Similar presentations:
Abnormalities of the expulsive forces
1.
ABNORMALITIES OFTHE EXPULSIVE FORCES
2.
Types of UterineDysfunction
• Uterine contractions are needed to dilate the cervix and to
expel the fetus.
• A contraction is initiated by spontaneous action potentials
in the membrane of smooth muscle cells.
• Unlike the heart, a single pacemaker or its site remain
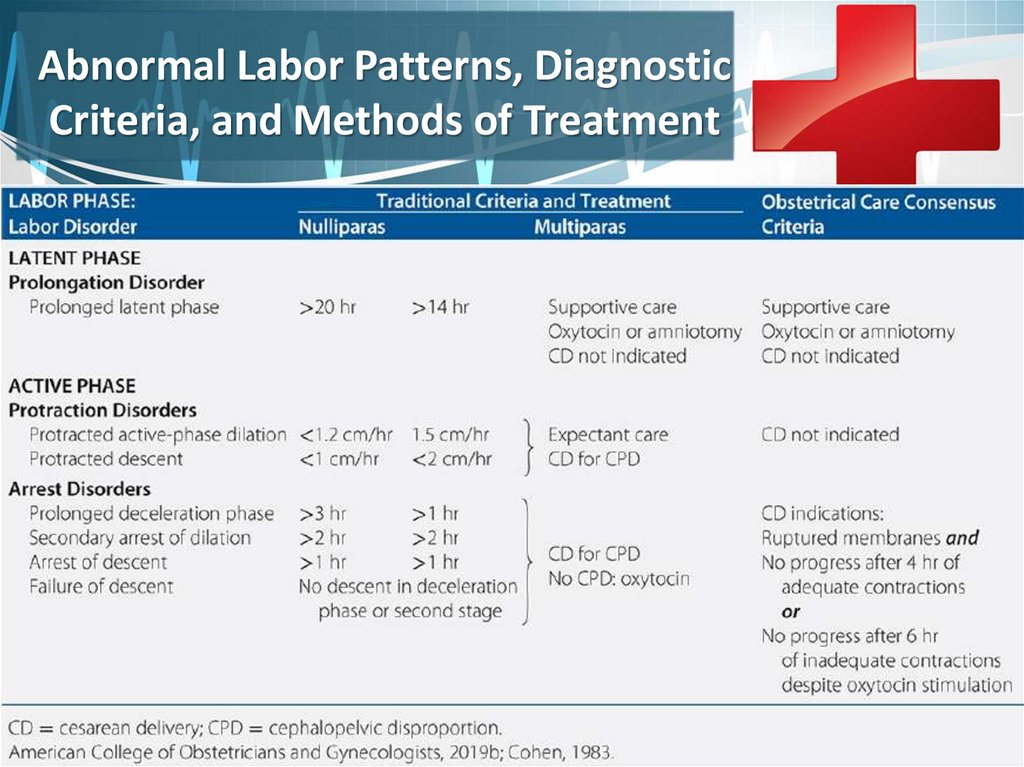
unresolved.
• Resulting uterine contractions in normal labor show a rising
and falling gradient of myometrial activity.
• Normal spontaneous contractions can exert pressures
approximating 60 mmHg .
• Even so, the lower limit of contraction pressure required to
dilate the cervix is 15 mmHg.
3.
Types of UterineDysfunction
• In abnormal labor, two physiological types of uterine
dysfunction may develop.
• In the more common hypotonic uterine dysfunction,
basal tone is normal and uterine contractions have a
normal gradient pattern (synchronous).
• However, pressure during a contraction is insufficient
to dilate the cervix.
• In the second type, hypertonic uterine dysfunction or
incoordinate uterine dysfunction, either basal tone is
elevated appreciably or the pressure gradient is
distorted.
4.
Risk Factors for UterineDysfunction
• Various factors are implicated in uterine
dysfunction.
• First, neuraxial analgesia can slow labor and has
been associated with longer first and second
stages of labor.
• With current anesthesia methods, however, its
effect on labor length is blunted.
5.
Risk Factors for UterineDysfunction
• Chorioamnionitis is associated with prolonged labor.
• Uterine infection may directly contribute to uterine
dysfunction or instead may simply be an associated
consequence of prolonged, dysfunctional labor.
• Affected gravidas are monitored for labor progress, and
augmentation of protracted labor is prudent.
6.
Risk Factors for UterineDysfunction
• A higher station at the onset of labor is
significantly linked with subsequent dystocia.
• Although a risk factor, most nulliparas without
fetal head engagement at diagnosis of active
labor still deliver vaginally.
• These observations apply especially for parous
women because the head typically descends later
in labor.
7.
Risk Factors for UterineDysfunction
• Dystocia rate rises proportionally with maternal age even
after adjusting for maternal and fetal weight and parity.
• Maternal obesity lengthens the first stages of labor by 30 to
60 minutes in nulliparas, even after adjusting for associated
diabetes, fetal weight, and parity.
• Dystocia-associated cesarean delivery rates are higher in
this group.
• Growing evidence suggests a pathologic biological effect of
obesity on normal parturition.
8.
Labor Disorders9.
Abnormal Labor Patterns, DiagnosticCriteria, and Methods of Treatment
10.
Latent-phase Prolongation• Uterine dysfunction can in turn lead to labor abnormalities.
• First, the latent phase may be prolonged, which is defined
as >20 hours in the nullipara and >14 hours in the
multipara.
• In some, uterine contractions cease, suggesting false labor.
• In the remainder, an abnormally long latent phase persists
and is often treated with amniotomy and oxytocin
stimulation.
• The diagnosis of uterine dysfunction in the latent phase is
difficult and commonly is made retrospectively.
• Women who are not yet in active labor often are
erroneously treated for perceived uterine dysfunction.
11.
Active-phase Disorders• In active labor, disorders are divided into
those with slow progress — a protraction
disorder or those with halted progress — an
arrest disorder.
• Terms presented in table and their diagnostic
criteria describe abnormal labor.
• To be diagnosed with either of these, a
woman must be in the active phase of labor.
12.
Active-phase Protraction• Of active-phase disorders, protraction disorders are less well
described.
• Previously, protraction has been defined as <1 cm/hr cervical
dilation for a minimum of 4 hours.
• For this disorder, observation for further progress is appropriate
treatment.
• In monitoring active labor, if hypotonic contractions are strongly
suspected, internal monitors may be placed with amniotomy and
again cervical change and contraction pattern are reassessed.
• Deficient Montevideo units and poor active labor progress typically
prompts oxytocin augmentation.
• Slow but progressive first-stage labor should not be an indication
for cesarean delivery.
13.
Montevideo units• To assess uterine activity, many methods have been
proposed, based on a complex mathematical
assessment of the duration of contractions, their
intensity and frequency over a certain period of time
(usually 10 minutes).
• The most widespread assessment of uterine activity is
in Montevideo units (MU).
• Montevideo units are the product of the contraction
intensity and the frequency of uterine contractions in
10 minutes.
• Normally, uterine activity increases as labor progresses
and amounts to 150-300 MU.
14.
15.
Active-phase Arrest• Handa and Laros (1993) diagnosed active-phase arrest, defined as
no dilation for ≥2 hours, in 5 percent of term nulliparas.
• Inadequate uterine contractions, defined as <180 Montevideo
units, were diagnosed in 80 percent of women with active-phase
arrest.
• Hauth and coworkers (1986, 1991) reported that when labor is
effectively induced or augmented with oxytocin, 90 percent of
women achieve 200 to 225 Montevideo units, and 40 percent
achieve at least 300 Montevideo units.
• These results suggest that certain minimums of uterine activity
should be achieved before performing cesarean delivery for
dystocia.
• Oxytocin regimens suitable to augment labor mirror those to induce
labor.
16.
Active-phase Arrest• Other criteria should also be met.
• First, the latent phase should be completed, and
the cervix is dilated ≥4 cm.
• Also, a uterine contraction pattern of ≥200
Montevideo units in a 10-minute period has been
present for ≥4 hours without cervical change
(Rouse, 1999).
• The Consensus Committee has extended this
further, as described next.
17.
Obstetric CareConsensus Committee
• The Obstetric Care Consensus series are
documents jointly developed with the Society
for Maternal-Fetal Medicine (SMFM) with
The American College of Obstetricians and
Gynecologists (ACOG) (a professional
association of physicians specializing in
obstetrics and gynecology in the United
States).
18.
Obstetric CareConsensus Committee
• Four recommendations of the Consensus
Committee apply to management of firststage labor.
• The first admonishes against cesarean delivery
in the latent phase.
• Specifically, a prolonged latent phase should
not be the sole indication for cesarean
delivery.
19.
Obstetric CareConsensus Committee
• The second directive, too, is conventional
practice.
• It recommends against cesarean delivery if
labor is progressive but slow—a protraction
disorder.
• This instance is typically managed with
observation, assessment of uterine activity,
and stimulation of contractions as needed.
20.
Obstetric CareConsensus Committee
• A third instruction addresses the cervical dilation
threshold that serves to herald active labor.
• Namely, a cervical dilation of 6 cm—not 4 cm—is
now the recommended threshold.
• Moreover, before this threshold, standards for
active-phase progress should not be applied.
• Of note, the WHO (2018) recognizes 5 cm as the
active-labor threshold.
• Other large studies noted labor acceleration after
5 cm (Ashwal, 2020; Oladapo, 2018).
21.
Obstetric CareConsensus Committee
• A fourth stipulation notes that cesarean
delivery for active-phase arrest is best
reserved for women with cervical dilation ≥6
cm and ruptured membranes who fail to
progress despite 4 hours of adequate uterine
activity or despite at least 6 hours of oxytocin
administration but inadequate contractions.
22.
Cervical dilation curves fromFriedman (1955) and Zhang (2002).
23.
Second-stage DescentDisorders
• Fetal descent largely follows complete
dilation.
• Moreover, the second stage incorporates
many of the cardinal movements necessary
for the fetus to negotiate the birth canal.
• Thus, disproportion of the fetus and pelvis
frequently becomes apparent during secondstage labor.
24.
Second-stage DescentDisorders
• Similar to first-stage labor, time boundaries have been
supported to limit second-stage duration to minimize
adverse maternal and fetal outcomes.
• The second stage in nulliparas has been limited to 2
hours and extended to 3 hours when regional analgesia
is used.
• For multiparas, 1 hour has been the limit, extended to
2 hours with regional analgesia.
• However, of maternal outcomes, higher rates of
chorioamnionitis, anal sphincter injury, operative
vaginal birth, and postpartum hemorrhage accrue as
the second stage lengthens.
25.
Second-stage DescentDisorders
• Newer guidelines have been promoted by the Consensus
Committee (2019b) for second-stage labor.
• These recommend that a nullipara push for at least 3 hours and a
multipara push for at least 2 hours before second-stage labor arrest
is diagnosed.
• Importantly, one caveat is that maternal and fetal status should be
reassuring.
• These authors provide options to these times before cesarean
delivery is performed.
• Namely, longer durations may be appropriate as long as progress is
documented.
• Also, a specific maximal length of time spent in second-stage labor
beyond which all women should undergo operative delivery has not
been identified.
26.
Maternal Pushing Efforts• With full cervical dilation, most women cannot resist the urge to push with
uterine contractions.
• The combined force created by contractions of the uterus and abdominal
musculature propels the fetus downward.
• However, at times, force created by abdominal musculature is
compromised sufficiently to slow or even prevent spontaneous vaginal
delivery.
• Heavy sedation or regional analgesia may reduce the reflex urge to push
and may impair the ability to contract abdominal muscles sufficiently.
• Allowing time for these to abate is reasonable.
• In other instances, the urge to push is overridden by the intense pain
created by bearing down.
• Depending on fetal station and anticipated second stage, options include
emotional support and encouragement, parenteral analgesia, pudendal
blockade, or neuraxial analgesia.
27.
Oxytocin• As previously emphasized, in many instances, preinduction
cervical ripening and labor induction are simply a
continuum.
• In this regard “ripening” can also stimulate labor.
• If not, induction or augmentation may be continued with
solutions of oxytocin given by infusion pump.
• Its use in augmentation is a key component in the active
management of labor.
• With oxytocin use, the American College of Obstetricians
and Gynecologists (2019a) recommends fetal heart rate
and uterine contraction monitoring.
• Contractions can be monitored either by palpation or by
electronic means.
28.
Oxytocin• preparation of solution: for intravenous
administration with a perfuser - 1 ml (5 IU) in 49
ml of 0.9% sodium chloride solution.
• Administration schemes:
• Low-dose infusion – starting dose 3 mU/min – 1.8
ml/hour (“step” – 1.8 ml/hour)
• High-dose infusion – starting dose 6 mU/min –
3.6 ml/h (“step” – 3.6 ml/h)
29.
Oxytocin• Increase the rate of oxytocin administration
every 20-30 minutes by 1 “step” until 4-5
contractions are achieved in 10 minutes/
• The monitoring of the condition of the mother
and fetus, then fix this minimally effective
dose.
• 33 mU/min (19.8 ml/hour) is an extremely
dangerous level.
30.
Oxytocin• If there is no effect from the administration of
Oxytocin:
• lack of labor and dynamics of cervical
dilatation within 3-5 hours
• inability to reach the active phase of labor
within 5-15 hours
• - resolve the issue of delivery by CS surgery.















 medicine
medicine