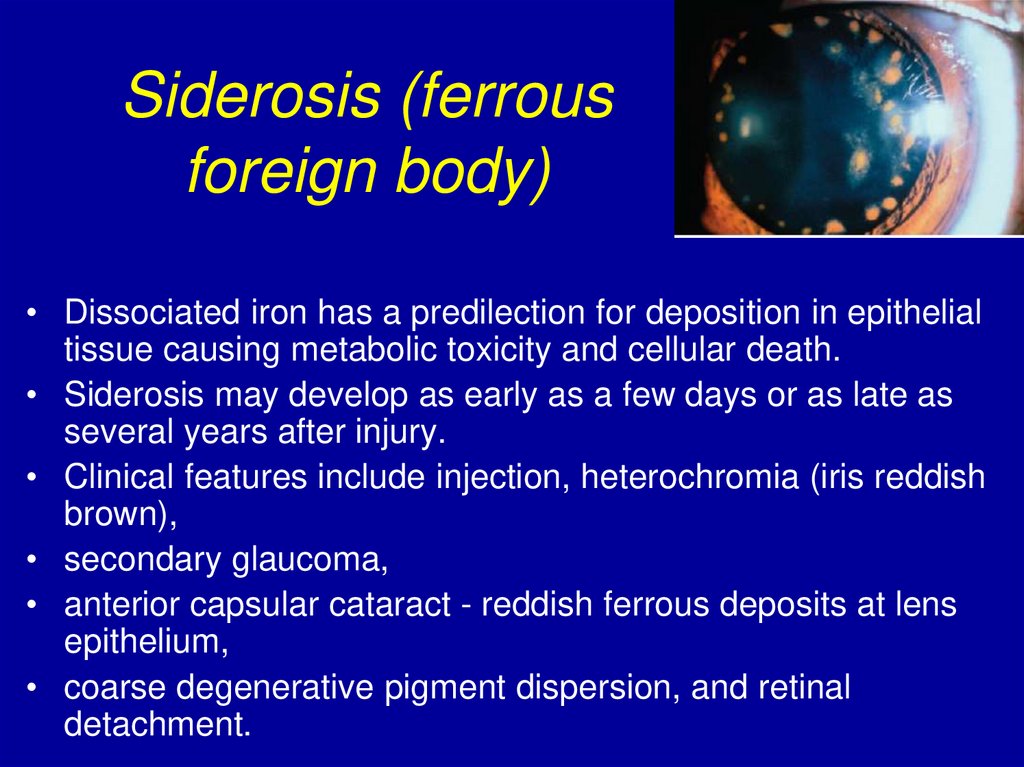
Siderosis (ferrousforeign body)
• Dissociated iron has a predilection for deposition in epithelial
tissue causing metabolic toxicity and cellular death.
• Siderosis may develop as early as a few days or as late as
several years after injury.
• Clinical features include injection, heterochromia (iris reddish
brown),
• secondary glaucoma,
• anterior capsular cataract - reddish ferrous deposits at lens
epithelium,
• coarse degenerative pigment dispersion, and retinal
detachment.
45.
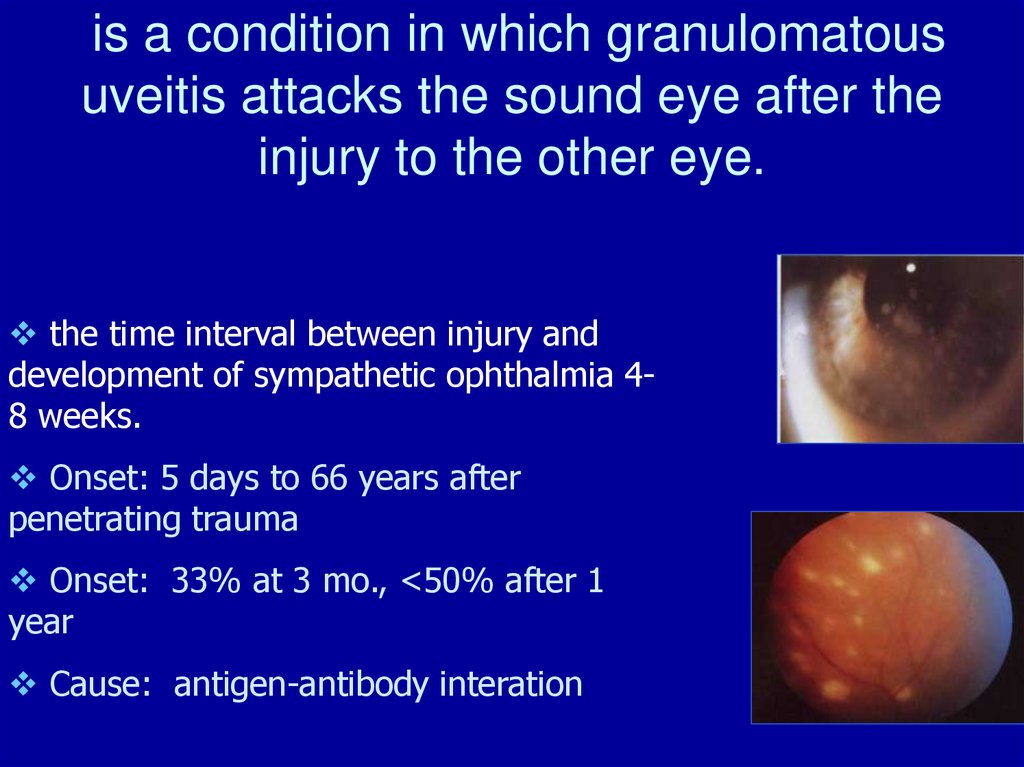
is a condition in which granulomatousuveitis attacks the sound eye after the
injury to the other eye.
the time interval between injury and
development of sympathetic ophthalmia 48 weeks.
Onset: 5 days to 66 years after
penetrating trauma
Onset: 33% at 3 mo., <50% after 1
year
Cause: antigen-antibody interation
46.
treatment of sympatheticinflammation.
1. Early excision of the injured eye.
2. anti-inflammatory treatment (topical
and systemic steroids)
3. immunosuppressent drugs
4. topical atropine

























 medicine
medicine