Similar presentations:
Hypnotics. Classification of hypnotics
1. Hypnotics
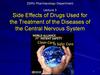
Hypnotics are drugs that promote the development of sleep,normalizing its depth and duration of sleep.
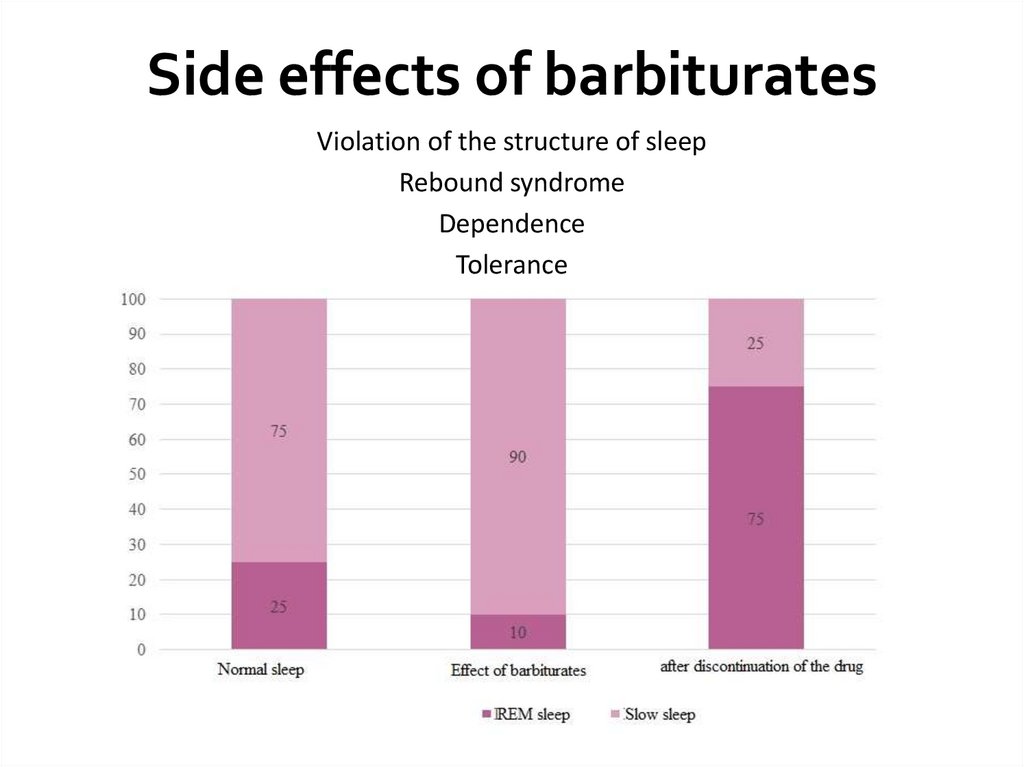
Physiological sleep is 2-phase: it helps to process information, restore
performance.
Slow-wave (Orthodox) sleep 75% of the total duration of a
night's sleep
REM (paradoxical) sleep 25% of the total duration of a
night's sleep
Types of sleep disorders:
Difficulty falling asleep (juvenile type of insomnia)
Shortened sleep
Sleep is intermittent with frequent awakenings
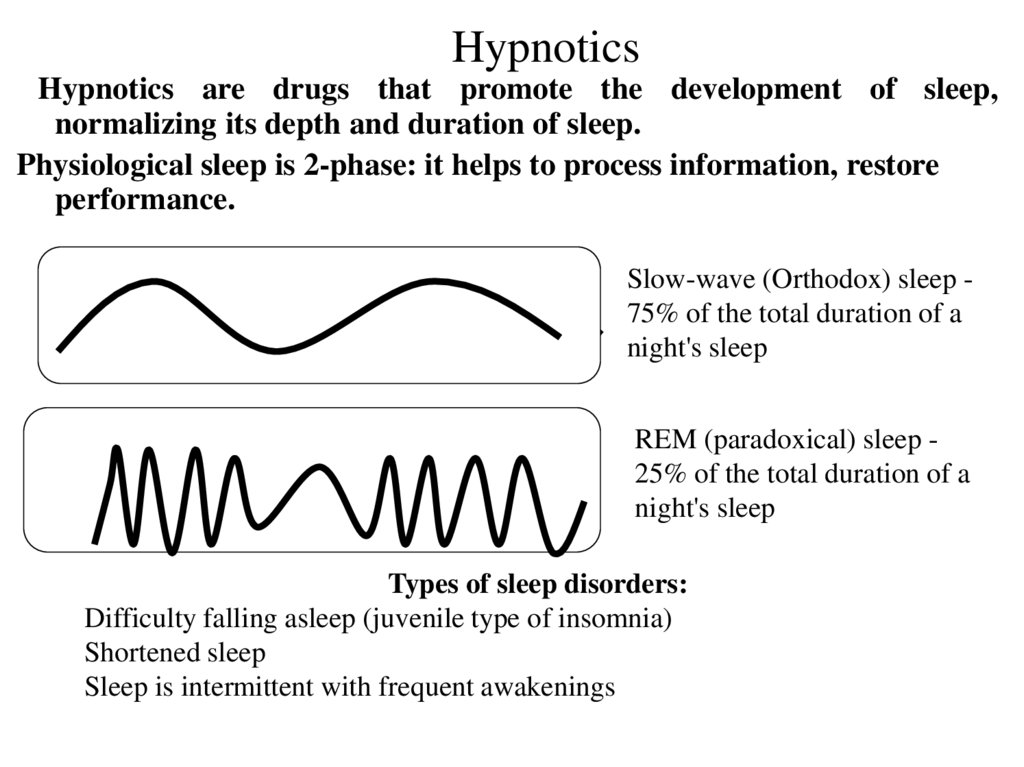
2. Classification of Hypnotics
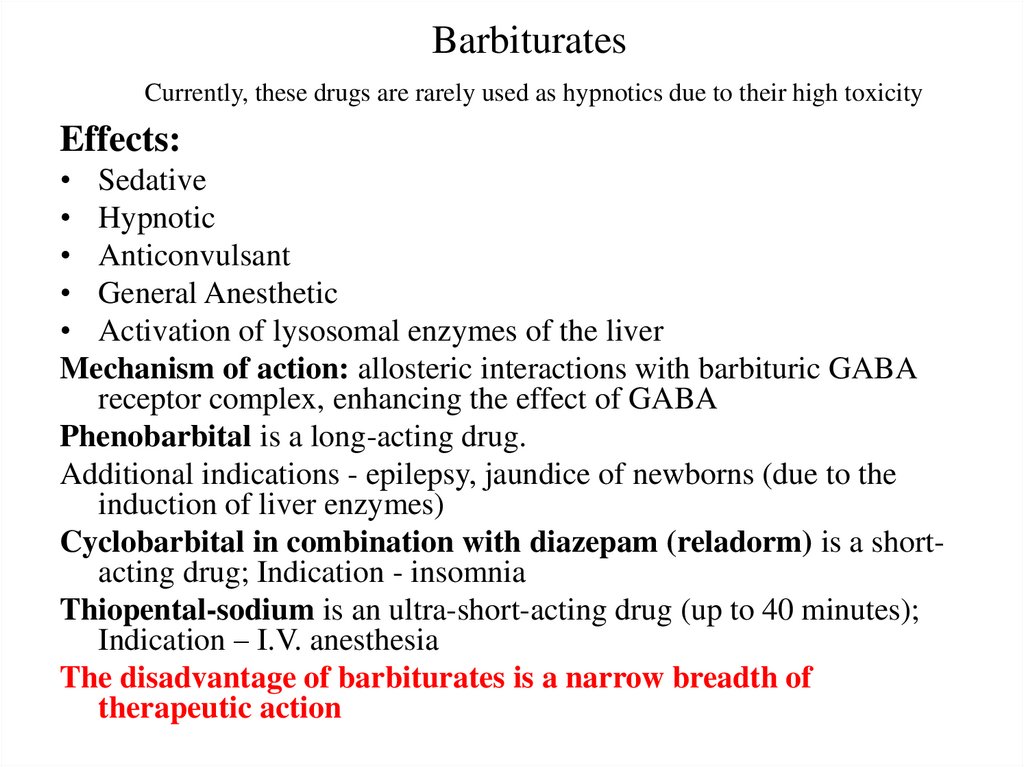
3. Barbiturates Currently, these drugs are rarely used as hypnotics due to their high toxicity
Effects:• Sedative
• Hypnotic
• Anticonvulsant
• General Anesthetic
• Activation of lysosomal enzymes of the liver
Mechanism of action: allosteric interactions with barbituric GABA
receptor complex, enhancing the effect of GABA
Phenobarbital is a long-acting drug.
Additional indications - epilepsy, jaundice of newborns (due to the
induction of liver enzymes)
Cyclobarbital in combination with diazepam (reladorm) is a shortacting drug; Indication - insomnia
Thiopental-sodium is an ultra-short-acting drug (up to 40 minutes);
Indication – I.V. anesthesia
The disadvantage of barbiturates is a narrow breadth of
therapeutic action
4. Side effects of barbiturates
Violation of the structure of sleepRebound syndrome
Dependence
Tolerance
5. Acute barbiturate poisoning
The picture of acute poisoning:A rapid increase in symptoms of CNS depression, sleep
goes into a coma.
Coma: deep depression of the Central nervous system
with loss of consciousness, depression of skeletal muscle
tone, inhibition of reflexes, loss of all types of sensitivity.
Death occurs from the suppression of the vital centers of
the medulla oblongata: the respiratory center and the
vasomotor center
Help:
Gastric lavage, adsorbents, laxatives
Analeptics (Bemegride), artificial lung ventilation
Forced diuresis (I.V. NaHCO3 + furosemide)
Hemosorbents (Gemodez), hemodialysis
Symptomatic treatment
6. Benzodiazepines and Zopiclone
Mechanism of action: excitation of benzodiazepinereceptors, increased affinity of GABA to GABA
receptors
Indications: all types of insomnia, including in patients
with neuroses, epilepsy, etc.
Side effects:
Violation of the structure of sleep
Rebound syndrome
Dependence
Tolerance
7. Tranquilizers as sleeping pills have a number of advantages over barbiturates:
• Less influence on the structure of sleep• After application, the person is easily
awakened
• Less of rebound syndrome
• Less cumulated. Less risk of poisoning
• Do not interfere with liver function
• Do not violate the functions of the CVS
• They have a great breadth of therapeutic action
8.
Doxylamine-
-
-
- Central H1-blocker, to a lesser extent M-ChB;
Effects - sedative, hypnotic, duration of action 6-8
hours;
Indications - insomnia, itching;
Contraindication-glaucoma;
Side effects: drowsiness, impaired coordination of
movements, mydriasis, paresis of accommodation,
constipation, urinary retention, dry mouth.
Unlike barbiturates and benzodiazepines, it does not
affect the structure of sleep
9. Melatonin (“Melaxen”) Synthetic analog of the natural peptide hormone of the epiphysis melatonin
Indications for use:Insomnia
Violation of daily biorhythms
when changing time zones
As an adaptogen
As an immunostimulator
10. ANTIEPILEPTIC DRUGS
Epilepsy is a chronic disease in which seizures result from theabnormal discharge of cerebral neurones. The seizures are
classified:
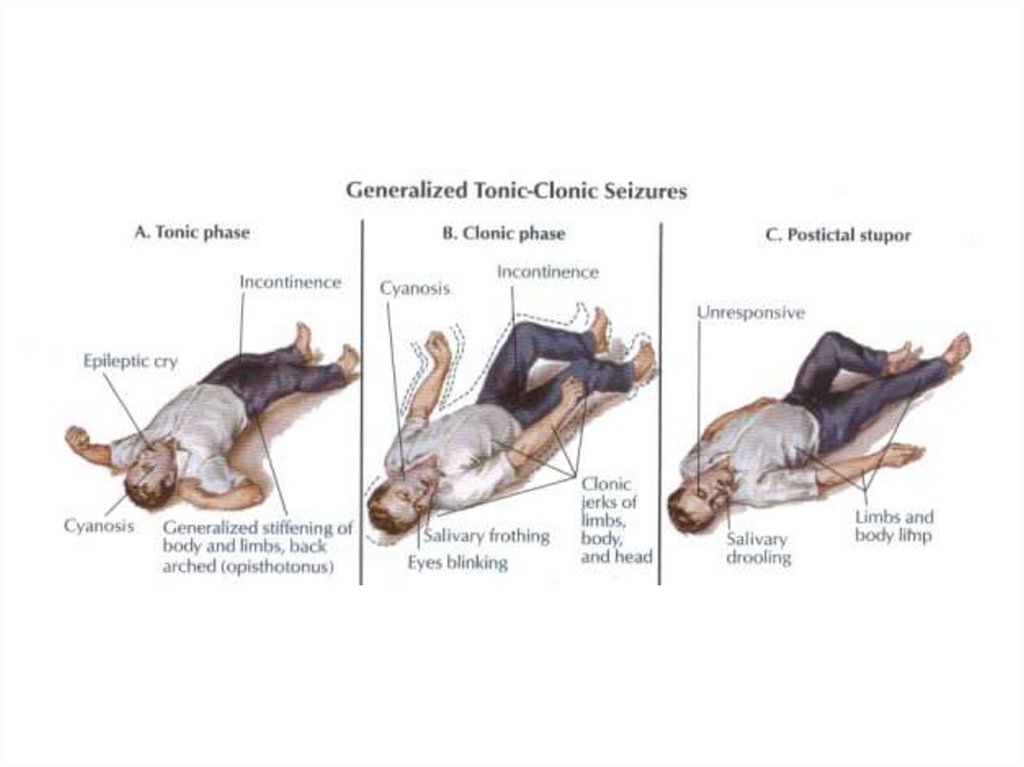
• Generalised tonic-clonic seizures: commonest, lasts 1–2 min. The
usual sequence is aura—cry—unconsciousness—tonic spasm of all
body muscles—clonic jerking followed by prolonged sleep and
depression of all CNS functions.
• Partial seizures: lasts 1/2–1 min. Often secondary. Convulsions
are confined to a group of muscles or localized sensory disturbance
depending on the area of cortex involved in the seizure, without
loss of consciousness.
11.
12.
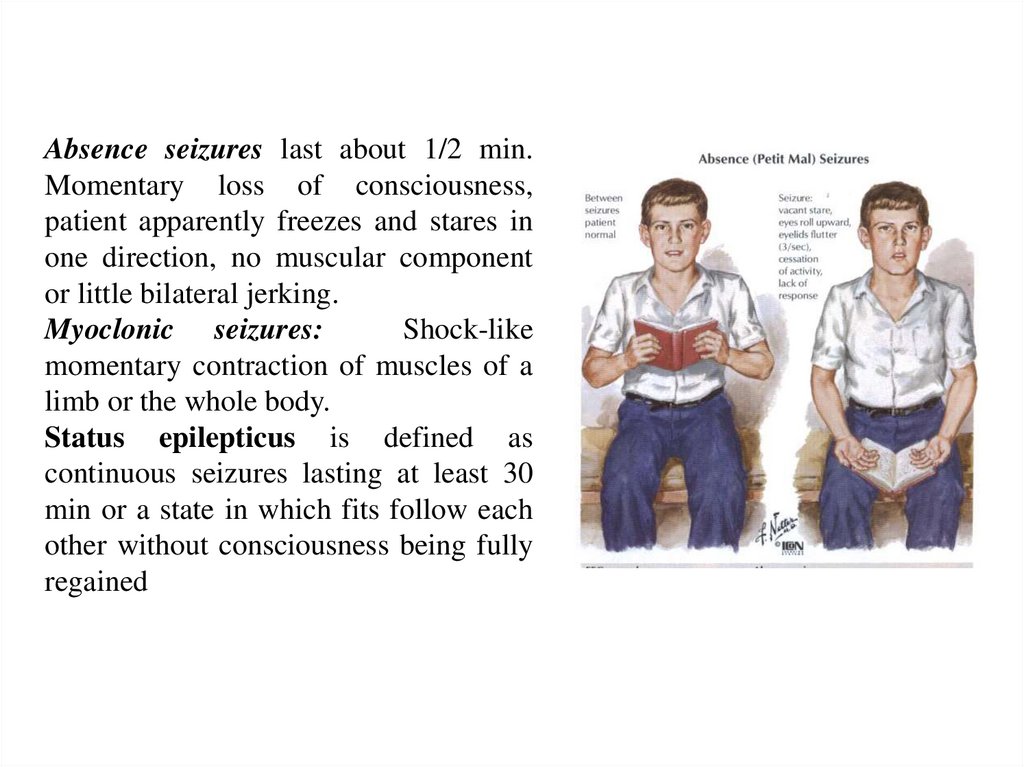
Absence seizures last about 1/2 min.Momentary loss of consciousness,
patient apparently freezes and stares in
one direction, no muscular component
or little bilateral jerking.
Myoclonic seizures:
Shock-like
momentary contraction of muscles of a
limb or the whole body.
Status epilepticus is defined as
continuous seizures lasting at least 30
min or a state in which fits follow each
other without consciousness being fully
regained
13.
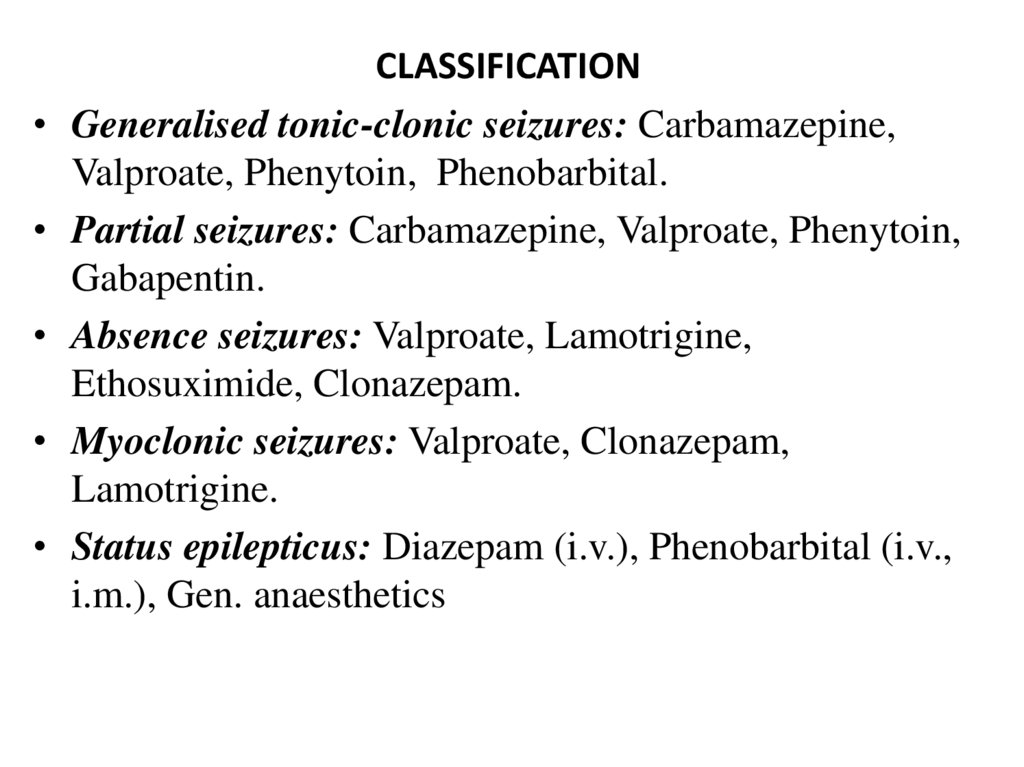
CLASSIFICATION
Generalised tonic-clonic seizures: Carbamazepine,
Valproate, Phenytoin, Phenobarbital.
Partial seizures: Carbamazepine, Valproate, Phenytoin,
Gabapentin.
Absence seizures: Valproate, Lamotrigine,
Ethosuximide, Clonazepam.
Myoclonic seizures: Valproate, Clonazepam,
Lamotrigine.
Status epilepticus: Diazepam (i.v.), Phenobarbital (i.v.,
i.m.), Gen. anaesthetics
14.
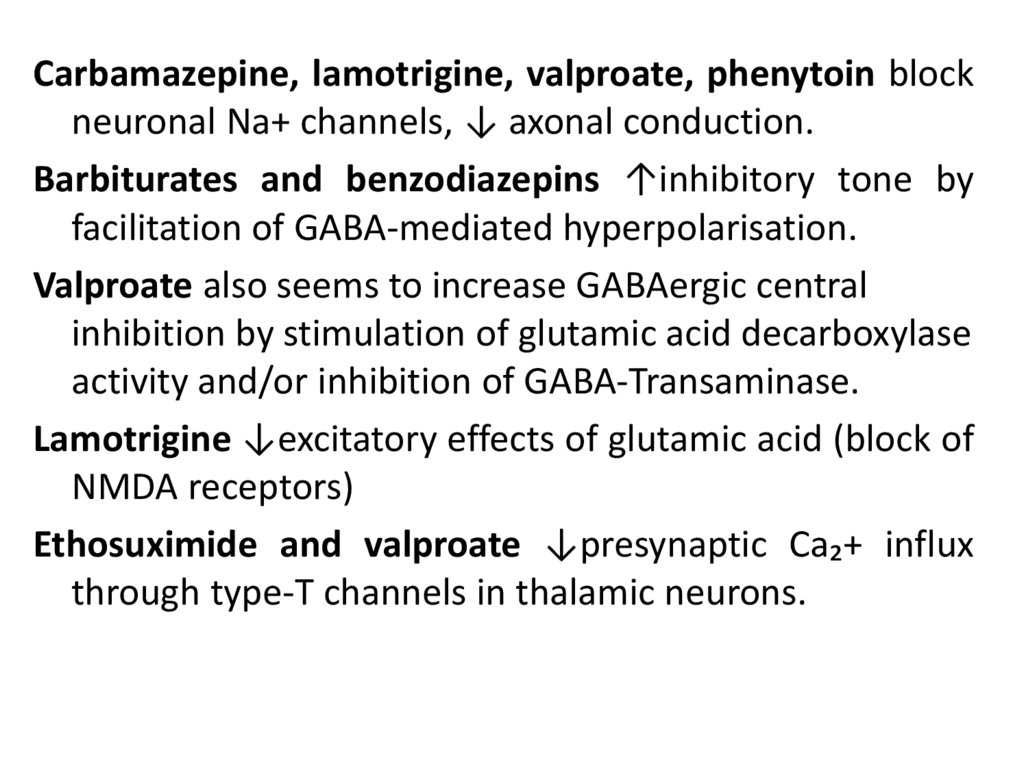
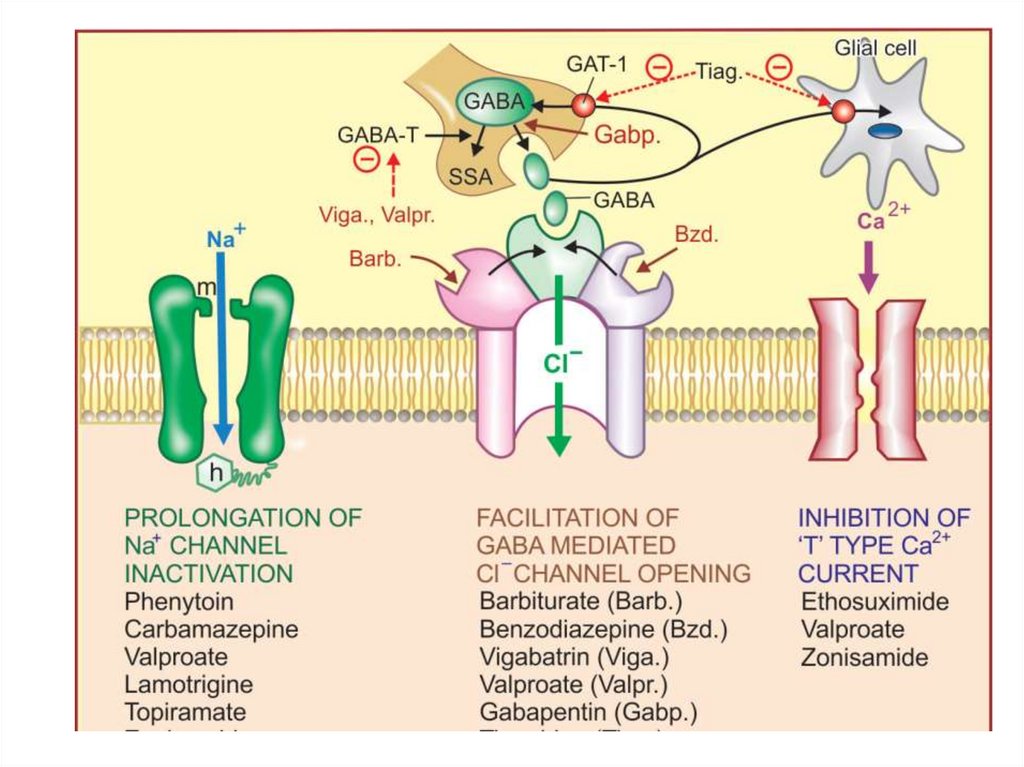
Carbamazepine, lamotrigine, valproate, phenytoin blockneuronal Na+ channels, ↓ axonal conduction.
Barbiturates and benzodiazepins ↑inhibitory tone by
facilitation of GABA-mediated hyperpolarisation.
Valproate also seems to increase GABAergic central
inhibition by stimulation of glutamic acid decarboxylase
activity and/or inhibition of GABA‐Transaminase.
Lamotrigine ↓excitatory effects of glutamic acid (block of
NMDA receptors)
Ethosuximide and valproate ↓presynaptic Ca₂+ influx
through type-T channels in thalamic neurons.
15.
16.
Phenytoin. Pharmacokinetics – variable absorption,induction of P450s;
Side effects: CNS depression, gingival hyperplasia,
osteomalacia (↓ vit.D), megaloblastic anemia (↓ folate),
hirsutism, teratogenicity (cleft lip and palate).
Carbamazepine is also used for trigeminal neuralgia.
Induces P450s.
Side effects: CNS depression, osteomalacia (↓ vit.D),
megaloblastic anemia (↓ folate, aplastic anemia),
exfoliative dermatitis, ↑ ADH secretion (dilutional
hyponatremia), teratogenicity (cleft lip and palate, spinal
bifida).
17.
Valproate can be used for migraines. Inhibits P450s. Sideeffects: hepatotoxicity, thrombocytopenia, pancretitis,
alopecia, teratogenicity (spinal bifida).
Ethosuximide. Side effects: nausea, vomiting, leukopenia.
Lamotrigine. Side effects: sleepiness, dizziness, diplopia,
ataxia, vomiting and Steven-Johnson syndrome.
Gabapentin can be used for neuropathic pain. Side effects
are mild sedation, tiredness, dizziness and unsteadiness.
Anticonvulsants are additive with other CNS depressants.
Avoid abrupt withdrawal, which may precipitate seizures.
 medicine
medicine