Similar presentations:
Birth trauma in newborns
1. Birth trauma in newborns
Ass.prof. of hospital pediatricdepartment
2.
Factors predisposing the infant to birth injuryinclude
macrosomia,
prematurity,
cephalopelvic disproportion,
dystocia,
prolonged labor,
abnormal presentation,
and certain operative deliveries, particularly
vacuum extraction.
3.
4.
Erythema and AbrasionsErythema and abrasions frequently occur when dystocia
has occurred during labor as a result of cephalopelvic
disproportion or when forceps have been used during
delivery. Injuries caused by dystocia occur over the
presenting part; forceps injury occurs at the site of
application of the instrument.
Forceps injury frequently has a linear configuration
across both sides of the face, outlining the position of
the forceps. The affected areas should be kept clean to
minimize the risk of secondary infection. These lesions
usually resolve spontaneously within several days with
no specific therapy.
5.
PetechiaeOccasionally, petechiae are present
on the head, neck, upper portion of
the chest, and lower portion of the
back at birth after a difficult
delivery; they are observed more
frequently after breech deliveries.
6.
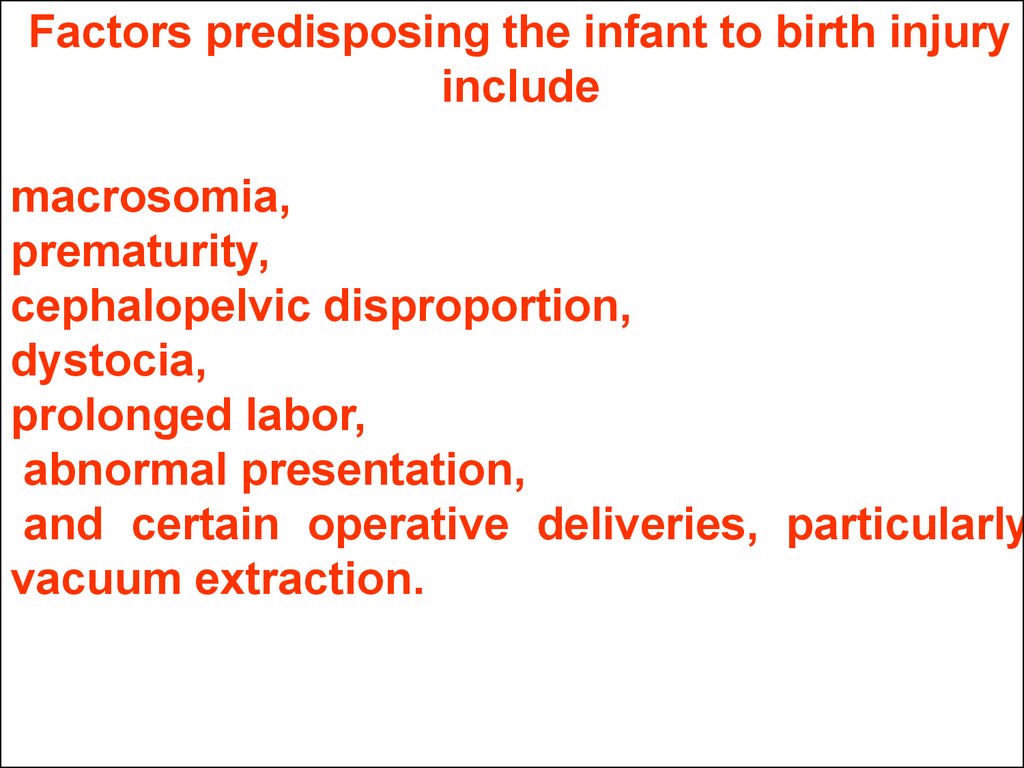
EcchymosesEcchymoses may occur after traumatic or breech
deliveries. The incidence is increased in premature
infants, especially after a rapid labor and poorly
controlled delivery. When extensive, ecchymoses
may reflect blood loss severe enough to cause
anemia and, rarely, shock. The reabsorption of blood
from an ecchymotic area may result in significant
hyperbilirubinemia .
TREATMENT
No local therapy is necessary. The rise in serum
bilirubin that follows severe bruising may be
decreased by the use of phototherapy.
Ecchymoses rarely result in significant anemia.
PROGNOSIS
The ecchymoses usually resolve spontaneously
within 1 week.
7.
Subcutaneous fat necrosis in a 2900-g term infant delivered vaginally; pregnancy,labor, and delivery were completely uncomplicated. Note nodular lesion located on
right buttock and surrounded by erythema (darkened area).
8.
9.
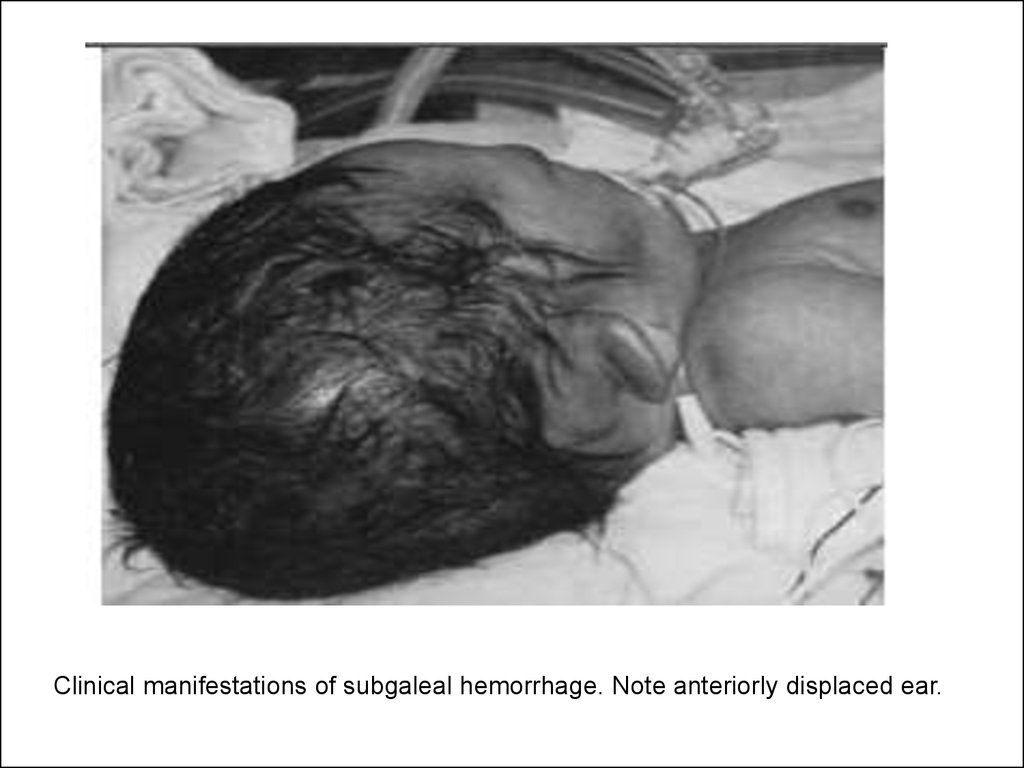
Clinical manifestations of subgaleal hemorrhage. Note anteriorly displaced ear.10.
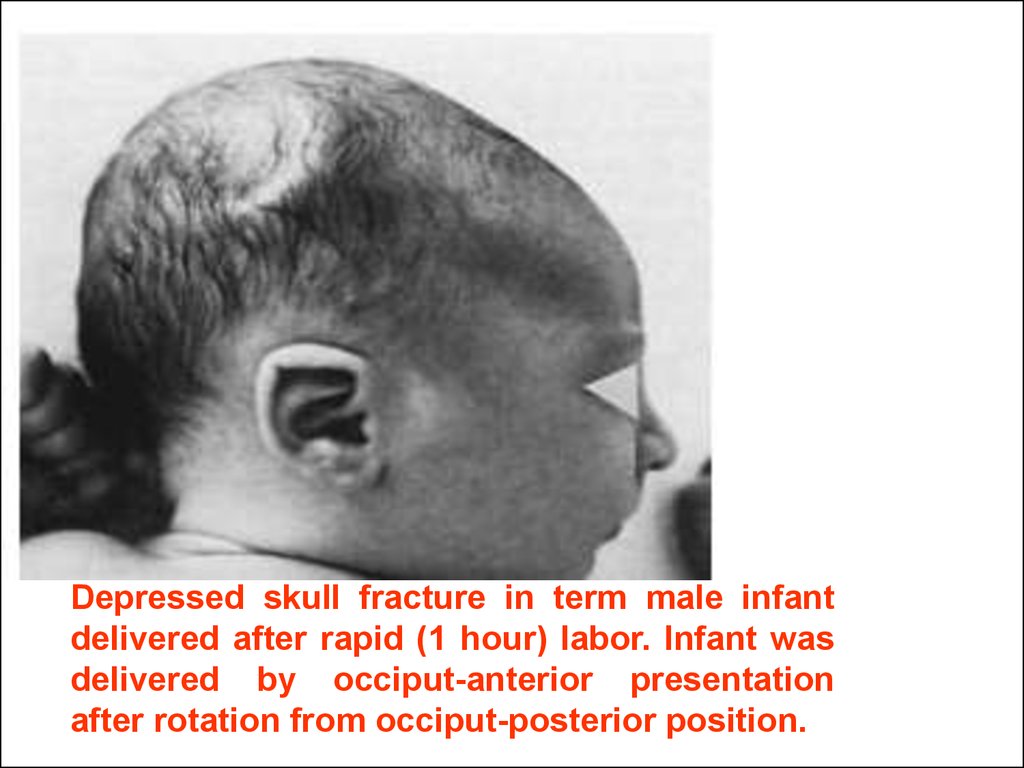
Depressed skull fracture in term male infantdelivered after rapid (1 hour) labor. Infant was
delivered by occiput-anterior presentation
after rotation from occiput-posterior position.
11.
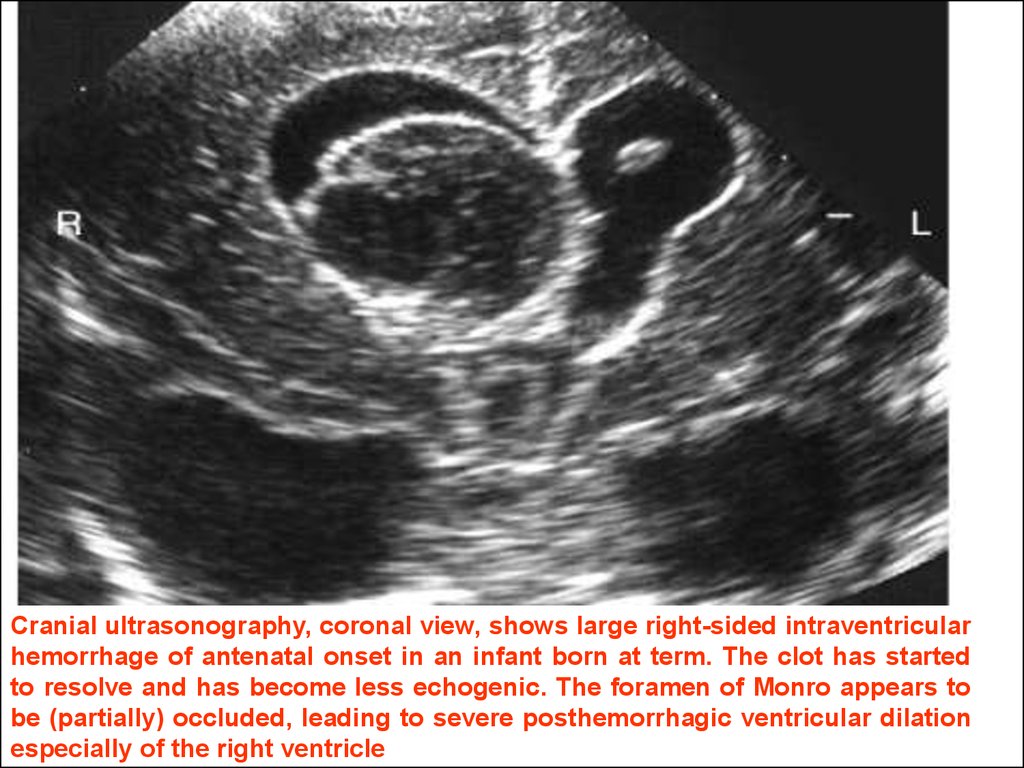
Cranial ultrasonography, coronal view, shows large right-sided intraventricularhemorrhage of antenatal onset in an infant born at term. The clot has started
to resolve and has become less echogenic. The foramen of Monro appears to
be (partially) occluded, leading to severe posthemorrhagic ventricular dilation
especially of the right ventricle
12.
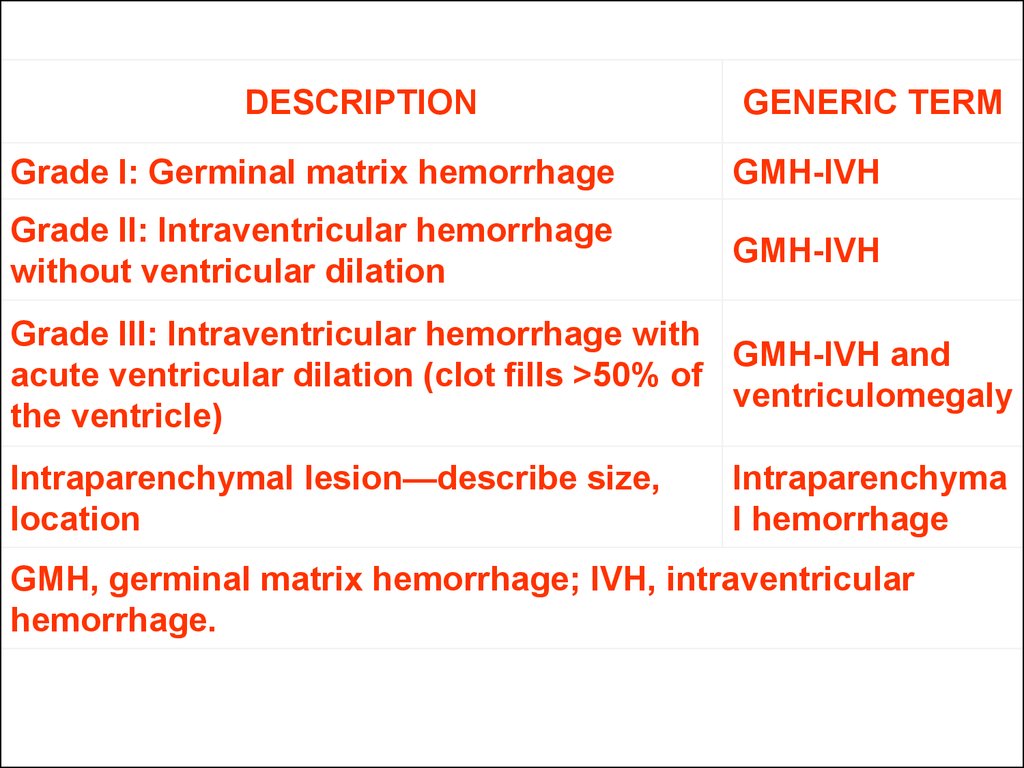
DESCRIPTIONGENERIC TERM
Grade I: Germinal matrix hemorrhage
GMH-IVH
Grade II: Intraventricular hemorrhage
without ventricular dilation
GMH-IVH
Grade III: Intraventricular hemorrhage with
GMH-IVH and
acute ventricular dilation (clot fills >50% of
ventriculomegaly
the ventricle)
Intraparenchymal lesion—describe size,
location
Intraparenchyma
l hemorrhage
GMH, germinal matrix hemorrhage; IVH, intraventricular
hemorrhage.
13.
Parenchymal HemorrhageThe most severe type of hemorrhage involves the
parenchyma. This type of lesion occurs in approximately 3%
to 15% of all hemorrhages.
Direct extension into the parenchyma from pressure of blood
in the ventricle is now considered unlikely. Some still take the
view that all parenchymal hemorrhages are originally
ischemic in origin, with any bleeding being a secondary
complication.
However, most agree that a unilateral parenchymal lesion
accompanying GMH-IVH is most often caused by the
presence of the GMH leading to impaired venous drainage
and venous infarction.
14.
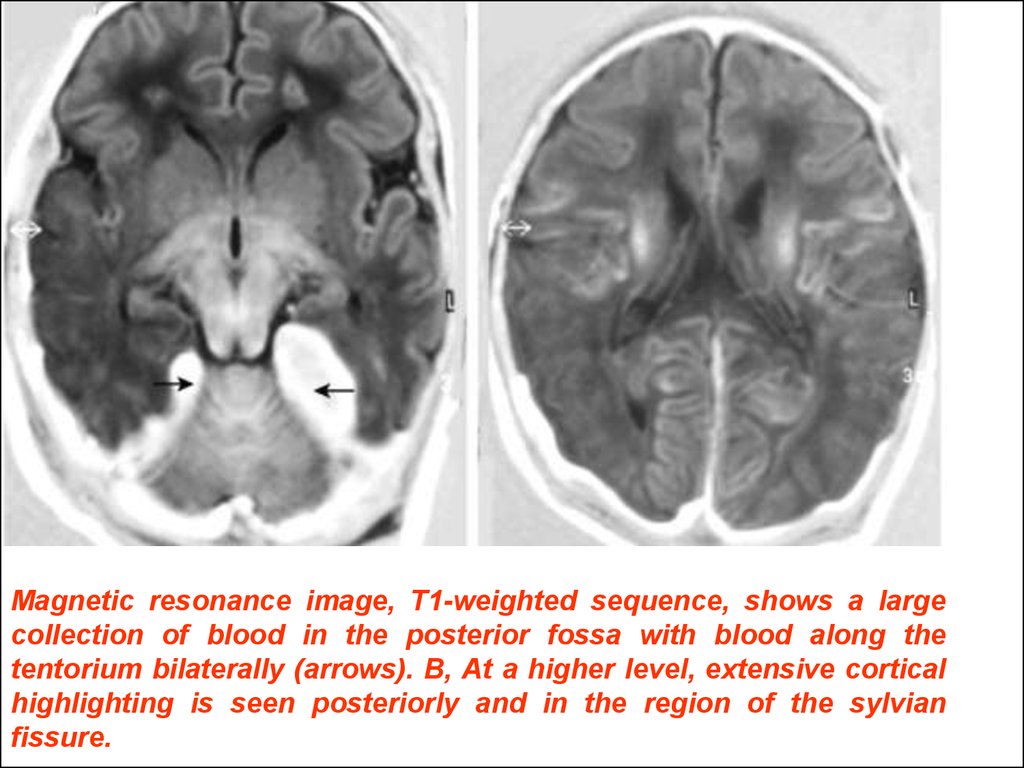
Magnetic resonance image, T1-weighted sequence, shows a largecollection of blood in the posterior fossa with blood along the
tentorium bilaterally (arrows). B, At a higher level, extensive cortical
highlighting is seen posteriorly and in the region of the sylvian
fissure.
15.
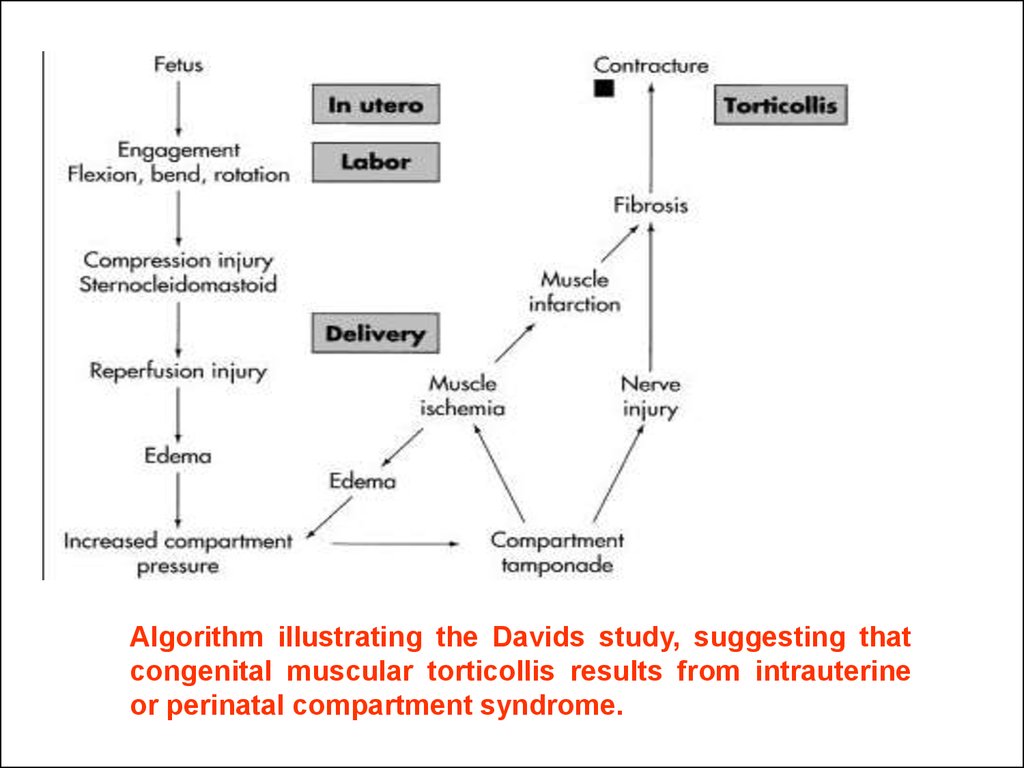
Algorithm illustrating the Davids study, suggesting thatcongenital muscular torticollis results from intrauterine
or perinatal compartment syndrome.

 medicine
medicine