Similar presentations:
Goodpasture syndrome
1.
GoodpastureSyndrome
2.
DEFINITION• A disease of the glomerular and alveolar basement
membranes, characterized by pulmonary
hemorrhage and crescentic glomerulonephritis.
• It’s associated with serum antibodies to glomerular
basement membrane and linear deposits of
antibodies along the glomerular and alveolar
basement membrane and may result in rapidly
progressive glomerulonephritis
3.
Goodpasture disease vsGoodpasture syndrome
• Goodpasture disease is characterized
by the presence of antibodies to
glomerular basement membrane.
• Goodpasture syndrome is the rapidly
progressive glomerulonephritis and
pulmonary hemorrhage.
4.
BackgroundIn 1919, Ernest Goodpasture described an 18
year- old man with a fever and cough, followed
by hemoptysis and renal failure. The discovery of
the role of anti GBM antibodies by Lerner et al in
1967 helped to provide both a better
understanding of the pathogeneses for this
specific form of pulmonary renal syndrome and a
more rational approach to treatment.
5.
Epidemiology- Goodpasture syndrome is diagnosed in 1 in
1 million persons each year.
- Whites are affected more than in any other
races.
- Incidence is slightly higher in men than in
women.
- The syndrome affects 2 different age
groups persons in their mid 30s and
persons in their late 50s.
6.
Causes1. Genetic predispositions
Anti-GBM antibody has been described in identical twins,
siblings and first cousins.
• HLA-DR2 is expressed in 88% of patients with anti-GBM
disease compared to 25-32% of a control group of blood
donors.
• Anti-GBM antibody is strongly associated with HLA DR15
and HLA-DR11 alleles.
• HLA-DR7 and HLA-DR5 have strong negative associations;
both are highly protective.
7.
8.
2. Environmental insults:• Cigarette smoking.
• Inhaled hydrocarbons.
Gasoline fumes or industrial solvents are
believed to induce chemical injury to the lung
or kidney .
9.
3. Viral infections:• Influenza type A2.
• Upper respiratory tract infection or flu like illness
occurred the onset of disease in 20-61% of adults with
ant GBM disease
10.
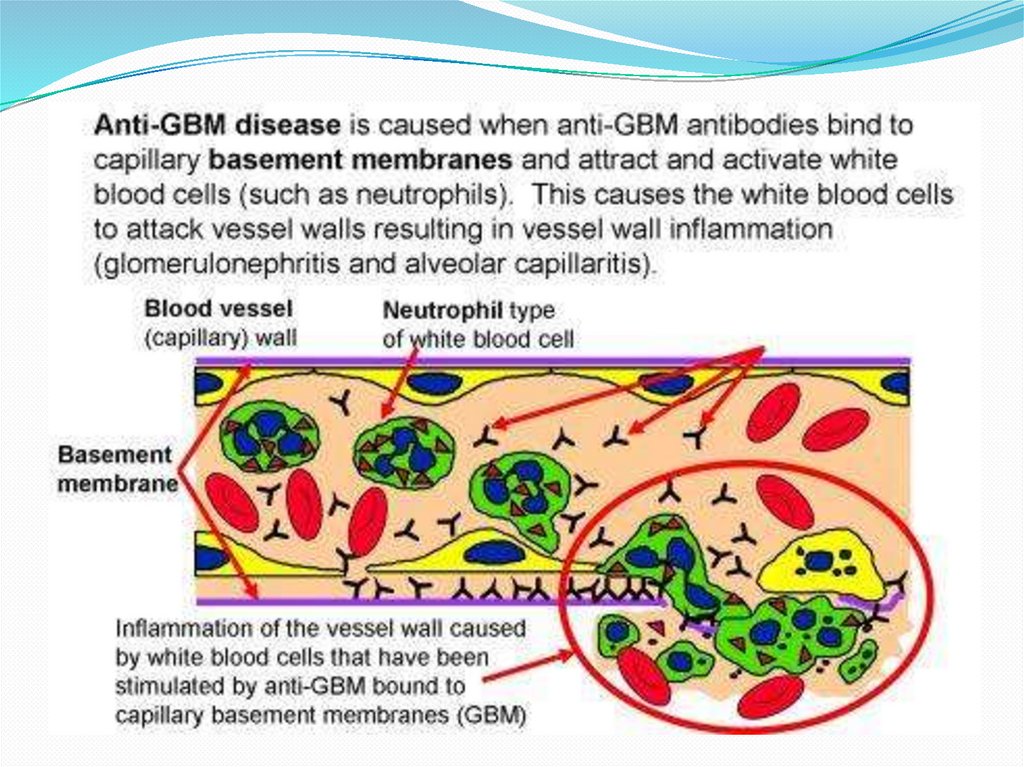
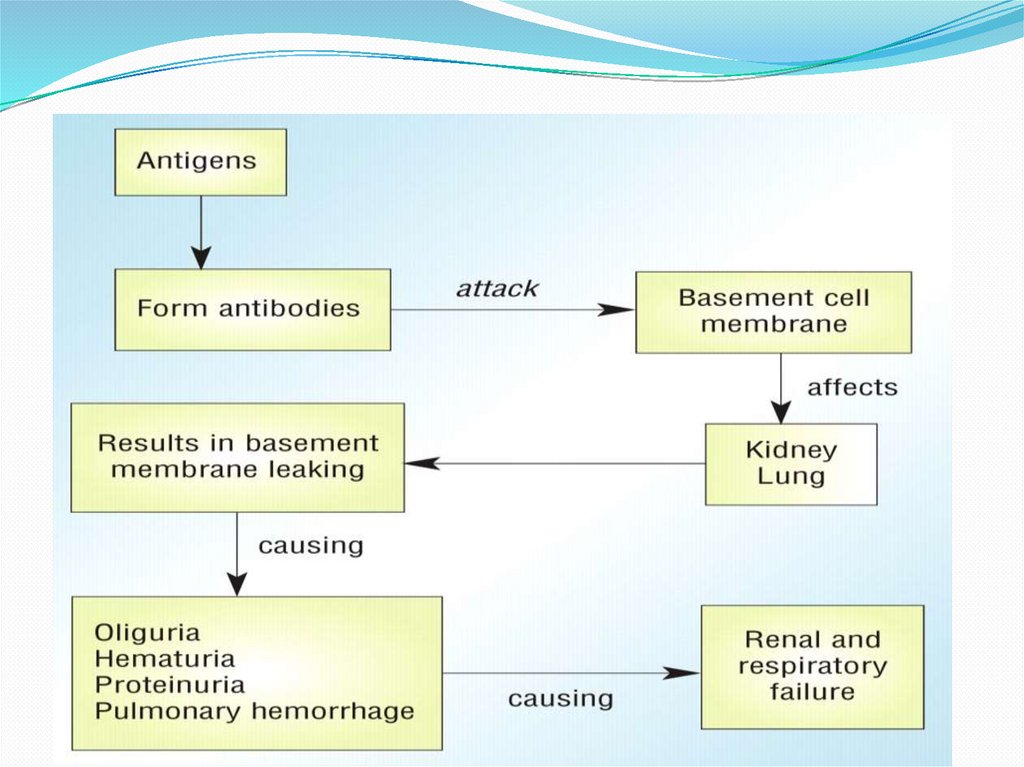
PathophysiologyPatients with Goodpasture syndrome is a type II hypersensitivity
reaction
In Good pasture syndrome the antibodies attack the NC1 domain
of the α3 chain of type IV collagen factor in the basement
membranes of the kidney and alevoli.
In the kidney the basement membrane is the principal selective
barrier of the glomerulus preventing plasma proteins, erythrocytes
and platelets from passing through into the nephrone. Deposit of
IgG, IgA and sometimes IgM antibodies in the basement
membrane breakdown collagen and interrupt membrane integrity.
This causes proteinuria, hematuria, oligouria and alveolar damage
with sub-basement pulmonary hemorrhage.
11.
12.
13.
Clinical Manifestation• The clinical manifestations vary, in some patients pulmonary signs and
symptoms occur weeks to months before renal manifestations are evident.
• The initial signs and symptoms consist of a flu like malaise followed by a
rapid onsets of microscopic hematuria and proteinuria.
• More than half of patients have pulmonary signs and symptoms including
(cough, mild shortness of breath and hemoptysis).
• The skin appears pale because of iron deficiency anemia.
• Renal manifestations can also include oedema and hypertension
Rarely patients may have arthritis, peripheral neuropathy, uveities or
leukocytoclastic vasculitis of the skin.
14.
Histopathological Features ofKidneys
Goodpasture’s
Syndromes.
Panel B (hematoxylin and
eosin)
shows
focal,
segmental necrosis of the
glomerular tuft in a kidney
from
a
patient
with
Goodpasture’s
syndrome.
Panel C (hematoxylin and
eosin) shows the crescent
formation of the glomerular
tuft in such a kidney.
15.
Differential diagnosis-Systemic vasculitis
-Wagner granulomatosis
-Polyarteritis Nodosa
-Systemic lupus erytheromatosis
-Infection
The occurrence of hemoptysis may be differentiated from other diseases,
including:
atrioventricular fistula, left ventricular failure, pulmonary embolism,
pulmonary hypertension, thrombocytopenia bronchitis, cystic fibrosis, lung
cancer, and multiple other causes.
16.
Investigations• Urine analysis, CBC current with differential BUN, creatnine and
electrolyte levels.
• ESR is usually mildly elevated.
• Specific serologic tests include assessments of anti GBM titers and ANCA
titers through indirect immunofluorescence testing, as well as enzyme
linked immunosorbet assay (ELISA) or radioimminssay (RIA) to evaluate
protease 3 and myeloperoxidase
• Circulating anti GBM titers may be elevated in more than 90% of
patients.
• Results from serologic studies such as antistreptolysim O (ASO) titers
and complement studies are usually negative.
ANCA titers are elevated in 20-30% of patients with anti GBM disease.
• Tests of ANA and rheumatoid factor are usually negative
17.
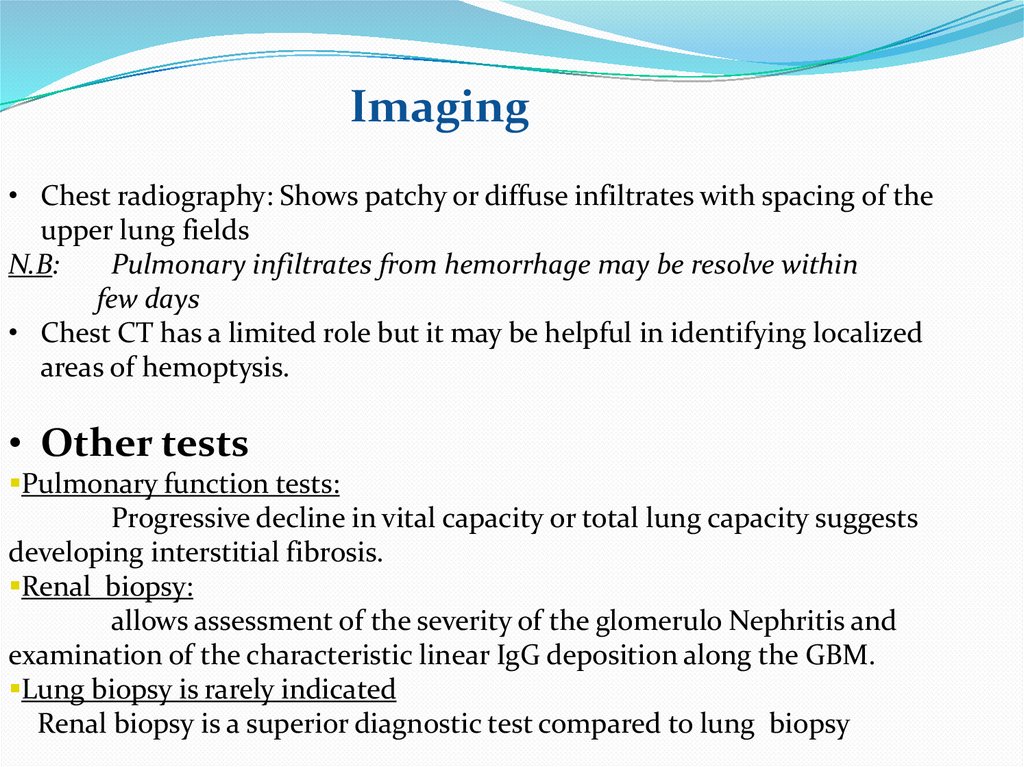
Imaging• Chest radiography: Shows patchy or diffuse infiltrates with spacing of the
upper lung fields
N.B:
Pulmonary infiltrates from hemorrhage may be resolve within
few days
• Chest CT has a limited role but it may be helpful in identifying localized
areas of hemoptysis.
• Other tests
Pulmonary function tests:
Progressive decline in vital capacity or total lung capacity suggests
developing interstitial fibrosis.
Renal biopsy:
allows assessment of the severity of the glomerulo Nephritis and
examination of the characteristic linear IgG deposition along the GBM.
Lung biopsy is rarely indicated
Renal biopsy is a superior diagnostic test compared to lung biopsy
18.
ManagementDie
Sodium restriction:
The daily total intake should not exceed 2gm
Fluid restriction
Depends on the patients renal function and whether the patient is
taking cyclophosphamide or not.
Plasma exchange
Every day for 14 days or every third day for a month and its replacement with
albumin and Fresh frozen plasma
19.
Immuno suppressive drugs1.Glucocorticoids e.g Methyl prednisolone
These agents have anti inflammatory properties and caused
profound and varied metabolic effects.
It’s used to treat pulmonary hemorrhage and rapidly
progressing glomerular Nephritis.
Dose
1gm IV qd for 3d (adult dose)
Or
Pulse dose of 10-30 mg/kg IV qd for 3d not exceeding 1g/d
(pediatric dose).
20.
-Prednisone-It decreases anti GBM antibody production.
Adult: 1-2 mg/kg/d for 8-12 w, alternatively, taper
weekly to 20mg/d with slower taper over 1-2 y.
-Children: 2mg/kg/d orally in divided doses for 1
month Not to exceed 80mg/d, then often 1 month
60-80mg/d given every morning for 1 additional
month.
21.
2.Alkylating agent- (Cyclophosphamide)Interferes with inflammatory response by decreasing
bone marrow response through the interference of DNA
cross linking. Decrease anti GBM antibody production.
Adult: 2-3mg/kg/d orally for 8-12 wk
Children: 2mg/kg/d orally for 8-12wk
Not to exceed 150mg/dose
22.
3.Monoclonal antibodies (Rituximab)anti-CD20)
Monoclonal antibody binds to pre B cells and Mature
B cells. It results in lymphocytotoxic effects to B cells,
which should results in reduced autoantibody
production.
4.Antibiotics
These agents are used to prevent opportunistic
infection with pneumocystis carinii.
23.
PrognosisHas greatly improved in the past 15 years. Reports
from the 1960s, before the advent of
immunosuppressive therapy and plasma exchange
indicate a 96% mortality rate in adults.
In the era of plasma exchange, the mortality rate in
adults is 0-41%.

















 medicine
medicine