Similar presentations:
Copy of DOC-20251016-WA0114._copy
1.
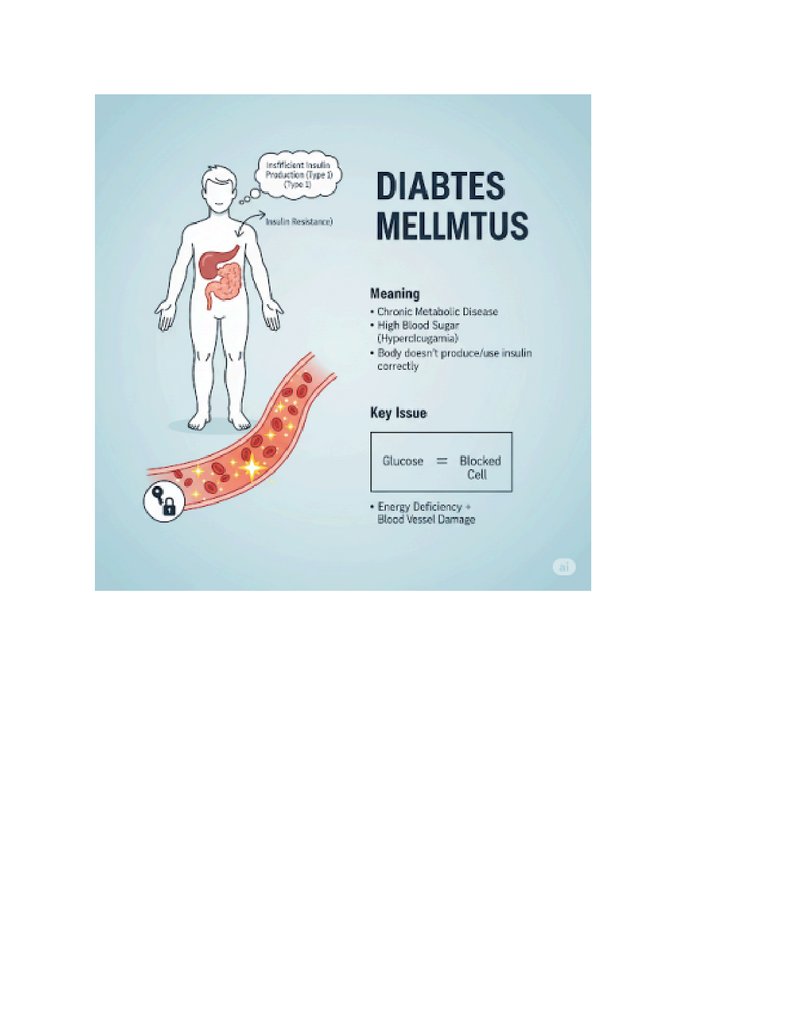
OVERVIEW OF CONDITIONWhat is the meaning of condition?
Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disease characterized
by high blood sugar levels. This occurs either because the body does not produce enough
insulin, or because the body's cells do not respond properly to the insulin that is produced.
Insulin, a hormone made by the pancreas, is essential for regulating blood glucose and allowing
cells to absorb glucose for energy. When glucose cannot enter the cells, it builds up in the
bloodstream, leading to various health problems. There are several types of diabetes, with the
most common being Type 1, Type 2, and Gestational Diabetes.
○ Type 1 Diabetes: An autoimmune condition where the body's immune system attacks and
destroys the insulin-producing beta cells in the pancreas. It typically develops in childhood or
adolescence but can occur at any age. People with Type 1 diabetes require daily insulin
injections to survive.
○ Type 2 Diabetes: The most common form, accounting for about 90% of all diabetes cases. In
Type 2 diabetes, the body either doesn't produce enough insulin or doesn't use insulin
effectively (insulin resistance). It is often linked to lifestyle factors such as obesity, physical
inactivity, and diet, and typically develops in adults, though it is increasingly seen in younger
people
.
○ Gestational Diabetes: A temporary form of diabetes that develops during pregnancy. It
usually resolves after childbirth, but women who have had gestational diabetes are at a higher
risk of developing Type 2 diabetes later in life.
2.
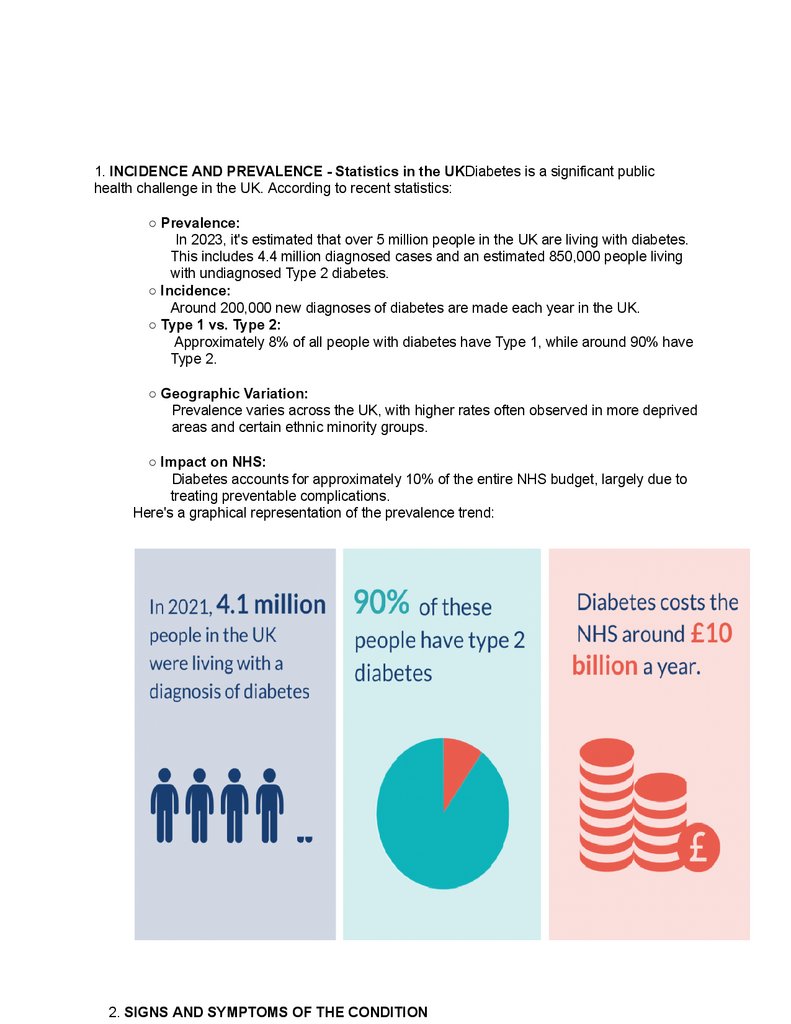
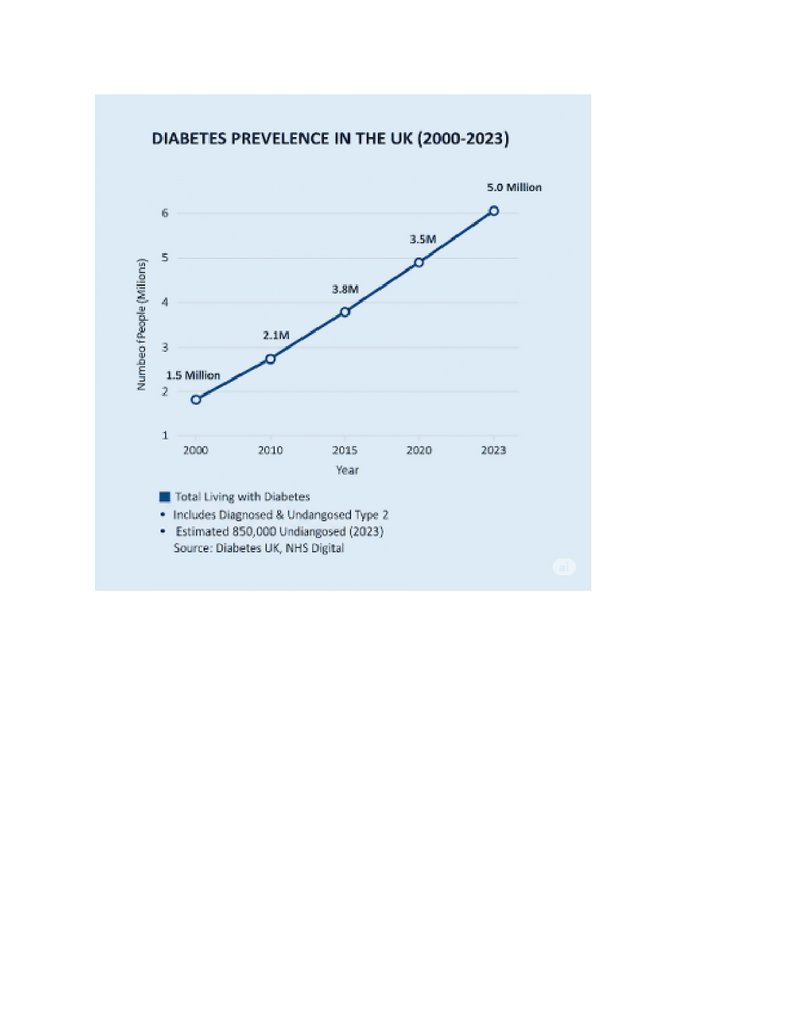
1. INCIDENCE AND PREVALENCE - Statistics in the UKDiabetes is a significant publichealth challenge in the UK. According to recent statistics:
○ Prevalence:
In 2023, it's estimated that over 5 million people in the UK are living with diabetes.
This includes 4.4 million diagnosed cases and an estimated 850,000 people living
with undiagnosed Type 2 diabetes.
○ Incidence:
Around 200,000 new diagnoses of diabetes are made each year in the UK.
○ Type 1 vs. Type 2:
Approximately 8% of all people with diabetes have Type 1, while around 90% have
Type 2.
○ Geographic Variation:
Prevalence varies across the UK, with higher rates often observed in more deprived
areas and certain ethnic minority groups.
○ Impact on NHS:
Diabetes accounts for approximately 10% of the entire NHS budget, largely due to
treating preventable complications.
Here's a graphical representation of the prevalence trend:
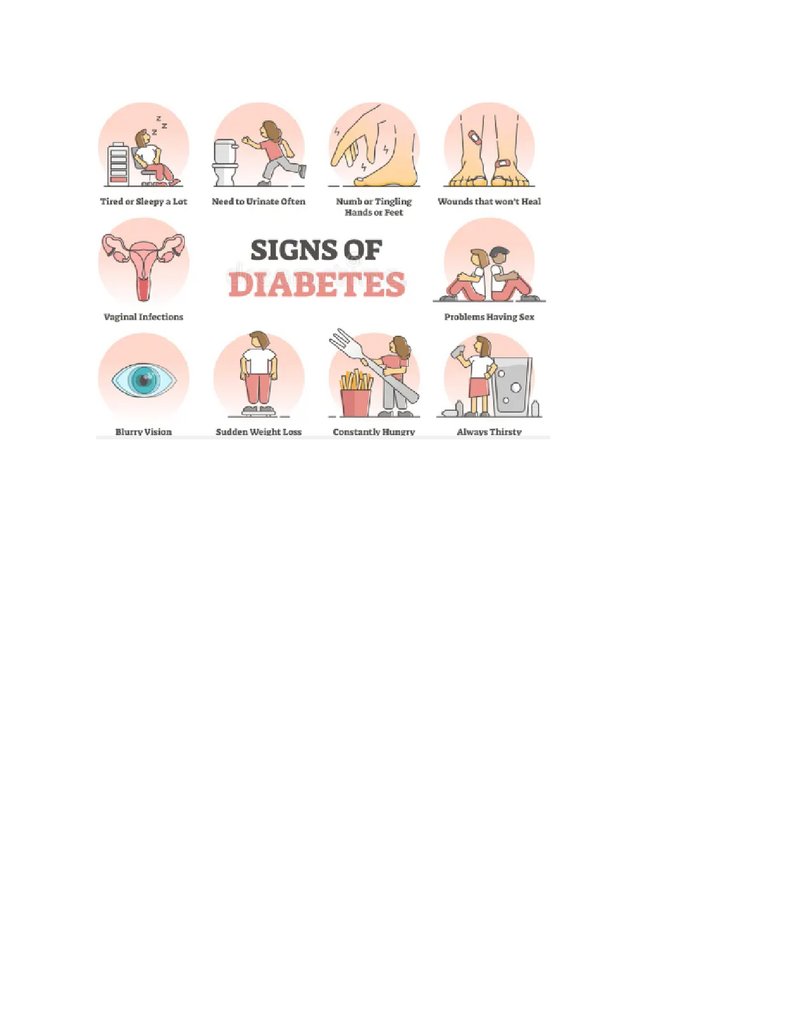
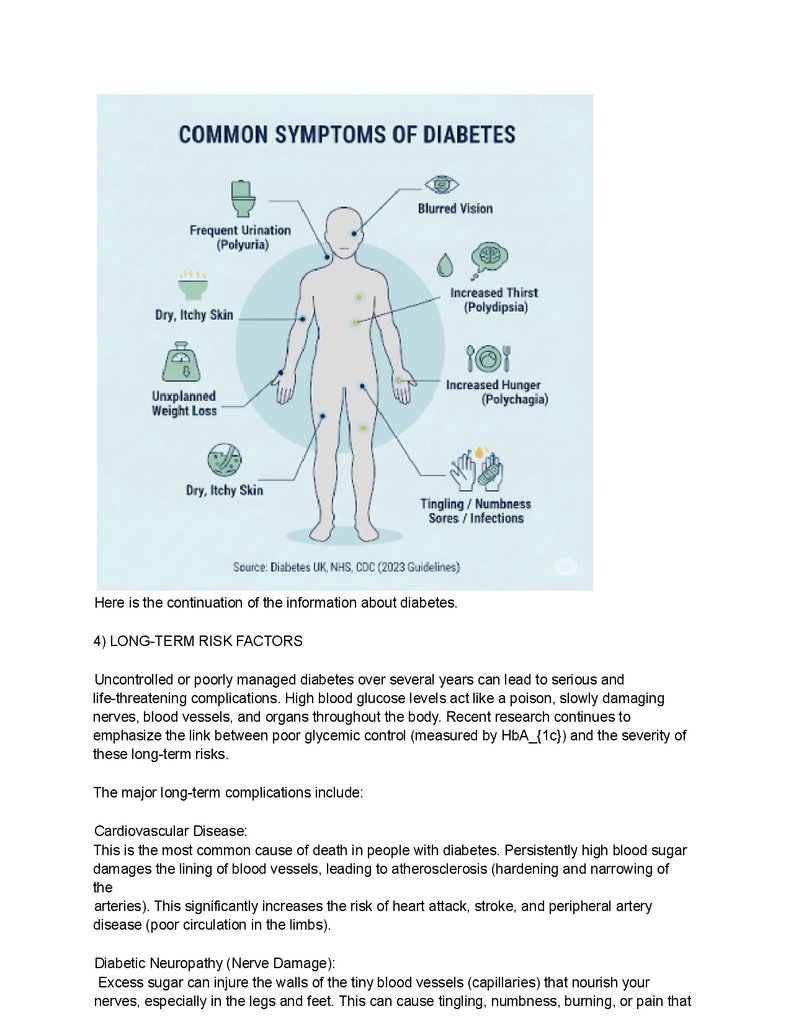
2. SIGNS AND SYMPTOMS OF THE CONDITION
3.
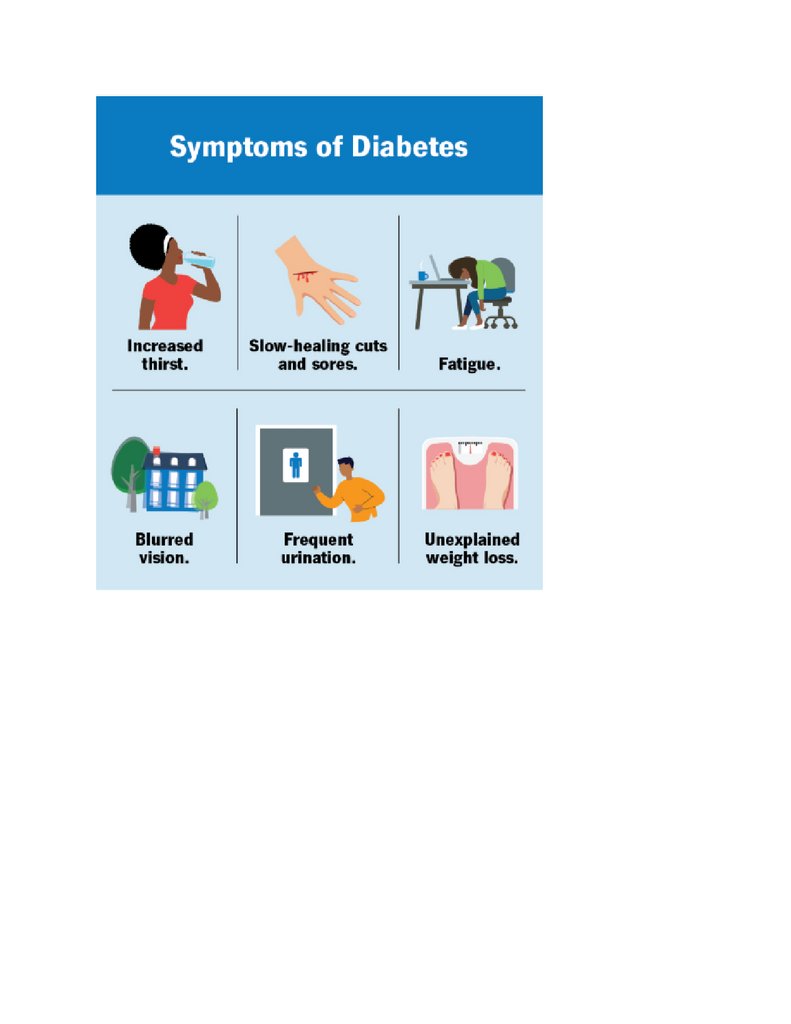
Information from recent articlesRecognizing the signs and symptoms of diabetes iscrucial for early diagnosis and management. While some symptoms are common to both
Type 1 and Type 2 diabetes, the onset can differ. Type 1 symptoms often appear rapidly,
while Type 2 symptoms may develop slowly over years and can be subtle.Based on
recent medical articles and guidelines, the key signs and symptoms include:
○ Frequent Urination (Polyuria): High blood sugar levels cause the kidneys to work
harder to remove excess glucose, leading to increased urine production.
○ Increased Thirst (Polydipsia): Excessive urination causes dehydration, triggering
intense thirst.
○ Increased Hunger (Polyphagia): Despite eating, cells may not be getting enough
glucose for energy, leading to constant hunger.
○ Unexplained Weight Loss:
Especially in Type 1 diabetes, the body starts breaking down muscle and fat for
energy when cells can't access glucose.
○ Fatigue and Lack of Energy:
Cells deprived of glucose cannot function properly, leading to persistent tiredness.
○ Blurred Vision:
High blood sugar can cause fluid to be pulled from the lenses of the eyes, affecting
their ability to focus.
○ Slow-Healing Sores or Frequent Infections:
High blood sugar can impair the immune system and affect circulation, making
wounds heal slowly and increasing susceptibility to infections (e.g., skin infections,
yeast infections).
○ Tingling or Numbness in Hands or Feet (Neuropathy):
Over time, high blood sugar can damage nerves.
○ Dry Skin and Itching:
Can be related to dehydration and poor circulation.
Here's an illustration summarizing these common symptoms:
4.
5.
6.
7.
8.
Here is the continuation of the information about diabetes.4) LONG-TERM RISK FACTORS
Uncontrolled or poorly managed diabetes over several years can lead to serious and
life-threatening complications. High blood glucose levels act like a poison, slowly damaging
nerves, blood vessels, and organs throughout the body. Recent research continues to
emphasize the link between poor glycemic control (measured by HbA_{1c}) and the severity of
these long-term risks.
The major long-term complications include:
Cardiovascular Disease:
This is the most common cause of death in people with diabetes. Persistently high blood sugar
damages the lining of blood vessels, leading to atherosclerosis (hardening and narrowing of
the
arteries). This significantly increases the risk of heart attack, stroke, and peripheral artery
disease (poor circulation in the limbs).
Diabetic Neuropathy (Nerve Damage):
Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your
nerves, especially in the legs and feet. This can cause tingling, numbness, burning, or pain that
9.
usually begins at the tips of the toes or fingers and gradually spreads upward. If left untreated, itcan lead to a complete loss of sensation in the affected limbs.
Diabetic Nephropathy (Kidney Disease):
Diabetes is a leading cause of chronic kidney disease. The high workload of filtering excess
sugar from the blood damages the delicate filtering systems in the kidneys. Over time, this can
lead to kidney failure, requiring dialysis or a kidney transplant.
Diabetic Retinopathy (Eye Damage):
High blood sugar can damage the blood vessels in the retina (the light-sensitive tissue at the
back of the eye). This can lead to vision problems and, if not treated, can cause blindness. It is
a leading cause of blindness in working-age adults.
Foot Damage:
Nerve damage (neuropathy) in the feet and poor blood flow increase the risk of various foot
complications. Minor cuts or blisters can go unnoticed, become infected, and develop into
serious ulcers that are difficult to heal. In severe cases, this can lead to amputation of a toe,
foot, or leg.
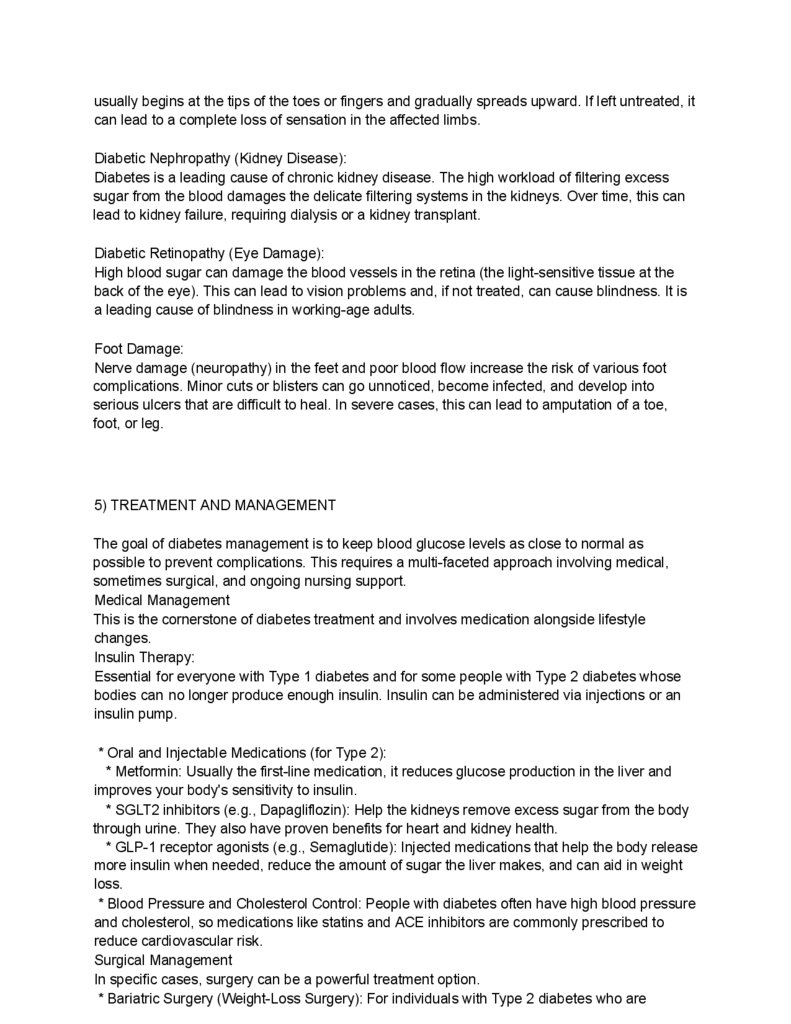
5) TREATMENT AND MANAGEMENT
The goal of diabetes management is to keep blood glucose levels as close to normal as
possible to prevent complications. This requires a multi-faceted approach involving medical,
sometimes surgical, and ongoing nursing support.
Medical Management
This is the cornerstone of diabetes treatment and involves medication alongside lifestyle
changes.
Insulin Therapy:
Essential for everyone with Type 1 diabetes and for some people with Type 2 diabetes whose
bodies can no longer produce enough insulin. Insulin can be administered via injections or an
insulin pump.
* Oral and Injectable Medications (for Type 2):
* Metformin: Usually the first-line medication, it reduces glucose production in the liver and
improves your body's sensitivity to insulin.
* SGLT2 inhibitors (e.g., Dapagliflozin): Help the kidneys remove excess sugar from the body
through urine. They also have proven benefits for heart and kidney health.
* GLP-1 receptor agonists (e.g., Semaglutide): Injected medications that help the body release
more insulin when needed, reduce the amount of sugar the liver makes, and can aid in weight
loss.
* Blood Pressure and Cholesterol Control: People with diabetes often have high blood pressure
and cholesterol, so medications like statins and ACE inhibitors are commonly prescribed to
reduce cardiovascular risk.
Surgical Management
In specific cases, surgery can be a powerful treatment option.
* Bariatric Surgery (Weight-Loss Surgery): For individuals with Type 2 diabetes who are
10.
significantly obese, procedures like a gastric bypass can lead to significant and sustainedremission of diabetes. By altering the digestive system, the surgery promotes weight loss and
improves the body's ability to produce and use insulin.
* Pancreas or Islet Cell Transplantation: A more complex and less common option, usually
reserved for people with very difficult-to-control Type 1 diabetes, often when they are also
receiving a kidney transplant. It involves transplanting a healthy pancreas or just the
insulin-producing islet cells to restore insulin production.
Nursing Management
Nurses, particularly diabetes specialist nurses, play a vital role in patient education and ongoing
support.
* Education: Teaching patients about their condition, how to monitor their blood glucose,
administer medication, and recognize signs of high (hyperglycemia) and low (hypoglycemia)
blood sugar.
* Lifestyle Counseling: Providing guidance on healthy eating, the importance of physical activity,
and strategies for weight management.
* Monitoring and Surveillance: Regularly checking for complications, such as performing routine
foot checks, monitoring blood pressure, and arranging for annual eye screenings. *
Psychosocial Support: Helping patients cope with the emotional and psychological burden of
living with a chronic illness.
11.
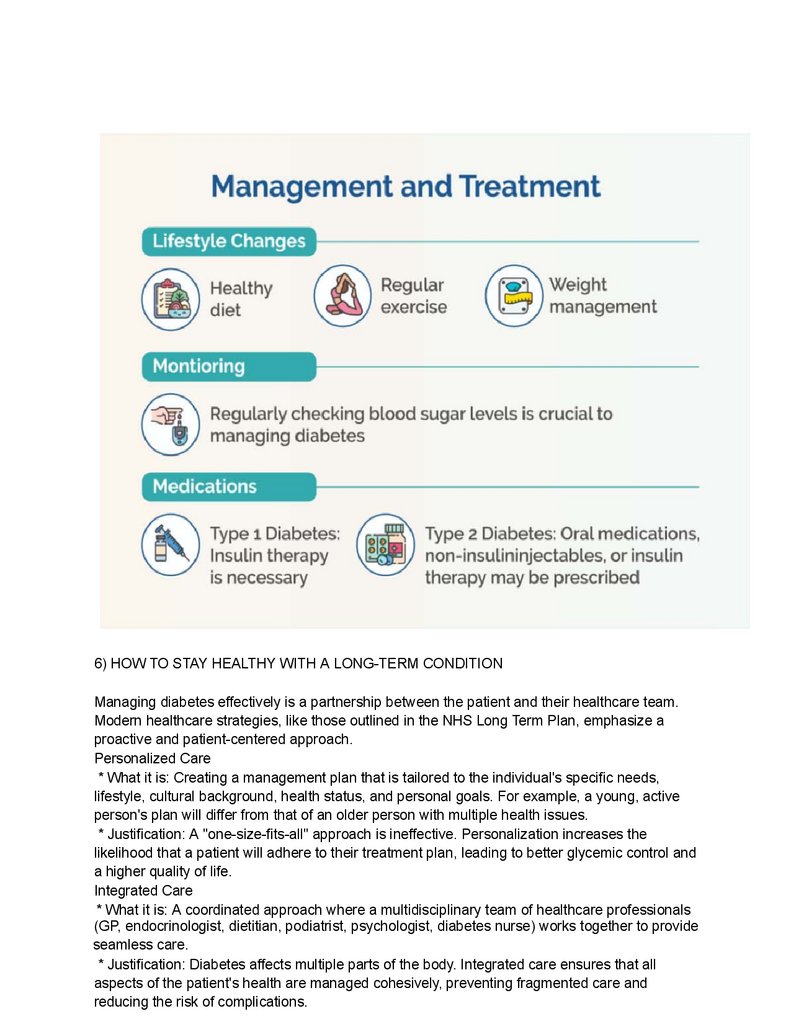
6) HOW TO STAY HEALTHY WITH A LONG-TERM CONDITIONManaging diabetes effectively is a partnership between the patient and their healthcare team.
Modern healthcare strategies, like those outlined in the NHS Long Term Plan, emphasize a
proactive and patient-centered approach.
Personalized Care
* What it is: Creating a management plan that is tailored to the individual's specific needs,
lifestyle, cultural background, health status, and personal goals. For example, a young, active
person's plan will differ from that of an older person with multiple health issues.
* Justification: A "one-size-fits-all" approach is ineffective. Personalization increases the
likelihood that a patient will adhere to their treatment plan, leading to better glycemic control and
a higher quality of life.
Integrated Care
* What it is: A coordinated approach where a multidisciplinary team of healthcare professionals
(GP, endocrinologist, dietitian, podiatrist, psychologist, diabetes nurse) works together to provide
seamless care.
* Justification: Diabetes affects multiple parts of the body. Integrated care ensures that all
aspects of the patient's health are managed cohesively, preventing fragmented care and
reducing the risk of complications.
12.
Shared Decision Making* What it is: A collaborative process where the clinician provides information on treatment
options, risks, and benefits, and the patient shares their values, preferences, and what's
important to them. Together, they make a decision about the best course of action.
* Justification: This process respects patient autonomy and empowers them to take an active
role in their health. Patients who are involved in decisions about their care are more likely to be
satisfied and follow the agreed-upon plan.
Collaborative Care Planning
* What it is: The practical outcome of shared decision-making. The patient and their healthcare
professional jointly create a written plan that outlines health goals (e.g., target HbA_{1c} level,
weight loss goal) and the steps to achieve them.
* Justification: A formal plan provides a clear roadmap for the patient, making goals tangible
and actionable. It serves as a reference point to track progress and make adjustments as
needed.
Self-Care Tips and Health Education
This is the most critical component, as the patient manages their condition 99% of the time.
* Healthy Eating: Focus on a balanced diet rich in whole grains, fruits, vegetables, and lean
protein. Limit processed foods, sugary drinks, and saturated fats. A dietitian can provide a
tailored meal plan.
* Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise (like
brisk walking, cycling, or swimming) per week. Exercise helps lower blood sugar and improves
insulin sensitivity.
* Blood Glucose Monitoring: Regularly check blood sugar levels as advised by your healthcare
team to understand how food, activity, and medication affect them.
* Medication Adherence: Take all medications, including insulin, exactly as prescribed. *
Foot Care: Check your feet every day for cuts, sores, or changes in colour. Wash and dry
them carefully and wear well-fitting shoes.
* Regular Check-ups: Attend all appointments, including annual eye screenings and kidney
function tests.
* Justification: Empowering patients with knowledge and skills for self-care is the single most
effective strategy for preventing long-term complications and maintaining a good quality of life.
Daily decisions have the biggest impact on overall health outcomes.
13.
7) CONCLUSIONDiabetes is a complex and demanding chronic condition, but it does not have to be a life
sentence of poor health. With the right knowledge, support, and personal commitment,
individuals with diabetes can live long, healthy, and fulfilling lives. The modern approach to
care,
centered on personalization, collaboration, and patient empowerment, has transformed diabetes
management from a simple prescription of medicine to a holistic partnership in health. The focus
14.
is shifting from simply treating high blood sugar to proactively preventing the devastatingcomplications it can cause.
"The greatest medicine of all is to teach people how not to need it."
Ultimately, managing diabetes is a journey, not a destination. It requires daily attention, but the
rewards—a life free from complications—are immeasurable. As the old saying wisely states:
"Prevention is better than cure."
8) REFERENCES (APA 7th Edition)
American Diabetes Association. (2024). Standards of care in diabetes—2024. Diabetes Care,
47(Supplement 1).
https://diabetesjournals.org/care/issue/47/Supplement_1
Diabetes UK. (2024). Diabetes statistics.
https://www.diabetes.org.uk/professionals/position-statements-reports/statistics National Health
Service. (2023). Diabetes. NHS.uk. https://www.nhs.uk/conditions/diabetes/ National Institute
for Health and Care Excellence. (2022). Type 2 diabetes in adults: management (NICE
Guideline NG28). https://www.nice.org.uk/guidance/ng28 Holman, N., Young, B., & Gadsby, R.
(2023). Current prevalence of Type 1 and Type 2 diabetes in adults: Estimates from the UK
Biobank. Diabetic Medicine, 40(4), e15048. https://doi.org/10.1111/dme.15048
Word count report