Similar presentations:
Psychotropic drugs
1. PSYCHOTROPIC DRUGS
Drugs of this group are used for the treatment ofmental illness:
Psychoses,
Neurotic and pseudoneurotic disoders, associated
with stress, nervousness, fear, anxiety.
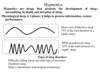
2.
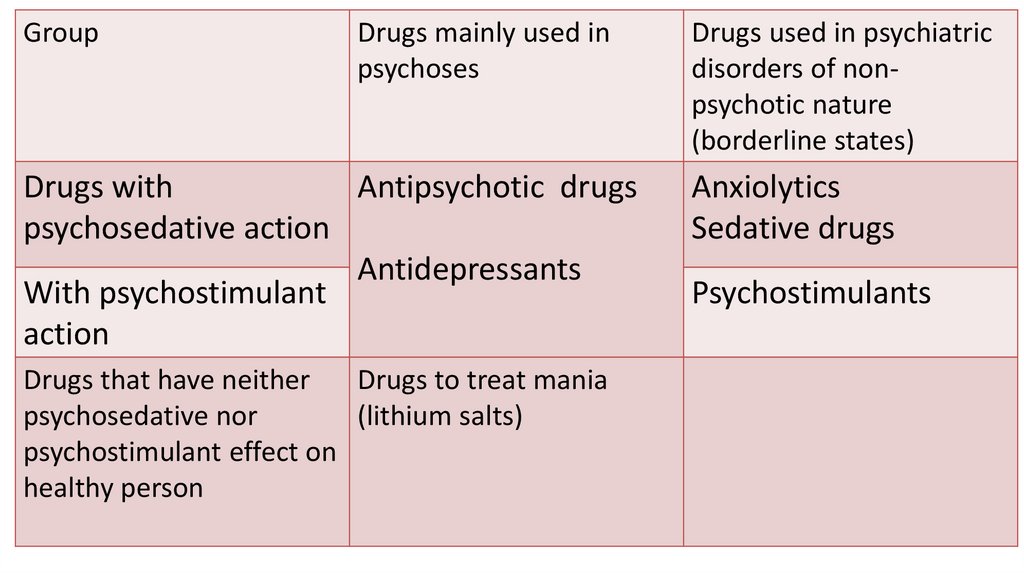
GroupDrugs mainly used in
psychoses
Drugs with
Antipsychotic drugs
psychosedative action
Antidepressants
With psychostimulant
action
Drugs that have neither
Drugs to treat mania
psychosedative nor
(lithium salts)
psychostimulant effect on
healthy person
Drugs used in psychiatric
disorders of nonpsychotic nature
(borderline states)
Anxiolytics
Sedative drugs
Psychostimulants
3.
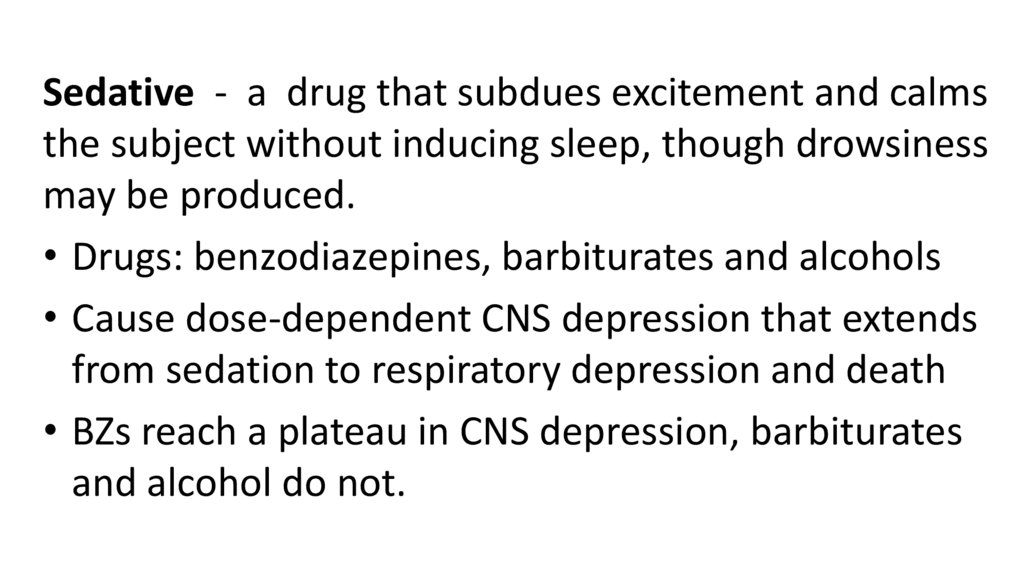
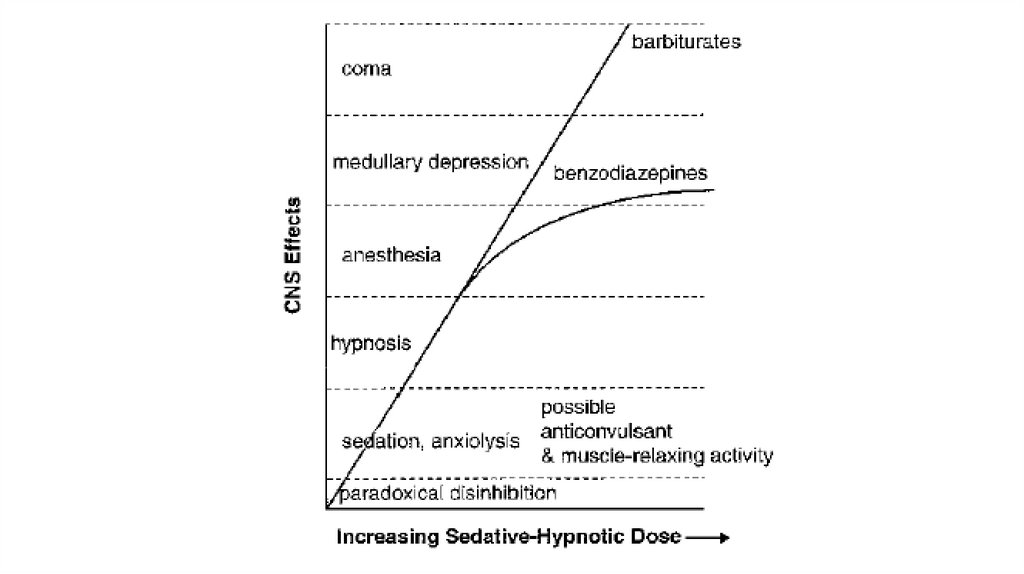
Sedative - a drug that subdues excitement and calmsthe subject without inducing sleep, though drowsiness
may be produced.
• Drugs: benzodiazepines, barbiturates and alcohols
• Cause dose-dependent CNS depression that extends
from sedation to respiratory depression and death
• BZs reach a plateau in CNS depression, barbiturates
and alcohol do not.
4.
5.
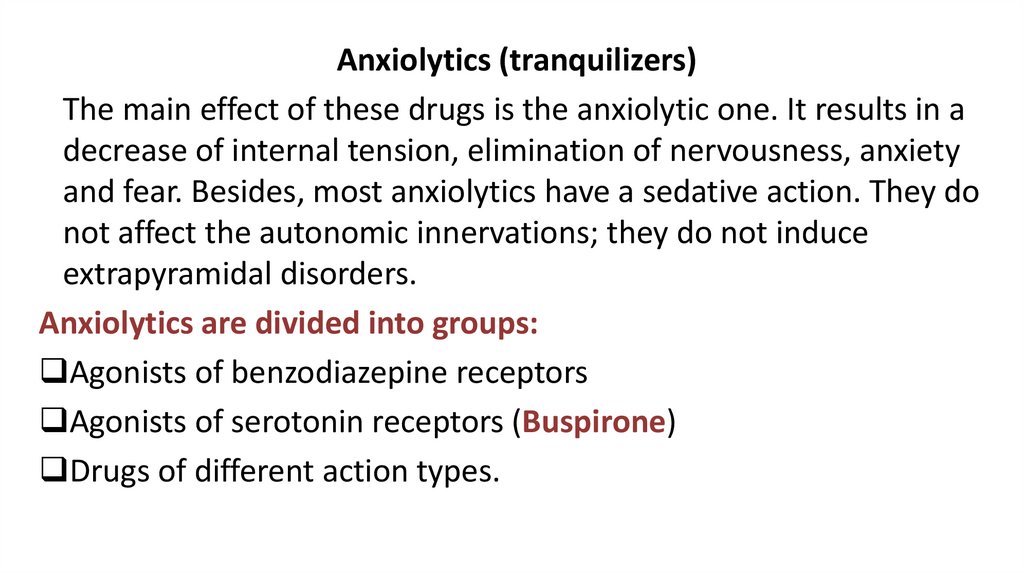
Anxiolytics (tranquilizers)The main effect of these drugs is the anxiolytic one. It results in a
decrease of internal tension, elimination of nervousness, anxiety
and fear. Besides, most anxiolytics have a sedative action. They do
not affect the autonomic innervations; they do not induce
extrapyramidal disorders.
Anxiolytics are divided into groups:
Agonists of benzodiazepine receptors
Agonists of serotonin receptors (Buspirone)
Drugs of different action types.
6.
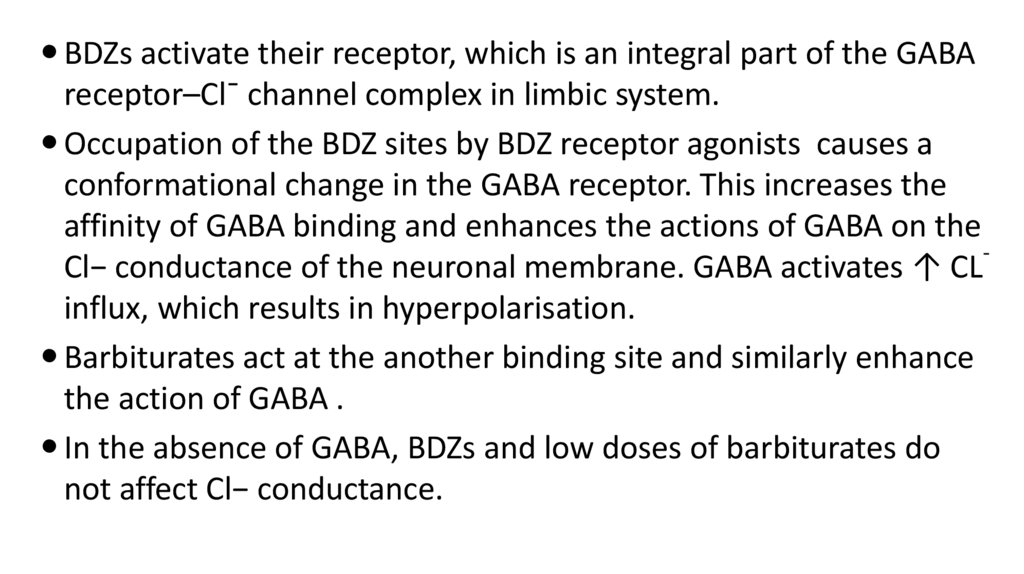
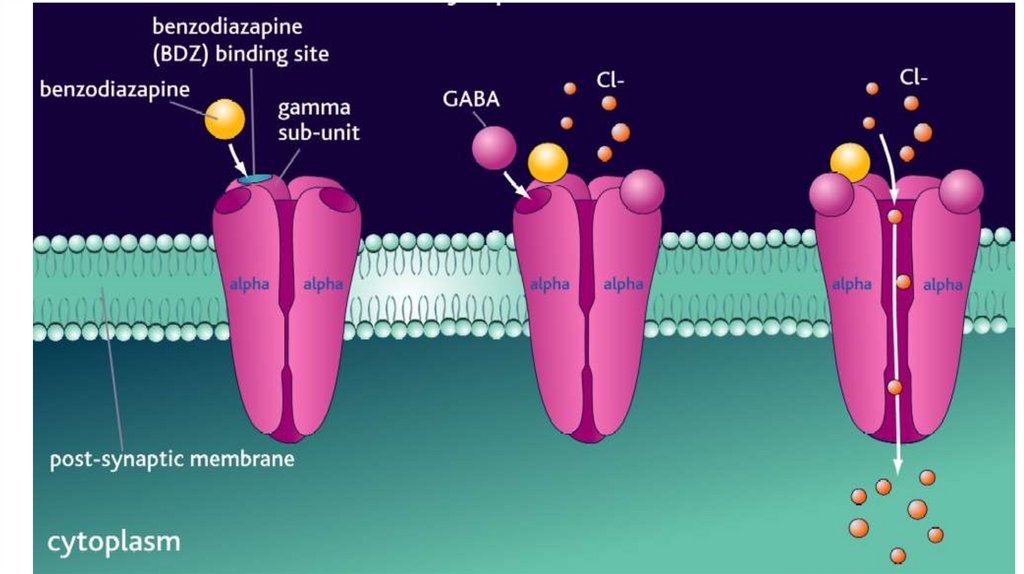
BDZs activate their receptor, which is an integral part of the GABAreceptor–Cl¯ channel complex in limbic system.
Occupation of the BDZ sites by BDZ receptor agonists causes a
conformational change in the GABA receptor. This increases the
affinity of GABA binding and enhances the actions of GABA on the
Cl− conductance of the neuronal membrane. GABA activates ↑ CL
influx, which results in hyperpolarisation.
Barbiturates act at the another binding site and similarly enhance
the action of GABA .
In the absence of GABA, BDZs and low doses of barbiturates do
not affect Cl− conductance.
7.
8.
9.
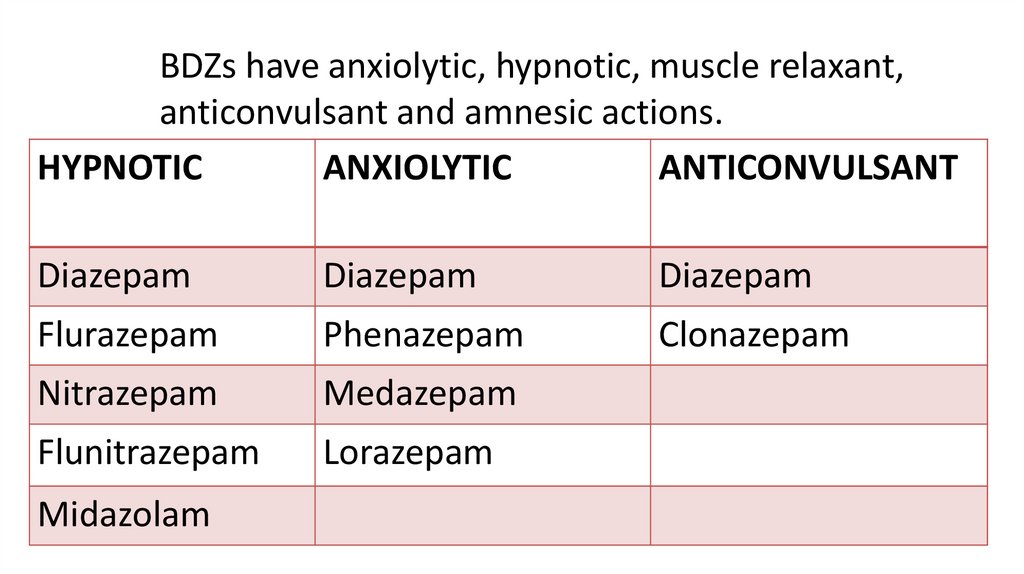
BDZs have anxiolytic, hypnotic, muscle relaxant,anticonvulsant and amnesic actions.
HYPNOTIC
ANXIOLYTIC
ANTICONVULSANT
Diazepam
Diazepam
Diazepam
Flurazepam
Phenazepam
Clonazepam
Nitrazepam
Medazepam
Flunitrazepam
Lorazepam
Midazolam
10.
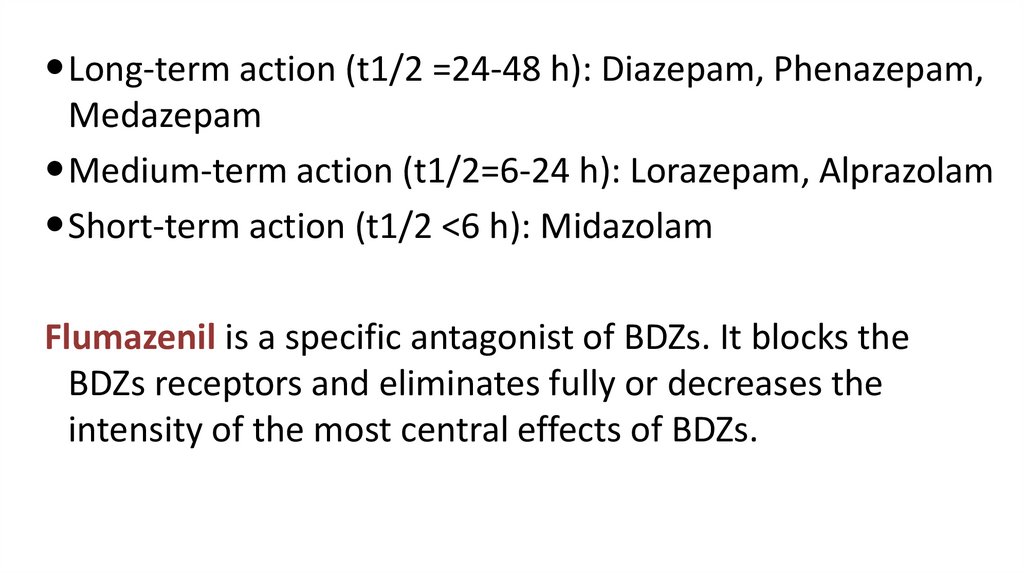
Long-term action (t1/2 =24-48 h): Diazepam, Phenazepam,Medazepam
Medium-term action (t1/2=6-24 h): Lorazepam, Alprazolam
Short-term action (t1/2 ˂6 h): Midazolam
Flumazenil is a specific antagonist of BDZs. It blocks the
BDZs receptors and eliminates fully or decreases the
intensity of the most central effects of BDZs.
11.
BDZs have marked anxiolytic and sedative properties. Byreducing emotional tension, they also promote the onset
of sleep. They are used in the treatment of neuroses,
neurosis-like conditions and insomnia.
There are BDZs with marked anxiolytic action and none or
minimal sedative-hypnotic action. Such drugs are called
“Day-time anxiolytics (tranquilizers)”. For example
Medazepam.
12.
BDZs cause muscle relaxation due to the depression ofthe spinal polysynaptic reflexes and disturbance of its
supraspinal regulation. These drugs are called central
muscular relaxants and used in neurology.
BDZs have anticonvulsant activity. They are effective in
status epilepticus.
They potentiate the CNS inhibition caused by drugs
with non-selective CNS depressants action. They are
administered for premedication before surgical
interventions.
13.
• BDZs are well absorbed from the digestive tract, easilypass through the blood-brain barrier and other biological
barriers.
• They undergo metabolism. Some metabolites have
marked and long-term anxiolytic effect.
• They bind with the plasma proteins and are deposited in
the fatty tissues.
• The kidneys are the main elimination route for the
metabolites and conjugates of BDZs.
14.
Side effectsIn high doses they can cause amnesia.
Drowsiness, delayed motor response, memory
impairment, weakness, diplopia, headache, nausea,
vomiting, dysmenorrhea, skin rashes.
During long-term therapy: tolerance and drug
dependence (psychological and physical, withdrawal
syndrome).
Teratogenic effect.
15.
Buspironе is the agonist of serotonin receptors. It hasmarked anxiolytic activity. After its administration the
effects develops slowly (over 1-2 weeks).
It has not sedative, anticonvulsive and muscle-relaxing
action.
It has a low tendency to induce tolerance and drug
dependence.
Side effects: nervousness, dizziness, headache,
paresthesias, nausea, diarrhea.
16.
SedativesBromide salts, valerian and motherwort preparations
belong to the sedative drugs. They have a moderate
calming action. They are administered for the treatment
of neuroses, increased irritability and sleeplessness.
Sodium bromide and potassium bromide are the most
widely used bromides. Their main action is associated
with the intensification of the inhibitory processes in the
brain cortex. The effect of bromide depends on the type
of nervous system (weak and strong type).
17.
Bromism – chronic poisoningThis is manifested by general lethargy, apathy, memory
disorder, skin lesions. The irritating action of bromide
leads to the inflammation of the mucous membranes,
which is associated with the cough, rhinitis, conjunctivitis
and diarrhea.
The treatment: discontinuation of bromide intake,
administration of large amount of sodium chloride,
drinking a lot of water, introduction of diuretics.
18.
Antipsychotic drugs (neuroleptic drugs) haveantipsycotic and sedative action.
Classification
1.Typical antipsychotic drugs
Phenothiazine derivatives: Chlorpromazinе,
Trifluoperazinе
Butyrophenone derivatives: Haloperidol, Droperidol
2. Atypical antipsychotic drugs:
Clozаpinе, Risperidonе
19.
Antipsychotic effect reduces the productivesymptoms of psychoses (delusions, hallucinations)
and delays further progression of schisophrenia.
The effect is associated with the block of
postsynaptic dopamine D2-receptors of mesolimbic
and mesocortical systems.
Haloperidol > Trifluoperazinе > Chlorpromazinе
Risperidonе blocks D2 and 5-НТ 2А receptors.
20.
Psychosedative actionis characterized by general sedation – elimination of
affective reactions, reduction of anxiety, nervousness,
decrease in motor activity.
is associated with their effect on the ascending reticular
formation of the brainstem, limbic system, hypothalamus.
They block α-adrenoceptors, H-receptors, serotonin
receptors and M-cholinoceptors.
Chlorpromazinе, Haloperidol, Droperidol
But Trifluoperazinе has psychostimulant action.
21.
ParkinsonismThe inhibition of the nigrostriatal transmission and
reduction of the suppression of the striatum of the
substantia nigra lead to a change of the effect of the
striatum on motor activity control. This results in the
enhancement of the activity of the spinal cord αmotoneurons, increase in muscular tone and development
of drug-indused parkinsonism (hypokinesia, rigidity,
tremor).
Typical antipsychotics cause parkinsonism.
Atypical antipsychotics cause very rarely.
22.
Other effectsHypnotic effect: superficial sleep, which is easily
interrupted by external stimuli.
Ability to potentiate action of a number of neurotropic
drugs, such as general anesthetics, hypnotics and opioid
analgetics.
Antiemetic effect, which is associated with the block of
the dopamine receptors of the trigger zone, located at the
bottom of the 4th ventricle. They can prevent vomiting
caused by antiblastomic drugs.
23.
• Chlorpromazine inhibits the center of termoregulation. Theoutcome depends on the temperature of the surrounding
environment. Often an insignificant hypothermia is observed
(due to an increase in heat loss).
If Chlorpromazine is applied under low temperatures (physical
cooling), there is a marked fall in the body temperature. This
effect is used in surgery.
Chlorpromazine has a typical muscle relaxing effect, which
results in a reduction of motor activity. It is associated with
the inhibition of supraspinal regulation of muscular tone.
24.
Cardiovascular system: Chlorpromazine decreased arterialpressure. This effect is associated with the inhibition of
hypothalamic centres, with the α-adrenoceptors blocking
effect and spasmolytic properties. Hypotension is
commonly associated with reflex tachycardia.
• Chlorpromazine possesses some M-cholinoceptors
blocking (atropine-like) properties. They result in mild
suppression of salivary, bronchial and digestive gland
secretion and also tachycardia.
25.
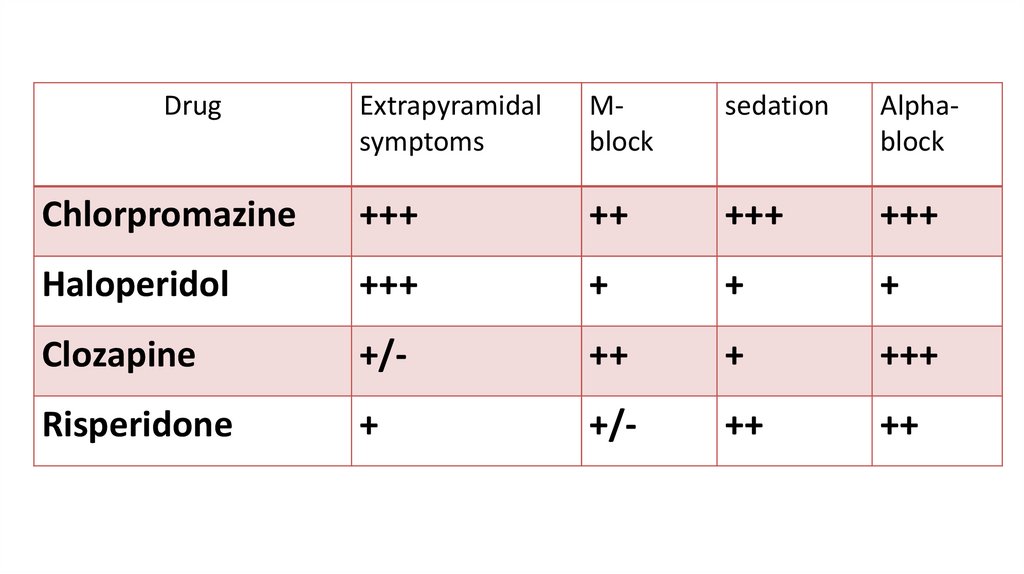
DrugExtrapyramidal
symptoms
Mblock
sedation
Alphablock
Chlorpromazinе
+++
++
+++
+++
Haloperidol
+++
+
+
+
Clozаpinе
+/-
++
+
+++
Risperidonе
+
+/-
++
++
26.
Side effects. Extrapyramidal disturbancesParkinsonism with typical manifestations— rigidity,
tremor, hypokinesia, mask like facies, disorders of gait;
Malignant neuroleptic syndrome : It occurs rarely with
high doses of potent agents. The patient develops marked
rigidity,
immobility,
tremor,
hyperthermia,
semiconsciousness, fluctuating BP and heart rate;
myoglobin may be present in blood. The syndrome lasts 5–
10 days after drug withdrawal and may be fatal.
27.
Side effects.CNS: Drowsiness, lethargy, mental confusion;
Hyperprolactinemia (due to D2 blockade), amenorrhoea,
infertility, galactorrhoea and gynaecomastia;
CVS Postural hypotension, tachycardia;
Dry mouth, blurring of vision, constipation, urinary retention in
elderly males;
Cholestatic jaundice;
Skin rashes, urticaria, contact dermatitis, photosensitivity;
Agranulocytosis.
28.
Use
Antipsychotics drugs are administered in psychoses with
marked excitation, affective reactions, aggressiveness,
delirium, hallucinations.
In complex with other drugs when treating drug
dependence (opioid analgetics, alcohol)
Phenothiazine and Haloperidole are used as antiemetic
drugs and in persistant hiccups.
They are used with general anesthetics, hypnotics and
opioid analgetics besause they can potentiate actions.
29.
Lithium salts are mainly used to manage and prevent maniaand bipolar (manic depressive) disorder.
The mechanism of antimanic and mood stabilizing action of
lithium:
Li+ partly replaces body Na+ and is nearly equally
distributed inside and outside the cells; this may affect
ionic fluxes across brain cells or modify the property of
cellular membranes.
Lithium decreases the presynaptic release of NA and DA.
30.
• Lithium carbonate differs from the other antipsychoticdrugs by a slowly onset of effect (2-3 weeks), more
selective action on manias, and a lack of sedative effect
(listlessness and apathy).
• The low therapeutic window has to be considered.
• Side effects: dyspeptic disorders, muscle weakness, tremor,
polyuria, thirst.
• Acute poisoning with the lithium salts: vomiting, diarrhea,
ataxia, disarthria, and cramps.

 medicine
medicine