Similar presentations:
Health Care
1. Health Care
HEALTH CAREBoza Chapter 10
2. Our Goals
■ To review the history of health disparities.■ To address why the United States spends more money than any other country in the
world for healthcare both in total dollars and by percentage of gross national
product with the latest technology to treat diseases with the best-trained physicians;
yet, we have a relatively high infant mortality rate and rank low in life expectancy in
comparison to other industrialized nations.
■ To additionally address issues with class, race, and gender inequalities of health
and healthcare delivery.
■ To distinguish demographics for R/E minorities.
3. History of Health Disparities
■ During slavery medical care was brutal and ineffective for most people.■ Slaves suffered innumerable kinds of maltreatment and misdiagnosis.
■ One account is that of John Brown.
– Brown wrote in his memoir (after his escape) of the treatment he suffered at
the hands of doctors.
– Page 252
4. History of Health Disparities
■ Live and Dead Bodies– In 1989 (GA) construction
workers found nearly 10,000
human bones and skulls
beneath what was once the
Medical College of GA.
– In the 19c, Drs. had ordered
porter to remove the bodies for
medical dissection.
– 75% were African American
■ Tuskegee Syphilis Experiment
– 1932
– PHS and the TI in AL recruited
400 poor black men for a
study on long-term syphilis.
– Did not diagnosis them
w/syphilis but rather “bad
blood.”
– Drs. wanted to know if left
untreated its effects on the
body.
5. History of Health Disparities
■ Involuntary Sterilization– In the early to mid-20c,
hundreds of black girls and
women were subjected to
involuntary sterilization.
– Done without permission
– Became known as the
‘Mississippi Appendectomy’
– P. 255
■ Experimental Radiation
– 1945
– Ebb Cade
– No consent given
– Eventually escaped the
hospital and ill treatment
– Later died of heart disease
6. History of Health Disparities
■ In 1953, the US Department ofDefense adopted the Nuremberg
Code.
■ Under this policy, research subjects
have to be provided with all
information about that nature and
duration of the experiment.
■ Participation was also required to
be voluntary.
■ The disparities are clear but how do
we explain them?
■ Is it racial discrimination?
■ Is it a genetic argument?
■ Could it be institutional racism?
■ Answers are harder to find than
identifying the problem.
7. Rising Healthcare Costs
■In 2010, Americans spent $2.6 trillion on
healthcare.
■
The United States spent more on
healthcare than any other advanced
modern nation.
c. Many physicians practice defensive
medicine (tests and procedures doctors
perform to protect themselves from
lawsuits).
■
■
■
There are several reasons why healthcare
in the United States is so expensive.
d. Malpractice lawsuits account for about
4 percent of total healthcare costs.
■
■
a. Profit drives the U.S. system.
e. Science keeps inventing costly new
tests and treatments.
■
b. The system is inefficient.
■
f. There is a shortage of primary-care
physicians and an overuse of specialists.
■
g. The highest part of healthcare bills is
prescription drugs—$307.4 billion in 2010
8. Does the High Cost of Healthcare Translate Into Good Health Consequences?
■ The United States spends more, butAmericans do not fare as well as
those in Western Europe,
Scandinavia, Canada, and Japan.
■ The United States ranks fortyseventy in average life expectancy.
■ The United States is the worst of
developed countries on “avoidable
mortality.”
■ Life span vs. life expectancy
■ Life span refers to the maximum
length of life of a species; for
humans, the longest that a human
has lived. (122)
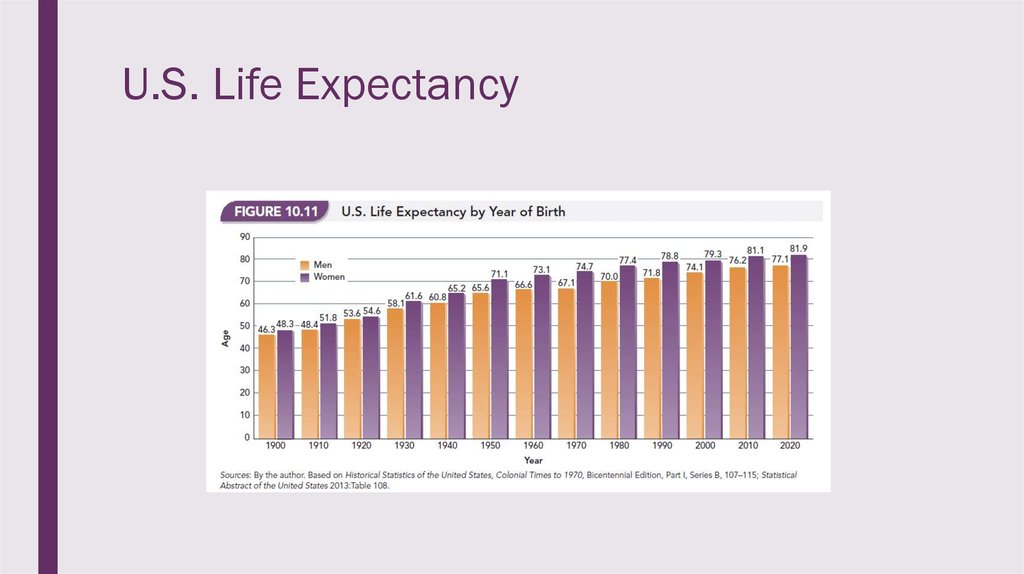
■ Life expectancy has changed since
the last century and Americans can
expect to live into their 70s and
80s.
9. U.S. Life Expectancy
10. Life Expectancy Global Picture
11. Who is uninsured?
12. Updating the Uninsured
■ In 2016, 27 million Americans remained uninsured.■ 5.1% were under the age of 18.
■ Latinos and Native Americans (2014) were the most likely uninsured r/e groups.
■ 13% of African Americans were uninsured compared to 10% of Asian Americans,
and 9% of Whites.
■ The largest age bracket for all groups uninsured is 19-34, followed closely by 35-54.
■ Family structure also influences coverage. For all groups, except African Americans
and Whites, families with children had more coverage than single adults.
13. Unequal Access
■ A key question in examining the structure of healthcare delivery is who benefits andwho suffers from the way the system is organized?
■ Three structures of inequity (class, race, and gender) are key determinants of health
(i.e., the distribution of health and disease) and healthcare delivery (i.e., the
distribution of treatment).
■ Social class (money) plays a large part in what access individuals have.
■ How people live, get sick, and die depends a great deal on their social class.
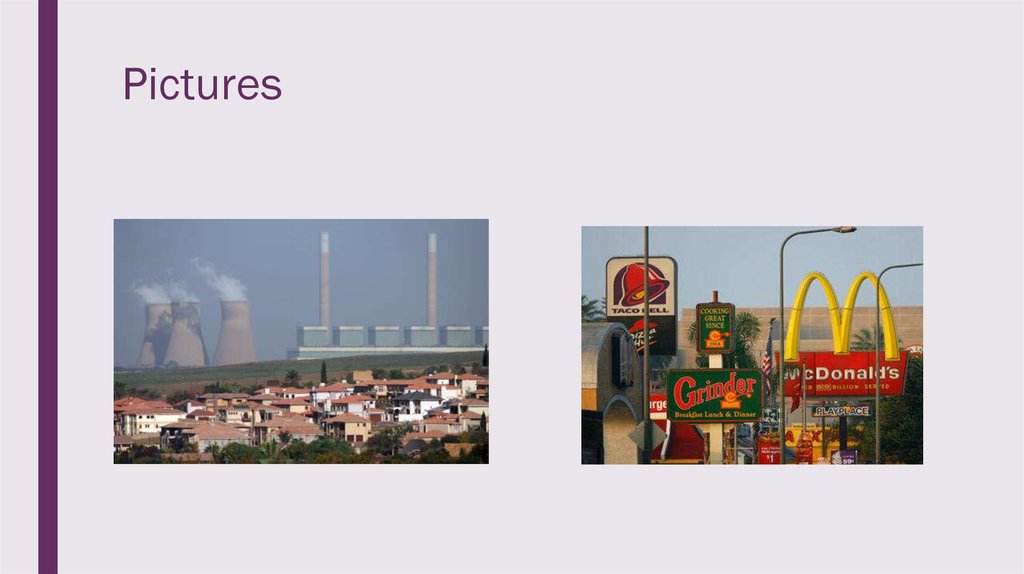
■ The physical health of poor people is more likely to be impaired than the affluent
because of differences in diet, lifestyle, sanitation, shelter, exposure to
environmental hazards, work conditions, and medical treatments and lifestyle.
14. Unequal Access
■ An advantage of the affluent is access to health-promoting and health-protectingresources, and to medical services typically paid for with health insurance.
■ The uninsured cannot afford the costs for physicians, dentists, and hospitals, so
they often do without.
■ Poor pregnant women often do not receive prenatal or postnatal health care,
resulting in a high maternal death rate and a relatively high infant mortality rate.
■ Ironically, when the uninsured go to a doctor, they pay more for services than
insured patients.
15. Unequal Access
■ Location matters too!– States with the lowest premiums are Arizona, New Mexico, Kentucky, DoC, and
Maryland.
– States with the highest premiums are NC, WY, NY, AK, and VT.
– States with the most doctors per capita are DoC, MA, RI, NY, and CT.
– States with the least doctors per capita are Utah, MS, Nevada, WY, and Idaho.
16. Unequal Access
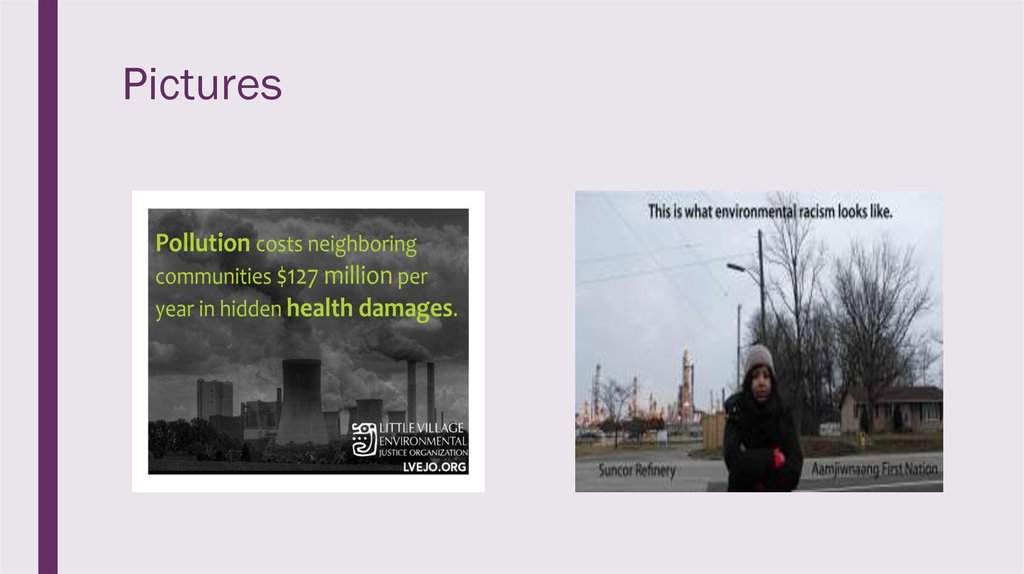
■ Environmental racism can’t be leftout either.
■ Subsequently, location and disease
are related.
■ Page 266
■ States with lowest rates of cancer
are NM, Nevada, and AZ. (Highest
are NY, PA, and LA.)
■ Holt Family p. 268
■ States with the lowest rates of heart
disease are HI, MN, and CO.
(Highest are LA, AL, and MS.)
17. Pictures
18. Pictures
19. Pictures
20. Pictures
21. Unequal Access: The Poor
■ When the poor do go to physicians they are more likely to receive inferior servicesbecause of several factors:
■ The poor are often served by understaffed clinics and hospitals.
■ There are disproportionately fewer physicians in poor urban and rural areas.
■ The belief that the poor are accountable for their health deficiencies blames the
victim and ignores the realities of social class.
■ Culture of Poverty (theory)
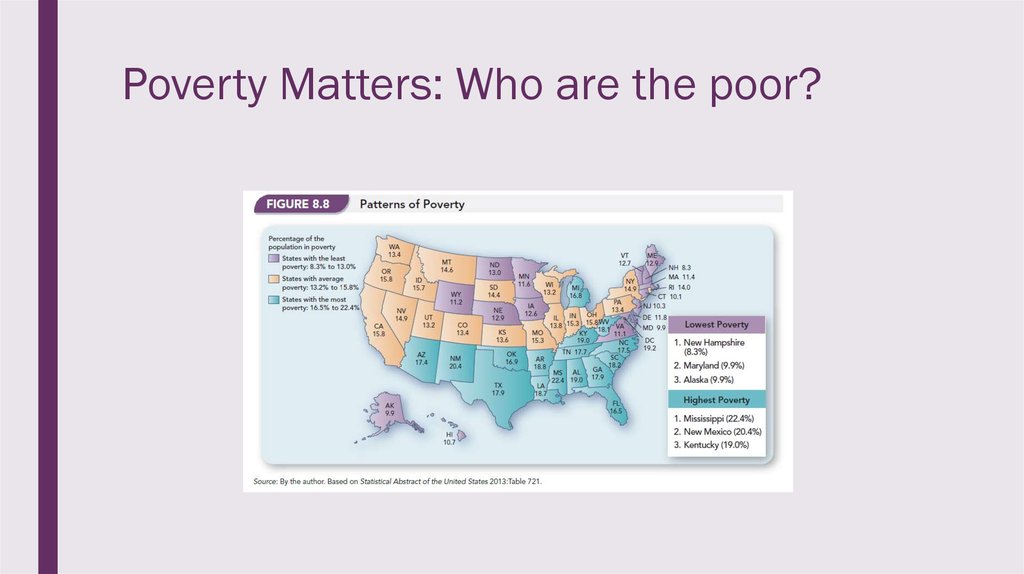
22. Poverty Matters: Who are the poor?
23. Poverty Matters: Who are the poor?
■Race-ethnicity is a major factor; Of these groups these are the percentages in poverty:
■
11% Whites (of all U.S. poor 44%)
■
12% Asian Americans (4%)
■
23% Latinos (25%)
■
27% African Americans (27%)
■
29% Native Americans (2%)
■
Education: Only 3% of people who finish college end up in poverty.
■
Gender: Sex of the head of household --- the feminization of poverty. Single-parent families headed by
women have a higher propensity of being poor.
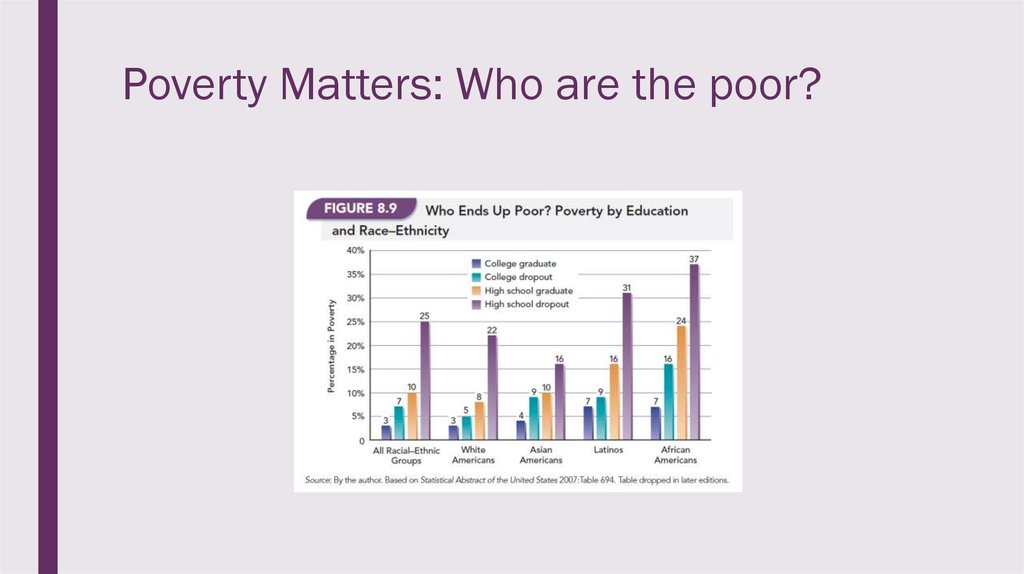
24. Poverty Matters: Who are the poor?
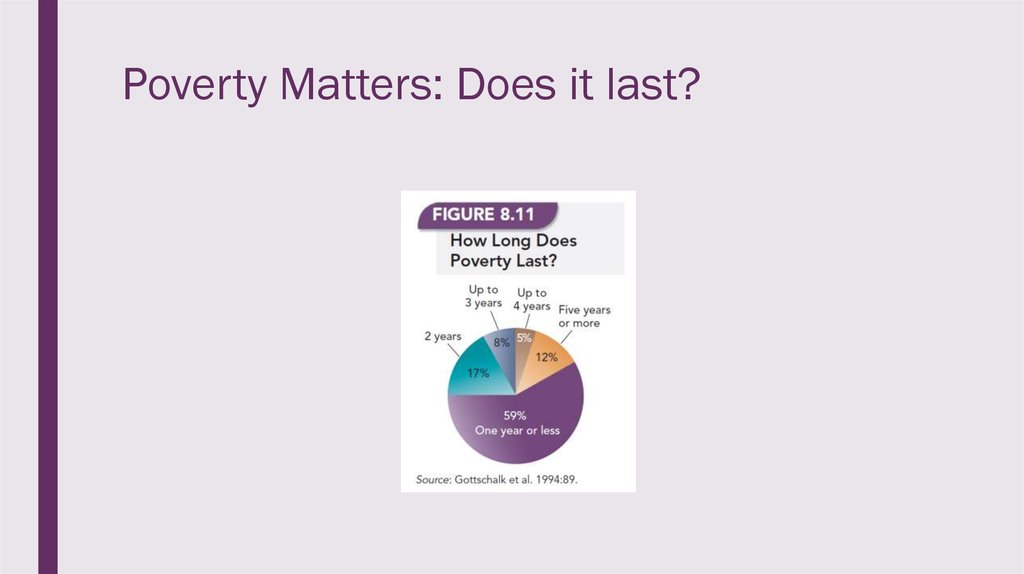
25. Poverty Matters: Does it last?
■ Research finds that most poverty is short-lived.■ The number of those who live in poverty remains consistent, meaning that as many
people move into poverty as move out of it.
■ About ¼ of the U.S. population is or has been poor for at least a year.
■ Sociologists look to such factors as inequalities in education, access to learning job
skills, racial, ethnic, age, and gender discrimination, and large scale economic
change to explain the patterns of poverty in society.
■ Another explanation focuses on how characteristics of individuals are assumed to
contribute to their poverty. Sociologists reject explanations that focus on qualities of
laziness or lack of intelligence to explain poverty.
26. Poverty Matters: Does it last?
27. Poverty Matters
28. Racial/Ethnic Discrepancies
■ Non-White people in the United Statesare disproportionately poor and
combined with racial discrimination
this leads to unfavorable patterns of
health and healthcare delivery.
■ Life expectancy for African American
males is 5.4 years less than White
males and for black females it is 3.7
years less than White females.
■ Native Americans have the poorest
health of any racial category.
■ The life expectancy for Native
Americans is ten years below the
national average.
■ In 2009, the infant mortality rate for:
■ (1) Whites was 6.7 deaths per 1,000
births.
■ (2) Blacks was 13.3 deaths per 1,000
births.
■ The rate among Latinos was 50
percent higher for Puerto Ricans than
Cubans.
■ There is a similar relationship among
Asians with the rate for Filipinos
almost double that of Chinese infants.
29. Racial/Ethnic Discrepancies
■ African American children are twice as likely to be born with low birth weight.■ Heart disease is the leading cause of death in the United States.
■ Black men are twice as likely as White men to die from heart disease before the age of
65.
■ Cancer:
■ a. The death rate from cancer is three and a half times greater for African American
males than for White males.
■ b. The problem is that African Americans (and Latinos) are more likely than Whites to be
diagnosed in later stages.
■ c. The cancer rate is higher for African Americans than Whites for all cancers except
stomach cancer and breast cancer.
30. Racial/Ethnic Discrepancies
■ d. Black women have lower breast cancer rates in part because of the tendency tohave children at younger ages.
■ e. Whites have a higher survival rate of cancer once detected.
■ f. Latinos have the lowest incidence of breast cancer but their chances of survival
are not as good as Whites.
■ g. Asian American women are much less likely than White or Black women to
develop breast cancer and have the best five-year survival rates.
31. Racial/Ethnic Discrepancies
■ African Americans are twice as likelyas Whites to have Alzheimer’s or
other forms of dementia.
■ Over 9 million Americans have visual
impairment, usually caused by
glaucoma, diabetes, and retinal
diseases.
■ Black adults are nearly twice as likely
as Whites to be legally blind or
visually impaired.
■ Latinos are more likely than Whites to
be blind primarily because of
complications from diabetes.
■ Diseases found among the poor (e.g.,
influenza, pneumonia, and
tuberculosis) are disproportionately
found among non-Whites because
racial minorities are
disproportionately poor.
32. Racial/Ethnic Discrepancies
■ The poor in general, and racial minorities in particular, are more likely than Whites torely on emergency room departments than on a family physician. This reliance has
four negative outcomes:
■ (1) The poor do not meet regularly with a physician who is familiar with their health
history.
■ (2) The number of hospitals in poor sections of cities is declining.
■ (3) Federal cutbacks resulted in decreased medical attention for the poor.
■ (4) Even when health services are accessible, minorities may face racial
discrimination.
33. Racial/Ethnic Discrepancies – more specifically
■Asian Americans:
–
81-87 life expectancy
–
Only 14.6% without health insurance
–
Low rates of obesity, heart disease, stroke,
car accidents, suicides, homicides, drug
abuse, and deaths due to AIDS.
–
Education, Income, Family Structure
■
African Americans:
–
Slaves often suffered immensely but could
not refuse treatment
–
Experiments were often performed without
awareness
–
Women involuntarily sterilized
–
Currently, more likely at every age to die
than any other racial group.
–
Twice as likely as Whites to die of diabetes,
five times as likely from homicide, and eight
times as likely from AIDS.
–
African Americans have a 32% higher ageadjusted death rate than Whites for all
causes.
–
Pages 251-256
34. Racial/Ethnic Discrepancies – more specifically
■ Latinos:– Health outcomes compare
favorably with those of other
groups.
– The age-adjusted death rate
for Latinos was lower than that
of all groups, except Asian
Americans.
– One explanation is the
Hispanic Paradox (p.263)
35. Racial/Ethnic Discrepancies – more specifically
■ Native Americans:– Higher death rates than whites
– Suicide is a leading cause of death
– Binge drinking is an issue – AIAN report more binge drinking episodes per
month and higher alcohol consumption per episode than any other racialethnic group. 24.9%
– According to the WH, “From 2003-2011, American Indian/Alaska Native were
more likely to need alcohol or illicit drug use treatment than persons of other
groups by age, gender, poverty level, and rural/urban residence.”
36. Racial/Ethnic Discrepancies – more specifically
––
–
–
–
–
CDC
The rate of past month binge alcohol use was rising among AI/AN adults than the
national average (30.6% vs. 24.5%)
The rate of past month illicit drug use was rising among AI/AN adults than the national
average (11.2% vs. 7.9%)
Cited by SAMHSA
Among AI/AN people, cancer is one of the leading causes of death followed by heart
disease.
Death rates from lung cancer have shown little improvement in AI/AN populations.
AI/AN people have the highest prevalence of tobacco use of any population in the
United States.
Deaths from injuries were higher among AI/AN people compared to non-Hispanic
whites.
37. Racial/Ethnic Discrepancies – more specifically
– Suicide rates were nearly 50 percent higher for AI/AN people compared to nonHispanic whites, and more frequent among AI/AN males and persons youngerthan age 25.
– Death rates from motor vehicle crashes, poisoning, and falls were two times
higher among AI/AN people than for non-Hispanic whites.
– Death rates were higher among AI/AN infants compared to non-Hispanic white
infants. Sudden infant death syndrome and unintentional injuries were more
common. AI/AN infants were four times more likely to die from pneumonia and
influenza.
– By region, the greatest death rates were in the Northern Plains and Southern
Plains. The lowest death rates were in the East and the Southwest. (CDC)
38. Conclusion
■ One of the core values of the U.S. is that everyone should have an equal opportunityto flourish.
■ How does this ideology coexist with the reality of health care access?
■ By discussing the issues with who has insurance, sexism in healthcare, R/E
discrepancies etc. we can be one step closer in answering this question.
■ What does your perfect health care system look like?
39. Sources
■ Race and Racisms, Boza■ Essentials of Sociology, Henslin
■ Social Problems, Eitzen
■ CB
■ CDC
■ SAMHSA














 english
english