Similar presentations:
Hip ultrasound: Why, When, and How?
1. Hip ultrasound: Why, When, and How?
Dorothy Bulas M.D.Children’s National Medical Center
Washington D.C.
2. Disclosure
• I have no relevant financial relationshipswith the manufacturers of any commercial
products and/or provider of commercial
services discussed in this CME activity
• I do not intend to discuss an unapproved use
of a commercial product/device in my
presentation
3. Objectives
• Review the risk factors for developmentaldysplasia of the hip (DDH)
• Understand the appropriate work up and
follow up of DDH
4. Changes in practice
• Use appropriateness criteria to assess fordevelopmental dysplasia.
• Selective screening by ultrasound after 2
weeks of age
5. Introduction
• Developmental dysplasia of the hip is thepreferred term to describe the condition in
which the femoral head has an abnormal
relationship to the acetabulum.
• DDH is a spectrum of abnormalities
–
–
–
–
frank dislocation (luxation)
partial dislocation (subluxation)
unstable - femoral head comes in & out of socket
inadequate formation of the acetabulum.
6. DDH
• Many of these findings may not be presentat birth
• SO - the term developmental more
accurately reflects the biologic features than
the term congenital.
7. Early Diagnosis
• The earlier a dislocated hip is detected, thesimpler and more effective is the treatment.
8. Late Diagnosis
• Late dx in children may lead to increasedsurgical intervention and complications.
• Late dx in adults can result in debilitating
end-stage degenerative hip joint disease.
9. Why Screen?
• Screening decreases the incidence of latediagnosis of DDH.
• Despite screening programs, DDH
continues to be diagnosed later in infancy
/childhood, delaying appropriate therapy
• Substantial number of malpractice claims
10. Incidence
• 1.5 : 1,000 Caucasian Americans– less frequent African Americans.
• F:M 6:1 (?hormonal)
• The reported incidence influenced by FH,
–
–
–
–
race,
diagnostic criteria,
experience /training of examiner,
age.
11. Incidence
• Family History– 6% risk - healthy parents & affected child
– 12% risk - affected parent
– 36% risk- affected parent & 1 affected child.
• Left hip 3 :1
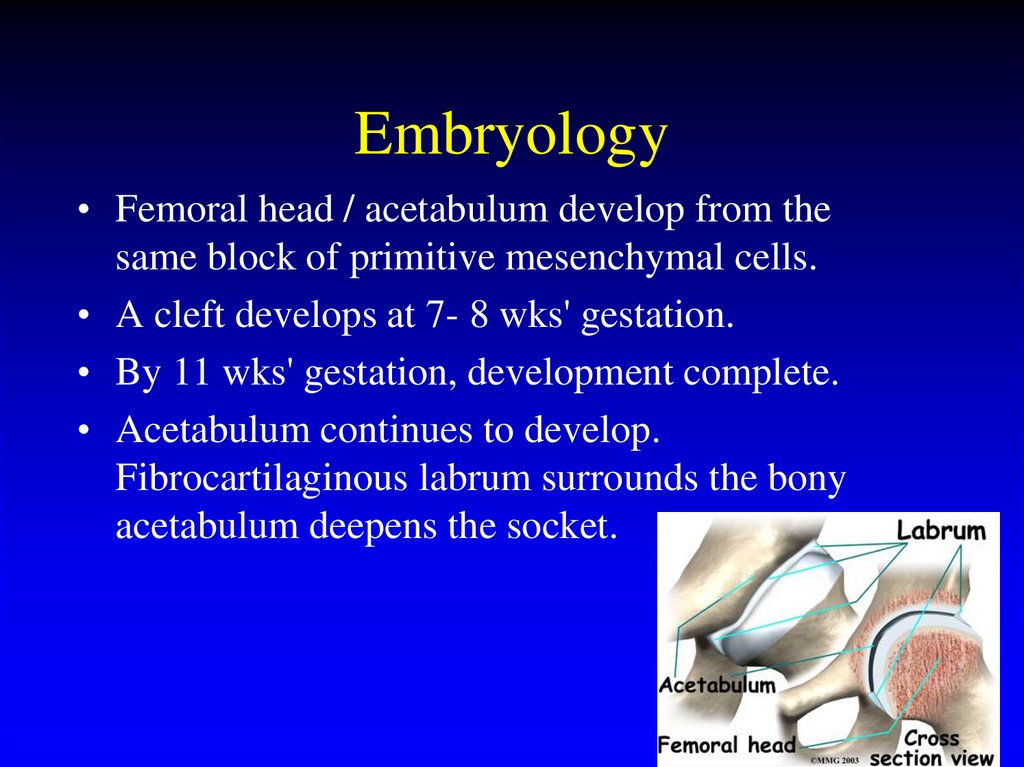
12. Embryology
• Femoral head / acetabulum develop from thesame block of primitive mesenchymal cells.
• A cleft develops at 7- 8 wks' gestation.
• By 11 wks' gestation, development complete.
• Acetabulum continues to develop.
Fibrocartilaginous labrum surrounds the bony
acetabulum deepens the socket.
13. Embryology
• Development of femoral head /acetabulumrelated, normal adult hip joints depend on
growth of these structures.
14. Embryology
Hip dysplasia may occur–
–
–
–
in utero,
perinatally
during infancy
childhood
15. Embryology
Dislocations divided into 2 types: teratologic/ typical.• Teratologic dislocations occur in utero and often
associated with neuromuscular disorders arthrogryposis/myelodysplasia, or syndromes.
• Typical dislocation occurs in otherwise healthy
infant - prenatally or postnatally.
16. Embryology
• Newborn period- laxity of hip capsule– femoral head may spontaneously dislocate and
relocate.
• If hip spontaneously relocates /stabilizes, hip
development is normal.
• If subluxation/ dislocation persists structural
anatomic changes develop.
17. Embryology
• Need deep concentric position of femoral head inacetabulum.
• If not, labrum flattens, acetabulum doesn’t
grow/remodel and becomes shallow.
• If dislocates, inferior capsule pulled up over empty
socket.
• Adductors contract, limiting hip abduction.
• Hip capsule constricts; hip cannot be reduced
manually
– operative reduction necessary.
18. Embryology
At risk 4 periods:1) 12th gest week- fetal lower limb rotates medially.
Teratologic.
2) 18th gest week – hip muscles dev.
Myelodysplasia/arthrogryposis lead to Teratologic
dislocations
3) Final 4 weeks of gestation
Oligohydramnios/breech. Breech 3% of births,
DDH up to 23%. Frank breech hip flexion /knee
extension at highest risk.
4) Postnatal period -swaddling, combined with
ligamentous laxity Typical
19. Risk Factors
– Family history– Breech
– Oligohydramnios
– Foot deformities
– Torticollis
20. Clinical evaluation
• Evolves - clinical examchanges.
• Should be performed at
each well-baby visit until
12 months.
• Newborn relaxed,
examined on firm
surface.
21. Physical Exam
• No signs are pathognomonic for adislocated hip.
– Asymmetrical gluteal folds (best observed prone)
– Apparent limb length discrepancy
– Restricted motion
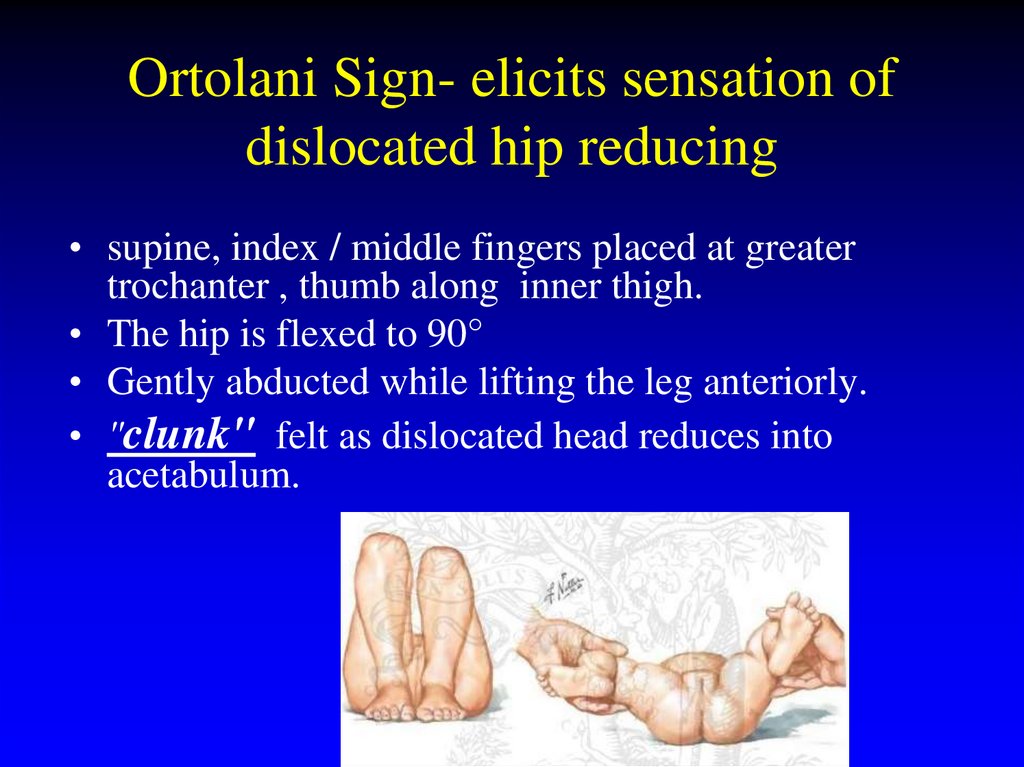
22. Ortolani Sign- elicits sensation of dislocated hip reducing
• supine, index / middle fingers placed at greatertrochanter , thumb along inner thigh.
• The hip is flexed to 90°
• Gently abducted while lifting the leg anteriorly.
• "clunk" felt as dislocated head reduces into
acetabulum.
23. Barlow Sign- detects unstable hip dislocating from acetabulum
• Supine hips flexed to 90°.• Leg adducted while
posterior pressure on knee.
• Palpable clunk as head
exits acetabulum.
• Forceful /repeated exam
can break the seal b/w
labrum /femoral head.
24. Physical Exam after 3 months
• By 8 - 12 weeks, capsule laxity decreases,muscle tightness increases
– Barlow /Ortolani maneuvers no longer
positive.
• After 3 mos, limitation of abduction most
reliable sign.
– Discrepancy of leg lengths.
25. Physical Exam
• False negative exam - Acetabular dysplasiamay have no subluxation/ dislocation.
• False Positive exam - <1 mos NORMALLY
increased capsular laxity - subluxation due to
maternal estrogens
• Equivocal examination
– asymmetric thigh or buttock creases
– Apparent or true short leg,
– Limited abduction.
26.
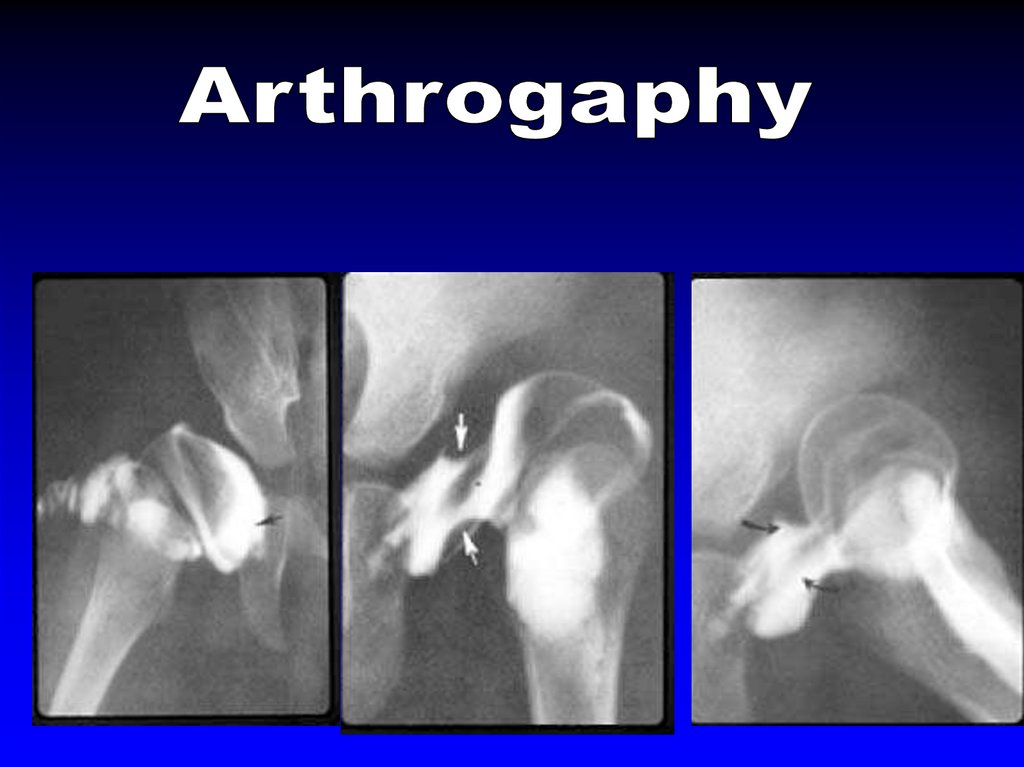
27. Radiographs
• Radiographs readily available, low cost.• In neonate- femoral heads cartilage, limited
– Displacement and instability undetectable
• 4 - 6 months, radiographs more reliable,
when ossification center develops.
28. Developmental Dysplasia of the Hip Radiologic Findings
• Acetabular index– slope of acetabular roof
> 30 0
• Line of Hilgenreiner
– triradiate cartilage
• Perkins line (vertical)
• Femoral epiphysis in
inner lower quadrant
• Shenton’s curve
29.
30.
31. Negative radiograph does not R/O dislocation
32.
33. Sonographic Evaluation
No sedation, no radiation
Rapid
Noninvasive
Inexpensive
• Cartilage visualized can assess the stability of the hip and
the morphologic features of the acetabulum.
34. Methods
• Graf method – single coronal plane• Dynamic or real-time method- Harckeassesses the hip for stability of femoral head
in socket, as well as static anatomy.
• With both techniques, considerable
interobserver variability, especially during
the first 3 weeks of life.
35. Sonographic Evaluation
• Assess– Acetabular
depth
– Position of
limbus
– Stability of hip
36.
37.
Ac Acetabular cartilageC Capsule
G Gluteus muscles
GT Greater trochanter
H Cartilaginous femoral head
IL Ilium
Is Ischium
L
Labrum
LT/P Ligamentum teres/ pulvinar
complex
M Femoral metaphysis
Tr Triradiate cartilage
38.
39.
•Single coronal image emphasizes acetabular development40. Graf Technique
– Type 1: normal α angle > 60o41. Graf Technique
-Type II :α
44-60o, β 55-88o
IIa < 3 months immature acetabulum
(40-59%)
No referral required
IIb,c,d require referral for treatment
42. Graf Technique
• Type III : α <44o, β>77oLow displacement
• Type IV : completely dislocated
– Immediate therapy
43. Coronal Harke method
44. Acetabular Coverage >50%
Acetabular Coverage >50%45. Acetabular Coverage >50%
Acetabular Coverage >50%46.
47.
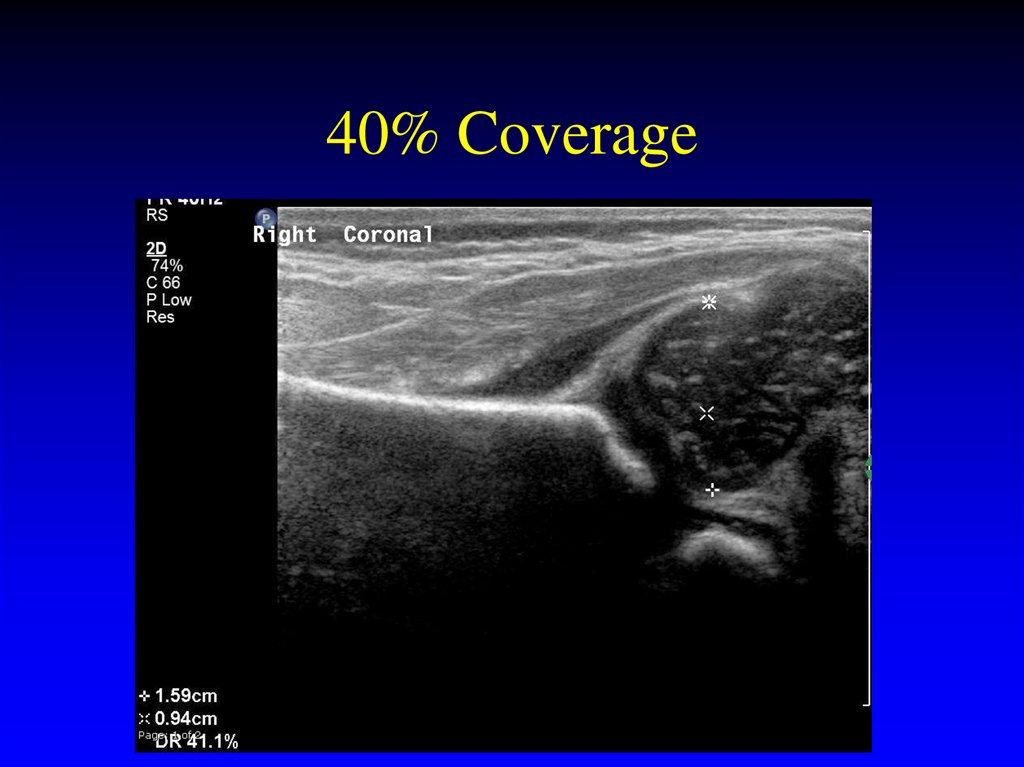
40% Coverage48. 40% Coverage
33% Coverage49. 33% Coverage
20% Coverage50. 20% Coverage
51.
52.
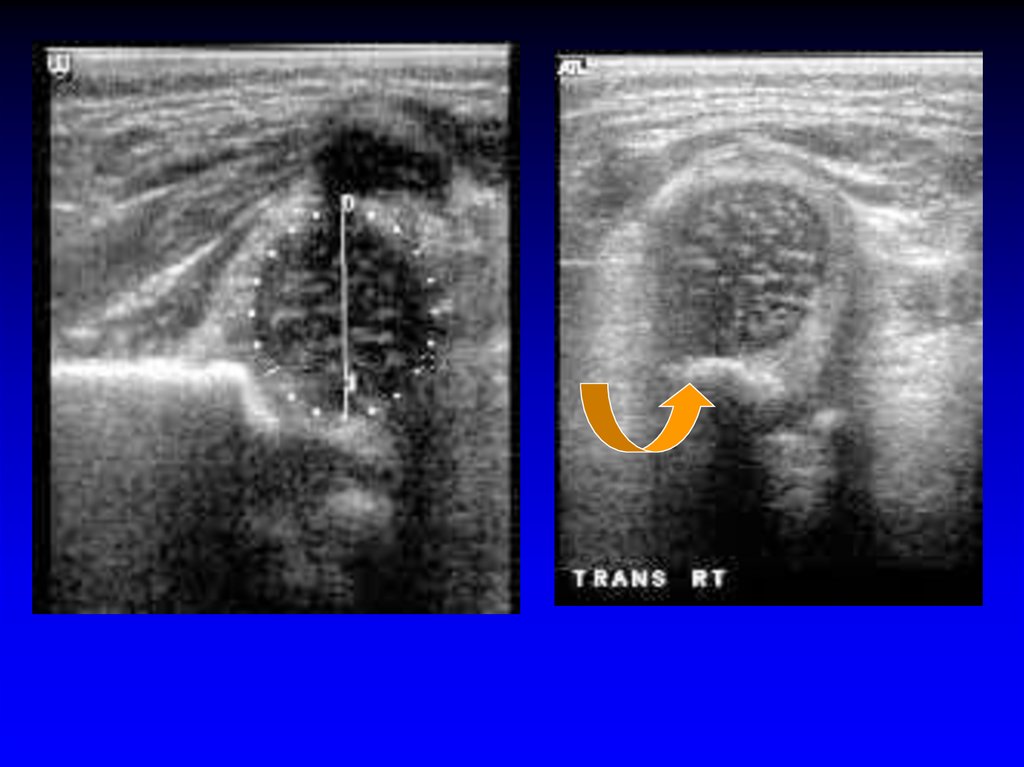
Dynamic Sonography-Technique• Supine or lateral
• Coronal view at rest
neutral or flexed
– stress view
optional
• Transverse flexion
view with stress
53. Dynamic Sonography-Technique
54.
55.
AcAcetabular cartilage
G Gluteus muscles
GT
Greater trochanter
H Cartilaginous femoral head
Is Ischium
L Labrum
LT/P
Ligamentum
complex
teres/pulvinar
M Femoral metaphysis
Pu
Pubis
Tr
Triradiate cartilage
56.
57.
58.
59.
60.
Stress - Stable61.
Stress - unstable62. Stress - Stable
63. Stress - unstable
Dislocated64.
Dislocated65. Dislocated
66. Dislocated
Calcified femoral epiphysis67.
68. Calcified femoral epiphysis
Peterlein et al BMC Pediatr. 2010 24;10:98.Reproducibility of different screening
classifications in US of the newborn hip.
• Concordance of 2 classifications of hip morphology and
subjective parameters by 3 investigators w/different
levels of experience.
• METHODS: 207 newborns: α-angle and β-angle,"femoral head
coverage" (FHC) shape of bony roof and position of cartilaginous roof.
• RESULTS: shape of bony roof (0.97) and position of cartilaginous roof
(1.0) demonstrated high intra-observer reproducibility.
• Best results were achieved for α-angle, followed by β-angle then FHC.
• CONCLUSIONS: Higher measurement
differences in objective scorings. Variations
by every investigator irrespective of level of
experience
69.
Follow up• Can perform exam in
Pavlik Harness
• Perform out of harness
only if requested and/or
hip appears stable
• Once femoral head
ossifies difficult to
assess position.
70. Peterlein et al BMC Pediatr. 2010 24;10:98. Reproducibility of different screening classifications in US of the newborn hip.
71. Follow up
Treatment• Dislocated – treat
• Stable – don’t treat
• Unstable (lax not displaced)
– ? Early treatment or observation??
– 80% normalize
72.
73. Treatment
DDH - 35%74.
One month later75.
76.
Follow Up77. DDH - 35%
Should we Screen?• There is no consensus on imaging screening
for DDH.
• Screening balanced between the benefits of
early detection of DDH and the increased
treatment and cost factors.
78. One month later
Who?• Universal Newborn Screening
– pro- treat early
– con-over treat minor abnormalities that
resolve
• Considerable resources
• Late cases missed
• Higher rate of therapy?
• Higher rate of avscular necrosis?
79.
Universal Screening• Randomized trials evaluating primary US
screening did not find significant decrease
in late diagnosis of DDH.
• This practice is yet to be validated by
clinical trial.
80. Follow Up
Who?Selective screening
• AAP US recommended as adjunct to
clinical evaluation. technique of choice to
clarify physical finding, assess high-risk
infant, and monitor DDH as is observed or
treated.
• Can guide treatment and may prevent
overtreatment
81. Should we Screen?
Who?• In the United States, hip US is selectively
performed
–
–
–
–
–
–
Club foot
Torticollis
Females in breech position
Optional males in breech position
Optional females with positive FH
Inconclusive PE
82. Who?
Studies – Selective Screening• British 10 yr prospective of 34,723
– 2,578 clinical instability or risk factor
– 77 unstable - 31% risk factor
• Irish 52,893 infants
– US – 5,484 with FH, breech, click.
– 18 dislocatable,153 (2.73%) dysplastic
3.2/1000 required Rx
• 33 center United Kingdom Hip Trial
– found reduces splinting, and no increase in
surgical Rx
83. Universal Screening
Preterm infants• DDH may be unrecognized.
• When the infant has cardiorespiratory problems,
the diagnosis and management are focused on
providing appropriate ventilatory and
cardiovascular support, careful examination may
be deferred until a later date.
• The most complete examination the infant
receives may occur at the time of discharge from
the hospital, and this single exam may not detect
subluxation or dislocation.
• critical to examine the entire child.
84. Who?
85. Who?
86. Studies – Selective Screening
87. Preterm infants
When?• PRO - US can detect abnormal position,
instability, and dysplasia not evident on clinical
examination.
• CON - during the first month minor degrees of
instability and acetabular immaturity.
– nearly all mild early findings not be apparent on PE,
resolve spontaneously without treatment.
• Newborn screening - high frequency of
reexamination and hips being unnecessarily
treated.
• screening with higher false-pos results yields increased
prevention of late cases.
88.
When?• Screen those at risk at 4-6 wks (9%)
–pro
• less expense,simpler process
• fewer false positives
–con
• miss late cases
89.
Hip EvaluationClinical Exam
Normal Exam
Abnormal Exam
No risk factors
Risk factors
Stable Click
Unstable Click
STOP
US 4 wks
US 4 wks
Us 1-2 wks
90.
What are the AAP recommendations?1. All newborns screened by PE by a properly
trained health care provider (Evidence strong.)
2. US of all newborns is not recommended.
(Evidence fair; consensus is strong.)
Although indirect evidence supports US screening of
all newborns, not advocated –
operator-dependent,
availability is questionable,
increases treatment,
interobserver variability is high,
increased costs.
91. When?
3. If positive Ortolani or Barlow signfound in the newborn, refer to an
orthopaedist.
4. If results of the PE at birth are
"equivocally" positive (ie, soft click, mild
asymmetry,), FU hip exam by the
pediatrician in 2 weeks is recommended.
(Evidence is good; consensus is strong.)
92. When?
• The hips must be examined at every wellbaby visit– (2–4 days for newborns discharged in less
than 48 hours after delivery, 1 mos, 2 mos, 4
mos, 6 mos, 9 mos, 12 mos).
• If DDH is suspected confirmation made by
a focused PE, by consultation with another
pediatrician, orthopaedist, by US if the
infant is < 5 months of age, or by
radiography if the infant > 4 months of age.
93. Hip Evaluation
Conclusions• US has become the standard of care in the
evaluation of the neonate with possible
developmental dysplasia of the hip.
• Availability widespread, however, accurate
results require training and experience.
94. What are the AAP recommendations?
Changes in practice• Use appropriateness criteria to assess for
developmental dysplasia.
• Selective screening by ultrasound after 2
weeks of age
95.
AAP Clinical Practice Guideline:Early Detection of DDH
• Committee on Quality Improvement,
Subcommittee on Developmental
Dysplasia of the Hip
























































































 english
english








