Similar presentations:
Early tirofiban infusion after intravenous thrombolysis for acute ischemic stroke
1.
EARLY TIROFIBAN INFUSION AFTERINTRAVENOUS THROMBOLYSIS FOR
ACUTE ISCHEMIC STROKE: ASSET-IT
TRIAL
2.
CONTENT01. Trial Identification: Phase 3, multicenter,
double-blind, randomized, placebo-controlled
trial (NCT06134622)
02. Objective: Evaluate whether early
intravenous tirofiban after thrombolysis
improves functional outcomes in acute ischemic
noncardioembolic stroke.
03. Population: Adults with acute ischemic
noncardioembolic stroke, within 4.5 hours of
onset, not eligible for thrombectomy.
04. Intervention: 24-hour tirofiban infusion
initiated within 60 minutes after thrombolysis.
05. Control: Placebo infusion, identical in
appearance and administration timing.
06. Primary Outcome: Excellent functional
outcome (modified Rankin scale score 0–1) at
90 days.
07. Key Safety Outcomes: Symptomatic
intracranial hemorrhage within 36 hours;
mortality at 90 days.
08. Main Finding: Tirofiban increased likelihood
of excellent functional recovery (65.9% vs
54.9%; RR 1.20; P=0.001) with a low but higher
rate of intracranial hemorrhage.
3.
Why Investigate Early Tirofiban afterThrombolysis?
Burden of Disease
• Acute ischemic stroke is the leading cause of death in china and a major cause globally.
• Despite thrombolysis within 4.5 hours, only ~50% achieve excellent functional outcomes
(mRS 0–1).
Problem with Current Treatment:
• Vascular reocclusion can occur after thrombolysis, compromising recovery.
• No standard early antiplatelet strategy exists within the first 24 hours post-thrombolysis
due to bleeding risk.
Rationale for Tirofiban:
• Potent, rapid-onset glycoprotein IIb/IIIa antagonist.
• Prevents platelet aggregation, reduces macrovascular reocclusion, and improves
cerebral blood flow in experimental models.
Previous Evidence Gaps:
• Earlier tirofiban studies were small, single-center, or observational, with inconclusive
results.
Study Hypothesis:
• Early tirofiban after thrombolysis in noncardioembolic stroke will improve functional
outcomes without significantly increasing serious bleeding.
4.
ASSET-IT TrialObjectives and Hypotheses
Primary Objective:
• To determine whether early intravenous tirofiban infusion after
standard intravenous thrombolysis improves the rate of
excellent functional outcome (mRS 0–1 at 90 days) in acute
ischemic noncardioembolic stroke.
Secondary Objectives:
• Assess effect on overall functional status distribution (ordinal
mRS shift analysis).
• Evaluate impact on functional independence (mRS 0–2) and
ability to ambulate or perform self-care (mRS 0–3).
• Assess changes in neurological deficits (NIHSS at 24–72 hours
and day 5–7/discharge).
• Measure quality of life (EQ-5D-5L) and daily living independence
(Barthel Index) at 90 days.
• Evaluate safety outcomes, including bleeding events and
mortality.
Primary Hypothesis:
• Early tirofiban infusion after thrombolysis increases the
proportion of patients achieving mRS 0–1 at 90 days
compared with placebo.
Safety Hypothesis:
• Early tirofiban will not significantly increase
symptomatic intracranial hemorrhage or mortality
compared to placebo.
5.
What is biochemistry?Design Type:
• Phase 3, multicenter, double-blind, randomized, placebo-controlled, parallel-group trial.
Setting:
• Conducted at 38 hospitals across China.
Participants:
• Adults (≥18 years) with acute ischemic noncardioembolic stroke within 4.5 hours of onset.
• Not eligible for mechanical thrombectomy.
Randomization:
• 1:1 allocation to tirofiban or placebo, stratified by trial center.
Blinding:
• Patients, treating clinicians, outcome assessors, and trial statisticians were blinded to treatment allocation.
Follow-up Duration:
• Clinical and imaging follow-up through 90 days post-randomization.
Protocol Compliance:
• Conducted per Declaration of Helsinki and ICH-GCP guidelines.
• Written informed consent obtained before enrollment.
Trial Oversight:
• Independent Data and Safety Monitoring Board.
• Independent Clinical-Events Committee adjudicated efficacy and safety endpoints.
6.
Participant Eligibility CriteriaInclusion Criteria:
• Age ≥18 years.
• Acute ischemic noncardioembolic stroke.
• Received intravenous thrombolysis (alteplase or tenecteplase) within
4.5 hours of symptom onset (or last known well).
• NIHSS score 4–25 at time of thrombolysis.
• Randomization within 55 minutes after thrombolysis completion.
• Tirofiban or placebo started within 5 minutes after randomization.
Exclusion Criteria:
• Prestroke disability score >1 on modified Rankin scale.
• History or ECG evidence of atrial fibrillation.
• Planned mechanical thrombectomy or other endovascular treatment.
• Intracranial hemorrhage on baseline imaging.
• Other clinical or imaging findings deemed unsafe for trial participation.
Ethnicity:
• Majority Han Chinese (n=830); small minority Hui (n=2).
7.
Where Was ASSET-IT Conducted?Geographic Scope:
Trial Coordination:
• Conducted across 38 medical
centers in China.
• Central coordination by the First
Affiliated Hospital of the University
of Science and Technology of China
(USTC).
Type of Facilities:
Neuroimaging:
• Large tertiary hospitals and
regional stroke centers with acute
stroke care capabilities.
• Baseline imaging with noncontrast
CT or MRI to exclude hemorrhage.
• Vascular imaging (CT angiography
or MR angiography) at treating
physician’s discretion.
• Imaging review performed by a
blinded independent core
laboratory.
Outcome Assessments:
• Functional outcomes assessed
via structured interviews by
centrally trained, blinded
evaluators.
• Voice recordings used to verify
mRS scoring.
Trial Oversight Infrastructure:
• Independent Data & Safety
Monitoring Board.
• Independent Clinical-Events
Committee for endpoint
adjudication.
8.
Treatment Protocol in ASSET-ITIntervention Group:
• Tirofiban intravenous infusion.
• Loading dose: 0.4 μg/kg/min for 30 minutes.
• Maintenance: 0.1 μg/kg/min for 23.5 hours.
• Started within 5 minutes of randomization (≤60 min after thrombolysis).
Control Group:
• Placebo infusion (0.9% saline) identical in appearance, volume, and rate to tirofiban regimen.
Post-Infusion Management (Both Groups):
• Discontinuation of infusion at exactly 24 hours.
• Subsequent care per national and international acute stroke management guidelines.
• Antiplatelet therapy initiated 24 hours after thrombolysis (monotherapy or dual therapy at clinician’s discretion).
Thrombolytic Agents Used Prior to Randomization:
• Alteplase: ~75% of patients.
• Tenecteplase: ~25% of patients.
Blinding Measures:
• Infusion solutions identical; trial staff and patients blinded to group allocation.
9.
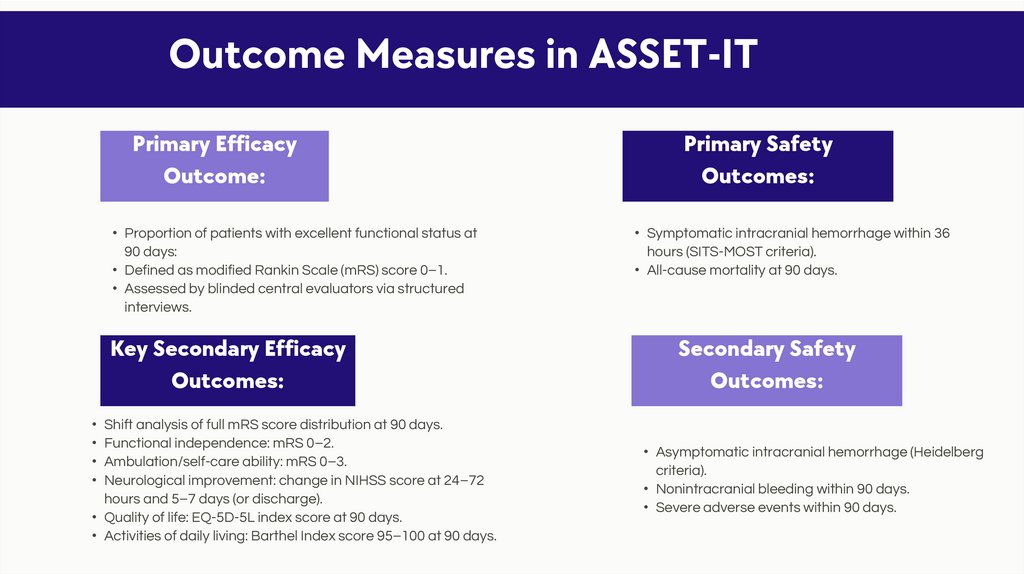
Outcome Measures in ASSET-ITPrimary Efficacy
Outcome:
• Proportion of patients with excellent functional status at
90 days:
• Defined as modified Rankin Scale (mRS) score 0–1.
• Assessed by blinded central evaluators via structured
interviews.
Key Secondary Efficacy
Outcomes:
• Shift analysis of full mRS score distribution at 90 days.
• Functional independence: mRS 0–2.
• Ambulation/self-care ability: mRS 0–3.
• Neurological improvement: change in NIHSS score at 24–72
hours and 5–7 days (or discharge).
• Quality of life: EQ-5D-5L index score at 90 days.
• Activities of daily living: Barthel Index score 95–100 at 90 days.
Primary Safety
Outcomes:
• Symptomatic intracranial hemorrhage within 36
hours (SITS-MOST criteria).
• All-cause mortality at 90 days.
Secondary Safety
Outcomes:
• Asymptomatic intracranial hemorrhage (Heidelberg
criteria).
• Nonintracranial bleeding within 90 days.
• Severe adverse events within 90 days.
10.
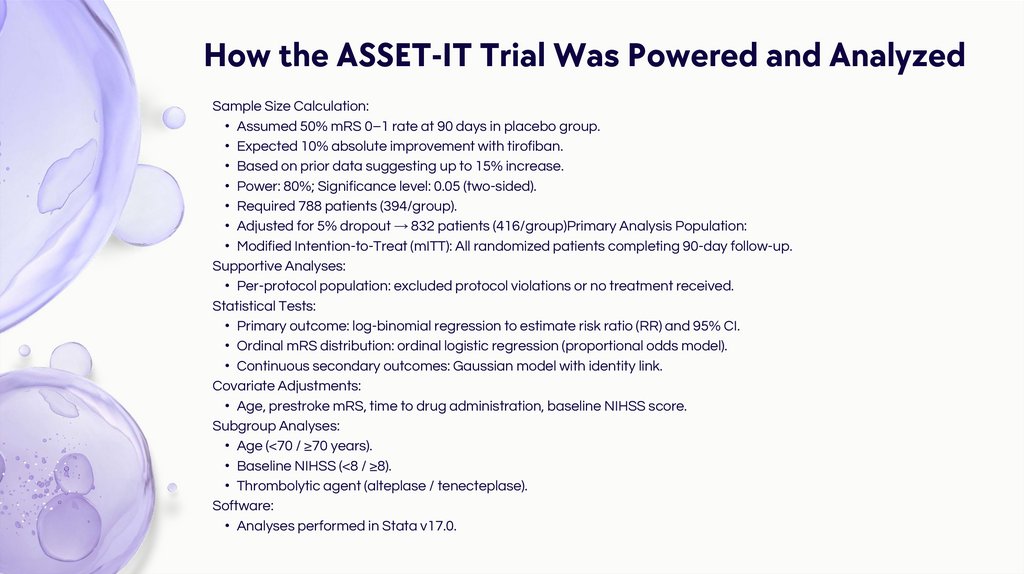
How the ASSET-IT Trial Was Powered and AnalyzedSample Size Calculation:
• Assumed 50% mRS 0–1 rate at 90 days in placebo group.
• Expected 10% absolute improvement with tirofiban.
• Based on prior data suggesting up to 15% increase.
• Power: 80%; Significance level: 0.05 (two-sided).
• Required 788 patients (394/group).
• Adjusted for 5% dropout → 832 patients (416/group)Primary Analysis Population:
• Modified Intention-to-Treat (mITT): All randomized patients completing 90-day follow-up.
Supportive Analyses:
• Per-protocol population: excluded protocol violations or no treatment received.
Statistical Tests:
• Primary outcome: log-binomial regression to estimate risk ratio (RR) and 95% CI.
• Ordinal mRS distribution: ordinal logistic regression (proportional odds model).
• Continuous secondary outcomes: Gaussian model with identity link.
Covariate Adjustments:
• Age, prestroke mRS, time to drug administration, baseline NIHSS score.
Subgroup Analyses:
• Age (<70 / ≥70 years).
• Baseline NIHSS (<8 / ≥8).
• Thrombolytic agent (alteplase / tenecteplase).
Software:
• Analyses performed in Stata v17.0.
11.
Ensuring Unbiased TreatmentAssignment in ASSET-IT
Randomization Method:
• Centralized system, stratified by trial center.
• 1:1 allocation to tirofiban or placebo.
Allocation Concealment:
• Randomization sequence concealed from enrolling clinicians and patients until assignment.
• Sealed electronic allocation to prevent prediction or manipulation.
Blinding:
• Participants: unaware of group assignment.
• Treating clinicians: blinded to treatment identity.
• Outcome assessors: blinded central evaluators using structured, voice-recorded mRS interviews.
• Data analysts: blinded to group codes during analysis.
Intervention Masking:
• Tirofiban and placebo infusions were visually identical in appearance, volume, and administration rate.
Maintenance of Blinding:
• Independent data and safety monitoring board had sole access to unblinded safety data.
• Clinical-events committee adjudicated endpoints without knowledge of treatment group.
12.
Enrollment and Allocation inASSET-IT
Screening:
• 1,699 patients assessed for eligibility (March–September 2024).
Randomization:
• 832 patients randomized:
⚬ Tirofiban group: 414
⚬ Placebo group: 418
Treatment:
• All randomized patients received assigned infusion.
Follow-up:
• 90-day follow-up completed for 831 patients.
• 1 patient in placebo group lost to follow-up.
Analysis Populations:
• Modified Intention-to-Treat (mITT): 831 patients (all randomized with 90-day outcome).
• Per-protocol: excluded patients with eligibility violations or no infusion received (numbers not
specified in abstract).
CONSORT Flow Diagram Elements:
• Enrollment → Randomization → Allocation to Intervention/Control → Follow-up → Analysis.
13.
When and How ASSET-IT Was Conducted• Recruitment Period:
• Trial Duration:
• March 14, 2024 –
September 25, 2024.
• Each participant followed
for 90 days postrandomization.
• Completion Status:
• Geographic Scope:
• Recruitment completed as
planned; trial not stopped
early.
• 38 centers across China
contributed patients within
recruitment timeframe.
• Follow-Up Windows:
• Primary outcome assessed
at day 90 (±14 days).
• Safety monitoring through
day 90.
• Neurological assessments
at 24–72 hours, and day 5–
7 (or discharge).
• Trial Coordination:
• Central monitoring ensured
protocol adherence across
all sites.
14.
Patient Profile at Randomization• Demographics:
• Median age: 69 years (IQR 59–76) in both groups.
• Female sex: ~36% overall.
• Pre-Stroke Function:
• Prestroke mRS score 1: 6.8% (tirofiban) vs 3.8%
(placebo).
• Stroke Severity at Baseline:
• Median NIHSS score: 6 (IQR 5–9) in both groups.
• Median NCCT ASPECTS score: 10 (IQR 9–10).
• Stroke Etiology:
• Large-artery atherosclerosis: 59.7% (tirofiban) vs
56.7% (placebo).
• Small-artery occlusion: ~34% in both groups.
• Undetermined cause: ~6% in both groups.
• Medical History:
• Hypertension: ~81% overall.
• Diabetes mellitus: ~23% overall.
• Previous stroke/TIA: ~28% overall.
• Hyperlipidemia: ~13% overall.
• Thrombolysis Details:
• Alteplase: ~75% of patients.
• Tenecteplase: ~25% of patients.
• Median onset-to-needle time: 155 min (tirofiban) vs
170 min (placebo).
15.
Who Was Included in the Analyses?• Primary Analysis Set:
• Outcome Data Availability:
• Modified Intention-to-Treat (mITT):
• Included all randomized patients with 90-day followup.
• Tirofiban: 414 patients.
• Placebo: 417 patients (1 lost to follow-up).
• No missing data for covariates in primary analysis.
• Sensitivity analysis for single missing outcome
used best- and worst-case scenarios.
• Per-Protocol Analysis:
• Excluded patients with eligibility violations or who
did not receive assigned treatment.
• Results consistent with mITT findings (exact counts
not detailed in abstract).
• Safety Analysis Set:
• All patients who received any amount of assigned
infusion.
• Analysis Method:
• Outcomes analyzed according to original group
allocation, regardless of treatment adherence
(intention-to-treat principle).
16.
Effect of Early Tirofiban on Excellent FunctionalOutcome
Primary Outcome:
• mRS score 0–1 at 90 days (excellent functional status).
Results:
• Tirofiban: 65.9% of patients.
• Placebo: 54.9% of patients.
• Absolute difference: +11.0 percentage points.
• Relative effect: Risk Ratio (RR) 1.20.
• 95% Confidence Interval: 1.07 to 1.34.
• P-value: 0.001 (statistically significant).
Interpretation:
• Early tirofiban infusion significantly increased the likelihood of excellent recovery compared with placebo in
noncardioembolic ischemic stroke post-thrombolysis.
Consistency:
• Effect persisted across supportive per-protocol analysis.
17.
Additional Functional and NeurologicalOutcomes
mRS Shift Analysis (90 days):
• Common Odds Ratio (COR) favored tirofiban — indicating better overall functional distribution (exact value in full
text).
Functional Independence (mRS 0–2):
• Higher in tirofiban group vs placebo.
Self-Care/Ambulation (mRS 0–3):
• Greater proportion achieved in tirofiban group.
Neurological Improvement (NIHSS):
• Greater median improvement at 24–72 hours and day 5–7/discharge with tirofiban.
Quality of Life (EQ-5D-5L Index at 90 days):
• Higher mean scores in tirofiban group, indicating better quality of life.
Activities of Daily Living (Barthel Index 95–100 at 90 days):
• More patients achieved near-complete independence with tirofiban.
Note on Interpretation:
• Secondary analyses were not adjusted for multiple comparisons; findings are supportive but exploratory.
18.
Safety Profile — Symptomatic ICH &Mortality
Symptomatic Intracranial Hemorrhage
(within 36 hours):
• Tirofiban: 1.7% of patients.
• Placebo: 0%.
• All cases adjudicated using modified SITS-MOST criteria.
All-Cause Mortality (at 90 days):
• Tirofiban: 4.1%.
• Placebo: 3.8%.
Interpretation:
• While symptomatic ICH occurred only in the tirofiban group, incidence was
low.
• No significant difference in mortality between groups.
Oversight:
• Independent Data and Safety Monitoring Board reviewed all safety events.
• Clinical-events committee performed blinded adjudication.
19.
Other Bleeding and AdverseEvents
Asymptomatic Intracranial Hemorrhage (ICH):
• Detected on follow-up imaging per Heidelberg criteria.
• Occurred in both groups at low rates (exact numbers in full text).
Non-Intracranial Bleeding (within 90 days):
• Included gastrointestinal and other systemic bleeding.
• Rates were low and similar between groups.
Severe Adverse Events (SAEs) within 90 days:
• Occurred in both groups; no major imbalance noted.
Hemorrhage Classification:
• Parenchymal hemorrhage types 1 & 2, hemorrhagic infarction types 1 & 2, and remote hemorrhage
categories used for classification.
Clinical Implication:
• Tirofiban increased symptomatic ICH risk modestly but did not substantially raise other serious bleeding
or non-bleeding adverse events.
20.
Effect of Tirofiban Across PatientSubgroups
Prespecified Subgroups:
• Age: <70 years vs ≥70 years.
• Baseline NIHSS: <8 vs ≥8.
• Thrombolytic Agent: Alteplase vs Tenecteplase.
Findings:
• Treatment effect on mRS 0–1 at 90 days generally consistent across subgroups.
• No statistically significant interaction between subgroup characteristics and treatment effect.
Notable Trends:
• Slightly greater absolute benefit in younger patients and those with milder baseline NIHSS scores, though not formally
significant.
• Similar relative benefit observed regardless of thrombolytic agent used.
Interpretation Caution:
• Subgroup analyses were exploratory; trial not powered to detect definitive subgroup-treatment interactions.
21.
Potential Constraints in Interpreting ASSET-ITFindings
Geographic Limitation:
• Conducted exclusively in China; results may not fully generalize to other populations or
healthcare systems.
Stroke Subtype Restriction:
• Included only noncardioembolic ischemic strokes; findings not applicable to cardioembolic
cases.
Treatment Eligibility:
• Excluded patients eligible for mechanical thrombectomy; limits applicability to broader stroke
populations.
Safety Events:
• Symptomatic intracranial hemorrhage rare but only occurred in tirofiban group — requires
careful consideration in practice.
Duration of Follow-Up:
• Outcomes measured at 90 days; no data on longer-term efficacy or safety.
Secondary Analyses:
• Not adjusted for multiple comparisons; secondary results should be interpreted as
exploratory.
Operational Factors:
• Variability in baseline vascular imaging practices and antiplatelet regimens after 24 hours
could influence outcomes.
22.
Applicability of ASSET-IT Results• Population:
• Findings most applicable to
adults with acute ischemic
noncardioembolic stroke,
treated with thrombolysis within
4.5 hours, and not eligible for
thrombectomy.
• Healthcare Setting:
• Conducted in high-volume stroke
centers in China with rapid imaging
and treatment capabilities.
• Generalisation to lower-resource
settings should consider differences
in infrastructure, imaging, and postthrombolysis care.
• Ethnicity:
• Treatment Protocol:
• Predominantly Han Chinese
population; potential differences in
genetic, environmental, and riskfactor profiles in other ethnicities.
Requires rapid infusion initiation
(<60 min post-thrombolysis), which
may not be feasible in all clinical
environments.
• Thrombolytic Agents:
• Overall:
• Both alteplase and
tenecteplase used; similar
benefit observed across
agents, supporting broader
applicability.
• Results are relevant for wellequipped stroke units globally,
but careful adaptation needed
in diverse clinical and
geographic contexts.
23.
What the ASSET-IT Trial Tells UsEfficacy:
• Early tirofiban infusion after intravenous thrombolysis significantly increased the proportion of patients achieving
excellent functional outcome at 90 days.
Safety:
• Low absolute rate of symptomatic intracranial hemorrhage, but events occurred only in the tirofiban group.
• No significant mortality difference between groups.
Mechanistic Implication:
• Supports the concept that early, potent platelet inhibition can reduce post-thrombolysis vascular reocclusion and
improve recovery.
Comparison to Previous Evidence:
• Confirms and strengthens findings from smaller, earlier studies showing potential benefit of tirofiban in acute ischemic
stroke.
Clinical Implication:
• May offer an additional therapeutic strategy for noncardioembolic stroke patients ineligible for thrombectomy.
Caution:
• Wider adoption should await confirmation in diverse populations and settings, and further evaluation of hemorrhage risk.
24.
Key Takeaways from ASSETITMain Finding:
• Early intravenous tirofiban after thrombolysis in acute ischemic noncardioembolic stroke improved
excellent functional recovery at 90 days.
Efficacy–Safety Balance:
• Benefit achieved with a low but higher incidence of symptomatic intracranial hemorrhage in tirofiban
group.
• Mortality unchanged between groups.
Clinical Relevance:
• Adds evidence for early potent antiplatelet therapy post-thrombolysis when thrombectomy is not an
option.
Practice Consideration:
• Requires rapid initiation post-thrombolysis and careful patient selection.
Future Needs:
• Multinational trials to assess reproducibility in other populations and healthcare systems.
• Longer follow-up to determine durability of benefits and late safety events.
25.
Who Supported ASSETIT?Funding Source:
• Supported by the Fundamental Research Funds for the Central Universities.
Role of Funder:
• No role in trial design, data collection, analysis, interpretation, or manuscript
preparation.
Conflict of Interest Declarations:
• Authors reported no relevant conflicts of interest related to the trial intervention.
Trial Registration:
• ClinicalTrials.gov Identifier: NCT06134622.
Ethics & Oversight:
• Conducted in accordance with the Declaration of Helsinki and ICH-GCP standards.
• Approved by ethics committees at all participating centers.
26.
ASSET-IT in aTrial Overview:
Nutshell
• Phase 3, double-blind, multicenter RCT in China.
• Tested early tirofiban infusion after thrombolysis in acute ischemic noncardioembolic stroke.
Key Results:
• Efficacy: Significant improvement in excellent functional recovery (mRS 0–1 at 90 days).
• Safety: Slightly increased symptomatic ICH risk; no difference in mortality.
Clinical Message:
• Early, potent platelet inhibition post-thrombolysis may reduce reocclusion and improve recovery in selected patients.
• Not a replacement for thrombectomy — applies to those ineligible for mechanical reperfusion.
Implementation Considerations:
• Requires rapid workflow (<60 min post-thrombolysis).
• Careful hemorrhage risk assessment is essential.
Next Steps:
• Validation in multinational, diverse cohorts.
• Long-term outcome and safety monitoring.
Bottom Line:
• ASSET-IT provides promising evidence that tirofiban, started promptly after thrombolysis, can meaningfully improve
outcomes in a high-risk stroke population.

 medicine
medicine








