Similar presentations:
Anaemia. Definition
1.
ANAEMIADr Ahmed M. Rashed
Lecturer Of Internal Medicine & Nephrology
2.
DefinitionA decrease in haemoglobin or RBCs count in the blood below the
reference level for the age and sex of the individual, which reflects
decreased oxygen carrying capacity.
Anaemia is the most common disorder of the blood.
3.
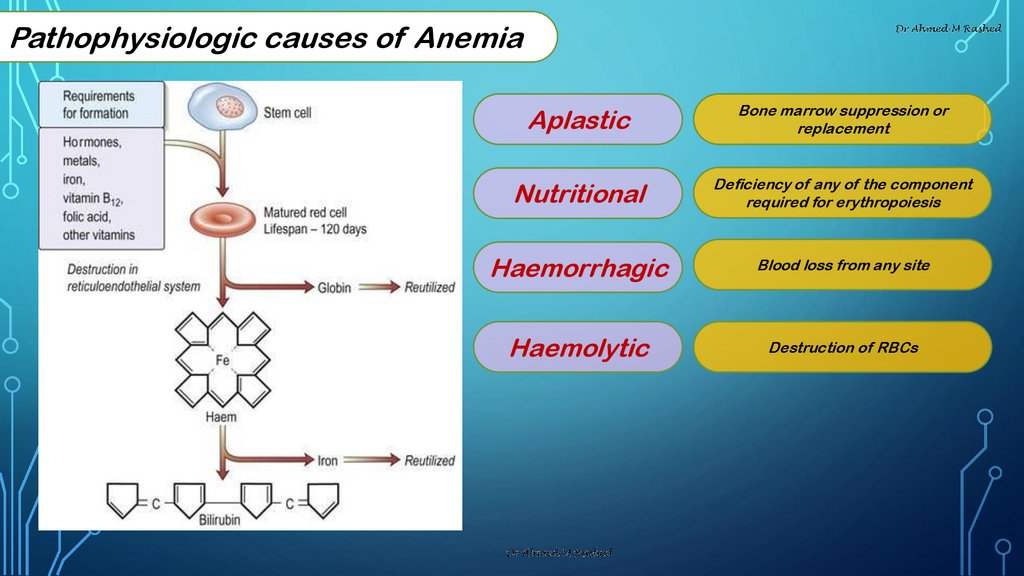
Pathophysiologic causes of AnemiaAplastic
Bone marrow suppression or
replacement
Nutritional
Deficiency of any of the component
required for erythropoiesis
Haemorrhagic
Blood loss from any site
Haemolytic
Destruction of RBCs
4.
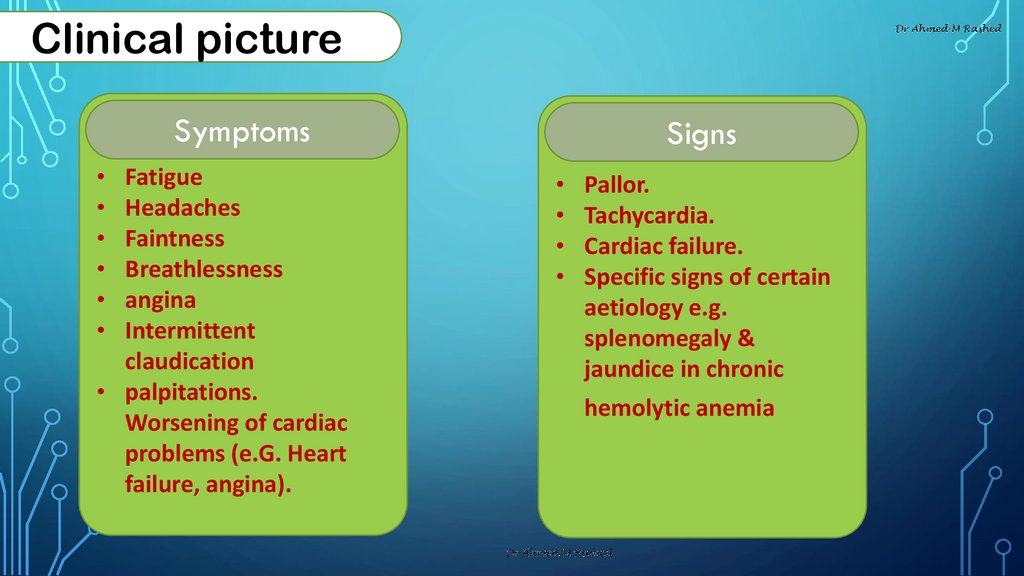
Clinical pictureSymptoms
Fatigue
Headaches
Faintness
Breathlessness
angina
Intermittent
claudication
• palpitations.
Worsening of cardiac
problems (e.G. Heart
failure, angina).
Signs
Pallor.
Tachycardia.
Cardiac failure.
Specific signs of certain
aetiology e.g.
splenomegaly &
jaundice in chronic
hemolytic anemia
5.
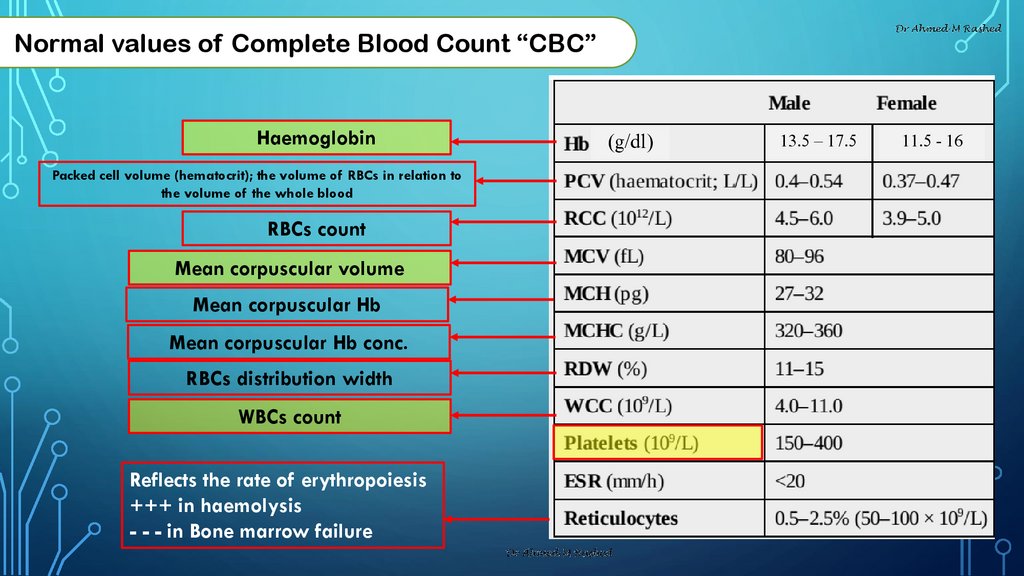
Normal values of Complete Blood Count “CBC”Haemoglobin
Packed cell volume (hematocrit); the volume of RBCs in relation to
the volume of the whole blood
RBCs count
Mean corpuscular volume
Mean corpuscular Hb
Mean corpuscular Hb conc.
RBCs distribution width
WBCs count
Reflects the rate of erythropoiesis
+++ in haemolysis
- - - in Bone marrow failure
(g/dl)
13.5 – 17.5
11.5 - 16
6.
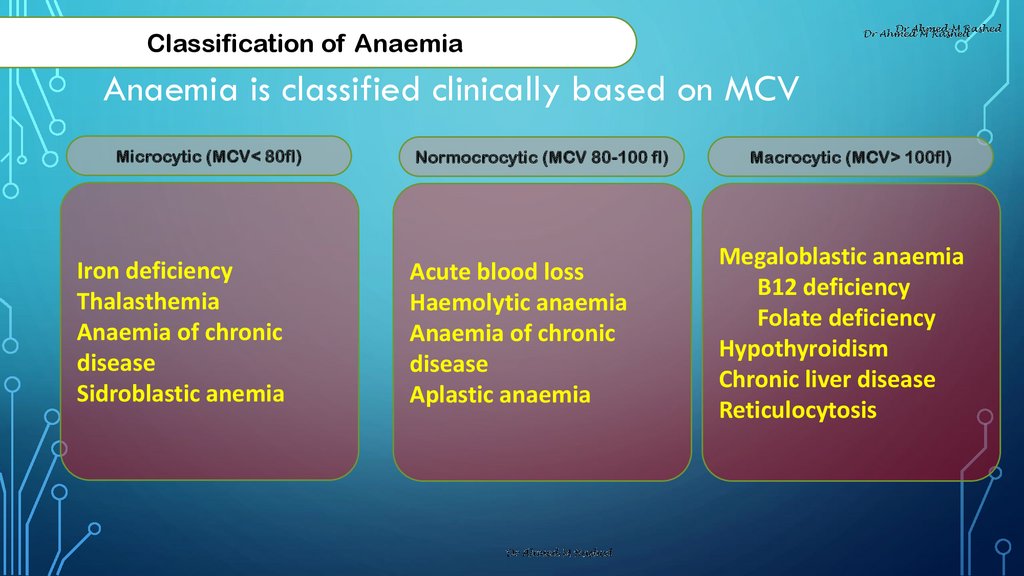
Classification of AnaemiaAnaemia is classified clinically based on MCV
Microcytic (MCV< 80fl)
Iron deficiency
Thalasthemia
Anaemia of chronic
disease
Sidroblastic anemia
Normocrocytic (MCV 80-100 fl)
Acute blood loss
Haemolytic anaemia
Anaemia of chronic
disease
Aplastic anaemia
Macrocytic (MCV> 100fl)
Megaloblastic anaemia
B12 deficiency
Folate deficiency
Hypothyroidism
Chronic liver disease
Reticulocytosis
7.
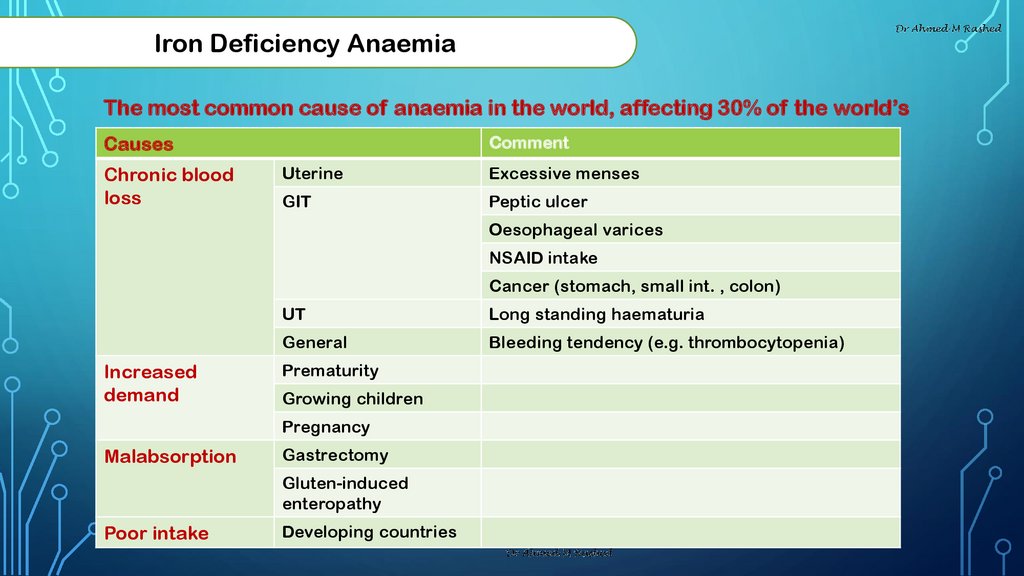
Iron Deficiency AnaemiaThe most common cause of anaemia in the world, affecting 30% of the world’s
population.
Comment
Causes
Chronic blood
loss
Uterine
Excessive menses
GIT
Peptic ulcer
Oesophageal varices
NSAID intake
Cancer (stomach, small int. , colon)
Increased
demand
UT
Long standing haematuria
General
Bleeding tendency (e.g. thrombocytopenia)
Prematurity
Growing children
Pregnancy
Malabsorption
Gastrectomy
Gluten-induced
enteropathy
Poor intake
Developing countries
8.
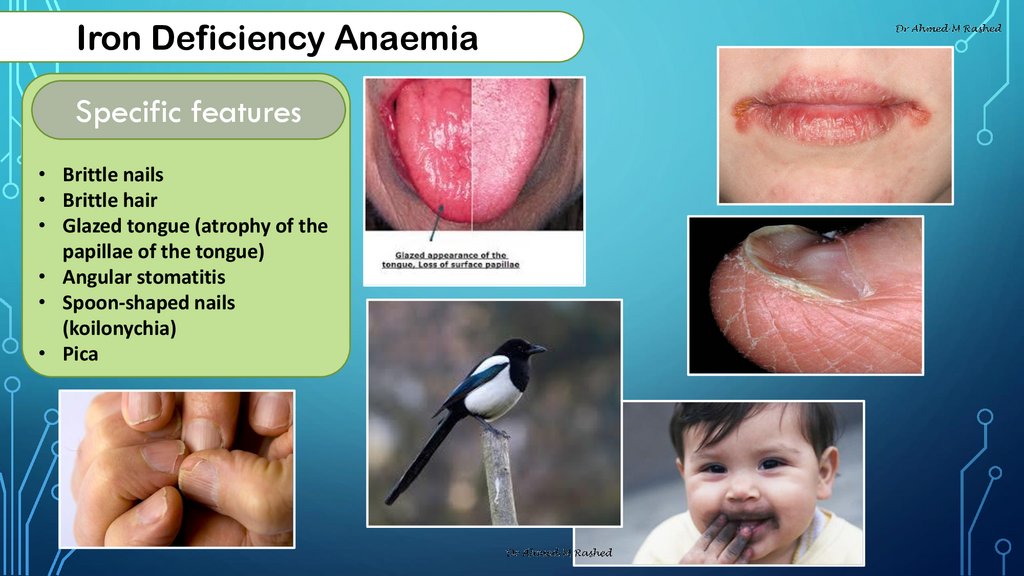
Iron Deficiency AnaemiaSpecific features
• Brittle nails
• Brittle hair
• Glazed tongue (atrophy of the
papillae of the tongue)
• Angular stomatitis
• Spoon-shaped nails
(koilonychia)
• Pica
9.
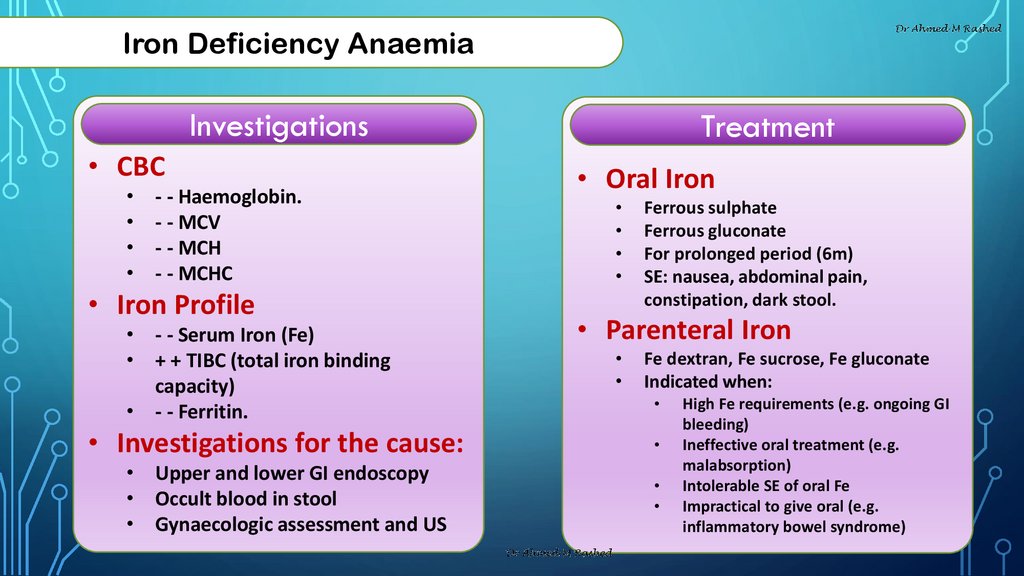
Iron Deficiency AnaemiaInvestigations
• CBC
- - Haemoglobin.
- - MCV
- - MCH
- - MCHC
• Iron Profile
• - - Serum Iron (Fe)
• + + TIBC (total iron binding
capacity)
• - - Ferritin.
• Investigations for the cause:
• Upper and lower GI endoscopy
• Occult blood in stool
• Gynaecologic assessment and US
Treatment
• Oral Iron
Ferrous sulphate
Ferrous gluconate
For prolonged period (6m)
SE: nausea, abdominal pain,
constipation, dark stool.
• Parenteral Iron
Fe dextran, Fe sucrose, Fe gluconate
Indicated when:
High Fe requirements (e.g. ongoing GI
bleeding)
Ineffective oral treatment (e.g.
malabsorption)
Intolerable SE of oral Fe
Impractical to give oral (e.g.
inflammatory bowel syndrome)
10.
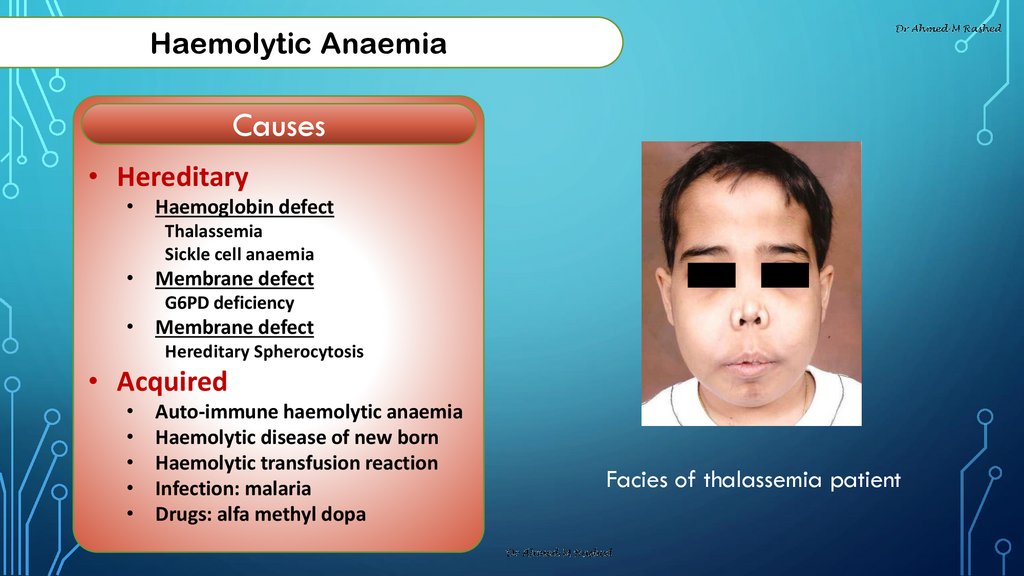
Haemolytic AnaemiaCauses
• Hereditary
• Haemoglobin defect
Thalassemia
Sickle cell anaemia
• Membrane defect
G6PD deficiency
• Membrane defect
Hereditary Spherocytosis
• Acquired
Auto-immune haemolytic anaemia
Haemolytic disease of new born
Haemolytic transfusion reaction
Infection: malaria
Drugs: alfa methyl dopa
Facies of thalassemia patient
11.
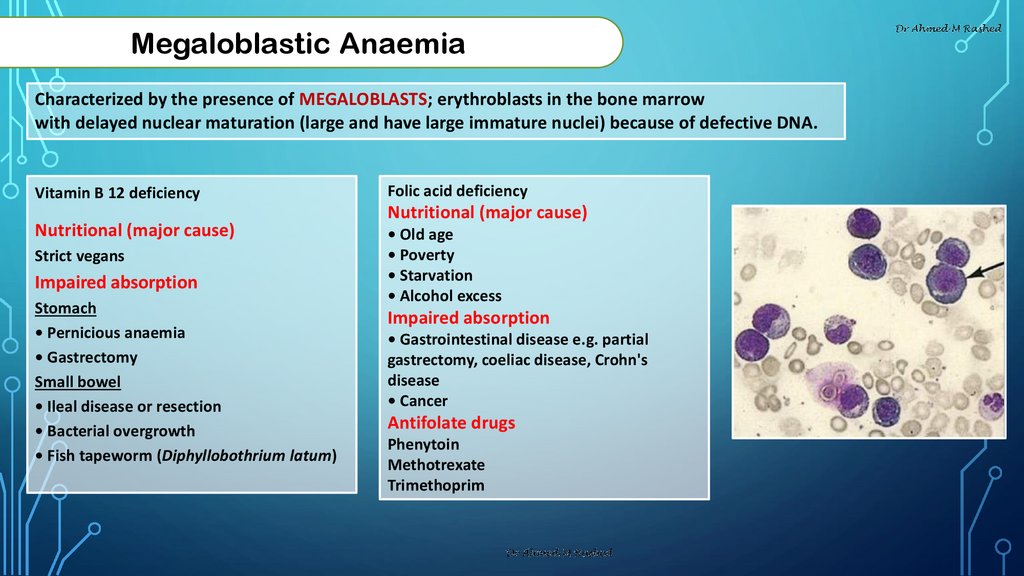
Megaloblastic AnaemiaCharacterized by the presence of MEGALOBLASTS; erythroblasts in the bone marrow
with delayed nuclear maturation (large and have large immature nuclei) because of defective DNA.
Vitamin B 12 deficiency
Nutritional (major cause)
Strict vegans
Impaired absorption
Stomach
• Pernicious anaemia
• Gastrectomy
Small bowel
• Ileal disease or resection
• Bacterial overgrowth
• Fish tapeworm (Diphyllobothrium latum)
Folic acid deficiency
Nutritional (major cause)
• Old age
• Poverty
• Starvation
• Alcohol excess
Impaired absorption
• Gastrointestinal disease e.g. partial
gastrectomy, coeliac disease, Crohn's
disease
• Cancer
Antifolate drugs
Phenytoin
Methotrexate
Trimethoprim
12.
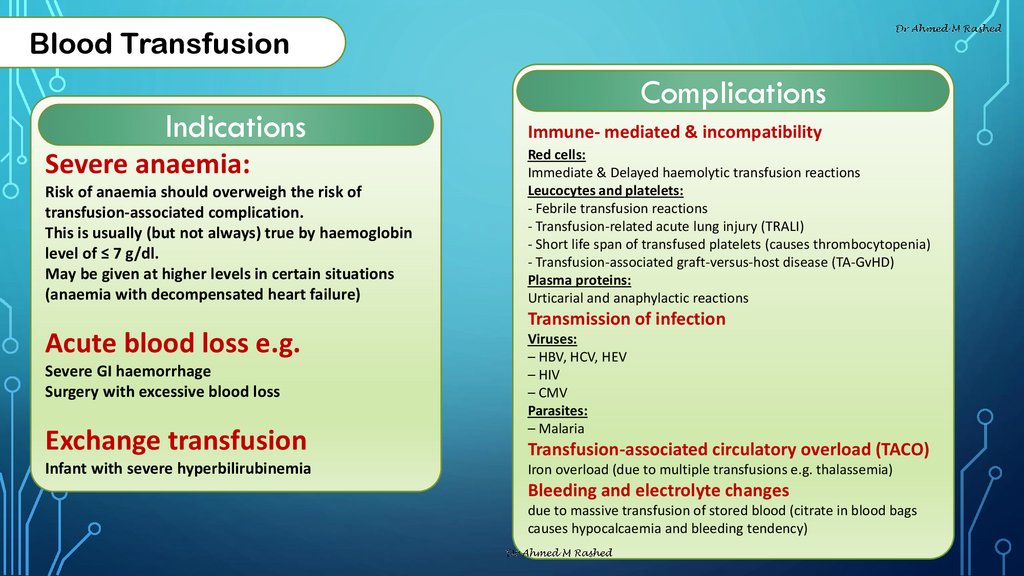
Blood TransfusionIndications
Severe anaemia:
Risk of anaemia should overweigh the risk of
transfusion-associated complication.
This is usually (but not always) true by haemoglobin
level of ≤ 7 g/dl.
May be given at higher levels in certain situations
(anaemia with decompensated heart failure)
Complications
Immune- mediated & incompatibility
Red cells:
Immediate & Delayed haemolytic transfusion reactions
Leucocytes and platelets:
- Febrile transfusion reactions
- Transfusion-related acute lung injury (TRALI)
- Short life span of transfused platelets (causes thrombocytopenia)
- Transfusion-associated graft-versus-host disease (TA-GvHD)
Plasma proteins:
Urticarial and anaphylactic reactions
Transmission of infection
Acute blood loss e.g.
Severe GI haemorrhage
Surgery with excessive blood loss
Exchange transfusion
Infant with severe hyperbilirubinemia
Viruses:
– HBV, HCV, HEV
– HIV
– CMV
Parasites:
– Malaria
Transfusion-associated circulatory overload (TACO)
Iron overload (due to multiple transfusions e.g. thalassemia)
Bleeding and electrolyte changes
due to massive transfusion of stored blood (citrate in blood bags
causes hypocalcaemia and bleeding tendency)
13.
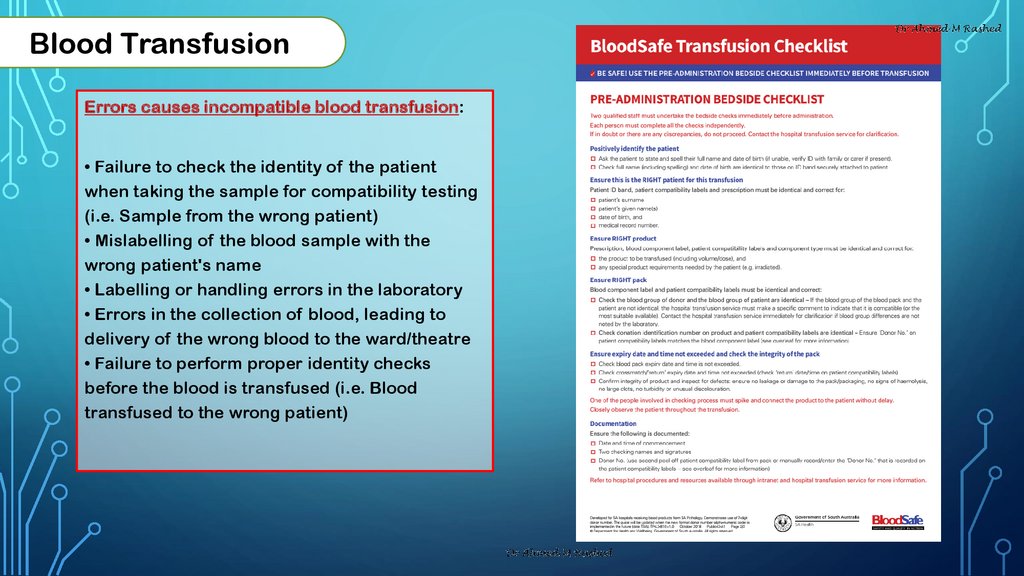
Blood TransfusionErrors causes incompatible blood transfusion:
• Failure to check the identity of the patient
when taking the sample for compatibility testing
(i.e. Sample from the wrong patient)
• Mislabelling of the blood sample with the
wrong patient's name
• Labelling or handling errors in the laboratory
• Errors in the collection of blood, leading to
delivery of the wrong blood to the ward/theatre
• Failure to perform proper identity checks
before the blood is transfused (i.e. Blood
transfused to the wrong patient)

 medicine
medicine