Similar presentations:
Dysentery( shigellosis)
1.
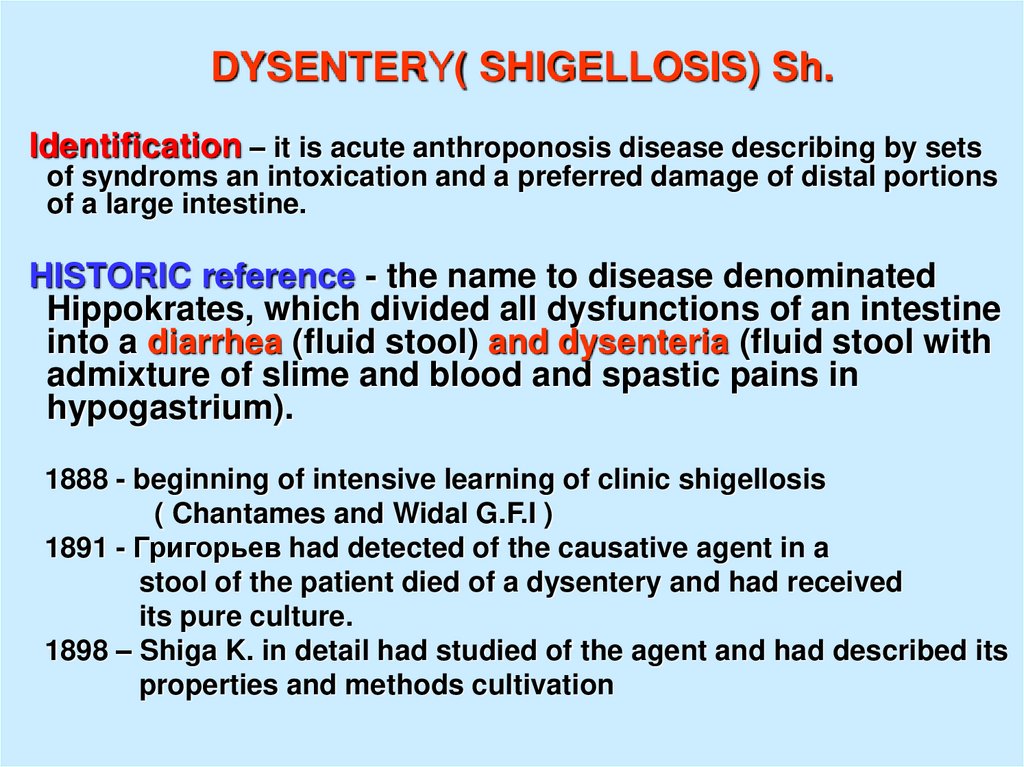
DYSENTERY( SHIGELLOSIS) Sh.Identification – it is acute anthroponosis disease describing by sets
of syndroms an intoxication and a preferred damage of distal portions
of a large intestine.
HISTORIC reference - the name to disease denominated
Hippokrates, which divided all dysfunctions of an intestine
into a diarrhea (fluid stool) and dysenteria (fluid stool with
admixture of slime and blood and spastic pains in
hypogastrium).
1888 - beginning of intensive learning of clinic shigellosis
( Chantames and Widal G.F.I )
1891 - Григорьев had detected of the causative agent in a
stool of the patient died of a dysentery and had received
its pure culture.
1898 – Shiga K. in detail had studied of the agent and had described its
properties and methods cultivation
2.
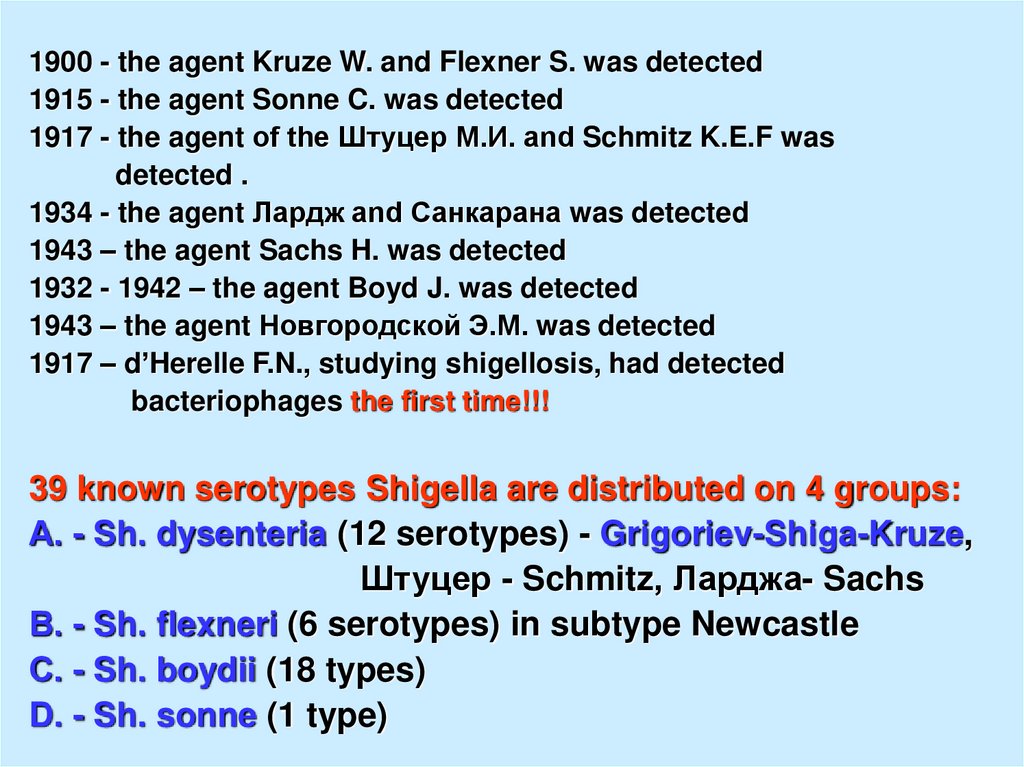
1900 - the agent Kruze W. and Flexner S. was detected1915 - the agent Sonne C. was detected
1917 - the agent of the Штуцер М.И. and Schmitz K.E.F was
detected .
1934 - the agent Лардж and Санкарана was detected
1943 – the agent Sachs H. was detected
1932 - 1942 – the agent Boyd J. was detected
1943 – the agent Новгородской Э.М. was detected
1917 – d’Herelle F.N., studying shigellosis, had detected
bacteriophages the first time!!!
39 known serotypes Shigella are distributed on 4 groups:
А. - Sh. dysenteria (12 serotypes) - Grigoriev-Shiga-Kruze,
Штуцер - Schmitz, Ларджа- Sachs
В. - Sh. flexneri (6 serotypes) in subtype Newcastle
С. - Sh. boydii (18 types)
D. - Sh. sonne (1 type)
3.
Main properties of causetive agents:- all shigellas are similar morphologically. They have
a size 0.3 – 0.6 on 1.5 - 3 microns, spores and capsules
will not derivate, gram (-), well grow on simple mediums.
- outside of an organism of the man survive from several
days to several months,
- desiccation and low temperature transfer well, but at 60 dg.
C - perish in 30 minutes and at boiling is very quickly!!!
- all desinfectants in usual concentrations are inactivated of
shigellas during 3 – 5 minutes.
- Sh. Sonei- will well be survive and is multiplied in nutrition
(milk)!!!
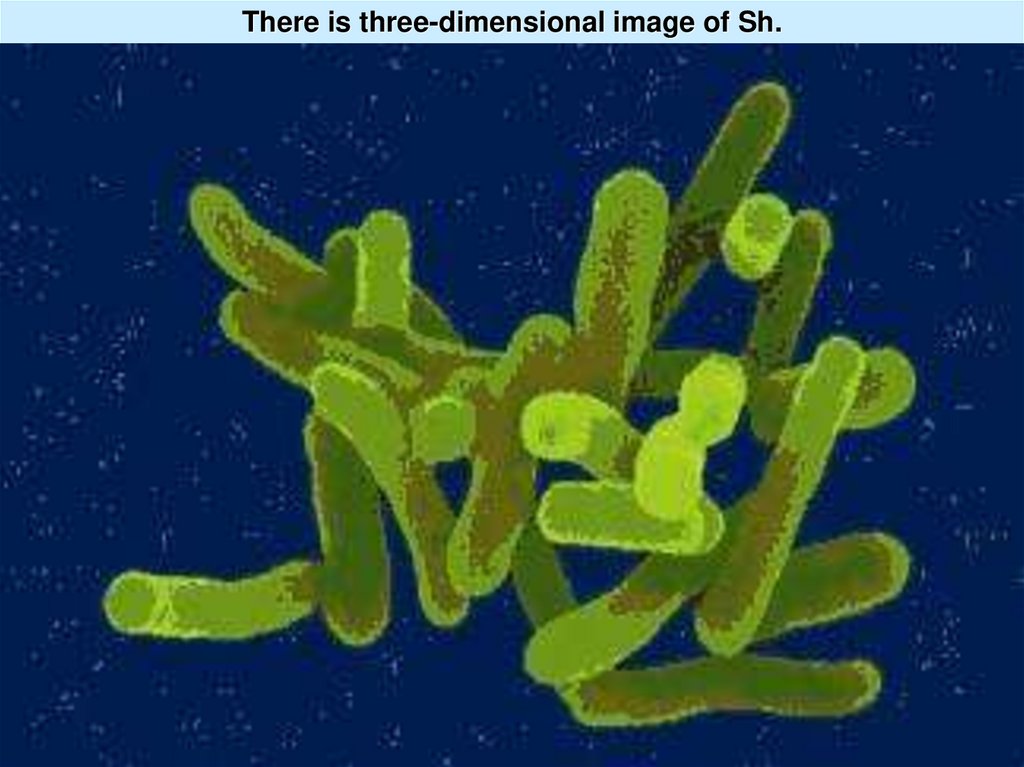
4. There is three-dimensional image of Sh.
5.
Antigenes:Sh. contain 2 thermostabile of an antigenes (typical and
group)
and 2 thermolabile antigenes (K - capsulated antigene –
( in groups shigellas A and B ) and fimbrial ( in group В)
Toxinoformation- exotoxin produces group A, which has
inhibited of protein synthesis in cells, has neurotoxity and
enterotoxity by operation and hemolytic activity.
Enterotoxical the operation of other groups shigellas is in
100- 1000 times is less expressed.
The endotoxin is freed at shigellas breakdown which differs
on operation from endotoxins gram (- ) negative bacteria a
little
6.
EpidemiologySource of an infection:
- the patients with the acute and chronic forms of disease
- and bacteriocarriers.
The mechanism of transmission - faecal-oral (main) and
rectal (homosexuals)
Sh
The factors of transmission: is more often, but this
dependence not hard !!!
- the water - Sh flexneri
- nutrition - Sh sonnei
- the contacts - Sh of type А
- the carriers ( fly, cockroaches )
7.
Seasonal prevalence - summer- autumn, but not so legibleas at a salmonellosis!!! A sporadic case rate - the year
round!!!
- the children in the age of from 1 tо 4 years often are sick
- as flashouts meets often in prisons, psychiatric hospitals,
barracrs, - (cause - lack of space and insanitary conditions
Pathogeny.
Infectious a dose from 100 up to 300 Sh.
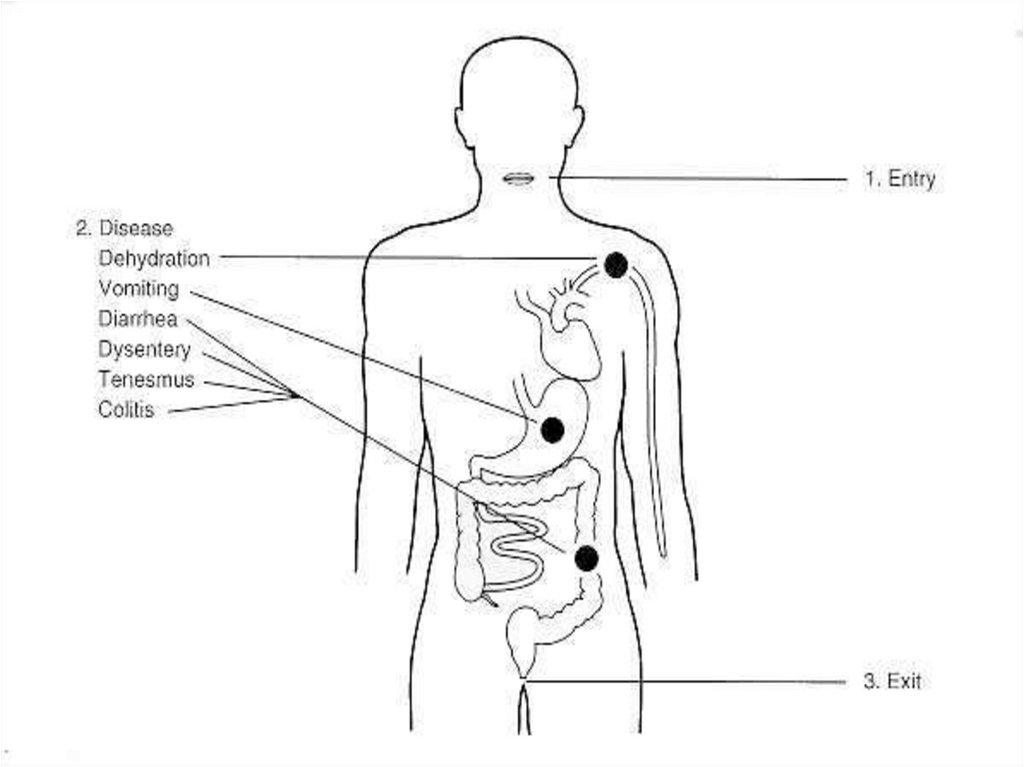
1. Infection through a mouth. Sh. free overcome of acidic
contents of a stomach (Sh. are survived in a stomach tо 4
hours) and infiltration into enterocytes of a small Intestine.
2. The enterocytes are damaged by an invagination a
cellular membrane with derivation phagosome with
subsequent lysis of it membrane and infiltration shigellas
in cytozole of enterocytes (within 15 minutes!!!) and start
intensively to be multiplied in them (in 3 hours the number
shigellas increases in 36 times!)
8.
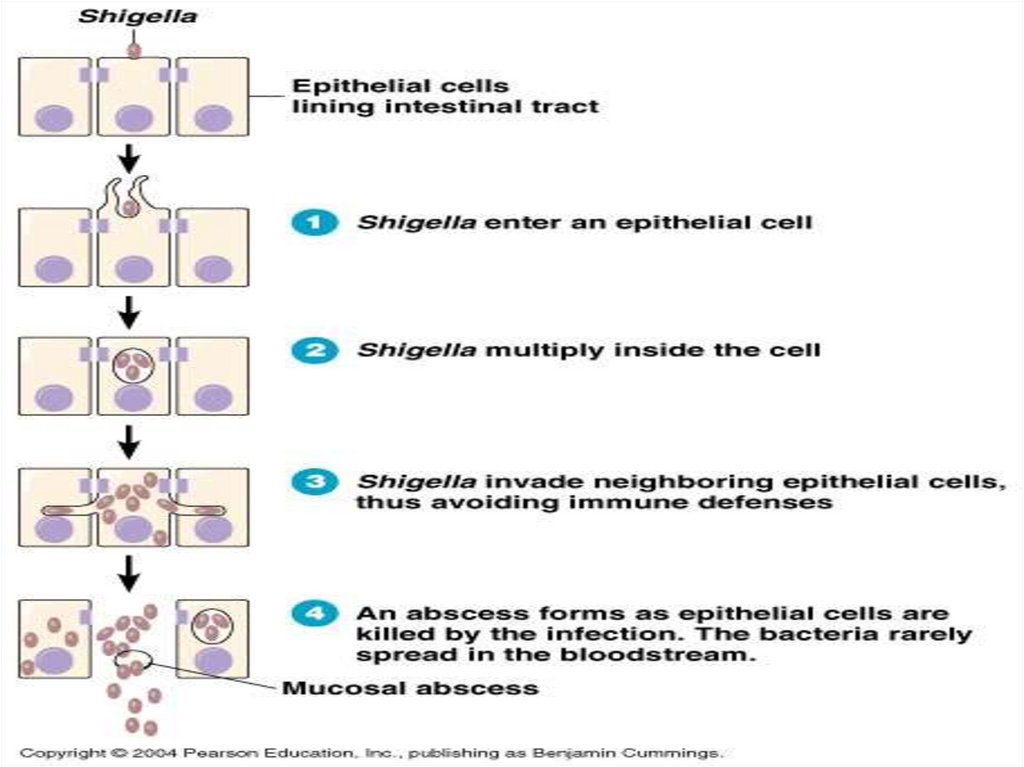
During the early stages of infection, bacteria aretranscytosed through the membrane of a cell into the
subepithelial space.
In the subepithelial space the Sh. are phagocytosed by
resident macrophages.
However, virulent shigellae are not killed and digested in
the macrophage phagolysome.
The bacteria lyse the phagosome and initiate apoptosis
(programmed cell death).
During this process, the infected macrophage releases the
inflammatory cytokine IL- 1, which elicits infiltration of
PMN.
9.
10. 5
3. The link of the struck enterocyteswith a membrane
5
mucous weakens and they reject together with shigellas
(rejtcted enterocyte + shigellas – it is “infectone”) and
mucous small intestine free oneself from the first
generation of Sh.
4. In 12 hours their concentration in 1 ml. a chyme makes
from 10 million to 1 billion - вecause of repetition of cycle
of implantation, reproduction and casting-off in new
enterocytes.
11.
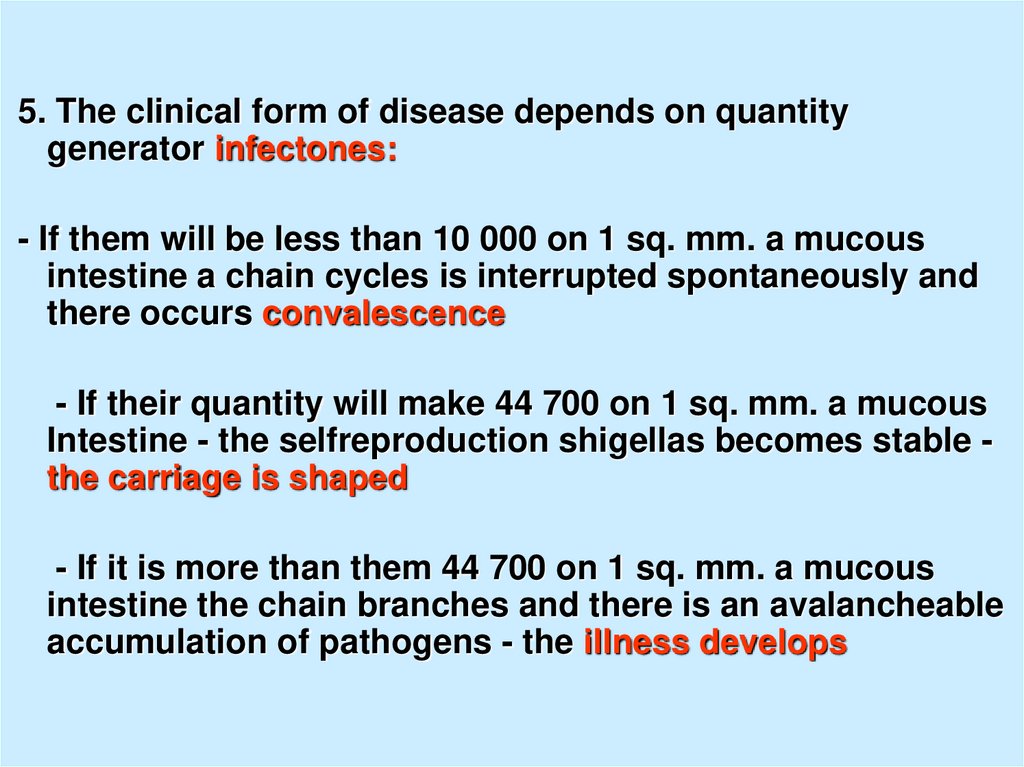
5. The clinical form of disease depends on quantitygenerator infectones:
- If them will be less than 10 000 on 1 sq. mm. a mucous
intestine a chain cycles is interrupted spontaneously and
there occurs convalescence
- If their quantity will make 44 700 on 1 sq. mm. a mucous
Intestine - the selfreproduction shigellas becomes stable the carriage is shaped
- If it is more than them 44 700 on 1 sq. mm. a mucous
intestine the chain branches and there is an avalancheable
accumulation of pathogens - the illness develops
12.
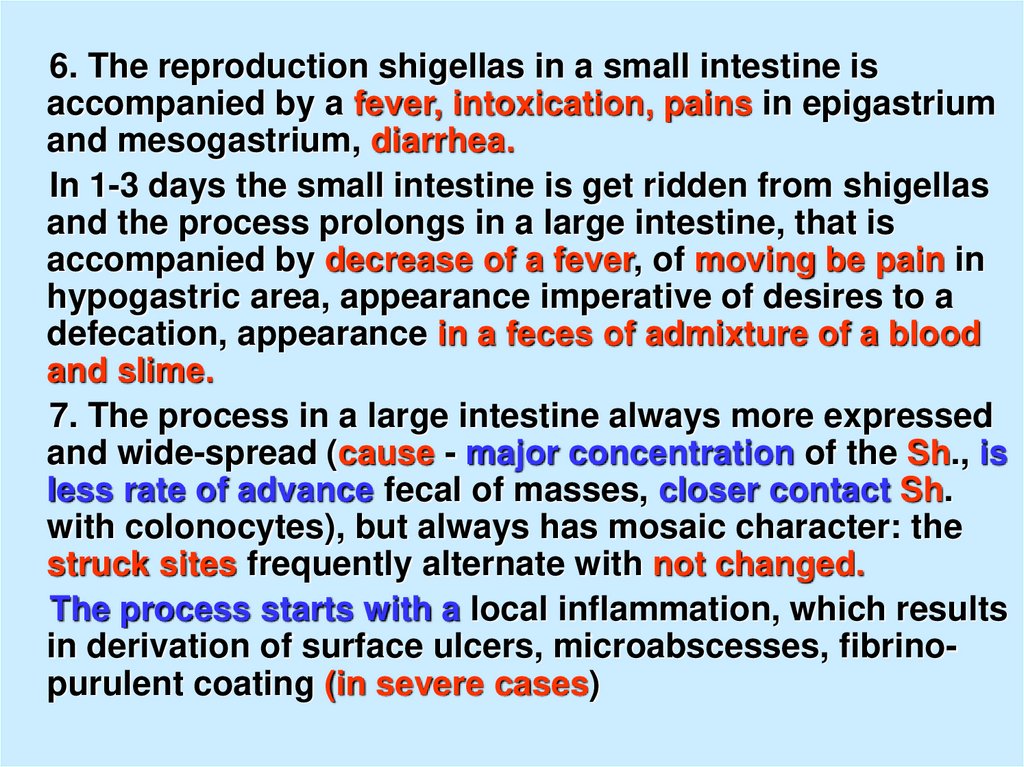
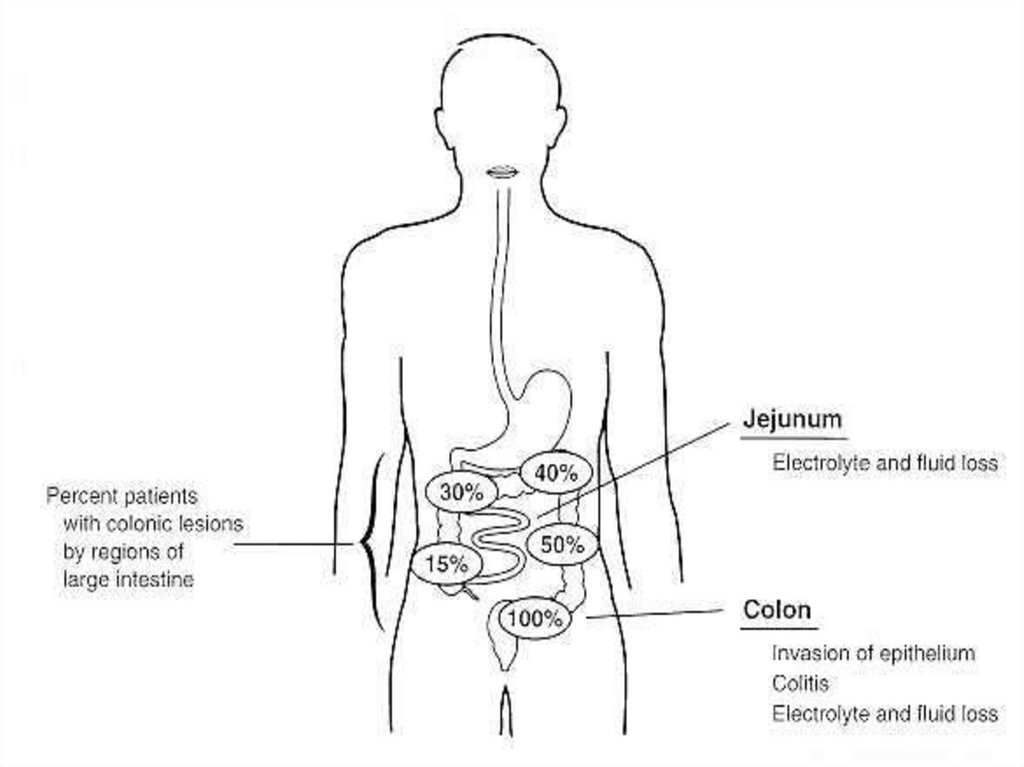
6. The reproduction shigellas in a small intestine isaccompanied by a fever, intoxication, pains in epigastrium
and mesogastrium, diarrhea.
In 1-3 days the small intestine is get ridden from shigellas
and the process prolongs in a large intestine, that is
accompanied by decrease of a fever, of moving be pain in
hypogastric area, appearance imperative of desires to a
defecation, appearance in a feces of admixture of a blood
and slime.
7. The process in a large intestine always more expressed
and wide-spread (cause - major concentration of the Sh., is
less rate of advance fecal of masses, closer contact Sh.
with colonocytes), but always has mosaic character: the
struck sites frequently alternate with not changed.
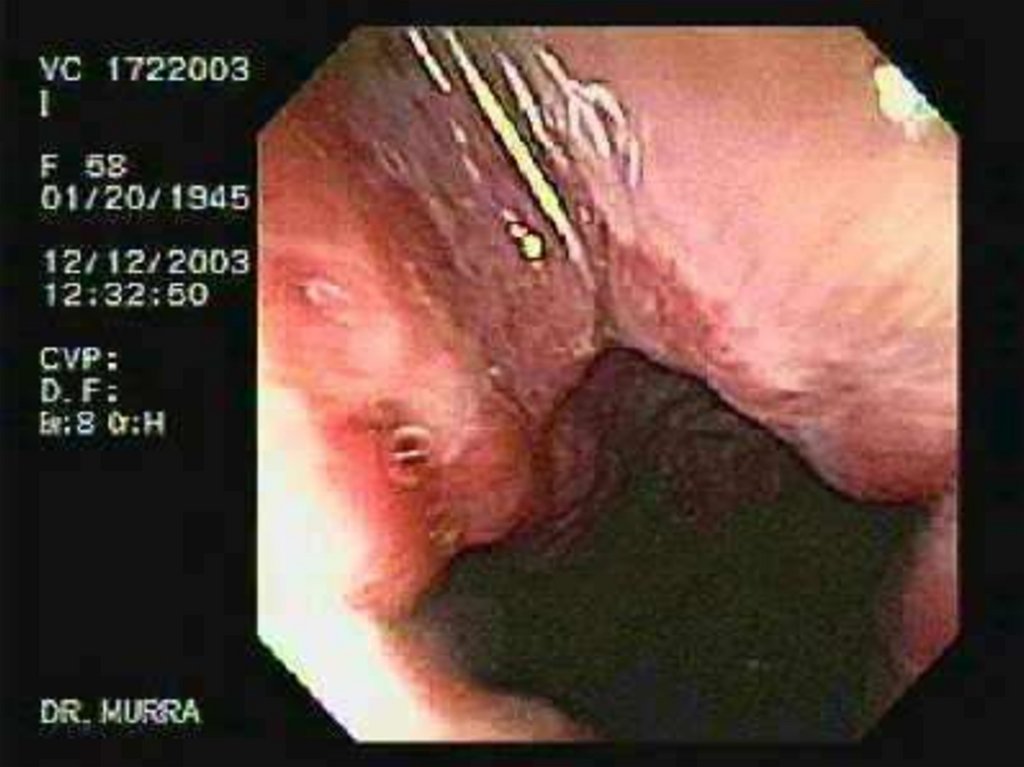
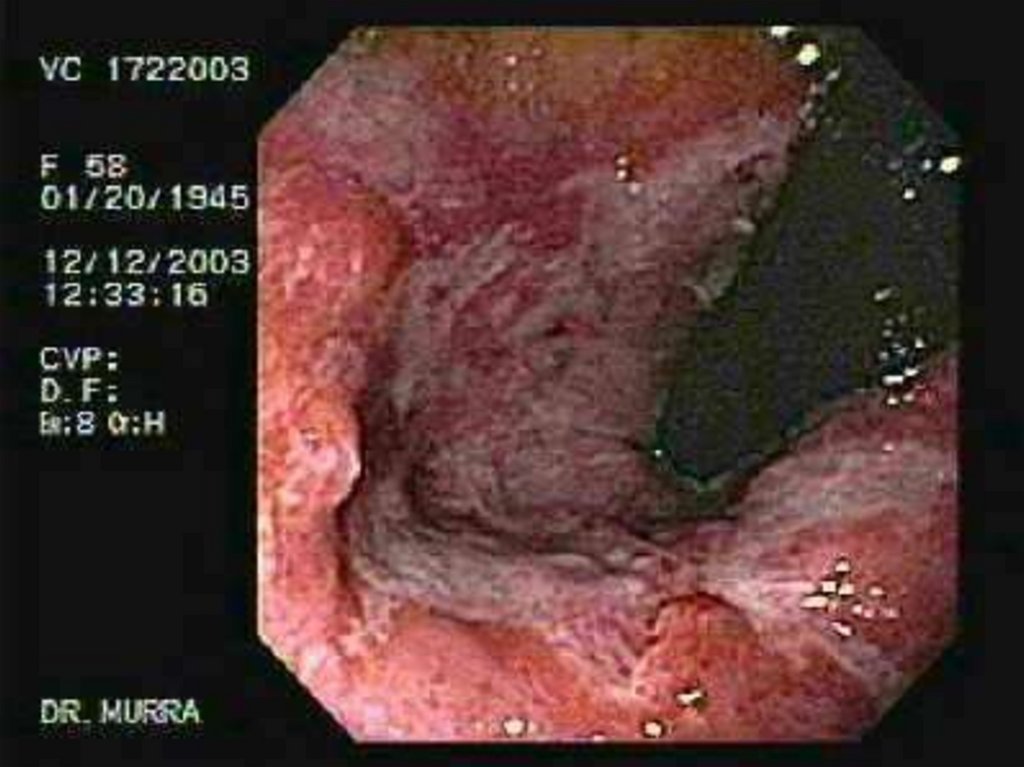
The process starts with a local inflammation, which results
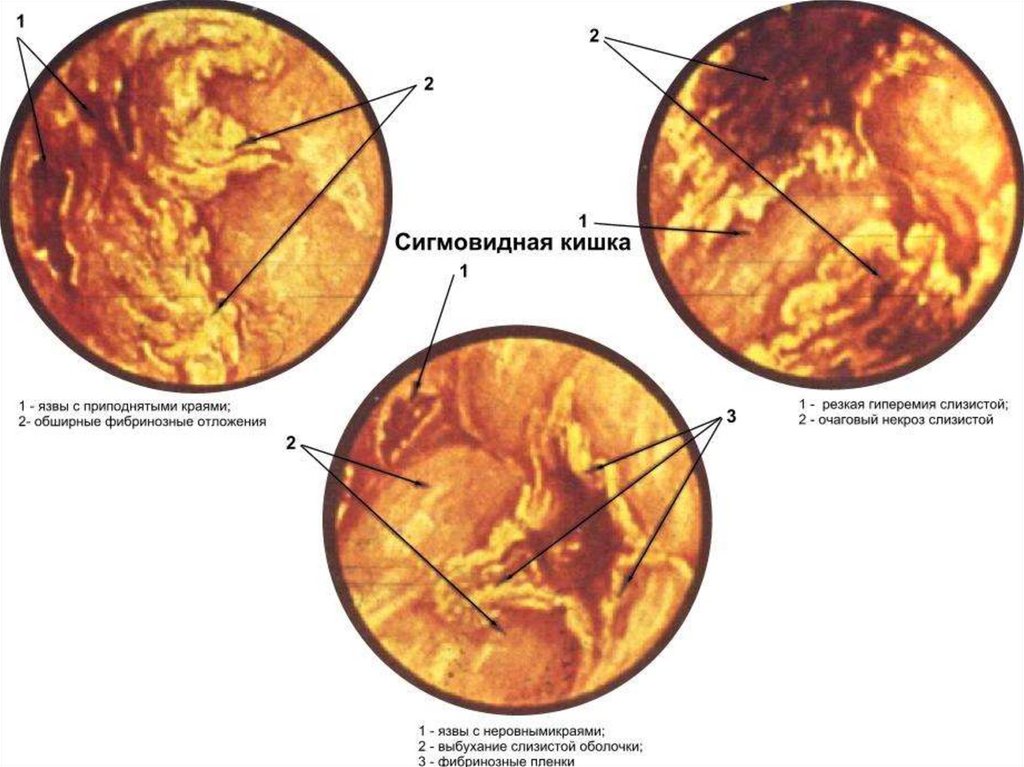
in derivation of surface ulcers, microabscesses, fibrinopurulent coating (in severe cases)
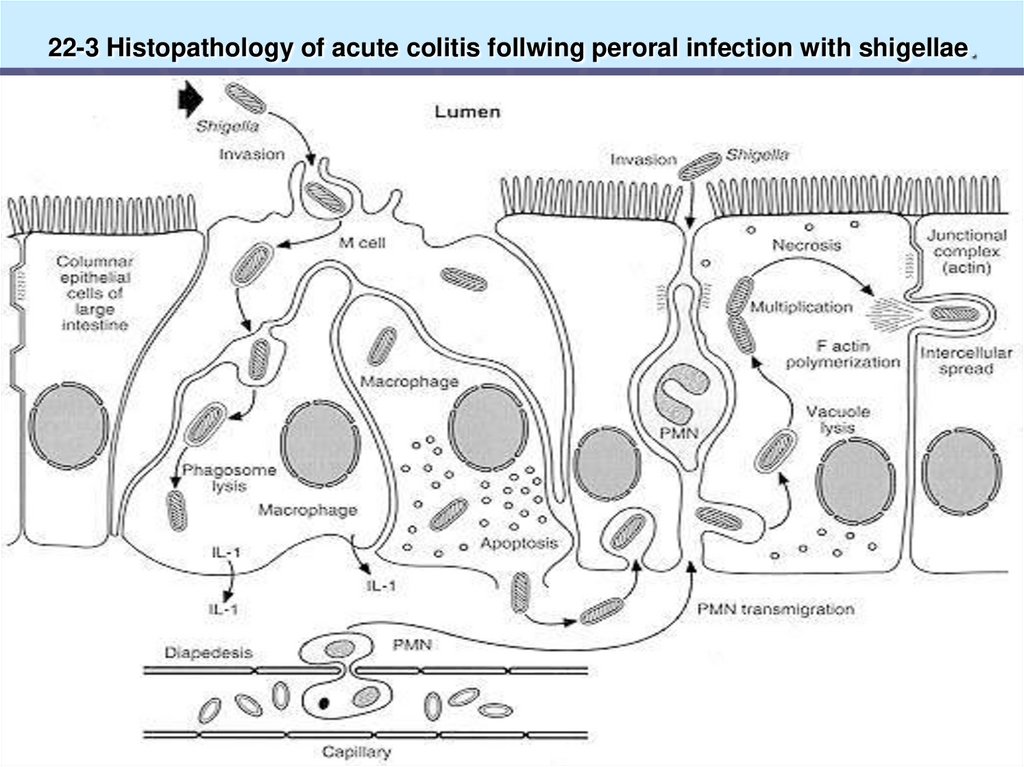
13. 22-3 Histopathology of acute colitis follwing peroral infection with shigellae.
14.
15.
16.
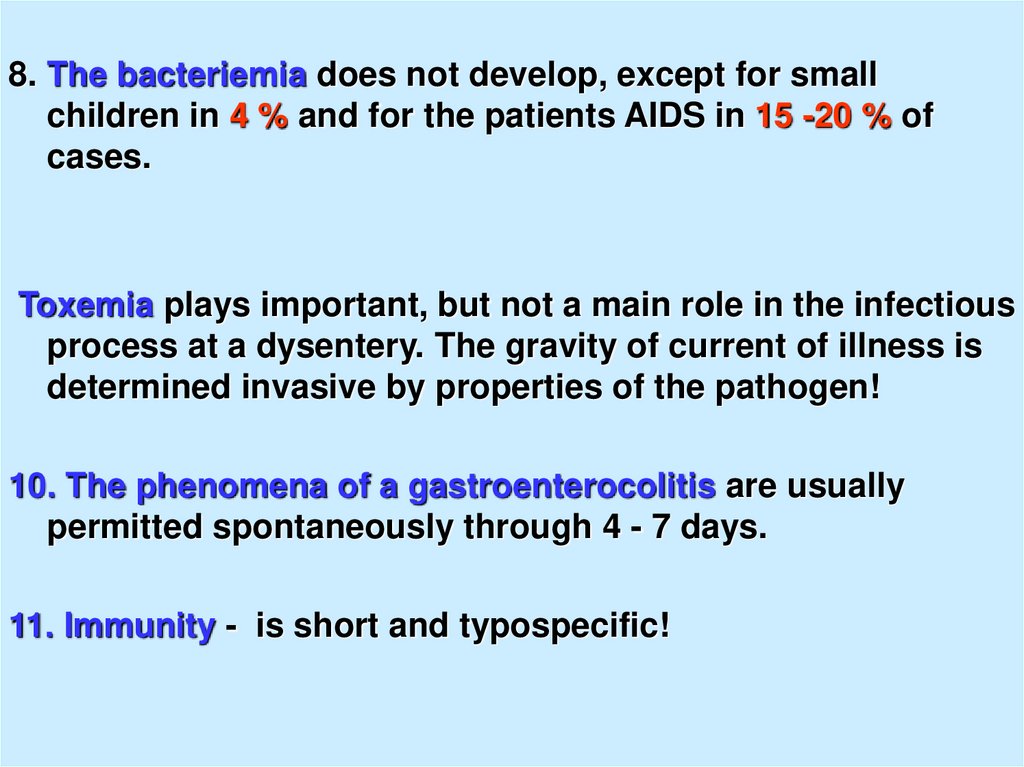
8. The bacteriemia does not develop, except for smallchildren in 4 % and for the patients AIDS in 15 -20 % of
cases.
Toxemia plays important, but not a main role in the infectious
process at a dysentery. The gravity of current of illness is
determined invasive by properties of the pathogen!
10. The phenomena of a gastroenterocolitis are usually
permitted spontaneously through 4 - 7 days.
11. Immunity - is short and typospecific!
17.
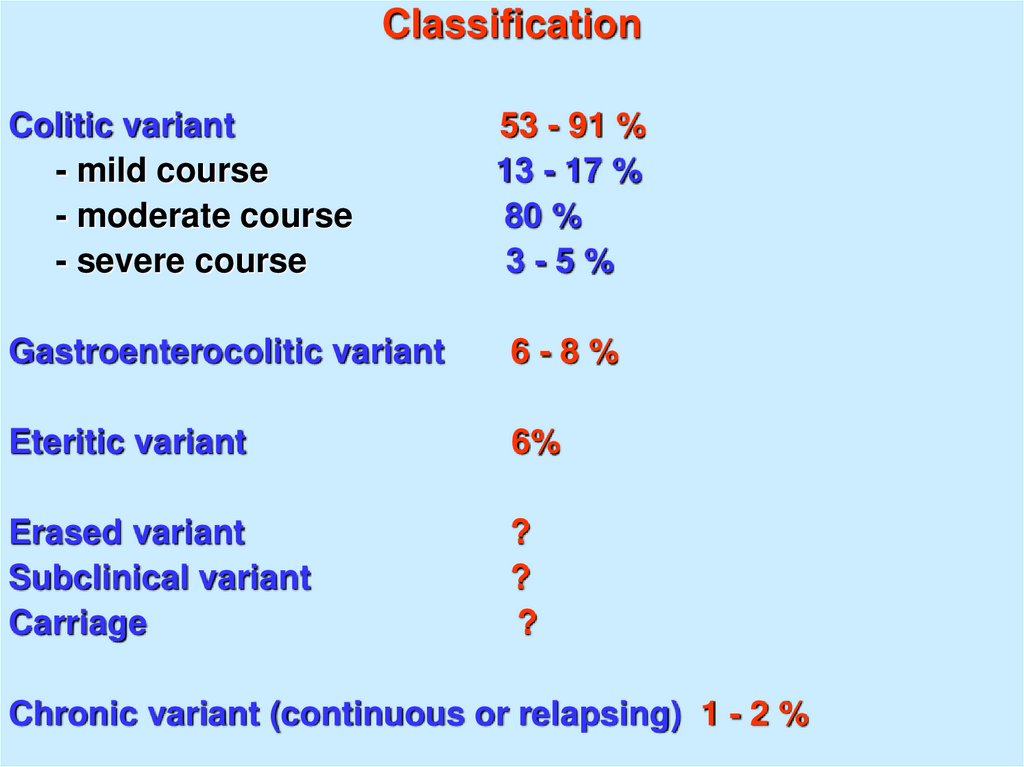
ClassificationColitic variant
- mild course
- moderate course
- severe course
53 - 91 %
13 - 17 %
80 %
3-5%
Gastroenterocolitic variant
6-8%
Eteritic variant
6%
Erased variant
Subclinical variant
Carriage
?
?
?
Chronic variant (continuous or relapsing) 1 - 2 %
18.
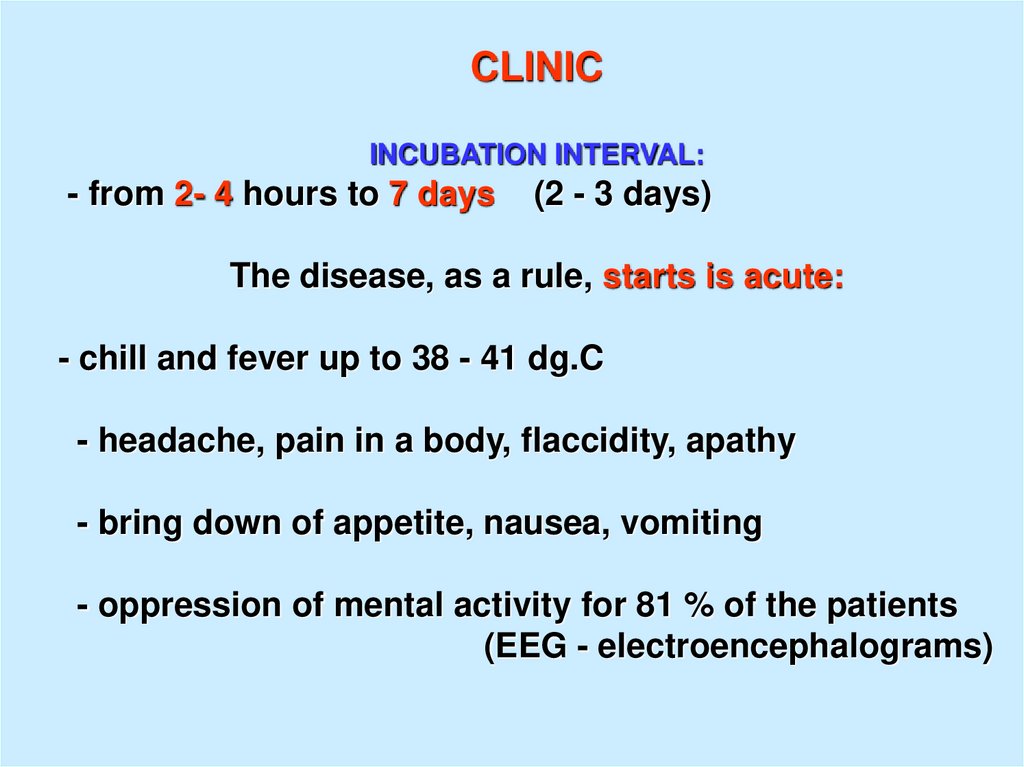
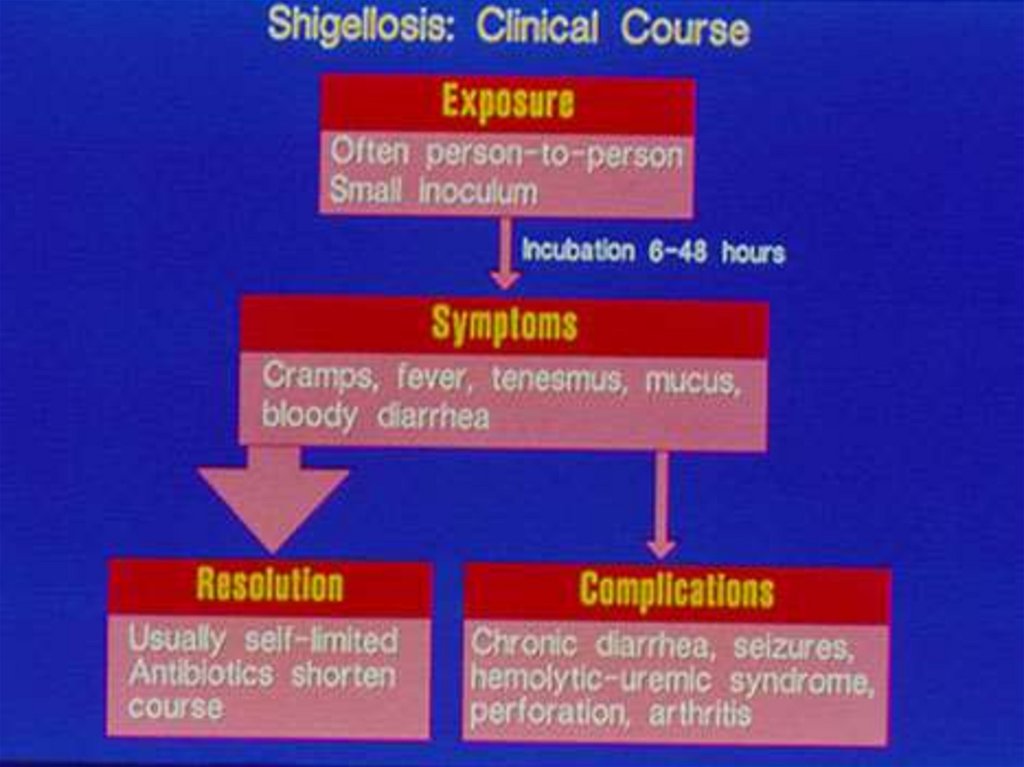
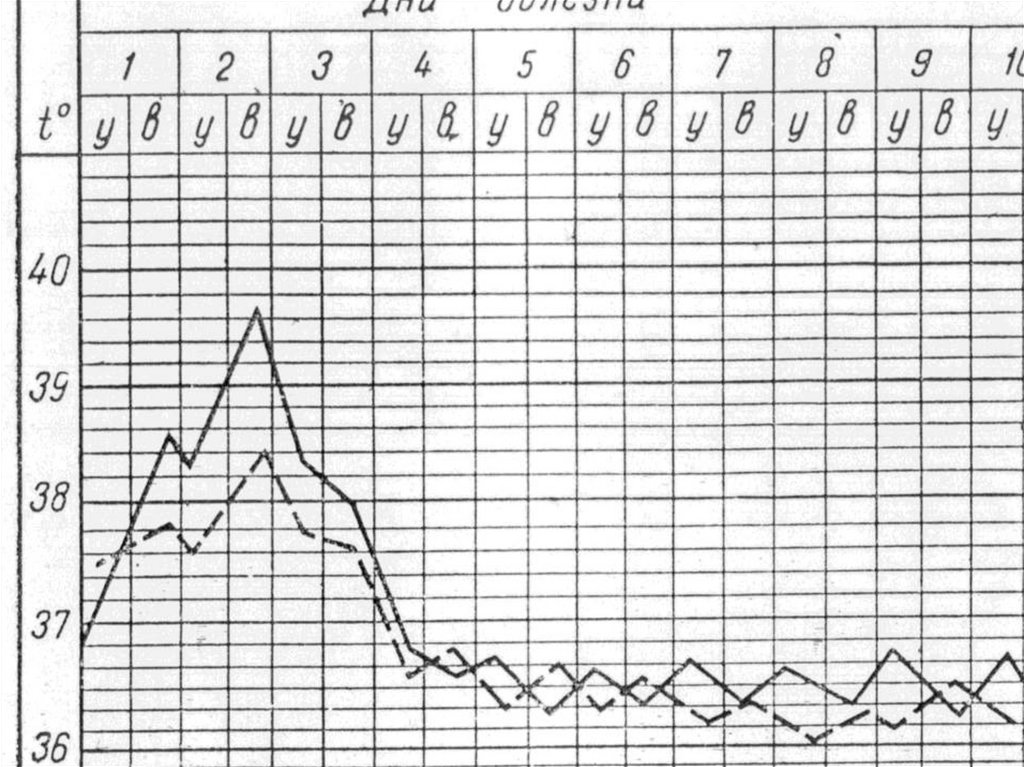
CLINICINCUBATION INTERVAL:
- from 2- 4 hours to 7 days
(2 - 3 days)
The disease, as a rule, starts is acute:
- chill and fever up to 38 - 41 dg.C
- headache, pain in a body, flaccidity, apathy
- bring down of appetite, nausea, vomiting
- oppression of mental activity for 81 % of the patients
(EEG - electroencephalograms)
19.
20.
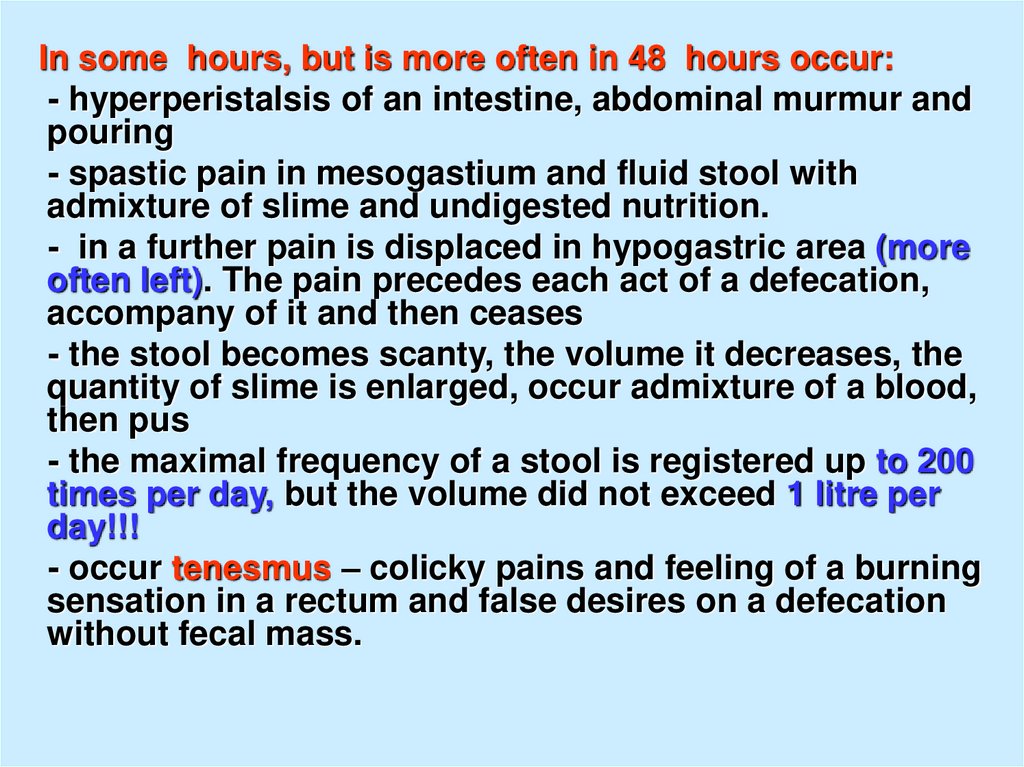
In some hours, but is more often in 48 hours occur:- hyperperistalsis of an intestine, abdominal murmur and
pouring
- spastic pain in mesogastium and fluid stool with
admixture of slime and undigested nutrition.
- in a further pain is displaced in hypogastric area (more
often left). The pain precedes each act of a defecation,
accompany of it and then ceases
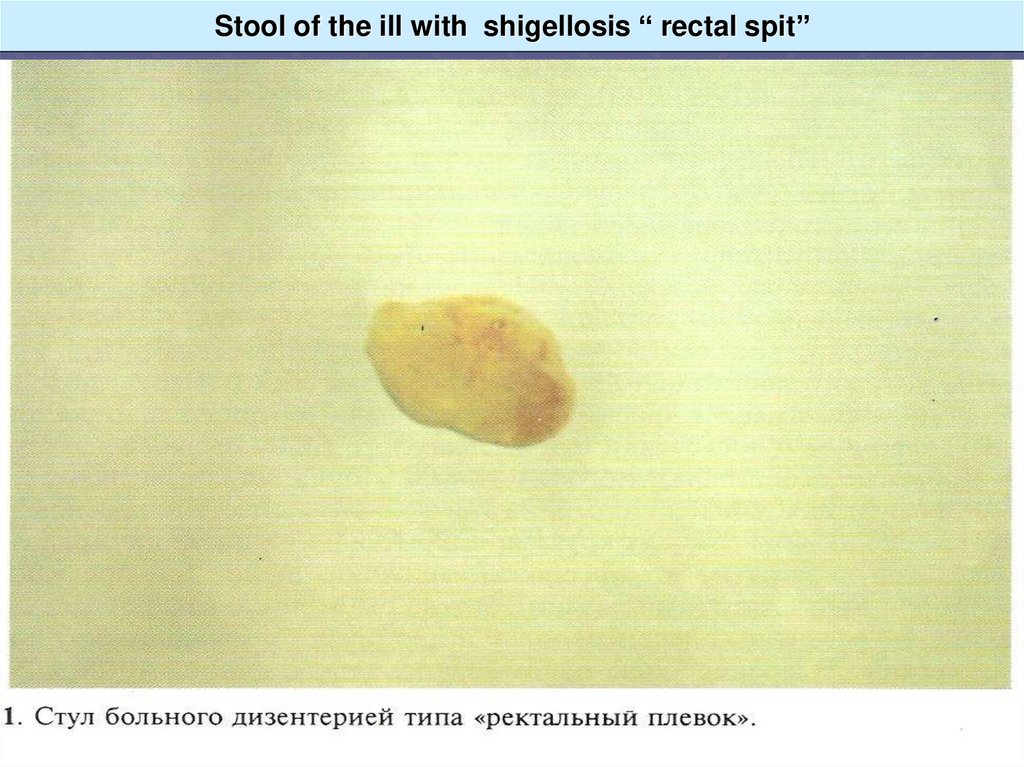
- the stool becomes scanty, the volume it decreases, the
quantity of slime is enlarged, occur admixture of a blood,
then pus
- the maximal frequency of a stool is registered up to 200
times per day, but the volume did not exceed 1 litre per
day!!!
- occur tenesmus – colicky pains and feeling of a burning
sensation in a rectum and false desires on a defecation
without fecal mass.
21.
22. Stool of the ill with shigellosis “ rectal spit”
23.
24.
25.
26.
27.
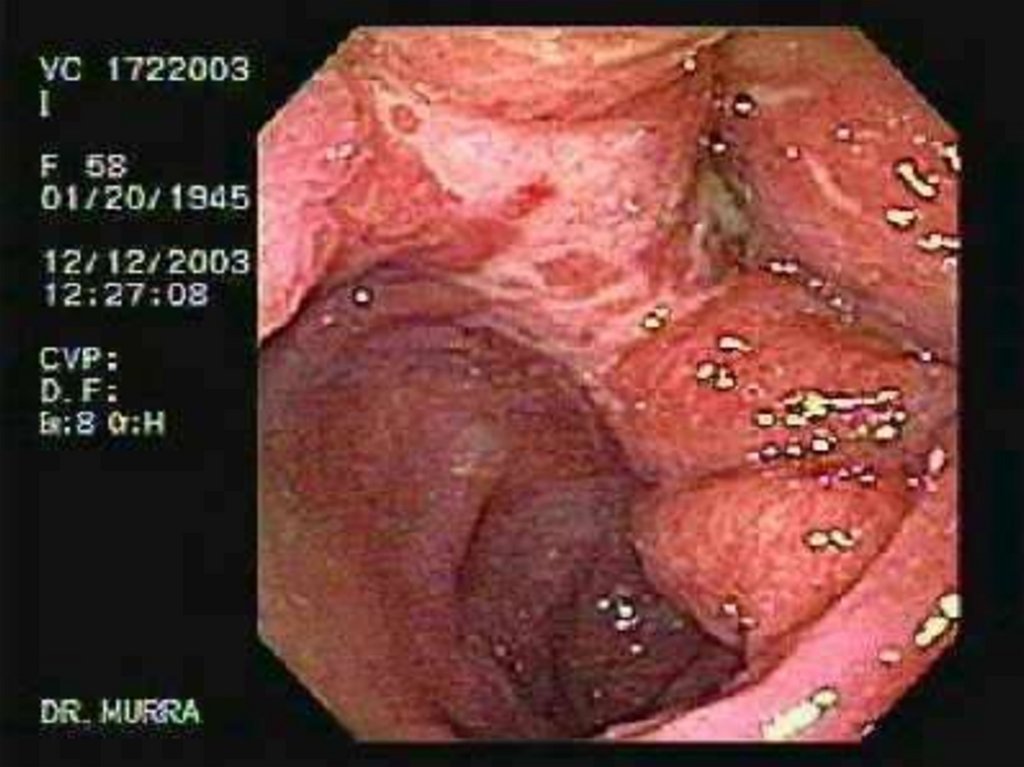
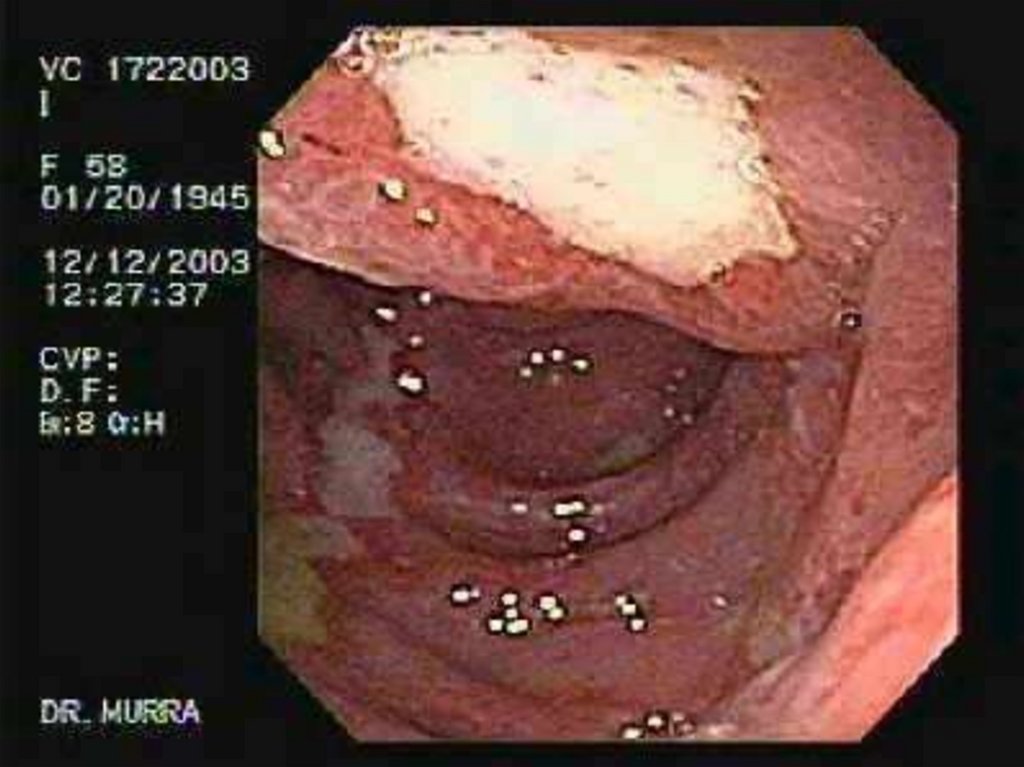
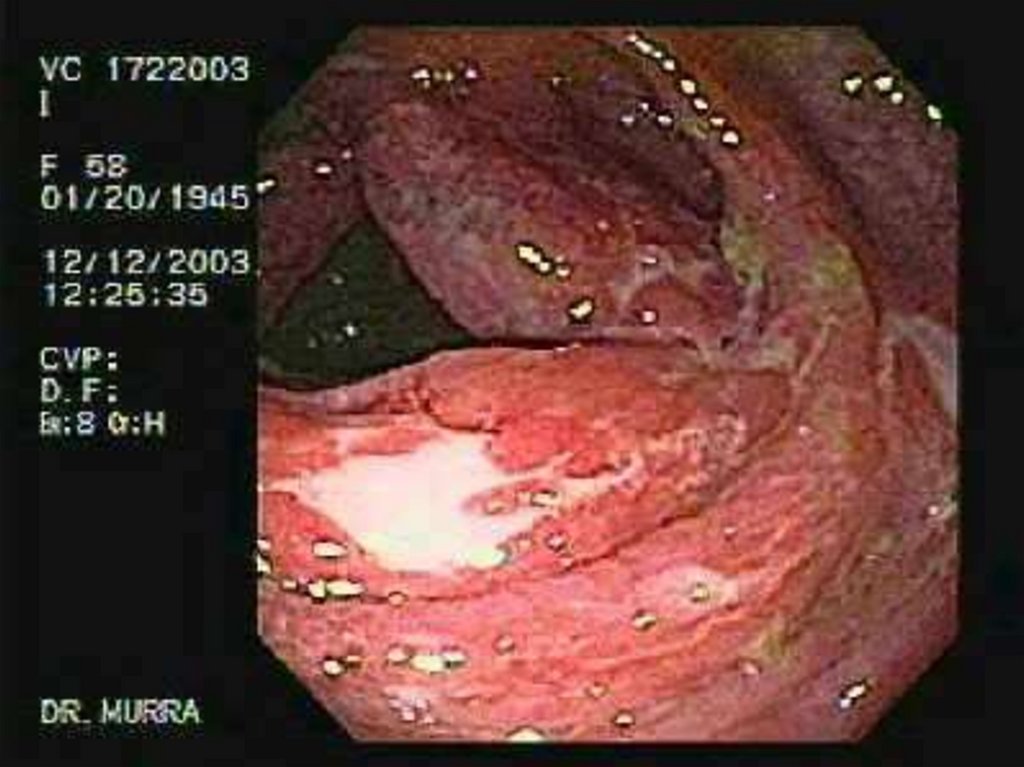
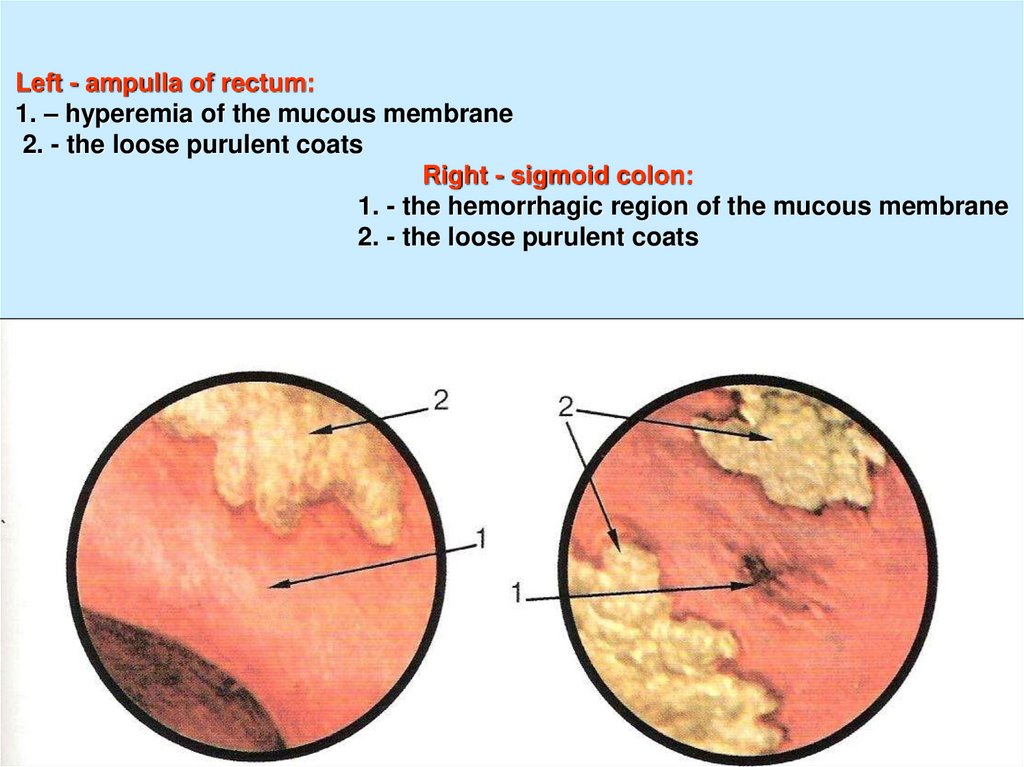
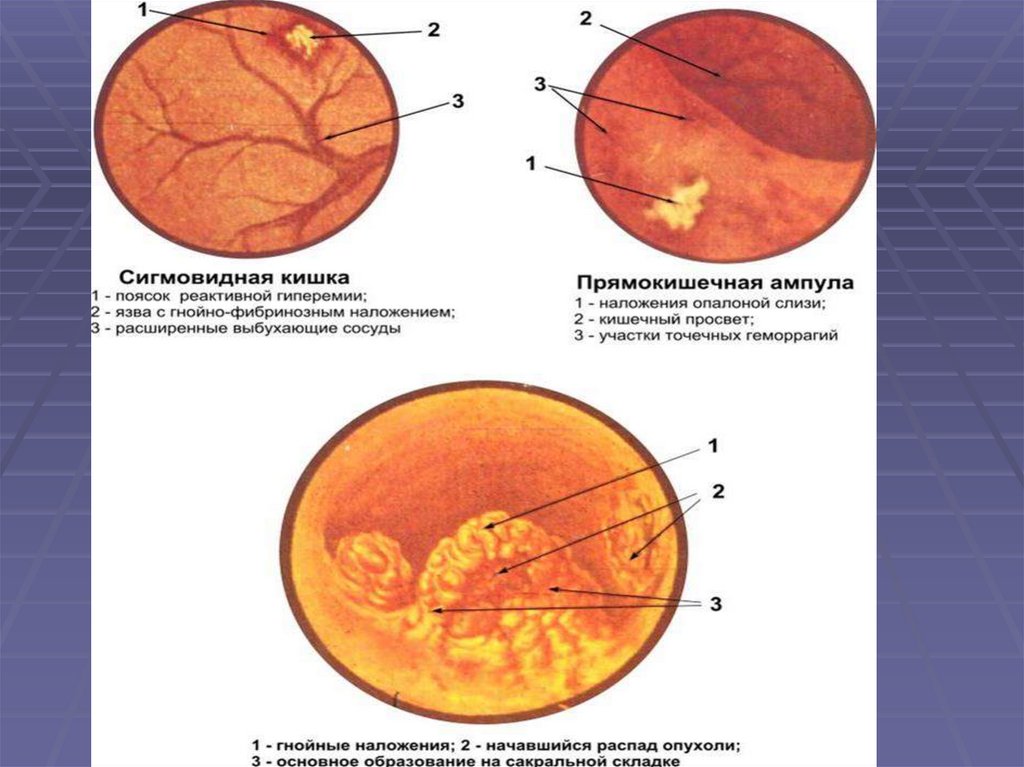
28. Left - ampulla of rectum: 1. – hyperemia of the mucous membrane 2. - the loose purulent coats Right - sigmoid colon: 1. - the
hemorrhagic region of the mucous membrane2. - the loose purulent coats
29.
30.
Objective signs of disease:- paleness of a skin, but sometimes hyperemia of
the face and neck
- tachycardia, lability of pulse, arrhythmia, sistolic
murmur on an apex, weakening of cardiac sounds,
hypotonia, bring down BP
- tаchypnea (adequate to a fever)
- dryness of a mucous oral cavity, white fur
31.
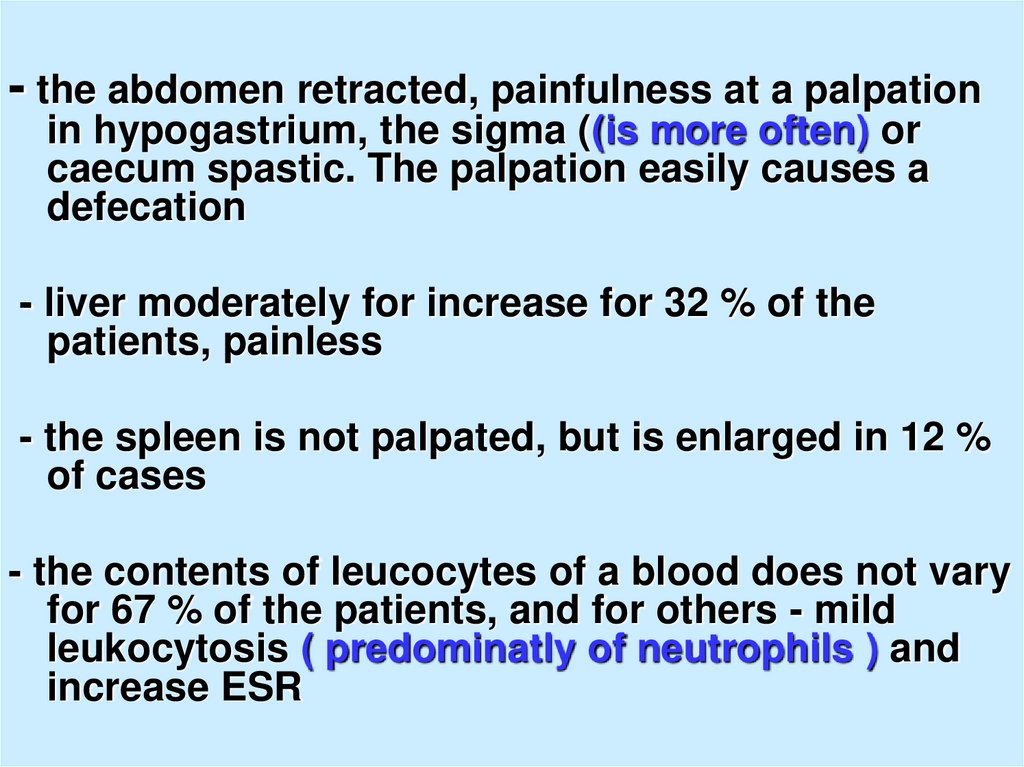
- the abdomen retracted, painfulness at a palpationin hypogastrium, the sigma ((is more often) or
caecum spastic. The palpation easily causes a
defecation
- liver moderately for increase for 32 % of the
patients, painless
- the spleen is not palpated, but is enlarged in 12 %
of cases
- the contents of leucocytes of a blood does not vary
for 67 % of the patients, and for others - mild
leukocytosis ( predominatly of neutrophils ) and
increase ESR
32.
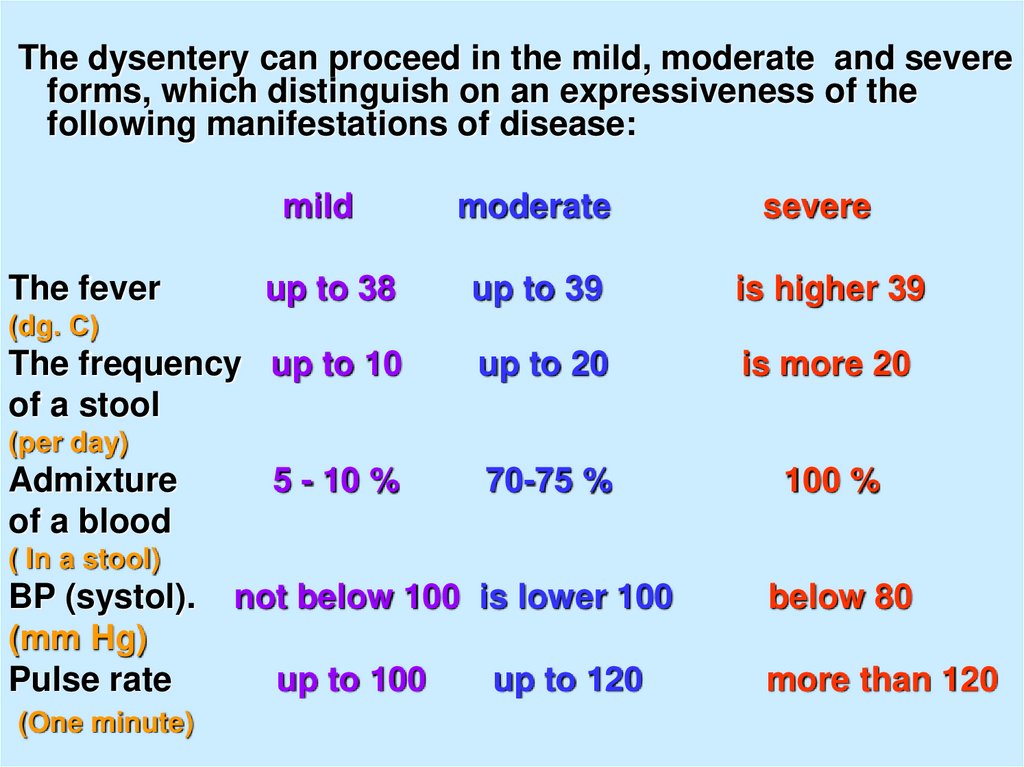
The dysentery can proceed in the mild, moderate and severeforms, which distinguish on an expressiveness of the
following manifestations of disease:
mild
The fever
moderate
severe
up to 38
up to 39
is higher 39
The frequency up to 10
of a stool
up to 20
is more 20
70-75 %
100 %
(dg. С)
(per day)
Admixture
of a blood
5 - 10 %
( In a stool)
BP (systol).
(mm Hg)
Pulse rate
(One minute)
not below 100 is lower 100
up to 100
up to 120
below 80
more than 120
33.
34.
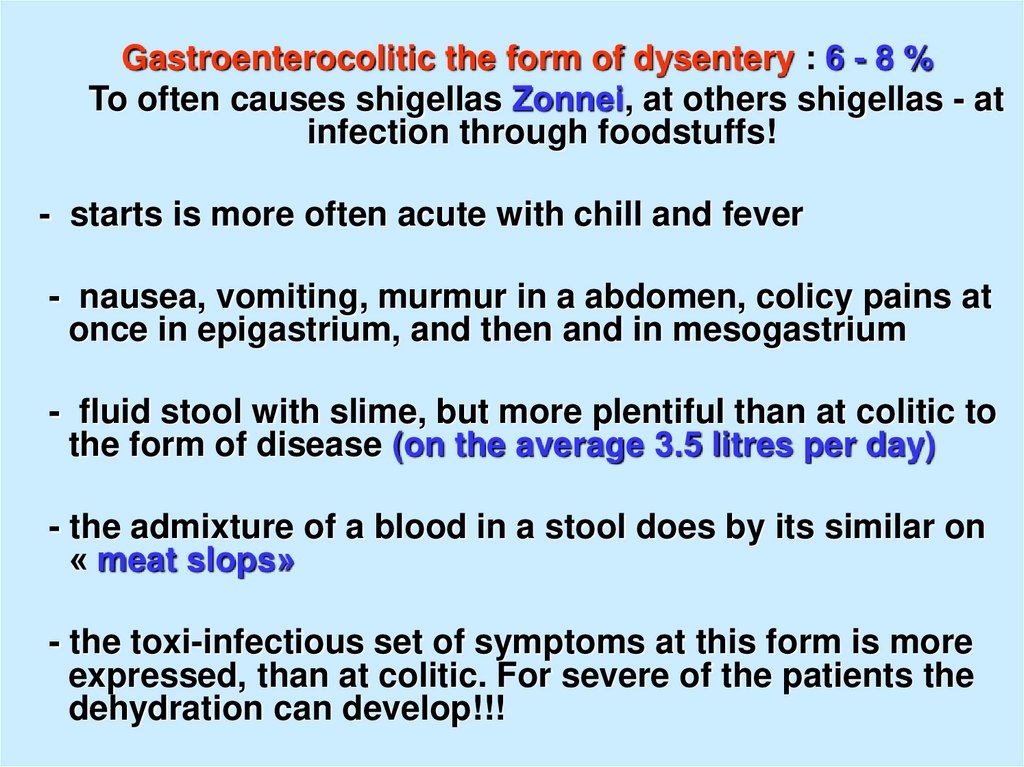
Gastroenterocolitic the form of dysentery : 6 - 8 %To often causes shigellas Zonnei, at others shigellas - at
infection through foodstuffs!
- starts is more often acute with chill and fever
- nausea, vomiting, murmur in a abdomen, colicy pains at
once in epigastrium, and then and in mesogastrium
- fluid stool with slime, but more plentiful than at colitic to
the form of disease (on the average 3.5 litres per day)
- the admixture of a blood in a stool does by its similar on
« meat slops»
- the toxi-infectious set of symptoms at this form is more
expressed, than at colitic. For severe of the patients the
dehydration can develop!!!
35.
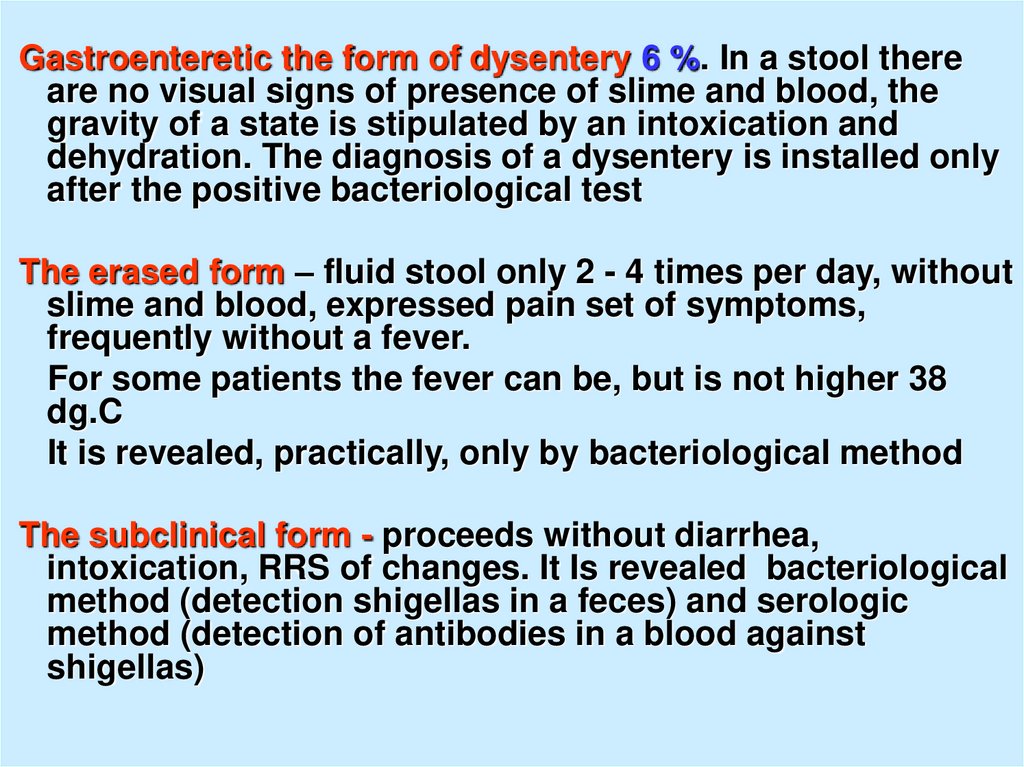
Gastroenteretic the form of dysentery 6 %. In a stool thereare no visual signs of presence of slime and blood, the
gravity of a state is stipulated by an intoxication and
dehydration. The diagnosis of a dysentery is installed only
after the positive bacteriological test
The erased form – fluid stool only 2 - 4 times per day, without
slime and blood, expressed pain set of symptoms,
frequently without a fever.
For some patients the fever can be, but is not higher 38
dg.C
It is revealed, practically, only by bacteriological method
The subclinical form - proceeds without diarrhea,
intoxication, RRS of changes. It Is revealed bacteriological
method (detection shigellas in a feces) and serologic
method (detection of antibodies in a blood against
shigellas)
36.
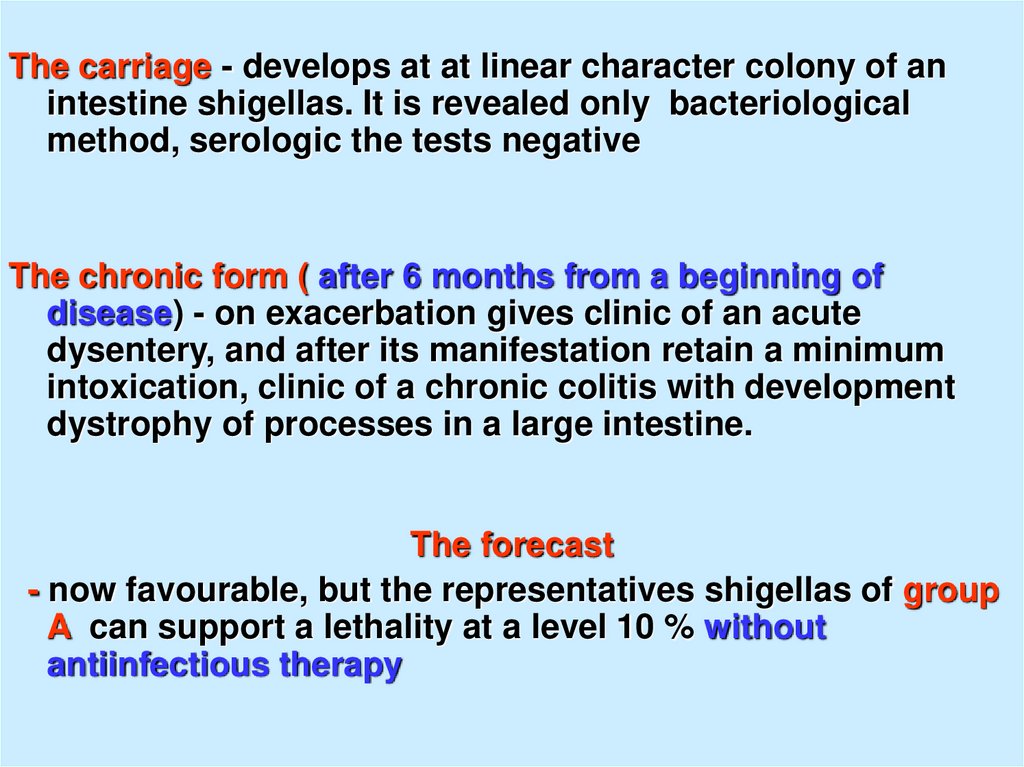
The carriage - develops at at linear character colony of anintestine shigellas. It is revealed only bacteriological
method, serologic the tests negative
The chronic form ( after 6 months from a beginning of
disease) - on exacerbation gives clinic of an acute
dysentery, and after its manifestation retain a minimum
intoxication, clinic of a chronic colitis with development
dystrophy of processes in a large intestine.
The forecast
- now favourable, but the representatives shigellas of group
A can support a lethality at a level 10 % without
antiinfectious therapy
37.
38.
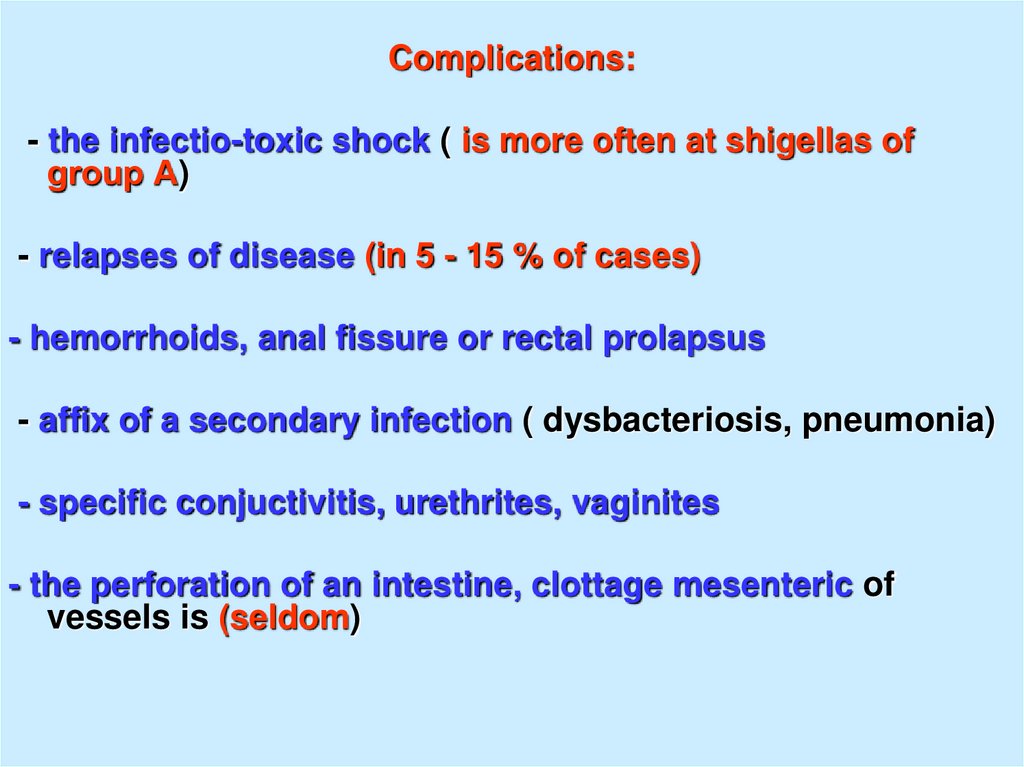
Complications:- the infectio-toxic shock ( is more often at shigellas of
group А)
- relapses of disease (in 5 - 15 % of cases)
- hemorrhoids, anal fissure or rectal prolapsus
- affix of a secondary infection ( dysbacteriosis, pneumonia)
- specific conjuctivitis, urethrites, vaginites
- the perforation of an intestine, clottage mesenteric of
vessels is (seldom)
39.
40.
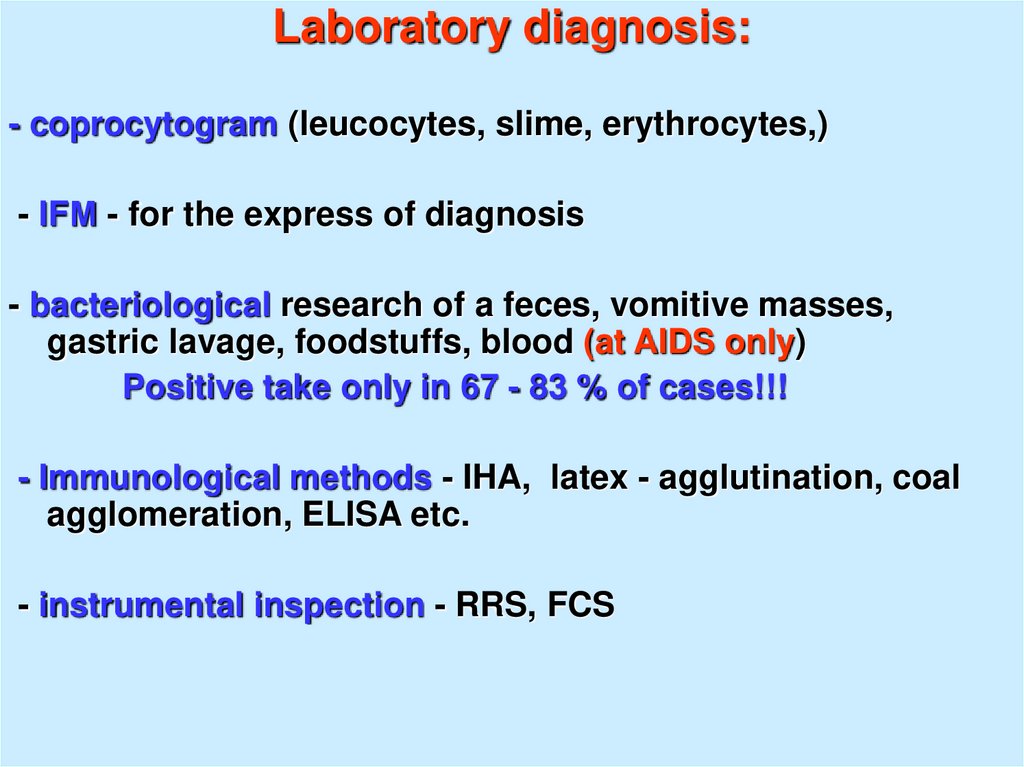
Laboratory diagnosis:- coprocytogram (leucocytes, slime, erythrocytes,)
- IFМ - for the express of diagnosis
- bacteriological research of a feces, vomitive masses,
gastric lavage, foodstuffs, blood (at AIDS only)
Positive take only in 67 - 83 % of cases!!!
- Immunological methods - IHA, latex - agglutination, coal
agglomeration, ELISA etc.
- instrumental inspection - RRS, FCS
41. Shigella Infections. Fecal leukocytes (shigellosis) (methylene blue stain). The presence of fecal leukocytes suggests a
bacterial diarrhea, thoughnot specific for Shigella infection.
42.
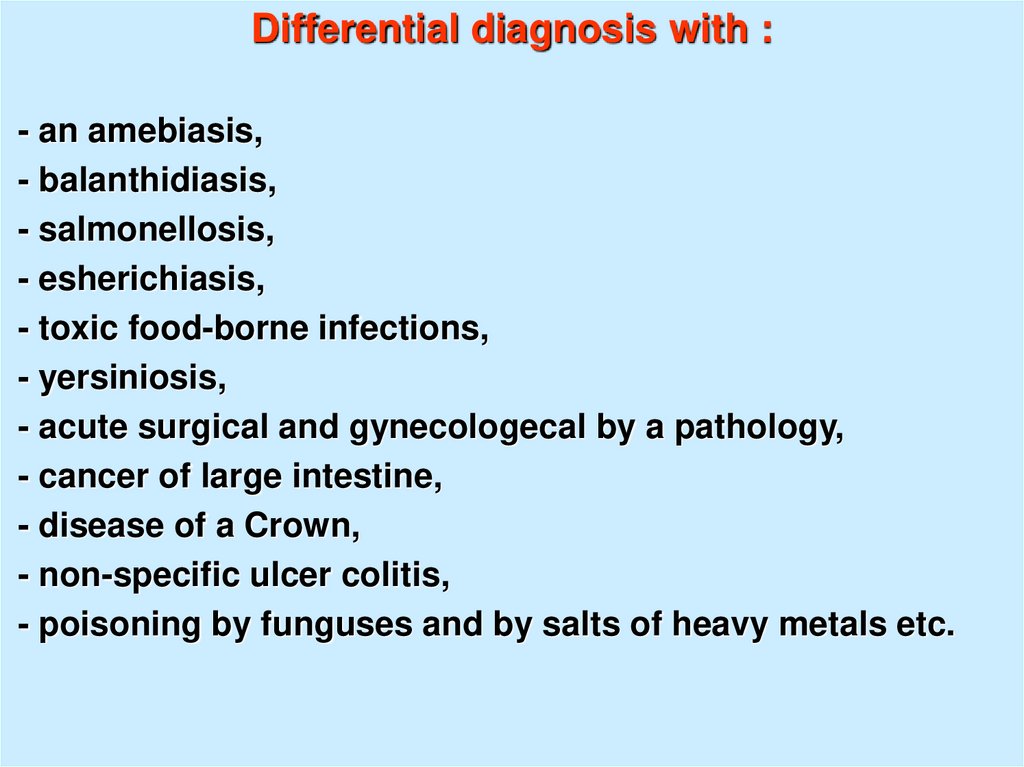
Differential diagnosis with :- an amebiasis,
- balanthidiasis,
- salmonellosis,
- esherichiasis,
- toxic food-borne infections,
- yersiniosis,
- acute surgical and gynecologecal by a pathology,
- cancer of large intestine,
- disease of a Crown,
- non-specific ulcer colitis,
- poisoning by funguses and by salts of heavy metals etc.
43.
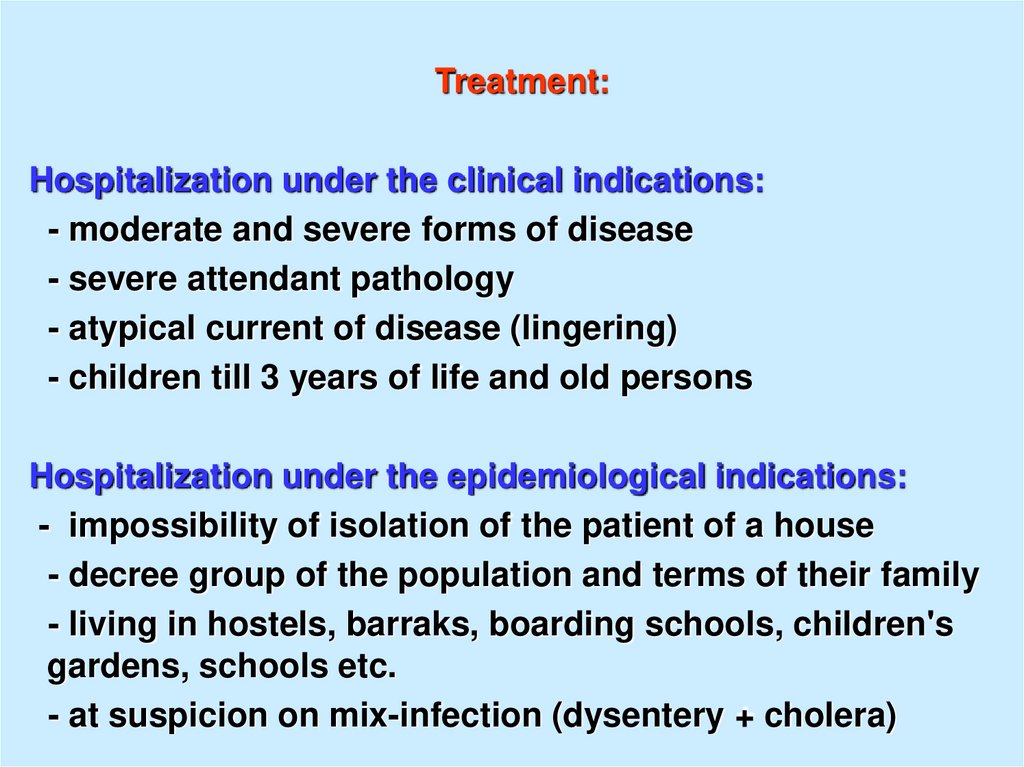
Treatment:Hospitalization under the clinical indications:
- moderate and severe forms of disease
- severe attendant pathology
- atypical current of disease (lingering)
- children till 3 years of life and old persons
Hospitalization under the epidemiological indications:
- impossibility of isolation of the patient of a house
- decree group of the population and terms of their family
- living in hostels, barraks, boarding schools, children's
gardens, schools etc.
- at suspicion on mix-infection (dysentery + cholera)
44.
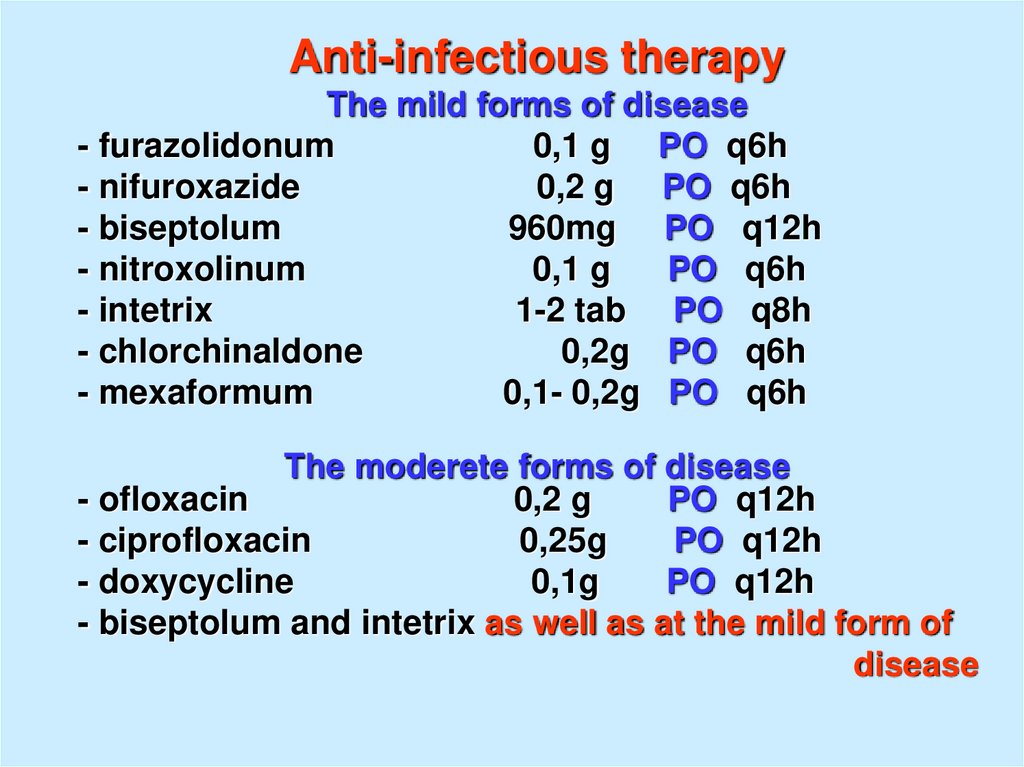
Anti-infectious therapyThe mild forms of disease
- furazolidonum
0,1 g PO q6h
- nifuroxazide
0,2 g PO q6h
- biseptolum
960mg PO q12h
- nitroxolinum
0,1 g
PO q6h
- intetrix
1-2 tab PO q8h
- chlorchinaldone
0,2g PO q6h
- mexaformum
0,1- 0,2g PO q6h
The moderete forms of disease
- ofloxacin
0,2 g
PO q12h
- ciprofloxacin
0,25g
PO q12h
- doxycycline
0,1g
PO q12h
- biseptolum and intetrix as well as at the mild form of
disease
45.
The severe forms of disease- ofloxacin
0,4 g
PO q12h
- ciprofloxacin
0,5 g
PO q12h
- ampicillinum
0,5 – 1,0 g
PO q4h
Introduction IM or IV and combination with : gentamicin,
kanamycinum, polymyxin М) sometimes is required
At the expressed hemocolitis - salazopyridazinum or
salazodimethoxinum for 1 g PO q12h.
- detoxication therapy
- rehydration therapy
- immunocorrection therapy
- antidiarrhea drugs (loperamide, gluconate of calcium)
- treatment dysbacteriosis (after research of a feces on
dysbacteriosis )
- symptomatic therapy (spasmolytics, antipyretics)
46.
47.
- at a chronic dysentery - biological preparations,stimulators of immunity and reparation mucous,
lactulose etc.
Prophylaxis of a dysentery:
- keeping personal, alimentary and hydrous hygiene,
disinsection (destroy of the fly, cockroaches)
- registration of all patients and carriers and them
sanitation
- planned inspection decree of groups of the population
and unplanned at any episode of a diarrhea
- regular current disinfection in the closed collectives of
subjects of use (toy, pots etc.)
- on all patients and carriers the emergency notice in SES
( sanitarno – epidemiologic station ) is referred and
isolation of the persons (house or in a hospital)
48.
The pathogenic mechanism that underlies thesepathological manifestations is diagrammed in Figure 22-3.
This cartoon incorporates experimental observations from
tissue cultures and from animal models of shigellosis such
as rabbit ligated ileal loops injected with virulent
organisms. In the latter model, Shigella infection is initiated
at the membranous (M) cells that are associated with
macroscopic lymphoid follicles (Peyer's patches). Biopsy
studies in rhesus monkeys suggest that shigellae also
infect microscopic lymphoid follicles of the primate colon.
During the early stages of infection, bacteria are
transcytosed through the M cells into the subepithelial
space. In the subepithelial space, the organisms are
phagocytosed by resident macrophages. However, virulent
shigellae are not killed and digested in the macrophage
phagolysome. The bacteria lyse the phagosome and
initiate apoptosis (programmed cell death). During this
process, the infected macrophage releases the
inflammatory cytokine IL-1, which elicits infiltration of
PMN.



 medicine
medicine