Similar presentations:
Features of childrens` blood. The semiotics of major hematological syndromes
1.
Features of childrens` blood. The semioticsof major hematological syndromes.
2.
The blood creations or hemogenesis is aprocess of origin and subsequent ripening of
blood cells in the so-called organs of blood
creations. The cells of blood pass whole row
stages in the organs of before abandoning
them forever.
3.
The single cell that gives life to all blood cellsis the polypotentic trunk cell of bone marrow
hemogenesis. The cells-predecessors of
blood cells (blastic cells) must not abandon
the organs of hemogenesis. Otherwise
speaking about unrestrained growth of
number of cells-predecessors as a process it
corresponds to the malignant tumour and is
named leukemia in fact.
4.
About the blood condition we can judge onthe base of peripheral blood composition
making blood tests. About the condition of
hemogenesis it is the most exactly possible to
judge basing on composition of marrow.
5.
Functions of blood and its formed elements.The functions of blood and its formed
elements are varied.
A blood is an original liquid organ and one
of the basic reservoirs of extracellular water.
The liquid part of blood (plasma, serum)
simultaneously is an object and mean to keep
up constancy of organism’s internal
environment (homeostasis). The chemical
composition of plasma is very composite and
counts the thousands known substances.
6.
Using blood circulation the nutrients andoxygen are delivered to the tissues and the
final metabolites are excreted. A blood is a
transporting highway, by means of which the
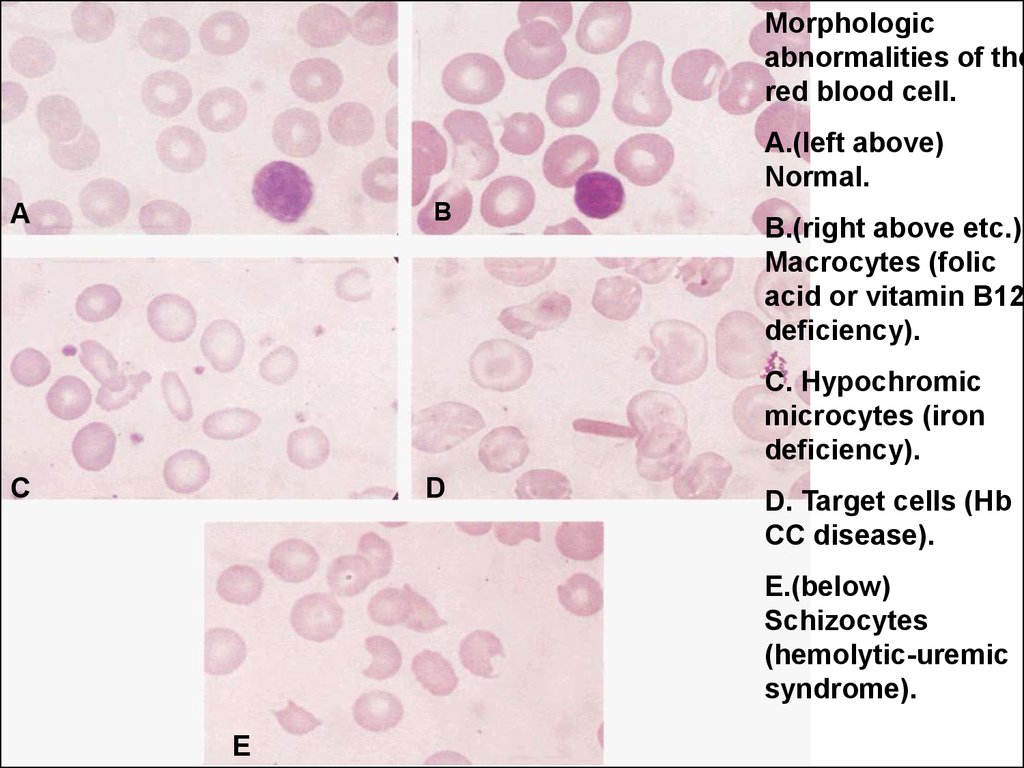
humoral regulation is carried out. Thus from
the moment of mediator or hormone throwing
in the blood to subsequent adaptive reaction
from a few seconds to a few minutes pass.
7.
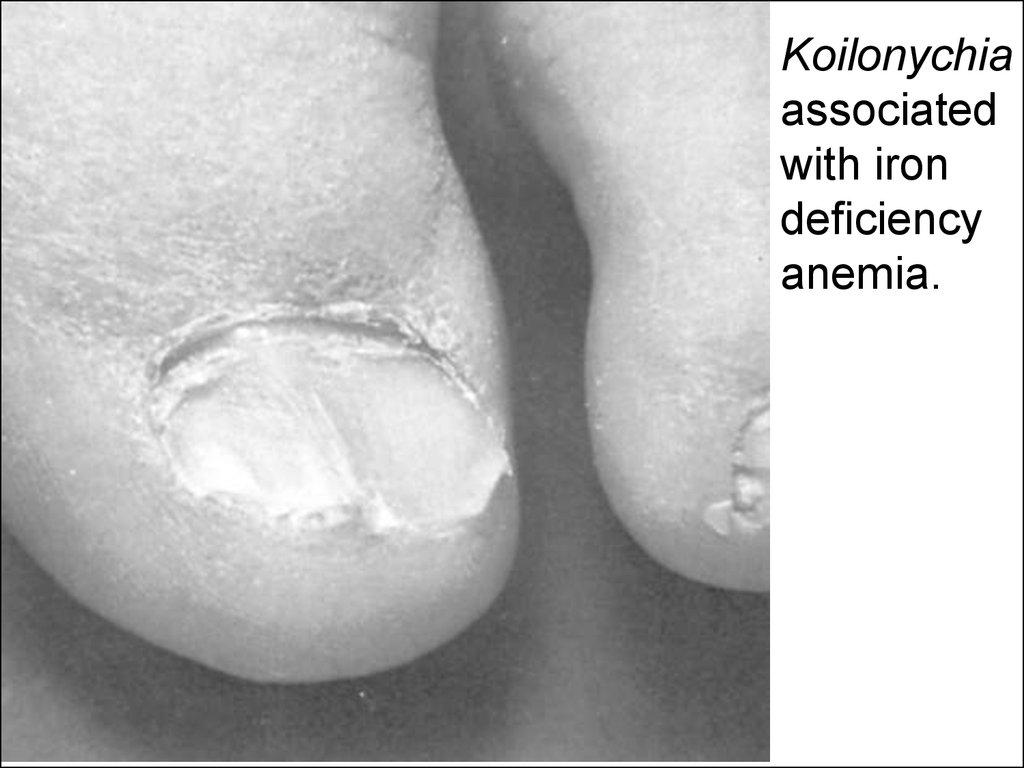
The blood cells also execute the great numberof functions. The long-living (to 100 days) red
cells execute the transport of oxygen. The
leucocytes (to 10 days) participate in the
specific (immunity) and unspecific protective
reactions. Their trophic function is additional.
8.
The leucocytes disintegrating feed intensivelyproliferative tissues by the products
contained in their kernels. The platelet cells
(they live hours, days) participate in
maintenance of blood coagulability. Also they
constantly renew the endothelium of blood
vessels including capillaries and also carry
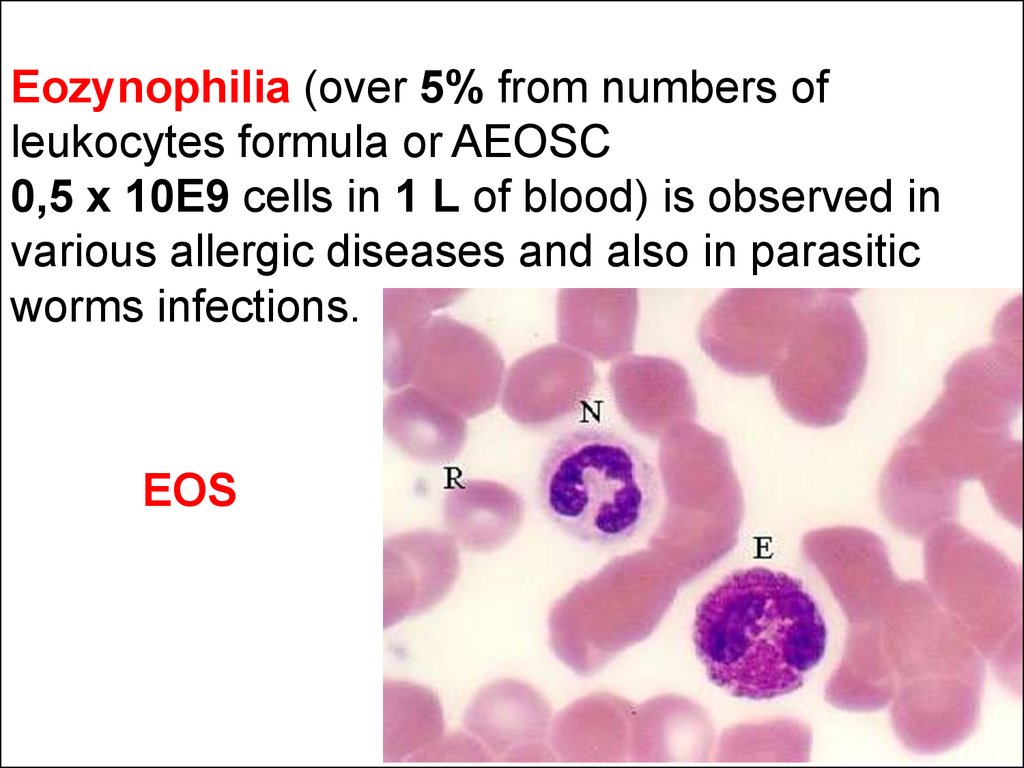
out a trophic function for other tissues.
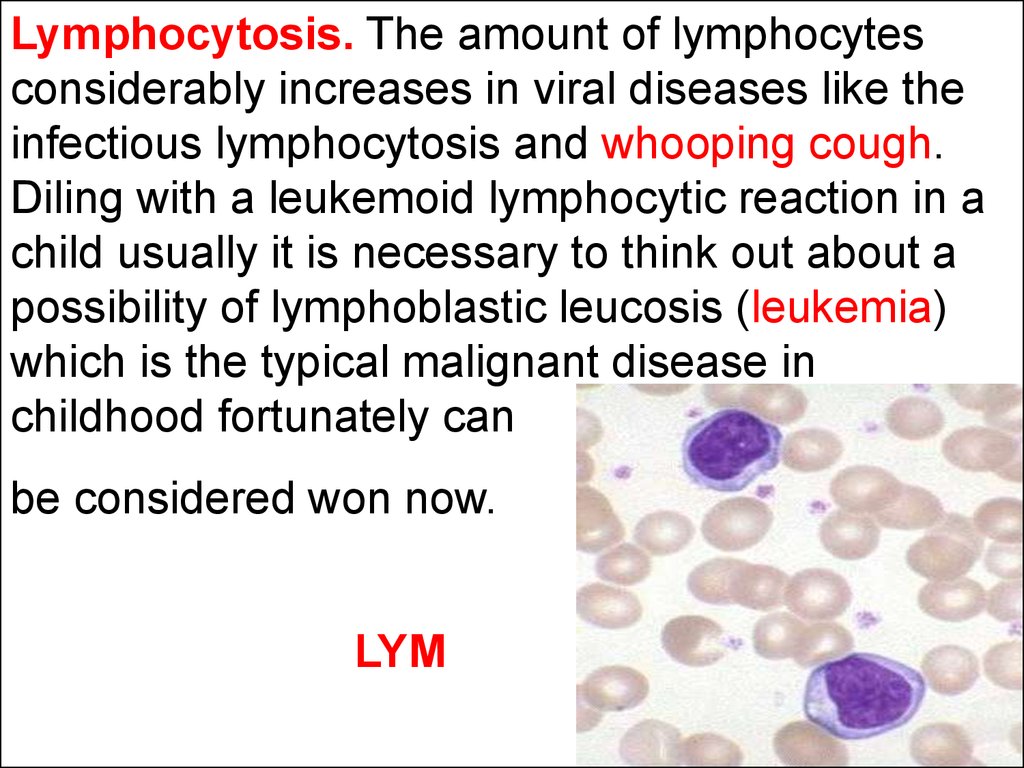
9.
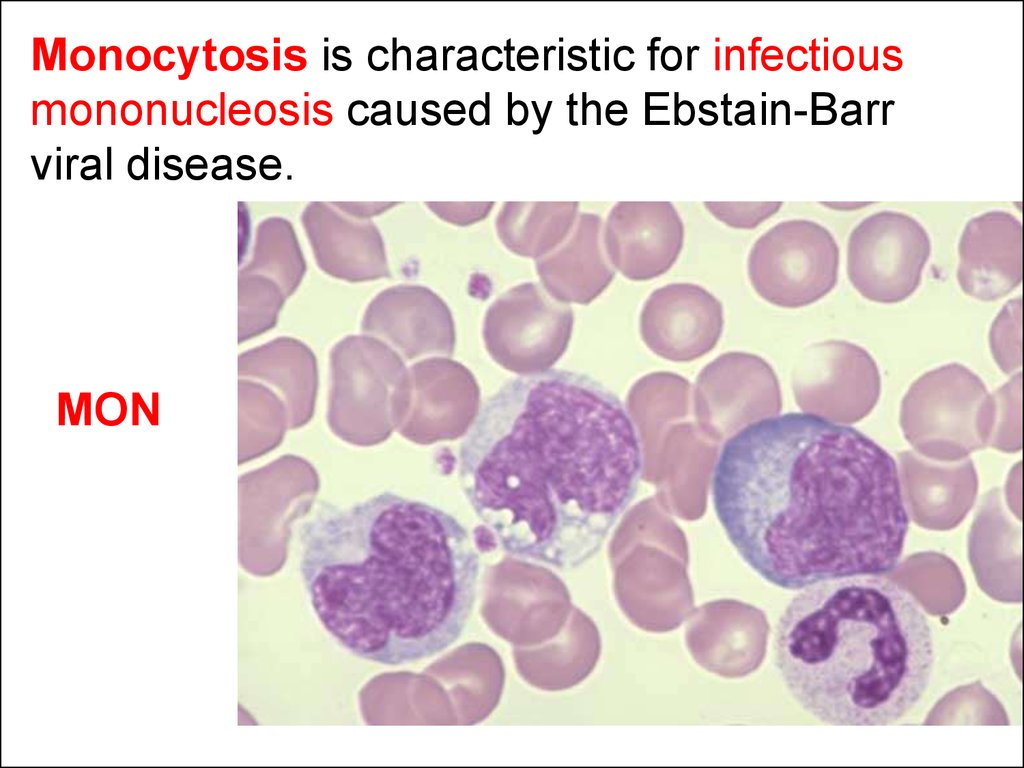
The concept of embryonic hemogenesis.In the period of prenatal life of fetus 3 periods
of hemogenesis are marked off. However its
stages are not strictly differentiated and each
other changes gradually.
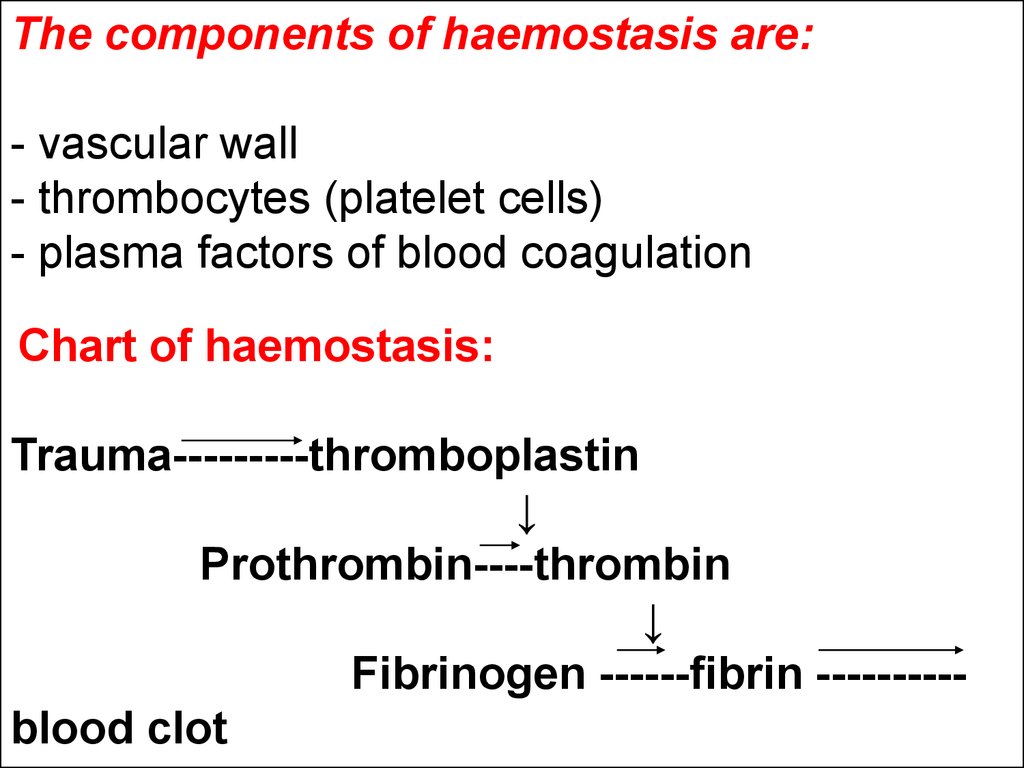
10.
The first stage of hemogenesis is revealed ina 19-th daily aged embryo in the bloody islets
of yolkbag. The initial priextraemmitive blood
cells containing hemoglobin and kernels
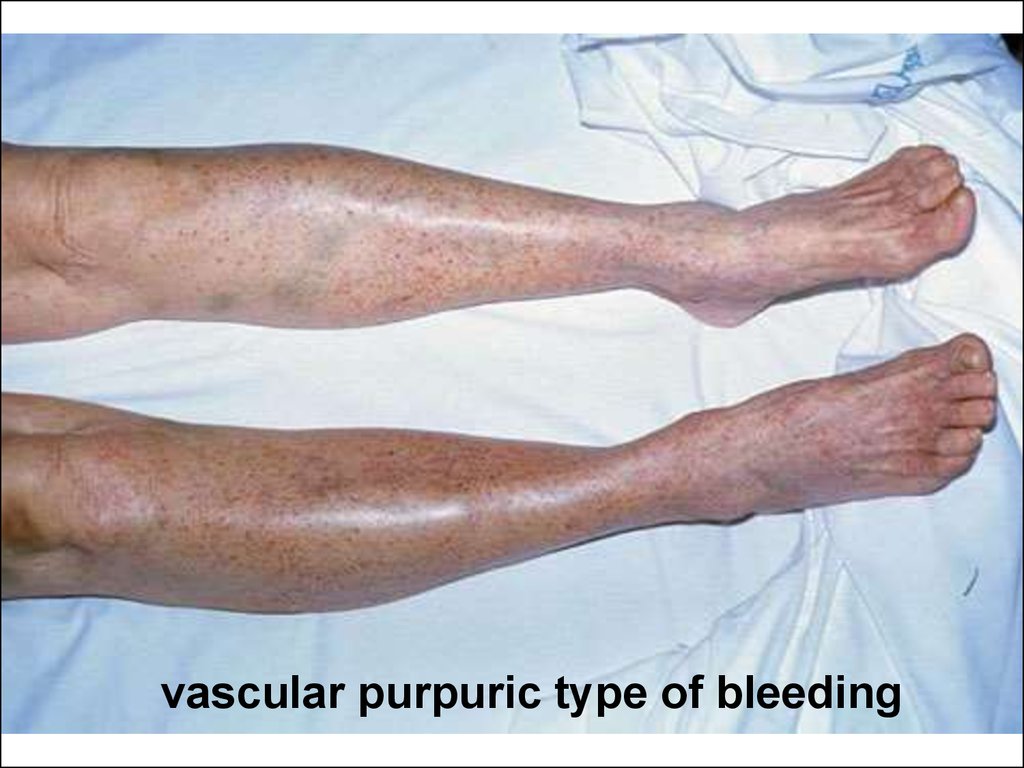
appear. They are megaloblasts. This first brief
period of hemogenesis or erythropoesis
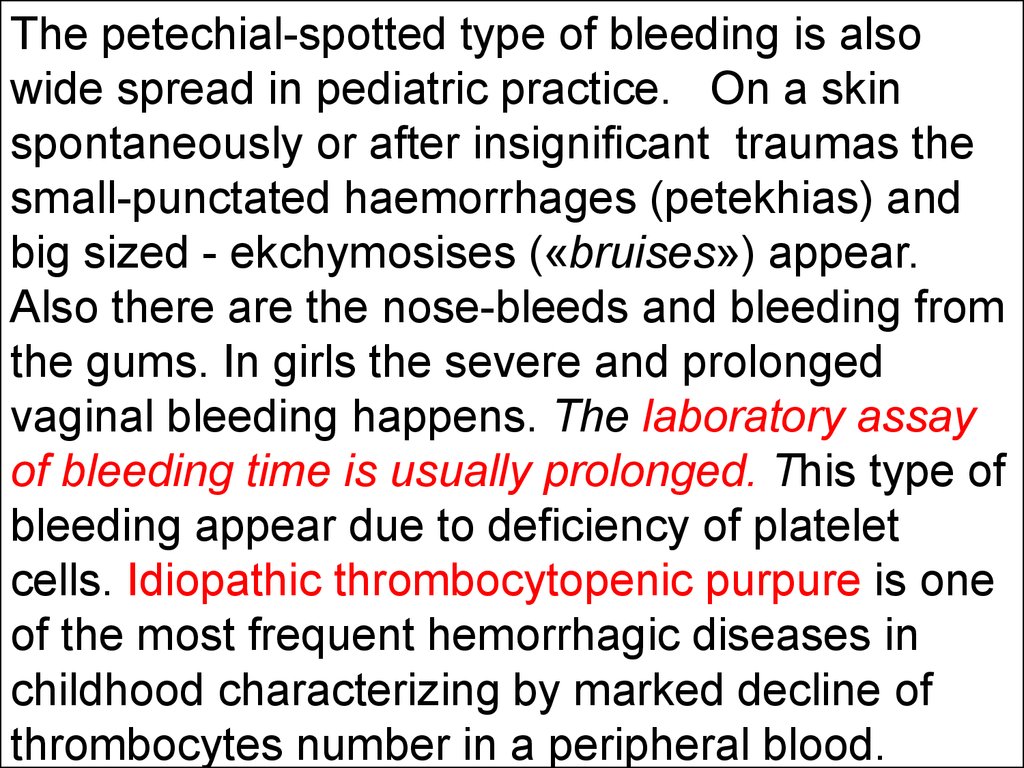
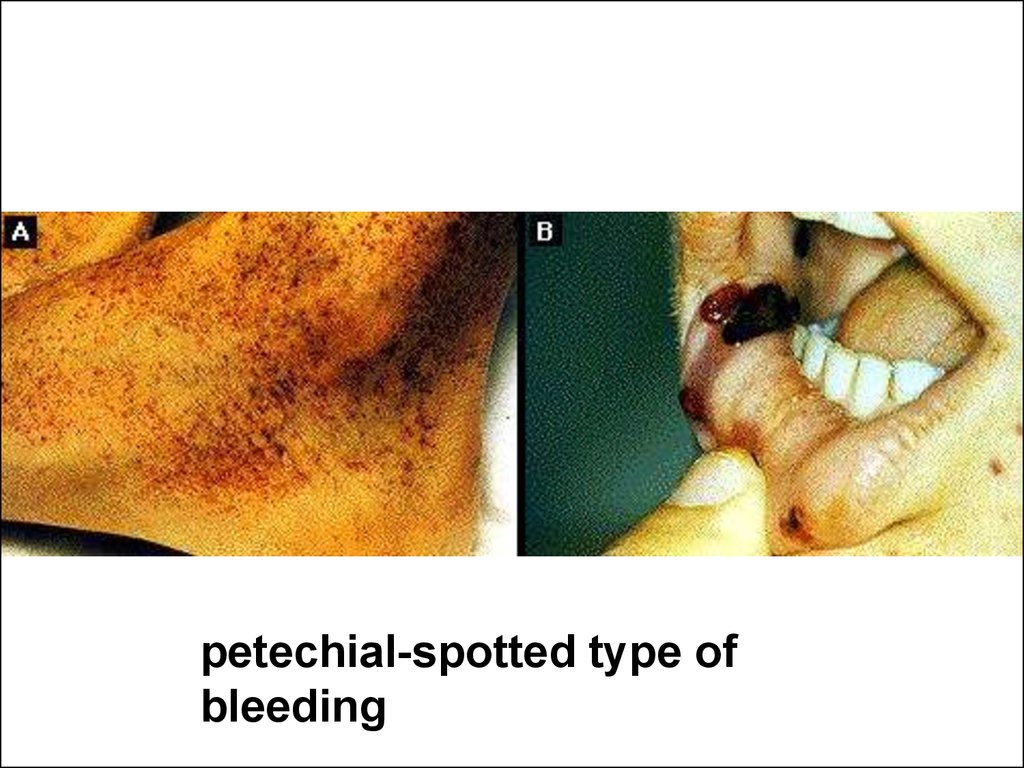
predominantly is called extra- embryonic
hemogenesis.
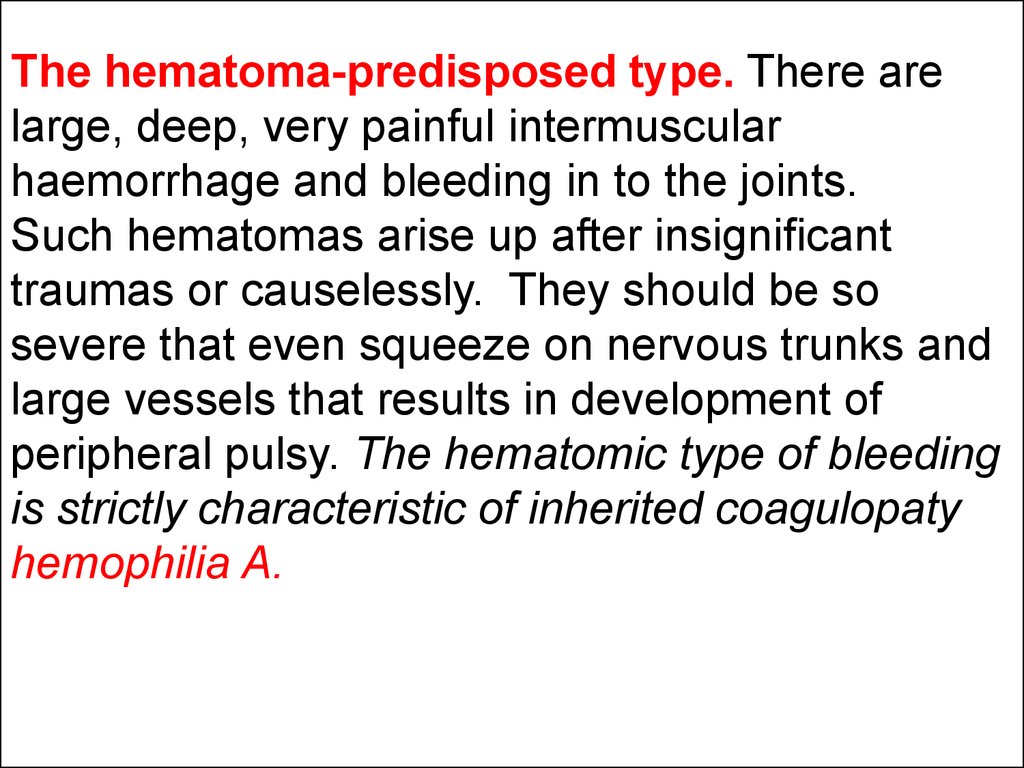
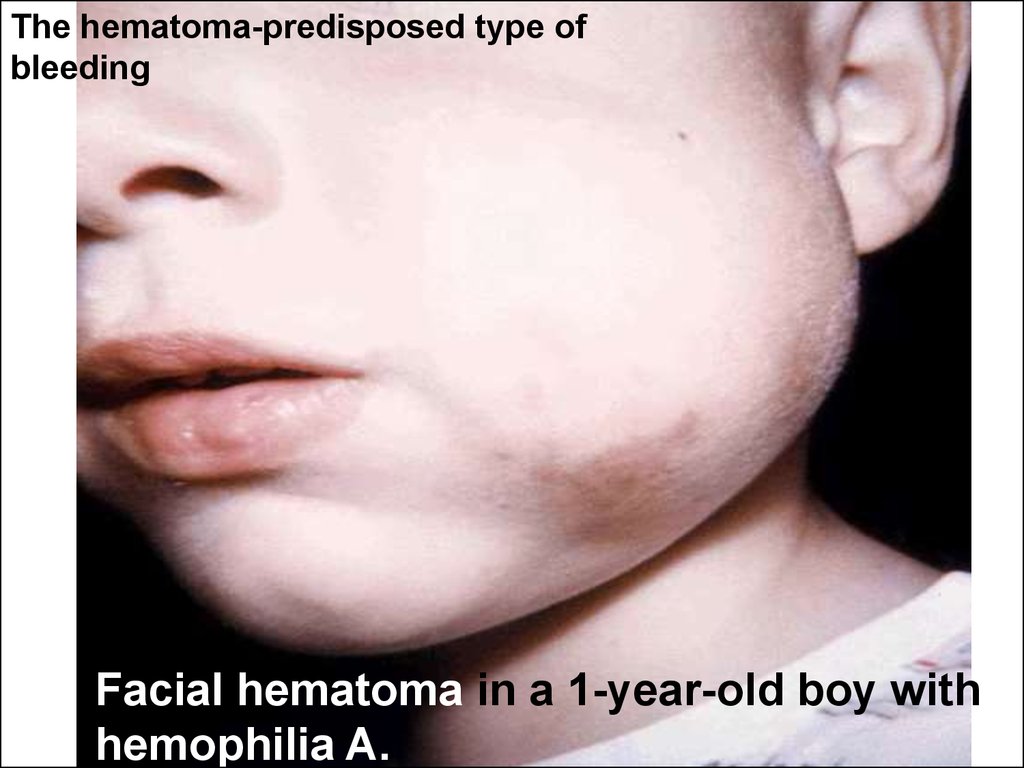
11.
The second (hepatic-splenic) period begins after 6weeks of intrauteral development and achieves its
maximum at the 5-th month of prenatal human life.
At first the hemogenesis takes place in a liver and
erythropoesis is the most expressed among
processes of hemogenesis. The leuko- and
trombocytopoesis are considerably weaker in this
period. The megaloblasts are gradually substituted
by erythroblasts. On the 3—4-th months of prenatal
life the spleen includes into the hemogenesis. Like
the most active organ of hemogenesis the spleen
functions from 5-th till the 7-th month of
ontogenesis. The erythro-, granulocyto- and
megacaryocytopoesis are carried out in it. The
active lymphopoesis arises up in spleen later —
from the end of 7-th month of prenatal development.
12.
The third or bone marrow period ofhemogenesis which gradually becomes
determinative in the production of blood cells
begins on the 4—5-th months of development
in utero.
13.
According to the different periods ofhemogenesis (extraembryonic, hepatic and
bone marrow) there are three different types
of hemoglobin: the embryonic (HbP), fetal
(НbF) and hemoglobin of adult (HbA). The
types of normal hamoglobin differ among
themselves by amino- acid composition and
affinity to oxygen.
14.
The embryonic hemoglobin (HbP) can befound only in the earliest stages of embryo’s
development. On 8 —10-th week of gestation
the fetus has the red blood cells containing
about 90 — 95% НЬF. At the same period the
HbA (5 — 10%) begins to appear. At birth the
amount of fetal hemoglobin varies from 45 to
90%. So the HbF is gradually substituted for
HbA within period of gastation.
15.
In children aged one year the commonhemoglobin level remains about 15% of НЬF
and in a 3 years old toddlers the amount of
HbF should not exceed 2%.
16.
Hemogenesis after the birth.Newborns’ marrow is the general source
of all blood cells production. At this time both
the flat and tubular bones are filled by the
active in regard to hemogenesis red marrow.
However already since the first year of life the
partial transformation of red marrow in most
tubular bones into the fatty (yellow) marrow
begins to be set. In 12—15 years old children
as well as in adult persons the hemogenesis
is saved in bone marrow of only flat bones.
17.
The rapidly exhausted marrow is incident tothe neonatal period of life. After an
unfavorable influences such as infections and
intoxications provoking anemia the children
of early age can have a return to the
embryonal type of hemogenesis. In this
situations in children the so-called
extramedullary centers of hemogenesis in
liver, spleen and even skin can appear.
18.
The features of blood in newborns.The common amount of circulatory blood
in newborns differs and depends on body
mass and maturity, time of umbilical cord
clumbing. In common situations in newborns
the average volume of blood is about 80 ml
per 1 kg of body mass. In adult persons this is
50—60 ml per kg.
19.
The level of hemoglobin (Hb) in the peripheralblood of well newborns is higher than in
infants and adult persons. Always it is 145—
200 g/L and 10 - 55% of it are formed by HbA.
The content of red corpuscles corresponds to
4,5 • 10E12/l — 7 • 10E12/l. The hematocrit (Ht)
which reflects correlation between the volume
of formed elements (mainly red cells) and
plasma after blood centrifugation is about 42 60%. In these condition a color coefficient
(CC) (it uses only in our national practice)
varies from 0,9 to 1,3 reflecting the
erythrocytes` saturation by hemoglobin.
20.
From the first hours after birth thedisintegration of red cells begins. This
process clinically causes the appearance of
physiological jaundice and declines declines
of red cells concentration in blood.
21.
The range of normal variations of generalleucocytes count (WBC) at birth is wide
enough and makes up 10x10E9/L - 30х10E9/L.
In subsequent days and weeks of life the
amount of leucocytes gradually goes down up
to 5 – 15х10E9/L.
22.
The leukocytes formula (or differential countor homograph) in newborns has features. For
the first days after birth the neutrophyles
prevail and arrive at approximately 60% from
the common number of white blood cells.
Thus the white cells formula at the moment of
birth looks like such in adult persons. During
the days after the birth the physiological
prevalence of neutrophyles cells gradually
disappear while the percent number of
lymphocytes grows up. On the 5 — 6th day of
life the percentage of neutrophyles and
lymphocytes in blood evens.
23.
The physiological prevalence of lymphocytesin comparison with other white cells is being
the normal phenomenon in children until the
age of 5 years and is called the physiological
lymphocytosis.
24.
The content of other white blood elementscomparatively less differs from the indexes of
adults’ blood.
The number of platelet cells (PLT) in the
neonatal period is 150 • 10E9/L — 400
10E9/L.
The bleeding time does not differ from
such one within other periods of childhood
and is equal to 2—4 min. In newborns the
bleeding time and the time of blood
coagulation can be prolonged especially in
children with neonatal jaundice.
ESR is low comparing with the results of
adult persons and makes 1 — 3 mm/hour.
25.
The blood in infants.In infants next to the neonatal period the gradual
decline of number of red cells, their sizes,
hematocrit, level of general hemoglobin and content
of hemoglobin in one erythrocyte are the main
features of babies’ peripheral blood composition. In
term born infants there are the lowest values of
them in age of 2-6 months. This important
phenomenon is not characteristic to any other age
period of human life. So, many well-children in this
age have general hemoglobin level less then 110 g/L.
The minimum possible normal level in 2 months is
95 g/L and 5% of normal infants have so low
hemoglobin. In this age the hematocrit makes up 3035% and amount of red cells about 3,5 • 10E12/L.
26.
The average volume of one erythrocyte in childrenin this age is equal to 75 - 100 fl, average content of
hemoglobin in 1 red cell makes up 25-30 picograms
that corresponds to the colour index less than 1
unit. It is the physiological state reminding
hypochromic and microcytic feature of red blood
cells and is observing in many children. It is
conditioned by some disparity between a large
necessity in iron which is needed for erythropoesis
and by rapid growth of child’s body mass, his or her
bloods` volume increasing and difficulties to obtain
enough iron with a milky food. Since the second
year of life the children begin to get the compound
feeding enriched by iron (eggs and meat). Most of
them overcame the deficit of iron and their level of
hemoglobin gradually approach to the adult one.
27.
The amount of leucocytes in healthy infantsvary in limits since 5 • 10E9/L until 15• 10E9/L.
The high number of leucocytes count in wellinfants unusual for adult persons can be
explained by predisposition to digestive
leukocytosis in infants. Besides in the
leukocytes formula of healthy children till the
5 years the physiological lymphotcytosis is
prevailing always.
28.
Second and subsequent years of child’s lifeSince the beginning of the second year of life
until to the pubertal period the morphological
composition of peripheral blood gradually
acquires traits characteristic for adults. In boys
and boy-teens the general hemoglobin makes up
135-165 g/L. In girls it is 115- 145 g/L. The
content of red cells respectively is 4.2-5.5 and
3.7 – 5.0 х 10E12/L. The hematokrit is 36-48%.
The volume of red cells is 80 -100 fl and average
hemoglobin in one erythrocyte 28 – 35
picograms.
29.
In a leukocytic formula in children aged 3-4years there is the tendency to gradual growth
of neutrophyles` percentage and
diminishment of lymphocytes. Between the
fifth and sixth year of life the 2-nd cross of
neutrophyles and lymphocytes amount in
formula happens. In this moment the content
of them in a peripheral blood is evened. The
further increasing of neurophiles` percentage
proceeds after 5 years upto the stable level
and the leukocytical formula becomes such
as in adult persons.
30.
Semyotics of blood changes.The modern blood test includes:
- Research of blood cellular composition.
- Assay of chemical composition of blood
serum.
- Conclusion about coagulative properties of
blood.
- Investigation of
biophysical properties
of blood (ESR).
Modern hematological analyzer
31.
red blood cells32.
The state of red blood cells is characterizedby next clinical and laboratory parameters.
1. The content of common hemoglobin
(Hb) in blood is measured in g/L. Before
measure of common Hb the whole blood
passes procedure of red cells destruction.
The lower acceptable value of normal
hemoglobin in blood below which the anemic
symptoms appear and it is possible to
diagnose anemia in patient is 110 g/L.
33.
There are some exceptions. This value is necessaryto increase up to 135 g/L in newborns because they
usually have higher Hb in comparison with other age
groups of people (see above the physiological
features of newborns) and to decrease up to 95 g/l in
children aged 2-3 months passing nadir of
physiological iron - deficiency.
Average content of hemoglobin in one red
corpuscle can be also measured by the modern
automatic cytometry and this parameter is widely
used in current clinical practice.
34.
If the average content of Hb (Meancorpuscular hemoglobin concentration MCH)
in one red cell is less than 25 pg it is a
symptom of hypochromia. The normal value
is 25-35 pg of Hb in one erythrocyte and this
condition corresponds to normochromia.
When the Hb is more than 35 pg in mean
erythrocyte it corresponds to sign called red
cells hyperchromia.
35.
With high accuracy the hematocryt (Ht, %)reflects a volume which is occupied by red
cells in analyzed sample of blood without
taking into account their individual size (or
mean volume of red cells).
36.
The amount of red cells (RBC) can be alsocalculated. The content of red cells less than
3х10E12/L and hematocrit less than 30%
testify the deficiency of erythrocytes. On the
other hand the red cells amount which
exceeds 6 х 10E12/L and Ht more than 60%
almost for certain must suggest the existence
in patient red cell polycytaemia.
37.
The average volume of one red cell (Meancorpuscular volume – MCV) can be also
measured by the cytometry. Usually it makes
up 80 – 100 ft. This sort of red cells with
normal size is named a normocytes. The
small red cells with a mean volume less than
80 ft are nominated as a microcytes. At
application of common microscopic
technique the pattern of microcytes in blood
is characterized by phenomenon of
anyzocytosis (by the variety of sizes) and
poikylocytosis (by the variety of form). The
red cells having an average volume more than
100 fl are named macrocytes.
38.
There is the extra - systematic value oferythrocytes system called color coefficient.
In proper measure it reflects content of
hemoglobin in one red cell, but without taking
into account its size and/or volume. It is
calculated by the division of hemoglobin
content on the number of red cells. If the
value of coefficient is less than 0.9 un this
condition corresponds in majority cases to
the hypochromia of red cells, 1 (0.9-1.1) to the
normochromia, and more than 1.1 to the
hyperchromia.
39.
Morphologicabnormalities of the
red blood cell.
A.(left above)
Normal.
B
A
B.(right above etc.)
Macrocytes (folic
acid or vitamin B12
deficiency).
C. Hypochromic
microcytes (iron
deficiency).
C
D
D. Target cells (Hb
CC disease).
E.(below)
Schizocytes
(hemolytic-uremic
syndrome).
E
40.
The anemic syndromes.The anemic syndrome is defined as a deficit
of hemoglobin and/or red cells with
characteristic performance of clinical
symptoms.
The common clinical symptoms of anemia are the
pallor of skin and mucous and easy fatiguability,
somnolence in patients. The last symptoms display
systemic hypoxia. The low viscosity of blood due to
deficiency of red cells seldom provokes the anemic
murmur in anemia on a pulmonary artery during the
heart auscultation. Also the anemia can be
accompanied with various skin disorders.
41.
According laboratory data all cases of anemicsyndrome or anemia can be divided into a
several group having individual sings and
features. This groups also differ on their
causative mechanisms. Dialing with
laboratory data, symptoms and anamnesis
in majority situation the well educated
physician can make accurate diagnosis of
anemia.
42.
Iron - deficiency anemia and anemia, causedby deficit of other components necessary for
the Hb synthesis in erythrocyte.
It is necessary to emphasize that in
routine practice the pediatrician very often
has to deal exactly with anemia of this type,
and, especially, with cases linked by irondeficiency state. Without exaggeration the
iron-deficient anemia should be nominated as
the commonest disease in children.
43.
For iron-deficient anemia it is typical of:The general hemoglobin is below than age dependant
normal level;
There is always red cell hypochromia (the average
content of hemoglobin in red cells is below than normal
and/or a colour value is below 0.9);
The erythrocytes usually are mycrocytic (the mean
volume of red cells is less then normal). Very often the
anizocytosis, poikylocytosis should be revealed by
microscopic technology.
The hematockrit is moderate low.
The common content of red cells in blood can be
normal.
Because the cause of this anemia is the deficit of iron
there is a low level of elementary iron in blood serum.
44.
Koilonychiaassociated
with iron
deficiency
anemia.
45.
The symptoms ofpromoted fatigueability in
children can look like as diminished motor activity.
The pallor which can be named as «waxen» is the
most important symptom of iron-deficient anemia. In
girls-teenagers with severe iron-deficiency anemia
on a background of difficult menstruations with
considerable big chronic losses of blood the pallor
can have a greenish tint. This state is called a
juvenile chlorosis. Sometimes the deficit of iron in
children provoke the original symptom of pica
(clorotica). It means a perverted appetite. The
children with pica can eat unsuitable things. The
involuntary desire to eat earth is complicated by
ascariasis and the iron- deficiency in this children
can worse.
46.
The cause of anemia can be a deficit in thechild’s organism of vitamin В12 and folic acid.
The number of red cells and level of hemoglobin
go down below than age dependant normal level.
The most important diagnostic sign of this type
anemia is the macrocytic and hyperchromic
characteristics of red blood cells in this patients.
megaloblastyc pathway
Diphyllobothrium latum (diphylobothriosis).
47.
The largest group of anemias is formed bynormochromic and normocytal cases.
The anemia due to bleeding first of all is
attributed to them. The fact of the occult, internal
or obvious bleeding is the characteristic sign of
this anemic type.
48.
As a result of red cells haemolysis also thenormochromic, normocytal anemias develop. A
jaundice (yellowish discoloration of skin and
mucouses as a result of serum indirect
hyperbilyrubinemia more then
50micromoles/litre) is important incriminative
sign. As a clinical example of this sort of anemia
the neonatal haemolytic disease due to
incompatibility by Rh- and blood group between
expectant mother and her fetus can be done. Also
a lot of hereditary form of hemolytic anemias exist
in pediatric practice.
49.
Finally, the normochromic and normocytalanemias develop as a result of red cells making
lack in the red marrow. They are hypo- and
aplastyc anemias. The anemias of this group
can be innate and acquired. The important
additional symptoms of their diagnostics are: the
decline of reticulocytes (PTC) (young form of red
cells) number – less then 1 % of all red cells in
peripheral blood) and the aplasia of bone marrow
with insufficient content of erythroblasts in it.
50.
The semyotics of red cells number increase1. Typically the abnormally high numbers of red cells
in a peripheral blood is wide spread sign of chronic
hypoxemia, first of all in congenital heart disease.
2. The development of seeming erythrocytosis is
possible in dehydration because of blood concentration.
The blood concentration shows up the increase of other,
so-called concentration values. For example, in
dehydrated patients the serum protein shows up
elevated.
3. The true polycytemia (erythremia) is connected
with neoplasmic (tumors`) proliferation of red cells in
bone marrow.
51.
Leucocytes52.
The characteristics of leukocytes are:1) The value of leucocytes count (WBC) in unit of blood
volume (in liter);
2) The composition of hemograph (or differential count
or leukocytes formula) as a correlation between the
number of leucocytes types shown in absolute count
(AC) in unit of volume (1 liter) or in percents in relation
to all leucocytes.
The leukocytosis and leukopenia appear as
concomitant reactions in various diseases or even
physiological states of human body. The unrestrained
proliferation of leucocytes known as a type of malignant
tumor process – leukemia (Blast cells) or severe
insufficiency of leukocytes production – bone morrow
aplasia are being an independent diseases.
53.
LeukocytosisThe leukocytes count (WBC) is defined as a
content of leucocytes of all types. Except for the
cases considered in connection with the
discussion of newborns and infants in all other
periods it is accepted to consider that normal
white blood cells count is not less than
2.5x10E9/l and above 13.5 х 10E9/l.
54.
The leukocytes count (WBC) exceeding 20 х10E9/L is named hyperleukocytosis or leukemoid
reaction because this condition can remind a
leucosis. In difficult cases the truth leukemia can
be distinguished from leukemoid reaction only on
the basis of the bone marrow investigation. The
benign leukemoid reaction does not show
malignant cell proliferation in opposite to the
leukemia.
55.
Neutrophylic leukocytosis (ANC) and leukemoidreaction of neutrophylic type appear in festeringinflammatory processes. The appearance in the
hemograhp of white cells called band
neutrophyles (the stick-nuclear and other young
forms) facilitates a judgment about microbialinflammatory character of hyperleukocytosis.
Also the toxic graininess of their cytoplasm helps
in it diagnostics.
NEU
56.
Eozynophilia (over 5% from numbers ofleukocytes formula or AEOSC
0,5 х 10E9 cells in 1 L of blood) is observed in
various allergic diseases and also in parasitic
worms infections.
EOS
57.
Lymphocytosis. The amount of lymphocytesconsiderably increases in viral diseases like the
infectious lymphocytosis and whooping cough.
Diling with a leukemoid lymphocytic reaction in a
child usually it is necessary to think out about a
possibility of lymphoblastic leucosis (leukemia)
which is the typical malignant disease in
childhood fortunately can
be considered won now.
LYM
58.
Monocytosis is characteristic for infectiousmononucleosis caused by the Ebstain-Barr
viral disease.
MON
59.
LeukopeniaThe leukopenia (the abnormal decline of leucocytes in
peripheral blood less then 2,5х10^9/L) is observed in such
infections, as typhoid fever, measles and German measles,
viral hepatitis, at hypersplenism. The sensitive lack (less
1,5х10^9/L) of granulocytes number (neutrophyles,
eozynophyles) is named as neutropenia and it can be caused
by influence of radio-active matters, x-rays, use of some
medicinal matters (sulfonamides, antipyretics and many
other), in condition of individual sensitiveness to them.
Almost the complete disappearances of granulocytes defined
as agranulocytosis takes place in some cases and is
represented as an independent disease. Sometimes there is
complete exhaustion of bone marrow — panmyelophtysis.
This patients suffer from the severe recurrent microbial
infections. The lymphopenia less then 0,25х10^9/L is specific
for a few immunodeficiency diseases including for AIDS
(acquired immunodeficiency syndrome).
60.
coagulative properties of blood61.
The adequate to the trauma early bleeding isbeginning right away after the damage of
vessel and it is selected as a normal.
62.
The components of haemostasis are:- vascular wall
- thrombocytes (platelet cells)
- plasma factors of blood coagulation
Chart of haemostasis:
Trauma---------thromboplastin
↓
Prothrombin----thrombin
↓
Fibrinogen ------fibrin ---------blood clot
63.
Easy bleeding (hemorrhagic syndrome).For the hemorrhagic syndrome the
inadequate easy bleeding and also late,
deferred from a moment of trauma bleeding
arising up in a few hours after a trauma or
operation are characteristic. Usual easy and
late bleedings develop in cases if a child
suffers from the disease in which the changes
in system of blood coagulation-haemostasis
are present.
64.
The damage of any component ofhemostasis causes haemorrhagic
syndromes which subdivide on:
- vasopathy (vessel pathology),
- thrombocytopenia, thrombocytopathy,
- coagulopaty.
65.
In accordance of represented factors ofhemorrhagic disease 3 clinical types of
pathologic bleeding are:
1. petechial (vasculitical) purpure,
2. echymosical –spotted purpure,
3. haematomical .
66.
The vascular purpuric type of bleeding shows upas the small-spotted hemorrhagic rash (skin
eruptions) sometimes confluent, with the possible
hearths of necrosis on the skin and on the
mucous membranes of oral cavity,
gastrointestinal tract and in the glomerulas of
kidneys. The bleeding into the gastrointestinal
tract and from kidneys therefore is possible. The
traumas by promoted bleeding are not
accompanied. In children this type of bleeding is
typical of blood vessel inflammation
(anaphylactoid vasculitis), periarteriitis, vitamin C
deficiency (scurvy).
67.
vascular purpuric type of bleeding68.
The petechial-spotted type of bleeding is alsowide spread in pediatric practice. On a skin
spontaneously or after insignificant traumas the
small-punctated haemorrhages (petekhias) and
big sized - ekchymosises («bruises») appear.
Also there are the nose-bleeds and bleeding from
the gums. In girls the severe and prolonged
vaginal bleeding happens. The laboratory assay
of bleeding time is usually prolonged. This type of
bleeding appear due to deficiency of platelet
cells. Idiopathic thrombocytopenic purpure is one
of the most frequent hemorrhagic diseases in
childhood characterizing by marked decline of
thrombocytes number in a peripheral blood.
69.
petechial-spotted type ofbleeding
70.
The hematoma-predisposed type. There arelarge, deep, very painful intermuscular
haemorrhage and bleeding in to the joints.
Such hematomas arise up after insignificant
traumas or causelessly. They should be so
severe that even squeeze on nervous trunks and
large vessels that results in development of
peripheral pulsy. The hematomic type of bleeding
is strictly characteristic of inherited coagulopaty
hemophilia A.
71.
The hematoma-predisposed type ofbleeding
Facial hematoma in a 1-year-old boy with
hemophilia A.
72.
biophysical properties of blood(ESR)
73.
ESR (erythrocytes sedimentation reaction).The spontaneous (not to mix up with
hematocrit) concretion of red cells takes place
because of their greater relative density as
compared to blood plasma. The red cells
spontaneously moving downward oust plasma
upwards. In a norm ascending and descending
influences on red cells are almost balanced,
therefore concretion of these cells is minimum.
The changes of erythrocytes sedimentation
reaction (ESR) are very significant in a different
pathological states especially chronic.
74.
ESR increases due to raise of serumfybrinogen, immunoglobulines, gaptoglobin,
cholesterol concentrations. It elevates also in
alkalosis, anemia.
75.
The normal values of ESR depend on persons`age and sex. In children ESR is lower (1—8
mm/h) than in adult persons. In newborns it is
rarely higher then 2 mm/h. In old men ESR is
below (1—10 mm/h, the average is 5 mm/h) than
in women (from 2 to 15 mm/h, the average is
9mm/h).
The ESR increases in the pathological states
which can be conditioned by inflammation
disease especially hidden such a connective
tissue diseases and malignant tumors. The
important conclusion is seemed quite obvious
that it is necessary to use ESR for chronic
diseases diagnostics and making their prognosis.
76.
At what age in childhood the hematocrit has thelowest normal level?
A.
B.
C.
D.
E.
1 hour
1 week
1 month
3 months
3 years
77.
At what age in childhood the hematocrit has thelowest normal level?
A.
B.
C.
D.
E.
1 hour
1 week
1 month
3 months
3 years
78.
Tiny, flat, round, red or purple spot on skincaused by minute submucosal or intradermal
hemorrhage is:
Ecchymosis
Petechia
Purpura
Macula
Roseola
79.
Tiny, flat, round, red or purple spot on skincaused by minute submucosal or intradermal
hemorrhage is:
Ecchymosis
Petechia
Purpura
Macula
Roseola
80.
The microcytic anemia is associated with:hemolytic disorders
folic acid deficiency
due to bleeding
chronic inflammation
iron deficiency
81.
The microcytic anemia is associated with:hemolytic disorders
folic acid deficiency
due to bleeding
chronic inflammation
iron deficiency
82.
A 8-year-old male is brought to the emergencydepartment with an allergic reaction to a bee
sting. Which leukocytes respond to an
allergic reaction?
monocytes
neutrothils
eosinophils
lymphocytes
basophils
83.
A 8-year-old male is brought to the emergencydepartment with an allergic reaction to a bee
sting. Which leukocytes respond to an
allergic reaction?
monocytes
neutrothils
eosinophils
lymphocytes
basophils
84.
Normal hemoglobin (Hb) values to neonate is:70 to 110 g/l
110 to 130 g/l
140 to 150 g/l
170 to 220 g/l
220 to 240 g/l
85.
Normal hemoglobin (Hb) values to neonate is:70 to 110 g/l
110 to 130 g/l
140 to 150 g/l
170 to 220 g/l
220 to 240 g/l


 medicine
medicine








