Similar presentations:
Prolapse of the female genital organs
1.
Prolapse of the femalegenital organs
2.
IntroductionDefinition
Pathophysiology
Types
Causes
Contents
Sign & symptoms
Stages
Medical Management
Nursing diagnosis
Nursing management
Complications
Prevention
3.
IntroductionPelvic organ prolapse is when 1 or more of the organs in
the pelvis slip down from their normal position and bulge
into the vagina. It can be the womb (uterus), bowel,
bladder or top of the vagina.
A prolapse is very unlikely to occur in a woman under
menopausal age, but though the muscles weaken with
age, they will have probably been injured years earlier, in
pregnancy, during a long labor or through having a large
baby
A prolapse is not life threatening, but it can cause pain
and discomfort.
4.
Anatomy of the uterus5.
The uterine supportsUpper uterine supports
normal position
Middle uterine supports:
- Cardinal ligament : lateral cervical ligaments
- utero-sacral ligaments: posterior cervical ligaments
- pubo-cervical ligaments:
Anterior cervical ligaments
6.
Lower uterine support: pelvic floor muscleFASCRA .. ENDOPELVIC FASICRA
pubo cervical ligament. Pass from the cervix to the pubic bones
Transverse/cardinal ligaments: from the sides of the cervix to the side
wall of the pelvics
Uterosacral ligaments: pass backwards from the cervix to bladder to
the pubic bones
7.
8.
9.
DefinitionProlapse
means descents of a genital organ below its normal
position.
Genital prolapse occurs when pelvic organs (uterus,
bladder, rectum)
slip down from their normal anatomical position and
either protrude into the vagina or press against the
wall of the vagina.
10.
TypesUterine prolapse
Vaginal prolapse
Combined vaginal and uterine prolapse.
This may be
uterovaginal or vaginouterine
prolapse of the ovaries and tubes
11.
Uterine prolapse12.
Etiology:- Congenital:
due to weakness of uterine
support, usually it is mobile.
- Acquired:
may be mobile, or fixed.
13.
Inversions of the uterusis a condition in which the uterus turns inside out. (obstetric
emergency)
- Acute uterine inversion: occurs during or immediately after the
3rd stage of labor (within 24hours of delivery.)
- Chronic uterine inversion occurs in non-pregnant women
(more than 30 days after delivery.)
14.
Vaginal prolapseProlapse occurs when a woman's pelvic floor muscles,
tissues and ligaments weaken and stretch. This can result in
organs dropping out of their normal position. Vaginal
prolapse refers to when the top of the vagina — also called
the vaginal vault — sags and falls into the vaginal canal
15.
Types of vaginal prolapse1. Prolapse of the anterior vaginal wall.
Descent of the upper two-thirds with the base of
the bladder (cystocele)
Descent of lower-third of the urethra
(urethrocele).
is a prolapse of the whole anterior vaginal wall
associated with the descend of the urethera &
base of urinary bladder.(cystourethrocele)
16.
2.Prolapse of the posterior vaginal wall:Descent of the upper-third with the
peritoneum of Douglas pouch
containing loops of intestine enterocele (hernia of Douglas pouch)
Descent of the middle-third with the
underlying rectum (rectocele).
17.
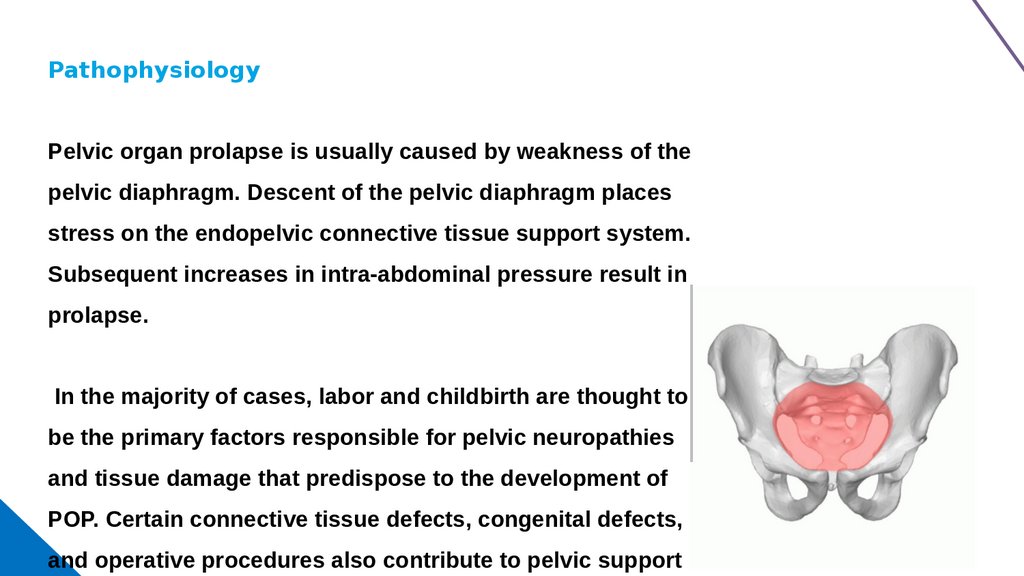
PathophysiologyPelvic organ prolapse is usually caused by weakness of the
pelvic diaphragm. Descent of the pelvic diaphragm places
stress on the endopelvic connective tissue support system.
Subsequent increases in intra-abdominal pressure result in
prolapse.
In the majority of cases, labor and childbirth are thought to
be the primary factors responsible for pelvic neuropathies
and tissue damage that predispose to the development of
POP. Certain connective tissue defects, congenital defects,
and operative procedures also contribute to pelvic support
18.
HOW DOES UTERINE PROLAPSE HAPPENS?Uterine prolapse occurs when pelvic floor
muscles and ligaments strech and weeken until
they no longer provide enough support for the
uterus
19.
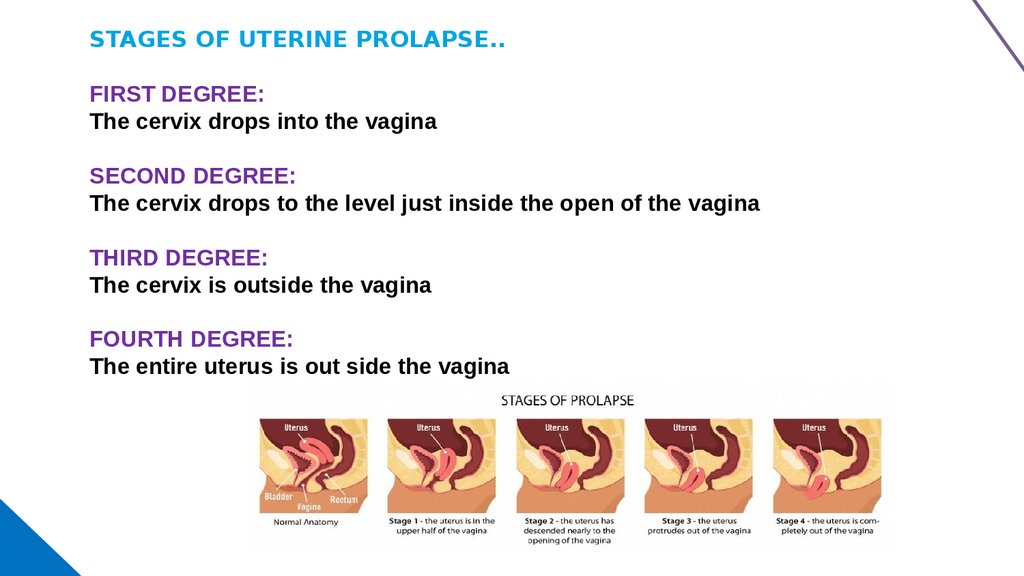
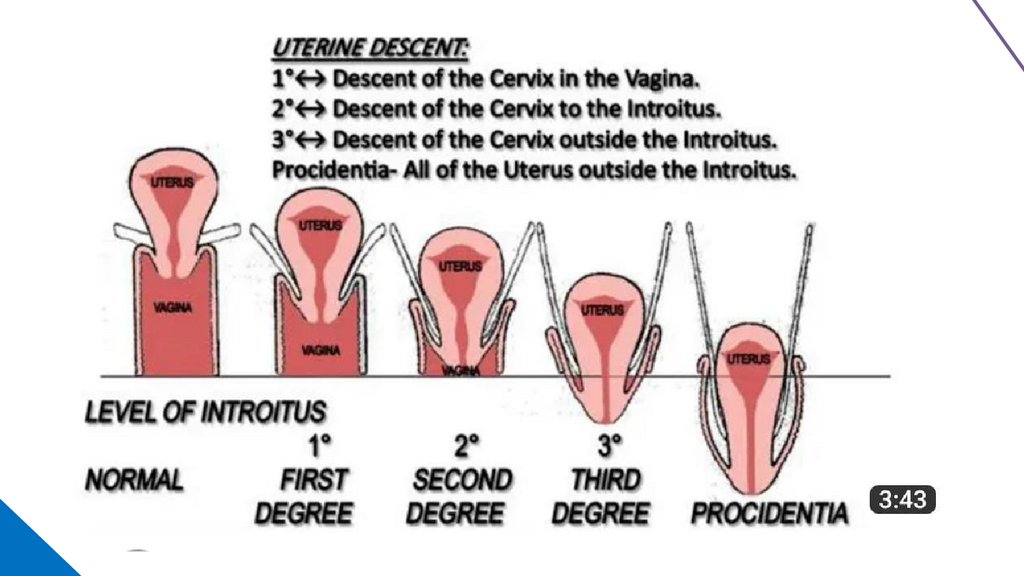
STAGES OF UTERINE PROLAPSE..FIRST DEGREE:
The cervix drops into the vagina
SECOND DEGREE:
The cervix drops to the level just inside the open of the vagina
THIRD DEGREE:
The cervix is outside the vagina
FOURTH DEGREE:
The entire uterus is out side the vagina
20.
21.
22.
Signs and symptomsA sensation of heaviness in pelvis due to a swelling in the vagina]
Low backache due to stretching of the uterosacral Ligaments by a uterine
prolapse.
Pain in the groins due to traction on round Ligaments.
Urinary symptoms may occur with a cystocele
a) Dysuria Sometimes the patient cannot micturate unless she pushes up the
cystocele with her finger in the vagina.
b) Retention of urine causes.
c) Stress incontinence.
23.
Rectal symptomsHeaviness in the rectum and dyschezia. (The patient may need to push the
rectocele upwards by a finger in the vagina to be able to defecate). Piles may
develop due to straining.
Dyspareunia due to a swelling in the vagina
Infertility; due to congestion of endometrium
24.
CausesI. Primary (predisposing) causes:
1- Weakness of the cervical ligaments
a) Congenital weakness (virginal or nulliparous prolapse)
b) Obstetric trauma (straining during the first stage of labor before the cervix is fully dilat
forceps or breech extraction before the cervix is fully dilated)
c) Postmenopausal atrophy (appearance of prolapse after menopause)
2- Injury of the pelvic floor
It is the result of child birth unrepaired; badly repaired or hidden perineal tear predispose
to prolapse
3- Retroversion of uterus
25.
||. Secondary ( precipitating) causes1. Increased intra- abdominal pressure, due to chronic
cough, chronic constipation, ascites, abdominal tumors
and obesity.
2. increased weight of the uterus, due to early pregnancy,
sub involution and small fibroids.
3. Traction on the uterus by a large cervical polyp or by
vaginal prolapse.
26.
Medical TreatmentI. Prophylactic treatment
During labor:
Avoid the factors which predispose to prolapse as:
Straining during the first stage of labor, forceps or breech extraction
before the cervix is fully dilated, etc.
Frequent emptying of the bladder, so that it is not pushed downward by
the fetal head.
Prophylactic episiotomy to avoid overstretching and weakness of pelvic
floor.
27.
AFTER LABORAny perineal or vaginal tear must be sutured immediately after delivery
pelvic floor exercises
patient is asked to lie on her abdomen for one hour daily to prevent
retroversion which predisposes to prolapse;
Treatment of puerperal constipation to avoid bearing down
If prolapse is detected during the Puerperium, a ring pessary is applied
for 3months until the supporting ligaments involute and restore their
tone
proper spacing of pregnancies;
28.
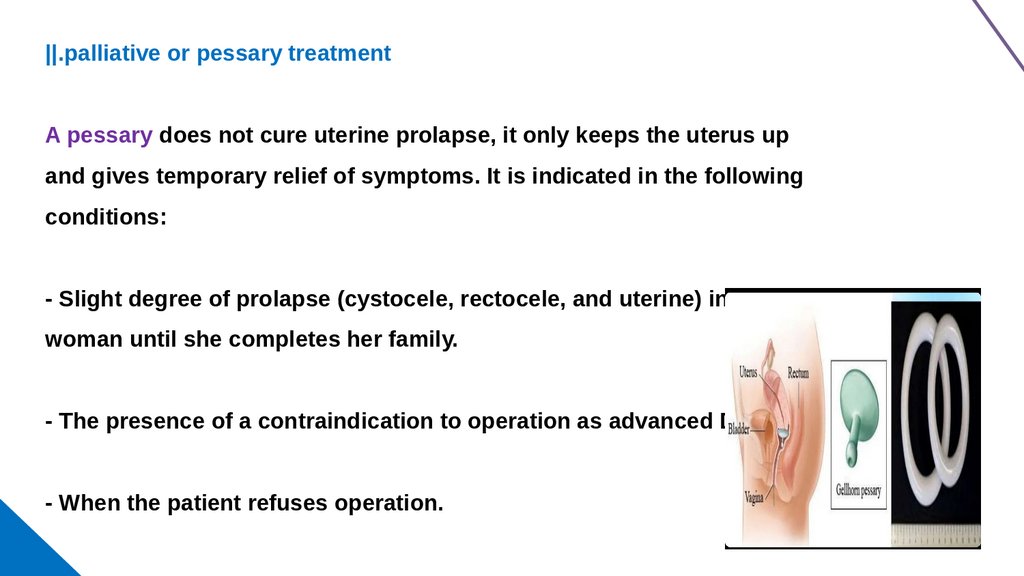
||.palliative or pessary treatmentA pessary does not cure uterine prolapse, it only keeps the uterus up
and gives temporary relief of symptoms. It is indicated in the following
conditions:
- Slight degree of prolapse (cystocele, rectocele, and uterine) in a young
woman until she completes her family.
- The presence of a contraindication to operation as advanced DM
- When the patient refuses operation.
29.
Nursing care plan:1) Nursing assessment
Complaint of lower abdominal pain
decreased appetite
generalized weakness,
difficult to walk because of uterine prolapsed.
30.
2) Nursing DiagnosisPain in lower abdomen related to displacement of pelvic organ
secondary to 3rd degree uterine prolapse.
Fatigue related to weakness secondary to uterine prolapsed
Activity intolerance related to lump in the vagina secondary to II
degree uterine prolapsed.
Imbalanced nutrition less than body requirement related to
Anxiety ,Fear, knowledge deficit- Risk for infection, skin integrity
sexual activity.
31.
3) Nursing InterventionPessaries or plastic rings, pulls or more, complex structures that are inserted
vaginally to prevent descent of the pelvic organs.
Provide adequate comfortable devices
Change the pessaries every 3-4 months
To teach the pelvic floor muscle exercise
Promote the client wash hand before and after
Maintain the personal hygiene
diet rich in iron, fiber.
32.
PreventionCan uterine prolapse be prevented?
There is no certain way to prevent uterine prolapse. However, the following can help
lower your risk:
Lose weight, if you’re overweight
Follow a diet rich in fiber and fluids to prevent constipation and straining
Avoid heavy lifting
Quit smoking, if you smoke
Seek prompt treatment for a chronic cough, which can place extra
pressure on your pelvic organs
Do Kegel exercises to strengthen your pelvic floor muscles
33.
These actions may also help if you already have uterineprolapse.
See your healthcare provider when symptoms first start
to bother you.
Don’t wait until your discomfort becomes severe.
Regular pelvic exams can help detect uterine prolapse
in its early stages
34.
Complicationsit can cause a few problems, such as:
Bladder control problems (urinary incontinence)
A kink in the urethra, the tube that carries your urine outside your body. ...
Bowel control problems (fecal incontinence), with liquid or solid stools coming
out.
Problems having bowel movements when stools get trapped.
Pain during sex.























 medicine
medicine