Similar presentations:
Secondary pulmonary hypertension
1.
SECONDARY PULMONARY HYPERTENSIONPRESENTED BY: SMIT BHAISARE
JOISY ALOOR
LEONARD SHAJU
2.
OVERVIEWPulmonary arterial hypertension (PAH) is a
progressive condition characterized by elevated
pulmonary arterial pressures leading to right
ventricular (RV) failure.
The pulmonary vascular injury underlying PAH
occurs in an idiopathic form or in association
with other disease states or exposures and is
probably a final common response to
environmental or disease-related inciting factors
coupled with genetically determined
susceptibilities.
3.
4.
INTRODUCTIONSecondary pulmonary arterial hypertension
(SPAH) is an adverse outcome of a variety of
systemic disorders.
These include collagen vascular diseases, chronic
thromboembolism, human immunodeficiency
virus, portopulmonary hypertension, and other
diseases.
Progression of SPAH may persist despite
stabilization of the causative disease, thereby
contributing to the poor quality of life and
unfavorable survival in these patients.
5.
6.
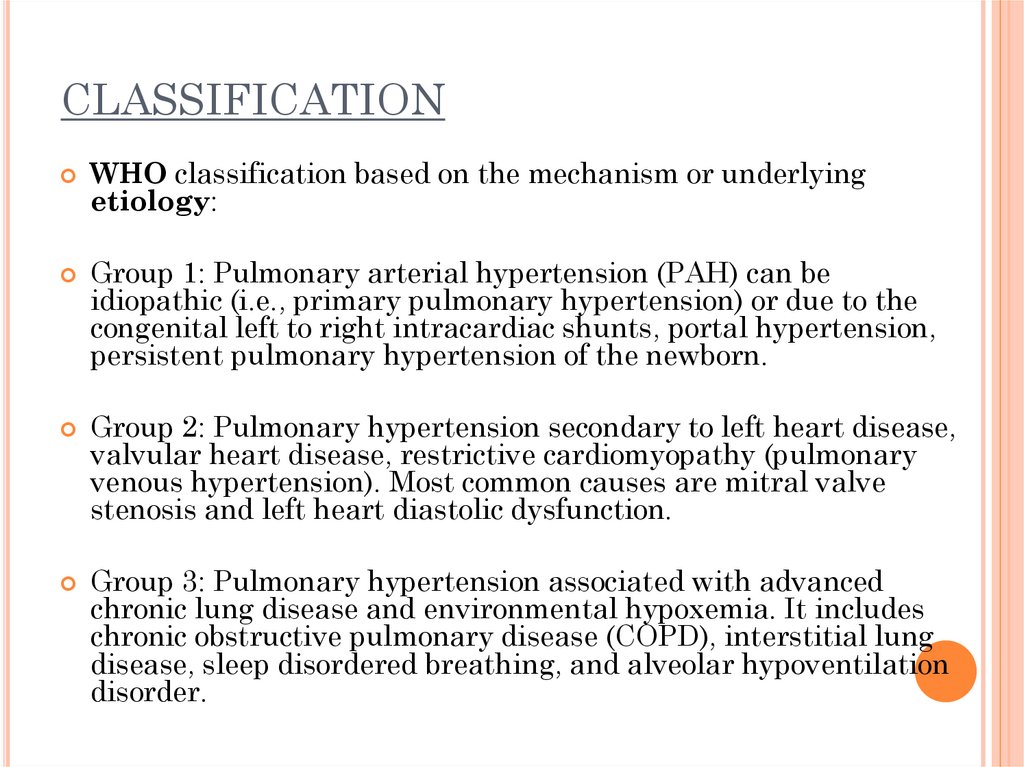
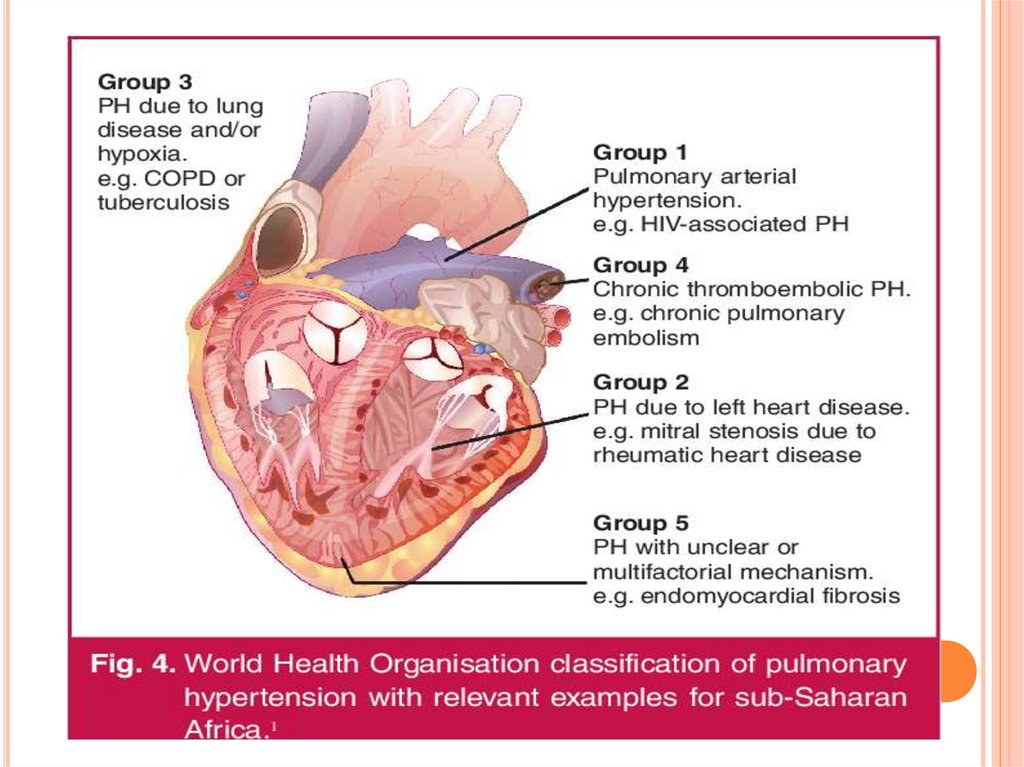
CLASSIFICATIONWHO classification based on the mechanism or underlying
etiology:
Group 1: Pulmonary arterial hypertension (PAH) can be
idiopathic (i.e., primary pulmonary hypertension) or due to the
congenital left to right intracardiac shunts, portal hypertension,
persistent pulmonary hypertension of the newborn.
Group 2: Pulmonary hypertension secondary to left heart disease,
valvular heart disease, restrictive cardiomyopathy (pulmonary
venous hypertension). Most common causes are mitral valve
stenosis and left heart diastolic dysfunction.
Group 3: Pulmonary hypertension associated with advanced
chronic lung disease and environmental hypoxemia. It includes
chronic obstructive pulmonary disease (COPD), interstitial lung
disease, sleep disordered breathing, and alveolar hypoventilation
disorder.
7.
Group 4: Pulmonary hypertension due to chronic thromboticdisease, embolic disease, or both.
Group 5: A miscellaneous complex group of disorders leading to
PH which includes metabolic disorders, systemic disorders,
hematologic diseases, and miscellaneous causes.
Metabolic disorders such as glycogen storage disease, thyroid
disease, Gaucher disease
Systemic diseases include sarcoidosis, vasculitis,
neurofibromatosis type 1
Hematologic diseases like myeloproliferative disorders.
Other causes include end-stage renal disease on dialysis, extrinsic
compression of pulmonary vessels, embolization of the tumor.
8.
9.
10.
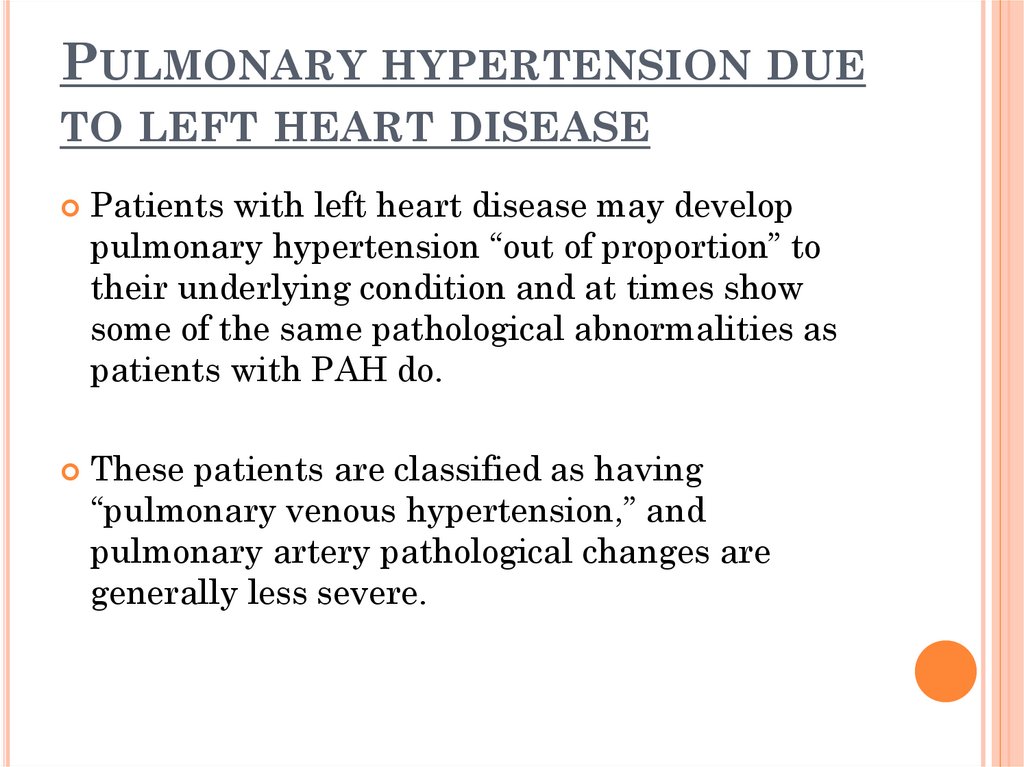
PULMONARY HYPERTENSION DUETO LEFT HEART DISEASE
Patients with left heart disease may develop
pulmonary hypertension “out of proportion” to
their underlying condition and at times show
some of the same pathological abnormalities as
patients with PAH do.
These patients are classified as having
“pulmonary venous hypertension,” and
pulmonary artery pathological changes are
generally less severe.
11.
LEFT VENTRICULAR SYSTOLICDISORDER
LVSD is a common and serious complication of
myocardial infarction (MI) that leads to greatly
increased risks of sudden death and of heart failure.
Valvular heart disease is characterized by damage
to or a defect in one of the four heart valves: the
mitral, aortic, tricuspid or pulmonary.
A stenosis valve forces blood to back up in the
adjacent heart chamber, while an incompetent valve
allows blood to leak back into the chamber it
previously exited.
12.
13.
PULMONARYADVANCED
HYPERTENSION ASSOCIATED WITH
CHRONIC
LUNG
DISEASE
AND
ENVIRONMENTAL HYPOXEMIA.
Pulmonary hypertension is common in patients with
obstructive or restrictive lung disease, but in most
cases, it is relatively mild.
Pulmonary arterial pressures correlate better with
oxygen saturation than with spirometer, and for
patients who are hypoxemic at rest (PaO2 55 to 59
mm Hg).
The patients with lung disease plus pulmonary
hypertension have low survival rates
Whether iloprost or other PAH medications will
improve symptoms or outcomes is unknown
14.
15.
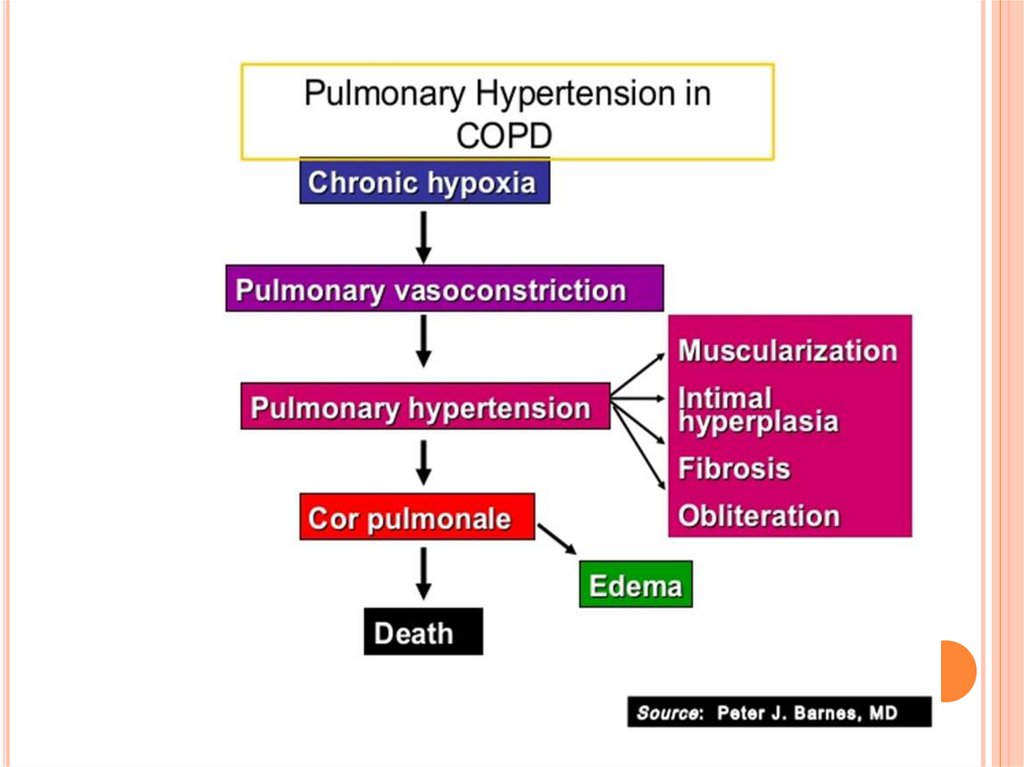
Chronic obstructive pulmonary disease (COPD) isa type of obstructive lung disease characterized by
long-term breathing problems and poor airflow.
One established complication of COPD is the
development of pulmonary hypertension (PH).
Typically, PH appears when airflow limitation is
severe and is associated with chronic hypoxemia, the
main pathophysiological cause being chronic alveolar
hypoxia, although new mechanisms have emerged
recently.
16.
17.
PULMONARYHYPERTENSION DUE TO CHRONIC
THROMBOTIC DISEASE, EMBOLIC DISEASE, OR
BOTH.
Chronic
thromboembolic pulmonary
hypertension is due to incomplete resolution
of pulmonary emboli leading to elevated
pulmonary pressures and RV failure.
Other
pulmonary artery obstructions.
Angiosarcoma or other tumor within the
blood vessels
Arteritis
Congenital pulmonary artery stenosis
Parasitic infection (hydatidosis)
18.
CHRONIC THROMBOEMBOLIC PULMONARYHYPERTENSION
The lungs and heart must exert pressure to move
blood throughout the body.
CTEPH is high blood pressure in the arteries in
the pulmonary system (lungs) caused by clots in
the blood vessels that last after at least 3 months
on blood thinners.
The clots typically leave scar tissue in the
arteries.
19.
20.
A MISCELLANEOUSCOMPLEX GROUP OF
DISORDERS LEADING TO
PH
Pulmonary hypertension with unclear
or multifactorial mechanisms
Hematologic diseases: chronic hemolytic anemia (including sickle
cell disease)
Systemic diseases: sarcoidosis,pulmonary Langerhans
cell histiocytosis: lymphangioleiomyomatosis, neurofibromatosis,
vasculitis
Metabolic disorders: glycogen storage disease, Gaucher
disease, thyroid diseases
Others: pulmonary tumoral thrombotic
microangiopathy, fibrosing mediastinitis, chronic kidney failure.
21.
22.
PATHWAYS AND REASONS LEADING TOSECONDARY PULMONARY ARTERY
HYPERTENSION
23.
GENETICSMutations in several genes have been associated
with this condition these include: Bone
Morphogenetic Protein Receptor 2 (BMPR2) and
Eukaryotic Translation Initiation Factor 2 Alpha
Kinase 4 Gene (EIF2AK4).
These account for 60% cases of inherited PAH.
24.
Hereditary haemorrhagic telangiectasia (orOsler-Weber-Rendu syndrome). This disorder is
characterized by the development of
mucocutaneous telangiectasia and arteriovenous
malformations in the brain, lungs, liver, and
gastrointestinal tract.
25.
OTHER CAUSESEmphysema and other forms of Chronic
Obstructive Pulmonary Disease (COPD).
Collagen Vascular diseases such as Scleroderma,
CREST Syndrome and Lupus.
Congenital heart disorders such as ventricular
and atrial septal defects.
Blood clots in lungs and pulmonary arteries.
HIV
26.
Liver DiseasesProblems with the mitral valve.
Diet drugs such as fenfluramine and
dexfenfluramine.
Worsening of Primary Pulmonary Artery
Hypertension.
Other autoimmune diseases
27.
28.
29.
PATHWAYSIt is believed that endothelial dysfunction results
in a decrease in the synthesis of endotheliumderived vasodilators such as nitric oxide and
prostacyclin.
Moreover, there is a stimulation of the synthesis
of vasoconstrictors such as thromboxane and
vascular endothelial growth factor (VEGF).
These results in a severe vasoconstriction and
vascular smooth muscle and adventitial
hypertrophy characteristic of patients with PAH.
30.
ENDOTHELIN:Endothelin-1 is a peptide (comprising 21 amino
acids) that is produced in endothelial cells.
It acts on the endothelin receptors ETA and ETB
in various cell types including vascular smooth
muscle cells and fibroblasts, leading to
vasoconstriction, hypertrophy, proliferation,
inflammation, and fibrosis.
31.
32.
PROSTACYCLIN AND THROMBOXANE:Prostacyclin is synthesized from arachidonic acid
in endothelial cells. In vascular smooth muscle
cells, prostacyclin binds mainly to the
prostaglandin I receptor. Prostacyclin signalling
also leads to anti-thrombotic, anti-fibrotic, and
anti-inflammatory effects.
The vasoconstrictor thromboxane is also
synthesized from arachidonic acid. In PAH, the
balance is shifted away from synthesis of
prostacyclin towards synthesis of thromboxane.
33.
NITRIC OXIDE-SOLUBLE GUANYLATECYCLASE PATHWAY:
In normal conditions, the vascular endothelial nitric
oxide synthase produces nitric oxide from L-arginine in
presence of oxygen.
This nitric oxide diffuses into neighbouring cells
(including vascular smooth muscle cells and platelets),
where it increases the activity of the enzyme soluble
guanylate cyclase, leading to increased formation of
cGMP from GTP.
34.
The cGMP then activates cGMP-dependentkinase or PKG (protein kinase G). Activated PKG
promotes vasorelaxation (via a reduction of
intracellular calcium levels), alters the
expression of genes involved in smooth muscle
cell contraction, migration and differentiation,
and inhibits platelet activation. Nitric oxide–
soluble guanylate cyclase signaling also leads to
anti-inflammatory effects.
Phosphodiesterase type 5 (PDE5), which is
abundant in the pulmonary tissue, hydrolyzes
the cyclic bond of cGMP. Consequently, the
concentration of cGMP (and thus PKG activity)
decreases.
35.
36.
37.
SYMPTOMSAs the disease progresses, the pulmonary
arteries become thicker and narrower.
The resulting increase in pressure forces the
heart to work harder to pump blood to the lungs.
This causes the heart muscle to enlarge and
become weaker, which can lead to Congestive
Heart Failure.
38.
Common symptoms include:1.
Exertional dyspnea progresses to dyspnea at rest as
disease advances.
2.
Fatigue
3.
Chest pain
4.
Dizziness or fainting
5.
Peripheral edema due to disease affecting the heart.
6.
Cyanosis
7.
Racing pulse or heart palpitations.
39.
DIAGNOSIS40.
ECHOCARDIOGRAPHYECG
PFT
CHEST X-RAY
CARDIAC CATHETERIZATION
CT SCAN
EXERCISE STRESS TEST
PULMONARY ANGIOGRAPHY
VENTILATION PERFUSION TEST
41.
ECHOCARDIGRAPHY42.
43.
44.
X-RAY45.
46.
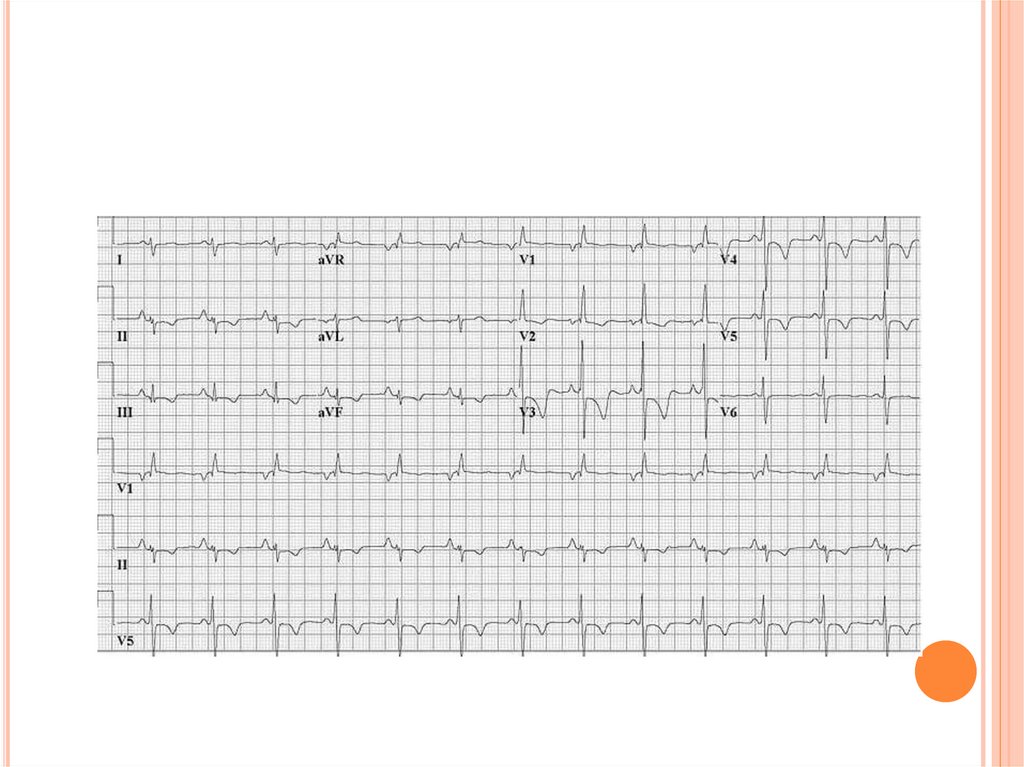
ECGRight ventricular hypertrophy
Right atrial enlargement
Increased amplitude of P-wave in lead II in all
groups.
It may show left ventricular hypertrophy in left
heart disease.
47.
48.
ANGIOGRAPHY49.
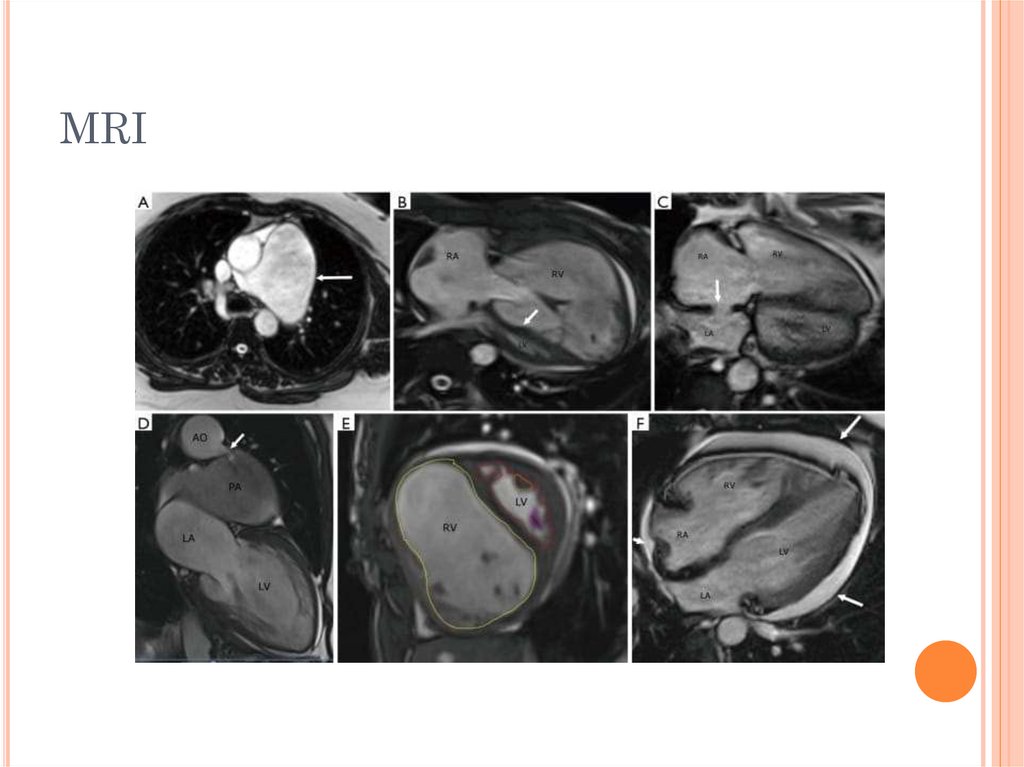
MRI50.
VENTILATION PERFUSION TESTPatients with perfusion defects are further
evaluated by CT pulmonary angiography and
heart catheterization.
51.
52.
CARDIAC CATHETERIZATION53.
THANK YOUTAKE CARE






































 medicine
medicine