Similar presentations:
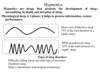
General anaesthetics
1. General anaesthetics
GENERAL ANAESTHETICS2.
General anaesthetics (GAs) are drugs which produce reversible loss of allsensation and consciousness.
The cardinal features of general anaesthesia are:
• Loss of all sensation, especially pain
• Sleep (unconsciousness) and amnesia
• Immobility and muscle relaxation
• Abolition of somatic and autonomic reflexes.
The balanced anaesthesia is achieved by using combination of inhaled and
i.v. drugs.
The first GAs were nitrous oxide (laughing gas in 1844. The first IV
anaesthetic thiopentone was introduced in 1935.
3.
Mechanismof action of anaesthetics
Anaesthetic potency correlates well with lipid solubility.
Anaesthetics might dissolve in the lipid bilayer of the
cell membranes and somehow produce anaesthesia by
expanding the membrane or increasing its fluidity.
It is now believed that anaesthetics bind to a hydrophobic
area of a protein (e.g. ion channel, receptor) and inhibit
its normal function.
Anaesthetics can inhibit the function of glutamate
receptors and can enhance γ‐aminobutyric acid
(GABA)ergic transmission.
4.
Properties of an ideal anaestheticA. For the patient:
It should be pleasant, nonirritating, should not cause
nausea or vomiting.
Induction and recovery should be fast with no after
effects.
B. For the surgeon:
It should provide adequate analgesia, immobility and
muscle relaxation.
It should be noninflammable and nonexplosive.
5.
C. For the anaesthetist:Its administration should be easy, controllable.
Heart, liver and other organs should not be affected.
It should be potent so that low concentrations are needed
and oxygenation of the patient does not suffer.
Rapid adjustments in depth of anaesthesia should be
possible.
It should be cheap, stable and easily stored.
6.
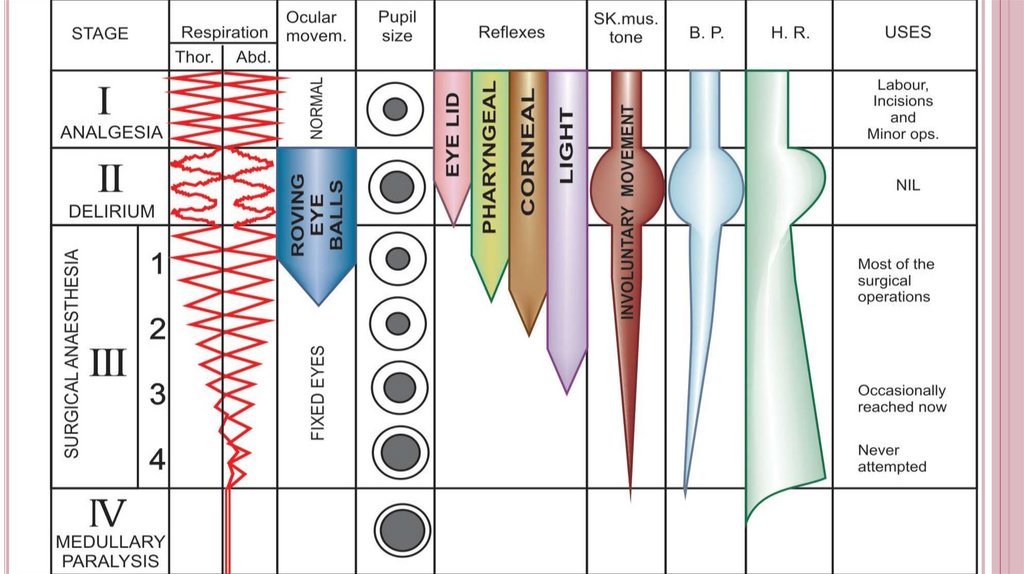
Stages of general anaesthesiaI. Stage of analgesia starts from beginning of anaesthetic inhalation
and lasts up to the loss of consciousness. Pain is progressively
abolished. Patient remains conscious.
II. Stage of delirium. Apparent excitement is seen—patient may
shout, struggle and hold his breath; muscle tone increases, jaws are
tightly closed, breathing is jerky; vomiting, involuntary micturition
or defecation may occur. Heart rate and BP may rise and pupils
dilate due to sympathetic stimulation.
III. Surgical anaesthesia extends from onset of regular respiration to
cessation of spontaneous breathing. This has been divided into 4
planes. These stages are not obvious with currently used
anaesthetics.
7.
8.
General anaesthesia usually involves the administration of different drugsFor premedication,
For induction of anaesthesia, and
For maintenance of anaesthesia.
Premedication has 4 main aims:
The prevention of the parasympathomimetic effects of anaesthesia
(bradycardia, bronchial secretion): Muscarinic blockers – Atropine
The reduction of pain: Opioid analgesics, e.g. morphine
The relief from anxiety: Benzodiazepines produce anxiolysis and amnesia
and are used in particularly anxious patients.
Postoperative antiemesis: The dopamine antagonist droperidol and
metoclopramide are widely used for this purpose and is effective against
opioid‐induced emesis.
9.
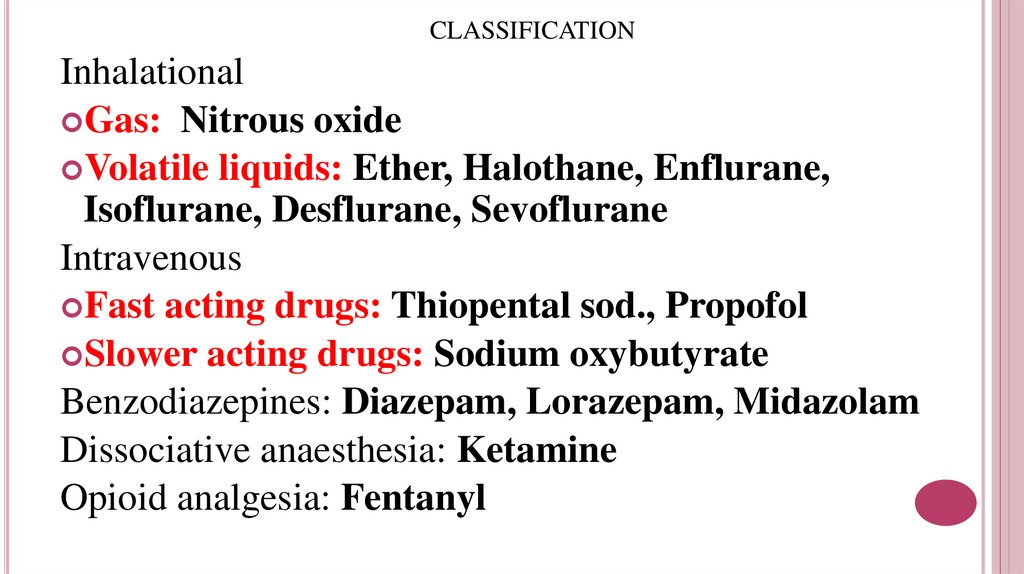
CLASSIFICATIONInhalational
Gas: Nitrous oxide
Volatile liquids: Ether, Halothane, Enflurane,
Isoflurane, Desflurane, Sevoflurane
Intravenous
Fast acting drugs: Thiopental sod., Propofol
Slower acting drugs: Sodium oxybutyrate
Benzodiazepines: Diazepam, Lorazepam, Midazolam
Dissociative anaesthesia: Ketamine
Opioid analgesia: Fentanyl
10.
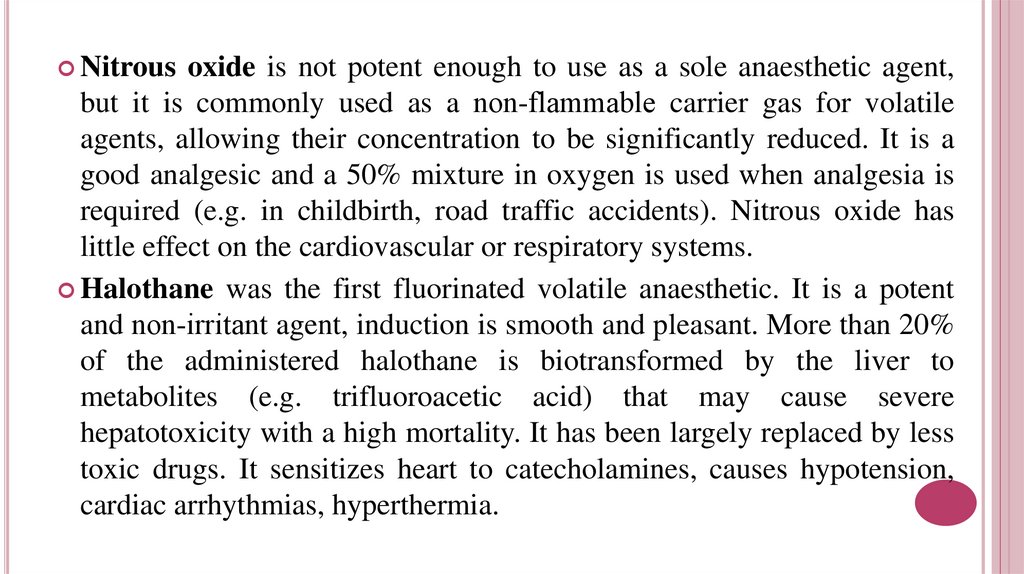
Nitrousoxide is not potent enough to use as a sole anaesthetic agent,
but it is commonly used as a non‐flammable carrier gas for volatile
agents, allowing their concentration to be significantly reduced. It is a
good analgesic and a 50% mixture in oxygen is used when analgesia is
required (e.g. in childbirth, road traffic accidents). Nitrous oxide has
little effect on the cardiovascular or respiratory systems.
Halothane was the first fluorinated volatile anaesthetic. It is a potent
and non‐irritant agent, induction is smooth and pleasant. More than 20%
of the administered halothane is biotransformed by the liver to
metabolites (e.g. trifluoroacetic acid) that may cause severe
hepatotoxicity with a high mortality. It has been largely replaced by less
toxic drugs. It sensitizes heart to catecholamines, causes hypotension,
cardiac arrhythmias, hyperthermia.
11.
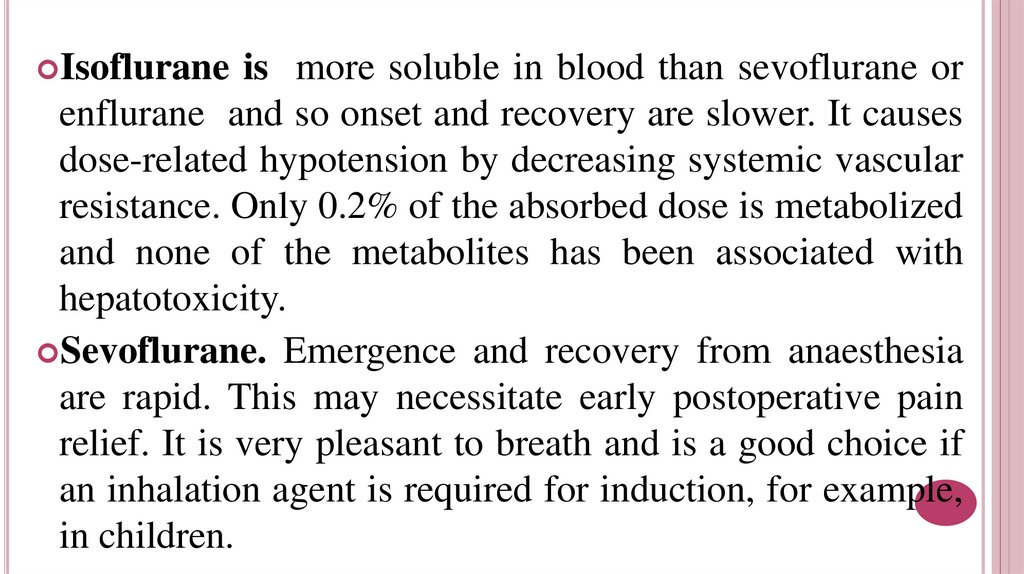
Isofluraneis more soluble in blood than sevoflurane or
enflurane and so onset and recovery are slower. It causes
dose-related hypotension by decreasing systemic vascular
resistance. Only 0.2% of the absorbed dose is metabolized
and none of the metabolites has been associated with
hepatotoxicity.
Sevoflurane. Emergence and recovery from anaesthesia
are rapid. This may necessitate early postoperative pain
relief. It is very pleasant to breath and is a good choice if
an inhalation agent is required for induction, for example,
in children.
12.
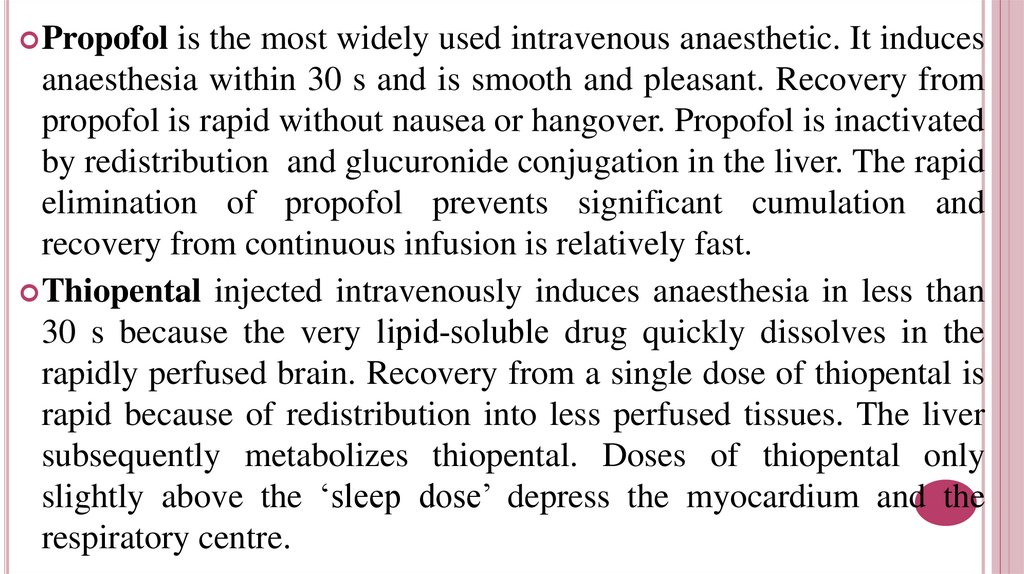
Propofolis the most widely used intravenous anaesthetic. It induces
anaesthesia within 30 s and is smooth and pleasant. Recovery from
propofol is rapid without nausea or hangover. Propofol is inactivated
by redistribution and glucuronide conjugation in the liver. The rapid
elimination of propofol prevents significant cumulation and
recovery from continuous infusion is relatively fast.
Thiopental injected intravenously induces anaesthesia in less than
30 s because the very lipid‐soluble drug quickly dissolves in the
rapidly perfused brain. Recovery from a single dose of thiopental is
rapid because of redistribution into less perfused tissues. The liver
subsequently metabolizes thiopental. Doses of thiopental only
slightly above the ‘sleep dose’ depress the myocardium and the
respiratory centre.
13.
Ketaminemay be given by intramuscular or intravenous
injection. It is analgesic in subanaesthetic doses, but
often causes hallucinations. It induces a so called
‘dissociative anaesthesia’ characterized by profound
analgesia, immobility, amnesia with light sleep. It
increases cardiac work and blood pressure.
Sodium oxybutirate may be given intravenously or
orally. It is used for induction and base anaesthesia. The
effect persists up to 2-3 hours. It increases the brain
resistance to hypoxia.
14.
COMPLICATIONS OF GENERAL ANAESTHESIAA. During anaesthesia
Respiratory depression. Cardiac arrhythmias, asystole. Fall in BP.
Salivation, respiratory secretions. Aspiration of gastric contents: acid
pneumonitis. Laryngospasm and asphyxia.
Delirium, convulsions and other excitatory effects.
B. After anaesthesia
Nausea and vomiting. Pneumonia, atelectasis. Organ toxicities: liver,
kidney damage.
Persisting sedation: impaired psychomotor function.
Cognitive defects.
15. ANTIEPILEPTIC DRUGS
Epilepsy is a chronic disease in which seizures result from theabnormal discharge of cerebral neurones. The seizures are
classified:
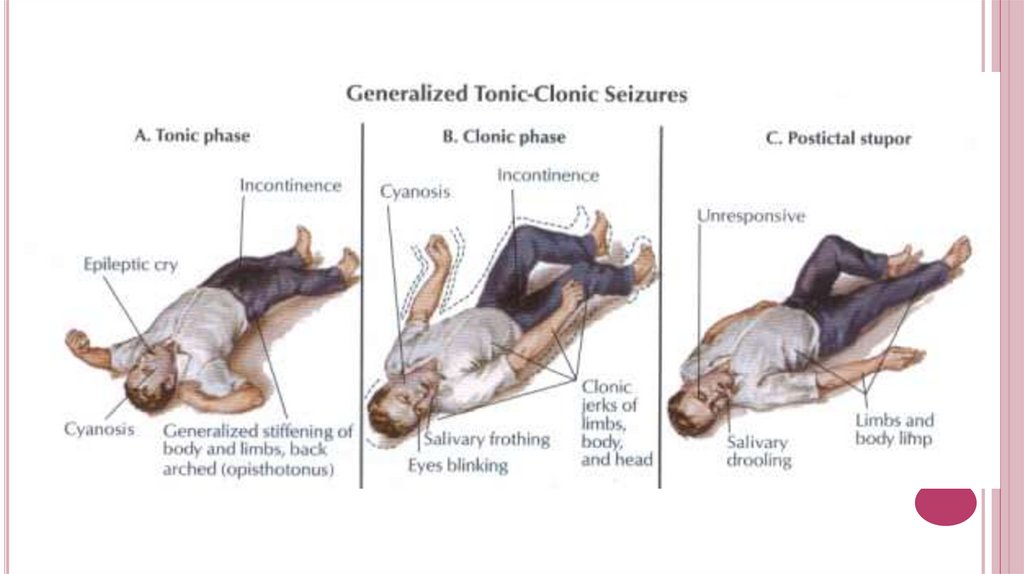
Generalised tonic-clonic seizures: commonest, lasts 1–2 min. The
usual sequence is aura—cry—unconsciousness—tonic spasm of all
body muscles—clonic jerking followed by prolonged sleep and
depression of all CNS functions.
Partial seizures: lasts 1/2–1 min. Often secondary. Convulsions are
confined to a group of muscles or localized sensory disturbance
depending on the area of cortex involved in the seizure, without loss
of consciousness.
16.
17.
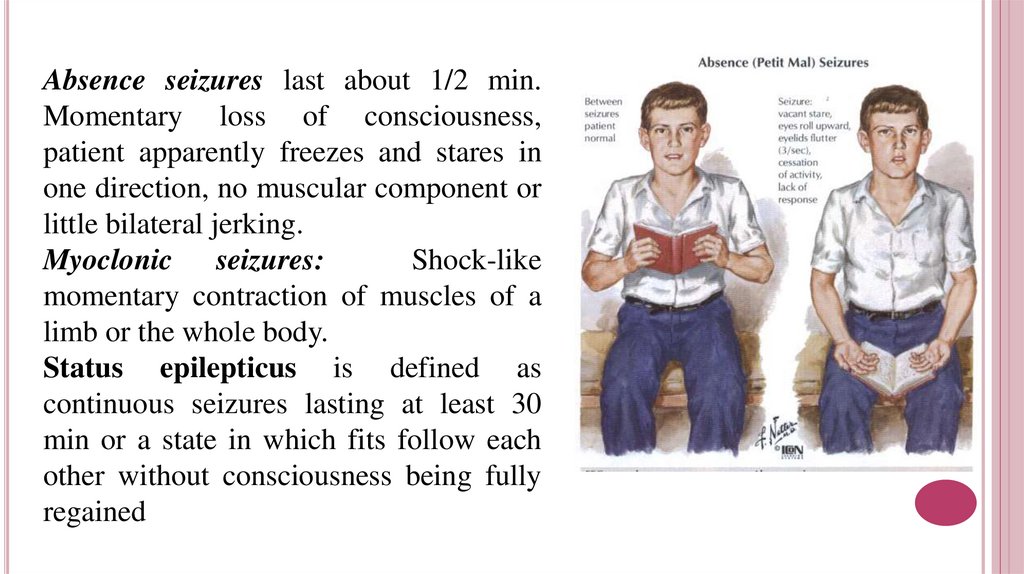
Absence seizures last about 1/2 min.Momentary loss of consciousness,
patient apparently freezes and stares in
one direction, no muscular component or
little bilateral jerking.
Myoclonic seizures:
Shock-like
momentary contraction of muscles of a
limb or the whole body.
Status epilepticus is defined as
continuous seizures lasting at least 30
min or a state in which fits follow each
other without consciousness being fully
regained
18.
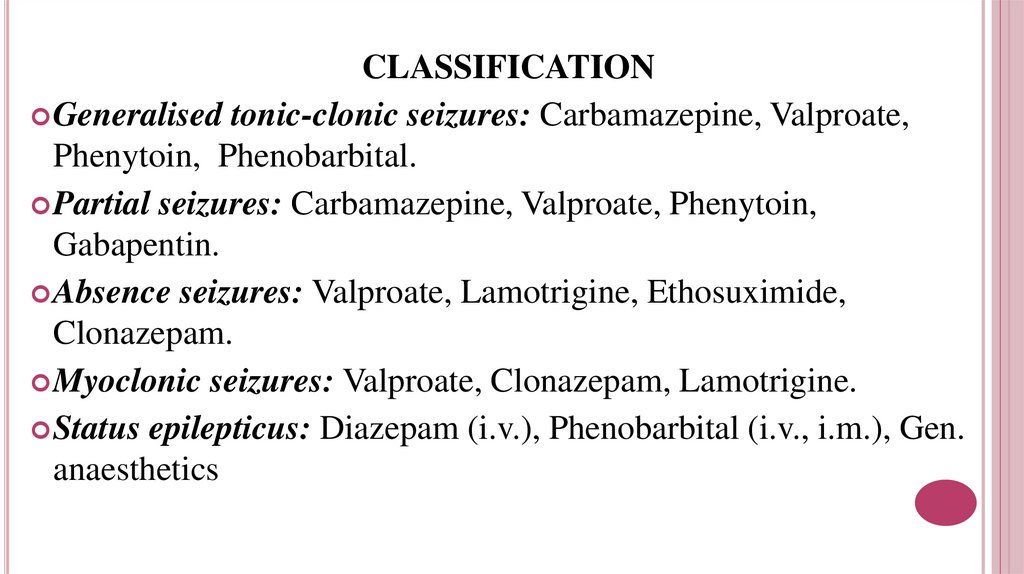
CLASSIFICATIONGeneralised tonic-clonic seizures: Carbamazepine, Valproate,
Phenytoin, Phenobarbital.
Partial seizures: Carbamazepine, Valproate, Phenytoin,
Gabapentin.
Absence seizures: Valproate, Lamotrigine, Ethosuximide,
Clonazepam.
Myoclonic seizures: Valproate, Clonazepam, Lamotrigine.
Status epilepticus: Diazepam (i.v.), Phenobarbital (i.v., i.m.), Gen.
anaesthetics
19.
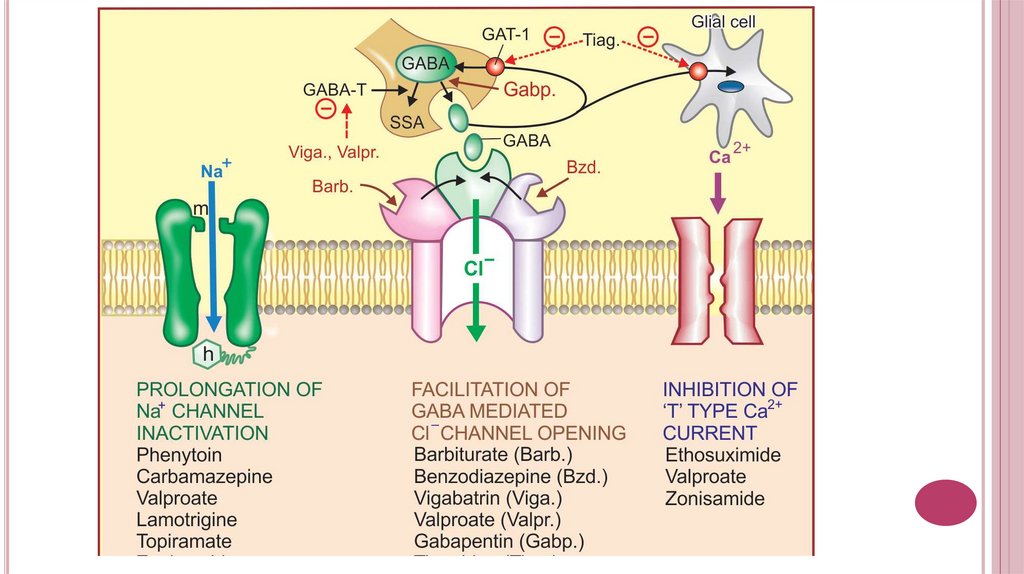
Carbamazepine, lamotrigine, valproate, phenytoin blockneuronal Na+ channels, ↓ axonal conduction.
Barbiturates and benzodiazepins ↑inhibitory tone by facilitation
of GABA-mediated hyperpolarisation.
Valproate also seems to increase GABAergic central inhibition by
stimulation of glutamic acid decarboxylase activity and/or
inhibition of GABA‐Transaminase.
Lamotrigine ↓excitatory effects of glutamic acid (block of NMDA
receptors)
Ethosuximide and valproate ↓presynaptic Ca₂+ influx through
type-T channels in thalamic neurons.
20.
21.
Pharmacokinetics – variable absorption,induction of P450s;
Side effects: CNS depression, gingival hyperplasia,
osteomalacia (↓ vit.D), megaloblastic anemia (↓ folate),
hirsutism, teratogenicity (cleft lip and palate).
Carbamazepine is also used for trigeminal neuralgia.
Induces P450s.
Side effects: CNS depression, osteomalacia (↓ vit.D),
megaloblastic anemia (↓ folate, aplastic anemia), exfoliative
dermatitis, ↑ ADH secretion (dilutional hyponatremia),
teratogenicity (cleft lip and palate, spinal bifida).
Phenytoin.
22.
Valproatecan be used for migraines. Inhibits P450s. Side
effects: hepatotoxicity, thrombocytopenia, pancretitis,
alopecia, teratogenicity (spinal bifida).
Ethosuximide. Side effects: nausea, vomiting, leukopenia.
Lamotrigine. Side effects: sleepiness, dizziness, diplopia,
ataxia, vomiting and Steven-Johnson syndrome.
Gabapentin can be used for neuropathic pain. Side effects are
mild sedation, tiredness, dizziness and unsteadiness.
Anticonvulsants
are additive with other CNS depressants.
Avoid abrupt withdrawal, which may precipitate seizures.
23.
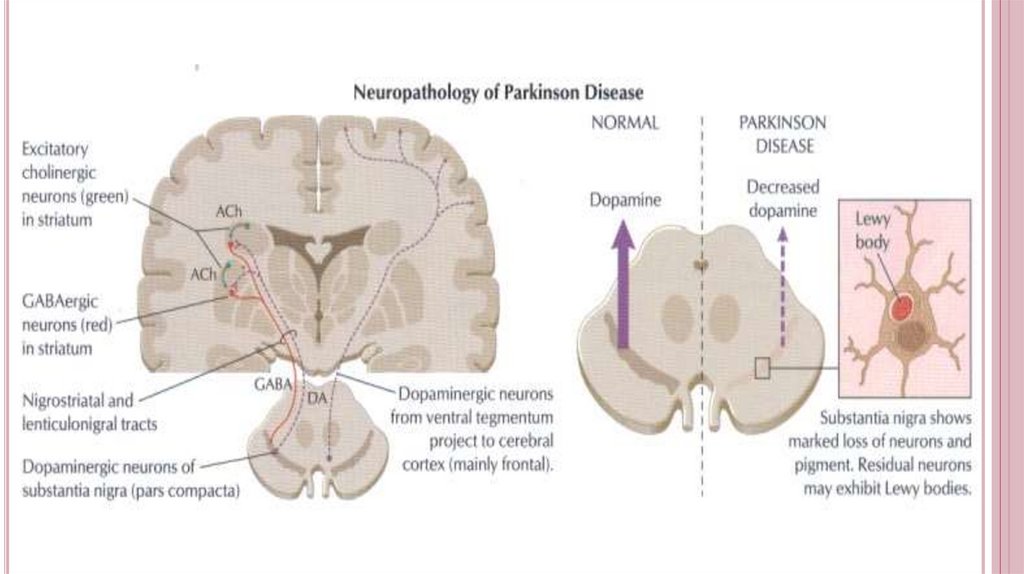
Antiparkinsonian Drugs.These are drugs that have a therapeutic effect in
parkinsonism.
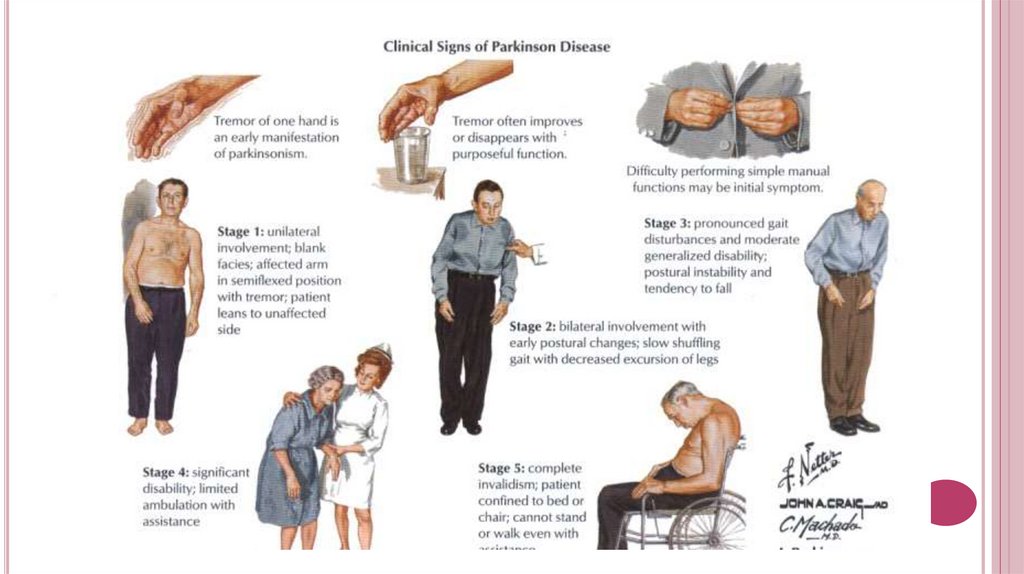
Parkinsonism. It is an extrapyramidal motor
disorder characterized by rigidity, tremor and
hypokinesia.
Pathology: degeneration of nigrostriatal dopamine
tracts with imbalance between dopamine (↓) and
Ach (↑).
24.
25.
26.
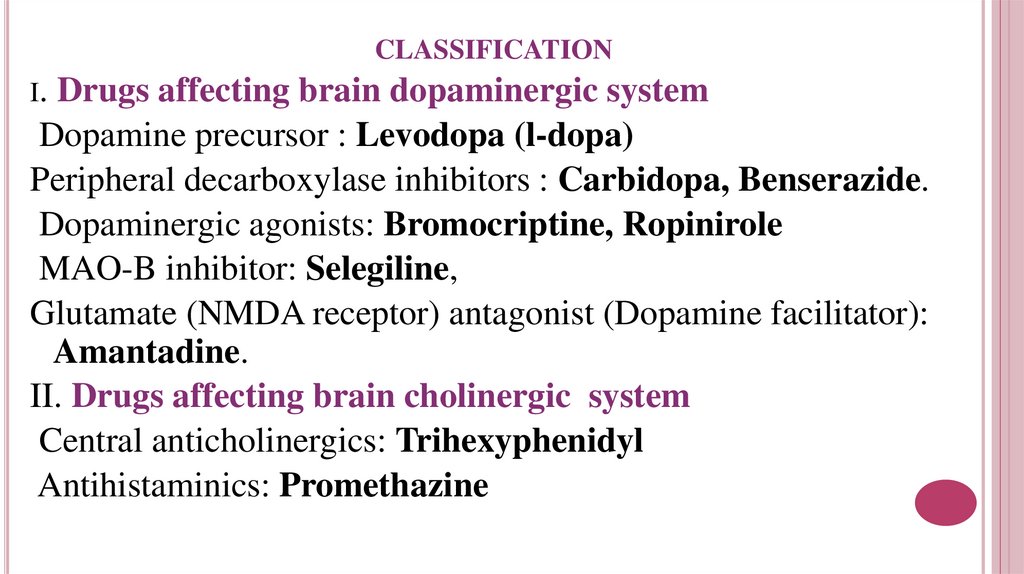
CLASSIFICATIONI.
Drugs affecting brain dopaminergic system
Dopamine precursor : Levodopa (l-dopa)
Peripheral decarboxylase inhibitors : Carbidopa, Benserazide.
Dopaminergic agonists: Bromocriptine, Ropinirole
MAO-B inhibitor: Selegiline,
Glutamate (NMDA receptor) antagonist (Dopamine facilitator):
Amantadine.
II. Drugs affecting brain cholinergic system
Central anticholinergics: Trihexyphenidyl
Antihistaminics: Promethazine
27.
28.
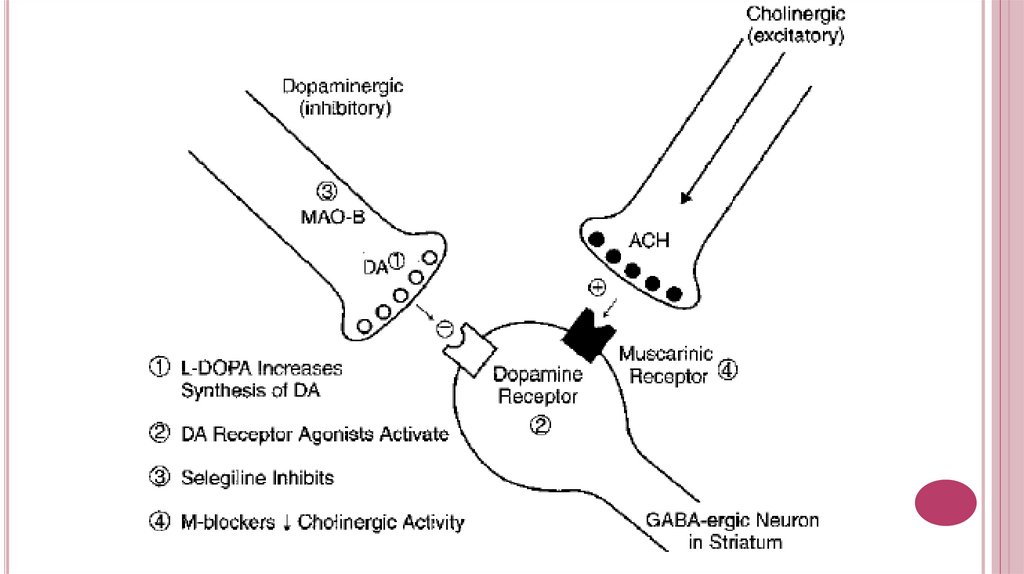
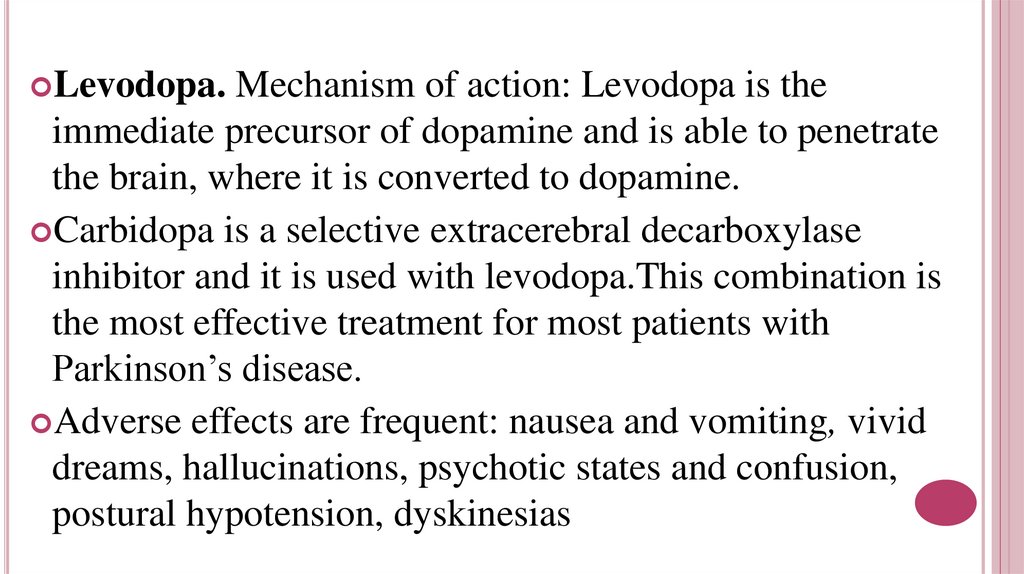
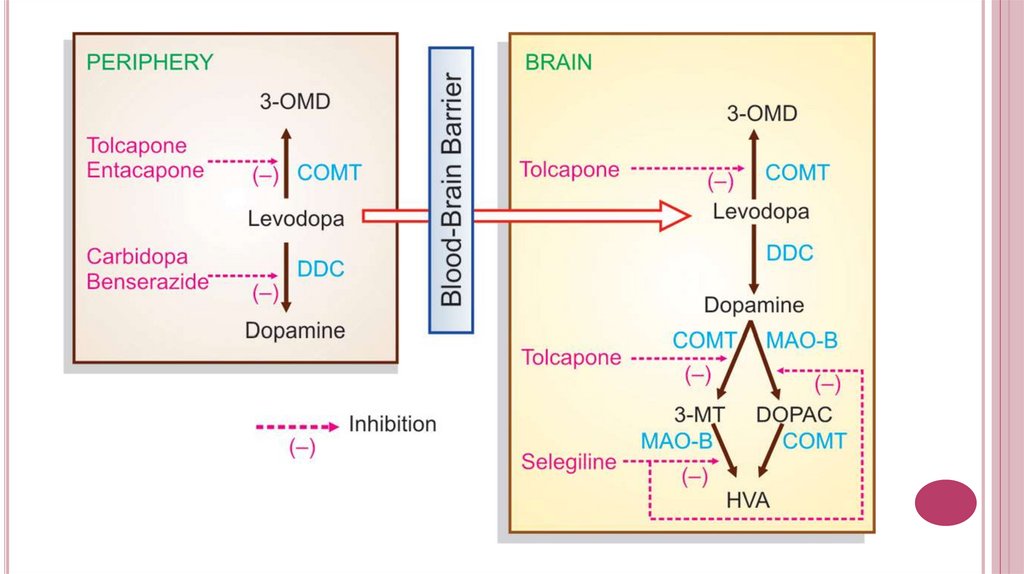
Levodopa.Mechanism of action: Levodopa is the
immediate precursor of dopamine and is able to penetrate
the brain, where it is converted to dopamine.
Carbidopa is a selective extracerebral decarboxylase
inhibitor and it is used with levodopa.This combination is
the most effective treatment for most patients with
Parkinson’s disease.
Adverse effects are frequent: nausea and vomiting, vivid
dreams, hallucinations, psychotic states and confusion,
postural hypotension, dyskinesias
29.
30.
The DA agonists can act on striatal DA receptorsBromocriptine is a potent agonist on D2receptors.
Side effects: vomiting, hallucinations, hypotension, nasal
stuffiness, conjunctival injection. Marked fall in BP with the
‘first dose’ has occurred in some patients, especially those on
antihypertensive medication.
Ropinirole is а selective D2/D3 receptor agonist. Side
effects: nausea, dizziness, hallucinations and postural
hypotension
31.
Amantadinehas muscarinic blocking actions and
probably increases dopamine release. It has modest
antiparkinsonian effects in a few patients, but tolerance
soon occurs.
Side effects: atropine-like.
Selegiline selectively inhibits MAO-B present in the
brain and reduces the metabolism of dopamine in the
brain and potentiates the actions of levodopa.
Side effects: postural hypotension, nausea,confusion,
insomnia and agitation.
32.
Muscarinicantagonists produce a modest
improvement in the early stages of Parkinson’s
disease.
Adverse effects: dry mouth, urinary retention and
constipation. Impairment of memory, organic
confusional states and blurred vision are more common
in the elderly.
The antihistaminics are less efficacious than
anticholinergics, but are better tolerated by older
patients. Their sedative action also helps.