Similar presentations:
Sexually transmitted bacterial diseases
1. SEXUALLY TRANSMITTED BACTERIAL DISEASES
2. PLAN
• Morphology• Culture
• Antigenic structure
• Virulence factors
• Pathogenesis
• Immunity
• Clinical syndromes
• Epidemiology
• Laboratory diagnosis
• Treatment
• Prevention
3.
• A 28-year-old hair dresser complained of a painless small ulcer on thepenis during the last 2 weeks. When asked, he said he had repeated
sexual relation with a female sexual worker approximately many
months back. On examination, the pus exudate from the smear did
not reveal any Treponema. Serum sample was found to be positive for
syphilis by the VDRL test. ELISA for HIV was negative
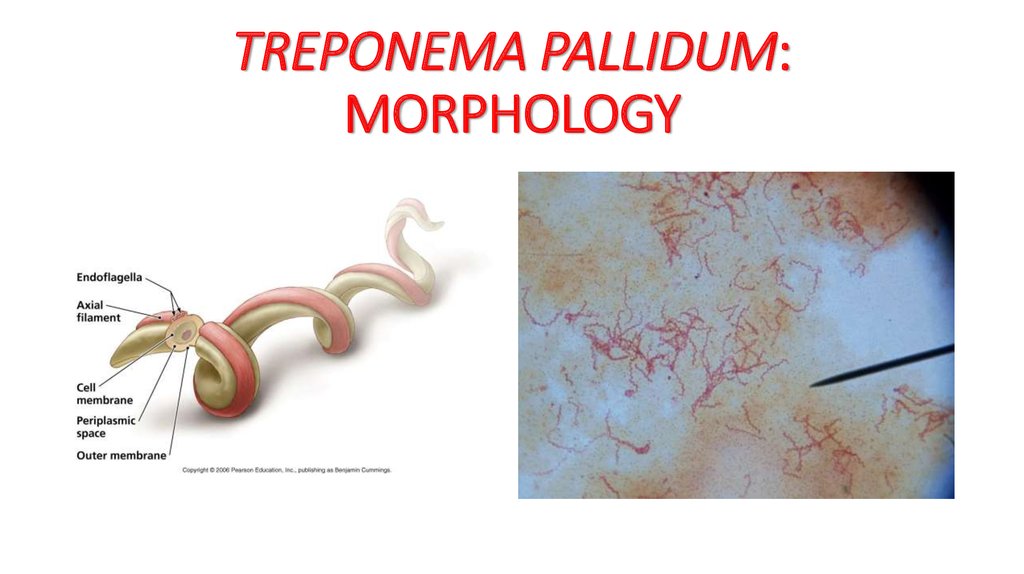
4. TREPONEMA PALLIDUM: MORPHOLOGY
5. TREPONEMA PALLIDUM : ANTIGENIC STRUCTURE
• Cardiolipin antigen• T. pallidum group-specific antigen
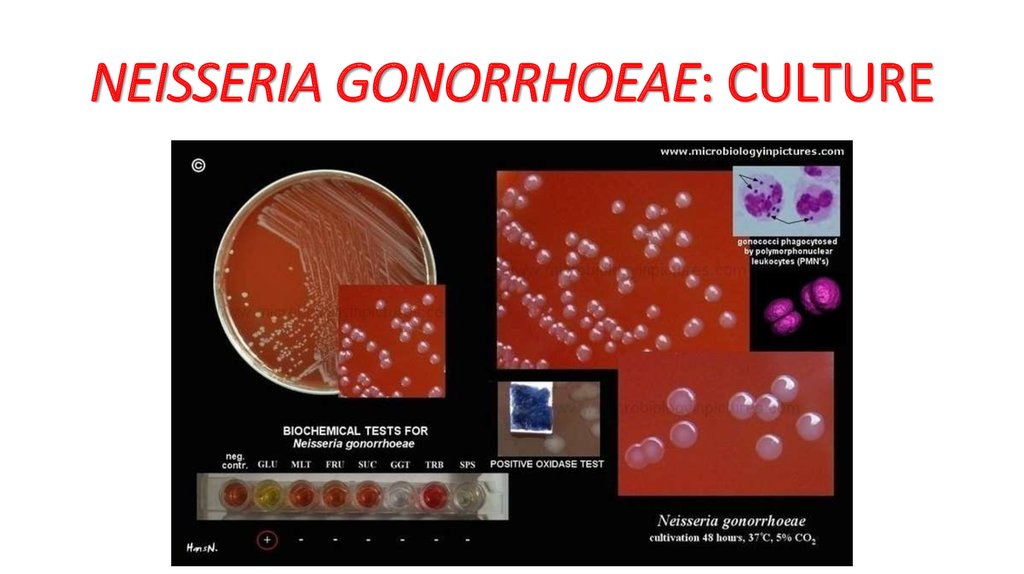
• T. pallidum species-specific antigen
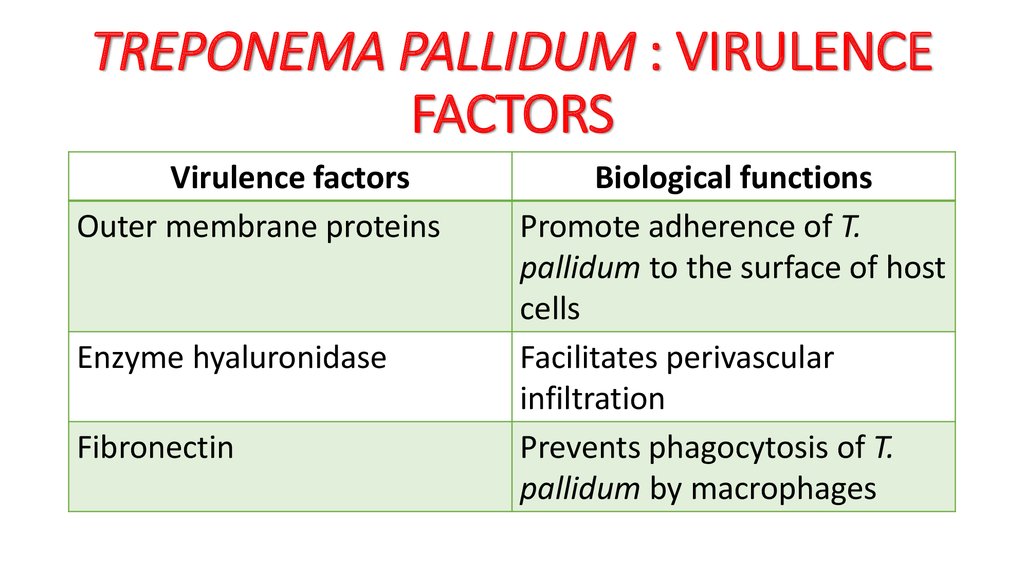
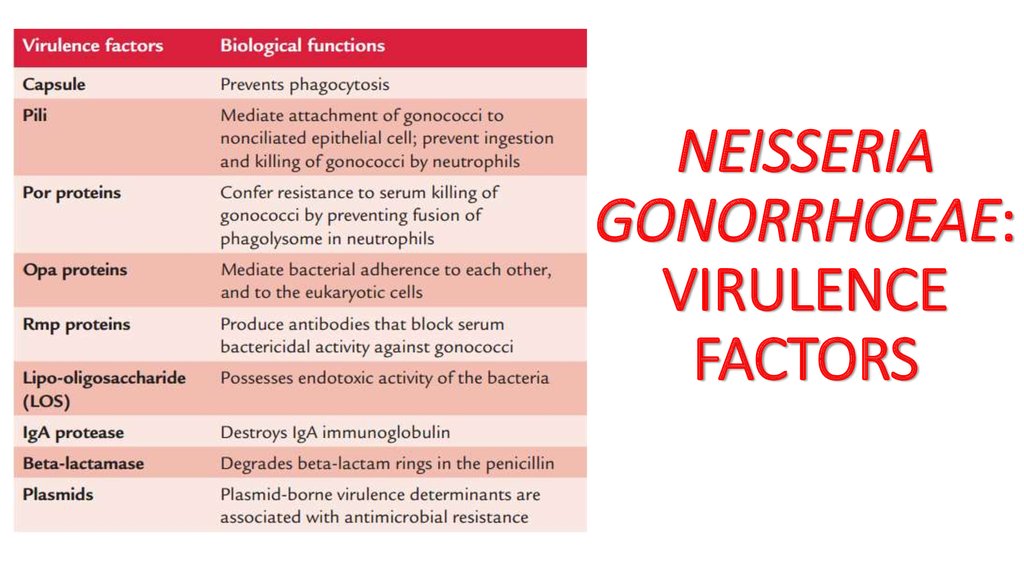
6. TREPONEMA PALLIDUM : VIRULENCE FACTORS
Virulence factorsOuter membrane proteins
Enzyme hyaluronidase
Fibronectin
Biological functions
Promote adherence of T.
pallidum to the surface of host
cells
Facilitates perivascular
infiltration
Prevents phagocytosis of T.
pallidum by macrophages
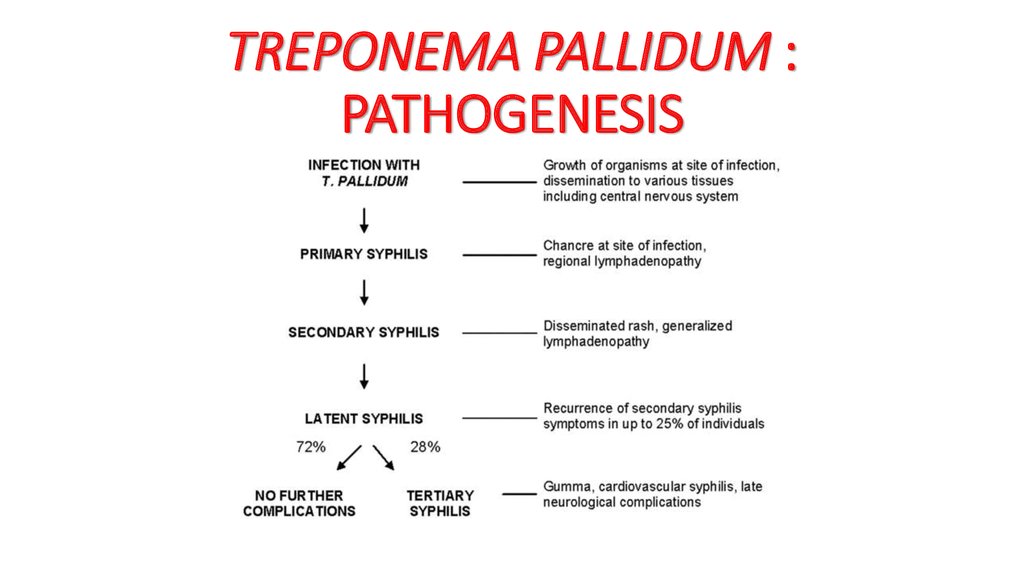
7. TREPONEMA PALLIDUM : PATHOGENESIS
8. TREPONEMA PALLIDUM : CLINICAL SYNDROMES
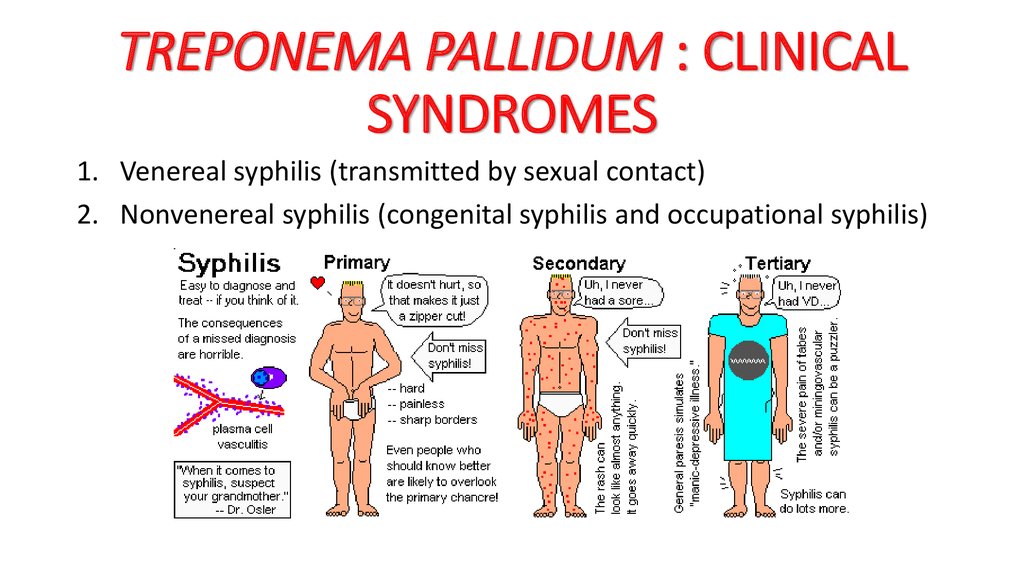
1. Venereal syphilis (transmitted by sexual contact)2. Nonvenereal syphilis (congenital syphilis and occupational syphilis)
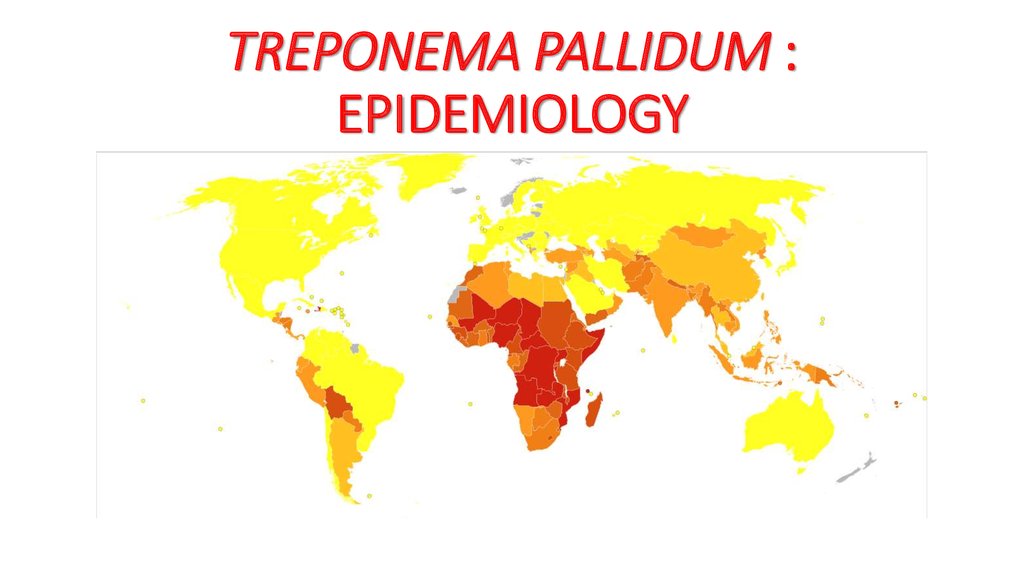
9. TREPONEMA PALLIDUM : EPIDEMIOLOGY
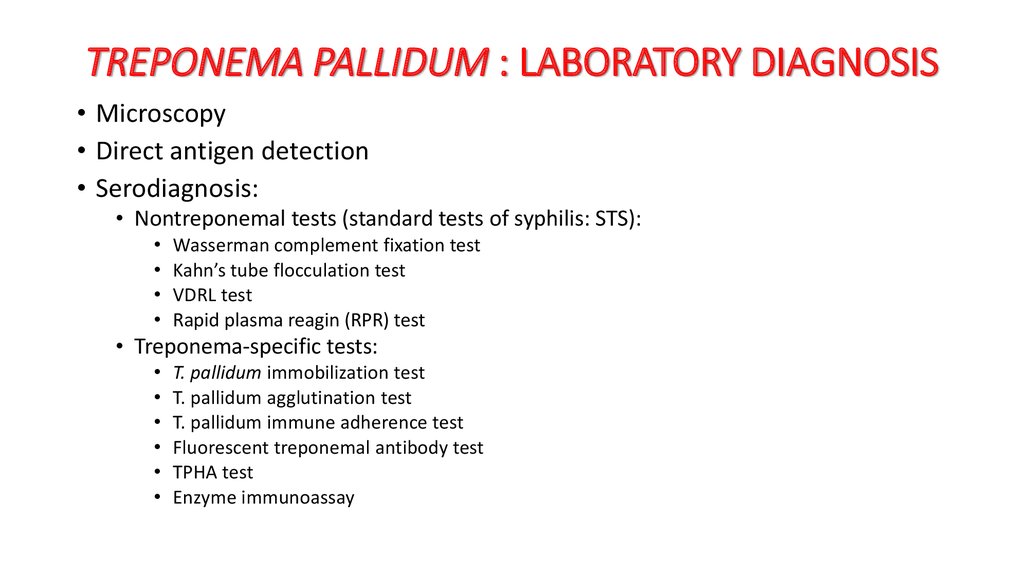
10. TREPONEMA PALLIDUM : LABORATORY DIAGNOSIS
• Microscopy• Direct antigen detection
• Serodiagnosis:
• Nontreponemal tests (standard tests of syphilis: STS):
Wasserman complement fixation test
Kahn’s tube flocculation test
VDRL test
Rapid plasma reagin (RPR) test
• Treponema-specific tests:
T. pallidum immobilization test
T. pallidum agglutination test
T. pallidum immune adherence test
Fluorescent treponemal antibody test
TPHA test
Enzyme immunoassay
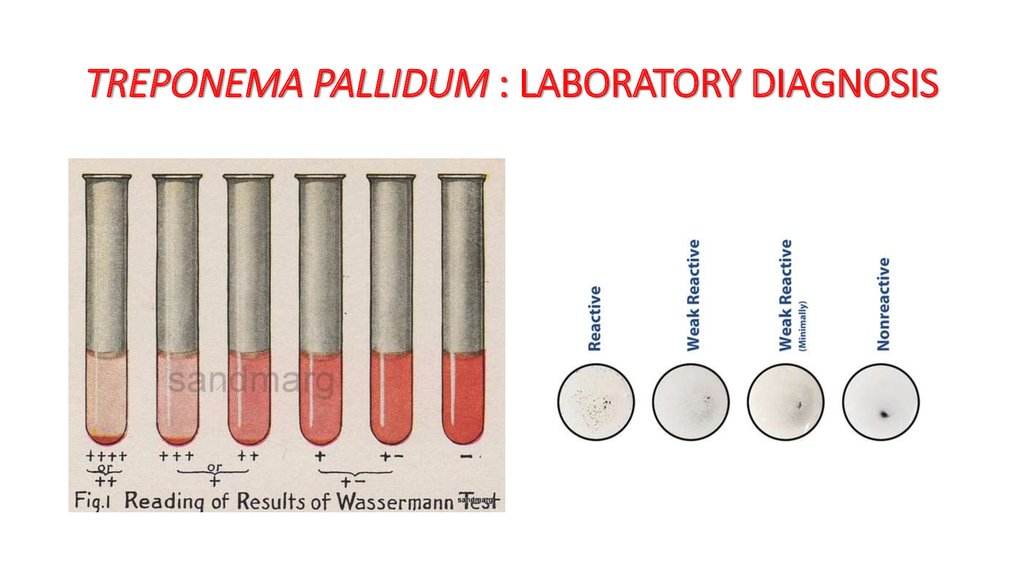
11. TREPONEMA PALLIDUM : LABORATORY DIAGNOSIS
12.
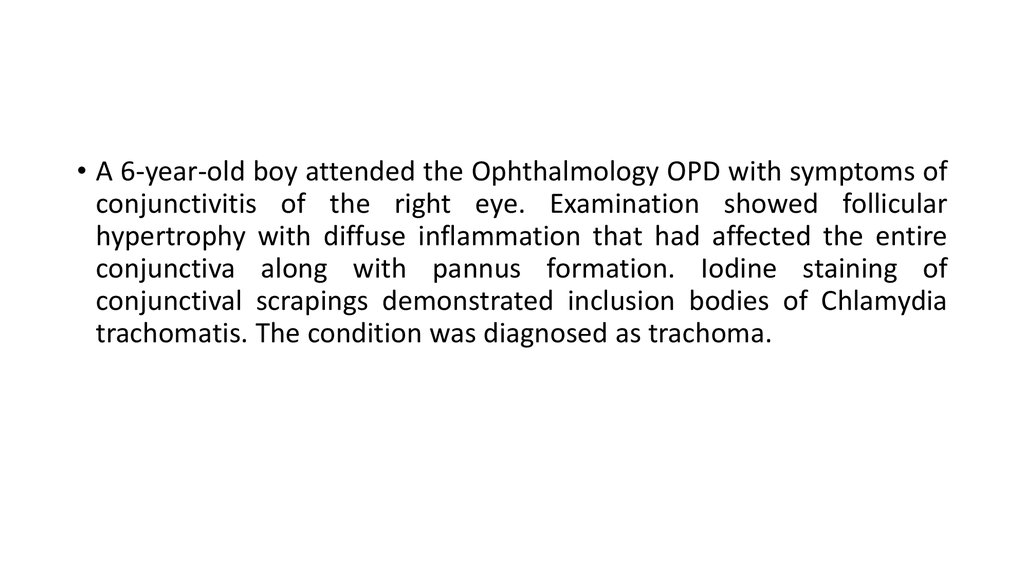
• A 6-year-old boy attended the Ophthalmology OPD with symptoms ofconjunctivitis of the right eye. Examination showed follicular
hypertrophy with diffuse inflammation that had affected the entire
conjunctiva along with pannus formation. Iodine staining of
conjunctival scrapings demonstrated inclusion bodies of Chlamydia
trachomatis. The condition was diagnosed as trachoma.
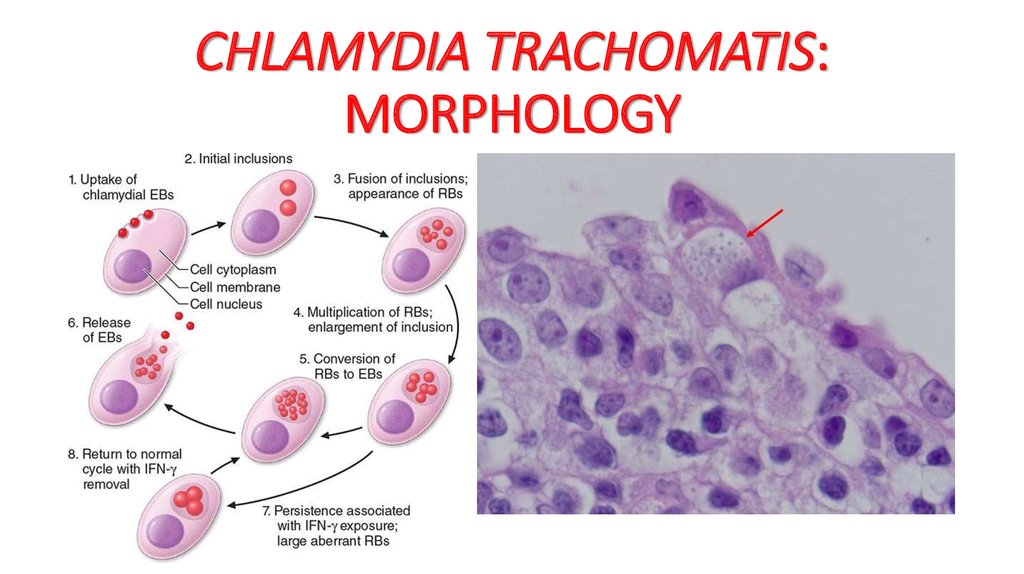
13. CHLAMYDIA TRACHOMATIS: MORPHOLOGY
14. CHLAMYDIA TRACHOMATIS: CULTURE
15. CHLAMYDIA TRACHOMATIS: ANTIGENIC STRUCTURE
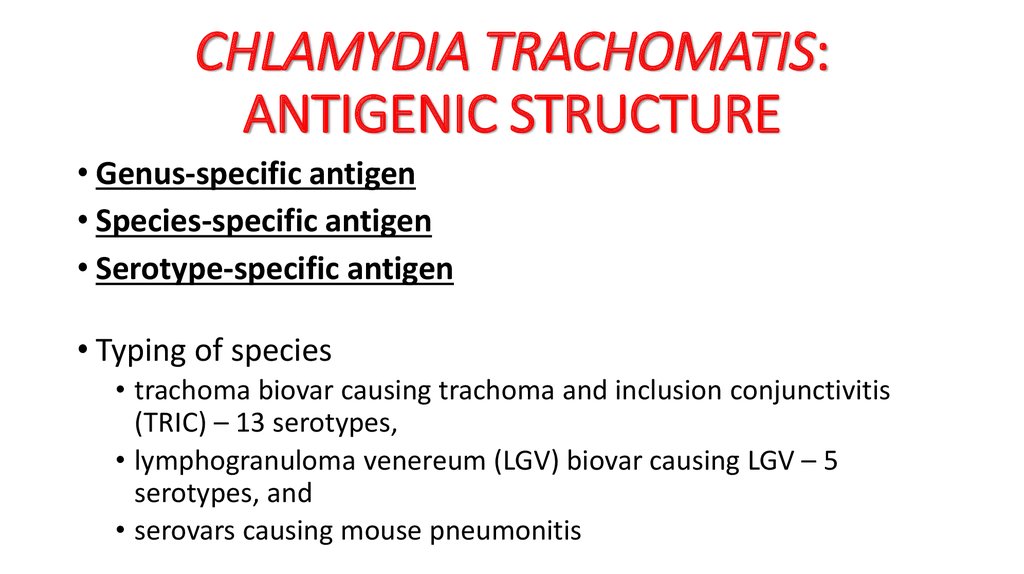
• Genus-specific antigen• Species-specific antigen
• Serotype-specific antigen
• Typing of species
• trachoma biovar causing trachoma and inclusion conjunctivitis
(TRIC) – 13 serotypes,
• lymphogranuloma venereum (LGV) biovar causing LGV – 5
serotypes, and
• serovars causing mouse pneumonitis
16. CHLAMYDIA TRACHOMATIS: VIRULENCE FACTORS
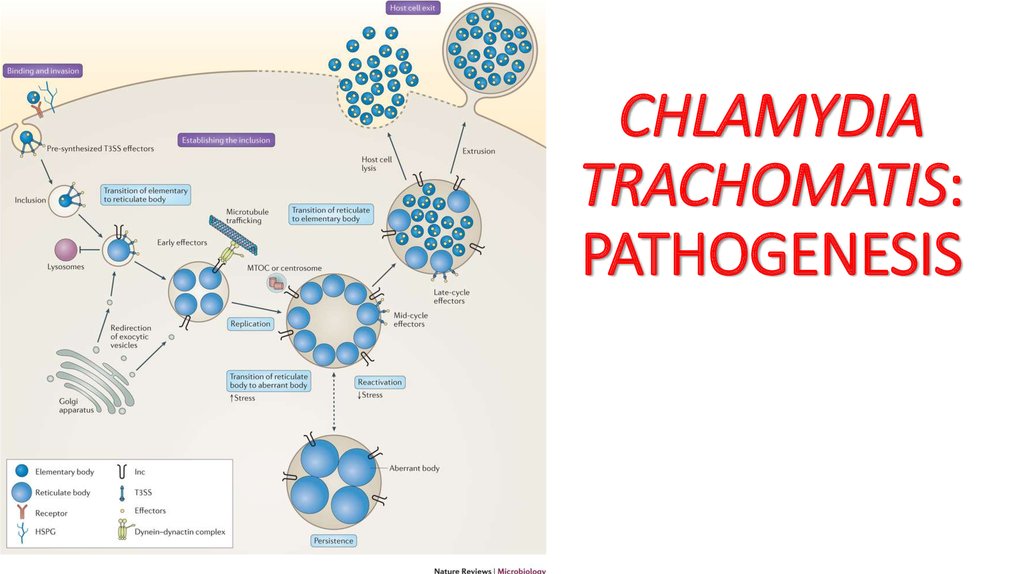
• The ability to multiply intracellularly in the infected cell is the keymechanism of virulence of C. trachomatis.
• The bacteria prevent fusion of phagolysosome with cellular
liposomes, thereby preventing intracellular killing of the bacteria by
the host cell.
• Repeated infections caused by C. trachomatis contribute to pathology
seen in the infected eye in trachoma.
17. CHLAMYDIA TRACHOMATIS: PATHOGENESIS
18. CHLAMYDIA TRACHOMATIS: CLINICAL SYNDROMES
• Lymphogranuloma venereum• Ocular LGV
• Trachoma
• Adult inclusion conjunctivitis
• Neonatal conjunctivitis
• Infant pneumonia
• Urogenital infections
19. CHLAMYDIA TRACHOMATIS: CLINICAL SYNDROMES
20. CHLAMYDIA TRACHOMATIS: LABORATORY DIAGNOSIS
• Microscopy• Culture
• Antigen detection
• Serodiagnosis
• Frei’s skin test
21.
• A 22-year-old female complained of lower abdominal pain on and offfor the last 3 months. She complained of a feeling of heaviness in the
pelvis and pain during sexual intercourse. On examination, a tender
mass was found to the right side during examination. Gram staining of
cervical swab showed plenty of pus cells and a few Gram-negative
cocci. She gave a history of allergy to penicillins.
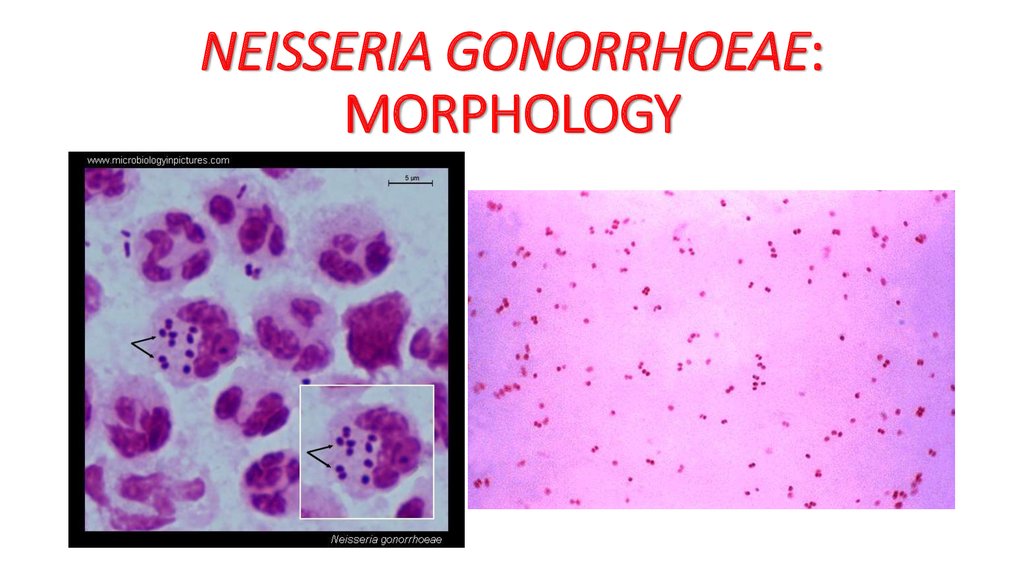
22. NEISSERIA GONORRHOEAE: MORPHOLOGY
23. NEISSERIA GONORRHOEAE: CULTURE
24. NEISSERIA GONORRHOEAE: VIRULENCE FACTORS
25. NEISSERIA GONORRHOEAE: PATHOGENESIS
26. NEISSERIA GONORRHOEAE: CLINICAL SYNDROMES
a)b)
c)
d)
gonorrhea,
disseminated gonococcal infections (DGI),
ophthalmia neonatorum, and
other gonococcal diseases
27. NEISSERIA GONORRHOEAE: LABORATORY DIAGNOSIS
• Microscopy• Culture
• Antigen detection
• SerodiagnosiS
28. NEISSERIA GONORRHOEAE: CLINICAL SYNDROMES
a)b)
c)
d)
gonorrhea,
disseminated gonococcal infections (DGI),
ophthalmia neonatorum, and
other gonococcal diseases
29. NEISSERIA GONORRHOEAE: LABORATORY DIAGNOSIS
• Microscopy• Culture
• Antigen detection
• SerodiagnosiS






 medicine
medicine