Similar presentations:
Yersinia pestis
1. Yersinia pestis
2. Yersinia pestis
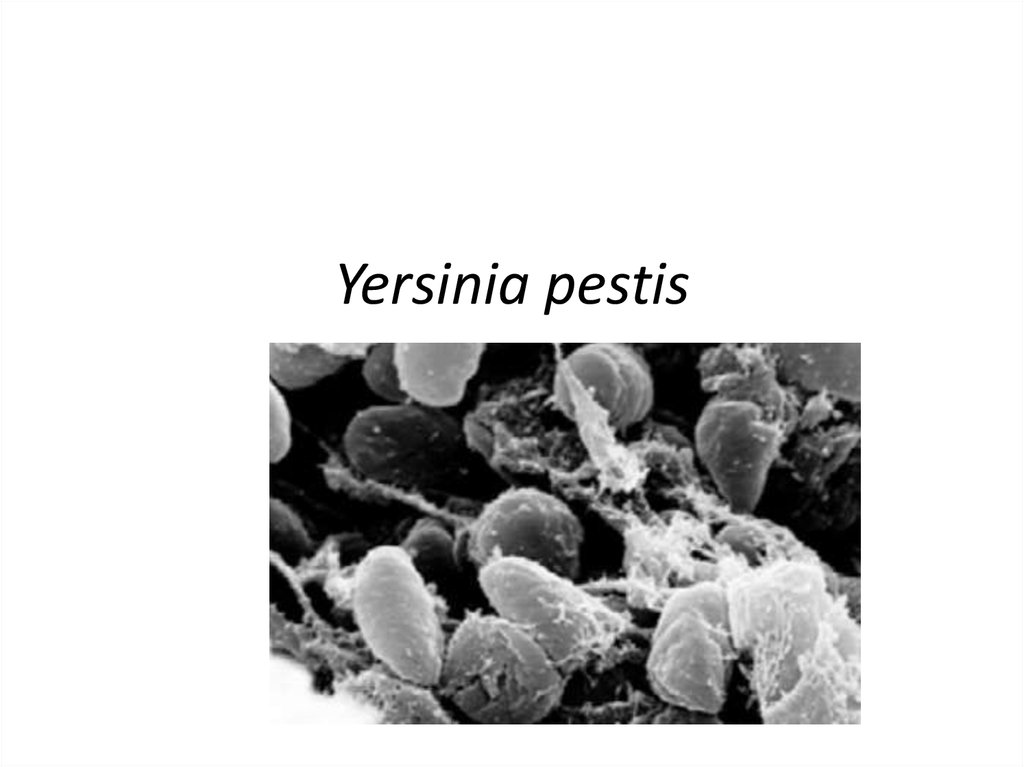
Yersinia pestis• (formerly Pasteurella pestis) is a Gramnegative
rodshapedbacterium belonging to the
family Enterobacteriaceae. It is
a facultative anaerobe that can infect
humans and other animals.
• Human Y. pestis infection takes three
main forms: pneumonic, septicemic,
and the notorious bubonic plagues. All
three forms are widely believed to have
been responsible for a number of highmortality epidemics throughout human
history, including the Black Death that
accounted for the death of at least onethird of the European population
between 1347 and 1353.
3. Role in Black Death
Confirmed presence of Y. pestis would
suggest that it was a contributing factor in
some of (though possibly not all) the
European plagues.
In 2000, Didier Raoult and others reported
finding Y. pestis DNA by performing a
"suicide PCR" on tooth pulp tissue from a
fourteenth-century
plague
cemetery
in Montpellier.
However, in 2003 geneticists at Oxford
University argued Raoult's approach was
inadequate and reported having been unable
to obtain any Y. pestis DNA from 121 teeth
from sixty-six skeletons found in fourteenthcentury mass graves. Lead author Alan
Cooper concluded that though "[w]e cannot
rule out Yersinia as the cause of the Black
Death ...right now there is no molecular
evidence for it."
The plague is believed to be the cause of the Black Death that swept through
Asia, Europe, and Africa in the 14th century and killed an estimated 50 million
people.
4. SYMPTOMS
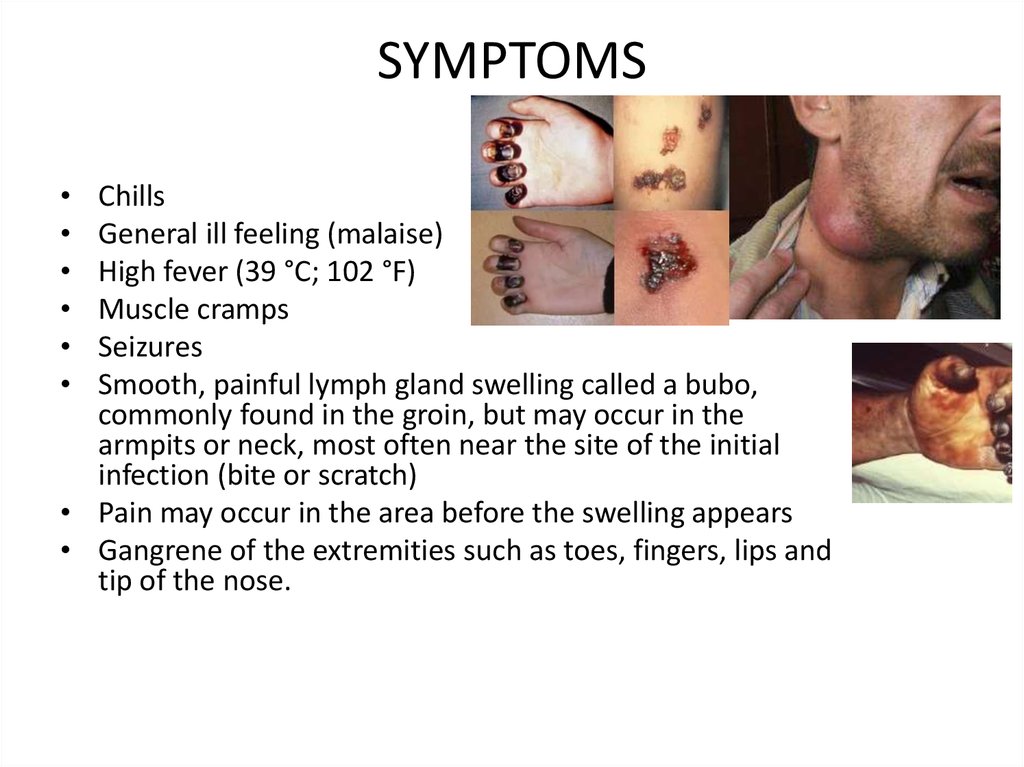
Chills
General ill feeling (malaise)
High fever (39 °C; 102 °F)
Muscle cramps
Seizures
Smooth, painful lymph gland swelling called a bubo,
commonly found in the groin, but may occur in the
armpits or neck, most often near the site of the initial
infection (bite or scratch)
• Pain may occur in the area before the swelling appears
• Gangrene of the extremities such as toes, fingers, lips and
tip of the nose.
5. Cause
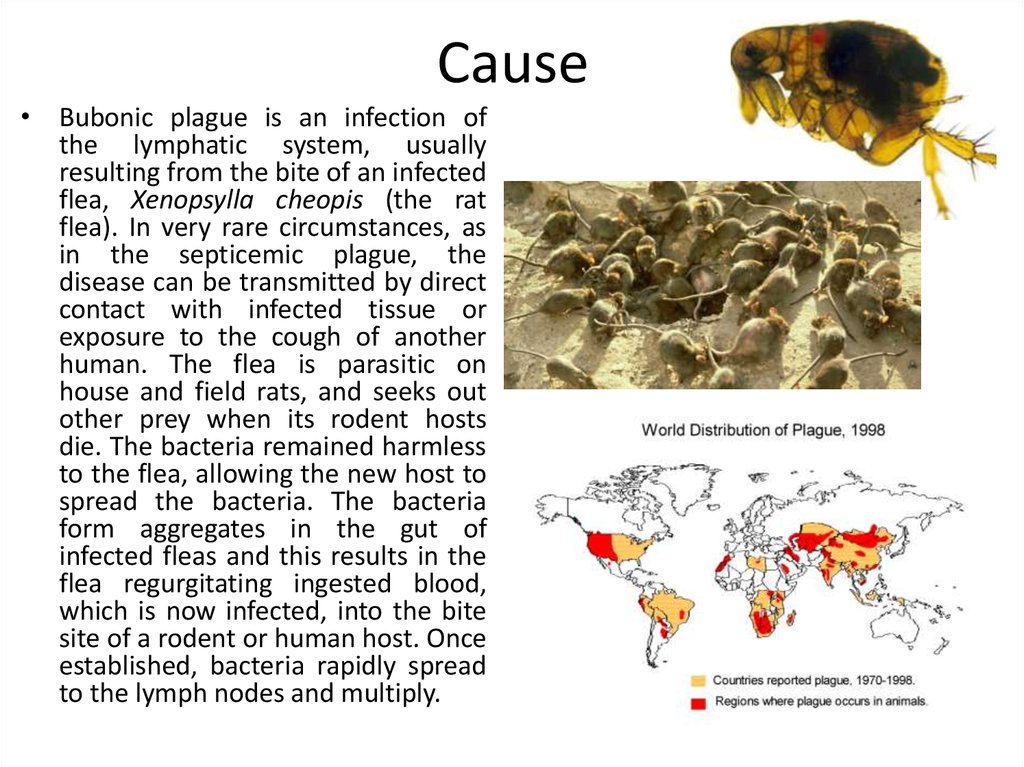
• Bubonic plague is an infection ofthe lymphatic system, usually
resulting from the bite of an infected
flea, Xenopsylla cheopis (the rat
flea). In very rare circumstances, as
in the septicemic plague, the
disease can be transmitted by direct
contact with infected tissue or
exposure to the cough of another
human. The flea is parasitic on
house and field rats, and seeks out
other prey when its rodent hosts
die. The bacteria remained harmless
to the flea, allowing the new host to
spread the bacteria. The bacteria
form aggregates in the gut of
infected fleas and this results in the
flea regurgitating ingested blood,
which is now infected, into the bite
site of a rodent or human host. Once
established, bacteria rapidly spread
to the lymph nodes and multiply.
6.
Antigenic structure• Flagellar H antigens
• Somatic antigens
• Antigens of virulence (v, w)
• According to the antigen Y 8
serovars
By the structure of the G antigen
Y, more than 50 serovars
Pathogenicity factors of Yersinia
Enterotoxin
Endotoxin
Cytotoxin
Enzymes of neuraminidase and
hyaluronidase
Peeled and outer membrane proteins
Invasive protein and proteins that interfere
with phagocytosis
Synthesis of serine protease
Antigenic associations of Yersinia with some
human tissue antigens
Plasmids (pVv 42-48 Mda and VM82 Mda)
7. Laboratory Diagnosis:
• Blood is taken for culture and lymph node aspirate forsmear and culture. Sputum culture for pneumonic plague,
Cerebrospinal fluid (CSF) for culture and smear in possible
meningitis, stained smear will show Y. pestis with bipolar
deep staining. Y. pestis can be grown on blood agar and
MacConkey’s agar.
• All cultures are highly infectious and must be handled with
care. Experimental animals should be deeply buried with
lime. The disease can be contracted if the infected material
comes in contact with broken skin (bite or scratch).
• A presumptive diagnosis can be confirmed in about 80% of
cases by fluorescent antibody staining. Microscopical
examination of buffy coat smear of peripheral blood may
show Y. pestis in septicaemic cases.
8. Biochemical Test and Identification of Yersinia pestis
Biochemical Test and Identification ofYersinia pestis
Basic Characteristics
Properties (Yersinia pestis)
Capsule
Positive (+ve)
Flagella
Non-Flagellated
Gas
Negative (-ve)
Gram Staining
Negative (-ve)
H2S
Negative (-ve)
Hemolysis
Negative (-ve)
Fermentation of
Glucose
Lactose
Maltose
Mannitol
Sucrose
Positive (+ve)
Negative (-ve)
Positive (+ve)
Positive (+ve)
Negative (-ve)
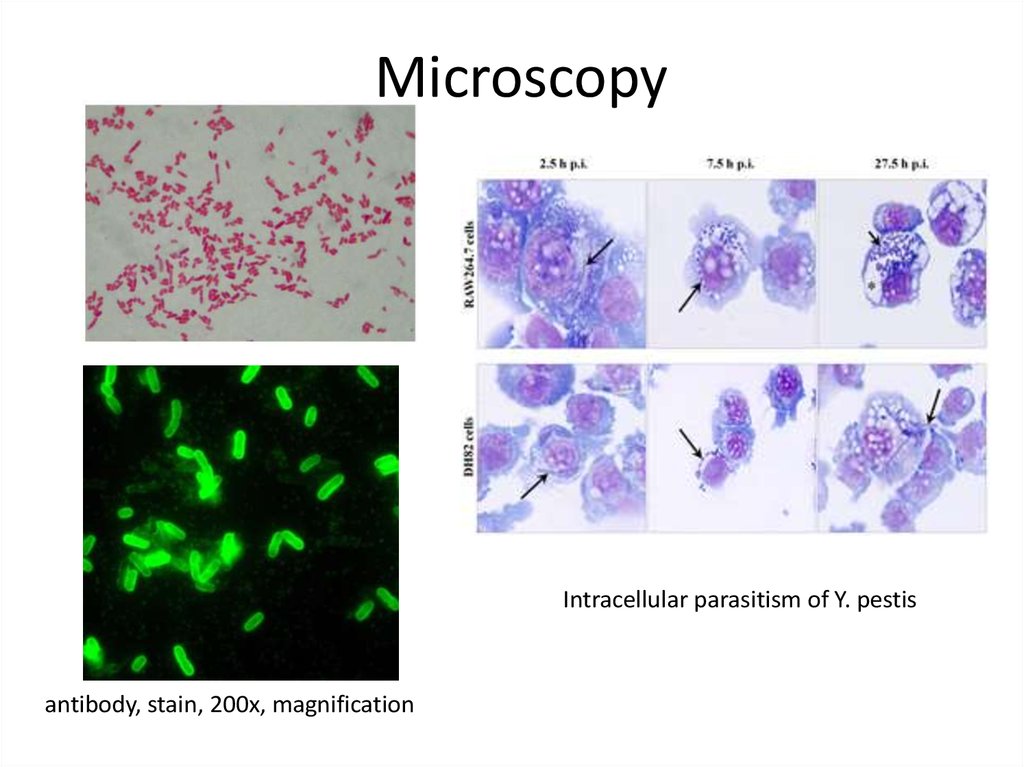
9. Microscopy
Intracellular parasitism of Y. pestisantibody, stain, 200x, magnification
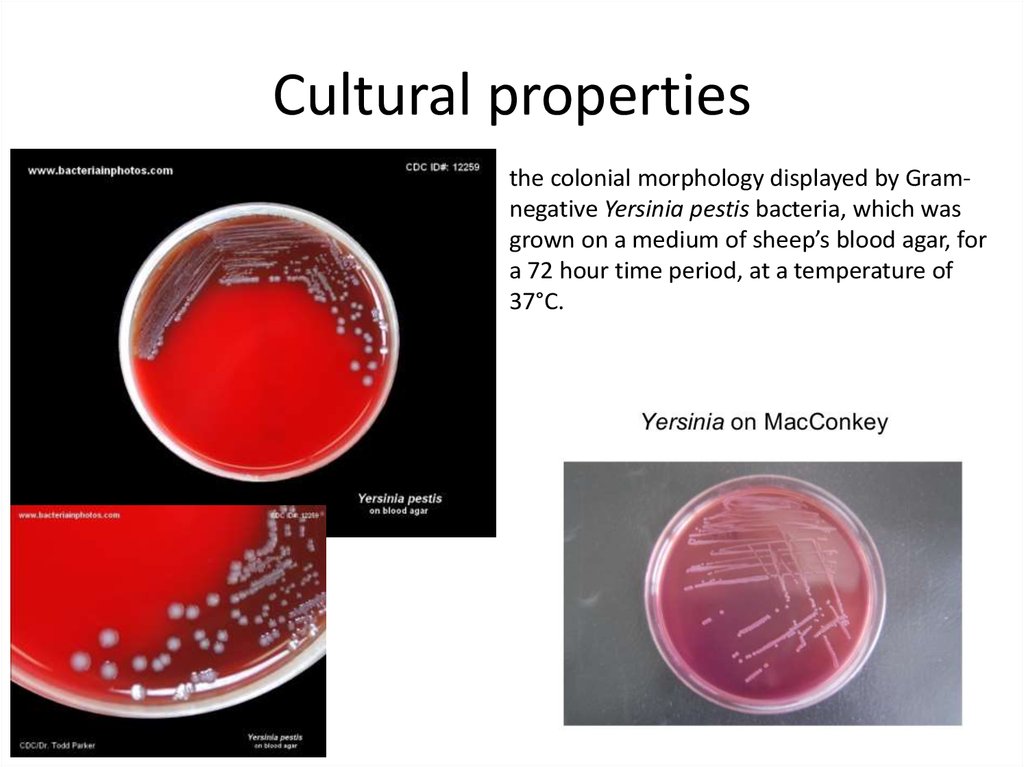
10. Cultural properties
the colonial morphology displayed by Gramnegative Yersinia pestis bacteria, which wasgrown on a medium of sheep’s blood agar, for
a 72 hour time period, at a temperature of
37°C.
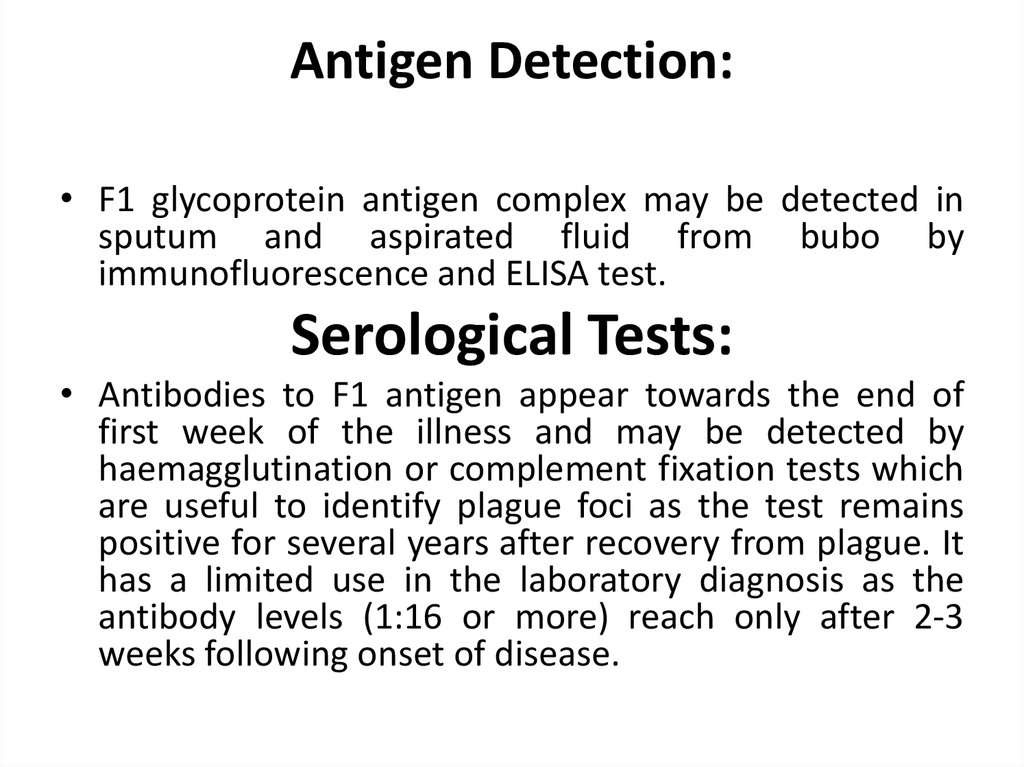
11. Antigen Detection:
• F1 glycoprotein antigen complex may be detected insputum and aspirated fluid from bubo by
immunofluorescence and ELISA test.
Serological Tests:
• Antibodies to F1 antigen appear towards the end of
first week of the illness and may be detected by
haemagglutination or complement fixation tests which
are useful to identify plague foci as the test remains
positive for several years after recovery from plague. It
has a limited use in the laboratory diagnosis as the
antibody levels (1:16 or more) reach only after 2-3
weeks following onset of disease.
12. Treatment
• Several classes of antibiotics are effective in treating bubonicplague.
These
include
aminoglycosides
such
as streptomycin and gentamicin, tetracyclines (especially doxycyclin
e), and the fluoroquinolone ciprofloxacin. Mortality associated with
treated cases of bubonic plague is about 1–15%, compared to a
mortality of 40–60% in untreated cases.
• People potentially infected with the plague need immediate
treatment and should be given antibiotics within 24 hours of the
first symptoms to prevent death. Other treatments include oxygen,
intravenous fluids, and respiratory support. People who have had
contact with anyone infected by pneumonic plague are given
prophylactic antibiotics. Using the broad-based antibiotic
streptomycin has proven to be dramatically successful against the
bubonic plague within 12 hours of infection.





 medicine
medicine








