Similar presentations:
Drugs affecting the cardiovascular system
1. Drugs affecting the cardiovascular system
DRUGS AFFECTINGTHE CARDIOVASCULAR SYSTEM
Cardiotonic agents
Antiarrythmic agents
2.
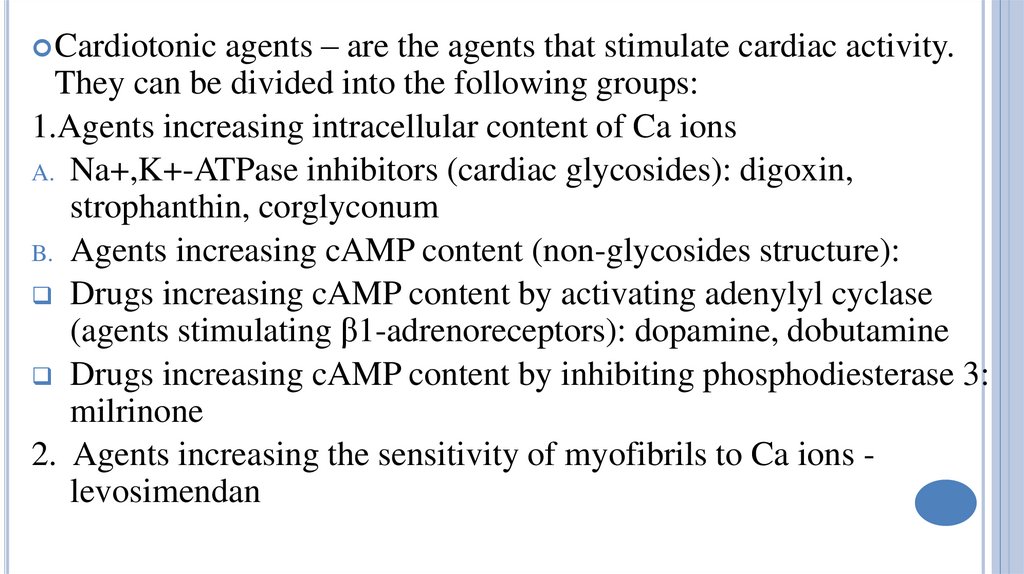
agents – are the agents that stimulate cardiac activity.They can be divided into the following groups:
1.Agents increasing intracellular content of Ca ions
A. Na+,K+-ATPase inhibitors (cardiac glycosides): digoxin,
strophanthin, corglyconum
B. Agents increasing cAMP content (non-glycosides structure):
Drugs increasing cAMP content by activating adenylyl cyclase
(agents stimulating β1-adrenoreceptors): dopamine, dobutamine
Drugs increasing cAMP content by inhibiting phosphodiesterase 3:
milrinone
2. Agents increasing the sensitivity of myofibrils to Ca ions levosimendan
Cardiotonic
3.
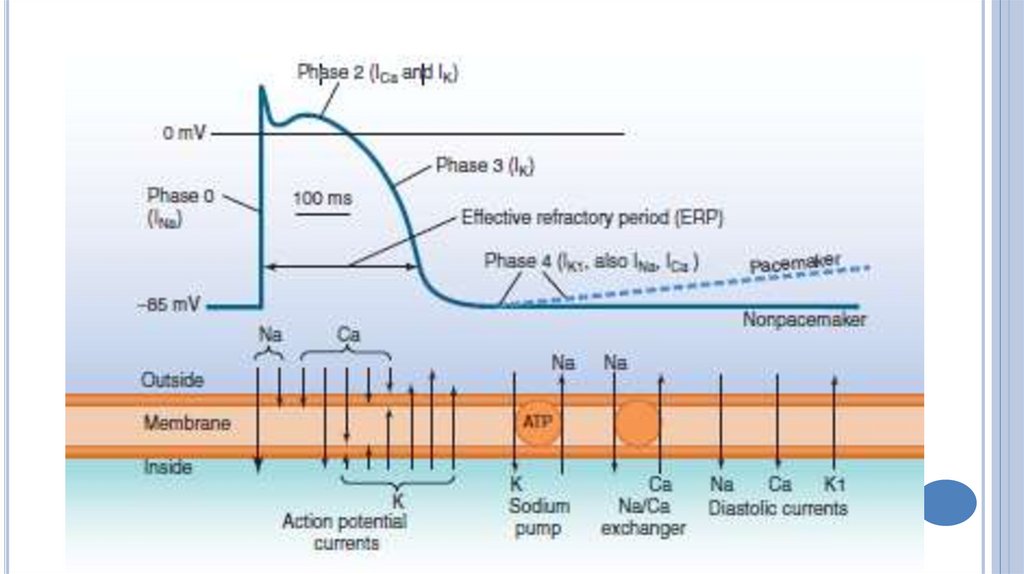
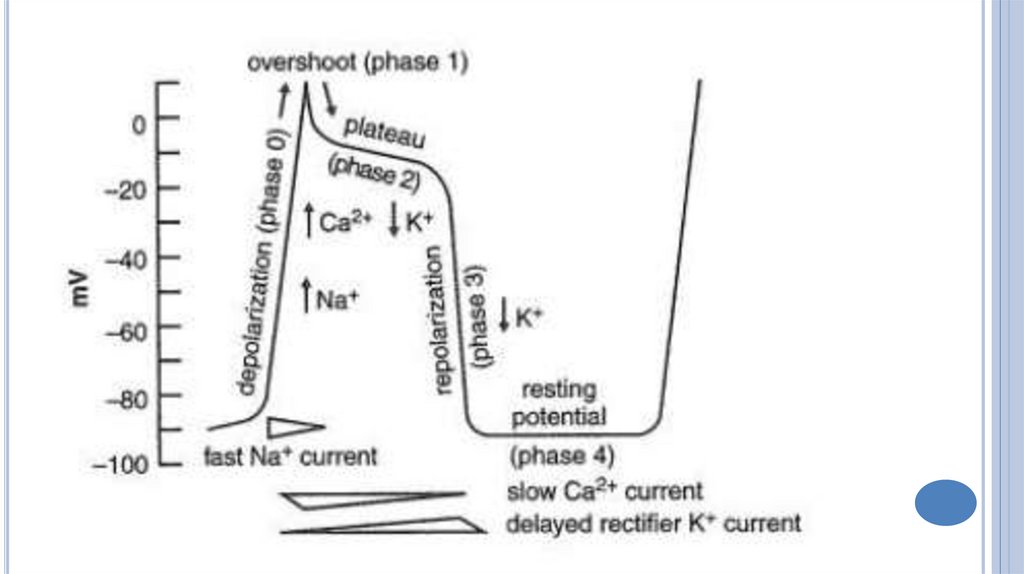
4.
Cardiacglycosides are agents of plant origin.
They produce marked cardiotonic effect, but
they do not increase the heart rate. They can
be used for the treatment of acute and chronic
heart failure.
The other drugs increase contractile force and
heart rate. They are used for the treatment of
acute heart failure only.
5.
DigitalisConvallaria
Strophanthus
Adonis vernalis
6.
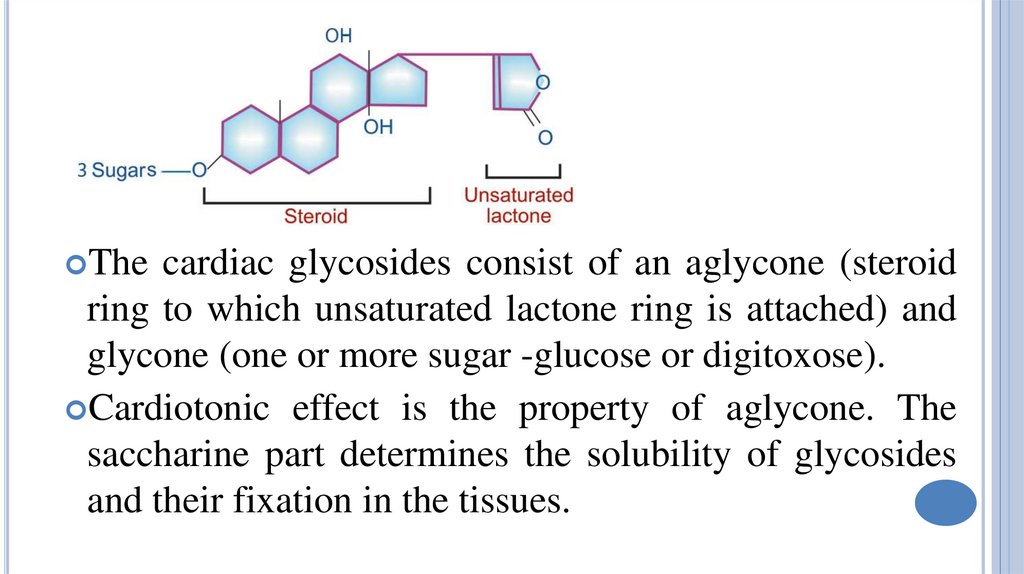
Thecardiac glycosides consist of an aglycone (steroid
ring to which unsaturated lactone ring is attached) and
glycone (one or more sugar -glucose or digitoxose).
Cardiotonic effect is the property of aglycone. The
saccharine part determines the solubility of glycosides
and their fixation in the tissues.
7.
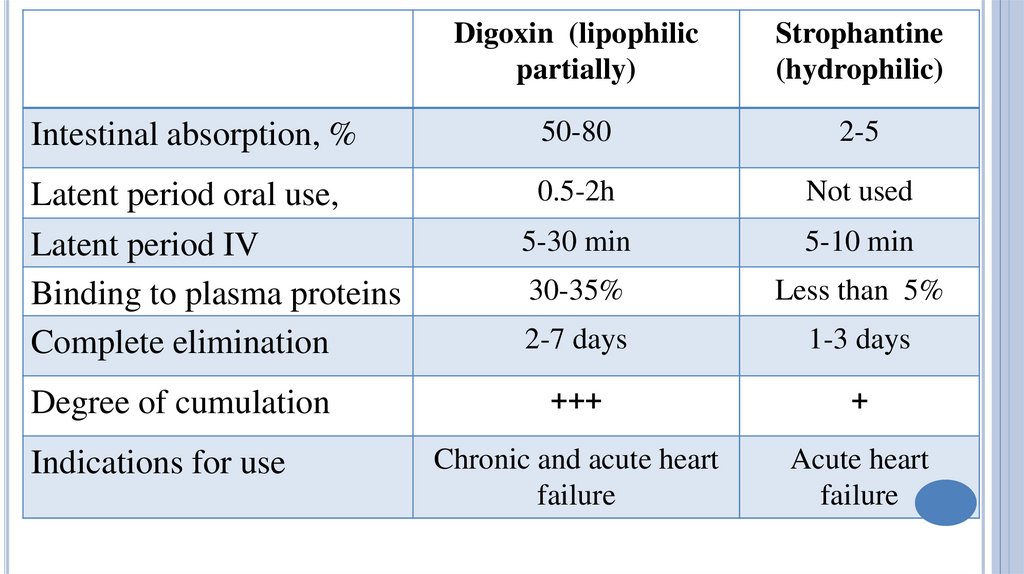
Digoxin (lipophilicpartially)
Strophantine
(hydrophilic)
Intestinal absorption, %
50-80
2-5
Latent period oral use,
Latent period IV
Binding to plasma proteins
Complete elimination
0.5-2h
Not used
5-30 min
5-10 min
30-35%
Less than 5%
2-7 days
1-3 days
+++
+
Chronic and acute heart
failure
Acute heart
failure
Degree of cumulation
Indications for use
8.
Cardiotonic effect (increase in systole, positive inotropic action)CGs block Na+,K+-ATPase → Na+,K+ flow disturbance → ↑
intracellular Na+, but ↓ K+ → ↑ intracellular Ca (Ca enters the
cardiomyocites from outside via the Ca L-channels and releases
from the sarcoplasmatic reticulum) → Ca interacts with the
troponine complex and eliminates its suppressive effect on the
contractile proteins.
Actin interacts with myosin→ rapid and intensive myocardial
contraction.
There is more complete emptying of failing and dilated ventricles—
cardiac output is increased and end-diastolic volume is reduced.
9.
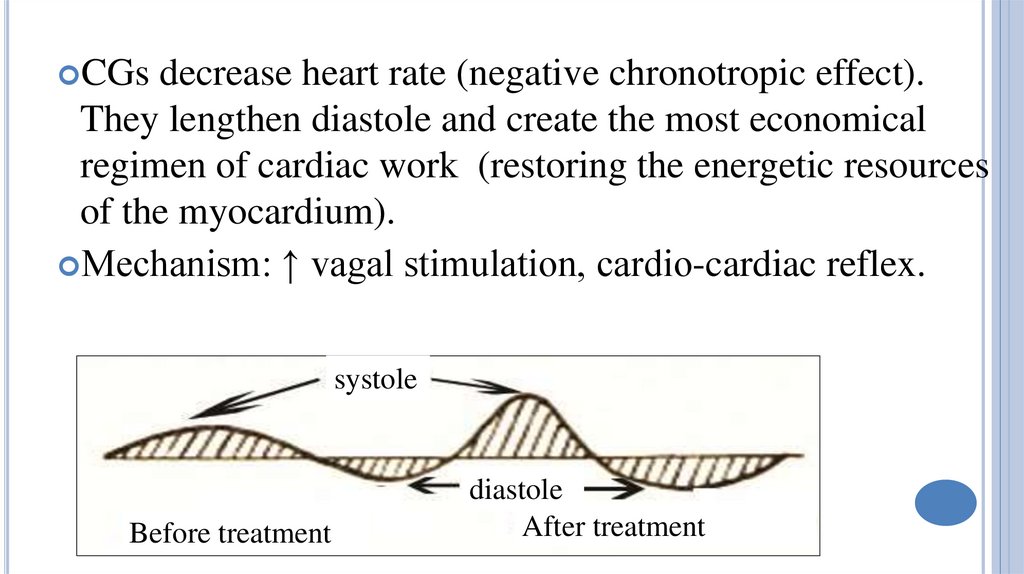
CGsdecrease heart rate (negative chronotropic effect).
They lengthen diastole and create the most economical
regimen of cardiac work (restoring the energetic resources
of the myocardium).
Mechanism: ↑ vagal stimulation, cardio-cardiac reflex.
systole
Before treatment
diastole
After treatment
10.
A-Vconduction is demonstrably slowed by therapeutic
doses (negative dromotropic effect).
Myocardial excitability is increased (positive
batmotropic effect).
CGs increase arterial blood pressure, but decrease venous
pressure. Peripheral vascular resistance decreases, blood
supply and tissue oxygenation are improved. The
dysfunction of organs ( the CNS, kidneys, lungs, liver,
GI) gradually resolve. Edema gradually disappear.
11.
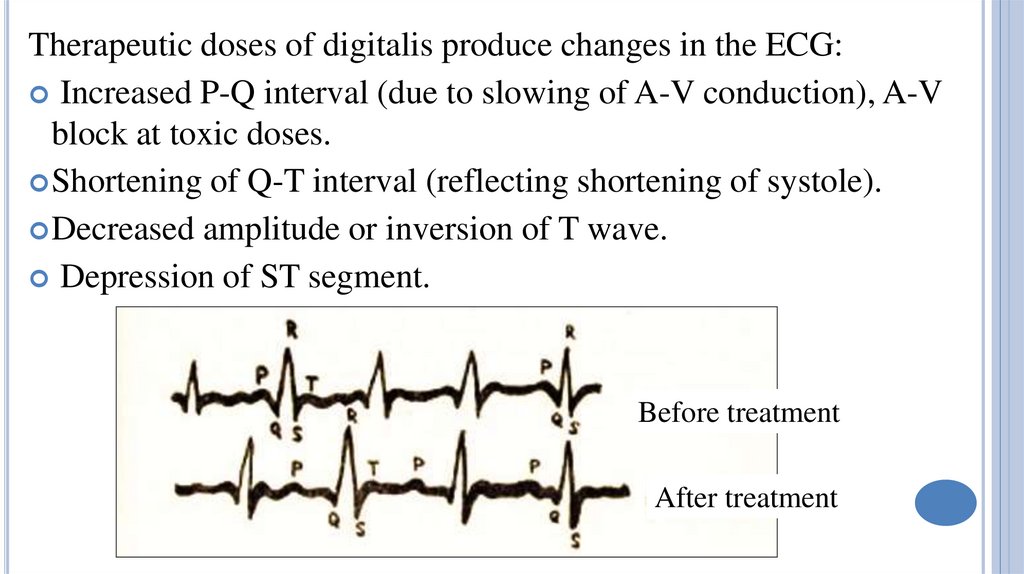
Therapeutic doses of digitalis produce changes in the ECG:Increased P-Q interval (due to slowing of A-V conduction), A-V
block at toxic doses.
Shortening of Q-T interval (reflecting shortening of systole).
Decreased amplitude or inversion of T wave.
Depression of ST segment.
Before treatment
After treatment
12. Intoxication with digitalis agents
INTOXICATION WITH DIGITALIS AGENTSSymptoms:
extrasystoles, partial or complete A-V
block; vision (colour) disturbances, fatigue, muscle
weakness, dyspepsia (nausea, vomiting, diarrhea),
mental disorders (agitation, hallucinations),
headache, skin rash.
Treatment:
potassium agents (“Asparcam”,
“Pananginum”), phenytoin, lidocaine, atropine;
digoxin Fab (digibind), unithiol (contains
sulfhydryl groups).
13.
Dopaminecauses positive inotropic effect
(β1R) combined with dilatation of kidneys
and mesenteric vessels (dopamine receptors
and β2 R).
D. is used for the treatment of cardiogenic
shock, is administered intravenously drip.
D.
can cause tachycardia, arrhythmia,
excessive increases in peripheral vascular
resistance and cardiac work.
14.
Levosimendanincreases the sensitivity of the myofibrils of
the heart to calcium ions.
Increases intensity of heart contractions without increased
myocardial oxygen consumption.
Dilates coronary vessels, increases oxygen delivery to the
myocardium.
Dilates blood vessels, reduces peripheral vascular resistance,
decreases pre- and afterload.
L. is used IV for the treatment of acute cardiac failure.
Side effects: arrhythmias, hypotension, headache, dizziness.
15.
Milrinoneincreases contractile
activity of the myocardium and
causes vasodilatation (↓ the
preload).
It is used intravenously drip in case
of acute cardiac decompensation.
Side effects: ↑heart rate,
arrhythmia, thrombocytopenia,
hypotension.
16.
Antiarrhythmicdrugs are used for the treatment and
prophylaxis of cardiac arrhythmias.
Classification
1.
D. mainly blocking ion channels of the cardiomyocytes
(of the cardiac conduction system and contractile
myocardium)
A) D. blocking sodium channels (membrane stabilizing D.)
Subgroup 1A: Quinidine, Procainamide
Subgroup 1B: Lidocaine, Phenytoin
Subgroup 1C: Propaphenone
17.
B) D. blocking potassium channels (agentsincreasing the duration of repolarization and
duration of action potential; class III):
Amiodaron
C) D. blocking L-type calcium channels (class IV):
Verapamil, Diltiazem
D) D. blocking sodium/potassium channels of
sinoatrial node (block of If inward current; group
V; bradycardic drugs): Ivabradine
18.
2. D.mostly affecting receptors of the afferent innervations ofthe heart:
D. that suppress adrenergic effects: β-adrenoblockers –
Propranolol, Metoprolol
D. that intensify adrenergic effects: Dobutamine,
Ephedrine
D. suppressing cholinergic effects: M-cholinoblockers
(Atropin)
3. Other drugs possessing antiarrhythmic activity:
Cardiac glycosides, Magnesium and potassium agents
19.
20.
21.
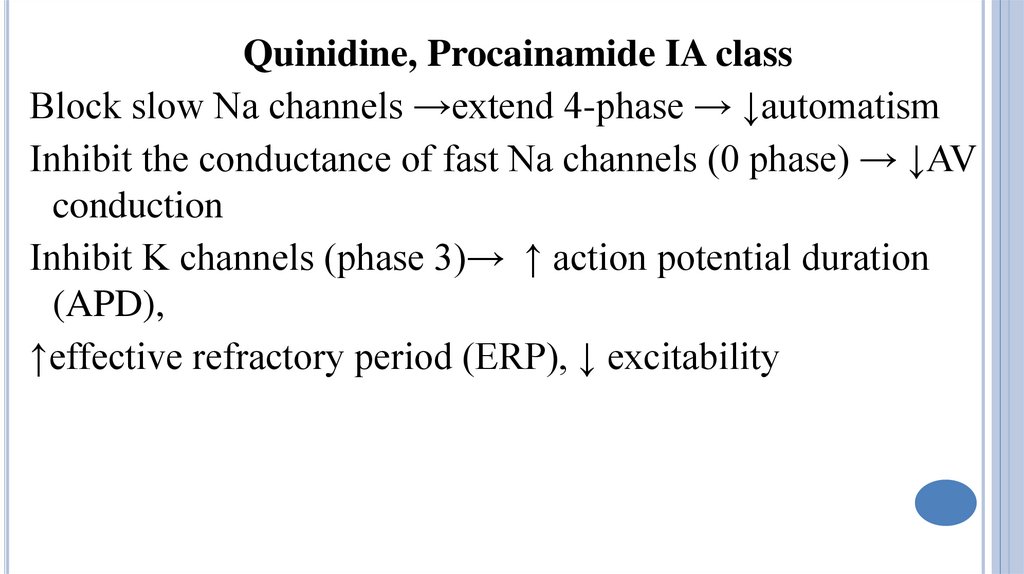
Quinidine, Procainamide IA classBlock slow Na channels →extend 4-phase → ↓automatism
Inhibit the conductance of fast Na channels (0 phase) → ↓AV
conduction
Inhibit K channels (phase 3)→ ↑ action potential duration
(APD),
↑effective refractory period (ERP), ↓ excitability
22.
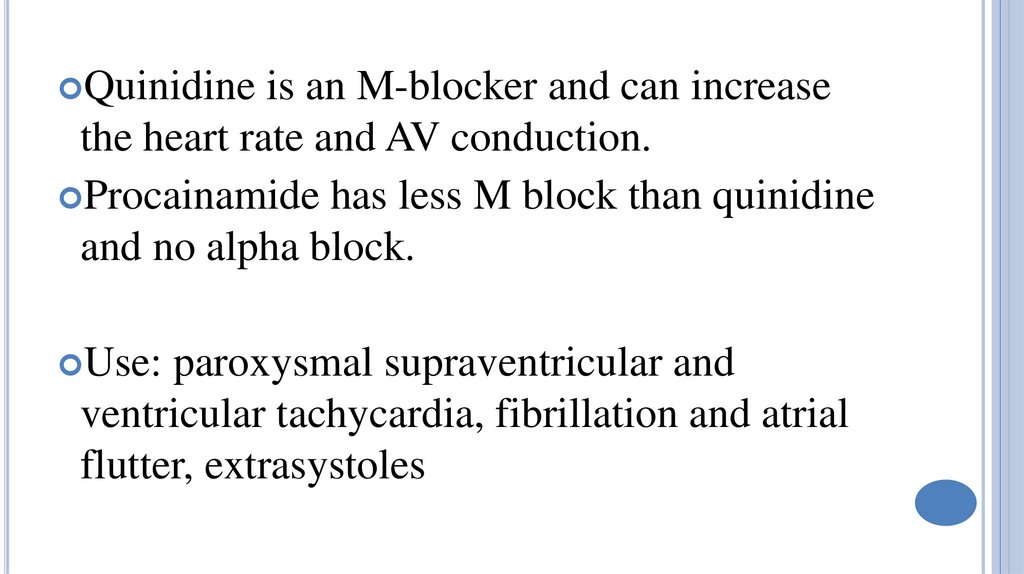
Quinidineis an M-blocker and can increase
the heart rate and AV conduction.
Procainamide has less M block than quinidine
and no alpha block.
Use:
paroxysmal supraventricular and
ventricular tachycardia, fibrillation and atrial
flutter, extrasystoles
23.
Side effectsQuinidine:
fall in BP, AV block, vomiting,
diarrhoea and neurological effects (ringing in
ears, vertigo, deafness, visual disturbances
and mental changes)
Procainamide:
nausea and vomiting,
weakness,
mental
confusion
and
hallucinations, hypotension hypersensitivity
reactions (rashes, fever, angioedema),
agranulocytosis and aplastic anaemia.
24.
25.
Lidocaine, PhenytoinInhibit slow Na channels - ↑ 4-phase →↓
automaticity in ectopic foci of Purkinje fibers
L. slightly inhibits fast Na channels→ decreases
APD in PF and ventricular muscle
Drugs
slightly affect conduction, increase
repolarization (activate K+ channels)
Use: ventricular tachyarrhythmias (extrasystoles)
26.
Lidocaineis injected intravenously drip. Side
effects: headache, drowsiness, nausea,
paresthesias, vision changes, tremor, seizures.
Phenytoin is used orally. Side effects:
nystagmus, ataxia, tremor, gingival hyperplasia,
dyspepsia.
27.
PropaphenoneDecreases
automatism;
slightly
affects
conduction, increases repolarization and ERP.
P. is used for the treatment of ventricular
arrhythmias orally or IV.
Side effects: nausea, vomiting, constipation,
bronchospasm,
weakness,
fatigue,
arrhythmogenic effect.
28.
29.
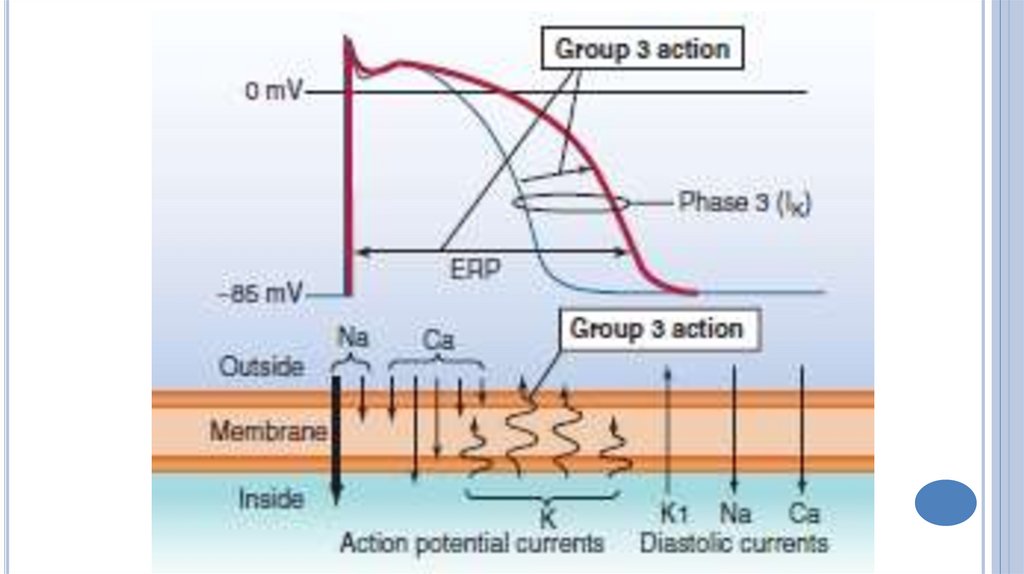
Amiodaronblocks K+-channels → slows repolarization and ↑ERP;
inhibits Na+ and Ca2+channels, ↑ APD;
↓ automaticity, excitability and conduction in the SA and
AV, ectopic foci;
blocks of β – and α-AR.
Use: supraventricular and ventricular tachycardia,
fibrillation and atrial flutter, extrasystoles.
30.
Adverseeffects: dyspepsia, pulmonary
fibrosis, bradycardia, AV-blockade, blue
pigmentation of the skin and the cornea,
phototoxicity, thyroid dysfunction.
31.
32.
Verapamil, DiltiazemBlocks the slow Ca2⁺ channels in SA and AV nodes,
↓spontaneous diastolic depolarization (4-phase)
→↓automaticity pacemaker - ↓heart rate;
Lengthens the 0-phase of action potential - ↓conduction;
Increases ERP, ↓ excitability.
They are used: sinus tachycardia, supraventricular
tachyarrhythmia.
Side effects: bradycardia, decreased heart contractility, ↓BP;
dizziness, swelling of the ankles, nausea, constipation.






 medicine
medicine